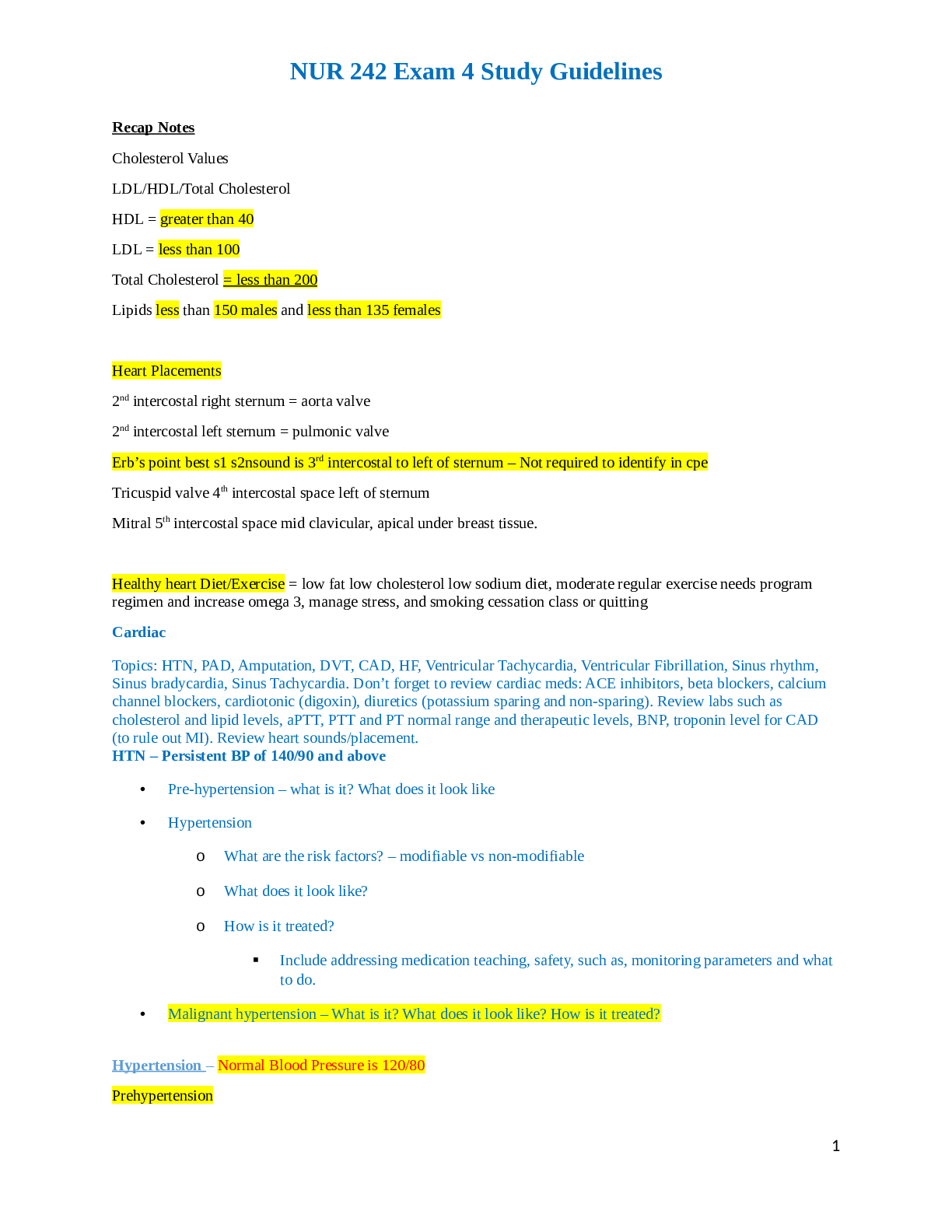
Recap Notes
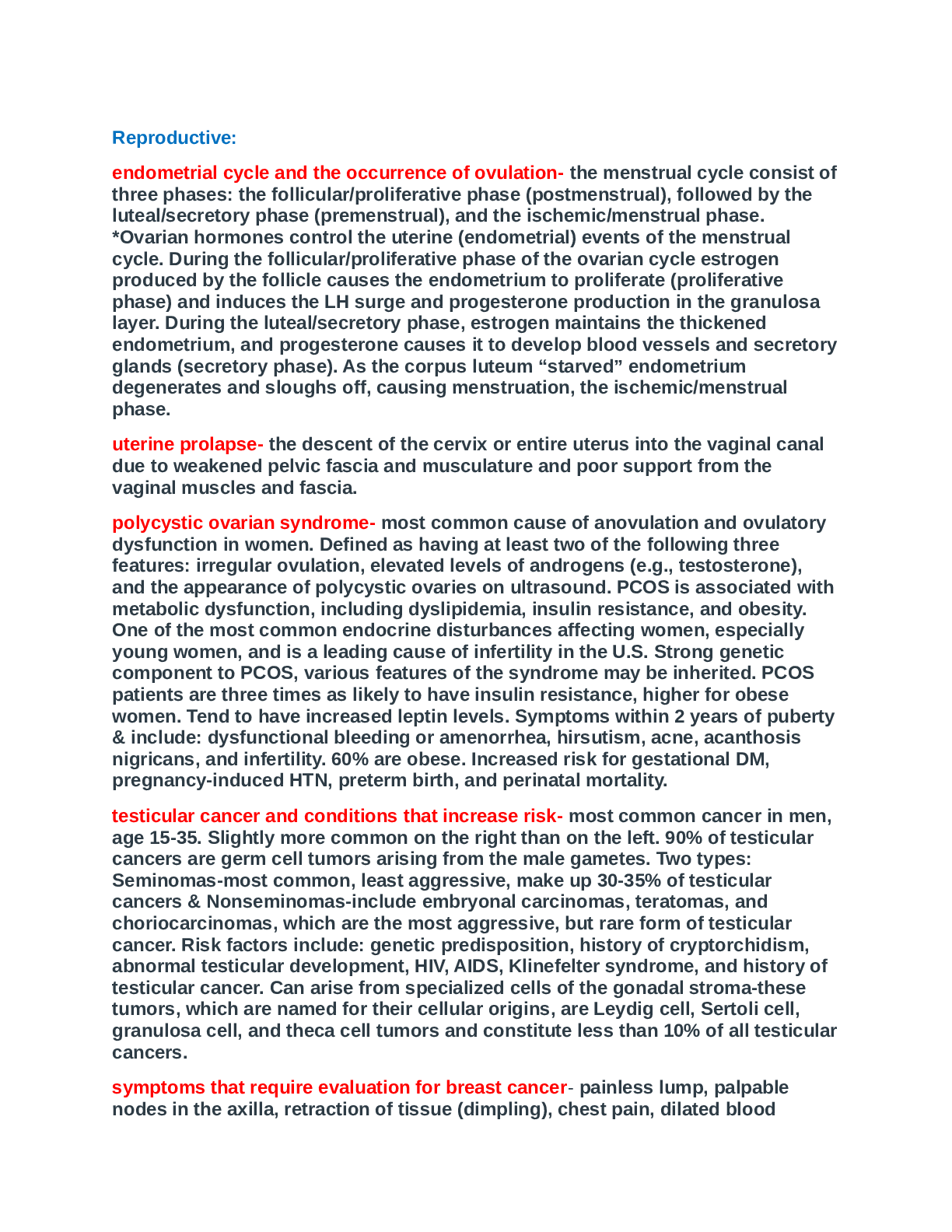
Cholesterol Values LDL/HDL/Total Cholesterol HDL = greater than 40
LDL = less than 100
Total Cholesterol = less than 200
Lipids less than 150 males and less than 135 females
Heart Placements
2nd int
...
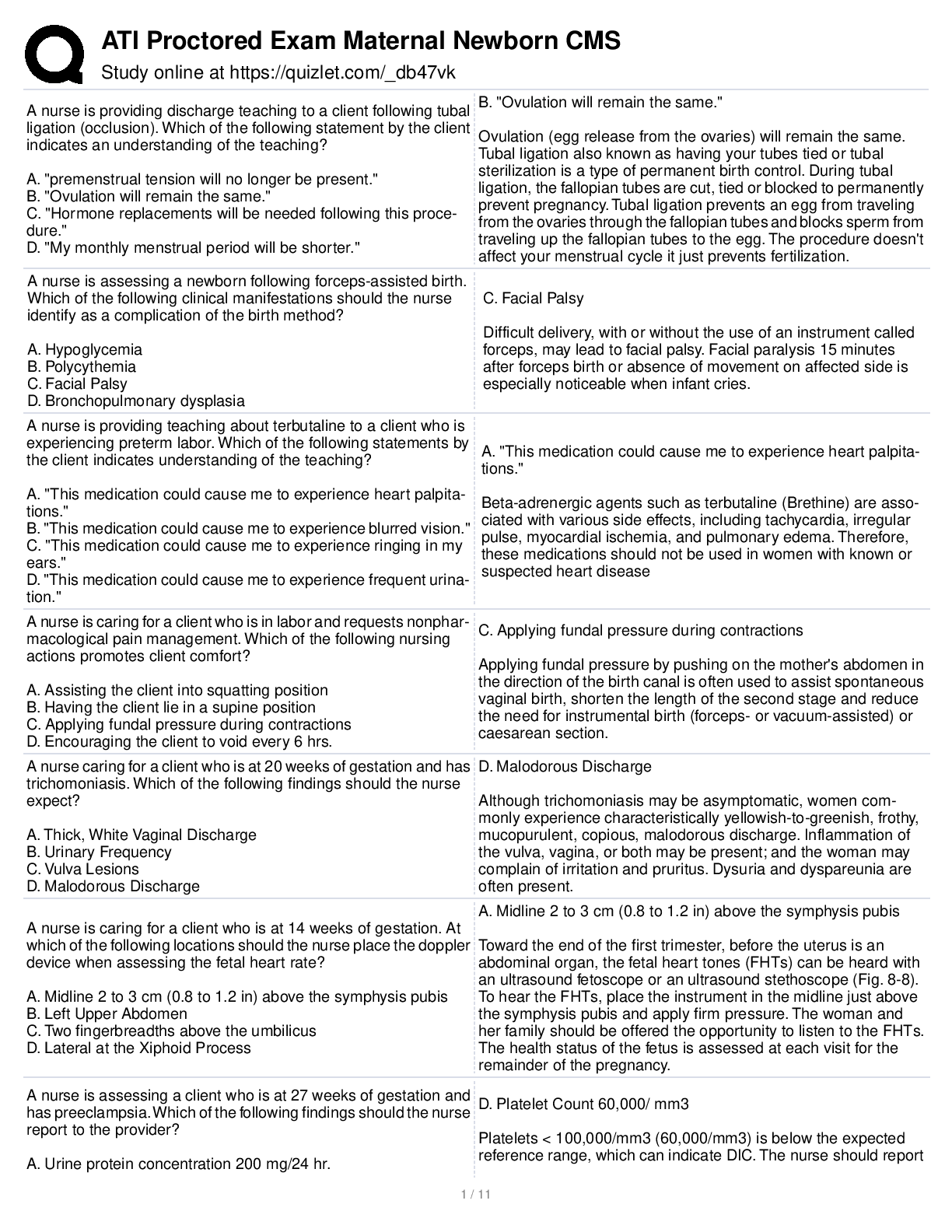
Recap Notes
Cholesterol Values LDL/HDL/Total Cholesterol HDL = greater than 40
LDL = less than 100
Total Cholesterol = less than 200
Lipids less than 150 males and less than 135 females
Heart Placements
2nd intercostal right sternum = aorta valve 2nd intercostal left sternum = pulmonic valve
Erb’s point best s1 s2nsound is 3rd intercostal to left of sternum – Not required to identify in cpe Tricuspid valve 4th intercostal space left of sternum
Mitral 5th intercostal space mid clavicular, apical under breast tissue.
Healthy heart Diet/Exercise = low fat low cholesterol low sodium diet, moderate regular exercise needs program regimen and increase omega 3, manage stress, and smoking cessation class or quitting
Cardiac
Topics: HTN, PAD, Amputation, DVT, CAD, HF, Ventricular Tachycardia, Ventricular Fibrillation, Sinus rhythm, Sinus bradycardia, Sinus Tachycardia. Don’t forget to review cardiac meds: ACE inhibitors, beta blockers, calcium channel blockers, cardiotonic (digoxin), diuretics (potassium sparing and non-sparing). Review labs such as cholesterol and lipid levels, aPTT, PTT and PT normal range and therapeutic levels, BNP, troponin level for CAD (to rule out MI). Review heart sounds/placement.
HTN – Persistent BP of 140/90 and above
• Pre-hypertension – what is it? What does it look like
• Hypertension
o What are the risk factors? – modifiable vs non-modifiable
o What does it look like?
o How is it treated?
▪ Include addressing medication teaching, safety, such as, monitoring parameters and what to do.
• Malignant hypertension – What is it? What does it look like? How is it treated?
Hypertension – Normal Blood Pressure is 120/80 Prehypertension
• 121-139 (systolic)
• 81-89 (diastolic)
• Gets worse over time Hypertension
• Persistent elevation of systolic or diastolic – NEEDS MORE THAN ONE READING TO DIAGNOSE needs a trend.
• What is the current standard???
• 140 systolic
• 90 diastolic Type
• Primary (essential) – no obvious medical cause
• Secondary - caused by other conditions that affect the kidneys, arteries, heart or endocrine system
• Isolated systolic - caused by other underlying conditions, such as a leaky heart valve, or hyperthyroidism)
• Refractory - resistant high blood pressure despite treatment regimen
• Malignant - a sudden and rapid development of extremely high blood pressure with diastolic typically above 130
Pathophysiology of Hypertension
• Primary (essential) hypertension
– persistently elevated vascular resistance
• Secondary hypertension
– Renal and adrenal gland diseases
– Medications and foods
– Acute stress
Assessment
• More common in African-American
• Increases with age
• More common in men in early age
• Women after menopause
• Pregnancy
• Sometimes no symptoms until pt. comes in with stroke, MI, or seizures. Manifestations
• Early stages—none
• Progressive stages
➢ Headache
➢ Fatigue and dizziness
Syncope
➢ Palpitations
➢ Flushing
➢ Blurred vision
➢ Epistaxis
• Syncope
• Postural hypotension
• Normal response when standing
• Syncopal response when standing
• Syncope management
Complications of Hypertension
➢ MI
➢ Stroke
➢ Atherosclerosis
➢ *Nephropathy
➢ PVD (PAD)
➢ Aortic aneurysms
➢ Heart Failure
➢ Hypertensive crisis
Hypertensive Crisis/Malignant Hypertension
• Severe increase in B/P (diastolic > 130)
• May lead to stroke
• Organ damage
• May develop to left ventricular failure
Signs and Symptoms- that are life threatening.
• Restlessness
• LOC changes
• Seizures
• Blurred vision/Visual changes.
• Dizziness
• Severe Headache
• Agitation
• N/V
• Renal insufficiency
• Hemolytic anemia
• Left ventricular failure (LVF)
• Pulmonary Edema (PE)
• Pt can come in comatose
Note Usually these are the patients that end up in ICU and need POTENT anti-hypertensive medications IV.
Medical Management/Treatment
• Revolves around 3 drug regimen:
➢ Diuretics – decreases volume load—Need to monitor potassium levels hyper/hypokalemia monitoring is essential.
Interventions
➢ Beta blockers - by blocking the effect of norepinephrine and epinephrine, beta blockers reduce heart rate and dilate blood vessels; might not be tolerated by persons with asthma, congestive heart failure, depression or underlying fatigue
➢ ACE inhibitors – inhibit conversion of Angiotensin I to Angeiotensin II, therefore serves purpose
of sodium excretion in urine
➢ Ca++ channel blockers - block voltage-gated calcium channels in blood vessels causing less muscle contraction therefore increasing arterial diameter (usually given to people who cannot tolerate beta blockers, people with asthma, or depression slows heart rate and dilates blood vessels.)
➢ Life style modification changes such as the Dash diet. Low sodium low fat, diet
➢ Teach about potassium and salt substitutes
• Weight reduction
• Lifestyle modifications
• Dietary changes
• DASH diet - Dietary Approaches to Stop Hypertension; low sodium, saturated fat, cholesterol and total fat
• Client teaching
✓ Exercise (helps increase HDL)
✓ Alcohol restriction
✓ Caffeine restriction
✓ Relaxation techniques
✓ Smoking cessation
✓ Potassium supplementation
✓ Pharmacologic interventions
PVD/PAD (Peripheral vascular disorder/Peripheral arterial disorder= They are the same. – Occlusion of peripheral arteries - insufficient blood supply
• What are the risk factors?
• What does it look like?
• How is it treated? (medical and surgical – revascularization)
• Post op care for fem-pop bypass surgery?
• What are the complications?
• Amputation
• Post op care
Peripheral Arterial Disease and Deep Vein Thrombosis
Overview
• Peripheral vascular disease (PVD) commonly referred to as peripheral arterial disease (PAD) or peripheral artery occlusive disease (PAOD), refers to the obstruction of large arteries not within the coronary, aortic arch, or brain
Six Classifications of PVD/PAD
• Mild Claudication- same as moderate, pain that occurs with walking and subsides at rest.
• Moderate Claudication pain that occurs with walking and subsides at rest.
• Severe Claudication- Pain at rest.
• Ischemic Pain at rest
• Minor Tissue Loss
• Major Tissue loss
With intermittent claudication an exercise program is necessary
Assessment
Signs and Symptoms
• Claudication - pain, weakness, numbness, or cramping in muscles due to decreased blood flow
• Rest Pain (if it has progressed)
• Decreased Pulses
• Sores, wounds, or ulcers that heal slowly or not at all
• Noticeable change in color (extremities) (blueness or paleness) or temperature (coolness) when compared to the other limb
• Diminished hair and nail growth on affected limb and digits.
• Skin is shiny and flakey
• Sluggish capillary refill
Signs and Symptoms- symptoms are increased when extremities elevated or legs crossed, they are intensified. Medical Management
• Promote arterial flow
• Trental – reduces viscosity
• Pletal – dilates arteries and reduces blood clotting ability
• Reduce risk
• Smoking cessation
• Control co-morbid diseases
• Exercise - walking
• Prevent injury
Surgical Management
• Surgical management (revascularization)
– Endovascular
• Angioplasty
• Atherectomy
• Stent placement
– Arterial bypass and reconstruction
Bypass surgery need to conduct neurovascular checks of that extremity make sure circulation is adequate and to see if nerve damage/compression.
Neurovascular checks---Check temperature, pulse, sensation, pins, needles, wiggle toes to see if there’s pain with movement, and monitor for swelling like compartment syndrome
Amputation- It is done when there is tissue damage or tissue loss can be any part of extremity. Amputation Preoperative Diagnoses
• Risk for Delayed Surgical Recovery related to preexisting health condition
• Anxiety related to impending loss of limb
• Chronic Pain related to ischemia of the limb
• Deficient Knowledge related to expectations after surgery
•
Amputation Postoperative Diagnoses
• Anxiety related to phantom sensation
• Ineffective Coping related to reaction to change in body image
• Deficient Knowledge related to gait training, care of the stump, care of the prosthesis
Amputation
• Preoperative care
– Assessment
– Anxiety
– Acute Pain
• Postoperative Care –
– Edema
– Stump care- how to dress and shape stump for prosthetic fitting, will require rehab, gait training with prosthetic.
– Pain and Phantom Pain
• – 24hrs post op we need to take care of the stump, stump should be elevated on pillows, reduce flexion, contraction of hip. Lower leg in prone position every 3-4 hours for 20 mins to reduce flexion contractions.
• After 24hours need to lower stump to prone position to promote circulation.
Planning & Intervention
• Positioning of clients to promote circulation – lower extremities in dependent position (below heart level)
• Maintain skin integrity Client Teaching
• Smoking Cessation
• Exercise program
• Prevention of injury, especially foot care
• Teach not to cross legs at the knees (PVD in genereal).
• Watch for edema and report to primary care physician
• Complications of taking antiplatelet and/or anticoagulant medications
• Evaluation
• Client states an understanding of lifestyle changes necessary to improve circulation
• Dietary changes such as low-fat diet
• Client can demonstrate and verbalizes importance of proper foot care
• Client can demonstrate and verbalizes importance of proper skin care Complications
• Usually if you have PVD you have CAD
• MI
• Carotid Stenosis leading to stroke
• Renal disease
• AFIB
Assessment & Diagnostic Tests
– Assess history
– Physical examination
• Peripheral pulses
• Skin integrity, color, and temperature
• Hair distribution
• Capillary refill
– Doppler ultrasonography
– Arteriography
Acute Arterial Occlusion
• Etiology and pathophysiology
– Trauma, embolism, thrombosis
• Clinical manifestations (six Ps)
– Pain, pulselessness, poikilothermic, pallor, paresthesias, paralysis
• Outcome management
– Surgical embolectomy
Arterial Ulcers
• Location
– Present almost anywhere on the leg; usually distal to impaired arterial supply, between toes or tips of toes, over phalangeal heads, around lateral malleolus, or at sites subjected to trauma or rubbing of footwear
• Characteristics
– Wound margins are even, sharply demarcated, and punched out
– Wound may be superficial or deep
– Wound beds may be pale, gray or yellow with no evidence of new tissue growth; necrosis or cellulitis may be present; commonly accompanied by dry necrotic eschar and exposed tendons
– Have minimum exudate.
– Periwound tissue may appear blanched or purpuric and is often shiny and tight; loss of hair at ankle or foot
– Usually very painful, often relieved by dependent leg position and aggravated by elevation.
• Management - revascularization
Buerger’s & Raynaud’s – circulation of extremities (particularly toes and fingers)
• What are they?
• What do they look like?
• How are they treated?
Buergers Disease
What is it?
• Buerger's disease (thromboangiitis obliterans) is a rare disease of the Occlusion of the arteries and veins in the distal portions of the arms and legs.
• Cause is unknown.
• Strong Association with tobacco smoking. What does it look like?
• Buerger's disease usually first shows in the hands and feet and may eventually affect larger areas of your arms and legs.
• S/S include ulceration/gangrene in digits, decreased pulses, cool extremities, red/cyanotic of extremities in dependent position, and claudication of arch of foot.
How is it treated?
• Smoking cessation usually arrests the disease process. Stop smoking = end results. What are the complications?
• Gangrene resulting in amputation.
Raynaud’s Disease
What is it?
• Vasospasm of arteries/arterioles of upper and lower extremities.
• Superficial skin vessels in fingers and toes constrict in response to aggravated with cold temperatures and stress.
• More common in women than men.
• Cause is unknown.
What does it look like?
• Blanching of the digits followed by cyanosis, cool painful, and some swelling noted.
• Numb, prickly feeling or stinging pain upon warming or stress relief How is it treated?
• Dressing for the cold in layers and wearing gloves or heavy socks usually are effective in dealing with mild symptoms of Raynaud's.
• More severe forms are treated with drugs to dilate vessels and promote circulation: calcium channel blockers, alpha blockers, vasodilators.
What are the complications? If severe,
• can cause deformities of toes and fingers
• gangrene leading to amputation.
DVT – blood clot in deep vein
• What are the risk factors?
• What does it look like?
• How is it treated?
• Complication?
DVT
• DVT is a blood clot that forms in a vein deep in the body
• Most often occurs in the deep veins of the legs, either above the knee or below it
• The blood clot or part of it can break free (called embolism) and become lodged in the blood vessels of the lung, causing pulmonary embolism (PE)
Causes
• Damage occurs to a vein's inner lining
• Blood flow is sluggish or slow
• The patient’s blood is thicker or more likely to clot than normal
Risks Factors for DVT
• Illness, injury or long travel that causes prolonged immobility increases the risk of a DVT
• Age >40 years (VTE risk increases with advancing age)
– Venous thromboembolism (VTE) is a disease that includes DVT and pulmonary embolism (PE).
• Birth control pills and hormone replacement therapy
• Cancer and its treatment
• Major surgery (example: abdomen, pelvis, or hip or knee replacement)
• Obesity
• Previous DVT or PE
• A family history of blood clots
• Certain heart problems
• Varicose veins
• Disorders or factors that make your blood thicker or more likely to clot than normal
Diagnosing DVT
• Diagnosis may begin by confirming that the patient has risk factors for DVT
• Medical history - general health, previous illnesses, including past episodes of DVT, medications, recent activities, recent surgery
• Physical examination
• Diagnostic tests
– Ultrasound
– D-dimer test. This test measures a substance in the blood that's released when a blood clot dissolves. If the test shows high levels of the substance, you may have a deep vein blood clot. If your test is normal and you have few risk factors, DVT isn't likely.
– Venography (ve-NOG-ra-fee). This test is used if ultrasound doesn't provide a clear diagnosis. Dye is injected into a vein, and then an x-ray is taken of the leg. The dye makes the vein visible on the x ray. The x ray will show whether blood flow is slow in the vein. This may indicate a blood clot.
Treating DVT
• Treatment of DVT can help reduce the risk of complications, such as PE
• The main goals in treating DVT are to help:
– Stop the clot from getting larger
– Reduce the chance of having another clot develop
– Prevent the clot from breaking off in the vein and moving to your lungs The best treatment is prevention.
Treating DVT
• Drugs
– Anticoagulants (heparin and Coumadin)
– Thrombolytic agents (drugs used to dissolve blood clots) not usual
• Planning and Interventions
– Elevate the affected leg whenever possible
– Apply heat to relieve pain and reduce swelling
– Wear compression stockings or support hose
– Avoid long periods of immobility Preventing DVT
– Ambulation as soon as possible after surgery or illness
– SCDs – sequential compression devices
– Low molecular heparin as prophylaxis
Summary
• DVT is a blood clot that forms in a vein deep in the body
• The clot or part of it may break off and travel to the lung
• Many conditions may increase risk for deep vein clots
• The more risk factors a person has, the greater the chances of developing DVT
• Not all people with DVT have symptoms
• The main goals in treating DVT are to stop the clot from getting bigger, to decrease the chance of having another clot, and to stop the clot from breaking off in the vein and traveling to your lungs
• Medicines are used to treat DVT and prevent DVT
CAD – fatty deposits (atherosclerosis) in heart (coronary) arteries
• Risk factors?
• What does it look like?
• How is it treated?
• Complication?
• Cardiac Catheterization
• Patient preparation (education)
• Post procedure care
• Coronary Artery Bypass Graft (CABG)
• Post op care
Coronary Artery Disease (AKA Coronary Vascular Disease)
The function of the heart is to circulate blood throughout the body by
• Pumping blood through the lungs to remove carbon dioxide and refresh the blood with oxygen
• The oxygenated blood is pumped to the body to provide oxygen and nutrients and to remove waste products.
• The coronary arteries are the blood vessels that supply nutrients and oxygen to the heart muscle.
•
Blood Supply to the Heart
• 2 coronary arteries branch from the main aorta just above the aortic valve. “No larger than drinking straws, they divide and encircle the heart to cover its surface with a lacy network resembles a slightly crooked crown (coronary comes from the Latin coronarius, belonging to a crown or wreath). They carry out about 130 gallons of blood through the heart muscle daily.” (Clark, 119)
•
Coronary Artery Disease
• Coronary artery disease is one of the most common and serious effects of aging. Fatty deposits build up in blood vessel walls and narrow the passageway for the movement of blood. The resulting condition, called atherosclerosis often leads to eventual blockage of the coronary arteries and a “heart attack”. What are signs and symptoms of a heart attack?
#1 killer Atherosclerosis
• can, and does, occur in almost any artery in the body. But in the heart it’s effects can be crucial. “The body
depends on a strong pumping heart to circulate life-giving blood, and this includes the heart muscle itself. If the coronary arteries become blocked, the cardiac muscle begins to fail, and so the blood circulation decreases, which includes the circulation to the heart muscle itself.” (Thibodeau, 494)
Causes
• High Blood Cholesterol
• High Blood Pressure
• Smoking
• Obesity
• Lack of Physical Activity
Treatment
• Many people are able to manage coronary artery disease with lifestyle changes and medications.
• Other people with severe coronary artery disease may need angioplasty or surgery
Catherization no bending legs for 6 hrs.to prevent bleeding or hematoma usually go home with antiacoagulants for 6 months.
Cabg- major thoracic surgery. Mediastinal chest tubes, aggressive pulmonary hygiene early ambulation and cardiac rehab program, heart healthy diet, and smoking cessation.
Medical Management
– Aspirin - anticoagulant
– Nitroglycerin - dilates narrowed coronary blood vessels
– Beta-blockers - reduce heart rate and blood pressure.
– Cholesterol-lowering medications - reduce the formation of blockages in heart arteries.
– ACE inhibitors (angiotensin-converting enzyme inhibitors) – lower blood pressure and may improve heart function after heart attacks.
– Calcium channel blockers – dilate coronary arteries and reduce high blood pressure
– Omega-3 fatty acids and vitamins - may reduce heart disease risk factors such as high cholesterol.
–
Heart Failure – heart cannot pump enough blood to meet the metabolic demands of body
• Risk factors
• What does it look like?
• Right and left sided heart failure
• How is it treated? (include pacemaker post op care)
• Patient education
• Complications?
• Pulmonary Edema – signs and symptoms and management
Heart Failure
Overview
• A physiologic state in which the heart cannot pump enough blood to meet the metabolic needs of the body
• Because heart failure causes vascular congestion, it is often called congestive heart failure
• Inability of heart to meet metabolic needs of the body
• Diminished PO2
• Results in
– Right sided failure - peripheral edema
– Left sided failure - lung congestion
Frank- Starling Law
– The heart muscle is like a rubber band. The greater the stretch, the greater the re-coil. Except at some point the rubber band becomes over stretched and can not contract effectively.
Risk Factors
• Myocarditis
• Congenital heart defects heart arrhythmias
• Other diseases - diabetes, severe anemia, hyperthyroidism, hypothyroidism, emphysema, lupus, hemochromatosis
Clinical Manifestations – Right Sided Failure
• Fluid backs up into abdomen, legs, feet
• Dependant edema
• JVD
• Abdominal distention
• Hepato and splenomegaly
• Anorexia/Nausea
• Weight gain
• Nocturnal diuresis
• Swelling of fingers and hands
• Increased B/P due to increased volume or decreased B/P due to pump failure
• Puffy hands, tree trunks, cyanotic
• fatigue
Clinical Manifestations – Left Sided Failure
• Pulmonary congestion
• Dyspnea
• Tachypnea
• Crackles
• Dry, hacking cough
• Paroxysmal nocturnal dyspnea
• Increased B/P due to increased fluid volume or decreased B/P due to pump failure
Diagnostics Tests
• Blood tests - brain natriuretic peptide (BNP) hormone in the blood – elevates in heart failure
• Chest X-ray
• Electrocardiogram
• Echocardiogram
• Ejection fraction
• Stress test
• Cardiac computerized tomography (CT) or magnetic resonance imaging (MRI)
• Coronary catheterization (angiogram) Medical Management
• Reduce Myocardial Workload
• Reduce Fluid Retention
• Improve Ventricular Pump Performance
• Supplement Oxygen
• Control Dysrhythmias
• Angiotensin-converting enzyme (ACE) inhibitors
• Angiotensin II receptor blockers
• Digoxin (Lanoxin)
• Beta blockers
• Diuretics
• Aldosterone antagonists
•
•
Surgical Management
• Coronary bypass surgery
• Heart valve repair or replacement
• Implantable cardioverter-defibrillators (ICDs)
• Cardiac resynchronization therapy (CRT) or biventricular pacing
– pacemaker sends timed electrical impulses to both of the left and right ventricles to pump in a more coordinated manner
• Heart pumps (left ventricular assist devices, or LVADs). These mechanical devices are implanted into the abdomen or chest and attached to a weakened heart to help it pump
• Heart transplant
• Pace make if there is a dysrhythmia.
•
Medical Management Pulmonary Edema
• High Fowlers
• Hi flow O2
• Morphine Sulfate
• No fluids
• Diuretics to reduce volume
• Digoxin to increase contractility
• Bronchodilators
• Vasodilators to decrease afterload
• Intubate prn---this is an emergency condition
Clinical Manifestations – Pulmonary Edema
• Blood tinged sputum
• Many of the same s/sx of Pulmonary Embolus
• Chest Pain
• SOB
• Tachypnea and tachycardia
• Anxiety
• Diaphoresis/clammy Nursing Diagnosis
• Decreased cardiac output
• Excess fluid volume
• Impaired gas exchange
• Ineffective tissue perfusion
• Risk for impaired skin integrity
• Anxiety
• Activity Intolerance
• Acute Confusion
•
Planning and Interventions
• Elevate Client’s Head
• Reduce Stress and Risk of Injury
• Monitor for reduced cardiac output
• Maintain adequate fluid balance
• Reduce myocardial workload
• Monitor for pulmonary edema
• Assess response to medical therapies
• Assess blood pressure - sitting and standing
• Monitor I&O’s
• Daily weights
• Measure abdominal girth and lower extremities
• Assess lung sounds
• Assess skin Client Teaching
• Instruct clients to call primary care provider if they lose or gain 2 to 3 pounds in 1 day or 5 to 7 pounds in one week
• Assess for edema
• Limit sodium intake – 2 gm
• Monitor blood pressure
• Modify activity - Balance Activity and Rest
• Adhere to prescribed medications
• Home Oxygen
• End-of-life care and heart failure
• heart failure may worsen to the point a heart transplant isn't an option
• Hospice care Evaluation
• Not smoking
• Controlling certain conditions, such as high blood pressure, high cholesterol and diabetes
• Staying physically active
• Eating healthy foods
• Maintaining a healthy weight
• Reducing and managing stress
Dysrhythmias
• Recognize rhythms: Normal Sinus Rhythm, Sinus Tachycardia, Sinus Bradycardia, V-tach, V-fib
• What are causes for the dysrhythmias?
• How is V-tach and V-Fib treated?
• What do we do about sinus tachycardia or bradycardia (when do we treat)?
Dysrhythmias
◆ Dysrhythmias are a deviation from normal cardiac rhythm. There are many causes of dysrhythmias: Cardiac disease
Electrolyte disturbances Myocardial infarction Respiratory disorders
Side effects of medications
Key Assessments
◆ Identify and interpret dysrhythmias
◆ Monitor level of consciousness
◆ Apical and peripheral pulses
◆ Respirations
◆ Blood pressure
◆ Oxygenation status
◆ Patient’s response to the dysrhythmia
◆ Syncope
◆ Chest pain
Planning and Implementation
◆ Clean skin and remove excess hair prior to attaching electrodes
◆ To verify rhythm, use 12-lead EKG
◆ Oxygen
◆ Peripheral IV access
◆ Institute safety measure
◆ BLS and ACLS
Diagnostic Assessment
◆ Electrocardiography
◆ Holter monitors
◆ Event monitors
◆ Electrophysiological study (EP)
Outcome Management
◆ Control or ablate dysrhythmia
◆ Dependent on type of dysrhythmia
◆ Increase cardiac output
Sinoatrial Node Dysrhythmias
◆ Disturbances in automaticity
Sinus tachycardia Sinus bradycardia Sinus dysrhythmia
◆ Etiology/risk factors
Physiological response Drug-induced Pathologic Cardiovascular disease
◆ Management – not treated unless symptomatic
Atrial Dysrhythmias Reentry of Impulses
◆ Types
Paroxysmal atrial tachycardia (PAT) – rate greater than 150 Atrial flutter
Atrial fibrillation
◆ Etiology/risk factors
Age
Heart disease
High blood pressure
Other chronic conditions – sleep apnea, hyperthyroidism Drinking alcohol – binge drinking
Family history
◆ Clinical manifestations: ECG appearance
◆ Outcome management – correct underlying cause, cardioversion, anticoagulation
Ventricular Dysrhythmias
◆ Types
Premature ventricular contractions Ventricular tachycardia Ventricular fibrillation
Torsades de pointes
◆ Etiology or risk factors
Generally, consequence of ischemic or structural heart disease or electrolyte deficiencies
◆ Clinical manifestations: ECG appearance
◆ Outcome management – ACLS protocol
Ventricular Dysrhythmias
◆ Types
Ventricular asystole Pulseless electrical activity
◆ Etiology or risk factors
◆ Clinical manifestations: ECG appearance
◆ Outcome management – ACLS protocol
Life Threatening Dysrhythmias Treatment
◆ Electrical therapy
Defibrillation and cardioversion
Automated external defibrillation (AED)
Automatic implantable cardioverter-defibrillator (AICD) Termination of resuscitation
Pacemaker methods
◆ Suppressing irritable foci – anti-arrhythmics, such as, procainamide, lidocaine, amiodarone
◆ Ablating conduction pathways
Dysrhythmias Nursing Diagnoses
◆ Decreased Cardiac Output
◆ Ineffective Health Maintenance
ECG, cardioversion, and medications Pacemaker and AICD care
◆ Ineffective Tissue Perfusion
◆ Activity Intolerance and Anxiety
Neuro – Remember patients with Stroke and Neuromuscular Disorders need an interdisciplinary team approach because of the “smorgasbord” of deficits.
Topics: seizures, Parkinson’s, Multiple Sclerosis, Stroke (CVA), TIA (RIND), cataract, retinal detachment, glaucoma, macular degeneration, Meinere’s disease, Migraine headache, Hearing loss (hearing aid)
Seizures – abnormal electrical signals in brain resulting in generalized or partial seizures
• What does it look like?
• Grand mal
• How do we treat it?
• Meds, patient education
• Safety
• What to do during a seizure?
• What is status epilepticus and how is it treated?
Seizures-Overview
• Seizures are disturbances in normal brain function resulting from abnormal electrical signals inside the brain
• Can cause loss of consciousness, uncontrolled body movements, changes in behaviors and sensation, and changes in the autonomic system
• Epilepsy is recurring seizures
• Seizures are classified as either partial or generalized
• based on how the abnormal brain activity begins
• In some cases, seizures can begin as partial and then become generalized.
Overview- Generalized Seizures Involve all of the Brain
• Absence seizures (also called petit mal)
• staring and subtle body movement, and can cause a brief loss of consciousness.
• Myoclonic seizures
• sudden jerks or twitches of arms and legs.
• Atonic seizures Also known as drop attacks
• loss of normal muscle tone and suddenly collapse or fall down
• Tonic-clonic seizures (also called grand mal). The most intense of all types of seizures
• loss of consciousness, body stiffening and shaking, and loss of bladder control.
Overview – Partial or Focal Seizures Abnormal activity in just one part of the brain.
• Simple partial seizures
• don't result in loss of consciousness
• may alter emotions or change the way things look, smell, feel, taste or sound
• may also result in involuntary jerking of part of the body, such as an arm or leg, and spontaneous sensory symptoms such as tingling, vertigo and flashing lights
• Complex partial seizures
• alter consciousness
• result in staring and non-purposeful movements — such as hand rubbing, twitching, chewing, swallowing or walking in circles
Risk Factors
• A family history
• Head injuries.
• Stroke and other vascular diseases
• Meningitis
• Lack of sleep, flashing lights, video games and prolonged television viewing may increase brain activity that may cause potential seizure activity
Complications
• Status epilepticus
• Give pam drugs, lorazepam, diazapam
• continuous seizure activity lasting more than five minutes
• or frequent recurrent seizures without regaining consciousness in between them
• an increased risk of permanent brain damage and death Medical Management Medication
• Most people with epilepsy can become seizure-free by using a single anti-epileptic drug
• May be able to discontinue seizure medication after several years
• Finding the right medication and dosage can be complex
• Prescribe a single drug at a relatively low dosage first increase the dosage gradually until seizures are well controlled
Assessment
• Men are slightly more at risk of developing epilepsy than are women.
• The onset of epilepsy is most common during early childhood and after age 65
• Dementia is a leading cause of epilepsy among older adults.
• High fevers in childhood can sometimes be associated with prolonged seizures and subsequent epilepsy later in life, particularly for those with a family history of epilepsy.
• Seizures during pregnancy pose dangers to both mother and baby, and certain anti-epileptic medications increase the risk of birth defects
• Most women with epilepsy can become pregnant and have a healthy baby - need to be carefully monitored throughout pregnancy, and medications may need to be adjusted
• Diagnostics Test
• Electroencephalogram (EEG)
• Computerized tomography (CT)
• Magnetic resonance imaging (MRI)
• Positron emission tomography (PET)
• use a small amount of low-dose radioactive material that's injected into a vein to help visualize active areas of the brain and detect abnormalities
• Single-photon emission computerized tomography (SPECT) -
• uses a small amount of low-dose radioactive material that's injected into a vein to create a detailed, 3-D map of the blood flow activity in the brain during seizures.
Clinical Manifestation
• Person with epilepsy will tend to have the same type of seizure each time, so the symptoms will be similar from episode to episode.
Planning & Intervention
• NURSING PRIORITIES
1. Prevent/control seizure activity.
2. Protect patient from injury.
3. Maintain airway/respiratory function.
4. Promote positive self-esteem.
5. Provide information about disease process, prognosis, and treatment needs.
Planning & Interventions During Seizure
• Position on side to prevent aspiration
• Clear secretions from mouth if necessary
• Put something soft under his or her head.
• Loosen tight neckwear.
• Don't try to put your fingers or anything else in the person's mouth
• Don't try to restrain someone having a seizure.
• Don't attempt to rouse the person by shouting at or shaking
• If the person is moving, clear away dangerous objects
• Reorient patient following seizure
• Document seizure activity and communicate to healthcare providers as appropriate. Include duration, objective observation about seizure behavior
Client Teaching
• lifestyle changes to reduce risk factors and protect self from injury
• Falling
• Drowning
• Car accidents – can drive once seizure free
• Take medications exactly as prescribed. Before switching to a generic version of your medication or taking other prescription medications, over-the-counter drugs or herbal remedies check with primary health care provider
• Never stop taking your medication without talking to your doctor.
• Notify your doctor immediately if new or increased feelings of depression, suicidal thoughts or unusual changes in mood or behaviors
• Notify your doctor immediately if new or increased feelings of depression, suicidal thoughts or unusual changes in mood or behaviors
• Get enough sleep - Sleep deprivation is a powerful trigger of seizures
• Wear a medical alert bracelet
• Explore with the patient the various stimuli that may precipitate seizure activity.
• Recognize seizure warning signs and usual seizure pattern.
• Keep all doctor’s appointments – blood work to determine therapeutic levels of anticonvulsants.
• Don’t change meds from generic to brand name Evaluation
• Will not experience injury during seizure.
• Will not aspirate during seizure
• Family will increase knowledge about seizures and be able to document seizures appropriately
• Seizures activity controlled
• Positive self-image displayed
• Disease process/prognosis, therapeutic regimen, and limitations understood
Parkinson’s – lack of dopamine (chemical messenger in brain), onset gradual and slowly progressive
• What does it look like?
• How is it treated/managed?
• Meds
• Safety
• ADLs
• Patient education
• Complications
• Pneumonia
• Aspiration
Parkinson’s Disease
• Parkinson's disease is a progressive disorder of the nervous system that affects movement
• Develops gradually, often starting with a barely noticeable tremor in just one hand
• Also commonly causes a slowing or freezing of movement
• No cure
Overview
• Genes. Researchers have found specific genetic mutations that likely play a role in Parkinson's disease. In addition, scientists suspect that many more changes in genes — whether inherited or caused by an environmental exposure — may be responsible for Parkinson's disease.
• Environmental triggers. Exposure to toxins or certain viruses may trigger Parkinson's signs and symptoms.
Overview
• A lack of dopamine - chemical messenger in the brain
• specific brain cells that produce dopamine die or become impaired. Why and exactly how this happens isn't known.
• Low norepinephrine levels due to damage to the nerve endings that make norepinephrine
• Norepinephrine plays a role in regulating the autonomic nervous system
• The presence of Lewy bodies. Unusual protein clumps called Lewy bodies are found in the brains of many people with Parkinson's disease. How they got there and what type of damage, if any, Lewy bodies might cause is still unknown.
Medical Management Medications
• Levodopa also combined with carbidopa to create the combination drug, Sinemet..
• increases levels of dopamine
• Dopamine agonists
• MAOB inhibitors
• Catechol O-methyltransferase (COMT) inhibitors
• Anticholinergics Glutamate (NMDA) blocking drugs
Medical Management Surgery
• Deep brain stimulation –
• surgical procedure involves implanting an electrode deep within the parts of the brain that control movement amount of stimulation delivered by the electrode is controlled by a pacemaker-like device placed under the skin in the chest
Assessment – Growth & Development
• Young adults rarely experience Parkinson's disease
• ordinarily begins in middle or late life, and the risk continues to increase with age.
• Having a close relative with Parkinson's increases the chances of developing the disease
• Men are more likely to develop Parkinson's disease than women are.
• Diagnostics Tests
• No specific tests
• Medical history
• Neurological exam
• walking and coordination, as well as some simple hand tasks
•
Clinical Manifestations
• Tremor - shaking begins in a hand. A back-and-forth rubbing of thumb and forefinger, known as pill- rolling, is common, and may occur when hand is at rest. Not everyone experiences tremors.
• Slowed motion (bradykinesia) -reduce ability to initiate voluntary movement. This may make even the simplest tasks difficult and time-consuming
• steps may become short and shuffling. – HAVE PATIENT MARCH TO A BEAT or walk with a beat
• feet may freeze to the floor, making it hard to take the first step.
• Impaired posture and balance become stooped, lean forward
• Balance problems also may occur, although this is usually in the later stages of the disease.
• Rigid muscles. Muscle stiffness can occur in any part of your body. Sometimes the stiffness can be so severe that it limits the range of movements and causes pain.
• first notice this sign when no longer swing arms when walking
• Loss of automatic movements
• Blinking, smiling and swinging arms when walking is diminished and even lost.
• Fixed staring expression and unblinking eyes.
• Others may no longer gesture or seem animated when they speak.
• Speech changes - speak more softly, rapidly or in a monotone, sometimes slurring or repeating words, or hesitating before speaking.
• Dementia - In the later stages of Parkinson's disease, some people develop problems with memory and mental clarity. Alzheimer's drugs appear to alleviate some of these symptoms to a mild degree.
• Depression
• Sleep problems
• trouble falling asleep
• may wake up frequently throughout the night
• experience sudden sleep onset, called sleep attacks, during the day
• Difficulty chewing and swallowing. The muscles used to swallow may be affected in the later stages of the disease, making eating more difficult.
• Urinary problems. urinary incontinence or urine retention
• Constipation - digestive tract works more slowly
• Sexual dysfunction - decrease in sexual desire
•
Nursing Diagnosis
• Risk for injury
• Anxiety
• Impaired physical mobility
• Impaired social interaction
• Impaired swallowing
• Impaired verbal communication
•
Planning & Intervention
• Teaching
• Providing safe home care
• NEEDS IDT TEAM AS WELL Client Teaching
• Eat a nutritionally balanced diet that contains plenty of fruits, vegetables and whole grains
• helping prevent the constipation that is common in Parkinson's disease
• provides nutrients, such as omega-3 fatty acids, that may be beneficial for people with Parkinson's disease.
• Take a fiber supplement, such as psyllium powder, Metamucil or Citrucel, be sure to introduce gradually and drink plenty of fluids daily
• Walking with care
• Try not to move too quickly.
• Aim for heel to strike the floor first when walking
• If shuffling, stop and check posture - stand up straight
• Practice walking to marching music
• Safe environment Client Teaching
• Dressing-fine motor control makes it hard to button and zip clothes, and even to step into a pair of pants. An occupational therapist can point out techniques that make daily activities easier
• Allow plenty of time so that patient doesn't feel rushed
• Lay clothes nearby
• Choose clothes that can slip on easily, such as sweat pants, simple dresses or pants with elastic waistbands.
• Use fabric fasteners, such as Velcro, instead of buttons Evaluation
• Expresses concerns
• Has a support system
• State the correct method of medication dosing
• Demonstrate how schedule will be maintaining
• Utilizes assistive measures to maintain ADLs
Complication
• Death r/t PNA
Multiple Sclerosis – chronic progressive, degenerative disease affecting myelin sheath
• What does it look like?
• How is it treated/managed?
• Patient Safety
• Patient education
• Complications
Multiple Sclerosis
Overview – Multiple Sclerosis
• A chronic progressive degenerative disease that affects the myelin sheath of neurons in the CNS
• Cause unknown – could be related to
• Genetic
• Virus
• Autoimmune response - antigen-antibody reaction Overview MS
• A chronic progressive degenerative disease that affects the myelin sheath of neurons in the CNS
• Cause unknown – could be related to
Risk Factors
• Genetic
• Virus
• Autoimmune response - antigen-antibody reaction
• Heredity
• Infections
• have one of the following autoimmune disorders
• Thyroid disease
• Type 1 diabetes
• Inflammatory bowel disease
•
goal is to slow progression of disease; we are unable to cure it. Do not go out on extreme heat or extreme
Medical Management- cold, loss of sensation does not take hot baths unless you have thermometer, avoid crowds due to immunomodulators. Avoid pregnancy.avoid fatigue and stress.
• Corticosteriods
• Immunomodulators – B-interferon
• Immunosuppressants
• Cholinergics - flaccid bladder
• Anticholinergic – spastic bladder
• Muscle relaxants
Assessment- Culture
• White people, particularly those whose families originated in northern Europe, are at highest risk of developing multiple sclerosis
• People of Asian, African or Native American descent have the lowest risk
• Multiple sclerosis is far more common in countries with temperate climates, including Europe, southern Canada, northern United States, New Zealand and southeastern Australia
• The risk seems to increase with latitude
Assessment- Growth & Development
• Although multiple sclerosis can occur at any age, it most often begins in people between the ages of 20 and 40
• Women are more likely to develop multiple sclerosis than are men
• Diagnostic Tests
• CSF analysis
• CT scan
• MRI
•
Clinical Manifestations – Usually stress triggers exacerbations. May vary
• Motor
• weakness or paralysis of the limbs, trunk, or head
• speech problems
• spasticity of the muscles
• Cerebellar signs
• Nystagmus, ataxia, dysarthria, dysphagia, ringing of the ears.
•
Clinical Manifestations Sensory
• numbness, tingling, paresthesia
• visual & hearing changes, tinnitus, decrease hearing
• Vertigo
• radicular pain (pain in thoracic area and abdominal region)
• Lhermitte’s phenomenon – electric or tinkling like sensation radiating down the spine, into the limbs with the flexion of the neck
Clinical Manifestations
• Bowel & Bladder functions can be affected
• Constipation
• Spastic bladder – incont.
• Flaccid bladder – no sensation of voiding
• Mood swings, intellect intact
• S/S may be triggered by physical, emotional trauma, fatigue, infection, anybody stress Nursing Diagnosis
• Pain
• Anxiety
• Hopelessness
• Risk for powerlessness
• Self-care deficit
• Disturbed sensory perception
• Risk for injury
•
Planning & Interventions
• Protect from injury
• Monitor for complications
• Bladder and bowel training
• Straight cath residuals – increasing amounts may require increasing frequency of catheterizations
• Avoid fatigue and stress – simply going out in hot weather fatigues
• Needs IDT Client Teaching
• Teach client self-care that is consistent with client’s beliefs
• treatment plan, including implications of medications, exercise program, use of adaptive equipment
• Safety measures – (decreased sensation) testing bath water with unaffected extremity, using pot holder when cooking, avoid heating pad, wearing gloves in cold weather.
Evaluation
• Knows how to utilize available resources
• Verbalizes appropriate plans for coping with stressful situations
• Functions at maximum level
•
Stroke – sudden neurological deficit due to cerebral circulation being interrupted
• What are the risk factors?
• What does it look like?
• How is it treated (both hemorrhagic and thrombotic)?
• Initial (to include nursing care with rtPA)
• Rehab
• Patient education
Need to find out the LAST SEEN NORMAL NON- Contrast CT
NPO – Nothing to eat until evaluated
Left hemisphere stroke is aware of deficit and aware they had a stroke and is more likely to suffer from depression. Wernickes aphasia is difficulty understanding speech and expressing themselves. Brocas aphasia have damage to the frontal lobe understand the speech of others fairly well, are able to speak in short sentences. Be patient don’t frustrate patient and allow them to have alternate methods of communications.
Right hemisphere- everything becomes left handed, spacial-perceptual deficit (where they ignore one side, such as eating one side of the food or combing only one side of head), make rash decisions, short attention span, impulsive behavior, time concepts, childlike behaviors. Not really aware of deficit, do not approach them from affected side it will startle them. Need to have them scan and recognize items on affected side.
Stroke
Overview
• Sudden neurological deficit
• Cerebral circulation is interrupted
• Neuro deficits develop
• Anoxia longer than 10 minutes results in tissue infarct and irreversible damage
Overview- Types of Stroke
• Ischemic stroke
• embolic or thrombotic
• blocked blood flow to the brain
• need thrombolytic, need to do risk assessment before thrombolytic. RNs role is vs, neuro-checks, any s/s of bleeding every 10-15 mins while being administered. When finished administering it continue you checks every 30 mins for 6 hours. Once finished with the 6 hours every hour for the next 24hrs. Keep blood pressure with systolic 180 and diastolic 105. Thrombolytic agents need close monitoring.
•
• Hemorrhagic:
• Intracerebral
• Subarachnoid
• Cerebral Aneurysm
• Vessel malformation – AVM
• need neuro consult because the treatment is surgery. Need to maintain lower blood pressure, very poor outcome unless they are able to operate.
• 150/105 must be below this parameter need to monitor
•
• TIA:
• This is a stroke, ischemic attack although symptoms resolve within an hour needs to be on anticoagulants, symptoms go away.
Medical Management Ischemic Stroke
• tPA=Thrombolytic agent
• Document time of symptom onset. (If awoke with symptoms, must go by time when last seen normal)
• Immediate head CT (check for blood)
• Evaluate for tPA administration (review exclusion/inclusion criteria)
•
Medical Management Hemorrhagic Stroke
• Do not give antithrombotics or anticoagulants
• Monitor and treat blood pressure greater than 150/105
• NPO, until swallow evaluation is completed
• Neurosurgical consult
• Possible administration of blood products
•
Assessment- Culture
• African Americans have 2 times more risk of stroke than other races have
• Hispanics and Asians have the greatest risk for hemorrhagic stroke Diagnostic Tests
• MRI/CAT scan before treatment is initiated to determine if hemorrhagic or thrombotic
• Carotid ultra sound
• Echo
• ECG monitoring for a-fib, MRI,
• fasting Lipid
• Clotting disorder blood work (Antiphospholipid, Factor V, Antithrombin III)
Assessment
• Findings depend on which side of the brain affected
• Airway
• Pulse (slow or bounding)
• Respirations (Cheyne-Stokes)
• BP (HTN)
• N/V
• Facial drooping
• Speech difficulties
• Vision loss
• Decreased sensations & movement
• Bowel and bladder incontinence
• Damage to the temporal lobe (the side portion) of the brain may result in a fluent aphasia called Wernicke’s aphasia
• Have difficulty understanding speech and expressing themselves
• People with Broca’s aphasia have damage to the frontal lobe of the brain
• Understand the speech of others fairly well; are able to speak in short sentences
Planning & Intervention
• IV fluids (Normal Saline or LR) – D/T patient having NPO
• Nutrition
• Swallowing assessment – dysphasia diet
• No Straws
• Pureed food and thickened fluids.
• Dietary evaluation
• Assistive devices for feeding
• Calorie Counts as ordered.
• Assess temperature -Treat if greater than 99 F with Tylenol, use cooling blanket and adjust room temperature.
• Assess blood glucose levels as prescribed- Need normal glycemic glucose levels is essential for healing.
• Rehab consults as soon as possible, if needed, needs Inter disciplinary care/team such as pt, ot, st, social services, behavioral such as psychiatrist, optomologist,
• Assess for intracranial hemorrhage
• Pillows under affected limbs
• Turn Q2 hours
• Accommodate limitations
• Safety in getting in and out of bed/ wheelchair
• Prevent contractures. Client Teaching
An occupational therapist can point out techniques that make daily activities easier
• Allow plenty of time so that patient doesn't feel rushed
• Lay clothes nearby
• Choose clothes that can slip on easily, such as sweat pants, simple dresses or pants with elastic waistbands. Provide self-independence
• Use fabric fasteners, such as Velcro, instead of buttons
• ROM & PT
• If patient has difficulty swallowing
• Provide thicken liquids
• Soft foods that have stickiness such mashed potatoes or macaroni & cheese
• Avoid straws
Evaluation
• Expresses concerns
• Has a support system
• Demonstrate how rehabilitation schedule will be maintained.
• Utilizes assistive measures to maintain ADLs
• Maintains nutrition & fluid balance
Migraine headache – intense headache caused by combination of vascular, genetic, neurologic, hormonal factors, spasms of arteries
• What does it look like?
• How is it treated?
• Patient education on medication management
Occurs more in women than men
Multiple causes- vascular, genetic, hormonal, environmental
Medications- triptons such as imitrex, need to take medications right away, works by activating serotonin receptors release serotonins. SSRI and St john’s wort. can’t be taken with imitrex d/t countering affect. Not safe for pregnant women in of imitrex needs to be on contraceptive.
Eye disorders
• Cataracts
• What does it look like?
• How is it treated?
Cataracts
• clouding of the normally clear lens of the eye
• bit like looking through a frosty or fogged-up window, halos
• make it more difficult to read, do not drive a car — especially at night
• non painful, gradually worsens. Overview
➢ The lens is positioned behind the iris
➢ The lens focuses light that passes into the eye, producing clear, sharp images on the retina
➢ the cataract scatters the light as it passes through the lens, preventing a sharply defined image from reaching the retina
➢ vision becomes blurred
Overview – Medical Management
The only effective treatment for cataracts is surgery
• removing the clouded lens and replacing it with a plastic lens implant- immediate improvement.
• done on one eye at a time, with a few weeks between surgeries
• outpatient basis
• uses local anesthesia
• carries a risk of infection and bleeding.
• increases the risk of retinal detachment
Assessment- Growth & Development
• With age, the lenses in the eyes become less flexible, less transparent and thicker
• Aging-related changes to the lens cause tissues to break down and to clump together, clouding small areas of the lens
• As the cataract continues to develop, the clouding becomes denser and involves a greater part of the lens.
Diagnostics Test
• visual acuity test
• slit-lamp examination
• retinal examination – dilating the pupils
• scan measurements – done when ocular surgery is done get lens to perfectly fit the pocket
Assessment
• Clouded, blurred or dim vision
• Increasing difficulty with vision at night
• Sensitivity to light and glare
• Seeing "halos" around lights
• Frequent changes in eyeglass or contact lens prescription
• Fading or yellowing of colors
• Double vision in a single eye Nursing Diagnosis
• Disturbed Sensory Perception
• Fear
• Risk for Injury
• Self-Care Deficit
• Impaired Home Maintenance
Planning & Intervention Postoperative teaching:
• Wear glasses during the day and eye shield at night
• Demonstrate procedure for instilling eye drops
• usually antibiotics & corticoidsteroids
• May be told to avoid straining with a bowel movement, lifting, bending or stooping as it increases IOP
• Monitor pain
Client Teaching
• Make sure your eyeglasses or contact lenses are the most accurate prescription possible
• Use a magnifying glass to read
• Improve the lighting in your home with more or brighter lamps
• When you go outside during the day, wear sunglasses or a broad-brimmed hat to reduce glare
• Limit your night driving
• Have regular eye exams
• Quit smoking
• Wear sunglasses
• wait to administer 10-15 mins in between drops. Ointment is instilling at the nose and move outward. Make sure not to contaminate tip of applicator. Need to be done on a schedule to get maximum therapeutic effect.
•
Evaluation
• Have sufficient vision
• Demonstrate procedure for instilling eye drops
• Have minimal or no pain
• Retinal Detachment
• What does it look like?
• How is it treated
• Eye Surgery – post op care/teaching
• Eye drops and eye ointments
• Patient education FOCUS on post op care – same as cataract Retinal Detachment
• Retinal detachment is a medical emergency requiring prompt surgical treatment to preserve vision.
• The retina is pulled away from the underlying choroid — a thin layer of blood vessels that supplies oxygen and nutrients to the retina.
• Retinal detachment leaves retinal cells deprived of oxygen. The longer the retina and choroid remain separated, the greater the risk of permanent vision loss in the affected eye.
• Fortunately, retinal detachment often has clear warning signs early diagnosis and treatment of retinal detachment can save vision.
Overview
• Retinal detachment occurs when vitreous humor leaks through a retinal tear and accumulates underneath the retina
• Leakage can also occur through tiny holes where the retina has thinned due to aging or other retinal disorders
• As liquid collects underneath it, the retina can peel away from the underlying layer of blood vessels (choroid)
• The areas where the retina is detached lose their blood supply and stop functioning Overview
• Retinal detachment is painless, but visual symptoms almost always appear before it occurs
• Warning signs of retinal detachment include:
• The sudden appearance of many floaters — small bits of debris in your field of vision that look like spots, hairs or strings and seem to float before the eyes
• Sudden flashes of light in one or both eyes
• A shadow or curtain over a portion of the visual field
• A sudden blur in your vision
Risk Factors
• Aging — retinal detachment is more common in people older than age 40
• Previous retinal detachment in one eye
• A family history of retinal detachment
• Extreme nearsightedness (myopia)
• Previous eye surgery, such as cataract removal
• Previous severe eye injury or trauma
Retinal Detachment Can occur as a result of:
• Trauma
• Advanced diabetes
• An inflammatory disorder, such as sarcoidosis or cytomegalovirus retinitis
• Sagging or shrinkage of the jelly-like vitreous that fills the inside your eye
Diagnostic Tests
• may be able to see a retinal hole, tear or detachment by looking at the retina with an ophthalmoscope
• If blood in the vitreous cavity blocks the view of your retina, ultrasound examination may be useful.
•
Clinical Manifestations
• The sudden appearance of many floaters — small bits of debris in your field of vision that look like spots, hairs or strings and seem to float before your eyes
• Sudden flashes of light in one or both eyes
• A shadow or curtain over a portion of your visual field Treatment
• Surgery is used to repair a retinal tear, hole or detachment
• Injecting air or gas into your eye
• Indenting the surface of your eye
• Draining and replacing the fluid in the eye Nursing Diagnosis
• Risk for injury
• Disturbed Sensory Perception: Visual
• Anxiety
•
Planning & Interventions
• Activity restrictions may be needed
• Assess for nausea & vomiting as can increase IOP
• Assess for drainage and bleeding from eye
• Pain management
• Keep head down and to the side if bubble used Client Teaching
• Help patient understand nature and limitations of disease
• Teach general eye care – including administration of eye drops- Return of vision is not immediate
• Wear eye shield or glasses during the day
• Avoid air travel for several mweeks if use of air/gas bubble Evaluation
• Able to cope with any vision loss
• Applies eye drops as prescribed
• Remains free of injury
• Glaucoma
• What does it look like?
• How is it treated?
Glaucoma
• Not just one disease, but a group of conditions resulting in optic nerve damage, which diminishes sight
• Increased intraocular pressure is usually associated with the optic nerve atrophy
• Pressure comes from a buildup of aqueous humor, a fluid naturally and continuously produced in the front of the eye – between lens and cornea
• Aqueous humor normally exits the eye where the iris and the cornea meet
• When aqueous humor can't filter out of the eye at its normal rate pressure builds within the eye The Most Common Types of Glaucoma
• primary open-angle glaucoma – open angel can be treated.
• painless and does not have acute attacks
• gradually progressive visual field loss
• primary angle-closure glaucoma
• sudden ocular pain, halos around lights, red eye, very high intraocular pressure, nausea and vomiting, sudden decreased vision, and a fixed, mid-dilated pupil
•
Primary open-angle Glaucoma (POAC)
• The most common type
• Aqueous humor is prevented from draining by an obstruction
• See diagram Black (2009) 65-1 page 1700
Primary angle-closure Glaucoma
• the iris bulges forward to narrow or block the angle formed by the cornea and the iris
• aqueous fluid can no longer flow from the posterior to anterior chamber, so the eye pressure increases abruptly
• acute angle-closure glaucoma usually occurs suddenly
Primary angle-closure glaucoma
• If you have a narrow drainage angle, sudden dilation of your pupils may trigger acute angle-closure glaucoma
• Pupils become dilated in response to darkness, dim light, stress, excitement and certain medications
• antihistamines, such as desloratadine (Clarinex) and cetirizine (Zyrtec); tricyclic antidepressants, such as doxepin (Sinequan) and protriptyline (Vivactil); and eyedrops used to dilate your pupils for a thorough eye exam
Overview
• Both open-angle and angle-closure glaucoma can be primary or secondary conditions
• primary when the cause is unknown and secondary when the condition can be traced to a known cause, such as eye injury, inflammation, tumor, or advanced cataract or diabetes
• secondary glaucoma, the signs and symptoms can include those of the primary condition as well as typical glaucoma symptoms
Risk Factors
• Elevated internal eye pressure (intraocular pressure).
• Family history of glaucoma
• Medical conditions
• Other eye conditions
• Severe eye injuries
• Retinal detachment
• eye tumors and eye inflammations, such as chronic uveitis and iritis
• Nearsightedness
• Prolonged corticosteroid use Overview
• If left untreated, glaucoma will cause progressive vision loss, typically in these stages:
• Blind spots in your peripheral vision
• Tunnel vision
• Total blindness
•
Medical Management
• drug therapy for glaucoma Includes
• Topical miotics
• Epinephrine
• Topical beta-blockers
• Topical adrenergic agents
• Oral carbonic anhydrase inhibitors
• Important point – how do you prevent systemic effects of eye drops?
• Surgical Management
• There are numerous procedures to help improve the flow of aqueous humor
• See BlacK (2009) PG, 1703
Assessment – Culture
• African-Americans are six to eight times more likely to get glaucoma than are Caucasians
• much more likely to experience permanent blindness as a result
• Mexican-Americans also face an increased risk
• Asian-Americans are at slightly higher risk of angle-closure glaucoma
• Japanese-Americans are at a greater risk of developing low-tension glaucoma
•
Assessment – Growth & Development
• Everyone older than 60 is at increased risk of glaucoma Diagnostic Tests
• Tonometry test measures the inner pressure of the eye. Usually drops are used to numb the eyes; special device measures the eye’s pressure.
• Ophthalmoscopy is used to visualize the optic nerve
• Visual field test - patient is asked look straight ahead and then indicate when a moving light passes the peripheral vision
• Gonioscopy is a painless eye test that checks if the angle where the iris meets the cornea is open or closed, showing if either open angle or closed angle glaucoma is present
Nursing Diagnosis
• Disturbed sensory perception
• Risk for ineffective therapeutic regime management
• Grieving
•
Planning & Interventions
• Determine visual loss & how patient is coping
• Assess pain
• Assess for increase in IOP
• Administer eye drops as prescribed Client Teaching
• See Black (2009) p. 1704 – client education guide
Evaluation
• No further vision loss
• Adheres to treatment plan
• Vocalizes loss of vision
• Macular Degeneration
• What does it look like?
• How is it treated?
Macular Degeneration
• Chronic eye disease marked by deterioration of tissue in the part of the eye that's responsible for central vision. The deterioration occurs in the macula which is in the center of the retina
• Macular degeneration doesn't cause total blindness, but it worsens quality of life by blurring or causing a blind spot in central vision. Clear central vision is necessary for reading, driving, recognizing faces and doing detail work.
• Wet AMD occurs when abnormal blood vessels behind the retina start to grow under the macula
• An early symptom of wet AMD is that straight lines appear wavy
• Dry AMD occurs when the light-sensitive cells in the macula slowly break down, gradually blurring central vision in the affected eye.
• The most common symptom of dry AMD is slightly blurred vision
Risk Factors
• Aging
• Family history
• Macular degeneration gene- for DRY MACULAR DEGENERATION
• Smoking
• Obesity
• Race
• Gender
Medical Management
• Wet AMD:
• Laser surgery – destroy the leaky blood vessels
• Photodynamic therapy - A drug called verteporfin is injected; travels to and sticks to the walls of the blood vessels in eye; then a light is shined in the eye activating the drug and destroying the new blood vessels
• Injections – of drug that blocks the effects of growth factor therefore blocking formation of new blood vessels
• Dry AMD:
• Advanced – no treatment
• high-dose formulation of antioxidants and zinc slows the progression
•
Assessment – Growth & development
• Macular degeneration tends to affect adults age 50 and older
• Diagnostics Tests
• Visual acuity test. This eye chart test measures how well you see at various distances.
• Dilated eye exam. Drops are placed in your eyes to widen, or dilate, the pupils. Your eye care professional uses a special magnifying lens to examine your retina and optic nerve for signs of AMD and other eye problems. After the exam, your close-up vision may remain blurred for several hours.
• Tonometry. An instrument measures the pressure inside the eye. Numbing drops may be applied to your eye for this test.
•
Distinguishing Symptoms Dry AMD:
• the most common early sign is blurred vision
• Progresses to where details are seen less clearly in front of them, such as faces or words in a book.
• Often this blurred vision will go away in brighter light.
• Small--but growing--blind spot in the middle of their field of vision. Wet AMD:
• the classic early symptom is that straight lines appear crooked
• small blind spot may also appear in wet AMD, resulting in loss of one's central vision.
•
Client Teaching
• Lifestyle can play a role in reducing your risk of developing AMD.
• Diet high in green leafy vegetables and fish
• Smoking cessation
• Blood pressure control
• Weight reduction
• Exercise
• Hearing Disorders
• Hearing loss and hearing aids
• Patient education
Hearing Impairment
• Conductive hearing loss
• Interference of sound transmission through external ear and middle ear
• Sensorineural hearing loss
• Impairment of function of the inner ear or eighth cranial nerve
• Mixed hearing loss
• Both conductive and sensorineural
• Etiology
• Ear obstruction
• Infection
• Otosclerosis
• Tympanosclerosis
• Trauma to tympanic membrane
Sensorineural Hearing Loss
• Etiology
• Presbycusis
• Sudden hearing loss
• Congenital hearing loss
• Noise-induced hearing loss
• Benign and malignant tumors
• Ménière’s disease
Prevention and Screening
• Primary prevention
• Minimize risks
• Principles and guidelines
• Secondary prevention
• Early detection
• Tertiary prevention
• Hearing rehabilitation programs
Clinical Manifestations
• No response to oral communication
• Loud speech
• Strained facial expression
• Tilting head
• Listen to TV at increased volume
• Faulty speech articulation
Medical Management
• Restore hearing
o Antibiotics
o Corticosteroids
• Hearing aids- lowest level, don’t shower, check batteries, clean ear mold, proper hearing aid care. When not in use remove batteries and turn off.
• Assistive listening devices
• Aural rehabilitation
o Speech reading
o Sign language
• Restore conductive hearing loss
• Stapedectomy
• Tumor excision
• Implantable hearing devices
• Cochlear implants
• Temporal bone stimulators
• Middle ear implants
Diagnosis, Interventions, Outcomes
• Impaired Verbal Communication related to effects of hearing loss
• Ineffective Coping related to recent loss of hearing
• Impaired Social Interaction related to perceived inability to interact with others
• Deficient Knowledge of managing hearing loss related to lack of previous experience
Otalgia (Earache)
• Etiology and risk factors
• External ear trauma
• Foreign bodies
• Eustachian tube disorders
• Infection
• Pathophysiology
• Inflammatory process
• Clinical manifestations
• Pain and pressure
• Risk for Infection related to tissue destruction
• Acute Pain related to inflammation in the external or middle ear or from referred pain in the head and neck area
•
• Meneire’s disease
• What is it?
• How is it treated?
• Excess fluid in the ear that affects coordination- vertigo
• Manage with medications such as diuretics, nicotine, antiemetic’s, valium, anti-anxiety
• Hydrops diet – no to little salt and low in sugar, no caffeine, no msg, limit alcohol intake, drink adequate fluids, don’t restrict and don’t over indulge fluid
• Both ears can be involved.
Musculo-skeletal
Topics: Osteoarthritis, Rheumatoid arthritis, Osteoporosis, joint protection, Low back pain (herniated disk, also cervical discectomy), carpal tunnel, fracture complications, osteomyelitis, gout
Osteoarthritis – degenerative joint disease where cartilage in joints deteriorates over time and smooth surface becomes rough, causing irritation > damage and pain
• Risk factors
• What does it look like?
• How is it treated?
• Surgery (hip/knee joint replacements)
• Post op care, safety, complications, patient education Osetoarhtritis -Overvew
• sometimes called degenerative joint disease, is the most common form of arthritis.
• occurs when the cartilage that cushions the ends of bones in joints deteriorates over time
• the smooth surface of the cartilage becomes rough, causing irritation
• eventually the cartilage wears down completely, may be left with bone rubbing on bone — causing the ends of the bones to become damaged and joints to become painful
While osteoarthritis can affect any joint in the body, the disorder most commonly affects joints in the:
• Hands
• Hips
• Knees
• Neck
• Lower back Risk Factors
• The aging process
• Joint injury or stress
• Heredity
• Muscle weakness
• Obesity #1 risk factor mostly knees affected
• Having gout, rheumatoid arthritis, Paget's disease of bone or septic arthritis can increase risk
• Construction jobs
•
•
Medical Management – Medications
• Tylenol first, because it has fewer side effects than other drugs.
• If pain continues nonsteroidal anti-inflammatory drugs (NSAIDs).
– Types of NSAIDs (high dose nsaids when Tylenol is not working for pain) include aspirin, ibuprofen, and naproxen.
– long-term use of NSAIDs can cause stomach problems, such as ulcers and bleeding. These drugs may also increase the risk for heart attacks and strokes.
• Celebrex (a COX-2 inhibitor) may work as well as other NSAIDs. Because of a risk for heart attacks and stroke, it is given only at the lowest possible dose for the shortest possible period of time
• Corticosteroids injected right into the joint can also be used to reduce swelling and pain - relief only lasts for a short time
• Glucosamine and chondroitin sulfate. There is some evidence that these supplements can help control pain, although they do not seem to grow new cartilage
– Some doctors recommend a trial period of 3 months to see whether glucosamine and chondroitin work.
• Capsaicin (Zostrix) skin cream may help relieve pain - usually begins within 1 - 2 weeks.
• Artificial joint fluid (Synvisc, Hyalgan) can be injected into the knee. It may relieve pain for 3 - 6 months Surgical Management
• Joint replacement (arthroplasty) removes damaged joint surfaces and replaces them with prostheses
• The hip and knee joints are the most commonly replaced joints.
• Implants can replace shoulder, elbow, finger or ankle joints
• Joint replacement surgery carries a small risk of infection and bleeding
• Artificial joints can wear or come loose and may need to eventually be replaced
•
Assessment – Growth & Development
• Females are twice as likely to have osteoarthritis
• Seen more with aging Diagnostics
• An x-ray of affected joints will show a loss of the joint space
• MRI- usually done when injecting cortico steroids but a simple xray can diagnose it
• Aspiration and analysis of synovial fluid
Nursing Diagnoses
• Deficient Knowledge
• Acute Pain and Chronic Pain
• Impaired Physical Mobility
• Risk for Peripheral Neurovascular Dysfunction
• Risk for Injury
• Risk for Infection
• Risk for Impaired Skin Integrity
• Risk for Ineffective tissue perfusion Planning & Interventions
• Heat or cold application
• Ionized wrist bracelets
• Pain management
• Rest-activity balance
• Nutrition and weight loss
• Self-care strategies
• Collaboration with occupational therapist
•
Planning & Interventions Joint Replacement
• Check vital signs, including temperature and level of consciousness, every 4 hours or more frequently as indicated.
• Perform neurovascular checks (color, temperature, pulses and
• Assess capillary refill, movement, and sensation on the affected limb
• Monitor incisional bleeding by emptying and recording suction drainage every 4 hours and assessing the dressing frequently
– Significant blood loss can occur with a total joint replacement, particularly a total hip replacement.
• Reinforce the dressing as needed
• Maintain intravenous infusion and accurate intake and output
• Maintain prescribed position of the affected extremity using a sling, abduction splint, brace, immobilizer, or other prescribed device.
• Remind the client to use the incentive spirometer
• Maintain PCA, epidural infusion, or other prescribed analgesia
• Prevent constipation from opioids & decreased mobility
• Help the client get out of bed as soon as allowed
• Teach and reinforce the use of techniques to prevent weight bearing on the affected extremity, such as the over-head trapeze, crutches, pivot turning
• Sequential compression devices or antiembolism stockings as prescribed.
• For the client with a total hip replacement, prevent hip flexion of greater than 90 degrees or adduction of the affected leg a lot of blood loss, lot of pain pt is usually on pca pump do neurovascular checks and incisional bleeding, reinforce dressing, provide iv hydration, make sure affected extremity is position correctly with abduction pillow. Incentive spirometer they will suffer from constipation d/t bed rest and pain meds, early ambulation, provide stool softeners. Scd and lovenox, nonbearing weight on affect limb with pivot on strong leg or overhead trapeze prevent hip flexion of 90 degrees use assistive devices to prevent hip dislocations hip discoloration looks like a shorter leg and lots of pain. Lead with strong side when getting in and out of bed, use trapeze use anticoagulants and scds hip pt are high risk for dvts, usually on pca pump slows motility hydration and stool softeners a must.
• Provide a seat riser for the toilet or commode
• Assess the client with a total hip replacement for signs of prosthesis dislocation
– pain in the affected hip or shortening of leg
– internal rotation of the affected leg
• For the client with a knee replacement, use a continuous passive range-of-motion (CPM) device or range- of-motion exercises as prescribed
• Provide a seat riser for the toilet or commode
• Dislocation is not a problem with a knee replacement, and more emphasis is placed on range-of-motion exercises in the early postoperative period
• High protein diet,
• Pt, tens units
• Lifestyle modifications, exercise, stop smoking.
• Cpm machine is used If knee is immobile adhesions will form and we will get a fused knee we need to prevent this. So cpm will be ordered to maintain as much ROM as possible. Constavac drain from knee needs to be sterile and must reinfused drainage
Client Teaching
• Stay at a healthy weight or lose weight if need to
• Be active
– A lack of exercise can cause muscles and joints to become weak
– light to moderate exercise can help keep muscles strong, reduce joint pain and stiffness, and slow the time it takes for arthritis to get worse
• Protect joints
– try not to do tasks that put repeated stress on joints, such as kneeling, squatting, or gripping
– use the largest joints or strongest muscles to do things. A single major injury to a joint or several minor injuries can damage cartilage over time
• Medications - side effects
• Applying heat and cold
• Eating a healthy, balanced diet
• Relaxation techniques
• Use assistive devices
– Cane
– Gripping and grabbing tools
Evaluation
• Maintain activities of daily living
• Maintain appropriate weight
• Utilizes assistive devices as needed
• Identifies medication regime
Rheumatoid arthritis – autoimmune disease attacks joints and other organs (cartilage becomes inflamed)
• What does it look like?
• How is it treated? Rheumatoid Arthritis (RA)
• another form of arthritis
• a systemic autoimmune disease which initially attacks the synovium, a connective tissue membrane that lines the cavity between joints and secretes a lubricating fluid
• synovium becomes inflamed, produces excess fluid, and the cartilage becomes rough and pitted
• can also affect other organs Overview
• joints affected is usually symmetrical, involves the hands and other joints and is worse in the morning
• systemic disease, can affect whole body with fevers and fatigue whereas osteoarthritis is limited to the joints
• signs and symptoms may vary in severity and may even come and go
• periods of increased disease activity alternate with periods of relative remission, during which the swelling, pain, difficulty sleeping and weakness fade or disappear
• severe joint deformities result, painful,
• in RA pain is decreased with activity Risk Factors
• genetic component appears likely - doesn’t actually cause rheumatoid arthritis, can make more susceptible to environmental factors — such as infection with certain viruses and bacteria — that may trigger the disease.
• research shows that the risk of developing RA is nearly double for current smokers compared with non-smokers
Growth & Development
• RA can occur at any age - generally occurs between the ages of 40 and 60
• two to three times more common in women than in men Diagnostic Tests
• Blood test - anti-CCP antibody test - diagnosing RA and distinguishing it from other types of arthritis
• Positive C-reactive protein (levels rise in response to inflammation)
• Erythrocyte sedimentation rate - elevated
• Joint x-rays, ultrasound or MRI
• Rheumatoid factor test (positive in about 75% of people with symptoms) tests c-reactive protein.
• Synovial fluid analysis
•
Clinical Manifestations
The disease usually begins gradually with:
• Fatigue
• Loss of appetite
• Morning stiffness lasting a few hours that is relieved after rising with activity
• Widespread muscle aches
• Weakness
• Low grade fever (is always low grade for inflammation anything high is NOT inflammation)
Nursing Diagnosis
• Chronic pain, related to joint inflammation
• Impaired home maintenance, related to fatigue
• Activity intolerance, related to the effects of inflammation
• Deficient knowledge: Therapeutic regimen Planning & Interventions
• Occupational therapist
• Exercise regularly – especially water aerobics
• Heat or cold application
• Relaxation techniques – stress reduction – coping
• Rest
• Support groups
• Prescribed medication
• Teach techniques to minimize joint stress while performing ADLs (application of warm compresses)
• Assess for pain
• Tear drops for Sjogerns’s syndrome
Medical Management
• Disease modifying antirheumatic drugs (DMARDs)
– can slow the progression of rheumatoid arthritis and save the joints and other tissues from permanent damage by decreasing inflammation
– Common DMARDs include methotrexate (Rheumatrex, Trexall), leflunomide (Arava), hydroxychloroquine (Plaquenil), sulfasalazine (Azulfidine) and minocycline (Dynacin, Minocin). Side effects vary but may include liver damage, bone marrow suppression and severe lung infections
• Anti-inflammatory medications
– NSAID packaging now carries a warning label to alert users of an increased risk for cardiovascular events and gastrointestinal bleeding
• Corticosteroids: These medications work very well to reduce joint swelling and inflammation. Because of potential long-term side effects, however, corticosteroids should be taken only for a short time and in low doses when possible
• Cyclooxygenase-2 (COX-2) inhibitors: block an inflammation-promoting enzyme called COX-2.
– numerous reports of heart attacks and stroke have prompted the FDA to re-evaluate the risks and benefits of the COX-2s. Celecoxib (Celebrex) is still available, but labeled with strong warnings and a recommendation that it be prescribed at the lowest possible dose for the shortest possible duration
• Specific white blood cell modulators: effectively control inflammation - Reduces the number of T-cells
– Orencia (abatacept) or Rituxan (rituximab) – Given subcutaneously or intravenously once a month
• Tumor necrosis factor (TNF) inhibitors: block a protein in the body involved in creating inflammation -
– adalimumab (Humira)
– etanercept (Enbrel)
– infliximab (Remicade)
– subcutaneously or intravenously
Client Teaching
• Preventing osteoporosis
• Smoking cessation
• Use of assistive devices
• Medication regime
• Need for eye examinations Evaluation
• Demonstrates an understand the disease and the therapeutic regime
• Verbalizes reduced pain while remaining active
• Copes physically, emotionally, and mentally
• Use assistive devices to minimize joint stress with ADLs
• Verbalize a plan to reduce responsibilities for home maintenance
• Express a willingness to plan rest breaks during the day
• Black (2009) Table 26-1 Show differences between osteoarthritis and rheumatoid arthritis
Osteoporosis – generalized progressive reduction of bone density, causing weakness of skeletal strength.
• What does it look like?
• Risk factors
• How is it treated?
• Medication education on bisphosphonates
• Patient (safety) education
Osteoporosis
• means "porous bones"
• thinning of bone tissue and loss of bone density over time
• so brittle that a fall or even mild stresses like bending over or coughing can cause a fracture
Highest risk is slender female Caucasian alcohol users, and steroid users. Medical Management
• Bisphosphonates (need to take with 8oz of water alone and sit upright from 30mins-1hr to avoid sunlight d/t photosensitivity) are the primary drugs used to both prevent and treat osteoporosis in postmenopausal women - taken by mouth once a week or once a month
– alendronate (Fosamax), ibandronate (Boniva), and risedronate (Actonel)
– intravenously are taken yearly
• Calcitonin slows the rate of bone loss and relieves bone pain-a nasal spray or injection main side effects are nasal irritation from the spray form and nausea from the injectable form.
• Teriparatide (Forteo) is approved for the treatment of postmenopausal women who have severe osteoporosis and are considered at high risk for fractures- given subcutaneously
• Raloxifene (Evista) is used for the prevention and treatment of osteoporosis - can reduce the risk of spinal fractures by almost 50%. However, it does not appear to prevent other fractures, including those in the hip. It may have protective effects against heart disease and breast cancer, though more studies are needed.
Growth & Development
• Drop in estrogen in women at the time of menopause and a drop in testosterone in men
• Women over age 50 and men over age 70 have a higher risk for osteoporosis
• White women are at highest risk Diagnostics Tests
• Bone mineral density testing (a densitometry or DEXA scan)
• Spine or hip x-ray noting fractures Clinical Manifestations
• There are no symptoms in the early stages of the disease
• Symptoms occurring late in the disease include:
– Bone pain or tenderness
– Fractures with little or no trauma
– Loss of height (as much as 6 inches) over time
– Low back pain or neck pain due to fractures of the spinal bones
– Kyphosis, also called a "dowager's hump"
– Spontaneous fx Nursing Diagnoses
– Imbalanced Nutrition: Less Than Body Requirements
– Impaired Physical Mobility
– Pain related to fracture
– Risk for Injury
– Deficient knowledge
Planning & Interventions
Regular exercise can reduce the likelihood of bone fractures
• Weight-bearing exercises -- walking, jogging, playing tennis, dancing
• Resistance exercises -- free weights, weight machines, stretch bands
• Balance exercises -- tai chi, yoga
• Riding a stationary bicycle
• Using rowing machines
at least 1,200 milligrams per day of calcium and 800 - 1,000 international units of vitamin D. Vitamin D helps the body absorb calcium
• may need supplement to get the calcium and vitamin D needed
• High-calcium foods include:
– Cheese
– Ice cream
– Leafy green vegetables, such as spinach and collard greens
– Low-fat milk
– Salmon
– Sardines (with the bones)
– Tofu
– Yogurt
• Limit alcohol intake
• Refer to an osteoporosis support group
• Provide realistic, yet optimistic, feedback about loss of height and bone integrity and the potential outcomes of treatment
• Review safety and fall precautions, and provide literature regarding how to create a safe home environment Client Teaching
• Prevent falls
• Avoid sedating medications and remove household hazards to reduce the risk of fractures
• Make sure vision is good
• Avoiding walking alone on icy days
• Using bars in the bathtub, when needed
• Wearing well-fitting shoes
• Treatment can be monitored with a series of bone mineral density measurements taken every 1 - 2 years Evaluation
• Verbalizes a decrease in pain
• Verbalizes an understanding of treatment regarding osteoporosis
• Verbalizes how stopping smoking can help prevent further progression of osteoporosis.
• Utilizes supplements and medications to prevent further bone loss
• Designs a program of physical activity to prevent complications of osteoporosis
• Verbalizes safety precautions to prevent fractures due to falls
Herniated disk (cervical and lumbar) – small portion of disk pushes out through a tear, irritating a nerve
• What does it look like?
• How it is treated?
• Post op care for discectomy and laminectomy (include complications) Herniated Disk
• Spine is made up of vertebrae that are cushioned by small disks consisting of a tough outer layer (annulus) and a soft inner layer (nucleus)
• A herniated (slipped) disk - a small portion of the nucleus pushes out through a tear in the annulus into the spinal canal
• Can irritate a nerve and result in pain, numbness or weakness in back, leg or arm – depending on where the herniation is located
Overview
• Most often the result of a gradual, aging-related wear and tear called degeneration of the disks
• Spinal disks lose some water content
– makes them less flexible and more prone to tearing or rupturing with even a minor strain or twist
• The lumbar area of the spine is the most common area for a herniated disk (most herniated disks injuries occur in lumbar area.)
• The cervical disks are affected 8% of the time if cervical usually arms are affected.
• The upper-to-mid-back (thoracic) disks are rarely involved
• Usually a herniated disk has sciatica pain Risk Factors
• Age. Herniated disks are most common in middle age, especially between 35 and 45, due to aging-related degeneration of the disks.
• Smoking. Increases risk of disk herniation because it decreases oxygen levels in the blood, depriving body tissues of vital nutrients
• Weight. Excess body weight causes extra stress on the disks in lower back
• Height. Being tall increases your risk of disk herniation
– Men taller than 5 feet 11 inches (180 centimeters) and women taller than 5 feet 7 inches (170 centimeters) appear to have a greater risk of a herniated disk
– Occupations that strain the spine. physically demanding jobs have a greater risk of back problems
– Repetitive lifting, pulling, pushing, bending sideways and twisting also may increase risk of a herniated disk
– Jobs that require prolonged sitting or standing in one position also may increase risk Medical Management
• Modified activity
– stay away from activities that aggravate symptoms, such as improper reaching, bending and lifting, using a rowing machine, and prolonged sitting
– right combination of rest and activity
– Physical therapy
– apply heat, ice, tens machine, traction, ultrasound and electrical stimulation for pain relief
– positions and exercises designed to minimize the pain of a herniated disk
– As the pain improves advance to a rehabilitation program
– Heat or cold
– Initially, cold packs can be used to relieve pain and inflammation
– After a few days’ heat to give relief and comfort.
– Pain medication
– NSAIDs
– Muscle relaxants
– Corticoidsteroids
– Anticonvulsants such as Neurontin
• Steroid injections into the back in the area of the herniated disk may help control pain for several months
– reduce swelling around the disk and relieve many symptoms
– done on an outpatient basis, using x-ray or fluoroscopy to identify the area where the injection is needed
Surgical Management- surgeries are not guaranteed it will work.
• 10 percent of people with herniated disks eventually need surgery
• Microdiskectomy
– spinal surgery that involves cutting away some of the vertebrae to access the herniated disks and compressed nerve roots
– a surgical microscope allows smaller incisions in the skin, muscles and bone overlying a herniated disk
– Smaller incisions and less disruption to surrounding tissue lessen pain and shorten recovery time Diagnostic Tests
• Neurological examination
• Spine x-ray may be done to rule out other causes of back or neck pain
• Spine MRI or spine CT will show spinal canal compression by the herniated disk
• EMG may be done to determine the exact nerve root that is involved
• Myelogram may be done to determine the size and location of disk herniation Clinical Manifestations
• Low back or neck pain can vary widely
– may feel like a mild tingling, dull ache, or a burning or pulsating sensation
– the pain can be severe enough that patients are unable to move
– may also have numbness
• The pain most often occurs on one side of the body
• Lumbar herniated disk may have sharp pain in one part of the leg, hip, or buttocks and numbness in other parts
• The affected leg may feel weak Assessment
• With a cervical disk herniation- pain when moving the neck, deep pain near or over the shoulder blade, or pain that radiates to the upper arm, forearm, or fingers
• The pain often starts slowly. It may get worse:
– After standing or sitting
– At night
– When sneezing, coughing, or laughing
– When walking more than a few yards
• May also have weakness in certain muscles Nursing Diagnosis
• Acute pain
• Disturbed Sleep Pattern
• Risk for constipation
• Deficient knowledge
• Impaired Physical Mobility
• Impaired Ability to Perform Activities of Daily Living
• Disturbed sensory perception
•
Planning & Interventions
• Manage stress - stress magnifies pain
– deep-breathing exercises and relaxation techniques
• Identify pain triggers & provide pain management
• Promote optimal functioning
• Support patient in rehabilitation process
• Firm mattress
• TENs may be useful
• Measures to prevent constipation Client Teaching
• Safe work and play practices, proper lifting techniques, and weight control may help prevent future back injury
• Regular exercise slows aging-related degeneration of the disks, and core-muscle strengthening helps stabilize and support the spine. Check with health care provider before resuming high-impact activities such as jogging, tennis and high-impact aerobics
• Good posture reduces the pressure on the spine and disks. Keep the back straight and aligned, particularly when sitting for longer periods. Also, lift heavy objects properly, making the legs — not the back — do most of the work
• Lying positions to reduce pressure
• Maintain a healthy weight -excess weight puts more pressure on the spine and disks, making them more susceptible to herniation
• Quit smoking Evaluation
• Pain relieved/manageable
• Demonstrates proper lifting, posture, exercises
• Motor function/sensation restored to optimal level
• Disease/injury process, prognosis, and therapeutic regimen understood
Carpel Tunnel- final exam Clinical Manifestations
• Numbness or tingling in the thumb and next two or three fingers of one or both hands
• Numbness or tingling of the palm of the hand
• Pain extending to the elbow, wrist orhands in one or both hands
• Problems with fin finger movements (coordination) in one or both hands
• Wasting away of the muscle under the thumb (in advance or long term cases.)
• Weak grip or difficulty carrying bags (a common complaint)
• Nerve compression
• Numbness, pain, and weakness
• Irritated nerve
Risk Factors
• Overuse or strain
• Repetitive forceful and awkward movement of wrists and hands
• Use of power tools
• Assembly line work
• Thyroid problems
• Repetitive computer use
Diagnostics
• Tinels test tingling in hands fingers when wrist is tapped.
• Phalens Test numbness and tingling following forceful flexion of wrist for 20-30 secs.
Medical Management
• Wrist immobilizer
• Nsaids
• Corticosteroid Injections
Teaching
• Avoid sleeping on wrists
• Hot/cold compresses
• Nsaids
• Reduce/avoid repeptive movements
• Exercise hands in warm water
Surgical Management
• Release compressed median nerve
• Incapacitated for 2 weeks
• Wide range of recovery
• complications nerve damage
Fractures
• Complications with casts
• Compartment syndrome
• Complication with long bone fracture
• Fat embolism
• Osteomyelitis – what is it and what does it look like?
• Complications
• Compartment syndrome
• Osteomyelitis
• Embolism
Gout – urate crystals deposit in joint > inflammation
• What does it look like?
• How is it treated?
Avoid cheese, red meat,
Heart Rhythms (need to know)
Nsr, - pqrst characteristic, nice round upright 0.1-0.2secs rate 60-100 ST – rate is over 100 no tx unless patient is symptomatic
SB – rate below 60 no tx only monitor. unless symptomatic – usually atropine that is given to speed it up Asystole- cpr or chemical resuscitation
Vfib/vimu;ttach defibrillate- 360 jewels. Then proceed to cpr
Eye drops admin
• Pocket drop let them close to eyelid move eyeball side to side, put pressure in lacrimal duct for one minute
• Ointment inner eye to outer eye.
[Show More]