WGU C172 Network and Security - Foundations; PA and OA set*** Questions and Answers 100% Pass
$ 15
TEST BANK for Precalculus: Mathematics for Calculus 8th Edition by James Stewart, Lothar Redlin and Saleem Watson
$ 27
Solutions Manual For Accounting Principles 8th Canadian Edition By Jerry Weygandt, Donald Kieso, Paul Kimmel, Barbara Trenholm, Valerie Warren, Lori Novak (Vol 1 Ch 1-10, Vol 2 Ch 11-18)
$ 25
ACCT 567 Week 4 Midterm (Version 5)/(Download To Score An A)
$ 8.5
RBT Training Questions and answers, 100% Accurate answers.
$ 17
Solutions Manual For Advanced Accounting 13th Edition (Global Edition) By Floyd Beams, Joseph Anthony, Bruce Bettinghaus, Kenneth Smith
$ 25
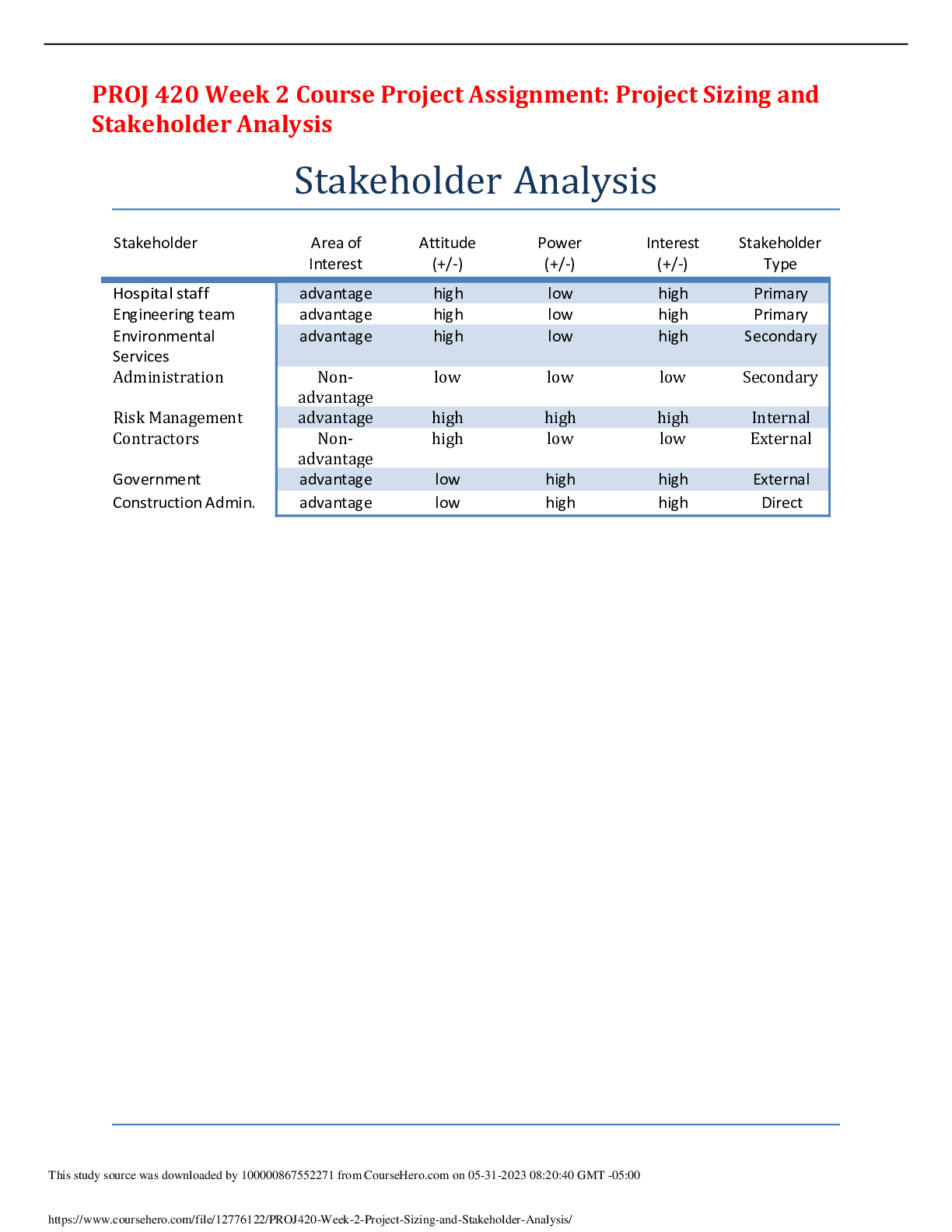
PROJ 420 Week 2 Course Project Assignment: Project Sizing and Stakeholder Analysis - Paper Graded An A
$ 8
Aviation exam questions and answers with verified solutions
$ 7.5

CHAPTER 22 MANAGEMENT CONTROL SYSTEMS, TRANSFER PRICING, AND MULTINATIONAL CONSIDERATIONS: ANSWERS
$ 7

ServiceNow CSA Exam | 130+ Questions with 100% Correct Answers
$ 10
ADM 201 - Salesforce Certification What is affected by changing the default locale set
$ 10
Solutions Manual for Mathematical Statistics with Applications 7th Edition by Wackerly, Mendenhall, and Scheaffer's
$ 17
Ortho NCLEX Questions with accurate answers, Graded A+
$ 9
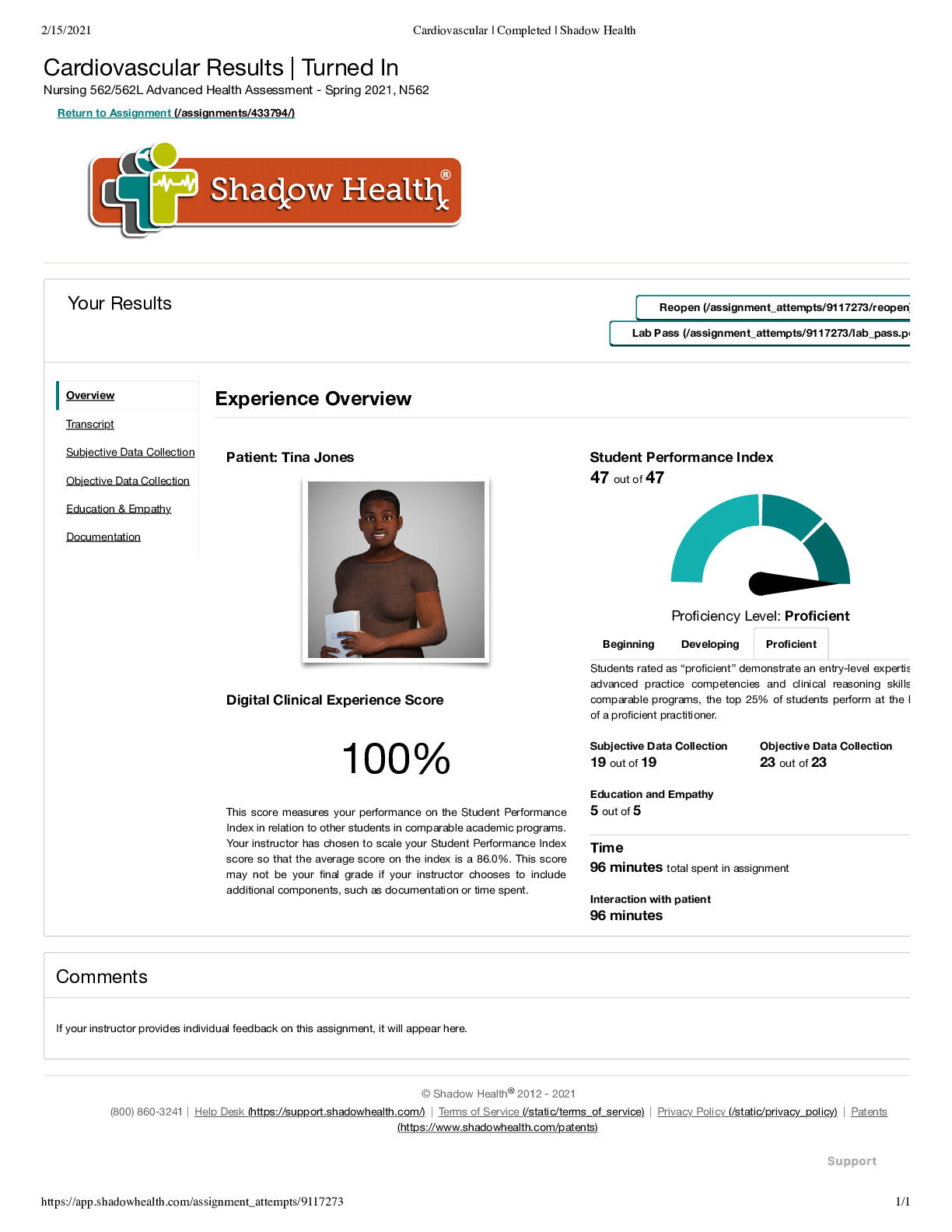
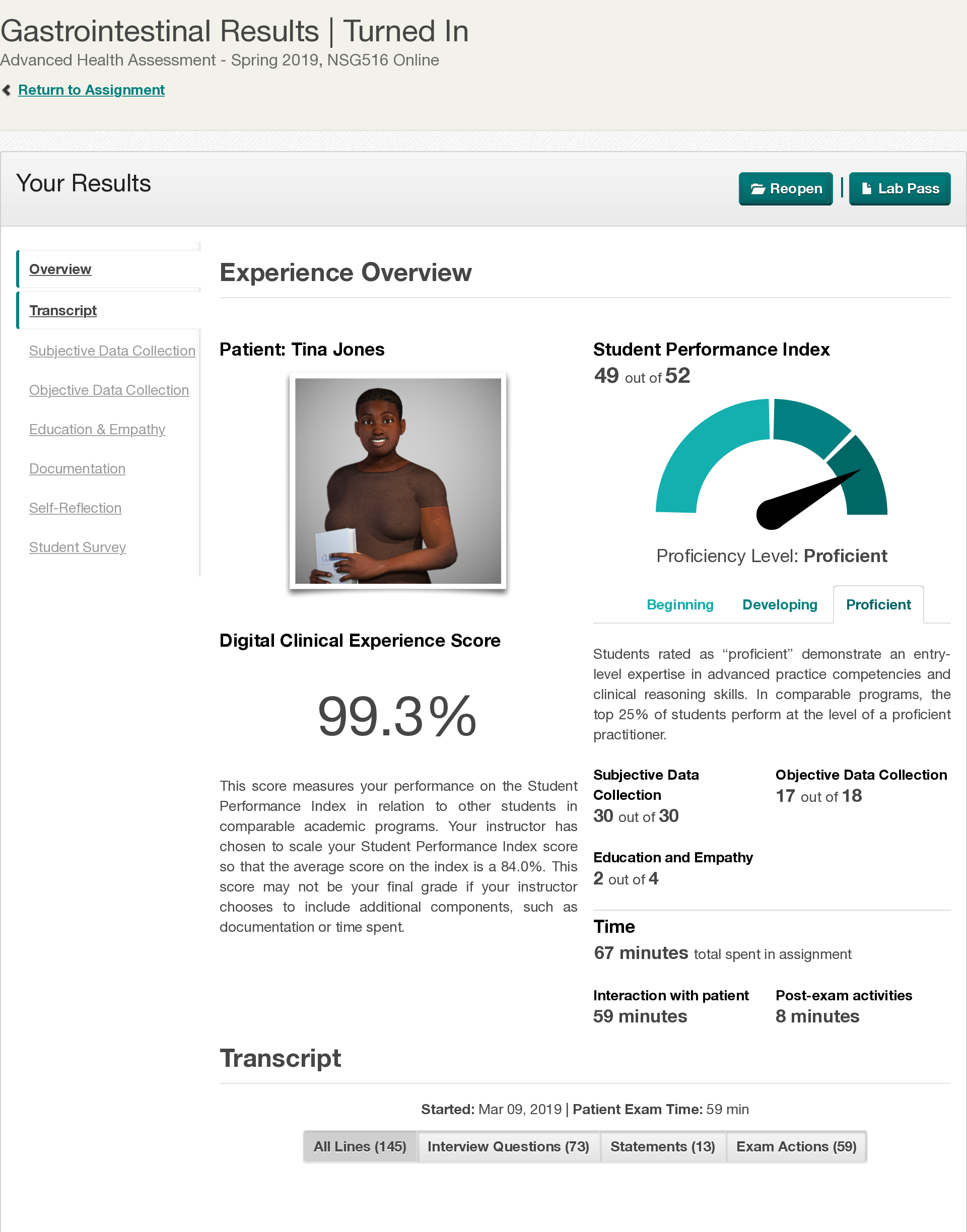
PSYCH C487 Shadow Health John Larsen
$ 4.5

ATI RN Comprehensive Predictor Form B 180 Questions and Answers 100% Correct
$ 12

Iowa State University MT 1Answers of MT1, MT2, Final and Required Readings
$ 15
eBook Urban Transformational Landscapes in the City-Hinterlands of Asia,Challenges and Approaches, 1st edition by Debnath Mookherjee, George M. Pomeroy, Le Thi Thu Huon