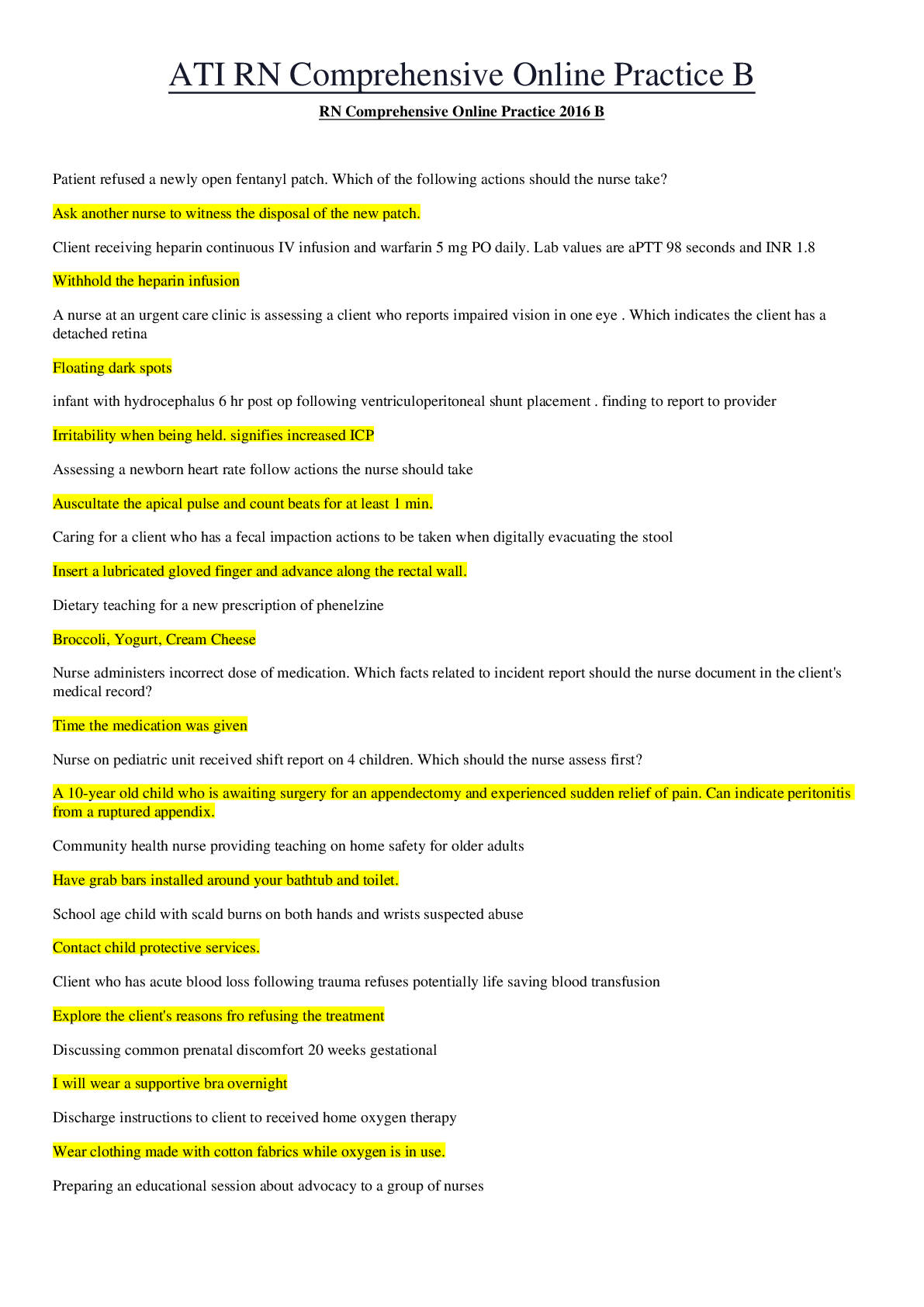
Pathophysiology > EXAM > NURS 5315 Advanced Pathophysiology Disorders of the Immune System | Module 3 (All)
NURS 5315 Advanced Pathophysiology Disorders of the Immune System | Module 3
Document Content and Description Below
NURS 5315 Advanced Pathophysiology Disorders of the Immune System Module 3 Disorders of the Immune System 2. Differentiate between the etiology, clinical manifestations and pathophysiology of ... select disorders of the immune system. Hypersensitivity: an altered immunologic response to an antigen that results in disease or damage to the host. Hypersensitivity reaction: can be classified in 2 ways - by the source of the antigen that the immune system is attacking (allergy, autoimmunity, alloimmunity) - by the mechanism that causes the disease (types I, II, III, IV) a. Evaluate the etiology, clinical manifestations and pathophysiology of Type I, Type II, Type III, and Type IV hypersensitivities and describe the implications clinical practice. -the four mechanisms are interrelated, and in most hypersensitivity reactions, several mechanism can be at work simultaneously or sequentially Hypersensitivity Etiology Clinical Manifestations Pathophysiology Type I (IgE-Mediated Hypersensitivity Reactions) Mediated by antigen-specific IgE and the products of tissue mast cells. Most type I reactions occur against environmental antigens Acute inflammatory response IgE has a relatively short life span in the blood b/c it rapidly binds to very-high-affinity Fc receptors on the plasma membranes of mast cells. With further exposure of antigen to sensitized individual- one molecule of antigen may bind simultaneously to 2 molecules of IgE-Fc receptor on mast cell, activating intracellular signaling pathways and mast cell degranulation Type II (Tissue-Specific Hypersensitivity Reactions) Characterized by a specific cell or tissue being the target on an immune response. “tissue specific antigens”- are expressed on the plasma membranes of only certain cells in specific tissues. Environmental antigens may bind to plasma membranes of specific cells and function as targets of type II reactions Determined by which tissue or organ expresses the particular antigen. 1. Cell can be destroyed by antibody and activate the complement cascade through the classical pathway, resulting in cell lysis. 2.Antibody may cause cell destruction through phagocytosis by macrophages. 3.Antibody and complement may attract neutrophils, initiating the complement cascade and attempt to phagocyte the tissue (cannot be completed), neutrophils release their granules which damages the tissue. 4.antibody-dependent cell-mediated cytotoxicity destroy target cells. 5.causes cell to malfunction - -- - - - - - - - - - - - - - - - - - - -- - - - - - - - - - - -or occurs through natural infection the protective IgG level may remain elevated for years. Aging and the Immune System 2. Differentiate between immune function in the fetus and neonate from a geriatric client and describe the implications for clinical practice. Neonate: In the last trimester the fetus is able to produce a primary immune response but is unable to produce a significant IgG response. The production of IgA is also underdeveloped. To protect the baby in utero and during the first few months is maternal IgG transported by the umbilical cord. Once the source of maternal antibodies is severed at birth the antibody’s titers drop rapidly as the neonate’s production of IgG begins to rise and the maternal antibodies are catabolized. The rate of catabolism is usually more rapid than the rate of production causing immunoglobulin levels to be at a minimum at 5-6 months old. This period leaves the infant more susceptible to infection. Clinical Implication: The first few months after maternal antibodies protect birth the infant they receive across the placenta. The maternal antibodies are catabolized and completely disappear by 10 months. Although the neonate begins producing IgG at birth, they do not reach protective levels until 6 months of age. Geriatric: old age results in decreased T-cell activity and reductions in cell-mediated response to infection. The thymus reaches about 15% of its maximum size by middle age causing a decrease in thymic capacity to mediate T-cell differentiation. B-cell function is altered by deceases in specific antigen production in response to antigens, increases in circulating immune complexes and autoantibodies (antibodies against self antigens) and a decrease in the number of circulating memory B cells. Clinical implication: T-cell activity id deficient in older adults causing an increased susceptibility to infection. Antibody production to specific antigens is inferior. [Show More]
Last updated: 3 years ago
Preview 1 out of 10 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$12.50
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Jan 17, 2021
Number of pages
10
Written in
All
Additional information
This document has been written for:
Uploaded
Jan 17, 2021
Downloads
0
Views
89







 – University of the People.png)