*NURSING > MED-SURG EXAM > MEDSURGE NUR1200Med Surge 2 Midterm 1 (All)
MEDSURGE NUR1200Med Surge 2 Midterm 1
Document Content and Description Below
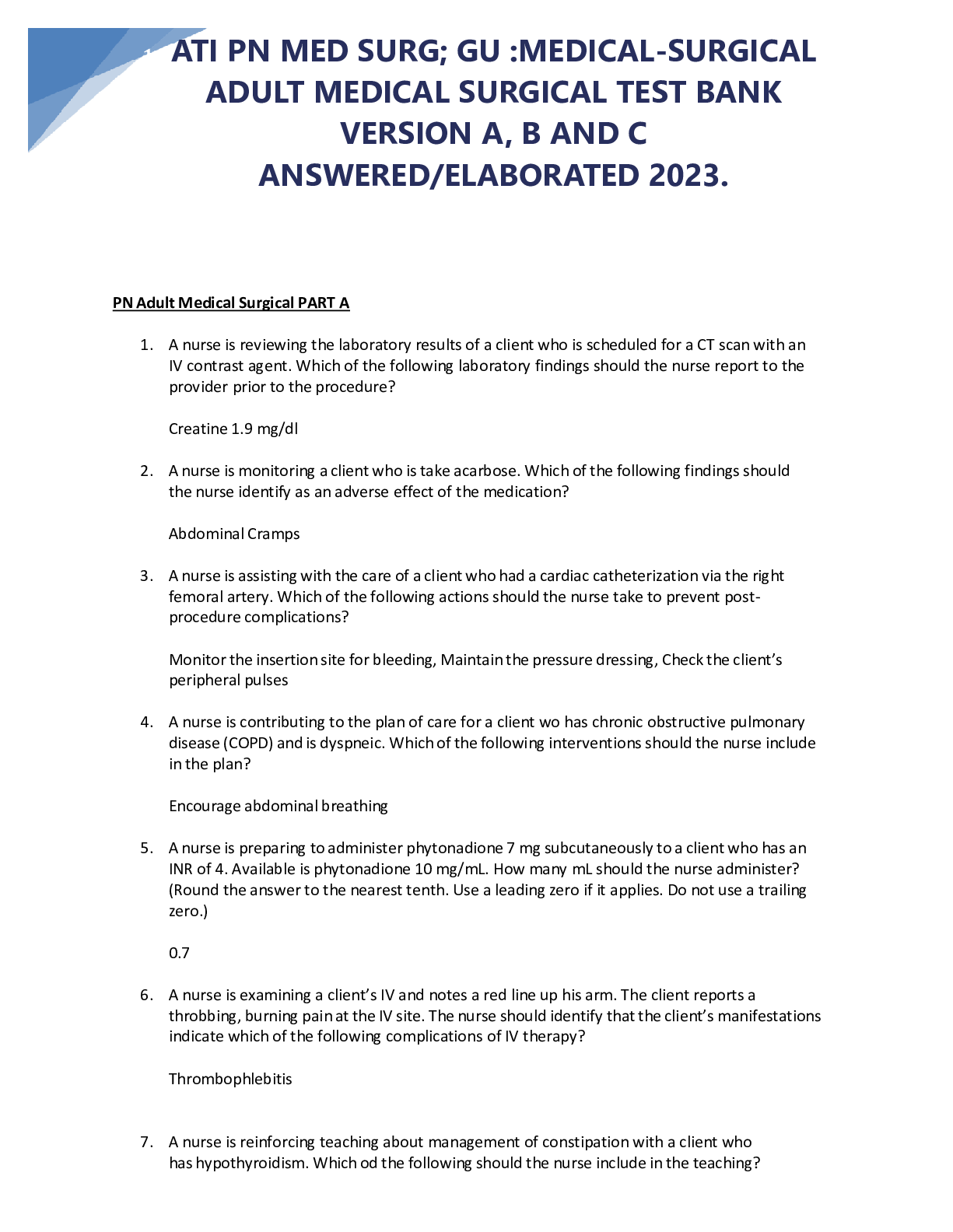
MEDSURGE NUR1200Med Surge 2 Midterm 1 Med-Surg 2 Mid-term 1. Which area of the alimentary canal is the most commonly affected by Crohn’s disease? a. Descending colon b. Ascending colon c. Termi ... nal ileum d. Sigmoid colon Answer: C 2. A client taking the prescribed dose of phenytoin to control seizures. Results of a phenytoin blood level study reveal a level of 18 mcg/mL. Which finding would be expected as a result of this laboratory result? a. Hypotension b. Slurred speech c. No abnormal finding d. Tachycardia Answer: C Rationale: The therapeutic phenytoin level is 10 to 20 mcg/mL. At a level higher than 20 mcg/mL, involuntary movements of the eyeballs (nystagmus) occur. At a level higher than 30 mcg/mL, ataxia and slurred speech occur 3. Which of the following dietary measures would be useful in preventing esophageal reflux? a. Eating small, frequent meals b. Increasing fluid intake with meals c. Adding a bedtime snack to the dietary plan d. Include milk with meals Answer: A Rationale: Esophageal reflux worsens when the stomach is overdistended with food. Therefore, an important measure is to eat small, frequent meals. Fluid intake should be decreased during meals to reduce abdominal distention. Milk does not prevent esophageal reflux. Food intake in the evening should be strictly limited to reduce the incidence of nighttime reflux, so bedtime snacks are not recommended. 4. The nurse is caring for a patient admitted with acute diverticulitis who responded well to the antibiotic therapy and the inflammation subsided. Prior to discharge the nurse should instruct the patient to increase which of the following foods in the diet? a. Oatmeal, barley, whole wheat flakes b. Tomatoes, peas, corn c. Cucumbers, popcorn, figs d. Peas, blackberries, okraAnswer: A Rationale: During diverticulitis the client consumes a clear liquid diet without fiber. After the resolution of diverticulitis the client returns to a high fiber diet without food with seed or cellulose skin. 5. A client is diagnosed with Intracranial Pressure. Nursing interventions include: a. Avoid: straining, cough, seizures, fever, opioids b. All other options are correct c. Head elevated, neck in neutral position d. Avoid elevation of legs or flexion of the hips Answer: B 6. A client diagnosed with dementia is disoriented, wandering, has a decreased appetite, and is having trouble sleeping. What is the priority nursing problem for this client? a. Disturbed though processes b. Risk for injury and safety c. Altered sleep pattern d. Imbalanced nutrition: less than required Answer: B Rationale: Safety is the priority nursing problem because clients with dementia are not cognitively aware of potential dangers 7. To help prevent aspiration while feeding a patient who has a right-sided paralysis, the nurse includes which interventions? (Select all that apply) a. Avoid mixing foods with different textures b. Place the patient in high Fowler’s position c. Place food in the left side of the mouth d. Instruct the patient to tilt the head and neck forward e. Instruct the patient to drink liquids through a straw Answer: A,B,C,D Rationale: Drinking through a straw rather than sipping from a cup increases the risk for aspiration. All other options will reduce the risk of aspiration in a stroke victim8. Nursing interventions related to Lumbar puncture are all except: a. Keep the patient in NPO before the procedure b. No Aspirin, clopidogrel or anticoagulants c. Empty bladder before the procedure d. Keep the patient in flat rest several hours after lumbar puncture Answer: A Rationale: Nursing interventions for lumbar puncture: -No need for NPO -Empty bladder -R/O ICP -NO: ASA, clopidogrel or anticoagulants -Position Post procedure: Flat rest for several hours 9. Following a supratentorial craniotomy to relieve increased intracranial pressure (ICP), the nurse will implement which intervention? a. Place drip to absorb cerebrospinal fluid drainage from the nose or ears b. Decrease frequency of deep breath and cough to every 4 hours c. Elevate the head of the bed 30 to 45 degrees d. Keep the patient stimulated to better assess changing level consciousness Answer: C Rationale: The head of bed is elevated to aid in reduction of ICP. Drip pads, patient stimulation, and changing positions frequently may increase ICP. 10. The nurse is assigned to care for a patient with achalasia. The nurse understands that the patient is likely to have which of the following clinical manifestations related to this diagnosis? a. Silent abdomen and lower quad pain b. Dysphagia and chest pain c. Frequent nausea and diarrhea d. Slow peristalsis and constipation Answer: B 11. A client with which of the following conditions may be likely to develop colo-rectal cancer? a. Adenomatous polyps b. Peptic ulcer disease c. Hemorrhoidsd. Diverticulitis Answer: A 12. Risk factors for colon cancer includes all except: a. High fiber diet b. Ulcerative colitis/Crohn’s disease c. Age older than 50 years d. Family history first degree Answer: A 13. A child seizure disorder has been prescribed carbamazepine. The child is being discharged home with the parent. Which statement made by the parent shows that discharge teaching was effective? a. “I will reduce the dose if my child becomes too sleepy with this drug.” b. “I will not allow my child to go swimming at any moment.” c. “I will place padded tongue blades in the bedroom and kitchen.” d. “I will call if my child presents sore throat or mouth ulcers.” Answer: D Rationale: Carbamazepine can produce leukopenia which manifests with sore throat and mouth ulcer. Blood testing (CBC) and medical attention are required. 14. The nurse is caring for an infant with a tentative diagnosis of pyloric stenosis. The nurse would anticipate what test to be done to confirm this diagnosis? a. Hemoconcentration with increased sodium and potassium b. Barium swallow (upper GI series) c. Anterior and lateral x-ray of the abdomen d. A colonoscopy with biopsy Answer: B Rationale: Upper GI series with barium demonstrate the pyloric stenosis and obstruction 15. A 68-year-old male has been admitted to the hospital with abdominal pain, anemia and melena. He complains of feeling weak and dizzy. He needs to urinate and move his bowels. The nurse should intervene by: a. Asking a male UAP to transfer him to BR for privacy b. Transferring him to BR in a wheelchair c. Helping him to bed side commoded. Offering him the bedpan and the urinal Answer: D Rationale: The client is weak and presenting symptoms of orthostatic hypotension. The client should not be allowed to get out of bed because of risk of falling 16. A patient is admitted to the Emergency Department with a large brain tumor is presenting with Cushing’s triad. A nurse would expect to find which of the following manifestations? (Select all that apply) a. Tachypnea b. Widening pulse pressure c. Diastolic hypertension d. Hyperreflexia e. Systolic hypertension f. Bradycardia Answer: B,E,F 17. Which of the following definitions best describes diverticulosis? a. The partial impairment of the forward flow of intestinal contents b. An abnormal protrusion of the mucosa in the intestinal lumen c. An inflamed outpouching of the intestine d. A non-inflamed outpouching of the intestine Answer: D Rationale: Diverticulosis are non inflamed outpouching of the intestine, more frequent localized in the left side of colon 18. A nurse is assisting a health care provider (HCP) with an assessment of a child with a diagnosis of suspected appendicitis. In assessing the intensity and progression of the pain, the health care provider palpates the child at McBurney’s point. The nurse understands that McBurney’s point is located midway between the: a. Left anterior superior iliac spine and the umbilicus b. Left anterior inferior iliac spine and the umbilicus c. Right posterior inferior iliac spine and the umbilicus d. Right anterior superior iliac spine and the umbilicus Answer: D Rationale: McBurney’s point is midway between the right anterior superior iliac spine and the umbilicus. It is usually the location of greatest pain in the child with appendicitis19. The nurse is providing postoperative teaching to a patient with transient ischemic attack (TIA). Which of the following teaching points should the nurse be certain to include in teaching? a. The patient will need to have assistance at home for a while. b. TIAs are a significant warning sign of impending stroke. c. Rehabilitative therapy may be required for up to 2 months. d. The patient may need to move to an assisted living facility. Answer: B 20. Transient ischemic attack (TIA) includes all except: a. Diplopia b. Ataxia/vertigo c. Dysarthria/aphasia d. Other permanent focal neurologic dysfunction Answer: D Rationale: Symptoms of TIA includes: Amaurosis fugax (retinal ischemia: belief episode of blindness in one eye) Diplopia Dysarthria/aphasia Sensory and/or motor deficits Ataxia/vertigo [Show More]
Last updated: 3 years ago
Preview 1 out of 14 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$12.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Nov 08, 2022
Number of pages
14
Written in
All
Additional information
This document has been written for:
Uploaded
Nov 08, 2022
Downloads
0
Views
99