Health Assessment - NUR 2092 Exam 1 (Muskus),100% CORRECT
Document Content and Description Below
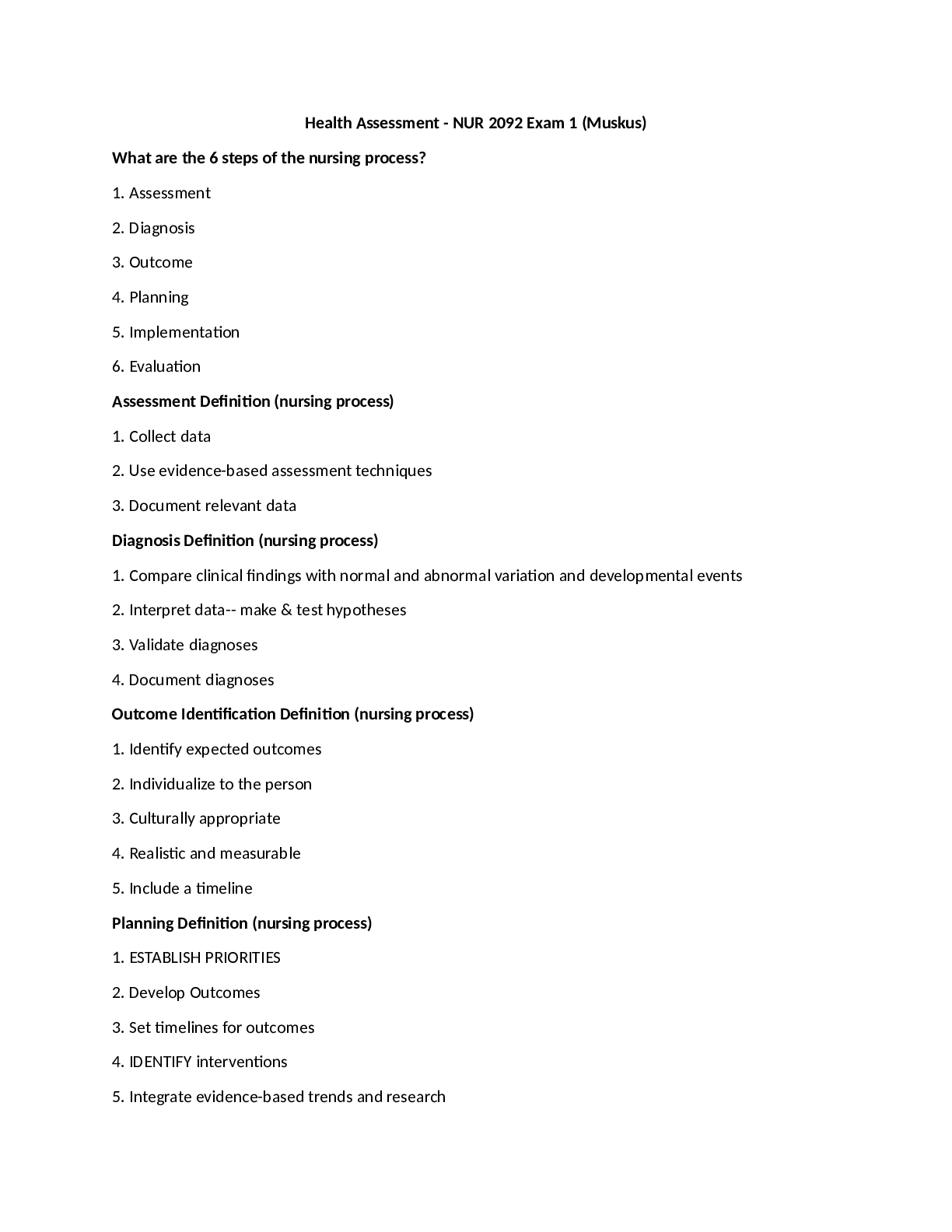
What are the 6 steps of the nursing process? 1. Assessment 2. Diagnosis 3. Outcome 4. Planning 5. Implementation 6. Evaluation Assessment Definition (nursing process) 1. Collect data 2. Use... evidence-based assessment techniques 3. Document relevant data Diagnosis Definition (nursing process) 1. Compare clinical findings with normal and abnormal variation and developmental events 2. Interpret data-- make & test hypotheses 3. Validate diagnoses 4. Document diagnoses Outcome Identification Definition (nursing process) 1. Identify expected outcomes 2. Individualize to the person 3. Culturally appropriate 4. Realistic and measurable 5. Include a timeline Planning Definition (nursing process) 1. ESTABLISH PRIORITIES 2. Develop Outcomes 3. Set timelines for outcomes 4. IDENTIFY interventions 5. Integrate evidence-based trends and research 6. Document plan of care Implementation Definition (nursing process) 1. Implement in a safe and timely manner 2. Use evidence-based interventions 3. Collaborate with colleagues 4. Use community resources 5. Coordinate care delivery 6. Provide health teaching and health promotion 7. Document implementation and any modifications. Evaluation Definition (nursing process) 1. Progress toward outcomes 2. Conduct systematic, ongoing, criterion-based evaluation. 3. Include patient and significant others 4. Use ongoing assessment to revise diagnoses, outcomes, and plan 5. Distribute results to patient and family Acute pain 1. Is short term and self-limiting, often follows a predictable trajectory, and dissipates after an injury heals. 2.Self-protective purpose; it warns the individual of actual or threatened tissue damage. Chronic Pain 1.Over 6 months in duration 2.Adaptive responses Phantom pain 1. Pain where limb used to exist Malignant pain Vs nonmalignant pain 1. Malignant pain is cancer-related and is caused by tumor cells that cause necrosis or stretching. 2. Nonmalignant pain is often associated with musculoskeletal conditions. Visceral pain Originates from internal organs. Somatic pain and deep somatic pain 1. Somatic pain originates from musculoskeletal tissues or the body surface 2. Deep somatic pain comes from sources such as blood vessels, joints, tendons, muscles, and bone. Referred pain Pain that is felt at a particular site but originates from another location. Nociceptive pain 1. Develops when functioning and intact nerve fibers in CNS are stimulated. 2. They are triggered by events outside nervous system from actual or potential tissue damage. 3.Nociception can be divided into four phases: (1) Transduction: (2) Transmission: the pain impulse moves from the level of the spinal cord to the brain. (3) Perception: signifies the conscious awareness of a painful sensation (4) Modulation: a built-in mechanism that will eventually slow down and stop the processing of a painful stimulus Neuropathic pain 1. Pain caused by a lesion or disease of the somatosensory nervous system. 2. This implies an abnormal processing of pain message from an INJURY to the NERVE FIBERS. 3. This pain is very difficult to treat and assess. Subjective Data Pain is always subjective. What the patient is complaining of; SYMPTOM Objective data What the nurse observes; SIGN Nutritional Status This balance is affected by many factors, including physiologic, psychosocial, developmental, cultural, and economic factors Nutritional Assessment Food intake 24 hour recall Food diary Food frequency Direct observation Anthropometric measurements Swallowing assessment prn Lab tests Pain assessment tools 1. Brief pain inventory: asks the patient to rate the pain within the past 24 hours using graduated scales (0 to 10) with respect to its impact on areas such as mood, walking ability, and sleep 2. McGill Pain Questionnaire: The short-form McGill Pain, asks the patient to rank a list of descriptors in terms of their intensity and to give an overall intensity rating to his or her pain 3. Initial Pain assessment: asks the patient to answer 8 questions concerning location, duration, quality, intensity, and aggravating/relieving factors. 4. Pain rating scales 5. Wong-Baker Faces pain rating scale Pain Assessment Posture/behavior Facial expression Sounds Skin inspection/palpation BP/pulse/respirations Pupil size How to assess domestic violence "Abuse assessment screen" is a tool used by many healthcare providers. Pulse Oximetry Noninvasive Estimate arterial oxygen saturation in blood Normal Resp. Rate for adult 10-20 Normal BP for Adult 120/80 BMI requirements for being underweight, normal weight, overweight, obese. Underweight = 18.5 BMI Normal weight = 18.5- 24.9 BMI Overweight= 25-29.9 BMI Obese= 30+ BMI How to document pulse 0=absent 1+= weak 2+= normal 3+= bounding Definition of Eupnea Normal/good breathing Definition of Apnea Breathing has stopped What does the acronym PQRSTU stand for? P= Precipitating/palliative/provocative, what brings it on? What were you doing when you noticed it? Q= Quality or Quantity, how does it feel, sound? How intense/severe is it? R=Region or Radiation, Where is it? Does it spread anywhere? S= Severity Scale, Scale of 1-10. Is it getting better/worse? T= Timing/ onset. When did it first occur? Duration? How long did it last? Frequency? U= Understand patient's perception of the problem. What do you think it means? Vital Signs Influences Blood Pressure Age Gender Race Diurnal variations Emotions Pain Personal habits Weight Respiratory Rate Exercise and anxiety Heart Rate (Pulse) Exercise, age, gender, anxiety, pain Temperature Diurnal variations - Lowest early AM, highest late afternoon/early evening Exercise – rises Menstrual cycle – increase mid cycle ovulation to menses Age – very young wider variation; older typically lower Drinks hot or cold Normal pulse rate for adult 50-90 What happens to BP if cuff is too small or big? If too small it will increase BP If too big it will lower BP Normal Oral temp + range 98.6. Range of 96.4 to 99.1 Is it normal for new born infant’s rectal temps to be higher? Yes, average is 100 How do you measure BP cuff size? With of bladder should equal 40% of circumference of persons arm. Length of bladder should equal 80% of circumference. What is the working phase of the interview? The working phase is the data-gathering phase. What are the steps to the "Tools of a physical Assessment", 4 Steps 1. Inspection—Visual examination of body 2. Palpation—texture, temp., rigidity, lumps, masses 3. Percussion—to evaluate size, borders, consistency, tenderness, extent of fluid 4. Auscultation—listening to sounds body produces; pitch, loud or soft, duration, and quality Delirium Vs Dementia 1. Delirium is an ACUTE confusion state 2. Dementia is a CHRONIC progressive loss of cognitive & intellectual functions. Disorientation, judgment loss, memory loss, impaired. Complete total health database Includes complete health history and full physical examination Describes current and past health state and forms baseline to measure all future changes Yields first diagnoses Episodic or problem-centered database For limited or short-term problems Concerns mainly one problem, one cue complex, or one body system History and examination follow direction of presenting concern Follow-up database Status of all identified problems should be evaluated at regular and appropriate intervals Note changes that have occurred Evaluate whether problem is getting better or worse Identify coping strategies being used Emergency database Rapid collection of data, often compiled concurrently with lifesaving measures Diagnosis must be rapid and comprehensive in nature Two primary components of health assessment Health history Physical examination Health history = Subjective data Physical Assessment – Objective Data Therapeutic Communication Open ended questions: narrative information; tell me about you, how are you doing today? Closed ended questions: specific information; do you have pain BARRIERS TO COMMUICATION Lack of interest or attention/ lack of respect Physical barriers – a curtain, a door, a computer, a monitor, pain, room temperature The patient’s inability to hear you, hearing deficit, or language barrier Language/ use of jargon, or speaking above someone's educational level Safety – fear Psychological barriers – embarrassment, disbelief, shock, anger, fear, grief, fatigue, hostility Culture Nonphysical traits – values, attitudes, beliefs, customs Race – Identification of individuals or groups by shared genetic heritage and biological or physical characteristics Ethnicity – associated with culture; awareness of belonging to a group in which certain characteristics differentiate from one group to another Material – dress, tools, art and ways they are used NON material – verbal and nonverbal language, beliefs, customs, social structures. Ethnocentrism – to believe one’s own beliefs or way of life as ‘superior’ Acculturation– Adapting to and acquiring another culture Assimilation– Developing new cultural identity and becoming like the dominant culture; more two way; new affecting old Biculturalism– Divided loyalty, identifies with two cultures Causes of illness Biomedical Disease caused by bacteria, viruses, etc. Involves scientific theories for cause of illness Naturalistic Illness caused when there is loss of natural balance May align with yin/yang, hot & cold theory Magicoreligious Illness caused by supernatural force May use folk remedies Culturally Competent Know self, understand own heritage Identify meaning of health to someone else Understand health care delivery system Gain knowledge re social backgrounds of clients Be familiar with language, resources for interpreters, and resources within community 6 steps of nursing process Assessment Diagnosis Outcome identification Planning Implementation Evaluation Assessment Interview, health history, ROS, physical examination, functional assessment, spiritual and cultural assessment Subjective data What patient SAYS Objective data What you OBSERVE SMART component in outcome identification Specific Measurable Attainable Relevant Time bound First level priority Emergent situations, life threading and needs immediate attention Second level priority Requires attention to avoid further deterioration Third level priorirty Can be addressed after more important problems are addressed Complete total health Database Full health history, and physical exam Yields first diagnosis Current and past health state Focused or problem centered database Limited and short term problems Concerned with mainly one problem, or one body system Follow up database Follow up care to evaluate if problem is getting better or worse Emergency database Rapid urgent collection of data Radio diagnosis Primary prevention Preventing health problems Ex: vaccines, safety glasses Secondary prevention Timely screenings to catch a problem early and reduce impact Example: mammograms Tertiary prevention Decrease impact of ongoing problem Example: cardiac rehab, support group. 2 primary components of health assessment Health history= subjective Physical examination = objective PQRSTU method of pain assessment Provocative/ palliative Quality/ quantity Region/ radiation Severity scale Timing (onset) Understand patient perception of the problem Organic disorder Disorder of the brain Psychiatric disorders Not yet determined to be organic More complete mental assessment maybe necessary if: Patients has anxiety/depression If family is concerned Deterioration in status from last visit Aphasia Acute psychiatric illness Objective cues of mental health ABCT Appearance Behavior Cognitive function Thought process Delirium Sudden onset Altered consciousness Rapid mood swings Rapid, inappropriate, rambling speech Can be reversed Can cause fever, pain, low blood glucose, infection Dementia Slow and gradual onset Flat agitation Consciousness not altered Repetitious speech Can't be reverse Can cause HIV, chronic alcoholism, Alzheimer's Ethnocentrism belief in the superiority of one's own ethnic group Ethnicity Associated with culture Awareness of belonging to a group in which certain characteristics differentiate from one group to another Race Identification of individual groups by shared genetic heritage and biological or physical characteristics Acculturation Adapting to and acquiring another culture Assimilation Developing a new culture identity and becoming like the dominant culture Biculturalism Identifies with two cultures Biomedical cause of illness Disease caused by bacteria, viruses Involves scientific theories Naturalistic cause of illness Illness caused due to loss of natural balance Yin/yang or hot and cold theory Magioreligious Illness caused by supernatural forces Percussion The sharp striking of one thing against another. Used to evaluate the size, borders, consistency, tenderness, extent of fluid Striking produces vibration Direct percussion Sinuses, CVA tenderness Indirect percussion Thorax, abdomen Flatness Bone or muscle Dullness Heart, liver, spleen Resonance Air filled lungs. Hollow Hyper resonance an abnormal booming sound produced during percussion of the lungs. Emphysematous lung Tympany Air filled stomach (drumlike) Auscultation Listening to sound produced by body Pulse oximetry Estimates oxygen saturation in blood Normal value: 95-100% COPD patients might have high 80s Temperature Normal range: 96.4 to 99.1 F Most accurate temperature Rectal Pulse Normal range 50-95 bpm Ear canal in older Pull and up Ear canal in children Pull and down Pulse and respiration rate is _________ in infants Faster Nociceptive pain Acute pain starts outside the nervous system Responsive to anti-inflammatory and opiates Neuropathic pain Chronic pain Abnormal processing Numbness, tingling, shooting, burning, phantom pain From injury to nerve fibers or CNS Phantom pain Pain felt in a body part that is no longer there Referred pain Felt at a site different from organ affected Breakthrough pain Pain restarts or escalates before next scheduled analgesic dose What does OLDCARTS stand for? Onset Location Duration Characteristics Aggravating/associated factor Relieving factors Treatments thus far Significance of symptoms When do you use "old carts"? Whenever a patient reports a symptom, it needs to be explored What does IPPA stand for? Inspection Palpation Percussion Auscultation -perform in that order What is an assessment? Collection of data about the individual’s health state Compare subjective and objective data. Subjective data is what the person says about themselves during history taking; objective data is data you observe by inspecting, percussing, palpating, and auscultating during the physical exam What elements form the database? -patients record -lab studies -subjective data (in pt. history) -objective data (in physical) What is the purpose of assessment? Make a judgement or diagnoses What is diagnostic reasoning? Process of analyzing health data and drawing conclusions to identify diagnoses What are the six phases of the nursing process? 1. Assessment 2. Diagnosis 3. Outcome identification 4. Planning 5. Implementation 6. Evaluation What are the six parts of a health assessment? -review of the clinical record -health history -physical examination -functional assessment -risk assessment -review of the literature What is a nursing diagnosis? A clinical judgement about a person’s response to an actual or potential health state What are the three types of nursing diagnoses? 1. Actual diagnoses 2. Risk diagnoses 3. Wellness diagnoses What is a medical diagnosis? Diagnosis that evaluates the cause or etiology of the disease What are the four different types of databases? -complete -focused or problem centered -follow-up -emergency What is a complete database? Complete health history and full physical exam What is a focused or problem centered database? For a limited or a short term problem What is a follow up database? When the status of identified problems are evaluated at regular and appropriate intervals What is an emergency database? A rapid collection of data, diagnosis must be swift and sure After completing an initial assessment of a patient, the nurse has charted that his respirations are eupneic and his pulse is 58 beats per minute. These types of data would be: Objective A patient tells the nurse that he is very nervous, is nauseated, and "feels hot." These types of data would be: Subjective The patient's record, laboratory studies, objective data, and subjective data combine to form the: Data base When listening to a patient's breath sounds, the nurse is unsure of a sound that is heard. The nurse's next action should be to: Validate the data by asking a coworker to listen to the breath sounds The nurse is conducting a class for new graduate nurses. During the teaching session, the nurse should keep in mind that novice nurses, without a background of skills and experience from which to draw, are more likely to make their decisions using: A set of rules Expert nurses learn to attend to a pattern of assessment data and act without consciously labeling it. These responses are referred to as: Intuition The nurse is reviewing information about evidence-based practice (EBP). Which statement best reflects EBP? EBP emphasizes the use of best evidence with the clinician's experience The nurse is conducting a class on priority setting for a group of new graduate nurses. Which is an example of a first-level priority problem? Individual with shortness of breath and respiratory distress When considering priority setting problems, the nurse keeps in mind that second-level priority problems include which of these aspects? Abnormal laboratory values Which critical thinking skill helps the nurse see relationships among the data? Clustering related cues The nurse knows that developing appropriate nurse interventions for a patient relies on the appropriateness of the ________ diagnosis Nursing The nursing process is a sequential method of problem solving that nurses use and includes which steps? Assessment, diagnosis, outcome identification, planning, implementation, and evaluation A newly admitted patient is in acute pain, has not been sleeping well lately, and is having difficulty breathing. How should the nurse prioritize these problems? Breathing, pain, sleep Which of these would be formulated by a nurse using diagnostic reasoning? Diagnostic hypothesis Barriers to incorporating EBP include: Nurses' lack of research skills in evaluating the quality of research studies What step of the nursing process includes data collection by health history, physical examination, and interview? Assessment During a staff meeting, nurses discuss the problems with accessing research studies to incorporate evidence based clinical decision making into their practice. Which suggestion by the nurse manager would best help these problems? Teach the nurses how to conduct electronic searches for research studies When reviewing the concepts of health, the nurse recalls that the components of holistic health include with of these? Holistic health views the mind, body, and spirit as interdependent The nurse recognizes that the concept of prevention in describing health is essential because: Prevention places the emphasis on the link between health and personal behavior The nurse is performing a physical assessment on a newly admitted patient. An example of objective information obtained during the physical assessment includes the: 2x5 cm scar on the right lower forearm A visiting nurse is making an initial home visit for a patient who has many chronic medical problems. Which type of data base is more appropriate to collect in this setting? A complete health data base because of the nurse’s primary responsibility for monitoring the patient's health Which situation is more appropriate during which the nurse performs a focused or problem centered history? Patient in an outpatient clinic has cold and influenza-like symptoms A patient is at the clinic to have her blood pressure checked. She has been coming to the clinic weekly since she changed medications 2 months ago. The nurse should: Collect a follow-up data base and then check her blood pressure A patient is brought by ambulance to the emergency department with multiple traumas received in an automobile accident. He is alert and cooperative, but his injuries are quite severe. How would the nurse proceed with data collection? Simultaneously ask history questions while performing the examination and initiating life-saving measures A 42-year-old patient of Asian descent is being seen at the clinic for an initial examination. The nurse knows that including cultural information in his health assessment is important to: Provide culturally sensitive and appropriate care In the health promotional model, the focus of the health professional includes: Helping the consumer choose a healthier lifestyle The nurse has implemented several planned interventions to address the nursing diagnosis of acute pain. Which would be the next appropriate action? Evaluate the individual's condition, and compare actual outcomes with expected outcomes Which statement best describes a proficient nurse? A proficient nurse is one who: Understands a patient situation as a whole rather than a list of tasks and recognizes the long-term goals for the patient The nurse is reviewing data collected after an assessment. Of the data listed below, which would be considered related cues that would be clustered together during data analysis? Select all that apply. a. Inspiratory wheezes noted in left lower lobes c. Nonproductive cough e. Patient reports dyspnea upon exertion f. Rate of respirations 16 breaths per minute Put the following patient situations in order according to the level of priority. 1st: A teenager who was stung by a bee during a soccer match is having trouble breathing. 2nd: An older adult with a urinary tract infection is also showing signs of confusion and agitation. 3rd: A patient newly diagnosed with type 2 diabetes mellitus does not know how to check his own blood glucose levels with a glucometer. A teenager who was stung by a bee during a soccer match is having trouble breathing. First level priority problems An older adult with a urinary tract infection is also showing signs of confusion and agitation Second level priority problems A patient newly diagnosed with type 2 diabetes mellitus does not know how to check his own blood glucose levels with a glucometer. Third level priority problems The nurse is reviewing data collected after an assessment. Of the data listed below, which would be considered related cues that would be clustered together during data analysis? Inspiratory wheezes notes in the left lower lobes, Nonproductive cough, Patient reports dyspnea upon exertion, Rate of respirations 16 breaths per minute [Show More]
Last updated: 2 years ago
Preview 1 out of 14 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$16.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Feb 13, 2021
Number of pages
14
Written in
Additional information
This document has been written for:
Uploaded
Feb 13, 2021
Downloads
0
Views
73