*NURSING > CASE STUDY > Jean Kelly _ Sepsis_SKINNY_Reasoning_Urinary tract Infection/Urosepsis | Part I: Recognizing RELEVA (All)
Jean Kelly _ Sepsis_SKINNY_Reasoning_Urinary tract Infection/Urosepsis | Part I: Recognizing RELEVANT Clinical Data
Document Content and Description Below
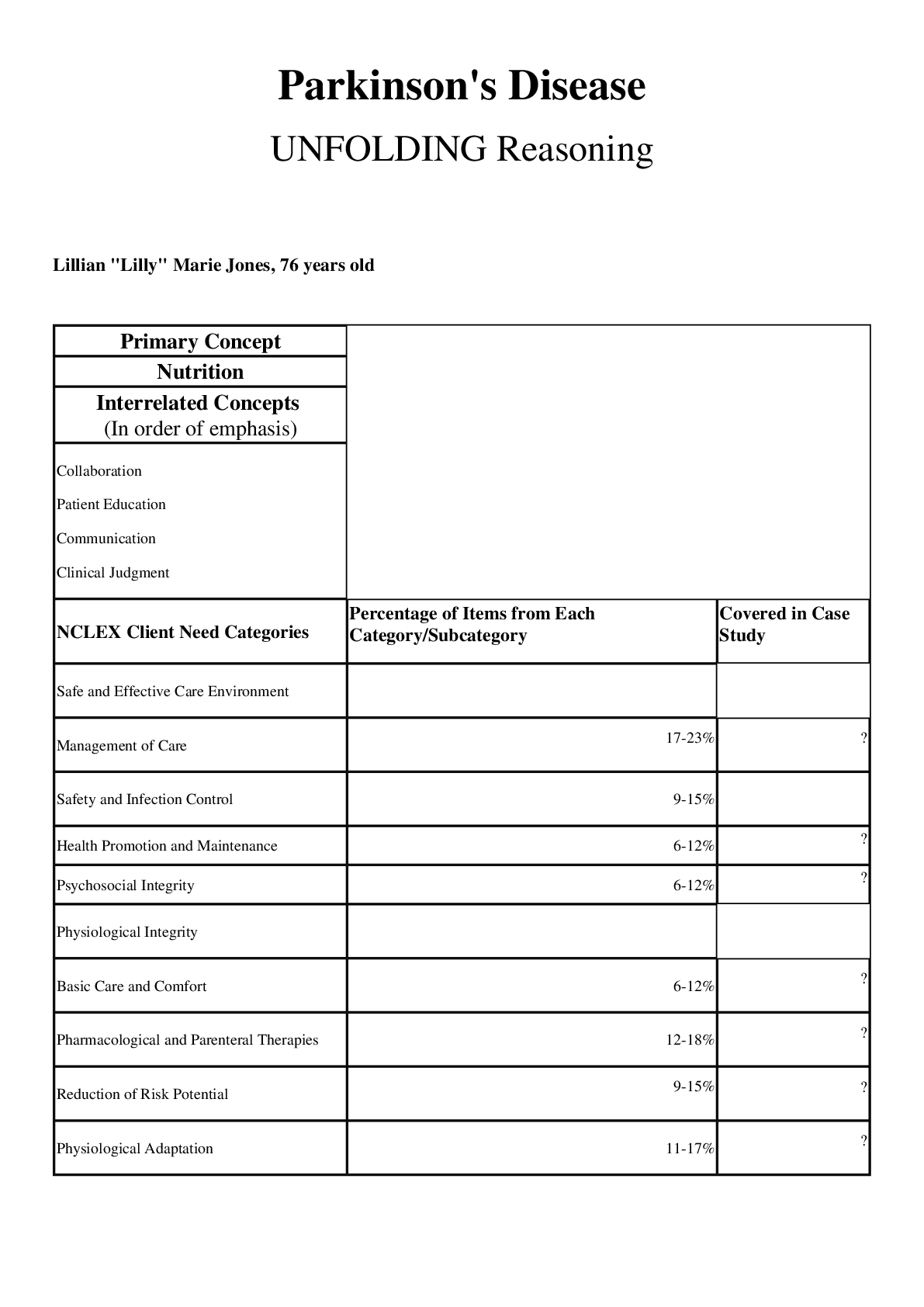
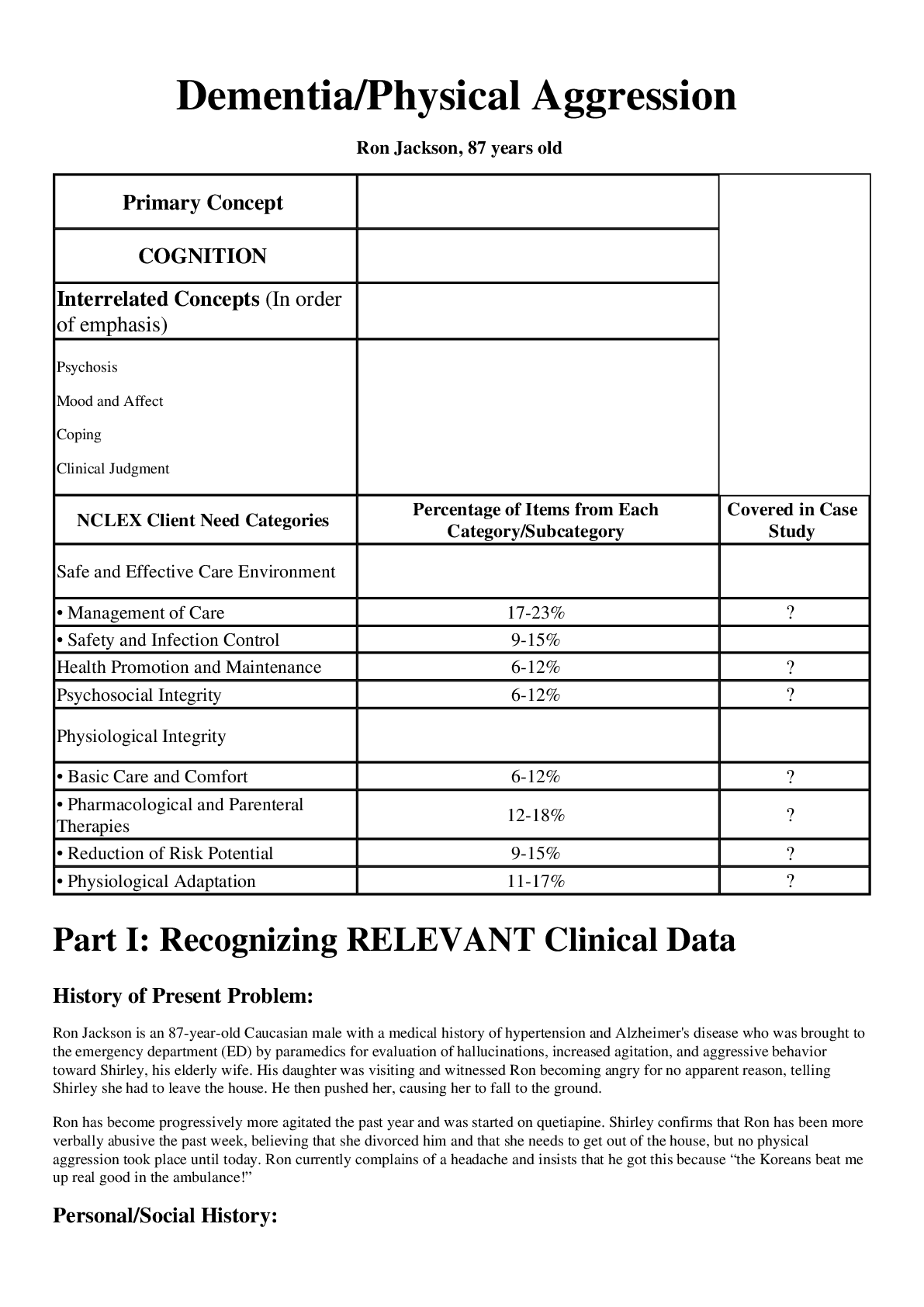
Jean Kelly _ Sepsis_SKINNY_Reasoning_Urinary tract Infection/Urosepsis | Part I: Recognizing RELEVANT Clinical Data Urinary Tract Infection/Urosepsis Jean Kelly, 82 years old Primary C... oncept Perfusion Interrelated Concepts (In order of emphasis) • Infection • Clinical Judgment • Patient Education NCLEX Client Need Categories Percentage of Items from Each Category/Subcategory Covered in Case Study Safe and Effective Care Environment • Management of Care 17-23% • Safety and Infection Control 9-15% Health Promotion and Maintenance 6-12% Psychosocial Integrity 6-12% Physiological Integrity • Basic Care and Comfort 6-12% • Pharmacological and Parenteral Therapies 12-18% • Reduction of Risk Potential 9-15% • Physiological Adaptation 11-17% SKINNY Reasoning Part I: Recognizing RELEVANT Clinical Data History of Present Problem: Jean Kelly is an 82-year-old woman who has been feeling more fatigued the last three days and has had a fever the last twenty-four hours. She reports a painful, burning sensation when she urinates as well as frequency of urination the last week. Her daughter became concerned and brought her to the emergency department (ED) when she did not know what day it was. She is mentally alert with no history of confusion. While taking her bath today, she was weak and unable to get out of the tub and used her personal life alert button to call for medical assistance. Personal/Social History: Jean lives independently in a senior apartment retirement community. She is widowed and has two daughters who are active and involved in her life. What data from the histories are important and RELEVANT and have clinical significance for the nurse? RELEVANT Data from Present Problem: Clinical Significance: More fatigued for the last 3 days Fever the last 24 hours Painful, burning sensation when she urinates as well as frequency of urination the last week Did not know what day it was. She is mentally alert with no history of confusion While taking her bath today, she was weak and unable to get out of the tub and used the help button to call for medical assistance. Though a general complaint, when clustered with the other symptoms of fever this is indicating that there is a likely PROBLEM present. Fever reflects the systemic inflammatory response initiated by the immune system and is there for a reason - to help the body fight off invading micro-organisms by increasing the production of neutrophils; the first responders of the immune system that are macrophages. The elevated temp also makes it less hospitable for bacteria to thrive and multiply. These symptoms are classic with a urinary tract infection (UTI). Suspecting a urinary infection, the nurse needs to know that if a patient meets the SIRs criteria, they should suspect sepsis. With an infection of any kind, sepsis is identified by having 2 or more of the following criteria of Systemic Inflammatory Response Syndrome (SIRS): • Temp >100.4 or <96.8 • HR >90 • RR >20 • WBC >12,000 or <4000 • Bands >10% New onset of confusion is always a clinical RED FLAG in the elderly, and when CLUSTERED with other symptoms is not representing a neurologic problem, but is commonly seen with an infection such as a UTI. This confirms the weakness and fatigue she has had the past 3 days. It is severe weakness and a clinical RED FLAG if she is unable to get out of the bath tub and needed to call for assistance. RELEVANT Data from Social History: Clinical Significance: Jean lives independently in a senior apartment retirement community. She is widowed and has two daughters who are active and involved in her life. Is functioning at a high level for an 82-year-old woman and is independent at this time. It is important for the nurse to re-evaluate the functional status anytime there is a hospital admission to ensure safety. If there is ever a question, consult social services. Supportive family is a positive influence that will increase her ability to maintain current autonomy. Patient Care Begins: Current VS: P-Q-R-S-T Pain Assessment (5th VS): T: 101.8 F/38.8 C (oral) Provoking/Palliative: Nothing/Nothing P: 110 (regular) Quality: Ache R: 24 (regular) Region/Radiation: Right flank - - - - - - - - - - - - -EMOTIONAL (How to develop a therapeutic relationship): Discuss the following principles needed as conditions essential for a therapeutic relationship: • Rapport • Trust • Respect • Genuineness • Empathy SPIRITUAL: • F-Faith or beliefs: What are your spiritual beliefs? Do you consider yourself spiritual? What things do you believe in that give meaning to life? • I-Importance and influence: Is faith important to you? How has your illness or hospitalization affected your belief practices? • C-Community: Are you connected to a faith center in the community? Does it provide support/comfort for you during times of stress? Is there a person/group who assists you in your spirituality? • A-Address: What can I do for you? What support can healthcare provide to support your spiritual beliefs/practices? These questions, if used in this scenario by the nurse, would naturally explore this patient’s spirituality. It is always best if the nurse has some comfort in the exploration of spirituality. Patients can sense discomfort or anxiety in approaching this portion of the assessment. The FICA model offers some open-ended questions to make spiritual assessment a natural part of the conversation. Use this spiritual assessment tool to make caring for the spirit an essential component of your nursing practice! Faith/beliefs are supported CULTURAL Considerations (IF APPLICABLE) Since religious worldviews provide a window to the prevailing values and ethnic norms of any cultural group, knowledge, and understanding of the most dominant religions of ethnic groups in your community are essential and will facilitate cultural sensitivity. But remember that there will always be exceptions, so be careful not to make assumptions! Becoming knowledgeable about another cultural group and integrating this knowledge into your practice is the essence of becoming culturally competent. It means respecting each patient’s cultural diversity and examining how their beliefs may affect their health care. When nursing care does not intersect with the patient’s worldview or belief set, compliance with the proposed treatment plan will be less likely (Ward, 2012). Cultural beliefs are supported 5. What educational/discharge priorities need to be addressed to promote health and wellness for this patient and/or family? (Health Promotion and Maintenance) o Though sepsis is not entirely preventable, as it relates to fluid volume deficit, and PREVENTING a UTI, the importance of INCREASING fluid intake must also be addressed. o With the elderly, it is always important to address safety in the home. She will most likely be weak from the hospitalization so she may need to spend some time in a rehab facility. Also important to include family in the plan of care. o Other educational priorities that are indirectly related to decreasing risk of infection include excellent control of blood glucose. Reinforce foundational tenets of diabetes education: diet, medications, exercise, and monitoring blood glucose/frequency of daily checks. Author Keith Rischer, RN, MA, CEN, CCRN Reviewers • Linda L. Gilbert, MSN, RN, Clinical Coordinator, Goodwin College, East Hartford, Connecticut • Julie A. Hogue, RN, MSN, Nursing Instructor, Illinois Valley Community College, Oglesby, Illinois • Sarah R. Pierce, DNP, AGACNP-BC, CCRN, PLNC, Freed-Hardeman University, Henderson, Tennessee References Badlissi, F., Schumacher, H., Adebajo, A., & Underwood, M. (2015). Gout. Retrieved from www.epocrates.com Bush, E. (2001). The use of human touch to improve the well-being of older adults: A holistic nursing intervention. Journal of Holistic Nursing, (19)3, 256-270. Daniels, R., Richmond, L., Andrus, P., & Walker, D. (2015). Sepsis in adults. Retrieved from www.epocrates.com Neviere, R. (2016). Sepsis syndrome in adults. Epidemiology, definitions, clinical presentation, diagnosis, and prognosis. Retrieved from www.uptodate.com Rex-Smith, A. (2007). Something more than presence. Journal of Christian Nursing, 24(2), 82–87. Sommers, M.S. & Fannin, E. (2015). Diseases and disorders: A nursing therapeutic manual. (5th ed.). Philadelphia, PA: F.A. Davis Company. Swanson, K. M. (1991). Empirical development of a middle range theory of caring. Nursing Research, 40(3), 161–166. Vallerand, A.H., Sanoski, C.A., & Deglin, J.H. (2014) Davis’s drug guide for nurses. (14th ed.). Philadelphia, PA: F.A. Davis Company. Van Leeuwen, A. & Bladh, M.L. (2015). Davis’s comprehensive handbook of laboratory and diagnostic tests with nursing implications. (6th ed.). Philadelphia, PA: F.A. Davis Company. Ward, J. (2012). Five strategies for a culturally competent patient care. Retrieved from http://www.nursetogether.com/5strategies-culturally-competent-patient-care#sthash.BroQf68H.dpuf [Show More]
Last updated: 2 years ago
Preview 1 out of 13 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$10.50
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Feb 21, 2021
Number of pages
13
Written in
Additional information
This document has been written for:
Uploaded
Feb 21, 2021
Downloads
0
Views
129






 - Georgia Southern University.png)


