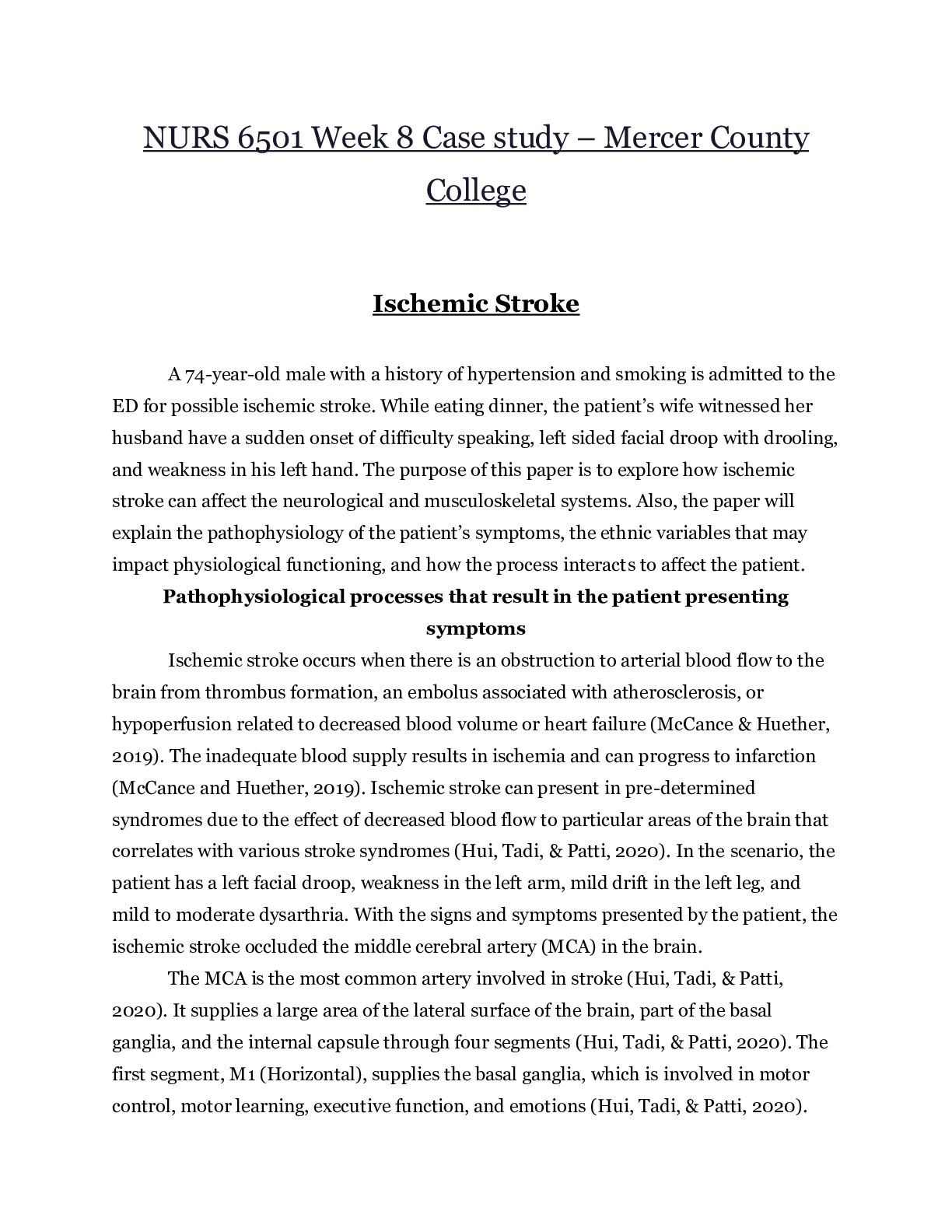
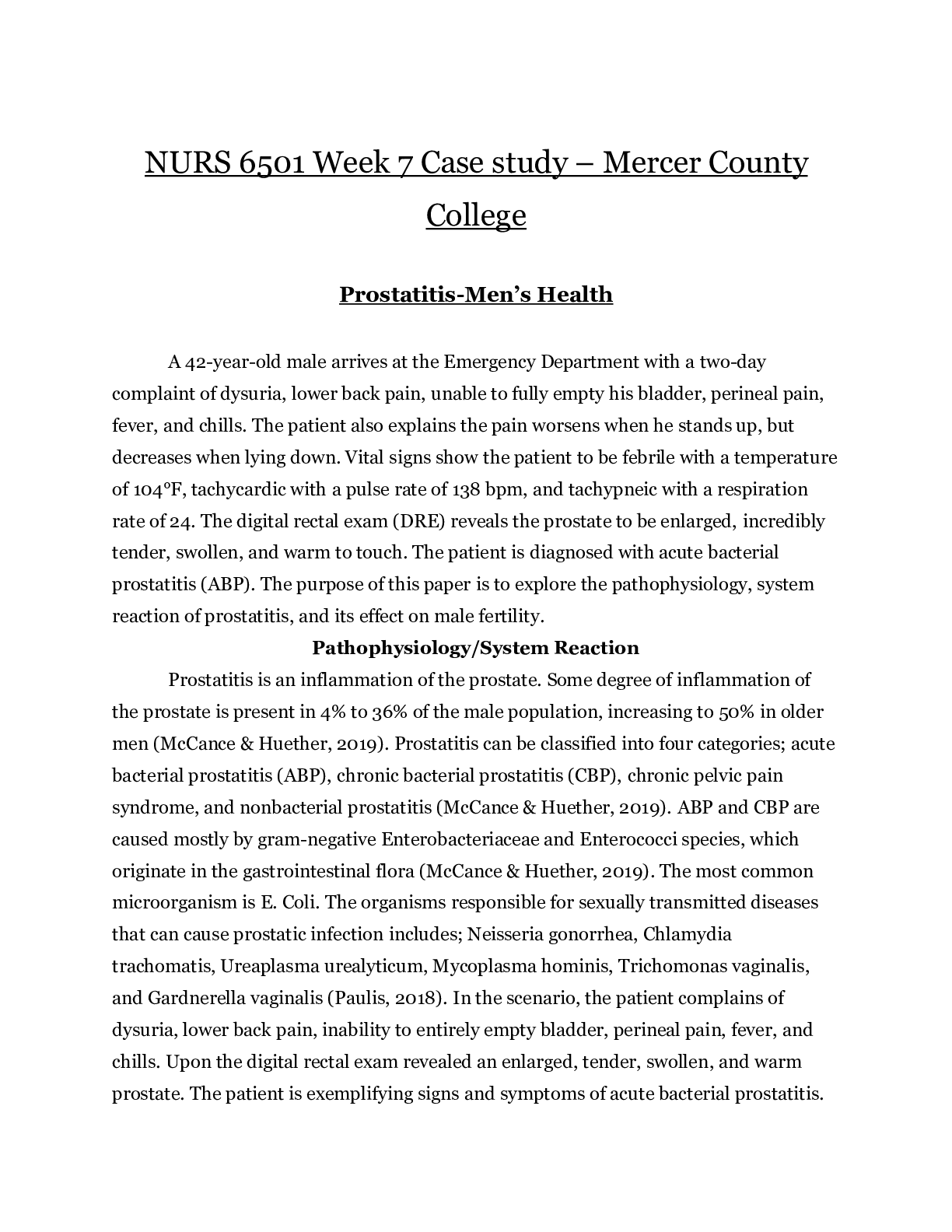
Pneumonia-COPD
Joan Walker, 84 years old
Primary Concept
Gas Exchange
Interrelated Concepts (In order of emphasis)
1. Infection
2. Acid-Base Balance
3. Thermoregulation
4. Clinical Judgement
5. PainHistory of P
...
Pneumonia-COPD
Joan Walker, 84 years old
Primary Concept
Gas Exchange
Interrelated Concepts (In order of emphasis)
1. Infection
2. Acid-Base Balance
3. Thermoregulation
4. Clinical Judgement
5. PainHistory of Present Problem:
Joan Walker is an 84-year-old female who has had a productive cough of green phlegm that
started four days ago that continues to persist. She was started three days ago on prednisone 40
mg PO daily and azithromycin (Zithromax) 250 mg PO x5 days by her clinic physician. Though
she has had intermittent chills, she had a fever last night of 102.0 F/38.9 C. She has had more
difficulty breathing during the last night and has been using her albuterol inhale every 1-2 hours
with no improvement so she called 9-1-1 and is brought to the emergency department (ED)
where you are the nurse who will be responsible for her care.
Personal/Social History:
Joan was widowed six months ago after 64 years of marriage and resides in assisted living. She
is a retired elementary school teacher. She called her pastor before coming to the ED and he has
now arrived and came back with the patient. The nurse walked in the room when the pastor
asked Joan if she would like to pray. The patient said to her pastor, “Yes please, I feel that this
may be the beginning of the end for me!”
What data from the histories is RELEVANT and has clinical significance to the nurse?
RELEVANT Data from Present Problem Clinical Significance:
Productive cough of green phlegm four
days ago that persists.
Started three days ago on prednisone 60
mg PO daily and azithromycin 250 mg
PO x5 days by her clinic physician.
Fever last night of 102.0
More difficulty breathing during the
night and has been using her albuterol
inhaler every 1-2 hours with no
improvement
Productive cough is a clinical manifestation.
Sputum in shades of
yellow- green indicates bacterial infection.
This respiratory infection was treated by an
antibiotic and steroids.
Nurse determine if treatment was effective,
Response to bacterial infection. Inflammatory
response.
Recurrent pneumonia is a common
complication of COPD and a
frequent cause of COPD exacerbation
RELEVANT Date from Social History Clinical Significance
She called her pastor and he has now
arrived and came back with the patient.
The nurse walked in the room when the
pastor asked Joan if she would like to
pray.
The patient said, “Yes, this may the
beginning of the end for me!”
Joan values spirituality. Spirituality is
important to patient and the nurse must be
sensitive
Emotional support will be a priority for
diseasePatient Care Begins:
Current VS: P-Q-R-S-T Pain Assessment (5th VS):
T: 103.2 F/39.6 C (oral) Provoking/Palliative: Deep breath/Shallow breathing
P: 110 (regular) Quality: Ache
R: 30 (labored) Region/Radiation: Generalized over right side of chest with
no radiation
BP: 178/96 Severity: 3/10
O2 sat: 86% 6 liters n/c Timing: Intermittent-lasting a few seconds
What VS data is RELEVANT and must be recognized as clinically significant by the nurse?
RELEVANT VS Data Clinical Significance:
T: 103.2 F/39.6 C (oral)
P: 110 (regular)
R: 30 (labored)
BP: 178/96
O2 sat: 86% 6 liters n/c
Pain: 3/10, ache, generalized over right side
of chest with no radiation, intermittentlasting
a few secs
Elevated due to infection
Elevated due to stress
Elevated due to Pneumonia/COPD
Elevated due to anxiety and stress
Elevated O2 is contraindicated in patients
with COPD
Pain level still should be assessed and
monitored,
Current Assessment:
GENERAL
APPEARANCE:
Appears anxious and in distress, barrel chest present
RESP: Dyspnea with use of accessory muscles, breath sounds very
diminished bilaterally and/post with scattered expiratory wheezing
CARDIAC: Pale, hot & dry, no edema, heart sounds regular—S1S1, pulses
strong, equal with palpation at radial/pedal/post-tibial landmarks
NEURO: Alert & oriented to person, place, time, and situation (x4)
GI: Abdomen soft/non-tender, bowel sounds audible per auscultation in
all 4 quadrants
GU: Voiding without difficulty, urine clear/yellow
SKIN: Skin integrity intact, skin turgor elastic, no tenting present
What assessment data is RELEVANT and must be recognized as clinically significant by the
nurse?
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
8. What nursing interventions will you initiate if this complication develops?
Respiratory failure
• Contact respiratory therapy stat to place on bipap
• Call a code if continues to decompensate to facilitate needed intubation
Sepsis/septic shock
• Call “Rapid Response” if team available in facility
• Establish second IV, preferably a large bore IV (18 g).
• Obtain VS every 15 minutes to TREND closely.
• Contact primary care provider as soon as change in status is identified as well as need to
transfer to ICU.
• Initiate IV bolus of at
9. What psychosocial needs will this patient and/or family have that will need to be addressed?
• Knowledge and education about what is taking place
• Emotional support
• Spiritual support
10. How will the nurse address these psychosocial needs?
Knowledge and education regarding illness and plan of care
- The nurse can integrate patient/family education naturally while providing care by simply
explaining at their level
everything that the nurse/physician has ordered and why it needs to be done.
Spiritual Support
- Spiritual care/support will be limited to encouragement, providing hope, and determining if the
patient would like to
have a chaplain or their spiritual leader notified.
Emotional support
-Being present and available for the patient and their family
- Once admitted, it would be appropriate to ask open-ended questions to assessCaring and the “Art” of Nursing
1. What is the patient likely experiencing/feeling right now in this situation?
The patient is probably anxious and. Supporting the patient and family by giving them as much
information about
their current status and explaining the plan of care is important .
2. What can you do to engage yourself with this patient’s experience and show that she
matters to you as a person?
Acknowledging Joan spiritually an offering support.
Use Reflection to THINK Like a Nurse
Reflection-IN-action (Tanner, 2006) is the nurse’s ability to accurately interpret the patient’s
response to an intervention in the moment as the events are unfolding to make a correct clinical
judgement.
1. What did you learn from this scenario?
I learned that Pneumonia and COPD are critical diseases and should be assessed frequently
2. How can I use what has been learned from this scenario t improve patient care in the
future?
I will use this to help me in the future create a care plan for Pneumonia and COPD patients and
use my new
knowledge to support the patient.
Brandi Griffin
[Show More]