*NURSING > QUESTIONS & ANSWERS > PEDS FINAL QUESTIONS TEST BANK, chapter 1 to chapter 35 questions & explained answers; A+ guide (lat (All)
PEDS FINAL QUESTIONS TEST BANK, chapter 1 to chapter 35 questions & explained answers; A+ guide (latest 2020).
Document Content and Description Below
PEDS FINAL QUESTIONS TEST BANK CHAPTER 1: 2. Which is the leading cause of death in infants younger than 1 year in the United States? a. Congenital anomalies b. Sudden infant death syndrome c. Di ... sorders related to short gestation and low birth weight d. Maternal complications specific to the perinatal period 3. What is the major cause of death for children older than 1 year in the United States? a. Heart disease b. Childhood cancer c. Unintentional injuries d. Congenital anomalies 4. In addition to injuries, what are the leading causes of death in adolescents ages 15 to 19 years? a. Suicide and cancer b. Suicide and homicide c. Drowning and cancer d. Homicide and heart disease 7. The nurse should assess which age group for suicide ideation since suicide in which age group is the third leading cause of death? a. Preschoolers b. Young school age c. Middle school age d. Late school age and adolescents 15. The nurse is aware that which age group is at risk for childhood injury because of the cognitive characteristic of magical and egocentric thinking? a. Preschool b. Young school age c. Middle school age d. Adolescent 8. Parents of a hospitalized toddler ask the nurse, What is meant by family-centered care? The nurse should respond with which statement? a. Family-centered care reduces the effect of cultural diversity on the family. b. Family-centered care encourages family dependence on the health care system. c. Family-centered care recognizes that the family is the constant in a childs life. d. Family-centered care avoids expecting families to be part of the decision-making process. 13. The nurse is planning care for a hospitalized preschool-aged child. Which should the nurse plan to ensure atraumatic care? a. Limit explanation of procedures because the child is preschool aged. b. Ask that all family members leave the room when performing procedures. c. Allow the child to choose the type of juice to drink with the administration of oral medications. d. Explain that EMLA cream cannot be used for the morning lab draw because there is not time for it to be effective. CHAPTER 2 8. How is family systems theory best described? a. The family is viewed as the sum of individual members. b. A change in one family member cannot create a change in other members. c. Individual family members are readily identified as the source of a problem. d. When the family system is disrupted, change can occur at any point in the system. 9. Which family theory is described as a series of tasks for the family throughout its life span? a. Exchange theory b. Developmental theory c. Structural-functional theory d. Symbolic interactional theory 10. Which family theory explains how families react to stressful events and suggests factors that promote adaptation to these events? a. Interactional theory b. Family stress theory c. Eriksons psychosocial theory d. Developmental systems theory 24. The nurse is planning to counsel family members as a group to assess the familys group dynamics. Which theoretic family model is the nurse using as a framework? a. Feminist theory b. Family stress theory c. Family systems theory d. Developmental theory 12. Which type of family should the nurse recognize when a mother, her children, and a stepfather live together? a. Traditional nuclear b. Blended c. Extended d. Binuclear 15. When assessing a family, the nurse determines that the parents exert little or no control over their children. This style of parenting is called which? a. Permissive b. Dictatorial c. Democratic d. Authoritarian 17. Which is a consequence of the physical punishment of children, such as spanking? a. The psychologic impact is usually minimal. b. The childs development of reasoning increases. c. Children rarely become accustomed to spanking. d. Misbehavior is likely to occur when parents are not present. a. Send the child to his or her room if the child has one. b. A general rule for length of time is 1 hour per year of age. c. Select an area that is safe and nonstimulating, such as a hallway. d. If the child cries, refuses, or is more disruptive, try another approach. The area must be nonstimulating and safe. The child becomes bored in this environment and then changes behavior to rejoin activities. The childs room may have toys and activities that negate the effect of being separated from the family. The general rule is 1 minute per year of age. An hour per year is excessive. When the child cries, refuses, or is more disruptive, the time-out does not start; the time-out begins when the child quiets. 27. The nurse is explaining different parenting styles to a group of parents. The nurse explains that an authoritative parenting style can lead to which child behavior? a. Shyness b. Self-reliance c. Submissiveness d. Self-consciousness 28. Parents of a preschool child ask the nurse, Should we set rules for our child as part of a discipline plan? Which is an accurate response by the nurse? a. It is best to delay the punishment if a rule is broken. b. The child is too young for rules. At this age, unrestricted freedom is best. c. It is best to set the rules and reason with the child when the rules are broken. d. Set clear and reasonable rules and expect the same behavior regardless of the circumstances. 2. The parents of a 5-year-old child ask the nurse how they can minimize misbehavior. Which responses should the nurse give? (Select all that apply.) a. Set clear and reasonable goals. b. Praise your child for desirable behavior. c. Dont call attention to unacceptable behavior. d. Teach desirable behavior through your own example. e. Dont provide an opportunity for your child to have any control. 11. Which type of family should the nurse recognize when the paternal grandmother, the parents, and two minor children live together? a. Blended b. Nuclear c. Extended d. Binuclear CHAPTER 6 3. A 4-month-old infant comes to the clinic for a well-infant checkup. Immunizations she should receive are DTaP (diphtheria, tetanus, acellular pertussis) and IPV (inactivated poliovirus vaccine). She is recovering from a cold but is otherwise healthy and afebrile. Her older sister has cancer and is receiving chemotherapy. Nursing considerations should include which? a. DTaP and IPV can be safely given. b. DTaP and IPV are contraindicated because she has a cold. c. IPV is contraindicated because her sister is immunocompromised. d. DTaP and IPV are contraindicated because her sister is immunocompromised. 4. Which serious reaction should the nurse be alert for when administering vaccines? a. Fever b. Skin irritation c. Allergic reaction d. Pain at injection site 7. Which vitamin supplementation has been found to reduce both morbidity and mortality in measles? a. A b. B1 c. C d. Zinc Evidence suggests that vitamin A supplementation reduces both morbidity and mortality in measles. 14. Herpes zoster is caused by the varicella virus and has an affinity for which? a. Sympathetic nerve fibers b. Parasympathetic nerve fibers c. Lateral and dorsal columns of the spinal cord d. Posterior root ganglia and posterior horn of the spinal cord 18. Which is usually the only symptom of pediculosis capitis (head lice)? a. Itching b. Vesicles c. Scalp rash d. Localized inflammatory response 20. The nurse should know what about Lyme disease? a. Very difficult to prevent b. Easily treated with oral antibiotics in stages 1, 2, and 3 c. Caused by a spirochete that enters the skin through a tick bite d. Common in geographic areas where the soil contains the mycotic spores that cause the disease 22. The nurse is preparing an airborne infection isolation room for a patient. Which communicable disease does the patient likely have? a. Varicella b. Pertussis c. Influenza d. Scarlet fever 25. The nurse is preparing to administer a measles, mumps, rubella, and varicella (MMRV) vaccine. Which is a contraindication associated with administering this vaccine? a. The child has recently been exposed to an infectious disease. b. The child has symptoms of a cold but no fever. c. The child is having intermittent episodes of diarrhea. d. The child has a disorder that causes a deficient immune system. 28. The nurse is assessing a child suspected of having pinworms. Which is the most common symptom the nurse expects to assess? a. Restlessness b. Distractibility c. Rectal discharge d. Intense perianal itching 1. The nurse is planning care for a child with chickenpox (varicella). Which prescribed supportive measures should the nurse plan to implement? (Select all that apply.) a. Administration of acyclovir (Zovirax) b. Administration of azithromycin (Zithromax) c. Administration of Vitamin A supplementation d. Administration of acetaminophen (Tylenol) for fever e. Administration of diphenhydramine (Benadryl) for itching 2. The nurse is planning care for an infant with candidiasis (moniliasis) diaper dermatitis. Which topical ointments may be prescribed for the patient? (Select all that apply.) a. Nystatin b. Bactroban c. Neosporin d. Miconazole e. Clotrimazole 5. The nurse is planning to administer immunizations to a 6-month-old infant. Which interventions should the nurse implement to minimize local reactions from the vaccines? (Select all that apply.) a. Select a needle length of 1 inch. b. Administer in the deltoid muscle. c. Inject the vaccine into the vastus lateralis. d. Draw the vaccine up from a vial with a filter needle. e. Change the needle on the syringe after drawing up the vaccine and before injecting. 6. The nurse is preparing to admit a 5-year-old child who developed lesions of varicella (chickenpox) 3 days ago. Which clinical manifestations of varicella should the nurse expect to observe? (Select all that apply.) a. Nonpruritic rash b. Elevated temperature c. Discrete rose pink rash d. Vesicles surrounded by an erythematous base e. Centripetal rash in all three stages (papule, vesicle, and crust) 7. The nurse is preparing to admit a 1-year-old child with pertussis (whooping cough). Which clinical manifestations of pertussis should the nurse expect to observe? (Select all that apply.) a. Earache b. Coryza c. Conjunctivitis d. Low-grade fever e. Dry hacking cough 8. The nurse is preparing to admit a 2-year-old child with rubella (German measles). Which clinical manifestations of rubella should the nurse expect to observe? (Select all that apply.) a. Sore throat b. Conjunctivitis c. Koplik spots d. Lymphadenopathy e. Discrete, pinkish red maculopapular exanthema CHAPTER 10 1. At which age does an infant start to recognize familiar faces and objects, such as his or her own hand? a. 1 month b. 2 months c. 3 months d. 4 months 2. During the 2-month well-child checkup, the nurse expects the infant to respond to sound in which manner? a. Respond to name. b. React to loud noise with Moro reflex. c. Turn his or her head to side when sound is at ear level. d. Locate sound by turning his or her head in a curving arc. 3. Which characteristic best describes the fine motor skills of an infant at age 5 months? a. Neat pincer grasp b. Strong grasp reflex c. Builds a tower of two cubes d. Able to grasp object voluntarily 4. The nurse is checking reflexes on a 7-month-old infant. When the infant is suspended in a horizontal prone position, the head is raised and the legs and spine are extended. Which reflex is this? a. Landau b. Parachute c. Body righting d. Labyrinth righting 5. In terms of gross motor development, what should the nurse expect an infant age 5 months to do? a. Sit erect without support. b. Roll from the back to the abdomen. c. Turn from the abdomen to the back. d. Move from a prone to a sitting position. 6. At which age can most infants sit steadily unsupported? a. 4 months b. 6 months c. 8 months d. 12 months 7. By which age should the nurse expect that an infant will be able to pull to a standing position? a. 5 to 6 months b. 7 to 8 months c. 11 to 12 months d. 14 to 15 months 8. According to Piaget, a 6-month-old infant should be in which developmental stage? a. Use of reflexes b. Primary circular reactions c. Secondary circular reactions d. Coordination of secondary schemata 9. At which age do most infants begin to fear strangers? a. 2 months b. 4 months c. 6 months d. 12 months 10. At which age should the nurse expect most infants to begin to say mama and dada with meaning? a. 4 months b. 6 months c. 10 months d. 14 months 11. At which age should the nurse expect an infant to begin smiling in response to pleasurable stimuli? a. 1 month b. 2 months c. 3 months d. 4 months 12. The nurse is discussing development and play activities with the parent of a 2-month-old boy. Which statement by the parent would indicate a correct understanding of the teaching? a. I can give my baby a ball of yarn to pull apart or different textured fabrics to feel. b. I can use a music box and soft mobiles as appropriate play activities for my baby. c. I should introduce a cup and spoon or pushpull toys for my baby at this age. d. I do not have to worry about appropriate play activities at this age. 13. What is an appropriate play activity for a 7-month-old infant to encourage visual stimulation? a. Playing peek-a-boo b. Playing pat-a-cake c. Imitating animal sounds d. Showing how to clap hands 14. What information should be given to the parents of a 12-month-old child regarding appropriate play activities for this age? a. Give large pushpull toys for kinetic stimulation. b. Place a cradle gym across the crib to help develop fine motor skills. c. Provide the child with finger paints to enhance fine motor skills. d. Provide a stick horse to develop gross motor coordination. 15. The parents of a 2-month-old boy are concerned about spoiling their son by picking him up when he cries. What is the nurses best response? a. Allow him to cry for no longer than 15 minutes and then pick him up. b. Babies need comforting and cuddling. Meeting these needs will not spoil him. c. Babies this young cry when they are hungry. Try feeding him when he cries. d. If he isnt soiled or wet, leave him, and hell cry himself to sleep. 16. The nurse is interviewing the father of a 10-month-old girl. The child is playing on the floor when she notices an electrical outlet and reaches up to touch it. Her father says no firmly and moves her away from the outlet. The nurse should use this opportunity to teach the father what? a. That the child should be given a time-out b. That the child is old enough to understand the word no c. That the child will learn safety issues better if she is spanked d. That the child should already know that electrical outlets are dangerous 19. An infant, age 6 months, has six teeth. The nurse should recognize that this is what? a. Normal tooth eruption b. Delayed tooth eruption c. Unusual and dangerous d. Earlier than expected tooth eruption 22. At what age is it safe to give infants whole milk instead of commercial infant formula? a. 6 months b. 9 months c. 12 months d. 18 months 25. What is the best age to introduce solid food into an infants diet? a. 2 to 3 months b. 4 to 6 months c. When birth weight has tripled d. When tooth eruption has started 26. The parent of 2-week-old infant asks the nurse if fluoride supplements are necessary because the infant is exclusively breastfed. What is the nurses best response? a. The infant needs to begin taking them now. b. Supplements are not needed if you drink fluoridated water. c. The infant may need to begin taking them at age 6 months. d. The infant can have infant cereal mixed with fluoridated water instead of supplements. 27. An infant, age 5 months, is brought to the clinic by his parents for a well-baby checkup. What is the best advice that the nurse should include at this time about injury prevention? a. Keep buttons, beads, and other small objects out of his reach. b. Do not permit him to chew paint from window ledges because he might absorb too much lead. c. When he learns to roll over, you must supervise him whenever he is on a surface from which he might fall. d. Lock the crib sides securely because he may stand and lean against them and fall out of bed. 30. The parent of an 8.2-kg (18-lb) 9-month-old infant is borrowing a federally approved car seat from the clinic. The nurse should explain that the safest way to put in the car seat is what? a. Front facing in back seat b. Rear facing in back seat c. Front facing in front seat with air bag on passenger side d. Rear facing in front seat if an air bag is on the passenger side 32. The nurse is performing an assessment on a 12-month-old infant. Which fine or gross motor developmental skill demonstrates the proximodistal acquisition of skills? a. Standing b. Sitting without assistance c. Fully developed pincer grasp d. Taking a few steps holding onto something 33. An infant weighed 8 lb at birth and was 18 inches in length. What weight and length should the infant be at 5 months of age? a. 12 lb, 20 inches b. 14 lb, 21.5 inches c. 16 lb, 23 inches d. 18 lb, 24.5 inches 35. The nurse is teaching parents about expected language development for their 6-month-old infant. The nurse recognizes the parents understand the teaching if they make which statement? a. Our baby should comprehend the word no. b. Our baby knows the meaning of saying mama. c. Our baby should be able to say three to five words. d. Our baby should begin to combine syllables, such as dada. 36. The nurse is performing an assessment on a 10-week-old infant. The nurse understands that the developmental characteristic of hearing at this age is which? a. The infant responds to his own name. b. The infant localizes sounds by turning his head directly to the sound. c. The infant turns his head to the side when sound is made at the level of the ear. d. The infant locates sound by turning his head to the side and then looking up or down. MULTIPLE RESPONSE 1. The nurse is teaching a group of parents at a community education program about introducing solid foods to their infants. Which recommendations should the nurse include? (Select all that apply.) a. Spoon feeding should be introduced after an entire milk feeding. b. It is best to introduce a wide variety of foods during the first year. c. As solid food consumption increases, the quantity of milk should decrease. d. Introduction of low-calorie milk and food should be done by the end of the first year. e. Introduction of citrus fruits, meats, and eggs should be delayed until after 6 months of age. f. Each new food item should be introduced at 5- to 7-day intervals. 6. The clinic nurse is assessing a 6-month-old infant during a well-child appointment. The nurse should use which approaches to alleviate the infants stranger anxiety? (Select all that apply.) a. Talk in a loud voice. b. Meet the infant at eye level. c. Avoid sudden intrusive gestures. d. Maintain a safe distance initially. e. Pick up the infant and hold him or her closely. 7. The nurse is evaluating a 7-month-old infants cognitive development. Which behaviors should the nurse anticipate evaluating? (Select all that apply.) a. Imitates sounds b. Shows interest in a mirror image c. Comprehends simple commands d. Actively searches for a hidden object e. Attracts attention by methods other than crying 8. The nurse is planning play activities for a 2-month-old hospitalized infant to stimulate the auditory sense. Which activities should the nurse implement? (Select all that apply.) a. Talk to the infant. b. Play a music box. c. Place a squeaky doll in the crib. d. Give the infant a small-handled clear rattle. MATCHING Match each neurologic reflex that appears in infancy to its description. a. Labyrinth righting b. Body righting c. Otolith righting d. Landau e. Parachute 1. When the body of an erect infant is tilted, the head is returned to an upright, erect position. 2. An infant in the prone or supine position is able to raise his or her head. 3. Turning the hips and shoulders to one side causes all the other body parts to follow. 4. When the infant is suspended in a horizontal prone position and suddenly thrust downward, the hands and fingers extend forward as if to protect against falling. 5. When the infant is suspended in a horizontal prone position, the head is raised and the legs and spine are extended. CHAPTER 12 2. What do the psychosocial developmental tasks of toddlerhood include? a. Development of a conscience b. Recognition of sex differences c. Ability to get along with age mates d. Ability to delay gratification 4. Parents of an 18-month-old boy tells the nurse that he says no to everything and has rapid mood swings. If he is scolded, he shows anger and then immediately wants to be held. What is the nurses best interpretation of this behavior? a. This is normal behavior for his age. b. This is unusual behavior for his age. c. He is not effectively coping with stress. d. He is showing he needs more attention. 5. A 17-month-old child should be expected to be in which stage, according to Piaget? a. Preoperations b. Concrete operations c. Tertiary circular reactions d. Secondary circular reactions 7. A toddler, age 16 months, falls down a few stairs. He gets up and scolds the stairs as if they caused him to fall. What is this an example of? a. Animism b. Ritualism c. Irreversibility d. Delayed cognitive development 8. What is a characteristic of a toddlers language development at age 18 months? a. Vocabulary of 25 words b. Use of holophrases c. Increasing level of understanding d. Approximately one third of speech understandable 9. Which characteristic best describes the gross motor skills of a 24-month-old child? a. Skips b. Broad jumps c. Rides tricycle d. Walks up and down stairs 10. What developmental characteristic does not occur until a child reaches age 2 1/2 years? a. Birth weight has doubled. b. Anterior fontanel is still open. c. Primary dentition is complete. d. Binocularity may be established. 13. A toddlers parent asks the nurse for suggestions on dealing with temper tantrums. What is the most appropriate recommendation? a. Punish the child. b. Explain to child that this is wrong. c. Leave the child alone until the tantrum is over. d. Remain close by the child but without eye contact. 17. A father tells the nurse that his daughter wants the same plate and cup used at every meal, even if they go to a restaurant. The nurse should explain that this is what? a. A sign the child is spoiled b. An attempt to exert unhealthy control c. Regression, which is common at this age d. Ritualism, an expected behavior at this age 20. What is the leading cause of death during the toddler period? a. Injuries b. Infectious diseases c. Childhood diseases d. Congenital disorders 25. The nurse is providing guidance strategies to a group of parents with toddlers at a community outreach program. Which statement by a parent indicates a correct understanding of the teaching? a. I should expect my 24-month-old child to express some signs of readiness for toilet training. b. I should be firm and structured when disciplining my 18-month-old child. c. I should expect my 12-month-old child to start to develop a fear of darkness and to need a security blanket. d. I should expect my 36-month-old child to understand time and proximity of events. 26. The nurse is assessing a toddlers visual acuity. Which visual acuity is considered acceptable during the toddler years? a. 20/20 b. 20/40 c. 20/50 d. 20/60 27. The nurse is teaching parents about toilet training. What should the nurse include in the teaching session? a. Bladder training is accomplished before bowel training. b. The mastery of skills required for toilet training is present at 18 months. c. By 12 months, the child is able to retain urine for up to 2 hours or longer. d. The physiologic ability to control the sphincters occurs between 18 and 24 months. 32. The nurse understands that which guideline should be followed to determine serving sizes for toddlers? a. 1/2 tbsp of solid food per year of age b. 1 tbsp of solid food per year of age c. 2 tbsp of solid food per year of age d. 2 1/2 tbsp of solid food per year of age MULTIPLE RESPONSE 1. The nurse is preparing a staff education program about growth and development of an 18-month-old toddler. Which characteristics should the nurse include in the staff education program? (Select all that apply.) a. Eats well with a spoon and cup b. Runs clumsily and can walk up stairs c. Points to common objects d. Builds a tower of three or four blocks e. Has a vocabulary of 300 words f. Dresses self in simple clothes 2. A parent asks the nurse, When will I know my child is ready for toilet training? The nurse should include what in the response? (Select all that apply.) a. The child should be able to stay dry for 1 hour. b. The child should be able to sit, walk, and squat. c. The child should have regular bowel movements. d. The child should express a willingness to please. 5. A toddler is in the sensorimotor, tertiary circular reactions stage of cognitive development. What behavior should the nurse expect to assess? (Select all that apply.) a. Refers to self by pronoun b. Gestures up and down c. Able to insert round object into a hole d. Can find hidden objects but only in the first location e. Uses future-oriented words, such as tomorrow 6. The nurse is teaching a parent of an 18-month-old about developmental milestones associated with feeding. What should the nurse include in the teaching? (Select all that apply.) a. The child will begin to use a fork. b. The child will be able use a straw and cup. c. The child will be able to hold a cup with both hands. d. The child will be able to drink from a cup with a lid. e. The child will begin to use a spoon but may turn it before reaching the mouth. 9. What child behavior indicates to the nurse that temper tantrums have become a problem? (Select all that apply.) a. The child is 2 to 3 years old b. Tantrums occur at bedtime c. Tantrums occur past 5 years of age d. Tantrums last longer than 15 minutes e. Tantrums occur more than five times a day CHAPTER 13 1. In terms of fine motor development, what should the 3-year-old child be expected to do? a. Tie shoelaces. b. Copy (draw) a circle. c. Use scissors or a pencil very well. d. Draw a person with seven to nine parts. 3. In terms of cognitive development, a 5-year-old child should be expected to do which? a. Think abstractly. b. Use magical thinking. c. Understand conservation of matter. d. Understand another persons perspective. 6. A 4-year-old child tells the nurse that she doesnt want another blood sample drawn because I need all of my insides and I dont want anyone taking them out. What is the nurses best interpretation of this? a. The child is being overly dramatic. b. The child has a disturbed body image. c. Preschoolers have poorly defined body boundaries. d. Preschoolers normally have a good understanding of their bodies. 7. Which type of play is most typical of the preschool period? a. Team b. Parallel c. Solitary d. Associative 8. What characteristic best describes the language skills of a 3-year-old child? a. Asks meanings of words b. Follows directional commands c. Can describe an object according to its composition d. Talks incessantly regardless of whether anyone is listening 12. What dysfunctional speech pattern is a normal characteristic of the language development of a preschool child? a. Lisp b. Echolalia c. Stammering d. Repetition without meaning 16. During the preschool period, the emphasis of injury prevention should be placed on what? a. Limitation of physical activities b. Punishment for unsafe behaviors c. Constant vigilance and protection d. Teaching about safety and potential hazards A 3-year-old child exhibits a more stable appetite than during the toddler years and is more willing to try different foods. A 4-year-old child is imaginative and indulges in telling tall tales and may have an imaginary playmate; these are normal findings, not signs of stress. Also a 4-year-old child has an increasing curiosity in sexuality, which is not a sign of child abuse. A 5-year-old child is usually tranquil, not aggressive like a 4-year-old child. 19. The nurse is explaining average weight gain during the preschool years to a group of parents. Which average weight gain should the nurse suggest to the parents? a. 1 to 2 kg b. 2 to 3 kg c. 3 to 4 kg d. 4 to 5 kg 20. The nurse is planning to bring a preschool child a toy from the playroom. What toy is appropriate for this age group? a. Building blocks b. A 500-piece puzzle c. Paint by number picture d. Farm animals and equipment 21. The nurse is conducting an assessment of fine motor development in a 3-year-old child. Which is the expected drawing skill for this age? a. Can draw a complete stick figure b. Holds the instrument with the fist c. Can copy a triangle and diamond d. Can copy a circle and imitate a cross 23. The nurse is explaining the preconventional stage of moral development to a group of nursing students. What characterizes this stage? a. Children in this stage focus on following the rules. b. Children in this stage live up to social expectations and roles. c. Children in this stage have a concrete sense of justice and fairness. d. Children in this stage have little, if any, concern for why something is wrong. MULTIPLE RESPONSE 1. What developmental achievements are demonstrated by a 4-year-old child? (Select all that apply.) a. Cares for self totally b. Throws a ball overhead c. Has a vocabulary of 1500 words d. Can skip and hop on alternate feet e. Tends to be selfish and impatient f. Commonly has an imaginary playmate 5. What are sources of stress in preschoolers? (Select all that apply.) a. Shares possessions b. Damages or destroys objects c. May fear dogs or other animals d. Seems to be in perpetual motion e. May stutter or stumble over words 8. The nurse is teaching parents of a 3-year-old child about gross motor developmental milestones. What milestones should the nurse include in the teaching session? (Select all that apply.) a. Rides a tricycle b. Catches a ball reliably c. Jumps off the bottom step d. Stands on one foot for a few seconds e. Walks downstairs using alternate footing 9. The nurse is teaching parents of a 4-year-old child about fine motor developmental milestones. What milestones should the nurse include in the teaching session? (Select all that apply.) a. Can lace shoes b. Uses scissors successfully c. Builds a tower of nine or 10 cubes d. Builds a bridge with three cubes e. Adeptly places small pellets in a narrow-necked bottle 10. The nurse is teaching parents of a 3-year-old child about language developmental milestones. What milestones should the nurse include in the teaching session? (Select all that apply.) a. Asks many questions b. Names one or more colors c. Repeats sentence of six syllables d. Uses primarily telegraphic speech e. Has a vocabulary of 1500 words or more 11. The nurse is teaching parents of a 4-year-old child about socialization developmental milestones. What milestones should the nurse include in the teaching session? (Select all that apply.) a. Very independent b. Has mood swings c. Has better manners d. Eager to do things right e. Tends to be selfish and impatient CHAPTER 15 1. What statement accurately describes physical development during the school-age years? a. The childs weight almost triples. b. Muscles become functionally mature. c. Boys and girls double strength and physical capabilities. d. Fat gradually increases, which contributes to childrens heavier appearance. 2. The parents of 9-year-old twin children tell the nurse, They have filled up their bedroom with collections of rocks, shells, stamps, and bird nests. The nurse should recognize that this is which? a. Indicative of giftedness b. Indicative of typical twin behavior c. Characteristic of cognitive development at this age d. Characteristic of psychosocial development at this age 3. What statement characterizes moral development in the older school-age child? a. Rule violations are viewed in an isolated context. b. Judgments and rules become more absolute and authoritarian. c. The child remembers the rules but cannot understand the reasons behind them. d. The child is able to judge an act by the intentions that prompted it rather than just by the consequences. 4. An 8-year-old girl tells the nurse that she has cancer because God is punishing her for being bad. What should the nurse interpret this as? a. A common belief at this age b. Indicative of excessive family pressure c. Faith that forms the basis for most religions d. Suggestive of a failure to develop a conscience 6. What is descriptive of the social development of school-age children? a. Identification with peers is minimum. b. Children frequently have best friends. c. Boys and girls play equally with each other. d. Peer approval is not yet an influence for the child to conform. 7. What statement best describes the relationship school-age children have with their families? a. Ready to reject parental controls b. Desire to spend equal time with family and peers c. Need and want restrictions placed on their behavior by the family d. Peer group replaces the family as the primary influence in setting standards of behavior and rules 10. What is descriptive of the play of school-age children? a. They like to invent games, making up the rules as they go. b. Individuality in play is better tolerated than at earlier ages. c. Knowing the rules of a game gives an important sense of belonging. d. Team play helps children learn the universal importance of competition and winning. 20. When teaching injury prevention during the school-age years, what should the nurse include? a. Teach children about the need to fear strangers. b. Teach basic rules of water safety. c. Avoid letting children cook in microwave ovens. d. Caution children against engaging in competitive sports. 25. A male school-age student asks the school nurse, How much with my height increase in a year? The nurse should give which response? a. Your height will increase on average 1 inch a year. b. Your height will increase on average 2 inches a year. c. Your height will increase on average 3 inches a year. d. Your height will increase on average 4 inches a year. 26. What does the nurse understand about caloric needs for school-age children? a. The caloric needs for the school-age children are the same as for other age groups. b. The caloric needs for school-age children are more than they were in the preschool years. c. The caloric needs for school-age children are lower than they were in the preschool years. d. The caloric needs for school-age children are greater than they will be in the adolescent years. 27. The school nurse is teaching female school-age children about the average age of puberty. What is the average age of puberty for girls? a. 10 years b. 11 years c. 12 years d. 13 years 28. The school nurse is teaching male school-age children about the average age of puberty. What is the average age of puberty for boys? a. 12 years b. 13 years c. 14 years d. 15 years 29. A female school-age child asks the school nurse, How many pounds should I expect to gain in a year? The nurse should give which response? a. You will gain about 2.4 to 4.6 lb per year b. You will gain about 3.4 to 5.6 lb per year. c. You will gain about 4.4 to 6.6 lb per year. d. You will gain about 5.5 to 7.6 lb per year. 30. The nurse is explaining about the developmental sequence in childrens capacity to conserve matter to a group of parents. What type of matter is last in the sequence for a child to develop? a. Mass b. Length c. Volume d. Numbers MULTIPLE RESPONSE 1. What growth and development milestones are expected between the ages of 8 and 9 years? (Select all that apply.) a. Can help with routine household tasks b. Likes the reward system for accomplished tasks c. Uses the telephone for practical purposes d. Chooses friends more selectively e. Goes about home and community freely, alone or with friends f. Enjoys family time and is respectful of parents 2. The nurse is planning strategies to assist a slow-to-warm child to try new experiences. What strategies should the nurse plan? (Select all that apply.) a. Attend after-school activities with a friend. b. Suggest the child move quickly into a new situation. c. Avoid trying new experiences until the child is ready. d. Allow the child to adapt to the experience at his or her own pace. e. Contract for permission to withdraw after a trial of the experience. CHAPTER 17 1. How does the onset of the pubertal growth spurt compare in girls and boys? a. In girls, it occurs about 1 year before it appears in boys. b. In girls, it occurs about 3 years before it appears in boys. c. In boys. it occurs about 1 year before it appears in girls. d. It is about the same in both boys and girls. 4. In boys, what is the initial indication of puberty? a. Voice changes b. Growth of pubic hair c. Testicular enlargement d. Increased size of penis 5. According to Piaget, adolescents tend to be in what stage of cognitive development? a. Concrete operations b. Conventional thought c. Postconventional thought d. Formal operational thought 6. What aspects of cognition develop during adolescence? a. Ability to see things from the point of view of another b. Capability of using a future time perspective c. Capability of placing things in a sensible and logical order d. Progress from making judgments based on what they see to making judgments based on what they reason 8. What is most descriptive of the spiritual development of older adolescents? a. Beliefs become more abstract. b. Rituals and practices become increasingly important. c. Strict observance of religious customs is common. d. Emphasis is placed on external manifestations, such as whether a person goes to church. 9. According to Erikson, the psychosocial task of adolescence is developing what? a. Identity b. Intimacy c. Initiative d. Independence 10. What is true concerning the development of autonomy during adolescence? a. Development of autonomy typically involves rebellion. b. Development of autonomy typically involves parentchild conflicts. c. Parent and peer influences are opposing forces in the development of autonomy. d. Conformity to both parents and peers gradually declines toward the end of adolescence. 19. The school nurse recognizes that pubertal delay in girls is considered if breast development has not occurred by which age? a. 10 years b. 11 years c. 12 years d. 13 years 20. The school nurse recognizes that pubertal delay in boys is considered if no enlargement of the testes or scrotal changes have occurred by what age? a. 11 1/2 to 12 years b. 12 1/2 to 13 years c. 13 1/2 to 14 years d. 14 1/2 to 15 years 23. The nurse is assessing the Tanner stage in an adolescent female. The nurse recognizes that the stages are based on which? a. The stages of vaginal changes b. The progression of menstrual cycles to regularity c. Breast size and the shape and distribution of pubic hair d. The development of fat deposits around the hips and buttocks 24. The nurse is assessing the Tanner stage in an adolescent male. The nurse recognizes that the stages are based on what? a. Hair growth on the face and chest b. Changes in the voice to a deeper timbre c. Muscle growth in the arms, legs, and shoulders d. Size and shape of the penis and scrotum and distribution of pubic hair MULTIPLE RESPONSE 1. The nurse is caring for children on an adolescent-only unit. What growth and development milestones should the nurse expect from 11- and 14-year-old adolescents? (Select all that apply.) a. Self-centered with increased narcissism b. No major conflicts with parents c. Established abstract thought process d. Have a rich, idealistic fantasy life e. Highly value conformity to group norms f. Secondary sexual characteristics appear 3. What are characteristics of middle adolescence (1517 years) with regard to relationships with peers? (Select all that apply.) a. Behavioral standards set by peer group b. Acceptance of peers extremely important c. Seeks peer affiliations to counter instability d. Exploration of ability to attract opposite sex e. Peer group recedes in importance in favor of individual friendship 4. What are characteristics of late adolescence (1820 years) with regard to sexuality? (Select all that apply.) a. Exploration of self-appeal b. Limited dating, usually group c. Intimacy involves commitment d. Growing capacity for mutuality and reciprocity e. May publicly identify as gay, lesbian, or bisexual CHAPTER 11 16. What is most descriptive of atopic dermatitis (AD) (eczema) in an infant? a. Easily cured b. Worse in humid climates c. Associated with hereditary allergies d. Related to upper respiratory tract infections 17. Where do eczematous lesions most commonly occur in an infant? a. Abdomen, cheeks, and scalp b. Buttocks, abdomen, and scalp c. Back and flexor surfaces of the arms and legs d. Cheeks and extensor surfaces of the arms and legs 18. The nurse is discussing the management of atopic dermatitis (eczema) with a parent. What should be included? a. Dress infant warmly to prevent chilling. b. Keep the infants fingernails and toenails cut short and clean. c. Give bubble baths instead of washing lesions with soap. d. Launder clothes in mild detergent; use fabric softener in the rinse. 32. The nurse is teaching parents about caring for their infant with seborrheic dermatitis (cradle cap). Which statement by the parents indicates understanding of the teaching? a. We will rinse off the shampoo quickly and dry the scalp thoroughly. b. We will shampoo the hair every other day with antiseborrheic shampoo. c. We will be sure to shampoo the hair without removing any of the crusts. d. We will use a fine-tooth comb to help remove the loosened crusts from the strands of hair. 33. The nurse is administering an oral antihistamine at bedtime to a child with atopic dermatitis (eczema). Which antihistamine should the nurse expect to be prescribed at bedtime? a. Cetirizine (Zyrtec) b. Loratadine (Claritin) c. Fexofenadine (Allegra) d. Diphenhydramine (Benadryl) 1. The nurse is planning care for an infant with eczema. Which interventions should the nurse include in the care plan? (Select all that apply.) a. Avoid giving the infant a bubble bath. b. Avoid the use of a humidifier in the infants room. c. Avoid overdressing the infant. d. Avoid the use of topical steroids on the infants skin. e. Avoid wet compresses on the infants most affected areas. 6. At a well-child check-up, the nurse notes that an infant with a previous diagnosis of failure to thrive (FTT) is now steadily gaining weight. The nurse should recommend that fruit juice intake be limited to no more than how much? a. 4 oz/day b. 6 oz/day c. 8 oz/day d. 12 oz/day 14. The nurse is examining an infant, age 10 months, who was brought to the clinic for persistent diaper rash. The nurse finds perianal inflammation with satellite lesions. What is the most likely cause? a. Impetigo b. Urine and feces c. Candida albicans infection d. Infrequent diapering 15. A new parent asks the nurse, How can diaper rash be prevented? What should the nurse recommend? a. Wash the infant with soap before applying a thin layer of oil. b. Clean the infant with soap and water every time diaper is changed. c. Wipe stool from the skin using water and a mild cleanser. d. When changing the diaper, wipe the buttocks with oil and powder the creases. 19. The parents of a 3-month-old infant report that their infant sleeps supine (face up) but is often prone (face down) while awake. The nurses response should be based on remembering what? a. This is acceptable to encourage head control and turning over. b. This is acceptable to encourage fine motor development. c. This is unacceptable because of the risk of sudden infant death syndrome (SIDS). d. This is unacceptable because it does not encourage achievement of developmental milestones. 20. After the introduction of the Back to Sleep campaign in 1992, an increased incidence has been noted of which pediatric issues? a. Sudden infant death syndrome (SIDS) b. Plagiocephaly c. Failure to thrive d. Apnea of infancy 21. The nurse is interviewing the parents of a 4-month-old boy brought to the hospital emergency department. The infant is dead, and no attempt at resuscitation is made. The parents state that the baby was found in his crib with a blanket over his head, lying face down in bloody fluid from his nose and mouth. The nurse might initially suspect his death was caused by what? a. Suffocation b. Child abuse c. Infantile apnea d. Sudden infant death syndrome (SIDS) 22. What is an important nursing responsibility when dealing with a family experiencing the loss of an infant from sudden infant death syndrome (SIDS)? a. Discourage the parents from making a last visit with the infant. b. Make a follow-up home visit to the parents as soon as possible after the childs death. c. Explain how SIDS could have been predicted and prevented. d. Interview the parents in depth concerning the circumstances surrounding the childs death. 23. What is an appropriate action when an infant becomes apneic? a. Shake vigorously. b. Roll the infants head to the side. c. Gently stimulate the trunk by patting or rubbing. d. Hold the infant by the feet upside down with the head supported. The correct dose of epinephrine to use in the emergency management of an anaphylactic reaction is 0.001 mg/kg up to a maximum of 0.3 mg, giving a range of 0.011 to 0.3 mg using a weight of 11 kg (24 lb). 8. What are risk factors for sudden infant death syndrome? (Select all that apply.) a. Postterm b. Female gender c. Low Apgar scores d. Recent viral illness e. Native American infants CHAPTER 14 6. What is a significant secondary prevention nursing activity for lead poisoning? a. Chelation therapy b. Screening children for blood lead levels c. Removing lead-based paint from older homes d. Questioning parents about ethnic remedies containing lead 7. What is an important nursing consideration when a child is hospitalized for chelation therapy to treat lead poisoning? a. Maintain bed rest. b. Maintain isolation precautions. c. Keep an accurate record of intake and output. d. Institute measures to prevent skeletal fracture. 8. What is the most common form of child maltreatment? a. Sexual abuse b. Child neglect c. Physical abuse d. Emotional abuse 9. A child is admitted with a suspected diagnosis of Munchausen syndrome by proxy (MSBP). What is an important consideration in the care of this child? a. Monitoring the parents whenever they are with the child b. Reassuring the parents that the cause of the disorder will be found c. Teaching the parents how to obtain necessary specimens d. Supporting the parents as they cope with diagnosis of a chronic illness 12. A 3-month-old infant dies shortly after arrival to the emergency department. The infant has subdural and retinal hemorrhages but no external signs of trauma. What should the nurse suspect? a. Unintentional injury b. Shaken baby syndrome c. Congenital neurologic problem d. Sudden infant death syndrome (SIDS) 17. A child with acetaminophen (Tylenol) poisoning has been admitted to the emergency department. What antidote does the nurse anticipate being prescribed? a. Carnitine (Carnitor) b. Fomepizole (Antizol) c. Deferoxamine (Desferal) d. N-acetylcysteine (Mucomyst) 21. A child has been admitted to the hospital with a blood lead level of 72 mcg/dL. What treatment should the nurse anticipate? a. Referral to social services b. Initiation of chelation therapy c. Follow-up testing within 1 month d. Aggressive environmental intervention 3. What can the nurse suggest to families to reduce blood lead levels? (Select all that apply.) a. Do not store food in open cans. b. Ensure the child eats regular meals. c. Mix formula with hot water from the tap. d. Vacuum hard-surfaced floors and window wells. e. Wash and dry the childs hands and face frequently. CHAPTER 16 4. The nurse should know what about Lyme disease? a. Very difficult to prevent b. Easily treated with oral antibiotics in stages 1, 2, and 3 c. Caused by a spirochete that enters the skin through a tick bite d. Common in geographic areas where the soil contains the mycotic spores that cause the disease 11. Parents are concerned that their 6-year-old son continues to occasionally wet the bed. What does the nurse explain? a. This is likely because of increased stress at home. b. Enuresis usually ceases between 6 and 8 years of age. c. Drug therapy will be prescribed to treat the enuresis. d. Testing will be necessary to determine what type of kidney problem exists. 12. The nurse is assisting the family of a child with a history of encopresis. What should be included in the nurses discussion with the family? a. Instruct the parents to sit the child on the toilet at twice-daily routine intervals. b. Instruct the parents that the child will probably need to have daily enemas. c. Suggest the use of stimulant cathartics weekly. d. Reassure the family that most problems are resolved successfully, with some relapses during periods of stress. 13. What is an important consideration in the diagnosis of attention deficit hyperactivity disorder (ADHD)? a. Learning disabilities are apparent at an early age. b. The child will always be distracted by external stimuli. c. Parental observations of the childs behavior are most relevant. d. It must be determined whether the childs behavior is age appropriate or problematic. 14. The nurse is facilitating a conference between the teachers and parents of a 7-year-old child newly diagnosed with attention deficit hyperactivity disorder (ADHD). What does the nurse stress? a. Academic subjects should be taught in the afternoon. b. Low-interest activities in the classroom should be minimized. c. Visual references should accompany verbal instruction. d. The childs environment should be visually stimulating. 16. A 9-year-old child has just been diagnosed with recurrent abdominal pain (RAP). In preparing for discharge, the nurse should include what in the home care instructions to the parents? a. Following a high-fiber diet b. Using stimulant laxatives c. Using ice packs on the abdomen when pain occurs d. Sitting on the toilet for 30 minutes after each meal Many cutaneous lesions are associated with local symptoms. Match the symptom with its definition. a. Pruritus b. Anesthesia c. Hyperesthesia d. Hypesthesia e. Paresthesia 1. Excessive sensitiveness 2. Itching 3. Diminished sensation 4. Abnormal sensation 5. Absence of sensation CHAPTER 18 1. Tretinoin (Retin-A) is a commonly used topical agent for the treatment of acne. What do nursing considerations with this drug include? a. Sun exposure increases effectiveness. b. Cosmetics with lanolin and petrolatum are preferred in acne. c. Applying of the medication occurs at least 20 to 30 minutes after washing. d. Erythema and peeling are indications of toxicity and need to be reported. 18. Descriptions of young people with anorexia nervosa (AN) often include which criteria? a. Impulsive b. Extroverted c. Perfectionist d. Low achieving 19. What behavior is the nurse most likely to assess in an adolescent with anorexia nervosa (AN)? a. Eats in secrecy b. Uses food as a coping mechanism c. Has a marked preoccupation with food d. Lacks awareness of how eating affects weight loss 20. During the physical examination of an adolescent with significant weight loss, what finding may indicate an eating disorder? a. Diarrhea b. Amenorrhea c. Appetite suppression d. Erosion of tooth enamel 21. What goal is most important when caring for a child with anorexia nervosa (AN)? a. Limit fluid intake. b. Prevent depression. c. Correct malnutrition. d. Encourage weight gain. 22. What do nursing responsibilities regarding weight gain for an adolescent with anorexia nervosa include? a. Administer tube feedings until target weight is achieved. b. Restore body weight to within 10% of the adolescents ideal weight. c. Encourage continuation of strenuous exercise as long as adolescent is not losing weight. d. Facilitate as rapid a weight gain as possible with a high-calorie diet. 34. The nurse is presenting an educational program to a group of parents about differences between anorexia nervosa (AN) and bulimia nervosa (BN) at a community outreach program. What statement by a parent would indicate a need for additional teaching? a. A child with AN will turn away from food to cope, but a child with BN turns to food to cope. b. A child with AN maintains rigid control and is introverted, but a child with BN is an extrovert and frequently loses control. c. A child with AN denies the illness, but a child with BN recognizes the illness. d. A child with AN is usually sexually active and seeks intimacy, but a child with BN avoids intimacy and is usually not sexually active. 35. The nurse is teaching an adolescent about acne care. What statement by the adolescent indicates a need for further teaching? a. I will cleanse my face twice a day. b. I will frequently shampoo my hair. c. I will brush my hair away from my forehead. d. I will use my antibacterial soap to cleanse my face. 36. After a treatment plan for acne has been initiated, which time period should the nurse explain to an adolescent before improvement will be seen? a. 2 to 4 weeks b. 4 to 6 weeks c. 6 to 8 weeks d. 8 to 10 weeks Inform patients that after a treatment plan for acne has been initiated, it will take 6 to 8 weeks to appreciate improvement in their skin. 2. The nurse is teaching an adolescent about the use of tretinoin (Retin-A). What should the nurse include in the teaching session? (Select all that apply.) a. Begin with a pea-sized dot of medication. b. Apply additional medication to the throat. c. Use sunscreen daily and avoid the sun when possible. d. Divide the medication into the three main areas of the face. e. Apply the medication immediately after washing the face. 3. The clinic nurse is assessing an adolescent on a topical antibacterial agent. The nurse should assess for which side effects that can be seen with topical antibacterial agents? (Select all that apply.) a. Burning b. Dryness c. Dry eyes d. Erythema e. Nasal irritation CHAPTER 21 9. A newborn assessment shows a separated sagittal suture, oblique palpebral fissures, a depressed nasal bridge, a protruding tongue, and transverse palmar creases. These findings are most suggestive of which condition? a. Microcephaly b. Cerebral palsy c. Down syndrome d. Fragile X syndrome 10. A 2-week-old infant with Down syndrome is being seen in the clinic. His mother tells the nurse that he is difficult to hold, that hes like a rag doll. He doesnt cuddle up to me like my other babies did. What is the nurses best interpretation of this lack of clinging or molding? a. Sign of detachment and rejection b. Indicative of maternal deprivation c. A physical characteristic of Down syndrome d. Suggestive of autism associated with Down syndrome 11. Many of the clinical features of Down syndrome present challenges to caregivers. Based on these features, what intervention should be included in the childs care? a. Delay feeding solid foods until the tongue thrust has stopped. b. Modify the diet as necessary to minimize the diarrhea that often occurs. c. Provide calories appropriate to the childs mental age. d. Use a cool-mist vaporizer to keep the mucous membranes moist and secretions liquefied. 12. What description applies to fragile X syndrome? a. Chromosomal defect affecting only females b. Second most common genetic cause of cognitive impairment c. Most common cause of uninherited cognitive impairment d. Chromosomal defect that follows the pattern of X-linked recessive disorders 20. Autism is a complex developmental disorder. The diagnostic criteria for autism include delayed or abnormal functioning in which area with onset before age 3 years? a. Parallel play b. Gross motor development c. Ability to maintain eye contact d. Growth below the fifth percentile 21. What intervention should be included in the nursing care of a child with autism spectrum disorder (ASD)? a. Assign multiple staff to care for the child. b. Communicate with the child at his or her developmental level. c. Provide a wide variety of foods for the child to try. d. Place the child in a semiprivate room with a roommate of a similar age. 28. The nurse is teaching feeding strategies to a parent of a 12-month-old infant with Down syndrome. What statement made by the parent indicates a need for further teaching? a. If the food is thrust out, I will reefed it. b. I will use a small, long, straight-handled spoon. c. I will place the food on the top of the tongue. d. I know the tongue thrust doesnt indicate a refusal of the food. 9. The nurse is counseling a pregnant 35-year-old woman about estimated risk of Down syndrome. What is the estimated risk for a woman who is 35 years of age? a. One in 1200 b. One in 900 c. One in 350 d. One in 100 5. The nurse is assessing a child with Down syndrome. The nurse recognizes that which are possible comorbidities that can occur with Down syndrome? (Select all that apply.) a. Diabetes mellitus b. Hodgkins disease c. Congenital heart defects d. Respiratory tract infections e. Acute megakaryoblastic leukemia 22. A hospitalized school-age child with phenylketonuria (PKU) is choosing foods from the hospitals menu. Which food choice should the nurse discourage the child from choosing? a. Banana b. Milkshake c. Fruit juice d. Corn on the cob 28. A child has been found to have a deficiency in 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase. Which condition is this child at risk for? a. Increased uric acid b. Hypercholesterolemia c. Increased phenylketones d. Altered oxygen transport a. Glucose b. Thyroxine c. Phenylalanine d. Phenylketones 0. Early diagnosis of congenital hypothyroidism (CH) and phenylketonuria (PKU) is essential to prevent which? a. Obesity b. Diabetes c. Cognitive impairment d. Respiratory distress CHAPTER 24 12. Ongoing fluid losses can overwhelm the childs ability to compensate, resulting in shock. What early clinical sign precedes shock? a. Tachycardia b. Slow respirations c. Warm, flushed skin d. Decreased blood pressure 34. What explains physiologically the edema formation that occurs with burns? a. Vasoconstriction b. Reduced capillary permeability c. Increased capillary permeability d. Diminished hydrostatic pressure within capillaries 35. What is a systemic response to severe burns in a child? a. Metabolic alkalosis b. Decreased metabolic rate c. Increased renal plasma flow d. Abrupt drop in cardiac output 36. A child is admitted with extensive burns. The nurse notes burns on the childs lips and singed nasal hairs. The nurse should suspect what condition in the child? a. A chemical burn b. A hot-water scald c. An electrical burn d. An inhalation injury 37. What is the most immediate threat to life in children with thermal injuries? a. Shock b. Anemia c. Local infection d. Systemic sepsis 38. After the acute stage and during the healing process, what is the primary complication from burn injury? a. Shock b. Asphyxia c. Infection d. Renal shutdown 39. What sign is one of the first to indicate overwhelming sepsis in a child with burn injuries? a. Seizures b. Bradycardia c. Disorientation d. Decreased blood pressure 40. A toddler sustains a minor burn on the hand from hot coffee. What is the first action in treating this burn? a. Apply burn ointment. b. Put ice on the burned area. c. Cover the hand with gauze dressing. d. Hold the hand under cool running water. 41. What finding is the most reliable guide to the adequacy of fluid replacement for a small child with burns? a. Absence of thirst b. Falling hematocrit c. Increased seepage from burn wound d. Urinary output of 1 to 2 ml/kg of body weight/hr 42. What is the purpose of a high-protein diet for a child with major burns? a. Promote growth b. Improve appetite c. Minimize protein breakdown d. Diminish risk of stress-induced hyperglycemia 3. Fentanyl and midazolam (Versed) are given before debridement of a childs burn wounds. What is the purpose of using these medications? a. Facilitate healing b. Provide pain relief c. Minimize risk of infection d. Decrease amount of debridement needed 44. Hydrotherapy is required to treat a child with extensive partial-thickness burn wounds. What is the purpose of hydrotherapy? a. Provide pain relief b. Dbride the wounds c. Destroy bacteria on the skin d. Increase peripheral blood flow 45. What is the nursing action related to the applying of biologic or synthetic skin coverings for a child with partial-thickness burns of both legs? a. Splint the legs to prevent movement. b. Observe wounds for signs of infection. c. Monitor closely for manifestations of shock. d. Examine dressings for indications of bleeding. 7. What consideration is important for the nurse when changing dressings and applying topical medication to a childs abdomen and leg burns? a. Apply topical medication with clean hands. b. Wash hands and forearms before and after dressing change. c. If dressings have adhered to the wound, soak in hot water before removal. d. Apply dressing so that movement is limited during the healing process. 48. What is a strategy used to minimize scarring with burn injury in a child? a. Applying of drying agents on skin b. Use of loose-fitting garments over healing areas c. Limitation of period without pressure to areas of scarring d. Immobilization of extremities while healing is occurring 49. Prevention of burn injury is important anticipatory guidance. In the infant and toddler period, which mode is the most common cause of burn? a. Matches b. Electrical cords c. Hot liquids in the kitchen d. Microwave-heated foods Infants and toddlers are most commonly injured by hot liquids in the kitchen and bathroom. This often occurs as a result of inadequate supervision of this curious and energetic age group. Matches and lighters are seen as toys by young children and should be kept out of reach. Older toddlers and preschool children are at risk of chewing on electrical cords and placing objects in outlets. Microwave-heated fluids and foods can become superheated, resulting in oral burns. Match the type of skin graft to its definition. a. Allografts b. Xenografts c. Autografts d. Isografts 1. Tissue obtained from undamaged areas of the patients own body 2. Histocompatible tissue obtained from genetically identical individuals 3. Skin that is obtained from genetically different members of the same species who are free of disease 4. Skin that is obtained from members of a different species, primarily pigskin CHAPTER 25 2. What urine test result is considered abnormal? a. pH 4.0 b. WBC 1 or 2 cells/ml c. Protein level absent d. Specific gravity 1.020 5. The nurse is teaching a client to prevent future urinary tract infections (UTIs). What factor is most important to emphasize as the potential cause? a. Poor hygiene b. Constipation c. Urinary stasis d. Congenital anomalies 6. A girl, age 5 1/2 years, has been sent to the school nurse for urinary incontinence three times in the past 2 days. The nurse should recommend to her parent that the first action is to have the child evaluated for what condition? a. School phobia b. Glomerulonephritis c. Urinary tract infection (UTI) d. Attention deficit hyperactivity disorder (ADHD) 7. What recommendation should the nurse make to prevent urinary tract infections (UTIs) in young girls? a. Avoid public toilet facilities. b. Limit long baths as much as possible. c. Cleanse the perineum with water after voiding. d. Ensure clear liquid intake of 2 L/day. 8. In teaching the parent of a newly diagnosed 2-year-old child with pyelonephritis related to vesicoureteral reflux (VUR), the nurse should include which information? a. Limit fluids to reduce reflux. b. Give cranberry juice twice a day. c. Have siblings examined for VUR. d. Surgery is indicated to reverse scarring. 9. What pathologic process is believed to be responsible for the development of postinfectious glomerulonephritis? a. Infarction of renal vessels b. Immune complex formation and glomerular deposition c. Bacterial endotoxin deposition on and destruction of glomeruli d. Embolization of glomeruli by bacteria and fibrin from endocardial vegetation 10. The nurse notes that a child has lost 3.6 kg (8 lb) after 4 days of hospitalization for acute glomerulonephritis. What is the most likely cause of this weight loss? a. Poor appetite b. Reduction of edema c. Restriction to bed rest d. Increased potassium intake 11. What measure of fluid balance status is most useful in a child with acute glomerulonephritis? a. Proteinuria b. Daily weight c. Specific gravity d. Intake and output 12. The parent of a child hospitalized with acute glomerulonephritis asks the nurse why blood pressure readings are being taken so often. What knowledge should influence the nurses reply? a. The antibiotic therapy contributes to labile blood pressure values. b. Hypotension leading to sudden shock can develop at any time. c. Acute hypertension is a concern that requires monitoring. d. Blood pressure fluctuations indicate that the condition has become chronic. 13. What laboratory finding, in conjunction with the presenting symptoms, indicates minimal change nephrotic syndrome? a. Low specific gravity b. Decreased hemoglobin c. Normal platelet count d. Reduced serum albumin 4. What is the primary objective of care for the child with minimal change nephrotic syndrome (MCNS)? a. Reduce blood pressure. b. Lower serum protein levels. c. Minimize excretion of urinary protein. d. Increase the ability of tissue to retain fluid. 15. A hospitalized child with minimal change nephrotic syndrome is receiving high doses of prednisone. What nursing goal is appropriate for this child? a. Stimulate appetite. b. Detect evidence of edema. c. Minimize risk of infection. d. Promote adherence to the antibiotic regimen. 16. The nurse is teaching a child experiencing severe edema associated with minimal change nephrotic syndrome about his diet. The nurse should discuss what dietary need? a. Consuming a regular diet b. Increasing protein c. Restricting fluids d. Decreasing calories 17. A child is admitted for minimal change nephrotic syndrome (MCNS). The nurse recognizes that the childs prognosis is related to what factor? a. Admission blood pressure b. Creatinine clearance c. Amount of protein in urine d. Response to steroid therapy 8. A 12-year-old child is injured in a bicycle accident. When considering the possibility of renal trauma, the nurse should consider what factor? a. Flank pain rarely occurs in children with renal injuries. b. Few nonpenetrating injuries cause renal trauma in children. c. Kidneys are immobile, well protected, and rarely injured in children. d. The amount of hematuria is not a reliable indicator of the seriousness of renal injury. Hematuria is consistently present with renal trauma. It does not provide a reliable indicator of the seriousness of the renal injury. Flank pain results from bleeding around the kidney. 19. What condition is the most common cause of acute renal failure in children? a. Pyelonephritis b. Tubular destruction c. Severe dehydration d. Upper tract obstruction 20. A child is admitted in acute renal failure (ARF). Therapeutic management to rapidly provoke a flow of urine includes the administration of what medication? a. Propranolol (Inderal) b. Calcium gluconate c. Mannitol (Osmitrol) or furosemide (Lasix) (or both) d. Sodium, chloride, and potassium 27. The nurse is conducting discharge teaching with the parent of a 7-year-old child with minimal change nephrotic syndrome (MCNS). What statement by the parent indicates a correct understanding of the teaching? a. My child needs to stay home from school for at least 1 more month. b. I should not add additional salt to any of my childs meals. c. My child will not be able to participate in contact sports while receiving corticosteroid therapy. d. I should measure my childs urine after each void and report the 24-hour amount to the health care provider. 36. What is an appropriate nursing intervention for a child with minimal change nephrotic syndrome (MCNS) who has scrotal edema? a. Place an ice pack on the scrotal area. b. Place the child in an upright sitting position. c. Elevate the scrotum with a rolled washcloth. d. Place a warm moist pack to the scrotal area. 37. What do the clinical manifestations of minimal change nephrotic syndrome include? a. Hematuria, bacteriuria, and weight gain b. Gross hematuria, albuminuria, and fever c. Hypertension, weight loss, and proteinuria d. Massive proteinuria, hypoalbuminemia, and edema 38. For minimal change nephrotic syndrome (MCNS), prednisone is effective when what occurs? a. Appetite increases and blood pressure is normal b. Urinary tract infection is gone and edema subsides c. Generalized edema subsides and blood pressure is normal d. Diuresis occurs as urinary protein excretion diminishes 39. A nurse is evaluating the effectiveness of teaching regarding care of a child with minimal change nephrotic syndrome (MCNS) that is in remission after administration of prednisone. The nurse realizes further teaching is required if the parents state what? a. We will keep our child away from anyone who is ill. b. We will be sure to administer the prednisone as ordered. c. We will encourage our child to eat a balanced diet, but we will watch his salt intake. d. We understand our child will not be able to attend school, so we will arrange for home schooling. 40. A parent asks the nurse what would be the first indication that acute glomerulonephritis was improving. What would be the nurses best response? a. Blood pressure will stabilize. b. Your child will have more energy. c. Urine will be free of protein. d. Urine output will increase. The first sign of improvement in acute glomerulonephritis is an increase in urinary output with a corresponding decrease in body weight. With diuresis, the child begins to feel better, the appetite improves, and the blood pressure decreases to normal with the reduction of edema. Gross hematuria diminishes, in part because of dilution of the red blood cells in the more dilute urine. Renal function and hypocomplementemia usually normalize by 8 weeks. 41. A child is admitted with acute glomerulonephritis. What should the nurse expect the urinalysis during this acute phase to show? a. Bacteriuria and hematuria b. Hematuria and proteinuria c. Bacteriuria and increased specific gravity d. Proteinuria and decreased specific gravity Urinalysis during the acute phase characteristically shows hematuria, proteinuria, and increased specific gravity. Proteinuria generally parallels the hematuria but is not usually the massive proteinuria seen in nephrotic syndrome. Gross discoloration of urine reflects its red blood cell and hemoglobin content. Microscopic examination of the sediment shows many red blood cells, leukocytes, epithelial cells, and granular and red blood cell casts. Bacteria are not seen, and urine culture results are negative. 42. A child with acute glomerulonephritis is in the playroom and experiences blurred vision and a headache. What action should the nurse take? a. Check the urine to see if hematuria has increased. b. Obtain the childs blood pressure and notify the health care provider. c. Obtain serum electrolytes and send urinalysis to the laboratory. d. Reassure the child and encourage bed rest until the headache improves. The premonitory signs of encephalopathy are headache, dizziness, abdominal discomfort, and vomiting. If the condition progresses, there may be transient loss of vision or hemiparesis, disorientation, and generalized tonic-clonic seizures. The health care provider should be notified of these symptoms. 43. The nurse is preparing to admit a child to the hospital with a diagnosis of acute poststreptococcal glomerulonephritis. The nurse understands that the peak age at onset for this disease is what? a. 2 to 4 years b. 5 to 7 years c. 8 to 10 years d. 11 to 13 years The peak age at onset for acute poststreptococcal glomerulonephritis is 5 to 7 years of age. 44. The nurse is preparing to admit a child to the hospital with a diagnosis of minimal change nephrotic syndrome. The nurse understands that the peak age at onset for this disease is what? a. 2 to 3 years b. 4 to 5 years c. 6 to 7 years d. 8 to 9 years 2. The nurse is caring for a child with a urinary tract infection who is on intravenous gentamicin (Garamycin). What interventions should the nurse plan for this child with regard to this medication? (Select all that apply.) a. Encourage fluids. b. Monitor urinary output. c. Monitor sodium serum levels. d. Monitor potassium serum levels. e. Monitor serum peak and trough levels. , B, E Garamycin can cause renal toxicity and ototoxicity. Fluids should be encouraged and urinary output and serum peak and trough levels monitored. It is not necessary to monitor potassium sodium levels for patients taking this medication. 3. The nurse is caring for a child with a urinary tract infection who is on trimethoprimsulfamethoxazole (Bactrim). What side effects of this medication should the nurse teach to the parents and the child? (Select all that apply.) a. Rash b. Urticaria c. Pneumonitis d. Renal toxicity e. Photosensitivity 4. The nurse is caring for a child with acute renal failure. What laboratory findings should the nurse expect to find? (Select all that apply.) a. Hyponatremia b. Hyperkalemia c. Metabolic alkalosis d. Elevated blood urea nitrogen level e. Decreased plasma creatinine level 8. What dietary instructions should the nurse give to parents of a child in the oliguria phase of acute glomerulonephritis with edema and hypertension? (Select all that apply.) a. High fat b. Low protein c. Encouragement of fluids d. Moderate sodium restriction e. Limit foods high in potassium 9. What dietary instructions should the nurse give to parents of a child with minimal change nephrotic syndrome with massive edema? (Select all that apply.) a. Soft diet b. High protein c. Fluid restricted d. No salt added at the table e. Restriction of foods high in sodium Match the classification of urinary tract infections of inflammations to its definition. a. Persistent urinary tract infection b. Cystitis c. Urethritis d. Pyelonephritis e. Urosepsis 1. Inflammation of the upper urinary tract and kidneys 2. Febrile urinary tract infection coexisting with systemic signs of bacterial illness 3. Persistence of bacteriuria despite antibiotic treatment 4. Inflammation of the urethra 5. Inflammation of the bladder CHAPTER 26 3. The mother of a child with cognitive impairment calls the nurse because her son has been gagging and drooling all morning. The nurse suspects foreign body ingestion. What physiologic occurrence is most likely responsible for the presenting signs? a. Gastrointestinal perforation may have occurred. b. The object may have been aspirated. c. The object may be lodged in the esophagus. d. The object may be embedded in stomach wall. Gagging and drooling may be signs of esophageal obstruction. The child is unable to swallow saliva, which contributes to the drooling. Signs of gastrointestinal (GI) perforation include chest or abdominal pain and evidence of bleeding in the GI tract. 6. What statement best describes Hirschsprung disease? a. The colon has an aganglionic segment. b. It results in frequent evacuation of solids, liquid, and gas. c. The neonate passes excessive amounts of meconium. d. It results in excessive peristaltic movements within the gastrointestinal tract. 8. A 3-year-old child with Hirschsprung disease is hospitalized for surgery. A temporary colostomy will be necessary. How should the nurse prepare this child? a. It is unnecessary because of childs age. b. It is essential because it will be an adjustment. c. Preparation is not needed because the colostomy is temporary. d. Preparation is important because the child needs to deal with negative body image. 9. A child has a nasogastric (NG) tube after surgery for Hirschsprung disease. What is the purpose of the NG tube? a. Prevent spread of infection. b. Monitor electrolyte balance. c. Prevent abdominal distention. d. Maintain accurate record of output. The NG tube is placed to suction out gastrointestinal secretions and prevent abdominal distention. The NG tube would not affect infection. Electrolyte content of the NG drainage can be monitored. Without the NG tube, there would be no drainage. After the NG tube is placed, it is important to maintain an accurate record of intake and output. This is not the reason for placement of the tube. 13. What clinical manifestation should be the most suggestive of acute appendicitis? a. Rebound tenderness b. Bright red or dark red rectal bleeding c. Abdominal pain that is relieved by eating d. Colicky, cramping, abdominal pain around the umbilicus Pain is the cardinal feature. It is initially generalized, usually periumbilical. The pain becomes constant and may shift to the right lower quadrant. Rebound tenderness is not a reliable sign and is extremely painful to the child. Bright or dark red rectal bleeding and abdominal pain that is relieved by eating are not signs of acute appendicitis. 14. When caring for a child with probable appendicitis, the nurse should be alert to recognize which sign or symptom as a manifestation of perforation? a. Anorexia b. Bradycardia c. Sudden relief from pain d. Decreased abdominal distention Signs of peritonitis, in addition to fever, include sudden relief from pain after perforation. Anorexia is already a clinical manifestation of appendicitis. Tachycardia, not bradycardia, is a manifestation of peritonitis. Abdominal distention usually increases in addition to an increase in pain (usually diffuse and accompanied by rigid guarding of the abdomen). 15. The nurse is caring for a child admitted with acute abdominal pain and possible appendicitis. What intervention is appropriate to relieve the abdominal discomfort during the evaluation? a. Place in the Trendelenburg position. b. Apply moist heat to the abdomen. c. Allow the child to assume a position of comfort. d. Administer a saline enema to cleanse the bowel. The child should be allowed to take a position of comfort, usually with the legs flexed. The Trendelenburg position will not help with the discomfort. If appendicitis is a possibility, administering laxative or enemas or applying heat to the area is dangerous. Such measures stimulate bowel motility and increase the risk of perforation. 20. A child with pyloric stenosis is having excessive vomiting. The nurse should assess for what potential complication? a. Hyperkalemia b. Hyperchloremia c. Metabolic acidosis d. Metabolic alkalosis Infants with excessive vomiting are prone to metabolic alkalosis from the loss of hydrogen ions. Potassium and chloride ions are lost with vomiting. Metabolic alkalosis, not acidosis, is likely. 21. What term describes invagination of one segment of bowel within another? a. Atresia b. Stenosis c. Herniation d. Intussusception Intussusception occurs when a proximal section of the bowel telescopes into a more distal segment, pulling the mesentery with it. The mesentery is compressed and angled, resulting in lymphatic and venous obstruction. Atresia is the absence or closure of a natural opening in the body. Stenosis is a narrowing or constriction of the diameter of a bodily passage or orifice. Herniation is the protrusion of an organ or part through connective tissue or through a wall of the cavity in which it is normally enclosed. 26. What signs or symptoms are most commonly associated with the prodromal phase of acute viral hepatitis? a. Bruising and lethargy b. Anorexia and malaise c. Fatigability and jaundice d. Dark urine and pale stools The signs and symptoms most common in the prodromal phase are anorexia, malaise, lethargy, and easy fatigability. Bruising would not be an issue unless liver damage has occurred. Jaundice is a late sign and often does not occur in children. Dark urine and pale stools would occur during the onset of jaundice (icteric phase) if it occurs. 28. The nurse is discussing home care with a mother whose 6-year-old child has hepatitis A. What information should the nurse include? a. Advise bed rest until 1 week after the icteric phase. b. Teach infection control measures to family members. c. Inform the mother that the child cannot return to school until 3 weeks after onset of jaundice. d. Reassure the mother that hepatitis A cannot be transmitted to other family members. Hand washing is the single most effective measure in preventing and controlling hepatitis. Hepatitis A can be transmitted through the fecaloral route. Family members must be taught preventive measures. Rest and quiet activities are essential and adjusted to the childs condition, but bed rest is not necessary. The child is not infectious 1 week after the onset of jaundice and may return to school as activity level allows. 35. The parents of a newborn with an umbilical hernia ask about treatment options. The nurses response should be based on which knowledge? a. Surgery is recommended as soon as possible. b. The defect usually resolves spontaneously by 3 to 5 years of age. c. Aggressive treatment is necessary to reduce its high mortality. d. Taping the abdomen to flatten the protrusion is sometimes helpful. The umbilical hernia usually resolves by ages 3 to 5 years of age without intervention. Umbilical hernias rarely become problematic. Incarceration, where the hernia is constricted and cannot be reduced manually, is rare. Umbilical hernias are not associated with a high mortality rate. Taping the abdomen flat does not help heal the hernia; it can cause skin irritation. 36. The nurse is preparing to care for a newborn with an omphalocele. The nurse should understand that care of the infant should include what intervention? a. Initiating breast- or bottle-feedings to stabilize the blood glucose level b. Maintaining pain management with an intravenous opioid c. Covering the intact bowel with a nonadherent dressing to prevent injury d. Performing immediate surgery Nursing care of an infant with an omphalocele includes covering the intact bowel with a nonadherent dressing to prevent injury or placing a bowel bag or moist dressings and a plastic drape if the abdominal contents are exposed. The infant is not started on any type of feeding but has a nasogastric tube placed for gastric decompression. Pain management is started after surgery, but surgery is not done immediately after birth. The infant is medically stabilized before different surgical options are considered. 38. A 3-day-old infant presents with abdominal distention, is vomiting, and has not passed any meconium stools. What disease should the nurse suspect? a. Pyloric stenosis b. Intussusception c. Hirschsprung disease d. Celiac disease The clinical manifestations of Hirschsprung disease in a 3-day-old infant include abdominal distention, vomiting, and failure to pass meconium stools. Pyloric stenosis would present with vomiting but not distention or failure to pass meconium stools. Intussusception presents with abdominal cramping and celiac disease presents with malabsorption. 9. A 6-month-old infant with Hirschsprung disease is scheduled for a temporary colostomy. What should postoperative teaching to the parents include? a. Dilating the stoma b. Assessing bowel function c. Limitation of physical activities d. Measures to prevent prolapse of the rectum In the postoperative period, the nurse involves the parents in the care of the child with a temporary colostomy, allowing them to help with feedings and observe for signs of wound infection or irregular passage of stool (constipation or true incontinence). Some children will require daily anal dilatations in the postoperative period to avoid anastomotic strictures but not stoma dilatations. Physical activities should be encouraged. There is not a risk of prolapse of the rectum in Hirschsprung disease, just strictures. 40. An infant is born with a gastroschisis. Care preoperatively should include which priority intervention? a. Prone position b. Sterile water feedings c. Monitoring serum laboratory electrolytes d. Covering the defect with a sterile bowel bag Initial management of a gastroschisis involves covering the exposed bowel with a transparent plastic bowel bag or loose, moist dressings. The infant cannot be placed prone, and feedings will be withheld until surgery is performed. Electrolyte laboratory values will be monitored but not before covering the defect with a sterile bowel bag. 48. What intervention is contraindicated in a suspected case of appendicitis? a. Enemas b. Palpating the abdomen c. Administration of antibiotics d. Administration of antipyretics for fever In any instance in which severe abdominal pain is observed and appendicitis is suspected, the nurse must be aware of the danger of administering laxatives or enemas. Such measures stimulate bowel motility and increase the risk of perforation. The abdomen is palpated after other assessments are made. Antibiotics should be administered, and antipyretics are not contraindicated. 50. The nurse is evaluating the laboratory results of a stool sample. What is a normal finding? a. The laboratory reports a stool pH of 5.0. b. The laboratory reports a negative guaiac. c. The laboratory reports low levels of enzymes. d. The laboratory reports reducing substances present. The normal stool finding is a negative guaiac. Stool pH should be 7.0 to 7.5. A stool pH <5.0 is suggestive of carbohydrate malabsorption; colonic bacterial fermentation produces short-chain fatty acids, which lower stool pH. There should be no enzymes or reducing substances present in a normal stool sample. 2. The nurse is preparing to admit a 3-year-old child with intussusception. What clinical manifestations should the nurse expect to observe? (Select all that apply.) a. Absent bowel sounds b. Passage of red, currant jellylike stools c. Anorexia d. Tender, distended abdomen e. Hematemesis f. Sudden acute abdominal pain 10. The nurse is preparing to admit a 2-month-old child with hypertrophic pyloric stenosis. What clinical manifestations should the nurse expect to observe? (Select all that apply.) a. Weight loss b. Bilious vomiting c. Abdominal pain d. Projectile vomiting e. The infant is hungry after vomiting 12. The nurse is preparing to admit a 5-year-old child with hepatitis A. What clinical features of hepatitis A should the nurse recognize? (Select all that apply.) a. The onset is rapid. b. Fever occurs early. c. There is usually a pruritic rash. d. Nausea and vomiting are common. e. The mode of transmission is primarily by the parenteral route. 13. The nurse is preparing to admit a 7-year-old child with hepatitis B. What clinical features of hepatitis B should the nurse recognize? (Select all that apply.) a. The onset is rapid. b. Rash is common. c. Jaundice is present d. No carrier state exists. e. The mode of transmission is principally by the parenteral route. Diagnosis of hepatitis B is confirmed by the detection of various hepatitis virus antigens, and the antibodies that are produced in response to the infection. Match the antibody or antigen to its definition. a. HBsAg b. Anti-HBs c. HBcAg d. HBeAg 1. Indicates active infection 2. Detected only in the liver 3. Indicates resolving or past infection 4. Indicates ongoing infection or carrier state CHAPTER 27 1. What respiratory condition or disease results in both increased compliance and increased resistance? a. Asthma b. Atelectasis c. Surfactant deficiency d. Bronchopulmonary dysplasia Compliance is a measure of the relative ease with which the chest wall expands. Resistance is determined primarily by airway size. Asthma results in increased compliance and increased resistance, both of which increase the work of breathing. Atelectasis and surfactant deficiency both decrease compliance but do not affect resistance. Bronchopulmonary dysplasia increases resistance but does not affect compliance. 6. Respiratory failure can result from many causes. What condition is a specific primary cause of inefficient gas transfer? a. Anemia b. Pneumothorax c. Cystic fibrosis d. Laryngospasm 24. A 5-month-old infant is in respiratory distress. What should the nurse expect to find? a. Nasal flaring b. Bradycardia c. Abdominal breathing d. Capillary refill of 2 seconds 9. A nurse is calculating the correlation of Pao2 with Sao2 according to the oxyhemoglobin dissociation curve. What parameter should indicate that the Pao2 is less than 50 to 60 mm Hg? a. Coarse lung sounds b. Temperature of 100 F c. Respiratory rate of 58 d. Pulse oximetry reading of 90% or less The Pao2 can be correlated with the Sao2 by means of the oxyhemoglobin dissociation curve, although changes in Pao2 do not cause identical (linear) changes in Sao2. The curve represents the relationship between Pao2(measured in the blood) and Sao2 (measured by the pulse oximeter). When the Pao2 is 60?9?mm?9?Hg, the Sao2 is 90%. The oxyhemoglobin dissociation curve does not correlate with lung sounds, temperature, or respiratory rate. 31. The nurse is caring for a child in respiratory distress. What is an early but less obvious sign of respiratory failure? a. Stupor b. Headache c. Bradycardia d. Somnolence An early but less obvious sign of respiratory failure is a headache. Stupor, bradycardia, and somnolence are signs of more severe hypoxia. CHAPTER 28 4. It is important that a child with acute streptococcal pharyngitis be treated with antibiotics to prevent which condition? a. Otitis media b. Diabetes insipidus (DI) c. Nephrotic syndrome d. Acute rheumatic fever 5. When caring for a child after a tonsillectomy, what intervention should the nurse do? a. Watch for continuous swallowing. b. Encourage gargling to reduce discomfort. c. Apply warm compresses to the throat. d. Position the child on the back for sleeping. 7. Parents bring their 15-month-old infant to the emergency department at 3:00 AM because the toddler has a temperature of 39 C (102.2 F), is crying inconsolably, and is tugging at the ears. A diagnosis of otitis media (OM) is made. In addition to antibiotic therapy, the nurse practitioner should instruct the parents to use what medication? a. Decongestants to ease stuffy nose b. Antihistamines to help the child sleep c. Aspirin for pain and fever management d. Benzocaine ear drops for topical pain relief 8. An 18-month-old child is seen in the clinic with otitis media (OM). Oral amoxicillin is prescribed. What instructions should be given to the parent? a. Administer all of the prescribed medication. b. Continue medication until all symptoms subside. c. Immediately stop giving medication if hearing loss develops. d. Stop giving medication and come to the clinic if fever is still present in 24 hours. 9. An infants parents ask the nurse about preventing otitis media (OM). What information should be provided? a. Avoid tobacco smoke. b. Use nasal decongestants. c. Avoid children with OM. d. Bottle- or breastfeed in a supine position. 10. Chronic otitis media with effusion (OME) differs from acute otitis media (AOM) because it is usually characterized by which signs or symptoms? a. Severe pain in the ear b. Anorexia and vomiting c. A feeling of fullness in the ear d. Fever as high as 40 C (104 F) OME is characterized by a feeling of fullness in the ear or other nonspecific complaints. OME does not cause severe pain. This may be a sign of AOM. Vomiting, anorexia, and fever are associated with AOM. 11. A 4-year-old girl is brought to the emergency department. She has a froglike croaking sound on inspiration, is agitated, and is drooling. She insists on sitting upright. The nurse should intervene in which manner? a. Make her lie down and rest quietly. b. Examine her oral pharynx and report to the physician. c. Auscultate her lungs and prepare for placement in a mist tent. d. Notify the physician immediately and be prepared to assist with a tracheostomy or intubation. This child is exhibiting signs of respiratory distress and possible epiglottitis. Epiglottitis is always a medical emergency requiring antibiotics and airway support for treatment. Sitting up is the position that facilitates breathing in respiratory disease. 12. The nurse is assessing a child with croup in the emergency department. The child has a sore throat and is drooling. Examining the childs throat using a tongue depressor might precipitate what condition? a. Sore throat b. Inspiratory stridor c. Complete obstruction d. Respiratory tract infection If a child has acute epiglottitis, examination of the throat may cause complete obstruction and should be performed only when immediate intubation can take place. Sore throat and pain on swallowing are early signs of epiglottitis. Stridor is aggravated when a child with epiglottitis is supine. Epiglottitis is caused by Haemophilus influenzae in the respiratory tract. 22. What statement is the most descriptive of asthma? a. It is inherited. b. There is heightened airway reactivity. c. There is decreased resistance in the airway. d. The single cause of asthma is an allergic hypersensitivity. In asthma, spasm of the smooth muscle of the bronchi and bronchioles causes constriction, producing impaired respiratory function. Atopy, or development of an immunoglobulin E (IgE)mediated response, is inherited but is not the only cause of asthma. Asthma is characterized by increased resistance in the airway. Asthma has multiple causes, including allergens, irritants, exercise, cold air, infections, medications, medical conditions, and endocrine factors. 23. What condition is the leading cause of chronic illness in children? a. Asthma b. Pertussis c. Tuberculosis d. Cystic fibrosis 24. A child has a chronic cough and diffuse wheezing during the expiratory phase of respiration. This suggests what condition? a. Asthma b. Pneumonia c. Bronchiolitis d. Foreign body in trachea Asthma may have these chronic signs and symptoms. Pneumonia appears with an acute onset, fever, and general malaise. Bronchiolitis is an acute condition caused by respiratory syncytial virus. Foreign body in the trachea occurs with acute respiratory distress or failure and maybe stridor. 25. A child with asthma is having pulmonary function tests. What rationale explains the purpose of the peak expiratory flow rate? a. To assess severity of asthma b. To determine cause of asthma c. To identify triggers of asthma d. To confirm diagnosis of asthma Peak expiratory flow rate monitoring is used to monitor the childs current pulmonary function. It can be used to manage exacerbations and for daily long-term management. The cause of asthma is known. Asthma is caused by a complex interaction among inflammatory cells, mediators, and the cells and tissues present in the airways. The triggers of asthma are determined through history taking and immunologic and other testing. The diagnosis of asthma is made through clinical manifestations, history, physical examination, and laboratory testing. 26. Children who are taking long-term inhaled steroids should be assessed frequently for what potential complication? a. Cough b. Osteoporosis c. Slowed growth d. Cushing syndrome The growth of children on long-term inhaled steroids should be assessed frequently to evaluate systemic effects of these drugs. Cough is prevented by inhaled steroids. No evidence exists that inhaled steroids cause osteoporosis. Cushing syndrome is caused by long-term systemic steroids. 27. One of the goals for children with asthma is to maintain the childs normal functioning. What principle of treatment helps to accomplish this goal? a. Limit participation in sports. b. Reduce underlying inflammation. c. Minimize use of pharmacologic agents. d. Have yearly evaluations by a health care provider. Children with asthma are often excluded from exercise. This practice interferes with peer interaction and physical health. Most children with asthma can participate provided their asthma is under control. Inflammation is the underlying cause of the symptoms of asthma. By decreasing inflammation and reducing the symptomatic airway narrowing, health care providers can minimize exacerbations. Pharmacologic agents are used to prevent and control asthma symptoms, reduce the frequency and severity of asthma exacerbations, and reverse airflow obstruction. It is recommended that children with asthma be evaluated every 6 months. 28. What drug is usually given first in the emergency treatment of an acute, severe asthma episode in a young child? a. Ephedrine b. Theophylline c. Aminophylline d. Short-acting b2-agonists Short-acting b2-agonists are the first treatment in an acute asthma exacerbation. Ephedrine and aminophylline are not helpful in acute asthma exacerbations. Theophylline is unnecessary for treating asthma exacerbations. 29. Cystic fibrosis (CF) may affect single or multiple systems of the body. What is the primary factor responsible for possible multiple clinical manifestations in CF? a. Hyperactivity of sweat glands b. Hypoactivity of autonomic nervous system c. Atrophic changes in mucosal wall of intestines d. Mechanical obstruction caused by increased viscosity of mucous gland secretions The mucous glands produce a thick mucoprotein that accumulates and results in dilation. Small passages in organs such as the pancreas and bronchioles become obstructed as secretions form concretions in the glands and ducts. The exocrine glands, not sweat glands, are dysfunctional. Although abnormalities in the autonomic nervous system are present, it is not hypoactive. Intestinal involvement in CF results from the thick intestinal secretions, which can lead to blockage and rectal prolapse. 0. What is the earliest recognizable clinical manifestation(s) of cystic fibrosis (CF)? a. Meconium ileus b. History of poor intestinal absorption c. Foul-smelling, frothy, greasy stools d. Recurrent pneumonia and lung infections 1. What tests aid in the diagnosis of cystic fibrosis (CF)? a. Sweat test, stool for fat, chest radiography b. Sweat test, bronchoscopy, duodenal fluid analysis c. Sweat test, stool for trypsin, biopsy of intestinal mucosa d. Stool for fat, gastric contents for hydrochloride, radiography 32. A child with cystic fibrosis (CF) receives aerosolized bronchodilator medication. When should this medication be administered? a. After chest physiotherapy (CPT) b. Before chest physiotherapy (CPT) c. After receiving 100% oxygen d. Before receiving 100% oxygen 33. A child with cystic fibrosis is receiving recombinant human deoxyribonuclease (DNase). What statement about DNase is true? a. Given subcutaneously b. May cause voice alterations c. May cause mucus to thicken d. Not indicated for children younger than age 12 years 34. The parent of a child with cystic fibrosis (CF) calls the clinic nurse to report that the child has developed tachypnea, tachycardia, dyspnea, pallor, and cyanosis. The nurse should tell the parent to bring the child to the clinic because these signs and symptoms are suggestive of what condition? a. Pneumothorax b. Bronchodilation c. Carbon dioxide retention d. Increased viscosity of sputum . 35. Pancreatic enzymes are administered to the child with cystic fibrosis. What nursing consideration should be included in the plan of care? a. Give pancreatic enzymes between meals if at all possible. b. Do not administer pancreatic enzymes if the child is receiving antibiotics. c. Decrease the dose of pancreatic enzymes if the child is having frequent, bulky stools. d. Pancreatic enzymes can be swallowed whole or sprinkled on a small amount of food taken at the beginning of a meal. 36. The nurse is giving discharge instructions to the parents of a 5-year-old child who had a tonsillectomy 4 hours ago. What statement by the parent indicates a correct understanding of the teaching? a. I can use an ice collar on my child for pain control along with analgesics. b. My child should clear the throat frequently to clear the secretions. c. I should allow my child to be as active as tolerated. d. My child should gargle and brush teeth at least three times per day. 38. A 6-year-old child has had a tonsillectomy. The child is spitting up small amounts of dark brown blood in the immediate postoperative period. The nurse should take what action? a. Notify the health care provider. b. Continue to assess for bleeding. c. Give the child a red flavored ice pop. d. Position the child in a Trendelenburg position. flavored ice pop should not be given and the Trendelenburg position is not recommended. 39. A 3-year-old child is experiencing pain after a tonsillectomy. The child has not taken in any fluids and does not want to drink anything, saying, My tummy hurts. The following health care prescriptions are available: acetaminophen (Tylenol) PO (orally) or PR (rectally) PRN, ice chips, clear liquids. What should the nurse implement to relieve the childs pain? a. Ice chips b. Tylenol PO c. Tylenol PR d. Popsicle The throat is very sore after a tonsillectomy. Most children experience moderate pain after a tonsillectomy and need pain medication at regular intervals for at least the first 24 hours. Analgesics may need to be given rectally or intravenously to avoid the oral route. 40. A 1-year-old child has acute otitis media (AOM) and is being treated with oral antibiotics. What should the nurse include in the discharge teaching to the infants parents? a. A follow-up visit should be done after all medicine has been given. b. After an episode of acute otitis media, hearing loss usually occurs. c. Tylenol should not be given because it may mask symptoms. d. The infant will probably need a myringotomy procedure and tubes. Children should be given for pain, and the infant will not necessarily need a myringotomy procedure. 45. A 3-year-old is brought to the emergency department with symptoms of stridor, fever, restlessness, and drooling. No coughing is observed. Based on these findings, the nurse should be prepared to assist with what action? a. Throat culture b. Nasal pharynx washing c. Administration of corticosteroids d. Emergency intubation 46. A 3-year-old child woke up in the middle of the night with a croupy cough and inspiratory stridor. The parents bring the child to the emergency department, but by the time they arrive, the cough is gone, and the stridor has resolved. What can the nurse teach the parents with regard to this type of croup? a. A bath in tepid water can help resolve this type of croup. b. Tylenol can help to relieve the cough and stridor. c. A cool mist vaporizer at the bedside can help prevent this type of croup. d. Antibiotics need to be given to reduce the inflammation. 48. A child is in the hospital for cystic fibrosis. What health care providers prescription should the nurse clarify before implementing? a. Dornase alfa (Pulmozyme) nebulizer treatment bid b. Pancreatic enzymes every 6 hours c. Vitamin A, D, E, and K supplements daily d. Proventil (albuterol) nebulizer treatments tid 49. A 6-year-old child is in the hospital for status asthmaticus. Nursing care during this acute period includes which prescribed interventions? a. Prednisolone (Pediapred) PO every day, IV fluids, cromolyn (Intal) inhaler bid b. Salmeterol (Serevent) PO bid, vital signs every 4 hours, spot check pulse oximetry c. Triamcinolone (Azmacort) inhaler bid, continuous pulse oximetry, vital signs once a shift d. Methylprednisolone (Solumedrol) IV every 12 hours, continuous pulse oximetry, albuterol nebulizer treatments every 4 hours and prn 0. In providing nourishment for a child with cystic fibrosis (CF), what factors should the nurse keep in mind? a. Fats and proteins must be greatly curtailed. b. Most fruits and vegetables are not well tolerated. c. Diet should be high in calories, proteins, and unrestricted fats. d. Diet should be low fat but high in calories and proteins. 51. A quantitative sweat chloride test has been done on an 8-month-old child. What value should be indicative of cystic fibrosis (CF)? a. Less than 18 mEq/L b. 18 to 40 mEq/L c. 40 to 60 mEq/L d. Greater than 60 mEq/L 52. A preschool child has asthma, and a goal is to extend expiratory time and increase expiratory effectiveness. What action should the nurse implement to meet this goal? a. Encourage increased fluid intake. b. Recommend increased use of a budesonide (Pulmicort) inhaler. c. Administer an antitussive to suppress coughing. d. Encourage the child to blow a pinwheel every 6 hours while awake. 53. A school-age child has asthma. The nurse should teach the child that if a peak expiratory flow rate is in the yellow zone, this means that the asthma control is what? a. 80% of a personal best, and the routine treatment plan can be followed. b. 50% to 79% of a personal best and needs an increase in the usual therapy. c. 50 % of a personal best and needs immediate emergency bronchodilators. d. Less than 50% of a personal best and needs immediate hospitalization. 5. A school-age child with cystic fibrosis takes four enzyme capsules with meals. The child is having four or five bowel movements per day. The nurses action in regard to the pancreatic enzymes is based on the knowledge that the dosage is what? a. Adequate b. Adequate but should be taken between meals c. Needs to be increased to increase the number of bowel movements per day d. Needs to be increased to decrease the number of bowel movements per day The amount of enzyme is adjusted to achieve normal growth and a decrease in the number of stools to one or two per day. 56. A term infant is delivered, and before delivery, the medical team was notified that a congenital diaphragmatic hernia (CDH) was diagnosed on ultrasonography. What should be done immediately at birth if respiratory distress is noted? a. Give oxygen. b. Suction the infant. c. Intubate the infant. d. Ventilate the infant with a bag and mask. 57. A child has a streptococcal throat infection and is being treated with antibiotics. What should the nurse teach the parents to prevent infection of others? a. The child can return to school immediately. b. The organism cannot be transmitted through contact. c. The child can return to school after taking antibiotics for 24 hours. d. The organism can only be transmitted if someone uses a personal item of the sick child. 58. What medication is contraindicated in children post tonsillectomy and adenoidectomy? a. Codeine b. Ondansetron (Zofran) b. Amoxil (amoxicillin) c. Acetaminophen (Tylenol) Codeine is contraindicated in pediatric patients after tonsillectomy and adenoidectomy. 1. The nurse is preparing a staff education program about pediatric asthma. What concepts should the nurse include when discussing the asthma severity classification system? (Select all that apply.) a. Children with mild persistent asthma have nighttime signs or symptoms less than two times a month. b. Children with moderate persistent asthma use a short-acting b-agonist more than two times per week. c. Children with severe persistent asthma have a peak expiratory flow (PEF) of 60% to 80% of predicted value. d. Children with mild persistent asthma have signs or symptoms more than two times per week. e. Children with moderate persistent asthma have some limitations with normal activity. f. Children with severe persistent asthma have frequent nighttime signs or symptoms. 2. The nurse is caring for a newborn with suspected congenital diaphragmatic hernia. What of the following findings would the nurse expect to observe? (Select all that apply.) a. Loud, harsh murmur b. Scaphoid abdomen c. Poor peripheral pulses d. Mediastinal shift e. Inguinal swelling f. Moderate respiratory distress 4. A tonsillectomy or adenoidectomy is contraindicated in what conditions? (Select all that apply.) a. Cleft palate b. Seizure disorders c. Blood dyscrasias d. Sickle cell disease e. Acute infection at the time of surgery 6. The nurse is preparing to admit a 7-year-old child with acute laryngotracheobronchitis (LTB). What clinical manifestations should the nurse expect to observe? (Select all that apply.) a. Dysphagia b. Brassy cough c. Low-grade fever d. Toxic appearance e. Slowly progressive , C, E Clinical manifestations of LTB include a brassy cough, low-grade fever, and slow progression. Dysphagia and a toxic appearance are characteristics of acute epiglottitis. 7. The nurse is preparing to admit a 3-year-old child with acute spasmodic laryngitis. What clinical features of hepatitis B should the nurse recognize? (Select all that apply.) a. High fever b. Croupy cough c. Tendency to recur d. Purulent secretions e. Occurs sudden, often at night 14. The nurse encourages the mother of a toddler with acute laryngotracheobronchitis to stay at the bedside as much as possible. What is the primary rationale for this action? a. Mothers of hospitalized toddlers often experience guilt. b. The mothers presence will reduce anxiety and ease the childs respiratory efforts. c. Separation from the mother is a major developmental threat at this age. d. The mother can provide constant observations of the childs respiratory efforts. 37. A child is admitted with acute laryngotracheobronchitis (LTB). The child will most likely be treated with which? a. Racemic epinephrine and corticosteroids b. Nebulizer treatments and oxygen c. Antibiotics and albuterol d. Chest physiotherapy and humidity Ch 29 Atrial septal defect The atrial septal defect results in increased pulmonary blood flow. Patent ductus arteriosus, atrial septal defect, and ventricular septal defect are acyanotic congenital heart defects. Patent ductus arteriosus 19. The physician suggests that surgery be performed for patent ductus arteriosus (PDA) to prevent which complication? a. Hypoxemia b. Right-to-left shunt of blood c. Decreased workload on the left side of the heart d. Pulmonary vascular congestion Coarctation of the aorta Bounding upper extremity pulses are a manifestation of coarctation of the aorta. Tetralogy of Fallot – VSD, PS, overriding aorta, right ventricular hypertrophy 21. What structural defects constitute tetralogy of Fallot? a. Pulmonary stenosis, ventricular septal defect, overriding aorta, right ventricular hypertrophy b. Aortic stenosis, ventricular septal defect, overriding aorta, right ventricular hypertrophy c. Aortic stenosis, ventricular septal defect, overriding aorta, left ventricular hypertrophy d. Pulmonary stenosis, ventricular septal defect, aortic hypertrophy, left ventricular hypertrophy Tetralogy of Fallot has these four characteristics: pulmonary stenosis, ventricular septal defect, overriding aorta, and right ventricular hypertrophy. 39. An infant has tetralogy of Fallot. In reviewing the record, what laboratory result should the nurse expect to be documented? a. Leukopenia b. Polycythemia c. Anemia d. Increased platelet level Persistent hypoxemia that occurs with tetralogy of Fallot stimulates erythropoiesis, which results in polycythemia, an increased number of red blood cells. 0. What child has a cyanotic congenital heart defect? a. An infant with patent ductus arteriosus b. A 1-year-old infant with atrial septal defect c. A 2-month-old infant with tetralogy of Fallot d. A 6-month-old infant with repaired ventricular septal defect Tetralogy of Fallot is a cyanotic congenital heart defect. Patent ductus arteriosus, atrial septal defect, and ventricular septal defect are acyanotic congenital heart defects. 44. A 1-year-old has been admitted for complete repair of a tetralogy of Fallot. What assessment finding should the nurse expect to be documented? a. Weight gain b. Pale skin color c. Increasing cyanosis d. Decrease in hemoglobin and hematocrit Elective repair of tetralogy of Fallot is usually performed in the first year of life. Indications for repair include increasing cyanosis and the development of hypercyanotic spells. The child would not have a weight gain, pale skin color, or decrease in hemoglobin and hematocrit. 18. What blood flow pattern occurs in a ventricular septal defect? a. Mixed blood flow b. Increased pulmonary blood flow c. Decreased pulmonary blood flow d. Obstruction to blood flow from ventricles The opening in the septal wall allows for blood to flow from the higher pressure left ventricle into the lower pressure right ventricle. This left-to-right shunt creates increased pulmonary blood flow. The shunt is one way, from high pressure to lower pressure; oxygenated and unoxygenated blood do not mix. The outflow of blood from the ventricles is not affected by the septal defect. 27. A parent of a 7-year-old girl with a repaired ventricular septal defect (VSD) calls the cardiology clinic and reports that the child is just not herself. Her appetite is decreased, she has had intermittent fevers around 38 C (100.4 F), and now her muscles and joints ache. Based on this information, how should the nurse advise the mother? a. Immediately bring the child to the clinic for evaluation. b. Come to the clinic next week on a scheduled appointment. c. Treat the signs and symptoms with acetaminophen and fluids because it is most likely a viral illness. d. Recognize that the child is trying to manipulate the parent by complaining of vague symptoms. These are the insidious symptoms of bacterial endocarditis. Because the child is in a high-risk group for this disorder (VSD repair), immediate evaluation and treatment are indicated to prevent cardiac damage. With appropriate antibiotic therapy, bacterial endocarditis is successfully treated in approximately 80% of the cases. The childs complaints should not be dismissed. The low-grade fever is not a symptom that the child can fabricate. 43. The health care provider suggests surgery be performed for ventricular septal defect to prevent what complication? a. Pulmonary hypertension b. Right-to-left shunt of blood c. Pulmonary embolism d. Left ventricular hypertrophy Congenital heart defects with a large left-to-right shunt (e.g., in ventricular septal defect, patent ductus arteriosus, or complete AV canal), which cause increased pulmonary blood flow, may result in pulmonary hypertension. If these defects are not repaired early, the high pulmonary flow will cause changes in the pulmonary artery vessels, and the vessels will lose their elasticity. The blood does not shunt right to left, a pulmonary embolism is not a complication of ventricular septal defect, and the left ventricle does not hypertrophy. 45. A 6-month-old infant presents to the clinic with failure to thrive, a history of frequent respiratory infections, and increasing exhaustion during feedings. On physical examination, a systolic murmur is detected, no central cyanosis, and chest radiography reveals cardiomegaly. An echocardiogram is done that shows left-to-right shunting. This assessment data is characteristic of what? a. Tetralogy of Fallot b. Coarctation of the aorta c. Pulmonary stenosis d. Ventricular septal defect Heart failure is common with ventricular septal defect that causes failure to thrive, respiratory infections, and an increase in exhaustion during feedings. There is a characteristic murmur. The other defects do not have left-to-right shunting. TRANSPOSITION OF GREAT VESSELS (TGV) 46. An infant is diagnosed with transposition of the great vessels. Prostaglandin E1 is given intravenously. The parents ask how long the child will remain on the prostaglandin E1. What is the appropriate response by the nurse? a. Prostaglandin E1 will be given intermittently until corrective surgery is performed. b. Prostaglandin E1 will be given continuously until corrective surgery is performed. c. Prostaglandin E1 will be given continuously throughout the preoperative and postoperative periods until the child is stable. d. Prostaglandin E1 will be given intermittently throughout the preoperative and postoperative periods until the child is stable. 47. What medication used to treat heart failure (HF) is a diuretic? a. Captopril (Capten) b. Digoxin (Lanoxin) c. Hydrochlorothiazide (Diuril) d. Carvedilol (Coreg) ENDOCARDITIS 27. A parent of a 7-year-old girl with a repaired ventricular septal defect (VSD) calls the cardiology clinic and reports that the child is just not herself. Her appetite is decreased, she has had intermittent fevers around 38 C (100.4 F), and now her muscles and joints ache. Based on this information, how should the nurse advise the mother? a. Immediately bring the child to the clinic for evaluation. b. Come to the clinic next week on a scheduled appointment. c. Treat the signs and symptoms with acetaminophen and fluids because it is most likely a viral illness. d. Recognize that the child is trying to manipulate the parent by complaining of vague symptoms. 28. What primary nursing intervention should be implemented to prevent bacterial endocarditis? a. Counsel parents of high-risk children. b. Institute measures to prevent dental procedures. c. Encourage restricted mobility in susceptible children. d. Observe children for complications, such as embolism and heart failure. 50. Bacterial infective endocarditis (IE) should be treated with which protocol? a. Oral antibiotics for 6 months b. Oral antibiotics (penicillin) for 10 full days c. IV antibiotics, diuretics, and digoxin d. IV antibiotics (penicillin type) for 2 to 8 weeks Treatment for IE includes the administration of high-dose antibiotics given intravenously for 2 to 8 weeks to completely eradicate the infecting microorganism. RHEUMATIC FEVER 29. What sign/symptom is a major clinical manifestation of rheumatic fever (RF)? a. Fever b. Polyarthritis c. Osler nodes d. Janeway spots 30. What action by the school nurse is important in the prevention of rheumatic fever (RF)? a. Encourage routine cholesterol screenings. b. Conduct routine blood pressure screenings. c. Refer children with sore throats for throat cultures. d. Recommend salicylates instead of acetaminophen for minor discomforts. 31. When caring for the child with Kawasaki disease, what should the nurse know to provide safe and effective care? a. Aspirin is contraindicated. b. The principal area of involvement is the joints. c. The childs fever is usually responsive to antibiotics within 48 hours. d. Therapeutic management includes administration of gamma globulin and salicylates. 32. Nursing care of the child with Kawasaki disease is challenging because of which occurrence? a. The childs irritability b. Predictable disease course c. Complex antibiotic therapy d. The childs ongoing requests for food 51. A child is recovering from Kawasaki disease (KD). The child should be monitored for which? a. Anemia b. Electrocardiograph (ECG) changes c. Elevated white blood cell count d. Decreased platelets 1. The nurse is caring for a child with Kawasaki disease in the acute phase. What clinical manifestations should the nurse expect to observe? (Select all that apply.) a. Osler nodes b. Cervical lymphadenopathy c. Strawberry tongue d. Chorea e. Erythematous palms f. Polyarthritis , C, E Clinical manifestations of Kawasaki disease in the acute phase include cervical lymphadenopathy, a strawberry tongue, and erythematous palms. Osler nodes are a clinical manifestation of endocarditis. Chorea and polyarthritis are seen in rheumatic fever. Chapter 30 SICKLE CELL ANEMIA 10. What condition occurs when the normal adult hemoglobin is partly or completely replaced by abnormal hemoglobin? a. Aplastic anemia b. Sickle cell anemia c. Thalassemia major d. Iron deficiency anemia 11. The parents of a child with sickle cell anemia (SCA) are concerned about subsequent children having the disease. What statement most accurately reflects inheritance of SCA? a. SCA is not inherited. b. All siblings will have SCA. c. Each sibling has a 25% chance of having SCA. d. There is a 50% chance of siblings having SCA. 12. The clinical manifestations of sickle cell anemia (SCA) are primarily the result of which physiologic alteration? a. Decreased blood viscosity b. Deficiency in coagulation c. Increased red blood cell (RBC) destruction d. Greater affinity for oxygen 13. A school-age child is admitted in vasoocclusive sickle cell crisis (pain episode). The childs care should include which therapeutic interventions? a. Hydration and pain management b. Oxygenation and factor VIII replacement c. Electrolyte replacement and administration of heparin d. Correction of alkalosis and reduction of energy expenditure 14. A child with sickle cell anemia (SCA) develops severe chest and back pain, fever, a cough, and dyspnea. What should be the first action by the nurse? a. Administer 100% oxygen to relieve hypoxia. b. Notify the practitioner because chest syndrome is suspected. c. Infuse intravenous antibiotics as soon as cultures are obtained. d. Give ordered pain medication to relieve symptoms of pain episode. TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 15. In a child with sickle cell anemia (SCA), adequate hydration is essential to minimize sickling and delay the vasoocclusion and hypoxiaischemia cycle. What information should the nurse share with parents in a teaching plan? a. Encourage drinking. b. Keep accurate records of output. c. Check for moist mucous membranes. d. Monitor the concentration of the childs urine. 19. In which condition are all the formed elements of the blood simultaneously depressed? a. Aplastic anemia b. Sickle cell anemia c. Thalassemia major d. Iron deficiency anemia 32. A 5-year-old child is admitted to the hospital in a sickle cell crisis. The child has been alert and oriented but in severe pain. The nurse notes that the child is complaining of a headache and is having unilateral hemiplegia. What action should the nurse implement? a. Notify the health care provider. b. Place the child on bed rest. c. Administer a dose of hydrocodone (Vicodin). d. Start O2 per the hospitals protocol. Any number of neurologic symptoms can indicate a minor cerebral insult, such as headache, aphasia, weakness, convulsions, visual disturbances, or unilateral hemiplegia. Loss of vision is usually the result of progressive retinopathy and retinal detachment. The nurse should notify the health care provider. 33. What pain medication is contraindicated in children with sickle cell disease (SCD)? a. Meperidine (Demerol) b. Hydrocodone (Vicodin) c. Morphine sulfate d. Ketorolac (Toradol) Meperidine (pethidine [Demerol]) is not recommended. Normeperidine, a metabolite of meperidine, is a central nervous system stimulant that produces anxiety, tremors, myoclonus, and generalized seizures when it accumulates with repetitive dosing. Patients with SCD are particularly at risk for normeperidine-induced seizures. 47. A child with sickle cell disease is in a vasoocclusive crisis. What nonpharmacologic pain intervention should the nurse plan? a. Exercise as a distraction b. Heat to the affected area c. Elevation of the extremity d. Cold compresses to the affected area 34. In anticipation of the admission of a child with hereditary spherocytosis (HS) who is experiencing an aplastic crisis, what action should the nurse plan? a. Secure an isolation room. b. Prepare for a transfusion of packed red blood cells. c. Anticipate preoperative preparation for a splenectomy. d. Gather equipment and medication for treatment of shock. B-THALASSEMIA 16. What statement best describes b-thalassemia major (Cooley anemia)? a. It is an acquired hemolytic anemia. b. Inadequate numbers of red blood cells (RBCs) are present. c. Increased incidence occurs in families of Mediterranean extraction. d. It commonly occurs in individuals from West Africa. 17. What therapeutic intervention is most appropriate for a child with b-thalassemia major? a. Oxygen therapy b. Supplemental iron c. Adequate hydration d. Frequent blood transfusions 10. The nurse is caring for a 12-year-old child with b-thalassemia. What clinical manifestations should the nurse expect to observe? (Select all that apply.) a. Anorexia b. Unexplained fever c. Enlarged spleen or liver d. Bronzed, freckled complexion e. Precocious sexual development , B, C, D The clinical manifestations of b-thalassemia include anorexia; unexplained fever; an enlarged spleen or liver; and a bronzed, freckled complexion. There is delayed sexual maturation, not precocious. HEMOPHILIA 21. What statement is descriptive of most cases of hemophilia? a. X-linked recessive deficiency of platelets causing prolonged bleeding b. X-linked recessive inherited disorder in which a blood clotting factor is deficient c. Autosomal dominant deficiency of a factor involved in the blood-clotting reaction d. Y-linked recessive inherited disorder in which the red blood cells become moon shaped DIF: Cognitive Level: Understanding REF: p. 1357 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 22. The nurse is teaching the family of a child, age 8 years, with moderate hemophilia about home care. What should the nurse tell the family to do to minimize joint injury? a. Administer nonsteroidal anti-inflammatory drugs (NSAIDs). b. Administer DDAVP (synthetic vasopressin). c. Provide intravenous (IV) infusion of factor VIII concentrates. d. Encourage elevation and application of ice to the involved joint. 35. A child with hemophilia A will have which abnormal laboratory result? a. PT (ProTime) b. Platelet count c. Fibrinogen level d. PTT (partial thromboplastin time) 36. A child with hemophilia A is scheduled for surgery. What precautions should the nurse institute with this child? a. Handle the child gently when transferring to a cart. b. Caution the child not to brush his teeth before surgery. c. Use tape sparingly on postoperative dressings. d. Do not administer analgesics before surgery. 39. The nurse is caring for a child with hemophilia A. The childs activity is as tolerated. What activity is contraindicated for this child? a. Ambulating to the cafeteria b. Active range of motion c. Ambulating to the playroom d. Passive range of motion exercises 2. What activity should the school nurse recommend for a child with hemophilia A? (Select all that apply.) a. Golf b. Soccer c. Rugby d. Jogging e. Swimming Ch. 31 NURSING CARE FOR A CHILD WITH CANCER 1. What childhood cancer may demonstrate patterns of inheritance that suggest a familial basis? a. Leukemia b. Retinoblastoma c. Rhabdomyosarcoma d. Osteogenic sarcoma 6. What guidelines should the nurse follow when handling chemotherapeutic agents? (Select all that apply.) a. Use clean technique. b. Prepare medications in a safety cabinet. c. Wear gloves designed for handling chemotherapy. d. Wear face and eye protection when splashing is possible. e. Discard gloves and protective clothing in a special container. 7. What strategies should the nurse implement to increase nutritional intake for the child receiving chemotherapy? (Select all that apply.) a. Allow the child any food tolerated. b. Fortify foods with nutritious supplements. c. Allow the child to be involved in food selection. d. Encourage the parents to place pressure on the importance of eating. e. Encourage the child to eat favorite foods during infusion of chemotherapy medications. 2. As part of the diagnostic evaluation of a child with cancer, biopsies are important for staging. What statement explains what staging means? a. Extent of the disease at the time of diagnosis b. Rate normal cells are being replaced by cancer cells c. Biologic characteristics of the tumor or lymph nodes d. Abnormal, unrestricted growth of cancer cells producing organ damage 3. What statement related to clinical trials developed for pediatric cancers is most accurate? a. Are accessible only in major pediatric centers b. Do not require consent for standard therapy c. Provide the best available therapy compared with an expected improvement d. Are standardized to provide the same treatment to all children with the disease 4. Chemotherapeutic agents are classified according to what feature? a. Side effects b. Effectiveness c. Mechanism of action d. Route of administration 5. What type of chemotherapeutic agent alters the function of cells by replacing a hydrogen atom of a molecule? a. Plant alkaloids b. Antimetabolites c. Alkylating agents d. Antitumor antibiotics 6. What side effect commonly occurs with corticosteroid (prednisone) therapy? a. Alopecia b. Anorexia c. Nausea and vomiting d. Susceptibility to infection 7. What chemotherapeutic agent is classified as an antitumor antibiotic? a. Cisplatin (Platinol AQ) b. Vincristine (Oncovin) c. Methotrexate (Texall) d. Daunorubicin (Cerubidine) 8. The nurse is administering an intravenous chemotherapeutic agent to a child with leukemia. The child suddenly begins to wheeze and have severe urticaria. What nursing action is most appropriate to initiate? a. Recheck the rate of drug infusion. b. Stop the drug infusion immediately. c. Observe the child closely for next 10 minutes. d. Explain to the child that this is an expected side effect. 9. Total-body irradiation is indicated for what reason? a. Palliative care b. Lymphoma therapy c. Definitive therapy for leukemia d. Preparation for bone marrow transplant 10. The parents of a child with cancer tell the nurse that a bone marrow transplant (BMT) may be necessary. What information should the nurse recognize as important when discussing this with the family? a. BMT should be done at the time of diagnosis. b. Parents and siblings of the child have a 25% chance of being a suitable donor. c. If BMT fails, chemotherapy or radiotherapy will need to be continued. d. Finding a suitable donor involves matching antigens from the human leukocyte antigen (HLA) system. 11. An adolescent will receive a bone marrow transplant (BMT). The nurse should explain that the bone marrow will be administered by which method? a. Bone grafting b. Intravenous infusion c. Bone marrow injection d. Intraabdominal infusion 12. After chemotherapy is begun for a child with acute leukemia, prophylaxis to prevent acute tumor lysis syndrome includes which therapeutic intervention? a. Hydration b. Oxygenation c. Corticosteroids d. Pain management 13. Nursing care of the child with myelosuppression from leukemia or chemotherapeutic agents should include which therapeutic intervention? a. Restrict oral fluids. b. Institute strict isolation. c. Use good hand-washing technique. d. Give immunizations appropriate for age. 14. In teaching parents how to minimize or prevent bleeding episodes when the child is myelosuppressed, the nurse includes what information? a. Meticulous mouth care is essential to avoid mucositis. b. Rectal temperatures are necessary to monitor for infection. c. Intramuscular injections are preferred to intravenous ones. d. Platelet transfusions are given to maintain a count greater than 50,000/mm3. 15. A school-age child with leukemia experienced severe nausea and vomiting when receiving chemotherapy for the first time. What is the most appropriate nursing action to prevent or minimize these reactions with subsequent treatments? a. Administer the chemotherapy between meals. b. Give an antiemetic before chemotherapy begins. c. Have the child bring favorite foods for snacks. d. Keep the child NPO (nothing by mouth) until nausea and vomiting subside. 16. A young child with leukemia has anorexia and severe stomatitis. What approach should the nurse suggest that the parents try? a. Relax any eating pressures. b. Firmly insist that the child eat normally. c. Serve foods that are either hot or cold. d. Provide only liquids because chewing is painful. 17. The nurse is preparing a child for possible alopecia from chemotherapy. What information should the nurse include? a. Wearing hats or scarves is preferable to a wig. b. Expose head to sunlight to stimulate hair regrowth. c. Hair may have a slightly different color or texture when it regrows. d. Regrowth of hair usually begins 12 months after chemotherapy ends. 18. What pain management approach is most effective for a child who is having a bone marrow test? a. Relaxation techniques b. Administration of an opioid c. EMLA cream applied over site d. Conscious or unconscious sedation 19. The nurse is caring for a child receiving chemotherapy for leukemia. The childs granulocyte count is 600/mm3 and platelet count is 45,000/mm3. What oral care should the nurse recommend for this child? a. Rinsing mouth with water b. Daily toothbrushing and flossing c. Lemon glycerin swabs for cleansing d. Wiping teeth with moistened gauze or Toothettes 20. What immunization should not be given to a child receiving chemotherapy for cancer? a. Tetanus vaccine b. Inactivated poliovirus vaccine c. Diphtheria, pertussis, tetanus (DPT) d. Measles, mumps, rubella (MMR) 21. What description identifies the pathophysiology of leukemia? a. Increased blood viscosity b. Abnormal stimulation of the first stage of coagulation process c. Unrestricted proliferation of immature white blood cells (WBCs) d. Thrombocytopenia from an excessive destruction of platelets 22. A child with leukemia is receiving intrathecal chemotherapy to prevent which condition? a. Infection b. Brain tumor c. Central nervous system (CNS) disease d. Drug side effects 23. A parent tells the nurse that 80% of children with the same type of leukemia as his sons have a 5-year survival. He believes that because another child on the same protocol as his son has just died, his son now has a better chance of success. What is the best response by the nurse? a. It is sad for the other family but good news for your child. b. Each child has an 80% likelihood of 5-year survival. c. The data suggest that 20% of the children in the clinic will die. There are still many hurdles for your son. d. You should avoid the grieving family because you will be benefiting from their loss. 1. The nurse is precepting a new graduate nurse at an ambulatory pediatric hematology and oncology clinic. What cardinal signs of cancer in children should the nurse make the new nurse aware of? (Select all that apply.) a. Sudden tendency to bruise easily b. Transitory, generalized pain c. Frequent headaches d. Excessive, rapid weight gain e. Gradual, steady fever f. Unexplained loss of energy 2. A child on chemotherapy has developed rectal ulcers. What interventions should the nurse teach to the child and parents to relieve the discomfort of rectal ulcers? (Select all that apply.) a. Warm sitz baths b. Use of stool softeners c. Record bowel movements d. Use of an opioid for discomfort e. Occlusive ointment applied to the area 42. What chemotherapeutic agent can cause an anaphylactic reaction? a. Prednisone (Deltasone) b. Vincristine (Oncovin) c. L-Asparaginase (Elspar) d. Methotrexate (Trexall) 43. A child with cancer being treated with chemotherapy is receiving a platelet transfusion. The nurse understands that the transfused platelets should survive the body for how many days? a. 1 to 3 days b. 4 to 6 days c. 7 to 9 days d. 10 to 12 days 44. Daily toothbrushing and flossing can be encouraged for the child on chemotherapy when the platelet count is above which? a. 10,000/mm3 b. 20,000/mm3 c. 30,000/mm3 d. 40,000/mm3 45. A parent of a hospitalized child on chemotherapy asks the nurse if a sibling of the hospitalized child should receive the varicella vaccination. The nurse should give which response? a. The sibling can get a varicella vaccination. b. The sibling should not get a varicella vaccination. c. The sibling should wait until the child is finished with chemotherapy. d. The sibling should get varicella-zoster immune globulin if exposed to chickenpox. Siblings and other family members can receive the live measles, mumps, and rubella vaccine and the varicella vaccine without risk to the child who is immunosuppressed. ACUTE LYMPHOID LEUKEMIA (ALL) 3. What are favorable prognostic criteria for acute lymphoblastic leukemia? (Select all that apply.) a. Male gender b. CALLA positive c. Early preB cell d. 2 to 10 years of age e. Leukocyte count ?7?50,000/mm3 31. The nurse is caring for a 6-year-old child with acute lymphoblastic leukemia (ALL). The parent states, My child has a low platelet count, and we are being discharged this afternoon. What do I need to do at home? What statement is most appropriate for the nurse to make? a. You should give your child aspirin instead of acetaminophen for fever or pain. b. Your child should avoid contact sports or activities that could cause bleeding. c. You should feed your child a bland, soft, moist diet for the next week. d. Your child should avoid large groups of people for the next week. A child with a low platelet count needs to avoid activities that could cause bleeding such as playing contact sports, climbing trees, using playground equipment, or bike riding. The child should be given acetaminophen, not aspirin, for fever or pain; the child does not need to be on a soft, bland diet or avoid large groups of people because of the low platelet count. 38. What is appropriate mouth care for a toddler with mucosal ulceration related to chemotherapy? a. Mouthwashes with plain saline b. Lemon glycerin swabs for cleansing c. Mouthwashes with hydrogen peroxide d. Swish and swallow with viscous lidocaine Administering mouth care is particularly difficult in infants and toddlers. A satisfactory method of cleaning the gums is to wrap a piece of gauze around a finger; soak it in saline or plain water; and swab the gums, palate, and inner cheek surfaces with the finger. Mouth rinses are best accomplished with plain water or saline because the child cannot gargle or spit out excess fluid. Avoid agents such as lemon glycerin swabs and hydrogen peroxide because of the drying effects on the mucosa. Lidocaine should be avoided in young children. NEUROBLASTOMA 35. A child, age 10 years, has a neuroblastoma and is in the hospital for additional chemotherapy treatments. What laboratory values are most likely this childs? a. White blood cell count, 17,000/mm3; hemoglobin, 15 g/dl b. White blood cell count, 3,000/mm3; hemoglobin, 11.5 g/dl c. Platelets, 450,000/mm3; hemoglobin, 12 g/dl d. White blood cell count, 10,000/mm3; platelets, 175,000/mm3 46. The nurse is collecting a 24-hour urine sample on a child with suspected diagnosis of neuroblastoma. What finding in the urine is expected with neuroblastomas? a. Ketones b. Catecholamines c. Red blood cells d. Excessive white blood cells Neuroblastomas, particularly those arising on the adrenal glands or from a sympathetic chain, excrete the catecholamines epinephrine and norepinephrine. Urinary excretion of catecholamines is detected in approximately 95% of children with adrenal or sympathetic tumors. RETINOBLASTOMA 39. The nurse should expect to care for which age of child if the admitting diagnosis is retinoblastoma? a. Infant or toddler b. Preschool- or school-age child c. School-age or adolescent child d. 5. The nurse is caring for a child with retinoblastoma that was treated with an enucleation. What interventions should the nurse plan for care of an eye socket after enucleation? (Select all that apply.) a. Clean the prosthesis. b. Change the eye pad daily. c. Keep the opposite eye covered initially. d. Irrigate the socket daily with a prescribed solution. e. Apply a prescribed antibiotic ointment after irrigation. CHAPTER 32 INCREASED ICP 2. What finding is a clinical manifestation of increased intracranial pressure (ICP) in children? a. Low-pitched cry b. Sunken fontanel c. Diplopia, blurred vision d. Increased blood pressure 11. What is a nursing intervention to reduce the risk of increasing intracranial pressure (ICP) in an unconscious child? a. Suction the child frequently. b. Turn the childs head side to side every hour. c. Provide environmental stimulation. d. Avoid activities that cause pain or crying. 33. The nurse is caring for a 10-year-old child who has an acute head injury, has a pediatric Glasgow Coma Scale score of 9, and is unconscious. What intervention should the nurse include in the childs care plan? a. Elevate the head of the bed 15 to 30 degrees with the head maintained in midline. b. Maintain an active, stimulating environment. c. Perform chest percussion and suctioning every 1 to 2 hours. d. Perform active range of motion and nontherapeutic touch every 8 hours. 1. The nurse is preparing to admit a 6-month-old infant with increased intracranial pressure (ICP). What clinical manifestations should the nurse expect to observe in this infant? (Select all that apply.) a. High-pitched cry b. Poor feeding c. Setting-sun sign d. Sunken fontanel e. Distended scalp veins f. Decreased head circumference 2. The nurse is caring for a child with increased intracranial pressure (ICP). What interventions should the nurse plan for this child? (Select all that apply.) a. Avoid jarring the bed. b. Keep the room brightly lit. c. Keep the bed in a flat position. d. Administer prescribed stool softeners. e. Administer a prescribed antiemetic for nausea. HEAD INJURY 16. A school-age child has sustained a head injury and multiple fractures after being thrown from a horse. The childs level of consciousness is variable. The parents tell the nurse that they think their child is in pain because of periodic crying and restlessness. What is the most appropriate nursing action? a. Explain that analgesia is contraindicated with a head injury. b. Have the parents describe the childs previous experiences with pain. c. Consult with a practitioner about what analgesia can be safely administered. d. Teach the parents that analgesia is unnecessary when the child is not fully awake and alert. 17. The nurse is assessing a child who was just admitted to the hospital for observation after a head injury. What clinical manifestation is the most essential part of the nursing assessment to detect early signs of a worsening condition? a. Posturing b. Vital signs c. Focal neurologic signs d. Level of consciousness 33. The nurse is caring for a 10-year-old child who has an acute head injury, has a pediatric Glasgow Coma Scale score of 9, and is unconscious. What intervention should the nurse include in the childs care plan? a. Elevate the head of the bed 15 to 30 degrees with the head maintained in midline. b. Maintain an active, stimulating environment. c. Perform chest percussion and suctioning every 1 to 2 hours. d. Perform active range of motion and nontherapeutic touch every 8 hours. MENINGITIS 20. The mother of a 1-month-old infant tells the nurse she worries that her baby will get meningitis like the childs younger brother had when he was an infant. The nurse should base a response on which information? a. Meningitis rarely occurs during infancy. b. Often a genetic predisposition to meningitis is found. c. Vaccination to prevent all types of meningitis is now available. d. Vaccinations to prevent pneumococcal and Haemophilus influenzae type B meningitis are available. 21. A toddler is admitted to the pediatric unit with presumptive bacterial meningitis. The initial orders include isolation, intravenous access, cultures, and antimicrobial agents. The nurse knows that antibiotic therapy will begin when? a. After the diagnosis is confirmed b. When the medication is received from the pharmacy c. After the childs fluid and electrolyte balance is stabilized d. As soon as the practitioner is notified of the culture results 22. The nurse is planning care for a school-age child with bacterial meningitis. What intervention should be included? a. Keep environmental stimuli to a minimum. b. Have the child move her head from side to side at least every 2 hours. c. Avoid giving pain medications that could dull sensorium. d. Measure head circumference to assess developing complications. 46. A child develops syndrome of inappropriate antidiuretic hormone secretion (SIADH) as a complication to meningitis. What action should be verified before implementing? a. Forcing fluids b. Daily weights with strict input and output (I and O) c. Strict monitoring of urine volume and specific gravity d. Close observation for signs of increasing cerebral edema The treatment of SIADH consists of fluid restriction until serum electrolytes and osmolality return to normal levels. SIADH often occurs in children who have meningitis. Monitoring weights, keeping I and O and specific gravity of urine, and observing for signs of increasing cerebral edema are all part of the nursing care for a child with SIADH. 49. A 23-month-old child is admitted to the hospital with a diagnosis of meningitis. She is lethargic and very irritable with a temperature of 102 F. What should the nurses care plan include? a. Observing the childs voluntary movement b. Checking the Babinski reflex every 4 hours c. Checking the Brudzinski reflex every 1 hour d. Assessing the level of consciousness (LOC) and vital signs every 2 hours 50. A lumbar puncture (LP) is being done on an infant with suspected meningitis. The nurse expects which results for the cerebrospinal fluid that can confirm the diagnosis of meningitis? a. WBCs; glucose b. RBCs; normal WBCs c. glucose; normal RBCs d. Normal RBCs; normal glucose 5. The nurse is preparing to admit a neonate with bacterial meningitis. What clinical manifestations should the nurse expect to observe? (Select all that apply.) a. Jaundice b. Cyanosis c. Poor tone d. Nuchal rigidity e. Poor sucking ability 6. The nurse is preparing to admit an adolescent with bacterial meningitis. What clinical manifestations should the nurse expect to observe? (Select all that apply.) a. Fever b. Chills c. Headache d. Poor tone e. Drowsiness 7. The nurse is caring for a child with meningitis. What acute complications of meningitis should the nurse continuously assess the child for? (Select all that apply.) a. Seizures b. Cerebral palsy c. Cerebral edema d. Hydrocephalus e. Cognitive impairments 8. What cerebrospinal fluid (CSF) analysis should the nurse expect with viral meningitis? (Select all that apply.) a. Color is turbid. b. Protein count is normal. c. Glucose is decreased. d. Gram stain findings are negative. e. White blood cell (WBC) count is slightly elevated. 11. What effects of an altered pituitary secretion in a child with meningitis indicates syndrome of inappropriate antidiuretic hormone (SIADH)? (Select all that apply.) a. Hypotension b. Serum sodium is decreased c. Urinary output is decreased d. Evidence of overhydration e. Urine specific gravity is increased , C, D, E EPILEPSY 25. What term refers to seizures that involve both hemispheres of the brain? a. Absence b. Acquired c. Generalized d. Complex partial 26. What is the initial clinical manifestation of generalized seizures? a. Confusion b. Feeling frightened c. Loss of consciousness d. Seeing flashing lights 27. What type of seizure may be difficult to detect? a. Absence b. Generalized c. Simple partial d. Complex partial 28. What is important to incorporate in the plan of care for a child who is experiencing a seizure? a. Describe and record the seizure activity observed. b. Suction the child during a seizure to prevent aspiration. c. Place a tongue blade between the teeth if they become clenched. d. Restrain the child when seizures occur to prevent bodily harm. 29. A 10-year-old child, without a history of previous seizures, experiences a tonic-clonic seizure at school that lasts more than 5 minutes. Breathing is not impaired. Some postictal confusion occurs. What is the most appropriate initial action by the school nurse? a. Stay with child and have someone else call emergency medical services (EMS). b. Notify the parent and regular practitioner. c. Notify the parent that the child should go home. d. Stay with the child, offering calm reassurance. 30. A child has been seizure free for 2 years. A father asks the nurse how much longer the child will need to take the antiseizure medications. How should the nurse respond? a. Medications can be discontinued at this time. b. The child will need to take the drugs for 5 years after the last seizure. c. A step-wise approach will be used to reduce the dosage gradually. d. Seizure disorders are a lifelong problem. Medications cannot be discontinued. 31. A young adolescent experiences infrequent migraine episodes. What pharmacologic intervention is most likely to be prescribed? a. Opioid b. Lorazepam c. Ergotamine d. Sumatriptan 32. The nurse is teaching the parents of a 3-year-old child who has been diagnosed with tonic-clonic seizures. What statement by the parent should indicate a correct understanding of the teaching? a. I should attempt to restrain my child during a seizure. b. My child will need to avoid contact sports until adulthood. c. I should place a pillow under my childs head during a seizure. d. My child will need to be taken to the emergency department [ED] after each seizure. 40. After a tonic-clonic seizure, what symptoms should the nurse expect the child to experience? a. Diarrhea and abdominal discomfort b. Irritability and hunger c. Lethargy and confusion d. Nervousness and excitability 41. What is the antiepileptic medication that requires monitoring of vitamin D and folic acid? a. Topiramate (Topamax) b. Valproic acid (Depakene) c. Gabapentin (Neurontin) d. Phenobarbital (Luminal) 42. A 2-year-old child starts to have a tonic-clonic seizure. The childs jaws are clamped. What is the most important nursing action at this time? a. Place a padded tongue blade between the childs jaws. b. Stay with the child and observe his respiratory status. c. Prepare the suction equipment. d. Restrain the child to prevent injury. 43. A child has been admitted with status epilepticus. An emergency medication has been ordered. What medication should the nurse expect to be prescribed? a. Lorazepam (Ativan) b. Phenytoin (Dilantin) c. Topiramate (Topamax) d. Ethosuximide (Zarontin) 45. A child has a seizure disorder. What test should be done to gather the most specific information about the type of seizure the child is having? a. Sleep study b. Skull radiography c. Serum electrolytes d. Electroencephalogram (EEG) 10. The nurse is preparing to admit a 7-year-old child with complex partial seizures. What clinical features of complex partial seizures should the nurse recognize? (Select all that apply.) a. They last less than 10 seconds. b. There is usually no aura. c. Mental disorientation is common. d. There is frequently a postictal state. e. There is usually an impaired consciousness. 13. The nurse is preparing to admit a 10-year-old child with absence seizures. What clinical features of absence seizures should the nurse recognize? (Select all that apply.) a. There is no aura. b. There is a postictal state. c. They usually last longer than 30 seconds. d. There is a brief loss of consciousness. e. There is an occasional clonic movement. 14. The nurse is teaching the parents of a child with a seizure disorder about the triggers that can cause a seizure. What should the nurse include in the teaching session? (Select all that apply.) a. Cold b. Sugared drinks c. Emotional stress d. Flickering lights e. Hyperventilation HYDROCEPHALUS 34. What clinical manifestations suggest hydrocephalus in an infant? a. Closed fontanel and high-pitched cry b. Bulging fontanel and dilated scalp veins c. Constant low-pitched cry and restlessness d. Depressed fontanel and decreased blood pressure 35. A pregnant woman asks about prenatal diagnosis of hydrocephalus. The nurses response should be based on which knowledge? a. It can be diagnosed only after birth. b. It can be diagnosed by chromosome studies. c. It can be diagnosed with fetal ultrasonography. d. It can be diagnosed by measuring the lecithin-to-sphingomyelin ratio. 36. A child is admitted for revision of a ventriculoperitoneal shunt for noncommunicating hydrocephalus. What is a common reason for elective revision of this shunt? a. Meningitis b. Gastrointestinal upset c. Hydrocephalus resolution d. Growth of the child since the initial shunting 39. A 6-year-old child is admitted for revision of a ventriculoperitoneal shunt for noncommunicating hydrocephalus. What sign or symptom does the child have that indicates a revision is necessary? a. Tachycardia b. Gastrointestinal upset c. Hypotension d. Alteration in level of consciousness In older children, who are usually admitted to the hospital for elective or emergency shunt revision, the most valuable indicators of increasing intracranial pressure are an alteration in the childs level of consciousness, complaint of headache, and changes in interaction with the environment. CHAPTER 33 16. Glucocorticoids, mineralocorticoids, and sex steroids are secreted by which gland? a. Thyroid gland b. Adrenal cortex c. Anterior pituitary d. Parathyroid glands GROWTH HORMONE DEFICIENCY 40. The nurse is assisting with a growth hormone stimulation test for a child with short stature. What should the nurse monitor closely on this child during the test? a. Hypotension b. Tachycardia c. Hypoglycemia d. Nausea and vomiting 6. The nurse is preparing to assist with a growth hormone provocative test for a child with short stature. The nurse recognizes that which pharmacologics should be used to provoke the release of growth hormone (GH)? (Select all that apply.) a. Larodopa (levodopa) b. Clonidine (Catapres) c. Propranolol (Inderal) d. Cortisone (hydrocortisone) e. Biosynthetic growth hormone 1. Homeostasis in the body is maintained by what is collectively known as the neuroendocrine system. What is the name of the nervous system that is involved? a. Central b. Skeletal c. Peripheral d. Autonomic 2. A child with hypopituitarism is being started on growth hormone (GH) therapy. Nursing considerations should be based on which knowledge? a. Therapy is most successful if it is started during adolescence. b. Replacement therapy requires daily subcutaneous injections. c. Hormonal supplementation will be required throughout childs lifetime. d. Treatment is considered successful if children attain full stature by adolescence. 3. A child with growth hormone (GH) deficiency is receiving GH therapy. When is the best time for the GH to be administered? a. At bedtime b. After meals c. Before meals d. After arising in morning 4. What is a condition that can result if hypersecretion of growth hormone (GH) occurs after epiphyseal closure? a. Cretinism b. Dwarfism c. Gigantism d. Acromegaly DIABETES INSIPIDUS The nurse is planning care for a child recently diagnosed with diabetes insipidus (DI). What intervention should be included? a. Encourage the child to wear medical identification. b. Discuss with the child and family ways to limit fluid intake. c. Teach the child and family how to do required urine testing. d. Reassure the child and family that this is usually not a chronic or life-threatening illness. 8. Intranasal administration of desmopressin acetate (DDAVP) is used to treat which condition? a. Hypopituitarism b. Diabetes insipidus (DI) c. Syndrome of inappropriate antidiuretic hormone (SIADH) d. Acute adrenocortical insufficiency DDAVP is the treatment of choice for DI. It is administered intranasally through a flexible tube. The childs response pattern is variable, with effectiveness lasting from 6 to 24 hours. SIADH 2. The nurse is preparing to admit a 9-year-old child with syndrome of inappropriate antidiuretic hormone (SIADH). What interventions should the nurse include in the childs care plan? (Select all that apply.) a. Provide a low-sodium, low-fat diet. b. Initiate seizure precautions. c. Weigh daily at the same time each day. d. Encourage intake of 1 l of fluid per day. e. Measure intake and output hourly. 8. The nurse is planning to admit a 10-year-old child with syndrome of inappropriate antidiuretic hormone (SIADH). What clinical manifestations should the nurse expect to observe in this child? (Select all that apply.) a. Polyuria b. Anorexia c. Polydipsia d. Irritability e. Stomach cramps 9. What nursing care should be included for a child diagnosed with syndrome of inappropriate antidiuretic hormone (SIADH)? a. Maintain the child NPO (nothing by mouth). b. Turn the child frequently. c. Restrict fluids. d. Encourage fluids. DM1 18. What form of diabetes is characterized by destruction of pancreatic beta cells, resulting in insulin deficiency? a. Type 1 diabetes b. Type 2 diabetes c. Gestational diabetes d. Maturity-onset diabetes of the young (MODY) 19. What statement is characteristic of type 1 diabetes mellitus? a. Onset is usually gradual. b. Ketoacidosis is infrequent. c. Peak age incidence is 10 to 15 years. d. Oral agents are available for treatment. 20. What clinical manifestation is considered a cardinal sign of diabetes mellitus? a. Nausea b. Seizures c. Impaired vision d. Frequent urination 1. The nurse is preparing a community outreach program for adolescents about the characteristic differences between type 1 and type 2 diabetes mellitus (DM). What concepts should the nurse include? (Select all that apply.) a. Type 1 DM has an abrupt onset. b. Type 1 DM is often controlled with oral glucose agents. c. Type 1 DM occurs primarily in whites. d. Type 2 DM always requires insulin therapy. e. Type 2 DM frequently has a familial history. f. Type 2 DM occurs in people who are overweight. 1. The nurse is preparing to administer a prescribed dose of desmopressin acetate (DDAVP) intramuscularly (IM) to a child with diabetes insipidus. What action should the nurse take before drawing the medication into a syringe? a. Mix the medication with sterile water. b. Mix the medication with sterile normal saline. c. Have another nurse double-check the medication dose. d. Hold the medication under warm water for 10 to 15 minutes and then shake vigorously. 21. What blood glucose measurement is most likely associated with diabetic ketoacidosis? a. 185 mg/dl b. 220 mg/dl c. 280 mg/dl d. 330 mg/dl 22. The parents of a child who has just been diagnosed with type 1 diabetes ask about exercise. What effect does exercise have on a type 1 diabetic? a. Exercise increases blood glucose. b. Extra insulin is required during exercise. c. Additional snacks are needed before exercise. d. Excessive physical activity should be restricted. 23. A child eats some sugar cubes after experiencing symptoms of hypoglycemia. This rapid-releasing sugar should be followed by which dietary intervention? a. Sports drink and fruit b. Glucose tabs and protein c. Glass of water and crackers d. Milk and peanut butter on bread 24. A 20-kg (44-lb) child in ketoacidosis is admitted to the pediatric intensive care unit. What order should the nurse not implement until clarified with the physician? a. Weigh on admission and daily. b. Replace fluid volume deficit over 48 hours. c. Begin intravenous line with D5 0.45% normal saline with 20 mEq of potassium chloride. d. Give intravenous regular insulin 2 units/kg/hr after initial rehydration bolus. 25. What clinical manifestation occurs with hypoglycemia? a. Lethargy b. Confusion c. Nausea and vomiting d. Weakness and dizziness 26. A 12-year-old girl is newly diagnosed with diabetes when she develops ketoacidosis. How should the nurse structure a successful education program? a. Essential information is presented initially. b. Teaching should take place in the childs semiprivate room. c. Education is focused toward the parents because the child is too young. d. All information needed for self-management of diabetes is taught at once. 27. The nurse is discussing with a child and family the various sites used for insulin injections. What site usually has the fastest rate of absorption? a. Arm b. Leg c. Buttock d. Abdomen 28. The nurse is teaching an adolescent about giving insulin injections. The adolescent asks if the disposable needles and syringes can be used more than once. The nurses response should be based on which knowledge? a. It is unsafe. b. It is acceptable for up to 24 hours. c. It is acceptable for families with very limited resources. d. It is suitable for up to 3 days if stored in the refrigerator. 29. A preadolescent has maintained good glycemic control of his type 1 diabetes through the school year. During summer vacation, he has had repeated episodes of hypoglycemia. What additional teaching is needed? a. Carbohydrates in the diet need to be replaced with protein. b. Additional snacks are needed to compensate for increased activity. c. The child needs to decrease his activity level to minimize episodes of hypoglycemia. d. Insulin dosage should be increased to compensate for a change in activity level. 30. To help an adolescent deal with diabetes, the nurse needs to consider which characteristic of adolescence? a. Desire to be unique b. Preoccupation with the future c. Need to be perfect and similar to peers d. Awareness of peers that diabetes is a severe disease 31. An adolescent diabetic is admitted to the emergency department for treatment of hyperglycemia and pneumonia. What are characteristics of diabetic hyperglycemia? a. Cold, clammy skin and lethargy b. Hunger and hypertension c. Thirst, being flushed, and fruity breath d. Disorientation and pallor 32. A school-age child with diabetes gets 30 units of NPH insulin at 0800. According to when this insulin peaks, the child should be at greatest risk for a hypoglycemic episode between when? a. Lunch and dinner b. Breakfast and lunch c. 0830 to his midmorning snack d. Bedtime and breakfast the next morning 33. The nurse is teaching the parent of a preschool child how to administer the childs insulin injection. The child will be receiving 2 units of regular insulin and 12 units of NPH insulin every morning. What should the parent be taught? a. Draw the insulin in separate syringes. b. Draw the regular insulin first and then the NPH into the same syringe. c. Draw the NPH insulin first and then the regular into the same syringe. d. Check blood sugar first, and if below 120, hold the regular insulin and give the NPH. 34. What statement applies to the current focus of the dietary management of children with diabetes? a. Measurement of all servings of food is vital for control. b. Daily calculate specific amounts of carbohydrates, fats, and proteins. c. The number of calories for carbohydrates remains constant on a daily basis; protein and fat calories are liberal. d. The intake ensures day-to-day consistency in total calories, protein, carbohydrates, and moderate fat while allowing for a wide variety of foods. 4. The nurse is teaching the family of a child with type 1 diabetes about insulin. What should the nurse include in the teaching session? (Select all that apply.) a. Unopened vials are good for 60 days. b. Diabetic supplies should not be left in a hot environment. c. Insulin can be placed in the freezer if not used every day. d. After it has been opened, insulin is good for up to 28 to 30 days. e. Insulin bottles that have been opened should be stored at room temperature or refrigerated. 12. The nurse is preparing to admit a 7-year-old child with type 2 diabetes. What clinical features of type 2 diabetes should the nurse recognize? (Select all that apply.) a. Oral agents are effective. b. Insulin is usually needed. c. Ketoacidosis is infrequent. d. Diet only is often effective. e. Chronic complications frequently occur. DKA 11. What are characteristics of diabetic ketoacidosis? (Select all that apply.) a. Pallor b. Acidosis c. Bradypnea d. Dehydration e. Electrolyte imbalance CH 34 FRACTURE 2. The nurse is caring for a child immobilized because of Russel traction. What interventions should the nurse implement to prevent renal calculi? (Select all that apply.) a. Monitor output. b. Encourage the patient to drink apple juice. c. Encourage milk intake. d. Ensure adequate fluids. e. Encourage the patient to drink cranberry juice. 3. The nurse is assisting with application of a synthetic cast on a child with a fractured humerus. What are the advantages of a synthetic cast over a plaster of Paris cast? (Select all that apply.) a. Less bulky b. Drying time is faster c. Molds readily to body part d. Permits regular clothing to be worn e. Can be cleaned with small amount of soap and water 4. A child has had a short-arm synthetic cast applied. What should the nurse teach to the child and parents about cast care? (Select all that apply.) a. Relieve itching with heat. b. Elevate the arm when resting. c. Observe the fingers for any evidence of discoloration. d. Do not allow the child to put anything inside the cast. e. Examine the skin at the cast edges for any breakdown. 5. The nurse is conducting preoperative teaching to parents and their child about an external fixation device. What should the nurse include in the teaching session? (Select all that apply.) a. Pin care b. Crutch walking c. Modifications in activity d. Observing pin sites for infection e. Full weight bearing will be allowed after 24 hours 3. What is a physiologic effect of immobilization on children? a. Metabolic rate increases. b. Venous return improves because the child is in the supine position. c. Circulatory stasis can lead to thrombus and embolus formation. d. Bone calcium increases, releasing excess calcium into the body (hypercalcemia). 44. A child has just returned from surgery for repair of a fractured femur. The child has a long-leg cast on. The toes on the leg with the cast are edematous, but they have color, sensitivity, and movement. What action should the nurse take? a. Call the health care provider to report the edema. b. Elevate the foot and leg on pillows. c. Apply a warm moist pack to the foot. d. Encourage movement of toes. 46. What should the nurse plan for an immobilized child in cervical traction to prevent deep vein thrombosis (DVT)? a. Elevate the childs legs. b. Place a foot cradle on the bed. c. Place a pillow under the childs knees. d. Assist the child to dorsiflex the feet and rotate the ankles. 47. The nurse is teaching a child with a cast about cast removal. What should the nurse teach the child about cast removal? a. The cast cutter will be a quiet machine. b. You will feel cold as the cast is removed. c. You will feel a tickly sensation as the cast is removed. d. The cast cutter cuts through the cast like a circular saw. 48. A 3-year-old child has a femoral shaft fracture. The nurse recognizes that the approximate healing time for this child is how long? a. 2 weeks b. 4 weeks c. 6 weeks d. 8 weeks The approximate healing times for a femoral shaft fracture are as follows: neonatal period, 2 to 3 weeks; early childhood, 4 weeks; later childhood, 6 to 8 weeks; and adolescence, 8 to 12 weeks. 4. What condition can result from the bone demineralization associated with immobility? a. Osteoporosis b. Pooling of blood c. Urinary retention d. Susceptibility to infection 5. What measure is important in managing hypercalcemia in a child who is immobilized? a. Provide adequate hydration. b. Change position frequently. c. Encourage a diet high in calcium. d. Provide a diet high in calories for healing. 6. The nurse is caring for an immobilized preschool child. What intervention is helpful during this period of immobilization? a. Encourage wearing pajamas. b. Let the child have few behavioral limitations. c. Keep the child away from other immobilized children if possible. d. Take the child for a walk by wagon outside the room. 8. Immobilization causes what effect on metabolism? a. Hypocalcemia b. Decreased metabolic rate c. Positive nitrogen balance d. Increased levels of stress hormones 9. What finding is characteristic of fractures in children? a. Fractures rarely occur at the growth plate site because it absorbs shock well. b. Rapidity of healing is inversely related to the childs age. c. Pliable bones of growing children are less porous than those of adults. d. The periosteum of a childs bone is thinner, is weaker, and has less osteogenic potential compared to that of an adult. 10. A 14-year-old is admitted to the emergency department with a fracture of the right humerus epiphyseal plate through the joint surface. What information does the nurse know regarding this type of fracture? a. It will create difficulty because the child is left handed. b. It will heal slowly because this is the weakest part of the bone. c. This type of fracture requires different management to prevent bone growth complications. d. This type of fracture necessitates complete immobilization of the shoulder for 4 to 6 weeks. 11. Parents bring a 7-year-old child to the clinic for evaluation of an injured wrist after a bicycle accident. The parents and child are upset, and the child will not allow an examination of the injured arm. What priority nursing intervention should occur at this time? a. Send the child to radiology so radiography can be performed. b. Initiate an intravenous line and administer morphine for the pain. c. Calmly ask the child to point to where the pain is worst and to wiggle fingers. d. Have the parents hold the child so that the nurse can examine the arm thoroughly. 12. A 7-year-old child has just had a cast applied for a fractured arm with the wrist and elbow immobilized. What information should be included in the home care instructions? a. No restrictions of activity are indicated. b. Elevate casted arm when both upright and resting. c. The shoulder should be kept as immobile as possible to avoid pain. d. Swelling of the fingers is to be expected. Notify a health professional if it persists more than 48 hours. 13. The nurse uses the five Ps to assess ischemia in a child with a fracture. What finding is considered a late and ominous sign? a. Petaling b. Posturing c. Paresthesia d. Positioning 14. A child is upset because, when the cast is removed from her leg, the skin surface is caked with desquamated skin and sebaceous secretions. What technique should the nurse suggest to remove this material? a. Soak in a bathtub. b. Vigorously scrub the leg. c. Carefully pick material off the leg. d. Apply powder to absorb the material. 16. What is an appropriate nursing intervention when caring for a child in traction? a. Removing adhesive traction straps daily to prevent skin breakdown b. Assessing for tightness, weakness, or contractures in uninvolved joints and muscles c. Providing active range of motion exercises to affected extremity three times a day d. Keeping child prone to maintain good alignment 17. The nurse is caring for a hospitalized adolescent whose femur was fractured 18 hours ago. The adolescent suddenly develops chest pain and dyspnea. The nurse should suspect what complication? a. Sepsis b. Osteomyelitis c. Pulmonary embolism d. Acute respiratory tract infection 18. What statement is correct regarding sports injuries during adolescence? a. Conditioning does not help prevent many sports injuries. b. The increase in strength and vigor during adolescence helps prevent injuries related to fatigue. c. More injuries occur during organized athletic competition than during recreational sports participation. d. Adolescents may not possess insight and judgment to recognize when a sports activity is beyond their capabilities. 19. The middle school nurse is speaking to parents about prevention of injuries as a goal of the physical education program. How should the goal be achieved? a. Use of protective equipment at the familys discretion b. Education of adults to recognize signs that indicate a risk for injury c. Sports medicine program to help student athletes work through overuse injuries d. Arrangements for multiple sports to use same athletic fields to accommodate more children 20. A young girl has just injured her ankle at school. In addition to notifying the childs parents, what is the most appropriate, immediate action by the school nurse? a. Apply ice. b. Observe for edema and discoloration. c. Encourage child to assume a position of comfort. d. Obtain parental permission for administration of acetaminophen or aspirin. 21. A student athlete was injured during a basketball game. The nurse observes significant swelling. The player states he thought he heard a pop, that the pain is pretty bad, and that the ankle feels as if it is coming apart. Based on this description, the nurse suspects what injury? a. Sprain b. Fracture c. Dislocation d. Stress fracture 22. An adolescent comes to the school nurse after experiencing shin splints during a track meet. What reassurance should the nurse offer? a. Shin splints are expected in runners. b. Ice, rest, and nonsteroidal antiinflammatory drugs (NSAIDs) usually relieve pain. c. It is generally best to run around and work the pain out. d. Moist heat and acetaminophen are indicated for this type of injury. 7. A 4-year-old child is placed in Buck extension traction for Legg-Calv-Perthes disease. He is crying with pain as the nurse assesses the skin of his right foot and sees that it is pale with an absence of pulse. What should the nurse do first? a. Reposition the child and notify the practitioner. b. Notify the practitioner of the changes noted. c. Give the child medication to relieve the pain. d. Chart the observations and check the extremity again in 15 minutes. 39. The nurse is teaching the parent of a 4-year-old child with a cast on the arm about care at home. What statement by the parent indicates a correct understanding of the teaching? a. I should have the affected limb hang in a dependent position. b. I will use an ice pack to relieve the itching. c. I should avoid keeping the injured arm elevated. d. I will expect the fingers to be swollen for the next 3 days. SCOLIOSIS 28. What term is used to describe an abnormally increased convex angulation in the curvature of the thoracic spine? a. Scoliosis b. Lordosis c. Kyphosis d. Ankylosis 29. When does idiopathic scoliosis become most noticeable? a. In the newborn period b. When the child starts to walk c. During the preadolescent growth spurt d. During adolescence 30. A preadolescent has been diagnosed with scoliosis. The planned therapy is the use of a thoracolumbosacral orthotic. The preadolescent asks how long she will have to wear the brace. What is the appropriate response by the nurse? a. For as long as you have been told. b. Most preadolescents use the brace for 6 months. c. Until your vertebral column has reached skeletal maturity. d. It will be necessary to wear the brace for the rest of your life. 31. A 17-year-old patient is returning to the surgical unit after Luque instrumentation for scoliosis repair. In addition to the usual postoperative care, what additional intervention will be needed? a. Position changes are made by log rolling. b. Assistance is needed to use the bathroom. c. The head of the bed is elevated to minimize spinal headache. d. Passive range of motion is instituted to prevent neurologic injury. DEVELOPMENTAL DYSPLASIA OF THE HIP 40. The nurse is teaching the parents of a 1-month-old infant with developmental dysplasia of the hip about preventing skin breakdown under the Pavlik harness. What statement by the parent would indicate a correct understanding of the teaching? a. I should gently massage the skin under the straps once a day to stimulate circulation. b. I will apply a lotion for sensitive skin under the straps after my baby has been given a bath to prevent skin irritation. c. I should remove the harness several times a day to prevent contractures. d. I will place the diaper over the harness, preferably using a superabsorbent disposable diaper that is relatively thin. CLUBFOOT 41. A neonate is born with mild clubfeet. When the parents ask the nurse how this will be corrected, what should the nurse explain? a. Traction is tried first. b. Surgical intervention is needed. c. Frequent, serial casting is tried first. d. Children outgrow this condition when they learn to walk. 42. An infant is born with one lower limb deficiency. When is the optimum time for the child to be fitted with a functional prosthetic device? a. As soon as possible after birth b. When the infant is developmentally ready to stand up c. At about ages 12 to 15 months, when most children are walking d. At about 4 years, when the healthy limb is not growing so rapidly 43. The nurse knows that parents need further teaching with regard to the treatment of congenital clubfoot when they state what? a. Well keep the cast dry. b. Were happy this is the only cast our baby will need. c. Well watch for any swelling of the foot while the cast is on. d. Were getting a special car seat to accommodate the cast. JUVENILE IDIOPATHIC ARTHRITIS 35. What is a major goal for the therapeutic management of juvenile idiopathic arthritis (JIA)? a. Control pain and preserve joint function. b. Minimize use of joint and achieve cure. c. Prevent skin breakdown and relieve symptoms. d. Reduce joint discomfort and regain proper alignment. 7. The nurse is caring for a 14-year-old child with juvenile idiopathic arthritis (JIA). What clinical manifestations should the nurse expect to observe? (Select all that apply.) a. Erythema over joints b. Soft tissue contractures c. Swelling in multiple joints d. Morning stiffness of the joints e. Loss of motion in the affected joints 36. A child with juvenile idiopathic arthritis (JIA) is started on a nonsteroidal antiinflammatory drug (NSAID). What nursing consideration should be included? a. Monitor heart rate. b. Administer NSAIDs between meals. c. Check for abdominal pain and bloody stools. d. Expect inflammation to be gone in 3 or 4 days. 37. What is an important nursing consideration when caring for a child with juvenile idiopathic arthritis (JIA)? a. Apply ice packs to relieve acute swelling and pain. b. Administer acetaminophen to reduce inflammation. c. Teach the child and family correct administration of medications. d. Encourage range of motion exercises during periods of inflammation. SYSTEMIC LUPUS ERTHEMATOSUS 38. What needs to be included as essential teaching for adolescents with systemic lupus erythematosus (SLE)? a. High calorie diet because of increased metabolic needs b. Home schooling to decrease the risk of infections c. Protection from sun and fluorescent lights to minimize rash d. Intensive exercise regimen to build up muscle strength and endurance 1. In teaching a 16-year-old adolescent who was recently diagnosed with systemic lupus erythematosus (SLE), what statements should the nurse include? (Select all that apply.) a. You should use a moisturizer with a sun protection factor (SPF) of 30. b. You should avoid pregnancy because this can cause a flare-up. c. You should not receive any immunizations in the future. d. You may need to be on a low-protein, high-carbohydrate diet. e. You should expect to lose weight while taking steroids. f. You may need to modify your daily recreational activities. 6. The nurse is caring for a 14-year-old child with systemic lupus erythematous (SLE). What clinical manifestations should the nurse expect to observe? (Select all that apply.) a. Arthralgia b. Weight gain c. Polycythemia d. Abdominal pain e. Glomerulonephritis CH 35 CEREBRAL PALSY 1. What is the most common cause of cerebral palsy (CP)? a. Central nervous system (CNS) diseases b. Birth asphyxia c. Cerebral trauma d. Neonatal encephalopathy 2. Spastic cerebral palsy (CP) is characterized by which clinical manifestations? a. Athetosis, dystonic movements b. Tremors, lack of active movement c. Hypertonicity; poor control of posture, balance, and coordinated motion d. Wide-based gait; poor performance of rapid, repetitive movements 3. What type of cerebral palsy (CP) is the most common type? a. Ataxic b. Spastic c. Dyskinetic d. Mixed type 4. The parents of an infant with cerebral palsy (CP) ask the nurse if their child will have cognitive impairment. The nurses response should be based on which knowledge? a. Affected children have some degree of cognitive impairment. b. Around 20% of affected children have normal intelligence. c. About 45% of affected children have normal intelligence. d. Cognitive impairment is expected if motor and sensory deficits are severe. 5. Gingivitis is a common problem in children with cerebral palsy (CP). What preventive measure should be included in the plan of care? a. High-carbohydrate diet b. Meticulous dental hygiene c. Minimum use of fluoride d. Avoidance of medications that contribute to gingivitis 6. What is a major goal of therapy for children with cerebral palsy (CP)? a. Cure the underlying defect causing the disorder. b. Reverse the degenerative processes that have occurred. c. Prevent the spread to individuals in close contact with the child. d. Recognize the disorder early and promote optimum development. 7. The parents of a child with spastic cerebral palsy (CP) state that their child seems to have significant pain. In addition to systemic pharmacologic management, the nurse includes which teaching? a. Patterning b. Positions to reduce spasticity c. Stretching exercises after meals d. Topical analgesics for muscle spasms 8. A child, age 3 years, has cerebral palsy (CP) and is hospitalized for orthopedic surgery. His mother says he has difficulty swallowing and cannot hold a utensil to feed himself. He is slightly underweight for his height. What is the most appropriate nursing action related to feeding this child? a. Bottle or tube feed him a specialized formula until he gains sufficient weight. b. Stabilize his jaw with caregivers hand (either from a front or side position) to facilitate swallowing. c. Place him in a well-supported, semireclining position. d. Place him in a sitting position with his neck hyperextended to make use of gravity flow. 9. An 8-year-old girl with moderate cerebral palsy (CP) recently began joining a regular classroom for part of the day. Her mother asks the school nurse about joining the after-school Girl Scout troop. The nurses response should be based on which knowledge? a. Most activities such as Girl Scouts cannot be adapted for children with CP. b. After-school activities usually result in extreme fatigue for children with CP. c. Trying to participate in activities such as Girl Scouts leads to lowered self-esteem in children with CP. d. Recreational activities often provide children with CP with opportunities for socialization and recreation. 21. The nurse is preparing a staff education in-service session for a group of new graduate nurses who will be working in a long-term care facility for children; many of the children have cerebral palsy (CP). What statement should the nurse include in the training? a. Children with dyskinetic CP have a wide-based gait and repetitive movements. b. Children with spastic pyramidal CP have a positive Babinski sign and ankle clonus. c. Children with hemiplegia CP have mouth muscles and one lower limb affected. d. Children with ataxic CP have involvement of pharyngeal and oral muscles with dysarthria. 22. The nurse should suspect a child has cerebral palsy (CP) if the parent says what? a. My 6-month-old baby is rolling from back to prone now. b. My 4-month-old doesnt lift his head when on his tummy. c. My 8-month-old can sit without support. d. My 10-month-old is not walking. 23. The nurse is caring for a 4-year-old child with cerebral palsy (CP). The child, developmentally, is at an infant stage. Appropriate developmental stimulation for this child should be what? a. Playing pat-a-cake with the child b. None so the child does not become overstimulated c. Putting a colorful mobile with music on the bed d. Giving the child a coloring book and crayons 36. What is the rationale for orthopedic surgery for a child with cerebral palsy? a. To cure spasticity b. To improve function c. For cosmetic purposes d. To prevent the need of physical therapy 37. A feeding technique the nurse can teach to parents of a child with cerebral palsy to improve use of the lips and the tongue to facilitate speech is which? a. Feeding pureed foods b. Placing food on the tongue c. Placing food at the side of the tongue d. Placing food directly into the mouth with a spoon 38. The nurse is teaching the family of an infant with cerebral palsy how to administer a diazepam (Valium) pill by gastrostomy tube. What should the nurse include in the teaching session? a. The pill should be crushed and mixed with a small amount of water. b. The pill should be crushed and mixed with the infants formula. c. After administering the medication, flush the tube with air. d. Before administering the medication, check the placement of the tube. 2. The nurse is teaching the family with a child with cerebral palsy (CP) strategies to prevent constipation. What should the nurse include in the teaching session? (Select all that apply.) a. Increase fluid intake. b. Increase fiber in the diet. c. Administer stool softeners daily as prescribed. d. Increase the amount of dairy products in the diet. e. Allow the child to decide when to try to have a bowel movement. 5. The nurse is preparing to admit a 7-year-old child with ataxic cerebral palsy. What clinical manifestations of ataxic cerebral palsy should the nurse expect to observe? (Select all that apply.) a. Wide-based gait b. Rapid, repetitive movements performed poorly c. Slow, twisting movements of the trunk or extremities d. Hypertonicity with poor control of posture, balance, and coordinated motion e. Disintegration of movements of the upper extremities when the child reaches for objects 6. What are some of the associated disabilities seen with cerebral palsy? (Select all that apply.) a. Visual impairment b. Hearing impairment c. Speech difficulties d. Intellectual impairment e. Associated heart defects MYELOMENINGOCELE 7. The nurse is preparing to admit a 5-year-old with spina bifida cystica that was below the second lumbar vertebra. What clinical manifestations of spina bifida cystica below the second lumbar vertebra should the nurse expect to observe? (Select all that apply.) a. No motor impairment b. Lack of bowel control c. Soft, subcutaneous lipomas d. Flaccid, partial paralysis of lower extremities e. Overflow incontinence with constant dribbling of urine 8. The nurse is preparing to admit a 2-year-old child with spina bifida occulta. What clinical manifestations of spina bifida occulta should the nurse expect to observe? (Select all that apply.) a. Dark tufts of hair b. Skin depression or dimple c. Port-wine angiomatous nevi d. Soft, subcutaneous lipomas e. Bladder and sphincter paralysis 26. What refers to a hernial protrusion of a saclike cyst of meninges, spinal fluid, and a portion of the spinal cord with its nerves through a defect in the vertebral column? a. Rachischisis b. Meningocele c. Encephalocele d. Myelomeningocele 27. A woman who is 6 weeks pregnant tells the nurse that she is worried that, even though she is taking folic acid supplements, the baby might have spina bifida because of a family history. The nurses response should be based on what? a. Prenatal detection is not possible yet. b. There is no genetic basis for the defect. c. Chromosome studies done on amniotic fluid can diagnose the defect prenatally. d. Open neural tube defects (NTDs) result in elevated concentrations of a-fetoprotein in amniotic fluid. 28. The most important nursing intervention when caring for an infant with myelomeningocele in the preoperative stage is which? a. Take vital signs every hour. b. Place the infant on the side to decrease pressure on the spinal sac. c. Watch for signs that might indicate developing hydrocephalus. d. Apply a heat lamp to facilitate drying and toughening of the sac. 29. Neuropathic bladder disorders are common among children with which disorder? a. Plagiocephaly b. Meningocele c. Craniosynostosis d. Myelomeningocele 30. What most accurately describes bowel function in children born with a myelomeningocele? a. Incontinence cannot be prevented. b. Enemas and laxatives are contraindicated. c. Some degree of fecal continence can usually be achieved. d. Colostomy is usually required by the time the child reaches adolescence. 31. The nurse is caring for a neonate born with a myelomeningocele. Surgery to repair the defect is scheduled the next day. What is the most appropriate way to position and feed this neonate? a. Prone with the head turned to the side b. On the side c. Supine in an infant carrier d. Supine, with defect supported with rolled blankets 32. A goal for children with spina bifida is to reduce the chance of allergy development. What is a priority nursing intervention? a. Recommend allergy testing. b. Provide a latex-free environment. c. Use only powder-free latex gloves. d. Limit use of latex products as much as possible. DUCHENNE MUSCULAR DYSTROPHY 20. What statement best describes Duchenne (pseudohypertrophic) muscular dystrophy (DMD)? a. It has an autosomal dominant inheritance pattern. b. Onset occurs in later childhood and adolescence. c. It is characterized by presence of Gower sign, a waddling gait, and lordosis. d. Disease stabilizes during adolescence, allowing for life expectancy to approximately age 40 years. 11. The nurse is preparing to admit a 10-year-old child with Duchenne muscular dystrophy. What clinical features of Duchenne muscular dystrophy should the nurse recognize? (Select all that apply.) a. Calf muscle hypertrophy b. Late onset, usually between 6 and 8 years of age c. Progressive muscular weakness, wasting, and contractures d. Loss of independent ambulation by 9 to 12 years of age e. Slowly progressive, generalized weakness during adolescence [Show More]
Last updated: 3 years ago
Preview 1 out of 171 pages
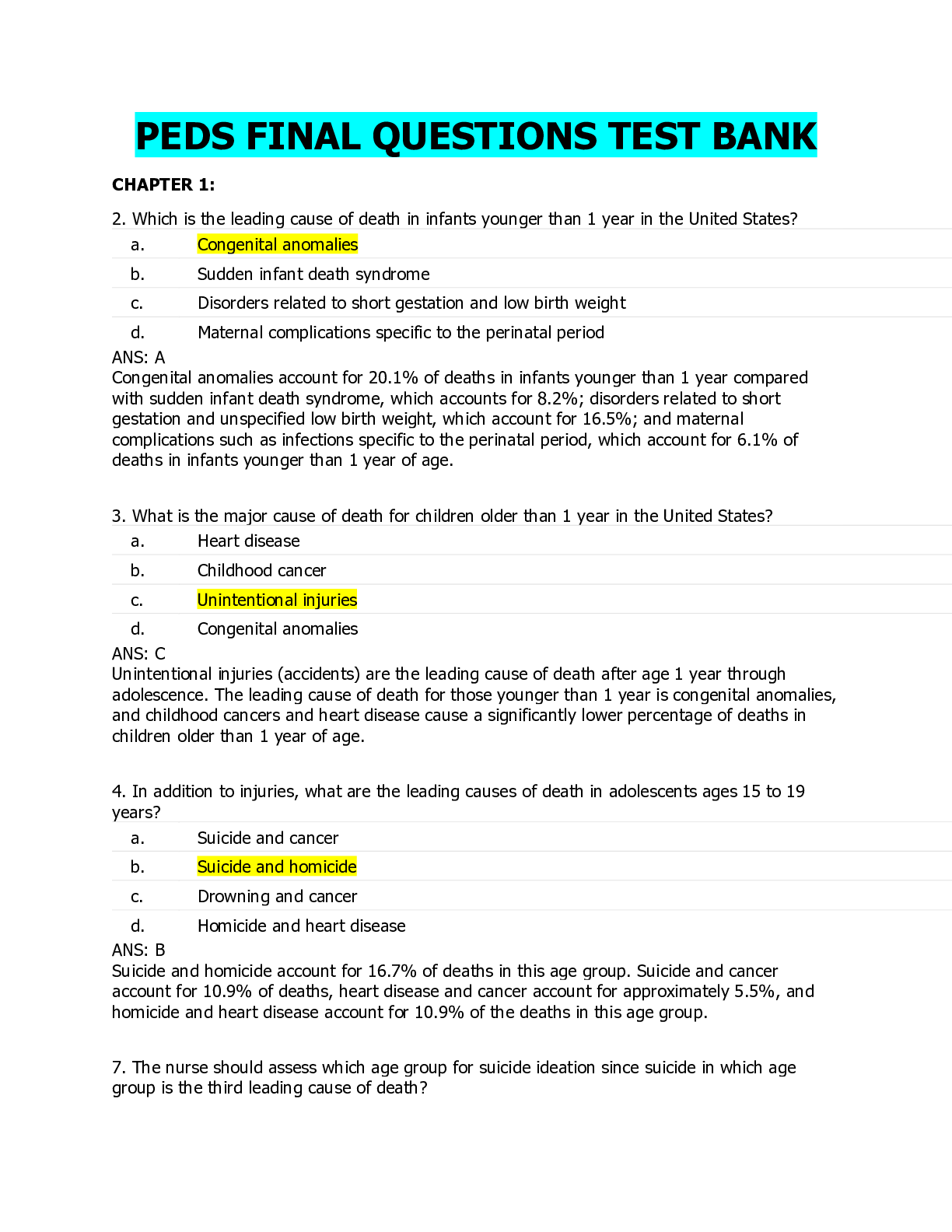
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$20.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Apr 17, 2020
Number of pages
171
Written in
All
Additional information
This document has been written for:
Uploaded
Apr 17, 2020
Downloads
0
Views
174