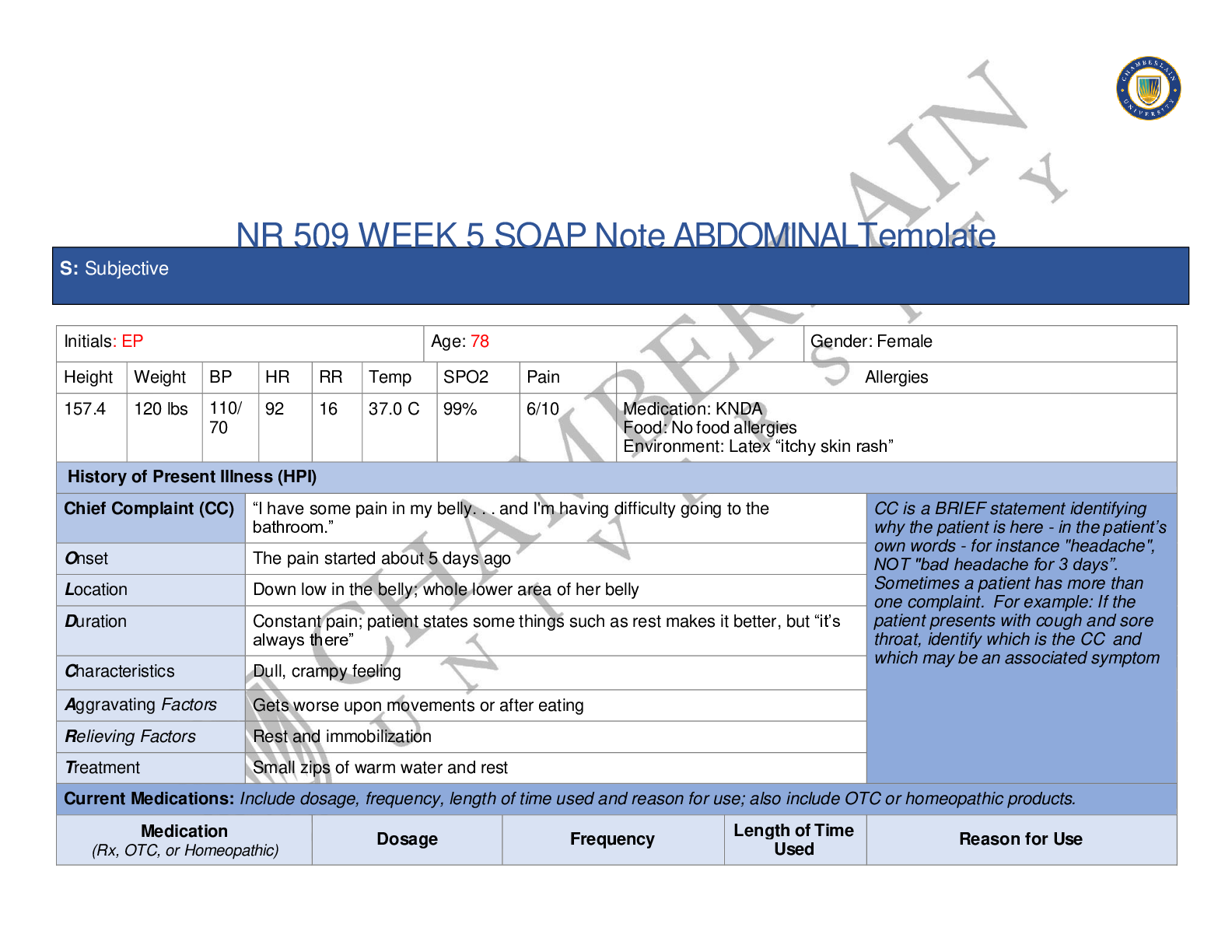
NR 509 WEEK 5 SOAP Note ABDOMINALTemplate
Initials: EP Age: 78 Gender: Female
Height Weight BP HR RR Temp SPO2 Pain Allergies
157.4 120 lbs 110/
70 92 16 37.0 C 99% 6/10 Medication: KNDA Food: No food allergies
...
NR 509 WEEK 5 SOAP Note ABDOMINALTemplate
Initials: EP Age: 78 Gender: Female
Height Weight BP HR RR Temp SPO2 Pain Allergies
157.4 120 lbs 110/
70 92 16 37.0 C 99% 6/10 Medication: KNDA Food: No food allergies
Environment: Latex “itchy skin rash”
History of Present Illness (HPI)
Chief Complaint (CC) “I have some pain in my belly. . . and I'm having difficulty going to the bathroom.” CC is a BRIEF statement identifying why the patient is here - in the patient’s own words - for instance "headache", NOT "bad headache for 3 days”.
Sometimes a patient has more than one complaint. For example: If the patient presents with cough and sore throat, identify which is the CC and which may be an associated symptom
Onset The pain started about 5 days ago
Location Down low in the belly; whole lower area of her belly
Duration Constant pain; patient states some things such as rest makes it better, but “it’s always there”
Characteristics Dull, crampy feeling
Aggravating Factors Gets worse upon movements or after eating
Relieving Factors Rest and immobilization
Treatment Small zips of warm water and rest
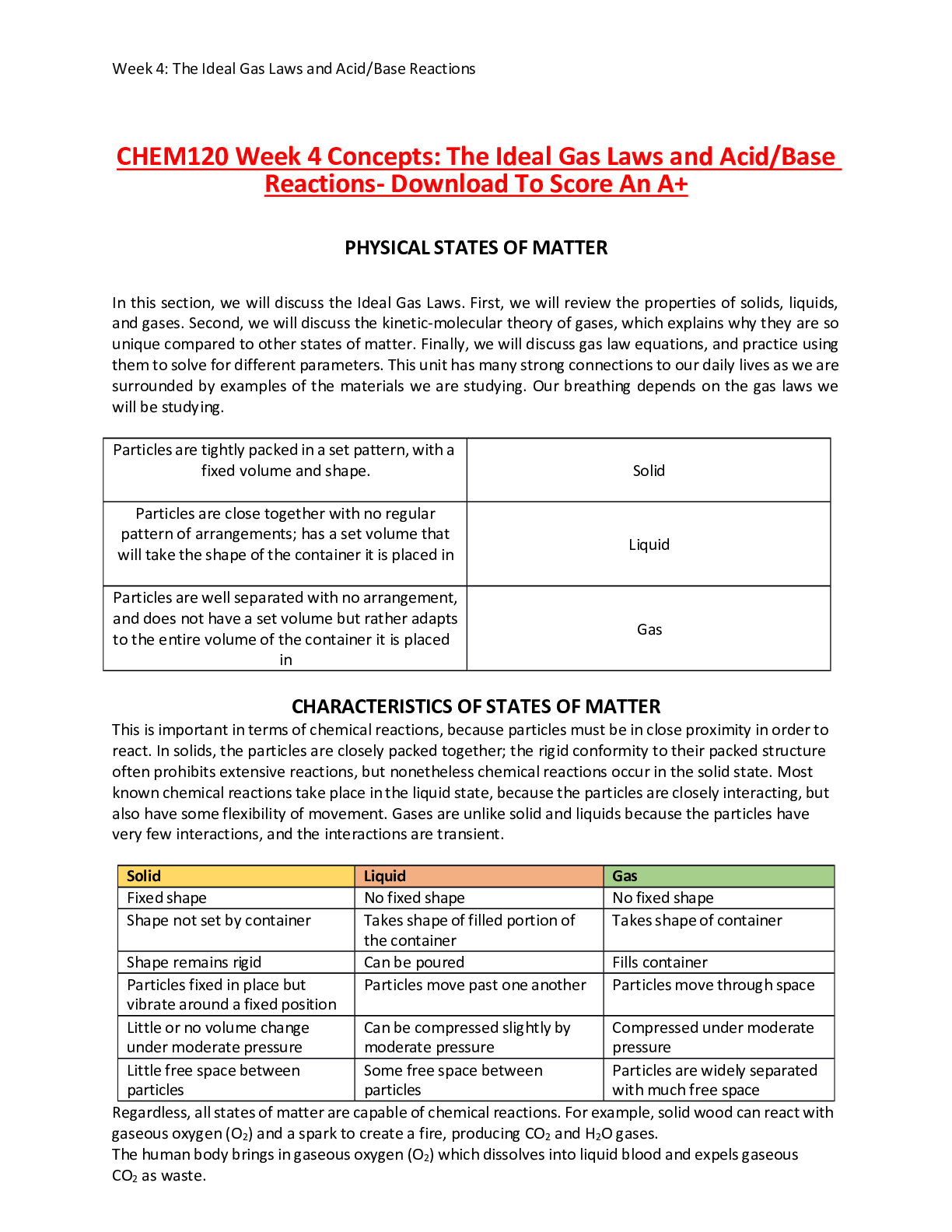
Current Medications: Include dosage, frequency, length of time used and reason for use; also include OTC or homeopathic products.
Medication
(Rx, OTC, or Homeopathic) Dosage Frequency Length of Time Used Reason for Use
Accupril 10 mg Daily; every day in the morning at 8am, after breakfast Unknown High blood pressure
Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text.
Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text.
Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text.
Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text.
Past Medical History (PMHx) – Includes but not limited to immunization status (note date of last tetanus for all adults), past major illnesses, hospitalizations, and surgeries. Depending on the CC, more info may be needed.
Mrs. EP is a 78 years old Korean female. She present to the clinic with a HX significant for,
1. Hypertension diagnosed at age 54
2. Gallstones
3. Immunizations up to date; has not had flu shot this year
4. Cholecystectomy at age 42
5. C-section (early 40’s)
6. Gravida: 3 Para: 3
7. She is unsure of date of last Tetanus
8. Colonoscopy about 10 year ago
9. Pap smear about 10 years ago
10. Mammogram about 5 years ago
11. Denies history of GERD disease
12. Denies any dietary supplements, herbal supplements, and vitamin intake
Social History (Soc Hx) - Includes but not limited to occupation and major hobbies, family status, tobacco and alcohol use, and any other pertinent data. Include health promotion such as use seat belts all the time or working smoke detectors in the house.
Mrs. EP is a 78 year old Korean female that lives with her daughter, Jennifer. Reports having a wonderful relationship with her. Mrs. EP reported to be married for nearly 50 years. Her husband, Shin, passed away 6 years ago. She now states to have a gentleman friend, Max. They’ve been together for almost a year. Denies to be sexually active. Patient states that “we have oral sex, but no intercourse.” Patient reports to exercise regularly. She keeps active by gardening, and walking. Patient takes exercise classes at a community center. At the community center she does water aerobics, and has recently started enjoying Pilates as well. Patient denies the use of any illicit drug, and smoking. Patient drinks one glass of dry white wine once a week, on Sundays.
Review of Systems (ROS): Address all body systems that may help rule in or out a differential diagnosis Check the box next to each positive symptom and provide additional details.
Constitutional Skin HEENT
☐ Fatigue: Pt denies
☐ Weakness: Pt denies
☐ Fever/Chills: PT denies
☐ Weight Gain: Pt denies
☐ Weight Loss: Pt denies
☐ Trouble Sleeping: Pt denies
☐ Night Sweat: Pt denies
☒Other:
Low energy; Pt states feeling that she needs to rest more frequently ☐ Itching Click or tap here to enter text.
☐ Rashes Click or tap
here to enter text.
☐ Nail Changes Click or tap here to enter text.
☐ Skin Color Changes
Click or tap here to enter text.
☐ Other:
Click or tap here to enter text. ☐ Diplopia Click or tap here to enter text.
☐ Eye Pain Click or tap
here to enter text.
☐ Eye redness Click or tap here to enter text.
☐ Vision changes Click or
tap here to enter text.
☐ Photophobia Click or tap here to enter text.
☐ Eye discharge Click or
tap here to enter text. ☐ Earache Click or tap here to enter text.
☐ Tinnitus Click or tap here
to enter text.
☐ Epistaxis Click or tap here to enter text.
☐ Vertigo Click or tap here
to enter text.
☐ Hearing Changes Click or tap here to enter text. ☐ Hoarseness Click or tap here to enter text.
☐ Oral Ulcers Click or tap here
to enter text.
☐ Sore Throat Click or tap here to enter text.
☐ Congestion Click or tap here
to enter text.
☐ Rhinorrhea Click or tap here to enter text.
☐ Other:
Click or tap here to enter text.
Respiratory Neuro Cardiovascular
☐ Cough: Pt denies
☐ Hemoptysis: Pt denies
☐ Dyspnea: Pt denies
☐ Wheezing: Pt denies
☐ Pain on Inspiration: Pt denies
☐ Sputum Production: Pt denies
☐ Other: Click or tap here to enter text. ☐ Syncope or Lightheadedness Click or tap here to enter text.
☐ Headache Click or tap here
to enter text.
☐ Numbness Click or tap here to enter text.
☐ Tingling Click or tap here to
enter text.
☐ Sensation Changes Choose an item.
☐ Speech Deficits Click or tap
here to enter text.
☐ Other: Click or tap here to enter text. ☐ Chest pain: Pt denies
☐ SOB: Pt denies
☒Exercise: Pt states intolerance to physical activities
☐ Orthopnea: Pt denies
☐ Edema: Pt denies
☐ Murmurs: None detected upon auscultation ☐ Palpitation: Pt denies
☐ Faintness: Pt denies
☐ OC Changes: No changes
☐ Claudications: No Claudication upon Inspection
☐ PND: Pt denies
☐ Other: Click or tap here to enter text.
MSK GI GU PSYCH
☐ Pain Click or tap here to enter text.
☐ Stiffness Click or tap here to enter
text.
☐ Crepitus Click or tap here to enter text.
☐ Swelling Click or tap here to enter
text.
☐ Limited ROM Choose an item.
☐ Redness Click or tap here to enter text.
☐ Misalignment Click or tap here to
enter text.
☐ Other: Click or tap here to enter text. ☐ Nausea/Vomiting: Pt denies
☐ Dysphasi: Pt denies
☐ Diarrhea: Pt reported having diarrhea a few days ago, watery and lose
☒Appetite Change: Pt reported change
in appetite and being unable to eat for 5 days.
☐ Heartburn: Pt denies
☐ Blood in Stool: Pt denies
☒Abdominal Pain: Discomfort, pain, Pt reports dull, cramps feeling
☐ Excessive Flatus: Pt reports being a
bit gassy
☐ Food Intolerance: Pt reports that it has been hard to eat.
☐ Rectal Bleeding: Pt denies
☒Other: Pt reports that for several days Its been hard to use the bathroom.
Excessive strain to have a bowel movement, and she can't make it happen. And the pain is there in her stomach. Pt reports feeling bloated. ☐ Urgency: Pt denies
☐ Dysuria: Pt denies
☐ Burning: Pt denies
☐ Hematuria: Pt denies
☐ Polyuria: Pt denies
☐ Nocturia: Pt denies
☐ Incontinence: Pt denies
☒Other: Pt reports less urination; dark urine Stress Being here,
☐ Anxiety Click or tap here to enter text.
☐ Depression Click or tap here
to enter text.
☐ Suicidal/Homicidal Ideation Click or tap here to enter text.
☐ Memory Deficits Click or tap
here to enter text.
☐ Mood Changes Click or tap here to enter text.
☐ Trouble Concentrating Click
or tap here to enter text.
☐ Other: A little bit forgetful
GYN
☐ Rash: Pt denies
☐ Discharge: Pt denies
☐ Itching: Pt denies ☐ Irregular Menses: PT denies
☐ Dysmenorrhea: Pt Denies
☐ Foul Odor: Pt denies ☐ Amenorrhea: Pt denies
☒LMP: 20 years ago, at age 54
☐ Contraception: Pt denies
☐ Other:Click or tap here to enter text.
Body System Positive Findings Negative Findings
General
Choose an item.
Mrs. Parker is a 78-year old female that appears her stated age. She is well groomed, neat appearance, with appropriate speech, and makes good eye contact. She is alert and oriented to her surroundings.There are no obvious signs or symptoms of distress noted. BP 110/70, HR 92, Resp 16, O2 sat 99%
Skin
Choose an item.
Slightly flushed cheeks
Skin is warm and dry, skin is wrinkled as expected for Mrs. Park age, no tenting is noted, skin is warm, dry, and intact.
HEENT
Choose an item.
Click or tap here to enter text.
Head and scalp symmetrical; symmetrical facial features; nasal septum moist and pink; oral mucosa moist and pink, ear canal were not inspected but looked symmetric bilaterally.
Respiratory
Choose an item.
Lungs where clear to auscultation, breath sounds in all areas. No adventitious lung sounds identified.
Neuro
Unable to Assess
Click or tap here to enter text. Pt appeared alert and oriented, able to follow commands.
Cardiovascular
Choose an item.
Click or tap here to enter text.
Chest was symmetric with no visible abnormal findings. Heart sounds were auscultated with belt and diaphragm of stethoscope.
S1 and S2 identified to all pericardial areas; no extra sounds heard;
S3 and S4 no audible;
No bruit to abdominal aorta identified, palpated at 2cm, no lateral pulsation;
No bruits identified to renal, illeac, and femoral arteries bilaterally
Musculoskeletal
Choose an item.
Click or tap here to enter text.
No edema noted to lower extremities
Gastrointestinal
Choose an item.
Dullness was noted over LLQ with percussion;
Patient rested to pain over LLQ with light and deep palpation with distention noted as well as firm oblong mass 2cmx4cm to the LLQ;
Pain evidenced by guarding
Symmetrical abdomen, flat contour, and no visible abnormalities like bruses, rashes, distention, or any changes in color;
1st horizontal scar noted in right upper abdomen just below right coastal margin, 2Nd horizontal scar noted approximately 1cm above pubic area;
No bruit heard over abdominal aorta, aortic width is 2 cm with no lateral pulsations;
Normoactive bowel sounds to all quadrants; No bruits identified to abdominal arteries; Tympanic spleen, no palpable spleen;
Liver spam 7 cm in the mid-clavicular line, palpable liver at 1 cm below the right costal margin;
No CVA tenderness; No palpable bladder,
No abdominal distention or tenderness; no masses, tenderness, and guarding to RLQ,RUQ, and LUQ Right or left kidney not palpable
Genitourinary
Click or tap here to enter text. Bladder not palpable, no distention or tenderness noted Kidneys not palpable, no CV tenderness
Urine clear, dar yellow and normal odor, PH 6.5-6.9 No additional substances detected on urinalysis
Psychiatric
Unable to Assess
Click or tap here to enter text.
Click or tap here to enter text.
Gynecological
Choose an item.
Click or tap here to enter text.
Pelvic exam performed no inflammation of the vulva, abnormal discharge, or bleeding, no masses, growths, or tenderness upon palpation; no hemorrhoids, fissures, or ulceration; strong sphincter tone, fecal mass detected in the rectal vault
Problem List
1. Abdominla pain 6 Click or tap here to enter text. 11 Click or tap here to enter text.
2 Constipation 7 Click or tap here to enter text. 12 Click or tap here to enter text.
3 Low energy levels 8 Click or tap here to enter text. 13 Click or tap here to enter text.
4 Appetite changes 9 Click or tap here to enter text. 14 Click or tap here to enter text.
5 Click or tap here to enter text. 10 Click or tap here to enter text. 15 Click or tap here to enter text.
A: Assessment
Medical Diagnoses. Provide 3 differential diagnoses which may provide an etiology for the CC. The first diagnosis (presumptive diagnosis) is the diagnosis with the highest priority. Provide the ICD-10 code and pertinent findings to support each diagnosis.
Diagnosis ICD-10 Code Pertinent Findings
Acute Constipation due to possible fecal impaction K59.00 Hard stool palpated on rectal vault while performing a digital rectal exam. Mass detected with deep palpation at a depth of 5-8cm. Difficulty going to the bathroom for 5 days as stated by the patient.
Obstruction of the colon/Bowel Obstruction K56.60 Left lower quadrant pain and guarding, Hard stool palpated on rectal vault, fecal impaction must be ruled out before treating the patient with laxatives and stool softeners. Patient might be at increased risk for bowel perforation.
Diverticulitis K57.92 Left lower quadrant pain with a palpable mass
P: Plan
Address all 5 parts of the comprehensive treatment plan. If you do not wish to order an intervention for any part of the treatment plan, write “None at this time” but do not leave any heading blank. No intervention is self-evident. Provide a rationale and evidence-based in-text citation for each intervention.
Diagnostics: List tests you will order this visit
Test Rationale/Citation
CBC A complete blood count (CBC) is a group of tests used for basic screening purposes that provides the enumeration of the cellular elements of the blood and the valuable diagnostic information regarding the overall health of the patient and the patient’s response to disease and treatment (Gajewski & Heering, 2018)
Blood cultures Blood cultures are performed to identify and detect aerobic and anaerobic pathogens in the blood in patients with suspected infection (Gajewski & Heering, 2018)
WBC Used as an indicator of immune status, it reflects the type and number of WBC available to rapidly respond to an infection (Van Leeuwen & Bladh, 2015)
Abdominal X-ray Abdominal X-ray is recommended to assess for peritonitis and perforation (March & Schub, 2018)
CT-scan CT scanning appears to be the best overall imaging modality in the diagnosis of possible diverticulitis
(Espinosa, Sharma, Lucerna, & Stranges, 2017)
Medications: List medications/treatments including OTC drugs you will order and “continue previous meds” if pertinent.
Drug Dosage Length of Treatment Rationale/Citation
Metronidazole 500 mg PO every 8 hrs 10-14 days In cases involving perforated bowel or complicated sigmoid diverticulitis, given the significant presence of organisms resistant to our empirical therapy, the judicious use of ceftriaxone and metronidazole is recommended (Tan, Rouse, Kew, Qin, La Paglia, & Toan Pham, 2018)
Fleets Enema 1 enema As a single dose, May repeat x1 Treat initial impaction. Any usage of laxatives and stool softeners are contraindicated until obstruction has been ruled out (Mounsey, Raleigh, & Wilson, 2015)
Magnesium citrate 300 ML As a single dose Magnesium citrate is a laxative used to treat occasional constipation on a short-term basis (AHFS, 2019)
Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text.
Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text.
Referral/Consults:
Gastroenterologist Colonoscopy Dietary consult Rationale/Citation The guidelines for diverticulitis diagnosing and treatment suggest Gastroenterologist referrals in order to standardize the treatment of patients with acute diverticulitis and to provide clinicians who deal with patients with diverticulitis on a daily basis, with an evidence- based medical approach in treating and counseling patients (Andeweg, et al., 2014).
Appropriate, request referral to a dietitian is essential
for diet assessment and patient education about meal planning and making healthy food choices (Schub, & Marcel, 2018)
Educate about the diagnosis of diverticulitis, strategies for
reducing the risk of diverticulitis, the importance of gradually introducing fiber in the diet, and individualized prognosis (Schub, & Marcel, 2018).
Education:
1- Patient should be advised to go to ER if pain suddenly increases, becomes sharp or tearing, or if patient starts vomiting.
2- Increase fiber on diet and fluid intake
3- Antibiotic therapy Rationale/Citation - Educate about the diagnosis of diverticulitis, strategies for reducing the risk of diverticulitis, the importance of gradually introducing fiber in the diet, and
individualized prognosis (Schub, & Marcel, 2018).
- Until xray/CT to diagnose cause of constipation vs obstruction, laxatives including osmotic laxatives are contraindicated (Mounsey, Raleigh, & Wilson, 2015; epocrates.com)
Follow Up: Indicate when patient should return to clinic and provide detailed instructions indicating if the patient should return sooner than scheduled or seek attention elsewhere.
1. Follow up in 5-7 days
2. Patient should return to clinic if her fever does not reduce after 48 hours of antibiotic treatment.
3. Will follow up with patient in regard to lab work during next appt or sooner via telephone for emergencies needs for medication changes due to infection Rationale/Citation Patients treated conservatively for diverticulitis are at high risk for an underlying CRC in the sigmoid colon, also in patients with a CT diagnosis of uncomplicated diverticulitis, hence, a a routine follow-up by a luminal examination of the sigmoid colon in patients above age 70 years is recommended (Grahnat, Hérard, Ackzell, & Andersson, 2016).
References
Include at least one evidence-based peer-reviewed journal article which relates to this case. Use the correct APA 6th edition formatting.
Andeweg, C. S., Mulder, I. M., Felt-Bersma, R. J. F., Verbon, annelies, van der Wilt, G. J., van Goor, H., … Bleichrodt, R. P. (2014). Guidelines of diagnostics and treatment of acute left-sided colonic diverticulitis. Digestive Surgery, 30(4–6), 278. Retrieved from https://search-ebscohost- com.chamberlainuniversity.idm.oclc.org/login.aspx?direct=true&db=edb&AN=94853152&site=eds-live&scope=site
Andrew Tan, Michael Rouse, Natalie Kew, Sharon Qin, Domenic La Paglia, & Toan Pham. (2018). The appropriateness of ceftriaxone and metronidazole as empirical therapy in managing complicated intra-abdominal infection—experience from Western Health, Australia. PeerJ, e5383. https://doi-org.chamberlainuniversity.idm.oclc.org/10.7717/peerj.5383
Espinosa, J., Sharma, R., Lucerna, A., & Stranges, D. (2017). Medical approach to right colon diverticulitis with perforation. Case Reports in Emergency Medicine, 1–3. https://doi-org.chamberlainuniversity.idm.oclc.org/10.1155/2017/2563218
Gajewski, K. R. B., & Heering, H. R. C. (2018). Blood culture: Obtaining. CINAHL Nursing Guide. Retrieved from https://search-ebscohost- com.chamberlainuniversity.idm.oclc.org/login.aspx?direct=true&db=nup&AN=T704043&site=eds-live&scope=site
Grahnat, C. J., Hérard, S., Ackzell, A., & Andersson, R. E. (2016). High probability of an underlying colorectal cancer among patients treated for acute diverticulitis. A Population-Based Cohort Follow-Up Study. World Journal Of Surgery, 40(9), 2283–2288. https://doi- org.chamberlainuniversity.idm.oclc.org/10.1007/s00268-016-3480-7
Magnesium Citrate. (2019). AHFS Consumer Medication Information. Retrieved from https://search-ebscohost- com.chamberlainuniversity.idm.oclc.org/login.aspx?direct=true&db=nup&AN=2013223213&site=eds-live&scope=site
March, P. P., & Schub, T. B. (2018). Diverticulitis: an Overview. CINAHL Nursing Guide. Retrieved from https://search-ebscohost- com.chamberlainuniversity.idm.oclc.org/login.aspx?direct=true&db=nup&AN=T707452&site=eds-live&scope=site
Schub, T. B., & Marcel, C. B. (2018). Diverticulitis: Diet. CINAHL Nursing Guide. Retrieved from https://search-ebscohost- com.chamberlainuniversity.idm.oclc.org/login.aspx?direct=true&db=nup&AN=T708198&site=eds-live&scope=site
Van Leeuwen, A., & Bladh, M. (2015). In Davis’s Comprehensive Handbook of Laboratory & Diagnostic Tests with Nursing Implications, 6th ed (p.
[Show More]