*NURSING > QUESTIONS and ANSWERS > ATI Pediatrics Proctored Exam All Chapter / ATI Peds pediatrics proctored exam (All)
ATI Pediatrics Proctored Exam All Chapter / ATI Peds pediatrics proctored exam
Document Content and Description Below
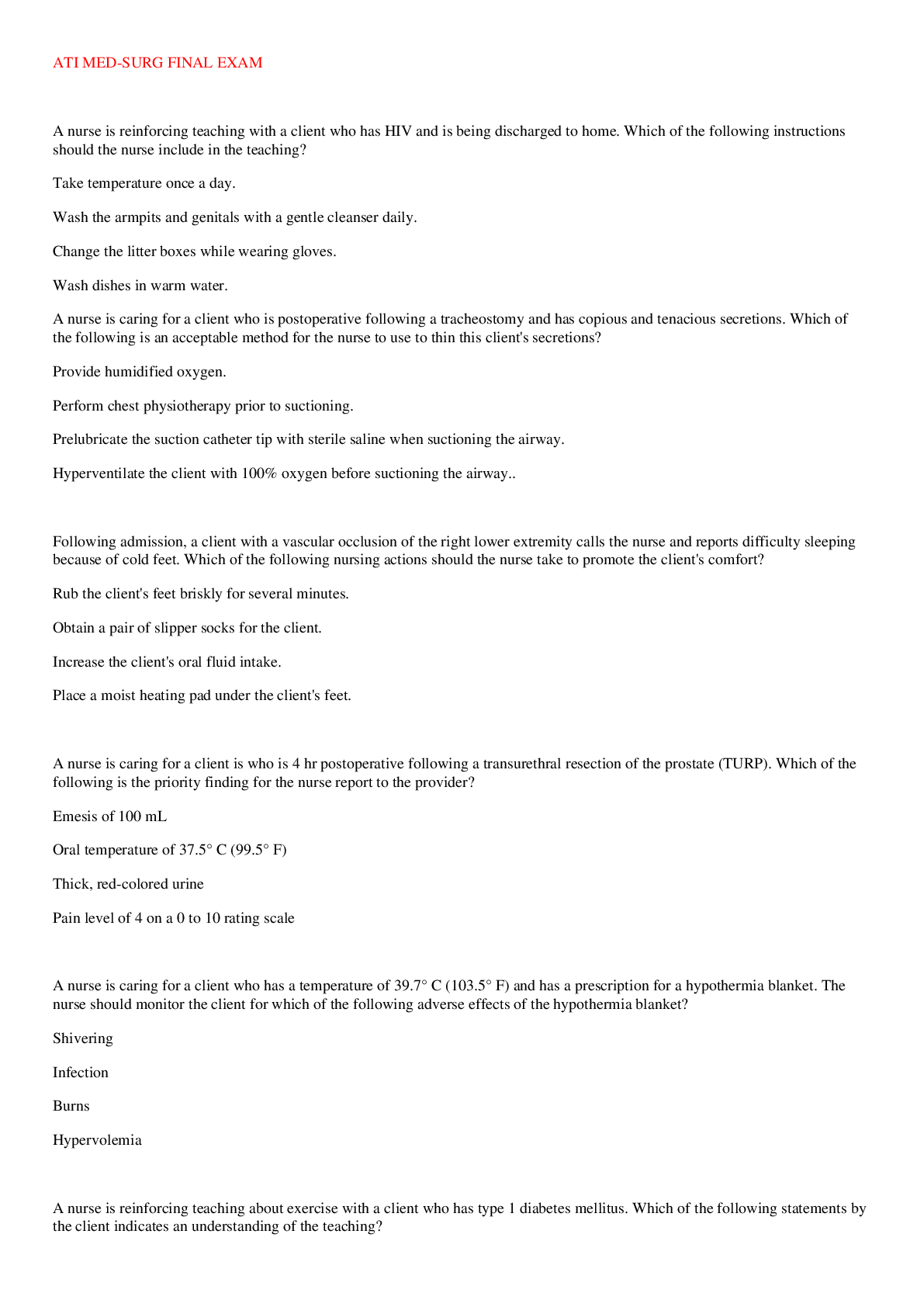
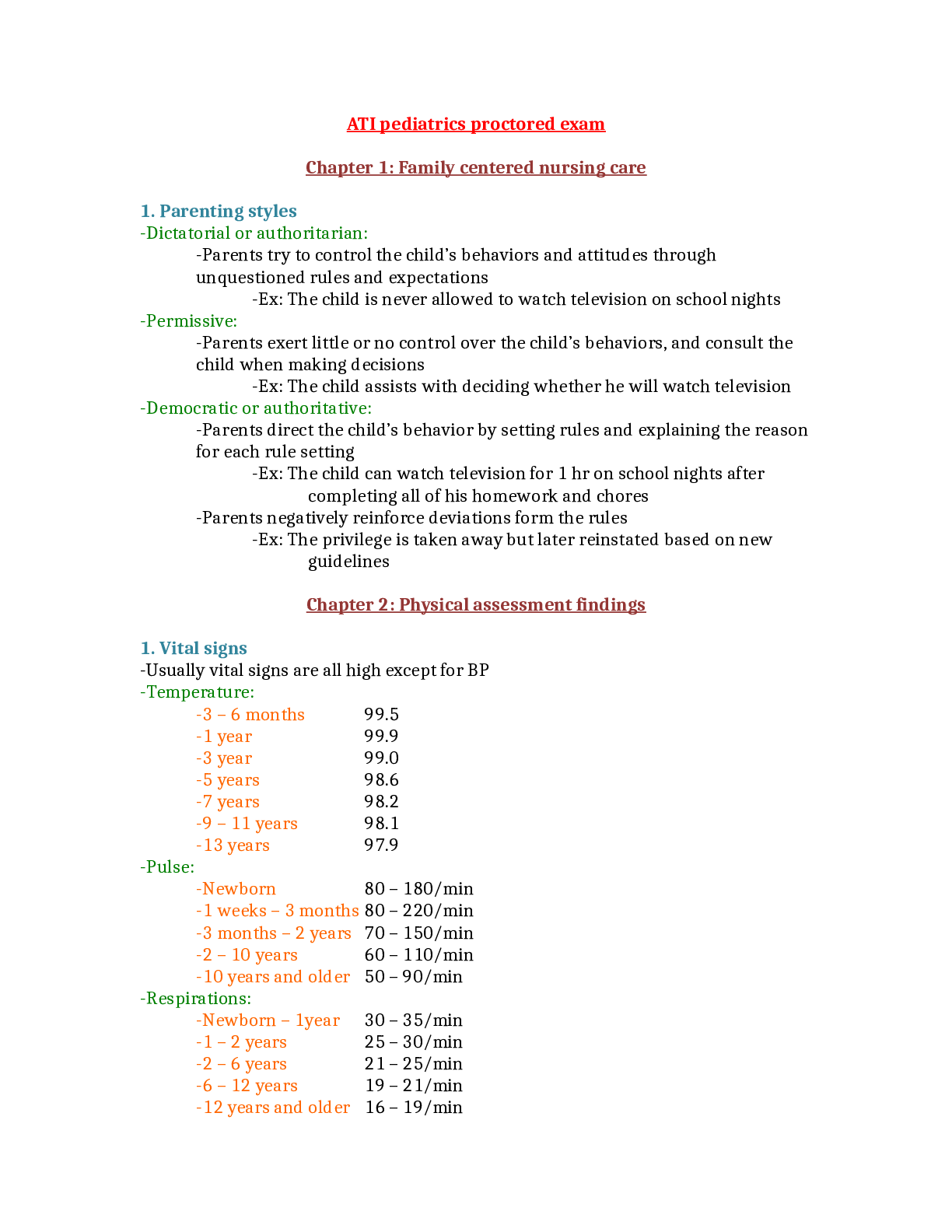
ATI pediatrics proctored exam ATI pediatrics proctored exam Chapter 1: Family centered nursing care 1. Parenting styles -Parents try tocontrolthe child’s behaviors and attitudes through unque... stioned rules and expectations -Ex:the child is never allowed towatch television on school nights -Parents exert little or no control overthe child’s behaviors, and consultthe child when making decisions -Ex:the child assists with deciding whether he will watch television -Parents directthe child’s behavior by setting rules and explainingthe reason for each rule setting -Ex:the child can watch television for 1 hr on school nights after completing all of his homework and chores -Parents negatively reinforce deviations formthe rules -Ex:the privilege is taken away but later reinstated based on new guidelines Chapter 2: Physical assessment findings 1. Vital signs -Usually vital signs are all high except for BP -3 – 6 months 99.5 -1 year 99.9 -3 year 99.0 -5 years 98.6 -7 years 98.2 -9 – 11 years 98.1 -13 years 97.9 -Newborn 80 – 180/min -1 weeks – 3 months 80 – 220/min -3 months – 2 years 70 – 150/min -2 – 10 years 60 – 110/min -10 years and older 50 – 90/min -Newborn – 1year 30 – 35/min -1 – 2 years 25 – 30/min -2 – 6 years 21 – 25/min -6 – 12 years 19 – 21/min -12 years and older 16 – 19/min -Low as a baby but increasesthe older they get -Infants: -Systolic: 65-78 -Diastolic: 41-52 2. Head -Fontanels should be flat -Closes by 6-8 weeks -Closes by 12-18 months 3. Teeth -Infants should have 6-8 teeth by 1 year old -Children and adolescents should have teeth that are white and smooth, and begin replacingthe 20 deciduous teeth with 32 permanent teeth 4. Infant Reflexes Stepping Birth to4 weeks Palmar Grasp Birth to3 months Tonic Neck Reflex (Fencer Position) Birth to3 – 4 months Sucking and Rooting Reflex Birth to4 months Moro Reflex (Fall backward) Birth to4 months Startle Reflex (Loud Noise) Birth to4 months Plantar Reflex Birth to8 months Babinski Reflex Birth to1 year Chapter 3: Health promotion of infants (2 days to1 year) 1. Physical Development -Doubled by 5 months -Tripled by 12 months -Quartered by 30 months -2.5 cm (1 in) per month forthe first 6 months -Increases by 50% by 12 months -First teeth erupt between 6-10 months 2. Motor skill development 1 Month o Head lag o Strong grasp reflex 2 Months o Lifts head when prone o Holds hand in open position | Grasp reflex fades 3 Months o Raises head and shoulders when prone | Slight head lag o No grasp reflex | Keeps hands loosely open 4 Months o Rolls from back toside o Grasp objects with both hands 5 Months o Rolls from front toback o Palmar grasp dominantly 6 Months o Rolls from back tofront o Holds bottle 7 Months o Bears full weight on feet | Sits, leaning forward on both hands o Moves objects from hand tohand 8 Months o Sits unsupported o Pincer grasp 9 Months o Pulls toa standing position | Creeps on hands and knees instead of crawling o Crude pincer grasp | Dominant hand is evident 10 Months o Prone tositting position o Grasps rattle by its handle 11 Months o Walks while holding onto something | Walks with one hand held o Places objects into a container | Neat pincer grasp 12 Months o Stands without support briefly | Sits from standing position without assistance o Tries tobuild a two-block tower w/o success | Can turn pages in a book 3. Cognitive development -Piaget: sensorimotor (birth to24 months) -Object Permanence: objects still exists when it is out of view -Occurs at 9-10 months 4. Language development -3-5 words bythe age of 1 year 5. Psychosocial development -Learn delayed gratification -Trust is developed by meeting comfort, feeding, simulation, and caring needs -Mistrust develops if needs are inadequately or inconsistently met or if needs are continuously met before being vocalized bythe infant 6. Social development -Separation Anxiety: protest when separated from parents -Begins around 4-8 months -Stranger Fear: ability todiscriminate between familiar and unfamiliar people -Begins 6-8 months 7. Age appropriate activities -Rattles -Playing pat-a cake -Brightly colored toys -Playing with blocks 8. Nutrition -Breastfeeding provides a complete diet for infants duringthe first 6 months -Solids are introduced around 4-6 months -Iron-fortified cereal isthe first tobe introduced -New foods should be introduced one at a time, over a 5-7 day period to observe for allergy reactions -Juice and water usually not needed for 1st year -Appropriate finger foods: -Ripe bananas -Toast strips -Graham crackers -Cheese cubes -Noodles -Firmly cooked vegetables -Raw pieces of fruit (except grapes) 9. Injury prevention -Avoid small objects (grapes, coins, and candy) -Handles of pots and pans should be kept turned tothe back ofthe stove -Sunscreen should be used when infants are exposed tothe sun -Infants and toddlers remain in a rear-facing car seat until age 2 -Crib slats should be no farther apart than 6 months -Pillows should be kept out ofthe crib -Infants should be placed on their backs for sleep Chapter 4: Health Promotion of Toddlers (1 to3 years) 1. Physical development -30 months: 4 timesthe birth weight -Toddlers grow 7.5 cm (3 in) per year -Usually equal by 1 to2 years of age 2. Cognitive development -Piaget: sensorimotor stage transitions topreoperational stage 19 – 24 months -Object Permanence: fully developed 3. Language development -1 year: using one-word sentences -2 years: 300 words, multiword sentences by combining 2-3 words 4. Psychosocial Development -Independence is paramount for toddlers who are attempting todo everything for themselves -Use negativism or negative responses toexpress their independence -Ritualism, or maintaining routines and reliability, provides a sense of comfort for toddlers as they begin toexplorethe environment beyond those most familiar tothem 5. Age appropriate activities -Parallel play: Toddlers observe other children and then might engage in activities nearby -Appropriate activities: -Playing with blocks -Push-pull toys -Large-piece puzzles -Thick crayons -Toilet training can begin when toddlers havethe sensation of needing tourinate or defecate 6. Motor skill development 15 Months o Walks without help | Creeps up stairs o Uses a cup well | Builds 2 tower blocks 18 Months o Runs clumsily | Throws overhand | Jumps in place w/ both feet | Pulls/Pushes toys o Manages a spoon w/o rotation | Turns pages 2-3 pages /time | Builds 3-4 blocks | Uses crayon toscribble spontaneously | Feeds self 24 Months (2 years) o Walks backwards | Walks up/down stairs w/ 2 feet on each step o Builds 6-7 blocks | Turns pages 1 @ a time 30 Months (2.5 years) o Balances on 1 leg | Jumps across floor / off chair w/ both feet | Walks tiptoe o Draws circles | has good hand-finger coordination 7. Nutrition -Whole milk at 1 year old -Can start drinking low-fat milk after 2 years of age -Juice consumption should be limited to4-6 oz. per day -Foods that are potential choking hazards: -Nuts -Grapes -Hot dogs -Peanut butter -Raw carrots -Tough meats -Popcorn Chapter 5: Health Promotion of Preschoolers (3-6 years) 1. Physical development -Weight: -Gain 2-3 kg (4.5-6.5 lb) per year -Height: -Should grow 6.9-9 cm per year 2. Fine and gross motor skills 3 Years o Toe and heel walks o Tricycle o Jumps off bottom step o Stands on one foot for a few seconds 4 Years o Hops on one foot | Skips o Throws ball overhead o Catches ball reliably 5 Years o Jumps rope o Walks backward o Throws and catches a ball 3. Cognitive development -Piaget: preoperational stage -Moves from totally egocentric thoughts tosocial awareness andthe ability to considerthe viewpoint of others -Magical thinking: -Thoughts are all-powerful and can cause events tooccur -Animism: -Ascribing life-like qualities toinanimate objects 4.Psychosocial development -Erikson: Initiative vs. guilt: -Preschoolers become energetic learners, despite not having all ofthe physical abilities necessary tobe successful at everything -Guilt can occur when preschoolers believe they have misbehaved or when they are unable toaccomplish a task -During stress, insecurity, or illness, preschoolers can regress toprevious immature behaviors or develop habits (nose picking, bed-wetting, thumb sucking) 5. Age appropriate activities -Preschooler’s transition toassociative play -Play is not highly organized, but cooperation does exist between children -Appropriate activities: -Playing ball -Putting puzzles together -Riding tricycles -Playing pretend dress up activities -Role-playing 6. Sleep and rest -On average, preschoolers need about 12 hours of sleep -Keep a consistent bedtime routine -Avoid allowing preschoolers tosleep with their parents Chapter 6: Health promotion of School-Age children (6-12 years) 1. Physical development -Weight: -Gain 2-3 kg (4.4-6.6 lb.) per year -Height: -Grows 5 cm (2 in.) per year 2. Cognitive development -Piaget: Concrete operations -Able toseethe perspective of others 3. Psychosocial development -Erikson: Industry vs. Inferiority -A sense of industry is achieved throughthe development of skills and knowledge that allowsthe child toprovide meaningful contributions to society -A sense of accomplishment is gained throughthe ability tocooperate and compete with others -Peer groups play an important part in social development 4. Age appropriate activities -Competitive and cooperative play is predominant -Play simple board and number games -Play hopscotch -Jump rope -Ride bicycles -Join organized sports (for skill building) 5. Sleep and rest -Need 9 hrs of sleep at age 11 6. Dental health -The first permanent teeth erupt around 6 years of age Chapter 7: Health promotion of Adolescents (12 to20 years) 1. Physical development -Girls stop growing at about 2-2.5 years afterthe onset of menarche -In girls, sexual maturation occurs inthe following order: -Breast development -Pubic hair growth -Axillary hair growth -Menstruation -In boys, sexual maturation occurs inthe following order: -Testicular enlargement -Pubic hair growth -Penile enlargement -Growth of axillary hair -Facial hair growth -Vocal changes 2. Cognitive development -Piaget: Formal operations -Increasingly capable of using formal logic tomake decisions 3. Psychosocial development -Erikson: Identity vs. role confusion -Adolescents develop a sense of personal identity and tocome toview themselves as unique individuals 4. Age-appropriate activities -Nonviolent videogames -Nonviolent music -Sports -Caring for a pet -Reading Chapter 8: Safe Medication Administration 1. Oral -This route of medication administration is preferred for children -Avoid mixing medication with formula or putting it in a bottle of formula becausethe infant might not takethe entire feeding, andthe medication can alterthe taste ofthe formula -Usethe smallest measuring liquid medication for doses of liquid medication -Avoid measuring liquid medication in a tsp. or tbsp. -Administerthe medication inthe side ofthe mouth in small amounts -Strokethe infant underthe chin topromote swallowing while holdingthe cheeks together 2. Otic -Children younger than years: -Pullthe pinna downward and straight back -Children older than 3 years: -Pullthe pinna upward and back 3. Intramuscular -Use a 22-25 gauge, 1/2-1 inch needle -Vastus lateralis isthe recommended site in infants and small children -Other sites: -Ventrogluteal and deltoid 4. Intravenous -Avoid terminology such as “bee sting” or “stick” -Apply EMLA tothe site for 60 minutes prior toattempt (helps numb) -Keep equipment out of site until procedure begins -Perform procedure in a treatment room (don’t do it in their room) -Allow parents tostay if they prefer -Swaddle infants -Offer nutritive sucking toinfants before, during, and afterthe procedure Chapter 9: Pain management 1. Atraumatic measures -Use play therapy toexplain procedures, allowingthe child toperformthe procedure on a doll or toy 2. Pharmacological measures -Give medications routinely, vs. PRN, tomanage pain that is expected tolast for an extended period of time 3. Pain assessment tool -Flacc: 2 months- 7 years -Faces: 3 years and older -Oucher: 3-13 years -Numeric scale: 5 years and older Chapter 10: Hospitalization, illness, and play 1. Infant -Experiences stranger anxiety between 6-18 months -Displays physical behaviors as expressions of discomfort due toinability toverbalize 2. Toddler -Limited ability todescribe illness -Limited ability tofollow directions -Experiences separation anxiety -Can exhibit an intense reaction toany type of procedure -Behavior can regress 3. Preschooler -Fears related tomagical thinking -Can experience separation anxiety -Might believe illness and hospitalization are a punishment -Explain procedures using simple, clear language -Avoid medical jargon -Give choices when possible, such as, “Do you want your medicine in a cup or spoon?” 4. School-age child -Ability todescribe pain -Increasing ability tounderstand cause and effect -Provide factual information -Encourage contact with peer group 5. Adolescent -Perceptions of illness severity are based onthe degree of body images -Develops body image disturbance -Experiences feelings of isolation from peers -Provide factual information -Encourage contact with peer group Chapter 11: Death and Dying 1. Grief and mourning -Anticipatory grief: -When death is expected or a possible outcome -Complicated grief: -Extends for more than 1 year followingthe loss 2. Current stages of development -Infants/toddlers (birth-3 years): -Have little tono concept of death -Mirror parental emotions -Can regress toan earlier stage of behavior -Preschool (3-6): -Magical thinking allows forthe belief that thoughts can cause an event such as death resulting in feeling guilt and shame -Interpret separation from parents as punishment for bad behavior -View dying as temporary -School-age (6-12): -Begin tohave adult concept of death -Fear often displayed through uncooperative behavior -Adolescent (12-20): -Can have adult-like concept of death -Can have difficulty accepting death -Rely more on peers thanthe influence of parents -Can become increasingly stressed by changes in physical appearance 3. Physical manifestations of death -Sensation of heat whenthe body feels cool -Decreased sensation and movement in lower extremities -Swallowing difficulties -Bradycardia/hypotension -Cheyne-strokes respirations 4. After death -Allow family tostay withthe body as long as they desire -Allow family torockthe infant/toddler -Remove tubes and equipment -Offer toallow family toassist with preparation ofthe body Chapter 12: Acute Neurological disorders 1. Meningitis -Viral (aseptic) Meningitis: supportive care for recovery -Bacterial (septic) Meningitis: contagious infection -Hib and PCV vaccines decreasethe incidence -Poor Muscle Tone -Weak Cry -Poor Suck | Refuses Feedings -Vomiting/Diarrhea -Bulging Fontanels (late sign) -Seizures with a High-Pitched Cry -Bulging Fontanels -Poor Feedings | Vomiting -Possible nuchal rigidity -Brudzinki’s sign and Kernig’s sign not reliable for diagnosis -Seizures (often initial sign) -Nuchal rigidity -Fever/chills -Headache/vomiting -Irritability/restlessness that can progress todrowsiness/stupor -Petechiae or purpuric type rash (with meningococcal infection) -+ Brudzinski Sign:flexion of extremities with deliberate flexion of the neck -+ Kernig’s Sign: resistance toextension ofthe leg from a flexed position -Blood Cultures | CBC | CSF Analysis -Viral CSF -Clear Color | Slightly Elevated WBC & Protein | Normal Glucose | - Gram -Bacterial CSF -Cloudy Color | Elevated WBC | Elevated Protein | Decreased Glucose | +Gram -Lumbar Puncture(Definitive Diagnostic Test) -Empty Bladder -EMLA Cream 45min – 1-hour prior -Side-lying Position, Head Flexed, Knees Drawn up toChest -Remain in Flat Position toprevent Leakage and Spinal HA -Droplet precautions -Maintain NPO status ifthe client has decreased LOC -Decrease environmental stimuli -IV antibiotics for bacterial infections -ICP: -Newborns and Infants -Bulging or Tense Fontanels -Increased Head Circumference -High-Pitched Cry | Irritability -Distended Scalp Veins -Bradycardia | Respiratory Changes -Children -Headache -N/V -Diplopia -Seizures -Bradycardia | Respiratory Changes 2. Reye Syndrome -Affectsthe liver (liver dysfunction) and brain (cerebral edema) -Follows a viral illness (Influenza | Gastroenteritis | Varicella) -Giving Aspirin for treating fevers -Elevated liver enzymes (ALT and AST) -Elevated serum ammonia -Liver biopsy/CSF analysis Chapter 13: Seizures 1. Risk factors -Febrile Episode -Cerebral Edema -Intracranial Infection / Hemorrhage -Brain Tumors / Cyst -Toxins or Drugs -Lead Poisoning -Hypoglycemia -Electrolyte imbalances 2. Generalized seizures -Tonic Phase (10-30 seconds) -Loss of Consciousness | Loss of Swallowing Reflex | Apnea leading to Cyanosis -Tonic Contraction of entire body: arms and legs flexed, head and neck extended -Clonic Phase (30-50 seconds) -Violent jerking movements ofthe body -Postictal State (30 minutes) -Remains semiconscious but arouses with difficulty and confused -No recollection ofthe seizure -Onset between ages 5 – 8 years and ceases bythe teenage years -Loss of Consciousness lasting 5 – 10 seconds -Minimal or no change in behavior -Resembles daydreaming or Inattentiveness -Can drop items being held, butthe child seldom falls -Lip Smacking | Twitching of Eyelids or Face | Slight Hand Movements -Brief contraction of muscle or groups of muscle -No postictal state -Muscle tone is lost for a few seconds 3. Diagnostic procedures -Abstain from caffeine for several hours prior tothe procedure -Wash hair (no oils or sprays) before and afterthe procedure to remove electrode gel 4. Nursing care -Pad side rails of Bed | Crib | Wheelchair -Keep bed free of objects that could cause Injury -Have Suction and Oxygen Equipment available -Protect from Injury (move furniture away, hold head in lap) -Maintain a position toprovide a patent airway -Suction Oral Secretions -Side-lying Position (decreases risk of aspiration) -Loosen restrictive clothing -Do NOT restrainthe child -Do NOT put anything inthe child’s mouth -Do NOT openthe jaw or insert an airway during seizure -This can damage teeth, lips, or tongue -Remain withthe child -Note onset, time, and characteristics of seizure -Allow seizure toend spontaneously -Side-lying position toprevent aspiration and facilitate drainage of secretions -Check for breathing, V/S and position of head -NPO until swallowing reflex has returned 5. Medications -Diazepam (Valium) | Phenytoin | Carbamazepine | Valporic Acid | 6. Therapeutic procedures -Focal Resection: of an area ofthe brain toremove epileptogenic zone -Corpus Callostomy: separation of two hemispheres inthe brain 7. Complications -Prolonged Seizure Activity that Lasts >30 minutes or Continuous seizure activity in whichthe client does not enter a Postictal Phase -Maintain Airway, Administer oxygen, IV access Chapter 14: Head injury 1. Physical assessment findings -Vomiting -Pallor -Irritability -Lethargy/drowsiness -Infants: -Bulging fontanel -Irritability (usually 1st sign) -High-pitched cry -Poor feeding -Children: -Nausea/headache -Forceful vomiting -Blurred vision -Seizures -Late signs: -Alterations in pupillary response -Posturing (flexion and extension) -Decreased motor response -Decreased response topainful stimuli -Cheyne-stokes respirations -Seizures -Flexion: severe dysfunction ofthe cerebral cortex -Extension: Severe dysfunction atthe level ofthe midbrain 2. Nursing care -Ensurethe spine is stabilized until a spinal cord injury is ruled out -Implement actions todecrease ICP: -Keepthe head midline withthe bed elevated 30 degrees, which will also promote venous draining -Avoid extreme flexion, extension, or rotation ofthe head and maintain in midline neutral position -Keepthe client’s body in alignment, avoiding hip flexion/extension -Minimize oral suctioning -Nasal suctioning is contraindicated -Instructthe client toavoid coughing and blowingthe nose -Insert and maintain indwelling catheter -Administer stool softeners toavoid straining 3. Medications -Osmotic diuretic used totreat cerebral edema -Antiepileptic: -Used toprevent or treat seizures -To help decrease edema 4. Therapeutic procedures -Craniotomy: tohelp relieve pressure 5. Complications -Bleeding betweenthe dura andthe skull -Bleeding betweenthe dura andthe arachnoid membrane -Downward shift of brain tissue Chapter 15: Cognitive and sensory impairments 1. Visual impairments -Sees close objects clearly, but not objects inthe distance -Sees distant objects clearly, but not objects that re close -Esotropia: inward deviation ofthe eye -Exotropia: outward deviation ofthe eye -Occlusion therapy: -Patch stronger eye tomake weaker eye stronger 2. Visual screening -Placethe client 10 feet fromthe chart with heels onthe 10-foot mark Chapter 16: Oxygen and Inhalation therapy 1. Metered-dose Inhaler -Shakethe inhaler 5-6 times -Attachthe spacer -Helps facilitate proper inhalation -Take a deep breath and then exhale -Tiltthe head back slightly, and pressthe inhaler -While pressingthe inhaler, begin a slow, deep breath that lasts for 3-5 seconds -Holdthe breath for 5-10 seconds 2. Dry powder inhaler -DO NOT shake 3. Chest physiotherapy -Is a set of techniques that includes manual or mechanical percussion, vibration, cough, forceful expiration (or huffing), and breathing exercises -Helps loosen respiratory secretions -Schedule treatments before meals or at least 1 hr after meals and at bedtime -Administer bronchodilator medication or nebulizer treatment prior 4 4. Hypoxemia -Tachypnea -Tachycardia -Restlessness -Use of accessory muscles -Nasal flaring 5. Oxygen toxicity -Can result from high concentrations of oxygen, long duration of oxygen therapy, andthe child’s degree of lung disease -Hypoventilation and increased PaCO2 levels allow for rapid progression into unconscious state Chapter 17: Acute and infectious respiratory illnesses 1. Tonsillitis -Report of sore throat with difficulty swallowing -Mouth odor/mouth breathing -Fever -Tonsil inflammation with redness and edema -Throat culture: -For GABHS -Antipyretics/analgesics: acetaminophen -Antibiotics: for Tx of GABHS -Side-lying position after then elevate HOB when child is awake -Assess for evidence of bleeding: -Frequent swallowing/clearingthe throat -Avoid red-colored liquids, citrus juice, and milk-based foods -Discourage coughing, throat clearing, and nose blowing in order to protectthe surgical site -Avoid straws: can damage surgical site -Alert parents that there can be clots or blood-tinged mucus in vomitus -Limit activity todecreasethe potential for bleeding -Fully recovery usually occurs in 14 days 2. Croup syndromes -Expected findings: -Drooling -Dysphonia: thick, muffled voice and froglike croaking sound -Dysphagia -High fever -Nursing care: -Avoid throat culture/putting tongue blade inthe mouth -Prepare for intubation -Administer ABX therapy starting with IV, then transition tooral to complete a 10-day course -Droplet isolation precautions for first 24 hr after IV ABX initiated 3. Influenza A and B -Sudden onset of chills and fever -Body aches -Amantadine, Zanamivir, Oseltamivir Chapter 18: Asthma 1. Triggers toasthma -Allergens -Smoke -Exercise -Cold air or changes inthe weather or temperature 2. Expected findings -Dyspnea -Cough -Audible wheezing -Use of accessory muscles 3. Medications -SE: tremors/tachycardia -Dries you up -Rinse mouth afterwards 4. How touse a peak flow meter -Ensurethe marker is zeroed -Close lips tightly aroundthe mouthpiece -Blow out as hard and as quickly as possible -Repeat 3 more times -Record highest number 5. Complications -Airway obstruction that is often unresponsive totreatment -Prepare for emergency intubation Chapter 19: Cystic Fibrosis 1. Cystic fibrosis -Both biological parents carrythe recessive trait for CF -Characterized by mucus glands that secrete an increase inthe quantity of thick, tenacious mucus, which leads tomechanical obstruction of organs 2. Expected findings -Wheezing, rhonchi -Dry, nonproductive cough -Dyspnea -Paroxysmal cough -Obstructive emphysema and atelectasis on chest x-ray -Cyanosis -Barrel-shaped chest -Clubbing of fingers and toes -Large, frothy, bulky, foul-smelling stools (steatorrhea) -Failure togain weight or weight loss -Delayed growth patterns -Distended abdomen -Thin arms and legs -Deficiency of fat-soluble vitamins (Vitamin A,D,E,K) -Sweat, tears, and saliva having high content of sodium and chloride 3. Diagnostic procedures -Sweat chloride test (most definitive) 4. Nursing care -Chest physiotherapy -High protein/calorie -Give pancreatic enzymes within 30 min of eating a meal or snack -Multivitamin A,D,E,and K 5. Medications -Dornase alfa (pulmozyme): decreases viscosity of mucus and improves lung function Chapter 20: Cardiovascular disorders 1. Defects that INCREASE pulmonary blood flow -A hole inthe septum betweenthe right and left ventricle that results in increased pulmonary blood flow (left-to-right shunt) -Expected finding: -Loud, harsh murmur atthe left sternal border -A hole inthe septum betweenthe right and left atria that results in increased pulmonary blood flow (left-to-right shunt) -Expected findings: -Loud, harsh murmur with a fixed split second heart sound -Connection between pulmonary artery and aorta stays open after birth causing mixing of blood -Expected findings: -Murmur (machine hum) -Bounding pulses 2. Defects that DECREASE pulmonary blood flow -A complete closure ofthe tricuspid valve that results in mixed blood flow -Pulmonary stenosis, right ventricular hypertrophy, overriding aorta, and ventricular septal defect (PROV) 3. Obstructive defects -A narrowing ofthe pulmonary valve or pulmonary artery that results in obstruction of blood flow fromthe ventricles -Expected findings: -Systolic ejection murmur -A narrowing ofthe aortic valve -A narrowing ofthe lumen ofthe aorta -Expected findings: (BP/pulse elevated on top, but not onthe bottom) -Elevated blood pressure inthe arms -Bounding pulses inthe upper extremities -Decreased blood pressure inthe lower extremities -Cool skin of lower extremities -Weak or absent femoral pulses 4. Mixed defects -A condition in whichthe aorta is connected tothe right ventricle instead of the left, andthe pulmonary artery is connected tothe left ventricle instead of the right -Expected findings: -Severe toless cyanosis depending onthe size ofthe associated defect -Failure of septum formation, resulting in a single vessel that comes off ofthe ventricles -Left side ofthe heart is underdeveloped -Expected findings: -Lethargy/cyanosis 5. Cardiac catherization -Check for allergies toiodine or shellfish -Provide for NPO status 4-6 hr prior -Locate and markthe Dorsalis pedis and posterior tibial pulses on both extremities -Prevent bleeding by maintainingthe affected extremity in a straight position for 4-8 hr 6. Heart medications -Infant: hold if pulse<90 -Children: hold if pulse <70 -Monitor for toxicity: -Bradycardia -Dysrhytmias -Nausea/vomiting -Anorexia -Watch for hypokalemia (nausea/vomiting/dizziness) -Foods high in potassium: -Bran cereal, potatoes, tomatoes, dark green leafy veggies, bananas, orange juice, oranges, and melons 7. Hypoxemia -Immediately placethe child inthe knee-chest position, attempt tocalmthe child, and call for help 8. Infective (bacterial) endocarditis -Counselthe family of high-risk children aboutthe need for prophylactic antibiotics prior todental and surgical procedures 9. Rheumatic fever -Usually occurs within 2-6 weeks following an untreated or partially treated upper respiratory infection (strep throat) with GABHS -Throat culture for GABHS -Serum antistreptolysin-O titer: -Elevated or rising titer, most reliable diagnostic test -The diagnosis of rheumatic fever is made onthe basis of modified jones criteria -The child should demonstratethe presence of 2 major criteria orthe presence of 1 major and 2 minor criterion following an acute infection with GABHS infection -Major criteria: -Carditis -Subcutaneous nodules -Polyarthritis -Rash (erythema marginatum) -Chorea: involuntary muscle movements -Minor criteria: -Fever -Arthralgia 10. Kawasaki disease -Acute systemic vasculitis (inflammation ofthe blood vessels inthe body) -Acute phase: -Fever greater than 102 F lasting 5 days to2 weeks and unresponsive to antipyretics -Irritability -Red eyes without drainage -Bright red, chapped lips -Strawberry tongue with white coating or red bumps onthe posterior aspect -Red oral mucous membranes with inflammation includingthe pharynx -Swelling of hand and feet with red palms and soles -Sub acute phase: -Peeling skin aroundthe nails, onthe palms/soles -Gamma globulin: IVGG -Aspirin -Avoid live immunizations for 11 months Chapter 21: Hematologic disorders 1. Epistaxis -Havethe child sit up withthe head tilted slightly forward toprevent aspiration of blood -Apply pressure tothe lower nose withthe thumb and forefinger for at least 10 min -If needed, pack cotton or tissue intothe side ofthe nose that is bleeding -Apply ice acrossthe bridge ofthe nose if bleeding continues 2. Iron deficiency anemia -Adolescents are at risk due topoor diet, rapid growth, menses, strenuous activities, and obesity -Excessive intake of cow’s milk in toddlers -Milk is not a good source of iron -Milk takesthe place of iron-rich solid foods -Modifythe infants diet toinclude high iron and vitamin C -Iron supplements: -Give 1 hr before or 2 hr after milk or antacid toprevent decreased absorption -Give with Vitamin c toincrease absorption -Use a straw toprevent staining ofthe teeth -Use a z-track method for injection -Do not massagethe injection site -Tarry green stools are expected -Instructthe child tobrush teeth after oral dose tominimize or prevent staining -Infants: Iron-fortified cereals and formula -Older children: Dried beans, lentils, peanut butter, green leafy veggies, iron- fortified breads and flour, and red meat 3. Sickle cell anemia -SCD is an autosomal recessive genetic disorder -Primarily affects African Americans -Causes cell tobe sickled shape causing increased blood viscosity, obstruction of blood flow, and tissue hypoxia -Reports of pain: due totissue ischemia -Shortness of breath/fatigue -Pallor -Jaundice -Severe pain, usually in bones, joints, and abdomen -Keep patient hydrated -Schedule administration of analgesics toprevent pain -CVA 4. Hemophilia -Bleeding time is extended due tolack of a factor required for blood toclot -Hemophilia A: deficient of factor VIII -Hemophilia B: deficient of factor IX -Excessive bleeding -Reports of joint pain and stiffness -Easy bruising -Activity intolerance -Prolonged PTT -PLT and PT within expected ranges -Avoid unnecessary skin punctures -Elevate and apply ice tothe affected joints -Set activity restrictions toavoid injury -Low-contact sports: bowling, fishing, swimming, and golf -Use soft-bristled toothbrushes -Control bleeding episodes using RICE (rest, ice, compress, and elevate) -Joint deformity Chapter 22: Acute infectious GI disorders 1. Rotavirus -Most common cause of diarrhea in children younger than 5 years -Fever -Diarrhea for 5-7 days -Vomiting for 2 days 2. Enterobius vermicularis (pinworm) -Perineal itching -Perform a tape test over anus at night 3. Diarrhea -Avoid: -Fruit juices, carbonated sodas, and gelatin -Caffeine -Chicken or beef broth -BRAT diet -Cleanse toys and childcare areas thoroughly toprevent further spread or reinfestation -Avoid undercooked or under-refrigerated food -Do not share dishes and utensils 4. Dehydration -Capillary refill greater than 2 seconds -Possible slight thirst -Capillary refill between 2-4 seconds -Possible thirst and irritability -Capillary refill >4 -Tachycardia -Extreme thirst -Very dry mucous membranes and tented skin -No tearing with sunken eyeballs -Sunken anterior fontanel -Oliguria and anuria Chapter 23: Gastrointestinal structural and inflammatory disorders 1. Cleft lip and cleft palate -Results from incomplete fusion ofthe oral cavity during intrauterine life -Apply elbow restraints -Results fromthe incomplete fusion ofthe palates during intrauterine life -Infant may be placed onthe abdomen (prone) -Use a wide-based nipple for bottle-feeding -Use a specialized bottle with a one-way valve and a specially cut nipple -Avoid havingthe infant suck on a nipple or pacifier -Ear infections and hearing loss -Speech and language impairment -Dental problems 2. GERD -Infants: -Sitting up or forceful vomiting -Irritability -Arching of back -Children: -Difficulty swallowing -Chronic cough -Non-cardiac chest pain -Small, Frequent Meals -Thicken infant’s formula with 1 tsp. to1 tbsp. rice cereal per 1oz formula -Avoid: Caffeine | Citrus | Peppermint | Spicy or Fried Foods -Assist with weight control -HOB elevated during and after meals (at least 30 degrees) -Nissen fundoplication: wrapsthe fundus ofthe stomach aroundthe distal esophagus todecrease reflux 3. Hypertrophic pyloric stenosis -Thickening ofthe pyloric sphincter, which creates an obstruction -Projectile vomiting -Constant hunger/dehydration -Olive-shaped mass inthe right upper quadrant ofthe abdomen -Pylorotomy 4. Hirschprung’s disease -Lack of ganglionic cells in segments ofthe colon resulting in decreased motility and mechanical obstruction -Newborn: -Failure topass meconium within 24-48 after birth -Episodes of vomiting bile -Refusal toeat -Abdominal distention -Child: -Foul-smelling, ribbon-like stool -High-protein/calorie and low-fiber diet -Surgical removal ofthe aganglionic section ofthe bowel -Temporary colostomy can be required 5. Intussusception -Proximal segment ofthe bowel telescopes into a more distal segment -Abdominal mass (sausage-shaped) -Stools mixed with blood and mucus that resemblesthe consistency of red currant jelly -Air enema 6. Appendicitis -Inflammation ofthe vermiform appendix -Average client age is 10 years -Abdominal pain inthe right lower quadrant -Decrease or absent bowel sounds -Fever -CBC -CT scans -Avoid applying heat tothe abdomen -Watch for pain: if patient no longer feels pain, appendix ruptured -Pre-op: -Give IV fluid replacement/IV antibiotic -Post-op: -Place NG tube for decompression Chapter 24: Enuresis and Urinary tract infections 1. Enuresis -Must be at least 5 years of age before there’s consideration about diagnosing enuresis -A child has never been free of bed-wetting for any extended periods of time -A child who started bed-wetting after development of urinary control -Nursing care: -Havethe child empty their bladder before bedtime -Encourage fluids duringthe day and restrict fluids inthe evening -Avoid fruit and fruit drink, caffeinated or carbonated drinks after 1600 -Use positive reinforcement -Avoid punishing, scolding, or teachingthe child following an incident 2. UTI -Infants: -Poor feeding, vomiting, or failure togain weight -Increase in thirst -Frequent urination -Foul-smelling urine -Fever -Seizure -Pallor -Urinalysis and urine culture and sensitivity: -Nitrates and leukocytes will be increased -Teach females towipethe perineal area from front toback -Suggestthe use of cotton underwear -Instruct avoidance of bubble baths -Encourage frequent voiding -Empty complete bladder Chapter 25: Structural Disorders ofthe genitourinary tract and Reproductive system 1. Defects ofthe genitourinary tract -Eversion ofthe posterior bladder throughthe anterior bladder wall and lower abdominal wall -Coverthe exposed bladder with sterile, nonadherent dressing -Preparethe child for immediate surgery -Urethral opening located just belowthe glans penis, behindthe glans penis, or onthe ventral surface ofthe penile shaft -Meatus opening belowthe glans penis -Urethra opened on dorsal surface ofthe penis -Inability toretract foreskin of penis -Pain is either acute or insidious in onset and radiates tothe groin area Chapter 26: Renal disorders 1. Acute glomerulonephritis -Associated with GABHS -Cloudy, tea-colored urine -Decreased urine output -Periorbital edema -Facial edema that is worse inthe morning but then spreads toextremities and abdomen with progression ofthe day -Mild tosevere HTN -Urinalysis: -Proteinuria, smoke or tea-colored urine, hematuria, increased specific gravity -Renal function: -Elevated BUN and creatinine -Antistreptolysin O (ASO) titer: -Positive indicator forthe presence of streptococcal antibodies -Possible restriction of sodium and fluid -Monitor for skin break down (at risk due toedema) -Encourage frequent turning and repositioning -Diuretics and antipyretics 2. Nephrotic syndrome -Alterations inthe glomerular membrane allow proteins (especially albumin) topass intothe urine, resulting in decreased serum osmotic pressure -Facial and periorbital edema: decreased throughoutthe day -Decreased frothy urine -BP within expected range -Urinalysis/24-hour urine: -Proteinuria: protein greater than 2+ on dipsticks -Serum chemistry: -Hypoalbuminemia: reduced serum protein and albumin -Hyperlipidemia: elevated serum lipid levels -Hemoconcentration: elevated Hgb, Hct, and platelets -Monitor daily weights -Monitor edema and measure abdominal girth daily -Salt can be restricted duringthe edematous phase -Assess skin for breakdown -Corticosteroids: prednisone -Diuretic: furosemide -25% albumin: increases volume and decrease edema Chapter 27: Fractures 1. Fractures -The fracture occurs without a break inthe skin -The fracture occurs with an open wound and bone protruding -The fracture results in injury toother organs and tissues 2. Nursing care -Maintain ABC’s -Stabilizethe injured area, avoiding unnecessary movement -Elevatethe affected limb and apply ice packs (not toexceed 20 min) -Sensation: Assess for numbness or tingling sensation ofthe extremity -Loss of sensation can indicate nerve damage -Skin Temperature:Assessthe extremity for temperature. -It should be warm, not cool, totouch -Skin Color: Assessthe color ofthe affected extremity -Check distal tothe injury and look for changes of pigmentation -Capillary Refill: Pressthe nail beds ofthe affected extremity until blanching occurs -Blood return should be within 3 seconds -Pulses: Should be palpable and strong -Pulses should be equal tothe pulses ofthe unaffected extremity -Movement:the client should be able tomovethe joints distal tothe injury -Move Fingers or Toes 3. Casting -Elevatethe cast abovethe level ofthe heart duringthe first 24 -Apply ice forthe first 24 hours toprevent swelling -Turn and position every 2 hours (cast dries faster | prevents cast from changing shape) -Assess for increased warmth or hot spots onthe cast surface (infection) -Plaster Casts: Use Palms of Hands toavoid Denting | Exposethe Cast toAir -Instructthe client not toplace any foreign objects insidethe cast toavoid trauma tothe skin 4. Traction care -Maintain body alignment -Pharmacological and Nonpharmacologic Interventions for Pain and Muscle Spasms -Assess and monitor neurovascular status -Assess pin sites for pain, redness, swelling, drainage, or odor -Weights should hang freely -Halo device: -Ensure thatthe wrench toreleasethe rod is readily available when using halo traction inthe event that CPR is necessary 5. Complications -Compression of nerves, blood vessels, and muscle inside a confined place, resulting in neuromuscular ischemia -Findings: 5 P’s: -Pain: unrelieved with elevation or analgesics, increases with passive movement -Paresthesia: numbness (early finding) -Pulselessness: distal tofracture -Paralysis: inability tomove digits (nerve damage) -Pale: cold skin and cyanosis tonail beds -Expected findings: -Fever -Tachycardia -Edema -Pain is constant but increases with movement -Nursing actions: -Administer IV and oral ABX therapy Chapter 28: Musculoskeletal congenital disorders 1. Clubfoot -A complex deformity ofthe foot and ankle -Therapeutic procedures: -Series of castings 2. Legg-calve-Perthes disease -Aseptic necrosis ofthe femoral head can be unilateral or bilateral -Intermittent painless limp -Hip stiffness -Limited ROM -Shortening ofthe affected leg -Abduction brace -Casts -Physical therapy -Traction -Osteotomy ofthe hip or femur 3. Developmental dysplasia ofthe hip (DDH) -Infant: -Asymmetry of gluteal and thigh folds -Limited hip abduction -Widened perineum -Positive Ortolani test: -Hip is reduced by abduction -Positive Barlow Test: -Hip is dislocated by adduction -Child: -One leg shorter thanthe other -Positive Trendelenburg sign: -While bearing weight onthe affected side,the pelvis tilts downward -Walk with a limp -For newborn to6 months -Maintain harness placement for ? to12 weeks -Check straps every 1 to2 weeks for adjustment -Perform neurovascular and skin integrity checks (2-3 times/day) -Teachthe family not toadjustthe straps -Teachthe family skin care: -Use an undershirt -Wear knee socks -Gently massage skin under straps -Avoid lotions/powders -Place diaper underthe straps -> 6 months -Hips flexed at 90-degree angle with buttock raised off ofthe bed -Evaluate hydration status frequently -Assess elimination status daily 4. Osteogenesis imperfecta -“Brittle bone disease” -An inherited condition that results in bone fractures and deformity along with restricted growth -Multiple bone fractures -Blue sclera -Early hearing loss -Small, discolored teeth -Pamidronate: Increase bone density -SE: decreases electrolytes -Teachthe family and client low-impact exercises 5. Scoliosis -Characterized by a lateral curvature ofthe spine and spinal rotation that causes rib asymmetry -Havethe child bend over atthe waist with arms hanging down and observe for asymmetry of ribs and flank -Customized braces slowthe progression ofthe curve -Used for curvatures >45 degrees Chapter 29: Chronic Neuromusculoskeletal disorders 1. Cerebral palsy -Is a non-progressive impairment of motor function, especially that of muscle control, coordination, and posture -Abnormal perception and sensation; visual, hearing, and speech impairment; seizures; and cognitive disabilities -Exact cause is unknown -Prenatal, perinatal, and postnatal risk factors -Spastic CP (pyramidal): -Hypertonicity, increased deep tendon reflex; clonus; and poor control of motion, balance and posture -Dyskinetic CP (nonspastic, extrapyramidal): -Involuntary jerking movements that appear slow, writhing, and wormlike -Ataxic CP (nonspastic, extrapyramidal): -Poor ability todo repetitive movements -Lack of coordination with purposeful movements (ex: reaching for an object) -Baclofen/Diazepam -Aspiration 2. Spina Bifida -Is failure ofthe osseous spine toclose -The sac contains spinal fluid and meninges -The sac contains spinal fluid, meninges, and nerves -Medications/substances taken during pregnancy -Insufficient folic acid intake during pregnancy -Protruding sac midline ofthe osseous spine (cystica) -Dimpling inthe lumbosacral area (occulta) -Closure of myelomeningocele sac is done as soon as possible toprevent complications of injury and infection -Apply a sterile, moist, nonadherent dressing with 0.9% sodium chloride on the sac, changing it every 2 hr -Place inthe infant in prone position with hips flexed, legs abducted -Skin ulceration -Latex allergy: -Also bananas, avocados, kiwi, and chestnuts -Increased intracranial pressure: -Infants: -High-pitched cry, lethargy, vomiting, bulging fontanels, and increased head circumference -Bladder issues -Orthopedic issues 3. Juvenile idiopathic arthritis -Chronic autoimmune inflammatory disease affecting joints and other tissues -Joint swelling/stiffness/redness/warmth that tends tobe worse inthe morning or after inactivity -Apply heat or warm moist packs tothe child’s affected joints prior to exercise -Encourage warm baths -NSAIDs: control pain and inflammation -Ibuprofen, naproxen, diclofenac, indomethacin, and tolmetin -DMARD: slows joint degeneration and progression of rheumatoid arthritis when NSAIDs do not work alone -Methotrexate -Corticosteroid: -Prednisone 4. Muscular dystrophy -Is a group of inherited disorders with progressive degeneration of symmetric skeletal muscle groups causing progressive muscle weakness and wasting -Isthe most common form of MD -Onset between 3 and 5 years -Muscle weakness beginning inthe lower extremities -Unsteady gait, with a waddle -Lordosis -Delayed motor skill development -Frequent falling -Learning difficulties -Progressive muscle atrophy -Respiratory and cardiac difficulties asthe disease progresses -Corticosteroids -Respiratory complications Chapter 30: Skin infections and infestations 1. Bacterial skin infections -Manifestations: -Reddish macule becomes vesicular -Erupts easily leaving moist erosion onthe skin, secretions dry forming crusts -Spreads by direct -Pruritus common -Management: -Topical bactericidal or triple antibiotic ointment -Burrow’s solution -Manifestations: -Firm, swollen, red area ofthe skin and subcutaneous tissue -Fever/malaise -Management: -Oral or parenteral ABX -Warm/moist compress 2. Fungal skin infections -Use selenium sulfide shampoos -Treat infected pets -Round erythematous scaling patch -Use topical antifungal (tolnaftate, Clotrimazole) -Between toes or onthe plantar surface ofthe feet 3. Skin infestations -Manifestations: -Itchy, especially at night -Rash, especially betweenthe fingers -Thin, pencil-like marks onthe skin -Infants: -Pimples onthe trunk -Blisters onthe palms ofthe hands and soles ofthe feet -Interventions: -Scabicide such as 5% permethrin all over body -Treat entire family and persons that have been in contact with infected person during and 60 days after infection -Wash underwear, towels, clothing, and sleepwear in hot water -Intense itching -Nits (white specs) onthe hair shaft -1% permethrin shampoo -Remove nits with a nit comb; repeat in 7 days after shampoo TX -Washing clothing, bedding in hot water with detergent -Teachthe parent tobag items that cannot be laundered into tightly sealed bag for 14 days -Teachthe parents toboil combs, brushes and hair accessories for 10 min or soak in lice-killing products for 1 hr -Discourage sharing of personal items Chapter 31: Dermatitis and Acne 1. Dermatitis -Nursing interventions: -Clean urine inthe perineal area with a nonirritating cleanser -Exposethe affected area toair -Use superabsorbent disposable diapers toreduce skin exposure (no cloth) -Apply a skin barrier (zinc oxide) -Poisonous plant exposure: -Cleanse exposed area as soon as possible with cold running water, then soap and water shower -Apply calamine lotion; burrow solution compresses, or natural colloidal oatmeal baths -Use topical corticosteroid gel -Seborrheic dermatitis: (thick flakes on scalp) -Treat by gently scrubbingthe scalp toremove scales and crusted areas -Petrolatum, vegetable oil, or mineral oil can be helpful -Use a fine-tooth comb toremovethe loosened crusts fromthe hair -Shampoo daily with antiseborrheic shampoo -Client education: -Encourage frequent diaper -Advise parents that their child should avoid bubble baths and harsh soaps -No talcum powder but cornstarch is okay toprevent friction -Keep fingernails trimmed short 2. Atopic dermatitis -Is a type of eczema -Dress in Cotton Clothing (avoid wool and synthetic fabrics) -Avoid excessive heat and perspiration (increase itching) -Avoid irritants (Bubble Baths | Soaps | Perfumes | Fabric Softeners) -Place gloves or cotton socks over hands for sleeping -Antihistamines/topical corticosteroids 3. Acne -Teachthe child togently washthe face and other affected areas, avoiding scrubbing and abrasive cleaners -Trentinoin: -Avoid Sun Exposure | Use Sunscreen Daily (SPF 15 or greater) -Benzoyl peroxide: -Can bleach clothing but not skin -Isotretinoin: -SE: -Elevated cholesterol/triglycerides -Depression/suicidal ideation/violent behaviors -Contraindicated in women who are not taking oral contraceptives Chapter 32: Burns 1. Stages of burns -Superficial: -Damage tothe epidermis (sunburn) -Pink tored in color with no blisters -Blanches with pressure -Painful -Second degree: -Superficial partial thickness: -Damage tothe entire epidermis -Dermal elements are intact -Painful, moist, red in color with blisters -Blanches with pressure -Sensitive totemperature changes, exposure toair, and light touch -Deep partial thickness: -Damage tothe entire epidermis and some parts ofthe dermis -Sweat glands and hair follicles remain intact -Red towhite in color, with blisters -Blanches with pressure -Painful -Sensitive totemperature changes and light touch -Full thickness: -Damage tothe entire epidermis and dermis and possible damage to the subcutaneous tissue -Red totan, black, brown, or waxy white in color -Dry, leathery appearance -Deep full thickness: -Damage toall layers ofthe skin that extends tomuscle, bone, and fascia -No pain is present 2. Nursing care -Check immunization status, and determinethe need for immunization -Administer tetanus vaccine if it has been more than 5 years -Educatethe family toavoid using greasy lotions or butter on burns -Maintain airway and ventilation -Initiate IV access with large-bore catheter -Multiple access points may be necessary -Fluid replacement is important duringthe first 24 hours -Isotonic crystalloid solutions, such as 0.9% sodium chloride or lactated ringer’s are used duringthe early stage of burn recovery -Maintain urine output of 0.5 to1 ml/kg/hr is <30 kg -Maintain urine output of 30 ml/hr for >30 kg -Manage pain: -Use IV opioid -Provide nutritional support: -Increase caloric intake/protein -Vitamin A, C, and zinc for wound healing -Maintain active and passive range of motion 3. Medications -Silver sulfadiazine/ Mafenide acetate -Use with 2nd and 3rd degree burns -Apply tocleansed, debrided area -Wear sterile gloves for applications -Bacitracin: -Use for prevention of secondary infection 4. Skin coverings -Allograft (homograft): -Skin from human cadavers that is used for partial and full thickness burn wounds -Xenograft: -Obtained from animals: pigs (partial thickness burns) -Autografts: -Client’s skin Chapter 33: Diabetes Mellitus 1. Risk factors -Genetics -Toxins/viruses: can destroythe beta cells ->type 1 DM -Obesity/physical inactivity/HTN -> type 2 DM 2. Expected findings -Hunger, lightheadedness, and shakiness -Pale, cool skin/diaphoresis -Decreasing LOC -Slurred speech -Headache and blurred vision -Seizures leading tocoma -Thirst -Polyuria (early sign)/oliguria (late sign) -Nausea, vomiting, and abdominal pain -Skin that is warm, dry, and flushed with poor turgor -Dry mucous membranes -Confusion -Weakness -Lethargy -Weak pulse -Diminished reflexes -Rapid, deep respirations with acetone/fruit odor due toketones (Kussmaul respirations) 3. Laboratory tests -An 8-hr fasting blood glucose level of 126 or more -Random blood glucose of 200 or more with classic sign of diabetes -An oral glucose tolerance test of 200 or more inthe 2 hr sample -Expected reference range is 4%-5.9% -Acceptable target for children who have diabetes: 6.5%-8% -If >7%: not regulating sugar well 4. Nursing care -Trimming toenails straight across with clippers and filing edges with a nail file -Cautionthe child against wearing sandals, walking barefoot, or wearing socks without socks -Dry feet completely -Can use mild foot powder: cornstarch -Never use commercial remedies for removing callus/corn -Sock: cotton or wool -No heating pads for feet -Monitor blood glucose and urinary ketone levels every 3 hr -Continue totake insulin or oral Antidiabetic agents -Encourage sugar-free, noncaffeinated liquids toprevent dehydration -Blood glucose >240 -Fever 102F -Positive ketones inthe urine -Disorientation or confusion occurs -Rapid breathing is experienced -Treat with 10-15 g simple carbohydrates (1tbsp sugar) -Ex: 4 OZ orange juice/8OZ milk -Administer glucagon SC or IM -Administer simple carbohydrates as soon as tolerated 5. Medications 6. Complications ->330 mg/dL -Expected findings: -Ketone levels inthe blood and urine -Fruity scent tothe breath -Mental confusion -Dyspnea -Nausea and vomiting -Electrolyte imbalances: Metabolic acidosis/hyperkalemia -Nursing actions: -Monitor serum potassium levels -Administer sodium bicarbonate by slow IV infusion for severe acidosis (pH <7) -Have a cardiac monitor Chapter 34: Growth Hormone deficiency 1. Expected findings -Short stature but proportional height and weight -Delayed epiphyseal closure -Delayed sexual development 2. Medications -Given until epiphyseal plate closes -Administer SC Chapter 35: Immunizations 1. Contraindications -Occurrence of encephalopathy within 7 days following prior doses ofthe vaccine -Anaphylactic reaction toneomycin, streptomycin or polymyxin B -Anaphylactic reaction toeggs, gelatin, and neomycin -Hypersensitivity toeggs -If taking corticosteroids -The common cold and other minor illnesses are not contraindications toimmunizations -Severe febrile illness is a contraindication toall immunizations -Do not administer live virus vaccines, such as varicella or MMR, toa child who is severely Immunocompromised 2. Nursing administration -Give IM immunizations inthe Vastus lateralis or ventrogluteal muscle in infants and young children -Give IM immunization inthe deltoid muscle for older children/adolescents -Give infants a concentrated oral sucrose solution 2 min prior to, during, and 3 min after immunization administration -Document date, route, site of immunization, lot number, manufacturer and exp. Date Chapter 36: Communicable Diseases 1. Conjunctivitis -Spread: Direct contact (viral/bacterial -Pink or red color inthe sclera ofthe eyes -Crusting ofthe eyelids inthe morning 2. Epstein-Barr virus (EBV)/mononucleosis -Spread: saliva -Fever -Swollen lymph glands -Splenomegaly -Hepatic involvement -Complications: ruptured spleen (no contact sports) 3. Erythema infectiosum (fifth disease)/parvovirus B19 -Spread: droplet/blood -Rash (7 days toseveral weeks): -Red rash on face (slapped cheek), which appears from day 1 to4 4. Mumps/paramyxovirus -Spread: droplet -Painful, swollen parotid glands 5. Pertussis (whooping cough)/Bordetella pertussis -Spread: direct contact/droplet/indirect contact with freshly contaminated articles -Common cold manifestations: -Runny nose/congestion, sneezing, mild fever, and mild cough -Severe coughing starts in 1-2 weeks: -Coughing fits -Violent and rapid coughing -Loud “whooping” sound upon inspiration 6. Rubella (German measles)/rubella virus -Spread: droplet -Red rash that starts onthe face and spreads tothe rest ofthe body, lasting 2- 3 days -Birth defects (deafness; heart defects; mental, liver, and spleen damage) in fetus of women infected during pregnancy 7. Rubeola (measles)/rubeola virus -Spread: droplet -Cough, runny nose, red eyes, and sore throat -Rash: -Koplik spots (tiny white spots) appear in mouth 2 days before rash 8. Varicella (chicken pox)/varicella-zoster virus -Spread: droplet (airborne) -Manifestations 1-2 days prior torash: -Fever/fatigue -Rash: -Macules start in center of trunk, spreading tothe face and proximal extremities -Progresses from macules, topapules, tovesicles, and crust formations follow 9. Nursing care -Do not administer aspirin, due tothe risk of Reye Syndrome -Provide calamine lotion for topical relief -Keepthe child’s fingernails clean and short 10. Medications -Antihistamine -Antiviral therapy: -Acyclovir for high-risk clients who have varicella Chapter 37: Otitis Media 1. Risk factors -Most common inthe first 24 months of life and again when children enter school ages (5-6) 2. Medications -For analgesia and reduce fever 3. Therapeutic procedures -A small incision is made inthe tympanic membrane -The tubes come out spontaneously (usually in 6-12 months) -Instruct parents tonotifythe provider when tubes come out -This is usually does not require replacement of tubes Chapter 38: HIV/AIDS 1. HIV/AIDS -HIV infection is a viral infection in whichthe virus primarily infects a specific subset of T-lymphocytes,the CD4 T cell causing immune dysfunction -This leads toorgan dysfunction and a variety of opportunistic illnesses in a weakened host 2. Expected findings -Lymphadenopathy -Hepatomegaly -Splenomegaly -Dermatitis -Parotitis -Multiple serious bacterial infections -Kaposi’s sarcoma: skin infection -Pneumocystis carinii pneumonia -Wasting syndrome 3. Laboratory findings -Ages >6: -CD4 T-lymphocyte count= lower than 500=some immunosuppression -CD4 T-lymphocyte count=lower than 200=severe immunosuppression 4. Nursing care -Diet high in calories and protein -Provide good oral care -Prevent infection using standard precautions -Does not need special precautions -Teachthe child and parents toavoid individuals who have colds/infections/viruses -Encourage immunizations: -Pneumococcal vaccine and yearly influenza vaccine 5. Medications -Antiretroviral -Antibiotics -IV gamma globulin Chapter 39: Organ neoplasms 1. Wilms’ tumor (Nephroblastoma) -Is a malignancy that occurs inthe kidneys or abdomen -Tumor is usually unilateral -Most cases diagnosed between 2-3 years of age -Metastasis is rare -Painless, firm, nontender abdominal swelling or mass -Fatigue, malaise, and weight loss -Fever -Abdominal ultrasonography -Abdominal and chest CT scan -Bone marrow aspiration (rule out metastasis) -IF WILM’S TUMOR IS SUSPECTED DO NOT PALPATEthe ABDOMEN (can cause spread) 2. Neuroblastoma -Is a malignancy that occurs inthe adrenal gland -Usually manifested during toddler years -Half of all cases have metastasized before diagnosis -Half of children who have a Neuroblastoma have few findings -Manifestations of metastasis: -Ill appearance -Periorbital ecchymosis -Bone pain -Irritability -Skull, neck, chest, abdominal and bone CT scans -Bone marrow aspiration (rule out metastasis) 3. Chemotherapy -Provide an antiemetic prior toadministration -Observethe mouth for mucosal ulcerations -Educate aboutthe SE of chemotherapy: -Mouth sores -Loss of appetite -Nausea/vomiting -Hair loss -Diarrhea/constipation -Increased risk of infection -Easy bruising or bleeding -Fatigue 4. Radiation -Nurse: wear lead aprons -Instructthe child and family not towash off marks onthe skin that outlinethe targeted areas -Avoid use of soaps, creams, lotions, and powders unless prescribed -Keepthe areas protected fromthe sun by wearing a hat and long-sleeved shirts 5. Complications -Encouragethe child toavoid crowds while undergoing chemotherapy -Avoid fresh fruits and vegetables -Avoid invasive procedures -Is a granulocyte colony-stimulating factor that stimulates WBC production -Given SC daily -Given SC 2-3 times per week -Stimulate RBC production -Given SC daily -For PLT formation -Encouragethe use of soft toothbrush -Lubricatethe child’s lips -Avoid hydrogen peroxide and lemon glycerin swabs Chapter 40: Blood Neoplasms 1. Leukemia -Isthe term of a group of malignancies that affectthe bone marrow and lymphatic system -Bone marrow aspiration or biopsy analysis: -Topical anesthetic such as EMLA cream 45 min-1 hr prior -CSF analysis: -Havethe child empty their bladder -EMLA cream 45 min-1 hr prior -Side-lying position withthe head flexed and knees drawn up toward the chest, and assist in maintainingthe position (during procedure) -Remain in bed 4-8 hr in a flat position toprevent leakage and a resulting spinal headache (after) Chapter 43: Pediatric Emergencies 1. Obstructed airway -Use abdominal thrusts -Combination of back blows and chest thrusts -Remove any visual obstruction or large debris fromthe mouth, but do not perform a blind finger sweep 2. Drowning -Encourage parents of toddlers tolock toilet seats when their child is at home -Instruct parents tonot leavethe child unattended inthe bathtub -Inform parents not toleavethe child unattended in a swimming pool, even ifthe child can swim -Encourage parents toprovide life jackets when boating 3. SIDS -Maternal smoking during pregnancy -Co-sleeping with parent or adult -Prone or side-lying sleeping -Low birth weight -Placethe infant onthe back for sleep -Avoid exposure totobacco smoke -Prevent overheating -Use a firm, tight-fitting mattress inthe infant’s crib -Remove pillows, quilts, and stuffed animals fromthe crib during sleep -Offer pacifier at naps and night -Encourage breastfeeding -Avoid co-sleeping 4. Poisoning -1st thing todo is call poison control center -Emesis or lavage -Chelation therapy using deferoxamine mesylate Chapter 44: Psychosocial issues of infants, children and adolescents 1. ADHD -Inattention: -Difficulty in sustaining attention -Easily distracted -Forgetfulness -Hyperactivity -Impulsivity -Methylphenidate, Dextroamphetamine: -Increases dopamine and norepinephrine levels -Give 30 min before meals -Give last dose ofthe day prior to1800 toprevent insomnia -Atomoxetine 2. Autism spectrum disorder 7-Distress when routines are changed -Unusual attachment toobjects -Delayed or absent language development -Withdrawn, labile mood -Avoiding eye contact -Decrease environmental stimulation -Introducethe child tonew situations slowly -Encourage support groups for parents [Show More]
Last updated: 1 year ago
Preview 1 out of 67 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 1 )

by Peter-Student · 4 years ago
$18.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Mar 07, 2021
Number of pages
67
Written in
Additional information
This document has been written for:
Uploaded
Mar 07, 2021
Downloads
3
Views
162