*NURSING > STUDY GUIDE > NR569 Differential Diagnosis in Acute Care Midterm Study Guide (100% Guaranteed Pass) Latest Update (All)
NR569 Differential Diagnosis in Acute Care Midterm Study Guide (100% Guaranteed Pass) Latest Update
Document Content and Description Below
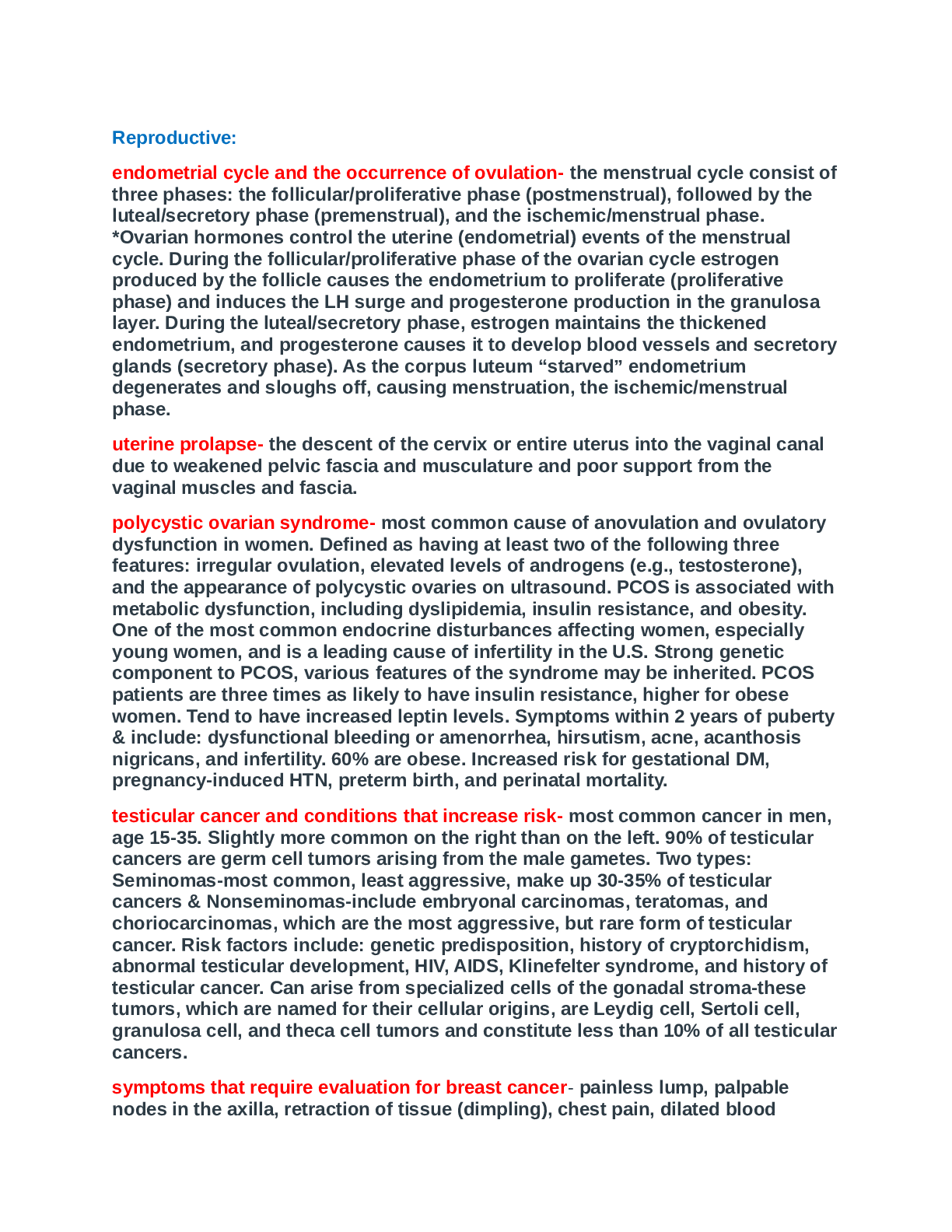
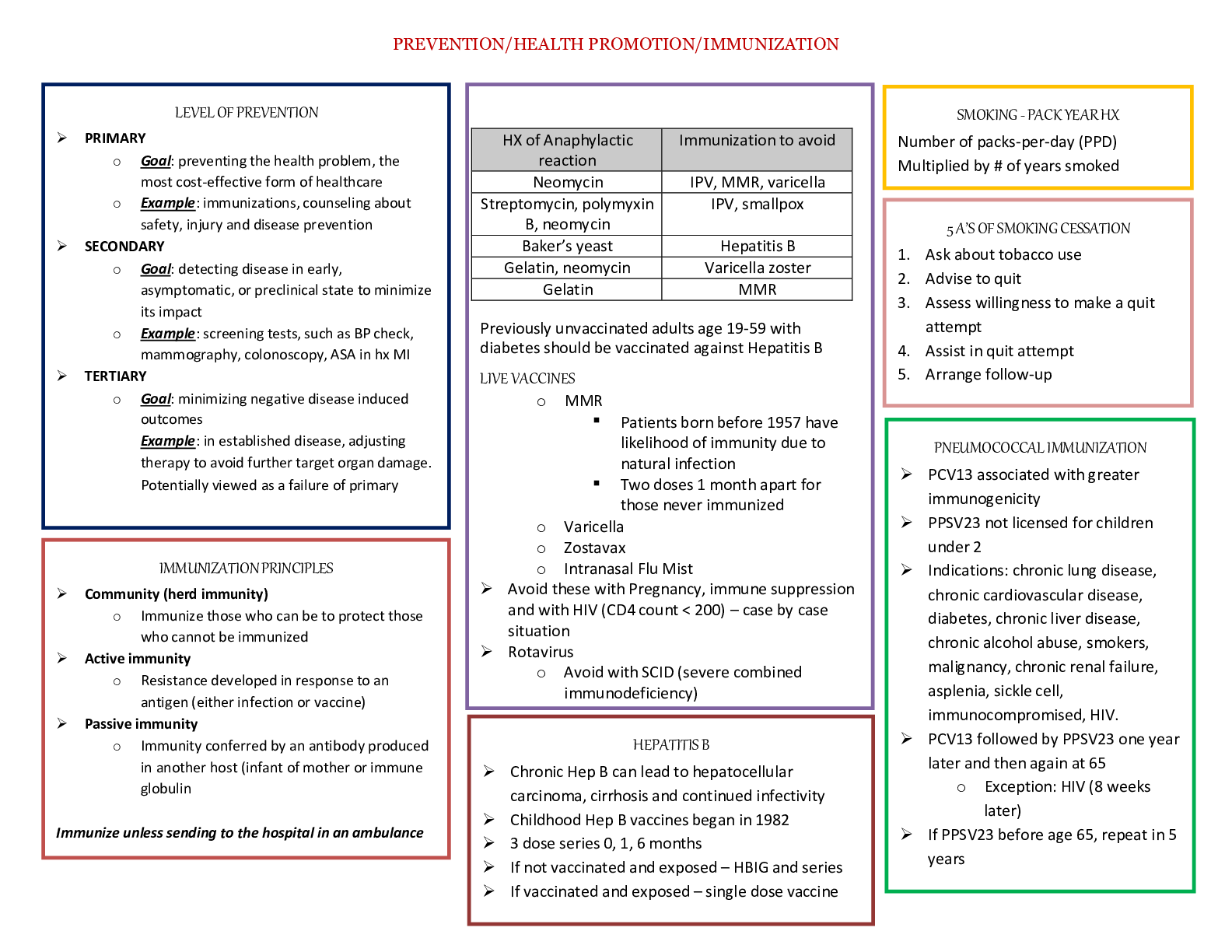
NR569 Differential Diagnosis in Acute Care Midterm Study Guide (100% Guaranteed Pass) Latest Update Comprehensive Patient Assessment - Appropriate for new patients in the office or hospital. - ... Provides fundamental and personalized knowledge about patient. - Strengthens the clinician-patient relationship. - Helps identify or rule out physical causes related to patient concerns. - Provides a baseline for future assessments. - Creates a platform for health promotion through education and counseling. - Develops proficiency in the skills of physical assessment. Focused Patient Assessment - Appropriate for established patients, especially during routine or urgent care visits. - Addresses focused concerns or symptoms. - Assesses symptoms restricted to a specific body system. - Applies examination methods relevant to assessing the concern or problem as thoroughly and carefully as possible. Brainpower Read More Subjective Information - The clinical record from the Chief Complaint (CC) through the Review of Systems (ROS) is considered SUBJECTIVE information. - Includes symptoms which are health concerns the patient tells the provider. - Includes feelings, perceptions, and concerns obtained from the clinical interview. - Examples: complaints of sore throat, headache, or pain. Objective Information - All physical examination, laboratory information and test data are objective data. Components of Comprehensive Adult Health History - Initial information (Identifying patient information/source/reliability) - Chief Complaint(s) - History of Present Illness - Past Medical History - Family History - Personal/Social History - Review of Systems (ROS) SNAPPS method - Summarize the history and findings. - Narrow the differential diagnosis to two to three possibilities. - Analyze the differential by comparing and contrasting the possibilities. - Probe the preceptor by asking questions about alternative approaches or uncertainties. - Plan the management of the patient's health issues. - Select an issue from the case for self-directed learning. Creating a Differential Diagnosis Hoofbeats = Horses NOT Zebras - The differential diagnosis process involves using clinical reasoning to distinguish between two or more conditions that share similar signs and symptoms. Based on the CC the NP gathers information through PMH (subjective data) and physical examination (objective data) to establish a broad list of common & uncommon diagnosis. As the provider collects more data, competing hypotheses are either confirmed, disproved, or their priority changes. Steps for Creating a Differential Diagnosis 1. Initially start with a broad list of diagnoses until further information or data is obtained. 2. List your top diagnosis FIRST followed by other potential diagnoses for a specific problem *but keep it problem oriented until you have an actual diagnosis.* 3. Aggressively prioritize work up of the most likely and most harmful (ie, life threatening) diagnoses under consideration. 4. Prioritize the work up of ACUTE and REVERSIBLE diseases followed by CHRONIC and IRREVERSIBLE (eg, delirium r/t a medical cause vs. chronic, progressive dementia). 5. As information or data that effectively rules out a particular diagnosis for a chief complaint becomes available, remove that diagnosis from your list & focus your attention on remaining possibilities. 6. Once a diagnosis has been confirmed, the problem list should be diagnosis-oriented rather than problem-oriented. Pertinent Positive - Symptoms or signs that are present that you would expect to find if a possible cause for for a patient's problem were true, which then supports the diagnosis. Pertinent Negative Expected symptoms or signs that are not present, facts that you would expect to find if a possible cause for a patient's problem were true, which then weaken this diagnosis by their absence. Principles of Good Documentation *Checklist to Ensure a Quality Clinical Record.* 1. Is the organization clear? - Make the headings clear. - Accent your organization with indentations and spacing. - Arrange the HPI in chronologic order, starting with the current episode, the filling in relevant background information. 2. Does the included information contribute directly to the Assessment? - Spell out the supporting evidence, both positive and negative, or each problem or diagnosis. Make sure there is sufficient detail to support your differential diagnosis and plan. 3. Are pertinent negatives specifically described? - Often portions of the history or examination suggest that an abnormality might exist or develop in that area. For example, for the pt with notable bruises, record the "pertinent negatives", such as the absence of injury or violence, familial bleeding disorders, or medications/nutritional deficits that might lead to bruising. 4. Are there overgeneralizations or omissions of important data? - REMEMBER THAT ANY INFORMATION NOT RECORDED IS INFORMATION LOST. 6. Is there too much detail? - Is there excess information or redundancy? Make your descriptions concise. You can omit unimportant structures even though you examined them, such as normal eyebrows and eye lashes. CONCENTRATE ON MAJOR NEGATIVE FINDINGS such as "no heart murmurs" rather than negative findings unrelated to the patient's complaints. 7. Is the written style succinct? Are phrases, short words, and abbreviations used appropriately? Is data unnecessarily repeated? - Using words or brief phrases instead of whole sentences is common, but abbreviations and symbols should be used only if they are readily understood. Omit unnecessary words. Describe what you observed, not what you did. 8. Are clear descriptions or images included whenever possible? - To ensure accurate evaluations and future comparisons, describe findings fully. Use measurements in centimeters, not fruits, nuts or vegetables. 9. Is the tone of the write up neutral and professional? - It is important to be objective. Hostile or disapproving comments have no place in the patient's record. Never use inflammatory or demeaning words or punctuation. Evaluation and Management (E/M) codes Evaluation and management (E/M) coding involves the use of CPT codes ranging from 99202-99499. These represent services by a provider in which the provider is either evaluating or managing a patient's health. Evidence-Based Medicine - The conscientious, explicit, judicious and reasonable use of modern, best evidence in making decisions about the care of individual patients. PICOT question - A mnemonic derived from the elements of a clinical research question - Patient, Intervention, Comparison, Outcome and Time. The PICOT process begins with a case scenario, and the question is phrased to elicit an answer. Sensitivity Sensitivity refers to a test's ability to designate an individual with a disease as positive. - A sensitive test correctly identifies patients do who have the disease in question. Tests with high sensitivity are ideal screening tests to discover as many patients as possible with the disease, frequently a tradeoff of increased false positive results. **Confirmatory testing may require a more specific test.** Sensitivity Formula - To calculate sensitivity the number of patients who do have the disease and test positive (true positive = TP) is divided by all who have the disease, including those who falsely test negative (false negative = FN) - TP/(TP + FN) Specificity - Specificity refers to the ability of testing to recognize patients who do not have the disease. - For example, D-Dimer has high sensitivity and will be positive in most cases of PE; however, this comes at the cost of a high false positive rate due to low specificity. A confirmatory, more specific, imaging test may be required to make the diagnosis. Specificity Formula - To calculate specificity, the number of patients who test negative and do not have the disease (true negative = TN) is divided by the total number without the disease, including those who falsely test positive (false positive = FP). - TN/(TN + FP) SPIN & SNOUT SPecific test rule IN disease (SPIN) while SeNsitive tests rule OUT disease (SNOUT). Positive Predictive Value (PPV) - Positive Predictive Value (PPV) reports the probability that a patient has the disease after testing positive for it. Positive predictive value is markedly dependent on the prevalence of the disease in question. - TP/(TP + FP) Negative Predictive Value (NPV) - Negative predictive value (NPV) describes the probability that a patient does not have the disease following a negative test result. Both positive and negative predictive values are dependent on the prevalence or pretest probability prior to testing. - TN/(TN + FN) Pretest Probability Pretest probability percentage represents them probability of a specific pathology for a patient prior to initiating further diagnostic testing. Pretest probability may be the prevalence of the disease in question in the population. At any point in the diagnostic work up, the clinician may pause and estimate the prevalence or pretest probability of disease in light of what information is known about the patient. The pretest probability of clinical gestalt is frequently delineated as low, intermediate, and high probabilty. Positive Likelihood Ration - The positive likelihood ratio is the likelihood that a patient with the disease tests positive compared to the likelihood that a patient without the disease tests positive. If a test result is positive and the likelihood ratio is greater than 1, then it is more likely than chance that the patient has the disease. However, if the likelihood ratio for the test is less than 1, then it is less likely the patient has the disease. Negative Likelihood Ratio - The negative likelihood ratio is the likelihood that a patient with the disease tests negative compared to the likelihood that a patient without the disease tests negative. Five Densities of Radiographic Densities 1. Air ([MOST RADIOLUCENT] blackest - least dense) 2. Fat 3. Water (soft tissue) 4. Mineral (Bone) 5. Metal ([MOST RADIOPAQUE] - whitest- MOST DENSE) **Listed from least to most dense** How does air appear on x-ray? - Air appears the blackest on radiograph *ABSORBS THE LEAST XRAY* How does fat appear on x-ray? - Fat appears as the darkest shade of GREY - **Lighter than air but DARKER than soft tissue/fluid** How do soft tissue and fluids appear on x-ray? - Both fluid and soft tissue have the same density on conventional radiographs. **It is impossible to differentiate blood from muscle inside the heart on x-ray.** How do minerals (specifically calcium = bone) appear on x-ray? - Most dense NATURALLY occurring material - absorbs most of the x-ray - lightest shade of grey. How does metal appear on x-ray? - Metal is the most dense material viewed on x-ray - absorbs all of the x-ray - BRIGHTEST WHITE What are the diagnostic utilities of radiographic studies in health care? - Diagnostic radiology uses these imaging results to identify a wide range of problems, from broken bones to heart conditions and blood clots. Interventional radiology also uses imaging such as CT scans, MRI and ultrasounds to guide medical procedures. What does USPSTF stand for? - United States Preventive Services Task Force USPSTF Guideline Ratings - Grade A: USPSTF recommends this service. There is a high certainty that the net benefit is substantial; Offer or provide this service. - Grade B: The USPSTF recommends this service There is high certainty that the net benefit is moderate or there is moderate certainty that the net benefit is moderate or substantial; Offer or provide this service. - Grade C: The USPSTF recommends SELECTIVELY offering or providing this service to individual patients based on professional judgement and patient preferences. There is at least moderate certainty that the net benefit is small; Offer or provide this service for selected patients depending on individual circumstances. - Grade D: The USPSTF recommends against this service. There is moderate or high certainty that the service has no net benefit or that the harms outweigh the benefits; Discourage the use of this service. - I Statement: The USPSTF concludes that the current evidence is insufficient to assess the balance of benefits and harms of the service. Evidence is lacking, of poor quality, or conflicting, and the balance of benefits and harms cannot be determined; Read the clinical considerations section of USPSTF recommendation statement. If the service is offered, patients should understand the uncertainty about the balance of benefits and harms. Macule - Description: Flat, in the plane of the skin, nonpalpable - Potential Cause: Drug rash, viral exanthema, syphilis, HIV Papule - Description: Small, solid, raised, palpable - Potential Cause: Viral, allergic reaction, stigmata of endocarditis Nodule - Description: Larger papule, solid - Potential Cause: Erythema nodoscum, fungal or atypical mycobacterial infections Vesicle/Bulla - Description: Fluid-filled blister, usually clear or bloody fluid. - Potential cause: Varicella, HSV, bullous disease, drug eruptions Pustule - Description: Small, blister filled with pus. - Potential Cause: Bacterial infection or super infection. Plaque - Description: Flat, like a macule, but palpable and usually larger; may have secondary changes such as scale or crusting. - Potential Cause: Psoriasis, MCTD, syphilis, atypical drug eruption, malignancy Rosacea - Rosacea is categorized as being one or combination of the following: erythematotelangiectatic, papulopustular, phymatous, and ocular. It is characterized by acneiform inflammation of the central face, with eythema, flushing episodes, telangiectasias, and often papules and pustules. *Usually confined to the face.* - Inpatient treatment: When rosacea flushing has predictable triggers, such as spicy foods, hot drinks, alcohol, caffiene, and extremes in temperature, avoidanceis the best treatment. Rosacea of at least moderate severity is treated with combination therapy, including a topical wash, topical antibiotics, and oral antibiotics. Physical Assessment of the Skin (Order) 1. Ask the patient to change into a gown with the opening in the back and clothes removed except for underwear. 2. Perform hand hygiene. 3. Start by examining the hair and scalp. Note the distribution, texture, and quantity of of hair. Then, using your fingers or a cotton-tipped applicator, separate the hair to examine the scalp from one side to the other. 4. Now inspect the head and neck, including forehead, eyes (including eyelids, conjunctivae, and sclerae), nose, ears, cheeks, lips, oral cavity, and chin. Examination should also include inspection of terminal hair of the eyebrows, eyelashes, and beard. 5. Ask the patient to lean forward and inspect the upper back. 6. Now inspect the shoulders, arms and hands. Inspect the fingernails. Note their color, shape, and any lesions. Longitudinal bands of pigment are normal in people with darker skin. 7. Now inspect the chest and abdomen. You may want to inspect the axillae at this point. 8. Inspect the anterior thighs and legs. 9. Inspect the feet and toes. Inspect and palpate the toenails, and inspect the soles and areas between toes. 10. Inspect the lower back and anterior thighs and legs. 11. Inspect the breasts, axillae, and genitalia, including axillary and pubic hair. Hypersensitivity Reaction Type I - Reaction mediated by IgE antibodies. - Examples: Systemic anaphylaxis and localized anaphylaxis such as hay fever, asthma, hives, food allergies and eczema. Hypersensitivity Reaction Type II - Cytotoxic reaction medicated by IgG or IgM antibodies. - Examples: Blood transfusion reactions, erythroblastosis fetalis, and autoimmune hemolytic anemia. Hypersensitivity Reaction Type III - Reaction mediated by immune complexes. - Examples: Localized Arthus reaction and generalized reactions such as serum sickness, necrotizing vasculitis, glomerulonephritis, rheumatoid arthritis, and systemic lupus erythematosus. Hypersensitivity Reaction Type IV - Delayed reaction mediated by cellular response. - Examples: Contact dermatitis, tubercular lesions, and graft rejection. Urticaria - A cutaneous disorder characterized by the presence of transient, pruritic, erythematous, slightly edematous plaques. Also known as HIVES. - Causes include: physical stimuli, medications, infections, and autoimmune disease. **In many cases the etiology is unknown.** Acute Urticaria - Defined as hives present for less than 6 weeks. Patients should be asked about changes in medications or diet, as well as recent illnesses, such as viral or streptococcal infection. In many instances, there may be no clear cause of urticaria for the patient's history. Urticarial Vasculitis - A rare clinicopathologic entity that manifests as a result of inflammatory injury to the small vessels of the skin. This condition is characterized by chronic or recurrent episodes of urticarial lesions showing features of leukocytoclastic vasculitis on histopathologic specimens. Cholinergic Urticaria - An abnormal and usually temporary vascular reaction of the skin, often associated with sweating, in susceptible individuals subjected to stress, strong exertion, or hot weather. The condition is characterized by small, pale, itchy, papules surrounded by reddish areas. Dermatographia urticaria - A benign dermatologic condition characterized by raised wheals in a distinctive pattern caused by pressure from or scraping by the fingers in a word pattern or design. It is known informally as skin writing because the wheals can be caused by irritation with the fingers in a word pattern or design. Vibratory Urticaria - A rare condition that is characterized by itching, reddish skin and swelling within minutes of local exposure to vibration. Areas of skin that are most exposed to the stimulus (often the hands) are generally more severely affected. Delayed Pressure Urticaria - A form of chronic inducible urticaria characterized by the appearance of wheals and/or angioedema after pressure to the skin. Pressure urticaria may occur immediately after a pressure stimulus or more commonly, in delayed pressure urticaria, after a delay of 4-6 hours. Lesions can be induced by a variety of stimuli including standing, walking wearing tight clothes, or sitting on a hard surface. Pressure urticaria can occasionally be aggravated by heat, aspirin or menstruation. Aquagenic Urticaria - A rare condition in which a person's skin develops red, itchy hives after exposure to water. Chronic spontaneous urticaria (CSU) - Defined by the presence of recurrent urticaria, angioedema, or both, for a period of six weeks or longer. There are several theories regarding the pathogenesis of CSU, none of which have been conclusively established. Roth Spots - Defined as a white centered retinal hemorrhage and are associated with multiple systemic illnesses, most commonly infective endocarditis. - Retinal emboli can cause round or oval hemorrhagic retinal lesions with small white centers. Janeway Lesions - Irregular, nontender hemorrhagic macules located on the palms, soles, thenar and hypothenar eminences of the hands, and plantar surfaces of the toes. They typically last for days to weeks. They are usually seen with the acute form of infective endocarditis. Osler's Nodes - Tender reddish or purplish subcutaneous nodules of the soft tissue on the ends of fingers or toes, seen in subacute bacterial endocarditis and usually lasting only 1-2 days. The nodes represent bacterial embolisms from the infected heart valve. Mnemonic for Hypersensitivity Reactions ACID Type I: Allergic Type II: Cytotoxic Type III: Immune Complex Deposition Type IV: Delayed Test to Evaluate Dyspnea - CXR - EKG - ABG - CBC - CTA - Transthoracic Echocardiogram (TTE) - BNP - Methemoglobin - Carboxyhemeglobin - D-Dimer - PFT - 6 minute walk test - CPET Infective Endocarditis - An acute or subacute bacterial infection of the endocardium or the heart valves or both. The condition is characterized by heart murmur, prolonged fever, bacteremia, splenomegaly, and embolic pneumonia. 3 Most common organisms for IE - S. Aureus - Streptococcus pyogenes - S. Pneumoniae Acute Bronchitis (Respiratory) - Acute inflammation of the mucous membranes of the tracheobronchial tree. Pathophysiologically, acute bronchitis increases airway resistance due to sputum production and airway epithelial inflammation. Patients with acute bronchitis typically present with cough and sputum production and may have rhonchi on exam. - Treatment: Not usually treated with with abx unless the patient has a preexisting lung condition such as COPD. Pneumonia (Respiratory) - An acute inflammation of the lungs, often caused by inhaled pneumococci of the species Streptococcus pneumoniae. The alveoli and brochioles of the lungs become plugged with a fibrous exudate. Pneumonia may also be caused by other bacteria, as well as by viruses, rickettsiae, and fungi. May increase airway resistance due to airway edema. May also lead to decreased compliance of the respiratory system due to regions of lung consolidation. Patients with PNA will note fever, complex pleuritic chest pain, and rales on exam. An infiltrate on CXR often confirms the diagnosis of pneumonia. - Treatment: The mainstays of treatment of PNA are antibiotics and supplemental oxygen. Aspiration Pneumonitis (Respiratory) - Refers to inhalational acute lung injury that occurs after aspiration of sterile gastric contents. Has a very similar physiologic mechanism and clinical presentation to pneumonia, and should be suspected in patients who were obtunded or have swallowing difficulties due to stroke or other neuromuscular problems. Treatment: Although aspiration pneumonitis due to gastric acid does not need to be treated with antibiotics, most clinicians add antimicrobial coverage, particularly if there is an elevation in the patient's temperature or WBCs, as there may be an infectious component due to aspiration of oral or GI flora. Asthma (Respiratory) - A respiratory disorder causing narrowing of the airway that may be due to allergy or hypersensitivity reactions. It is a complex disorder involving biochemical, immunological, infectious, endocrinological, and psychological factors. Patients with asthma often present with complaints of "chest tightness", a sensation attributed to stimulation of airway receptors, and a sensation of an "inability to take a deep breath" and "air hunger", which likely arises from increased drive to breathe and limited inspiratory capacity resulting from hyperinflation. Treatment: Includes bronchodilators and steroids. Chronic Obstructive Pulmonary Disease (COPD) (Respiratory) - A progressive and irreversible condition characterized by diminished inspiratory and expiratory capacity of the lungs. The condition is aggravated by cigarette smoking and air pollution. Treatment: Bronchodilators and steroids; anticholingeric inhalers may be effective in COPD. Stridor (Respiratory) - An abnormal high-pitched musical sound caused by an obstruction in the trachea or larynx. It is usually heard during inspiration. Stridor may indicate several neoplastic or inflammatory conditions, including glottic edema, asthma, diphtheria, laryngospasm, and papillopma. Considered a medical emergency. Treatment: may require emergent intubation or surgical airway. Occasionally, the patient can be temporized with administration of inhaled heliox (a mixture of helium and oxygen). Pleural Effusion (Respiratory) - An abnormal accumulation of fluid in the intrapleural spaces of the lungs. It is characterized by chest pain, dyspnea, adventitious lung sounds, and nonproductive cough. Patients with pleural effusions usually present primarily with complaints of pleuritic chest pain or dyspnea as well as symptoms that relate to the underlying cause of the effusion, that is, cough and fever from pneumonia, abdominal pain and distention from ascites in liver disease, anuria in renal disease, or cachexia from metastatic malignancy. Treatment: Thoracentesis, surgical drainage, or chest tube placement. Aspiration pneumonia - An inflammatory condition of the lungs and bronchi caused by inhaling foreign material or acidic vomitus. Community-Acquired Pneumonia (CAP) - Refers to an acute infection of the pulmonary parenchyma acquired outside of the hospital. Ventilator Acquired Pneumonia (VAP) - Refers to pneumonia acquired within 48 hours after endotracheal intubation. Auspitz Sign - The appearance of small bleeding points after successive layers of scale have been removed from the surface of psoriatic papules or plaques. Collin's Sign - Patients with gallstone pain would attempt to demonstrate this by placing their hand behind the back and thumb pointing upwards. Acute nausea & vomiting - Are associated with acute infections (especially in the GI tract), ingestion of toxins, GI obstruction or ischemia, new meds, pregnancy, or head trauma/ increase ICP. Chronic nausea & vomiting - Usually defined as persistence of symptoms for more than 1 month, suggest partial mechanical obstruction, intracranial pathology, dysmotility such as gastroparesis, metabolic or endocrine etiology, or a psychologic disturbance. [Show More]
Last updated: 1 year ago
Preview 5 out of 23 pages

Loading document previews ...
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Also available in bundle (1)
Click Below to Access Bundle(s)
NR569 Midterm Exam and Final Exam Package Deal (LATEST UPDATE) Questions and Answers (100% Guaranteed Pass)
NR569 Midterm Exam and Final Exam Package Deal (LATEST UPDATE) Questions and Answers (100% Guaranteed Pass)
By Prof. Goodluck 1 year ago
$19
3
Reviews( 0 )
$11.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Jul 25, 2024
Number of pages
23
Written in
All
Additional information
This document has been written for:
Uploaded
Jul 25, 2024
Downloads
0
Views
51