WEEK 14 FLUID AND ELECTROLYTE
Lewis
Chapter 17, pages 285-298 & 308-309
Potter & Perry
Chapter 41 pages 882-910, & 914-915
Adams & Urban
Chapter 36 pages 566-579
Touhy & Jett pp. 92, 140-143
[ATI fund
...
WEEK 14 FLUID AND ELECTROLYTE
Lewis
Chapter 17, pages 285-298 & 308-309
Potter & Perry
Chapter 41 pages 882-910, & 914-915
Adams & Urban
Chapter 36 pages 566-579
Touhy & Jett pp. 92, 140-143
[ATI fundamental book Page 610]
Nursing care of the adult and *geriatric client with body fluid and electrolyte disturbances:
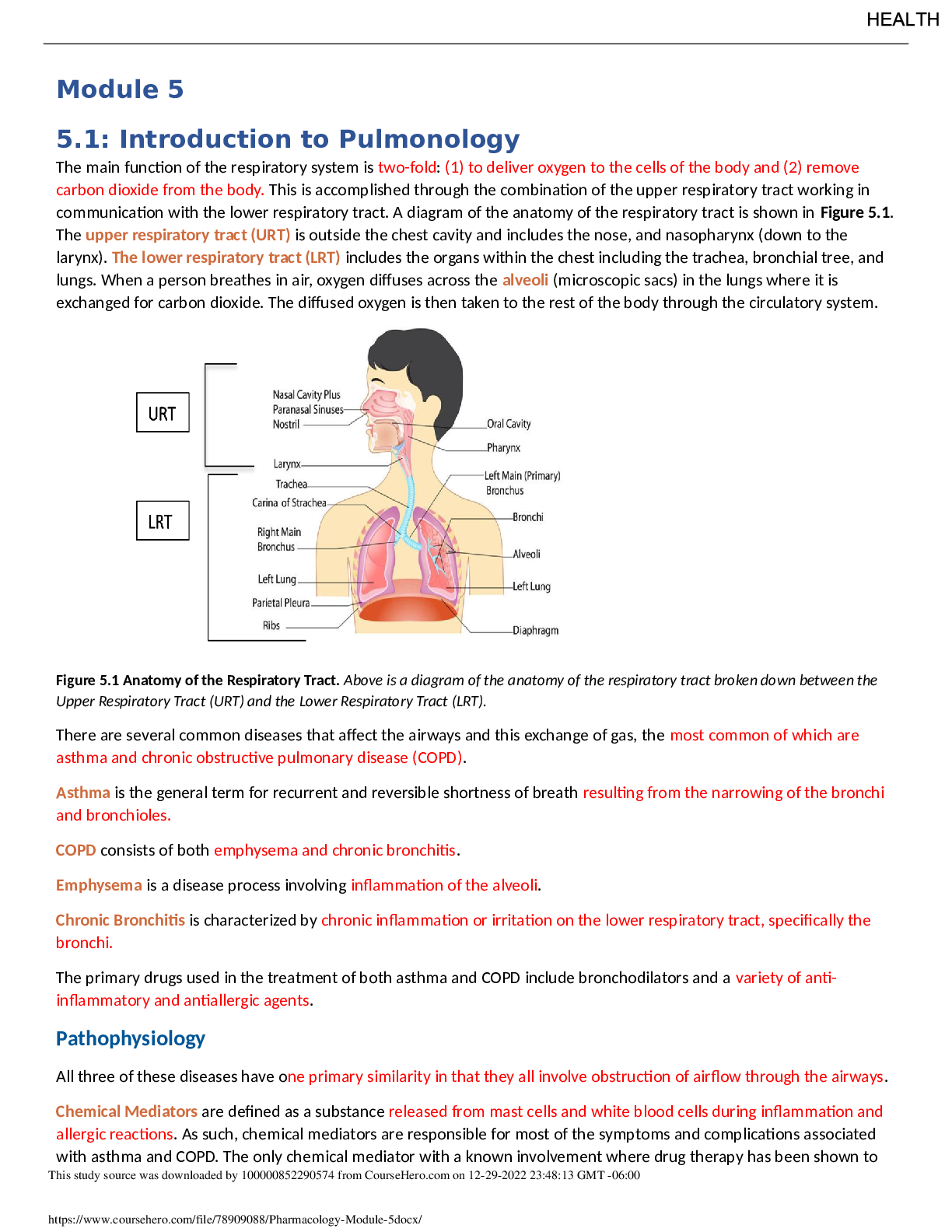
1. Describe the distribution, composition, movement and regulation of body fluids.
• Body fluids and function
o Transportation of nutrients (example oxygen and nutrients to cells)
o Carry away waste products
o Maintain blood volume
o Regulate body temperature
o Homeostasis can be compromised if a fluid or electrolyte problem is not addressed.
• Percent of weight that is fluid
o Infant 75%
o Adult 60%
o Elderly 45%
o To know how much they’re losing or gaining weight
• Average adult’s fluid intake and losses
o Insert chart presentation 1 slide 10
• Clinical applications
o Clients with neurological and psychological problems can be at risk for F&E problems, and infants, children and older adults are particularly vulnerable populations. (note: body fat is essentially free of fluids)
• Compare a client’s intake and output to these normal
o Intake – 30 mL/kg per day
▪ Expect intake to be higher than output (insensible fluid loss)
o Output – 0.5-1.0 mL per kg per day
• There may be additional fluid intake and output needs
o Intake
▪ Iv fluids, IO, irritations, instillations (enemas)
• Thirst mechanism is less acute as we age
• Daily output
o Insensible and sensible loss impacted by illness d/t increased respirations and evaporation from the skin
o GI illness can increase loss diarrhea
• Tremendous turnover
o GU- filtration of 180 L. of plasma to produce 1200-1500 mLs fluid
o GI- 3-6 liters of fluid moves through the GI tract the majority of is shifted to the extra cellular fluid- resulting in 100 to 200 mls in the feces in 24 hours
• Clinical applications
o Output
▪ Emesis
▪ Liquid stool (colostomy & ileostomy)
▪ Drainage- drains
▪ Saturated dressings (1 gram is = to one ml)
• Weight dry dressing (standardized in the industry)
• Weight the wet dressing and subtract the difference which would give you the mLs
• Two major reservoirs
o ICF (inside the cell)
▪ K, Mg, PO higher in ICF than ECF
▪ 45% body weight
▪ fluid within cells
▪ contains substances for F&E balance
▪ essentially the same electrolyte however the proportions are different metabolic chemical reaction take place within the cells
o ECF (outside of the cell)
▪ Na, Cl, HCO3- higher in ECF than ICF
▪ 20% total body weight
▪ fluids outside the cells
▪ intravascular
• blood plasma
• Intravascular fluid is the liquid potion of the blood.
▪ interstitial
• fluid between cells and outside the blood vessels
• Interstitial fluid is located between the cells and outside the blood vessels.
▪ other fluids of ECF
• the lymph system
▪ in constant motion
▪ fluid and electrolytes constantly shifting from compartment to compartment
▪ in order to provide
• tissue oxygenation
• acid base balance
• urine formation
• fluid spacing (DISTRIBUTION SLO)
o distribution of body water
o first space
▪ normal distribution including ICF and ECF
• everything is where it’s supposed to be
o second space
▪ abnormal accumulation interstitial fluid
• example- pulmonary edema
▪ edema can be due to
• increase capillary permeability
o inflammation
• decrease apillary hydraulic pressure
o inflammation
• decreased plasma oncotic pressure
o inflammation
• lymphatic obstruction
o cancer,crutches,
▪ third spacing
• accumulation in a portion of the body not easily exchanged therefore trapped in example burns (trapped inside bubbles), ascites (trapped inside tissues and can’t get it out)
• the body responds as if it is in fluid volume deficit (FVD)
o resulting in tachycardia
o decreased urine out put
▪ possible renal damage
▪ IV solutions used for treatment
• Lactated ringers & 0.9 sodium chloride
▪ Contraindicated IV solutions
• 5% dextrose & 0.45 sodium chloride
• low blood pressure, tachycardia, they are probably dehydrated
• Electrolytes
o Mineral salts
o Electronically charged ions
o Capable of conducting electricity
o Positively charged ions cations
▪ Na, K, Ca, Mg
▪ Cations may be replaced by another cation when one leaves the cell
o Negatively charged ions – anions
o Cl, HCO,PO4, SO4
o Chief ions of ECF Sodium & chloride
o Chief ion of ICF potassium
o Unit of measure
▪ Milliequivalents – mEq/L
▪ Represents the number of grams of the specific electrolyte dissolved in a liter of plasma known as a solute.
▪ The solution in which a solute is dissolved is known as a solvent.
• Fluids
o Direction of flow depends on differences
▪ Hydrostatic pressure greater than colloidal osmotic pressure at the end of the vessels- fluid moves out of cells
• On the way to drop off nutrients
• Higher inside the vessels
▪ If osmotic force is greater than the hydrostatic pressure at the venous end of the fluid reenters the capillary (Edema)
• Lowest in venous system
• Osmotic higher in interstitial fluid
▪
• fluid regulation movement of water and electrolytes
o balance must be maintained
• active transport
o fluid in different compartments contain different electrolytes
o ATP’s must be expended to move E+ across cell membranes against their concentrated gradient
▪ From areas of lower concentration to areas of higher concentration (example sodium potassium pump)
o Example of active transport is the sodium-potassium pump. Which moves Na out of a cell and K into it, keeping ICF lower in Na and higher in K than the ICF.
• Diffusion
o Solvent moves by concentration gradient
o Passive movement of electrolytes or other particles down the concentration gradient. (from areas of higher concentration to lower concentration)
o For example: when a sodium channel in a cell membrane is open, Na diffuses passively across the cell membrane into the ICF b/c concentration is lower in the
ICF. Opening of ion channels is tightly controlled and plays an important part in muscle and nerve function.
• Fluid regulation-diffusion
o Passive movement of electrolytes
o Movement of solvents from areas of higher concentration to areas of lower concentration
o Within a body compartment (example exchange of O2 & CO2 at alveoli)
o When moving across cell membranes require proteins that “serve as ion channels”
• Facilitated diffusion
o Passive mediated transport
o Transport of molecules across a biological membrane via a specific protein
• Fluid regulation osmosis
o Water moved through semi permeable cell membrane
▪ Water can cross but are not permeable to come particles
▪ Osmotic pressure is the inward pulling force
▪ Water moves into the compartment that has a higher osmotic pressure (inward-pulling force)
• Resulting in dilution
• Acities and edema a lot of protein molecules and the body (liver) cant (acities) so the water goes to that area cause there’s a higher concentration
• Osmosis
o Osmotic pressure an inward-pulling force caused by particles in the fluid. The particles already exist in the cell exert ICF osmotic pressure, which tends to pull water into the cell. The particles already in the ICF osmotic pressure, which tends to pull water out of the cell.
o When water moves across the cell membrane (semipermeable). Water moves to into the compartment that has a higher osmotic pressure (inward pulling force) until the particle concentration is equal in the two compartments.
o Example: when a hypotonic solution (more dilute than normal body fluids) is administered IV, it dilutes the interstitial fluid, decreasing it osmotic pressure below intracellular osmotic pressure. Water moves rapidly into the cell until the two osmotic pressures are equal again.
o Example: when a hypertonic solution IV (more concentrated than normal body fluids) causes water to leave the cells my osmosis to equalize the osmolality between interstitial and intracellular compartments.
• Normal plasma osmolarity
o How concentrated or not that it is
o More solvent lower osmolarity
o 275-295 mOm/kg
• Fluid regulation
o classification
▪ hypertonic 296 mOsm/kg
• pulls water from the cell
• associated with cellular shrinkage
• go to the bathroom a lot and cells shinking
▪ isotonic 275-295 mOsm/kg – expands body fluid volume without causing a fluid shift
• usually things stay the same
▪ hypotonic < 274 insufficient solute (particles)
• water excess (dilution of E+)
• associated with cellular swelling
• push fluid back into tissues
• Fluid regulation
o Collodial oncotic pressure
▪ Keeps fluid within the intravascular compartment
▪ Water is attracted to large protein molecules (albumin) with in the vascular system and therefore stays with in the vascular system
o Active transport
▪ Requires energy
o Filtration
▪ Water and diffusible substances move together in response to fluid pressure
•
2. Describe the regulation and movement of major electrolytes: Na and K.
• Sodium 135-145 mEq/L
o Responsible for body water and nerve function
o Most plentiful electrolyte in the ECF
• Potassium 3.5-5 mEq/L
o Major ICF cation
o 98% stored in the ICF
o plays a role in acid base balance
▪ H & K shift back and forth between ECF & ICF
o ECF K+ is responsible for maintenance of action potentials in muscles, neurons and other tissues.
o Important to response of cardiac muscle
o Involved in controlling intracellular osmolality
o Kidneys eliminate approximately 90%
o Tissues drama may release additional K
o Dietary sources
3. Describe common disturbances in fluid and electrolytes.
• NANDA
o Risk for deficient fluid volume
o Deficit fluid volume
o Risk for imbalances fluid volume (isotonic FVD; fluid volume deficit)
▪ Water and electrolytes are lost
▪ Etiological factors
▪ Defining characteristics
o Excess fluid volume (fluid and sodium retained in isotonic proportions)
• Acid base balance
o Chemical balance maintained by the regulation of acids and bases
o Body needs to maintain pH of 7.35 to 7.45
o Body compensates without our knowledge
▪ Breathing out CO2.
▪ Urinary system buffering system
▪ About 7 –not optimal
▪ Can measure through the ABG
o When body is unable to compensate, its when symptoms occur
o
o Temperature warmer people drop off oxygen a little better (to shift curve to the right)
o Calming people down and breathing a little more normal
▪ breathing out a lot of CO2 will move it to the left (acid)
4. Compare and contrast fluid dehydration and fluid overload. (slide 37, ppt. 3)
• Extracellular fluid deficits
o ECF fluid outside the cells
o FVD may occur alone of in combination with other deficits
o FVD basic changes
▪ Isotonic fluid loss [balance, what goes in is the same as there or what was loss is the same as what we’re replacing] [most common is 0.9% NaCl
( NS)]
• Solute & fluids lost in proportional amounts
• Serum osmolality remains the same
▪ Hypertonic dehydration –rarely ever used as RNs wouldn’t be testing much on them since not using a lot. Acute neuro units with increased ICP. (3% Saline, Manitol)
• More water is lost than solute creating a fluid volume deficit & increase in osmolality (concentration gradient. How many particles dissolved in the blood) more water than solutes, more osmolality. Vice versa.
• Can actually full fluid off and get rid of fluid.
▪ Hypotonic dehydration (need to hydrate and push fluid into tissues) hypotonic for short term, then switch to isotonic solution
• greater loss of electrolytes- leading to a < osmolality
o Etiological factors
▪ Water loss
• Insensible
o Fever, increased respiration
• Sensible
o Sweating, loss of 0-1000 mls/hr, sodium imbalance may occur as well.
▪ Urine
• Polyuria
o Hyperglycemia (issue with FVD), hyperosmolar coma, head injury would cause extra ADH secretion. DKA (diabetic ketoacidosis) Type 1 – not making insulin Type 2-
▪ Defining characteristics
• Rapid or slow. Milk moderate or severe, weight loss
• Quick review
o < skin & tongue turgor
o < moisture oral cavity
o < urinary output
o > specific gravity
o disrupted BUN
▪ going to increase FVD. Less circulating volume
o change in V/S
o Edema
▪ Etiology
• Fluid overload, compromised regulatory system (CHF), excessive intake of sodium, water intoxication, lymphatic obstruction.
▪ Pathophysiology
• Primary cause is cardiovascular dysfunction (HF), may have increase of ADH secretion
o Third spacing
▪ (Quick review) presents many of the same characteristics as FVD
▪ shift of fluid from the vascular system into a portion of the body that is not easily exchanged with the rest of the ECF (Methany)
▪ Phases**
• Shift-out of vascular system
o Not easily exchanged with ECF
• Return to the vascular system
o Temporary hypervolemia
o Takes 2-10 days to get rid off the body
• Associated with
o Trauma, surgery, burns, intestinal obstruction, inflammation of the abdominal organs, ascites,
• Concern- initially fluid leaves circulation-body will go into FVD mode
• When fluid shifts back-circulatory system may be overloaded.
• Nursing diagnosis deficient fluid volume, risk for deficient fluid volume. Goal? Expected outcome?
▪ Don have all fluid circulating, its stuck in the tissues its in all the wrong
places (stuck in interstitial tissue and back into vascular space) FVD
[ because it all stuck in one place, not circulating, not circulating volume]
o Nursing measures
▪ Assessments
• Take daily weight, I&O, access postural for hypotension, check skin tongue & skin turgor, check specific gravity (high-greater than
1.030 dehydration/concentrated urine), check gag reflex & swallow reflex. (checking hypo reflexes)
▪ Interventions
• Provide oral fluids, IV fluids, antiemetic if indicated, implement aspiration precaution.
5. Compare and contrast hypo and hyper K and Na.
• Hyponatremia
o May result from a gain of relatively more water than salt or loss of relatively more salt than water.
o Excessive dilution condition of interstitial fluid causes water to enter cells by osmosis, cause the cells to swell. (over hydrated this person; going to edemous- generalized) (high blood pressure/tachycardia, normal temp, respiratory increase too much CO2, oxygen sat decrease)
o Sodium levels less than normal
o May be due to a loss of sodium or a disproportionate gain of water
o A severe discrepancy is an indicator of underlying disease
o Etiology
▪ Diuretics
• Water and salt follow each other, peeing out water salt will go
▪ Adrenal insufficiency
▪ GI fluid loss
• Vomit or diarrhea
▪ SIADH syndrome
• In this condition, high levels of the anti-diuretic hormone (ADH) are produced, causing your body to retain water instead of excreting it normally in your urine.
o Clinical manifestations
▪ Apprehension
• Nervousness, anxiety
• Decreased LOC (confusion, lethargy, muscle weakness)
▪ Postural dizziness
• Low blood pressure
▪ Nausea/Vomiting and tachycardia
▪ Fingerprints remaining on sternum
• Generalized edema
▪ Low serum osmolality
▪ Low specific gravity
o NANDAs for hyponatremia
▪ Excess fluid volume, disturbed sensory perception, risk for falls, risk for injury, risk for impaired skin/tissue integrity
o Therapeutic management
▪ Continued monitoring of client
• V/S, I&O, daily weight
▪ Replacement therapies
• -< Na+ with normal volume- water restriction & Tx. With -< volume –NS or LR for ECF replacement
• loop diuretics such as Lasix (lose potassium retain sodium)
▪ restoration of balance
• follow medical orders, important to raise Na levels
▪ protect client from injury, employ dietary interventions, oral replacement TX, client education
• Hypernatremia
o Two causes: loss of relatively more water than salt or gain of relatively more salt than water.
o Serum levels about 245 mEq/L
o To restore equilibrium between ECF & ICF water will shift from the ICF to the ECF resulting in cellular shrinkage/dehydration
o High levels lead to an increase in neurological activity
o In response to high sodium levels in the body uses the thirst mechanism
o Etiology
▪ Age, meds, diet
▪ Increased intake sodium
▪ Decreased intake water
▪ Diarrhea
▪ Water loss d/t fever, hyperventilation, diuretics TX, burns
o Clinical manifestations
▪ Tachycardia
▪ Dry sticky mucus membranes
▪ Thirst
▪ Agitation and hallucination
▪ Nausea/thirst
o NANDAs
▪ Risk for injury, risk for fluid volume deficit, impaired physical mobility, risk for altered mucous membranes
o Therapeutic management
▪ Restoration of normal levels
▪ Monitor of client
• Labs, I&O, weight (can gain weight very quickly). CNS
▪ Decrease sodium intake
• Restrict sodium
▪ Promote sodium excretion
• Hypernatremia with hypovolemia- initially with NaCl IV
▪ Restoration of balance
• Important to gradually reduce > levels d/t sensitive cerebral cells
• 50% of calculated imbalance corrected during the first 12-24 hour with the rest over 1-2 days
▪ maintain safe environment
▪ dietary reduction
▪ Heat stroke
• Slowly increase exposure to hot weather
• Drink cool liquids, water – balances E+solutions
• Limit strenuous exercise on hot days
• Lose porous light colored clothing
• Provide plenty of liquids for the debilitated & the young
• Hypokalemia
o Etiology
▪ BODY HAS DIFFICULTY WITH RAPID SHIFTS
▪ Inadequate intake
• TPN, PPN, malnourished
▪ K wasting diuretics (Lasix/Foromouside)
▪ K Sparring (hydrochlorothiazide)
▪ Starvation
▪ High G+
▪ Increased secretion of aldosterone (heart failure)
o Clinical manifestations
▪ More apparent if lab is 3.0 or less
• Weak therady pulse
▪ ECG changes – PVCs
• Digoxin toxicity abnormal wave after a T wave
▪ > effects of digoxin
▪ muscle weakness
▪ 40 mEq/ liter
▪ Replacement TX PO
• Daily prophylactic dose in 20 mEq
• Dose may be given more replacement TX
• Take after meals
• Do not use salt substitutes
▪ Client education
• Hyperkalemia
o Elevated serum potassium
o K moves from the ECF to the ICF & increases cell excitability so that cells respond to stimuli of less intensity
o Myocardium is the most excitable tissue
o Etiology
▪ > intake- PO or IV
▪ decreased excretion
• renal problems
▪ massive tissue trauma
▪ GI bleeds
▪ Renal failure
▪ Excrete potassium
• Diuretics or diarrhea
o Clinical manifestations
▪ Irregular, slow heart beat (v-fib)
▪ Muscle weakness, paralysis, respiratory failure
▪ GI hyper motility
▪ Abdominal cramping
▪ Diarrhea
▪ Muscle cramps
▪ Irritably
o NANDAs
▪ Risk for injury r/t muscle weakness & SZ, risk for decreased cardiac output r/t dysrhythmias, altered nutrition r/t decreased renal function, diarrhea related to neuromuscular changes and irritability
o Therapeutic management
▪ Assessments
• Monitor for > 5.0 mEq/L, ECG, metabolic acidosis
▪ Decreased K+ intake
▪ Promote K+ excretion
▪ Restoration of balance
• Dialysis (renal patients)
▪ Medication Tx
• Kayexalate
o Causes diarrhea
• Sorbitol
• Ca. gluconate (to antagonize effect of K+ ion myocardium_
• Regular insulin
• Diuretic TX- K+ wasting i.e. thiazide
▪ Client education
6. Identify the variables affecting normal fluid and electrolyte balance.
• Fluid intake
o Thirst
▪ Mechanism diminishes with age
o Hypothalamus
▪ Osmoreceptors respond to hypovolemia
• Fluid distribution
o Movement of fluid among various compartments
o Between extracellular and intercellular spaces
o Fluid move between the vascular and interstitial compartments by filtration
• Fluid output
o Includes skin, lungs, GI
o Urine formation
▪ 0.5-1.0 mL per kg per hour
▪ rennin angiotensin
o factors affecting glomerular filtration
▪ age, intake, medical conditions, medications may impact HEAD INJURIES
• osmolality
• selective retention of needed substances
• response to pH changes acid/base
• Hormones
o Antidiuretic hormone (ADH)
▪ Regulates osmolality (fluid measure - # of particles per kg of water)
▪ Synthesized by the neurons in the hypothalamus
▪ Influence how much water is excreted via urine
▪ Causes renal cells to reabsorb water
▪ Activation can occur
• Severe dehydration, hemorrhage
o Aldosterone
o Atrial natriuretic factor (ANF)
▪ Atrial natriuretic peptide (ANF)
▪ Cells of the atria (heat) release ANP when stretched
▪ ANP-inhibits ADH results in loss of sodium and water into the urine
• Causes you to pee
o Rennin-Angiotensin-Aldosterone system
▪ Regulated ECF includes how much sodium and water are excreted via urine
▪ Contributes to the regulation of blood pressure
▪ Rennin- acts on angiotensin I which then activated Angiotensin II (by pulmonary enzymes)
▪ Angiotensin II vasoconstriction, aldosterone
▪ Aldosterone reabsorption of sodium and water, increases urinary excretion of potassium and hydrogen
7. Describe laboratory studies associated with fluid and electrolyte imbalances.
8. Utilizes the nursing process to assess identify, plan and implement, and evaluate care of the adult and geriatric clients with fluid and electrolyte imbalances.
• Clinical assessment
o 1. State of hydration LOC
o 2. I&O
▪ do not over look
• Intake irrigations (PEG,PEJ, gastric tubes, patency checks), PO,SQ, IV, feedings
• Output wounds, drainage tubes, pressure ulcers stool & urine.
Remember intake should be slightly ahead of output (d/t insensible water loss)
• Lack of fluid can lead to pain-joint pain, etc.
• TPN (IV and feedings morphed) always administered through central line and higher risk for infection. Bag usually hangs for 24 hours. People who are resting their GI system (Chron’s, colitis)
• PPN (IV & feedings morph)
o 3. Urine output
▪ Normal 0.5-2 mL / kg
▪ Hypovolemia Oliguria (small amounts of urine coming out)
▪ Increased output
o 4. Skin turgor
▪ Forehand looking for tenting
▪ Older adults on clavicle (already lacking elastin and collagen wrinkles)
▪ Depends on the interstitial fluid volume
▪ Also measures skin elasticity
▪ FVD- results in decrease in skin turgor- stays longer
▪ Difficult to assess in patients over 55
o 5. Tongue turgor
▪ normal hydration one longitudinal furrow
▪ FVD- added furrows and tongue is smaller
▪ Hypernatremia – tongue will be red & swollen (FVD)
o 6. Oral cavity
▪ dry mouth may be d/t FVD or mouth breathing
• lips are the easiest to see (cracking). Stringy mucous thicker and viscous
▪ pockets of moisture if client is mouth breathing
▪ hypernatremia- dry sticky membranes
o 7. Body weight
▪ A pound if about 454 grams
▪ 1 liter if fluid – 2.2 pounds or 1 kg
▪ weight gain of 3 pounds can occur over 2-5 days
▪ remember to weight daily (same time of day, same scale, same amount of clothing, before breakfast and after voiding)
▪ multiple your weight by that percentage and that’s how many pound you
need to lose to have those losses. (convert them to pounds) (Edema will be looking at sevre FVE)
▪ Rapid 2% loss mild FVD
▪ Rapid 5% loss moderate FVD
▪ Rapid 8% loss severe FVD
▪ Rapid 2% gain mild FVE
▪ Rapid 5% gain mild FVE
▪ Rapid 8% gain severe FVE
▪ CHF, renal patients, dialysis patients,
▪ *need to know the impact on what its going to have on somebody
o 8. Thirst
▪ subjective symptom
▪ d/t concentration of extracellular fluid
▪ pulling liquid from the cells in the thirst control center (via osmosis)- resulting thirst
▪ remember there is a decreased perception of thirst in individuals over the
age of 60
▪ individuals that are debilitated or have neurological dysfunction may not be able to respond to thirst
▪ baroreceptors in the carotid triggers thirst then goes to hypothalamus
o 9. Tearing and salivation
▪ decreases with dehydration
▪ not making much saliva anymore
o 10. Skin
▪ FVD- skin is cool and pale d/t vasoconstriction
▪ Fight or flight shunt blood and fluid to the core.
▪ Turgor
• Important to access in an age appropriate manner for example the sternum for seniors
o 11. Facial appearance
▪ FVD- pinched appearance, eye sunken back, no pockets
▪ Decreased intraocular pressure- eyes appear sunken and soft to touch
▪ FVE-swollen
▪ Anaphylactic shock & acities sends a lot of fluids and nutrients to get ride of the things to get rid of
o 12. Edema
▪ excessive accumulation of interstitial fluid, does not become apparent until the interstitial volume has increased by 2 and a half to 3 liters. May be localized or systemic.
▪ Causes
• Increased capillary permeability (inflammatory response, sickness, acute disease response) , increased capillary hydraulic pressure(inflammation-natural response) , decrease oncotic pressure(tissue pushing back), lymphatic obstruction
▪ Dependent edema
• Seen in lower extremities of ambulatory patients or in the sacral area of clients on bed rest
• Probably have mild to moderate FVE anda the body is not
managing the extra fluid. Its not going back to the heart and circulating around the body
▪ Generalized edema
• Spread throughout the body, may accumulate in the periorbital tissues or in the scrotum. Remember – this impacts internal organs as well.
• Fluid being dumped anywhere in the body
• Also going on inside the body as well
▪ After removal of pressure the skin returns to normal. 1+ pitting = Na content has increased by approx. 400 mEq. graded on how many mm it goes in. twice the width if finger nail is 2x more 4+ 1600 mEq sodium content increased
▪ Note there is no peripheral edema when only water is retained ( as in excessive ADH secretion) only cellular swelling ( which would be noted by pressing one’s finger over the sternum and producing a visible finger print)
▪ Pulmonary edema
• Cardiogenic- causes > alveolar fluid
o Not getting oxygen- hypoxia
• Noncardiogenic causes interstitial edema
o Renal failure where fluid goes in the body and the pathways
▪ Third spacing
o 13. Body temperature
▪ Hypernatremia – elevation of body temp, up to 105 F, d/t excessive water loss. Insufficient fluids for perspiration.(marathon runners) Dehydration has an affect on hypothalamus ( elevated temperature and have to wonder why, look for dehydration)
▪ Note: temp elevation between 101-103F (get them more fluid, because body is burning off fluids) increases the 24 hours fluid requirements by 500 mLs. d/t temp greater than 103F increases demands by 10000 mls per day.
▪ Isotonic FVD slightly hypothermic (cool room) moderate FVD 97F- 99F. rectal severe FVD 95-98F
• Decreased basal metabolic rate, everything starting to slow down
and die.
o 14. Pulse
▪ FVD. Hypokalemia – tachycardia (weaker pulse) – body is trying to get rid of the fluid down to the kidneys to get rid of it
▪ Hyperkalemia- bradycardia
▪ Potassium imbalance magnesium deficit – irregular pulse
• PVC-premature ventricular contraction
▪ FVE- full or bounding pulse (also tachycardia)
o 15. Respirations
▪ Deep rapid respirations compensation for metabolic acidosis. Can cause alkalosis (going on too long) [ stress, anxiety, fear]
▪ Slow shallow compensation for metabolic alkalosis. Disorder causing respiratory acidosis (increase CO2) [opioids/dying ]
▪ Hypokalemia, hyperkalemia weakness or paralysis of respiratory system
▪ FVE rales in the absence of cardiopulmonary disease
o 16. Blood pressure
▪ intravascular volume deficit, orthostatic hypotension hypotension, drop of 15 mmHg [laying to standing 2 min in-between], increase pulse of 15 bpm
▪ fluid volume excess hypertension [causing extra pressure]
o 17. Neck veins (FVE)
▪ built in manometer for CVP
▪ place the patient in semi fowlers
• neck straight and upper chest
• measure the level to which the veins are distended
o reported as cm. above or below sternal angle.
▪ Expected pt. supine, external jugular fills to sternocleidomastoid muscle
▪ Decreased plasma volume pt. supine, flat neck veins
▪ WNL pt. at 45 degrees, venous distension do not extend higher then 2 cm. above sternal angle
▪ Elevated venous pressure (seen in sever heart failure) at. At 45 degrees,
distended neck veins from the portion of the sternum to the angle of the jaw.
• JVD +1, 2, 3, 4 how many finger will occlude vein
o 18. Hand veins
▪ Expected elevation of the hands causes the hand veins to empty in 4-5 seconds, placing the hand in dependent position-takes hand vein 3-5 seconds to fill [ trick to learn when starting IVs)
▪ Decreased plasma volume hand vein take longer then 3-5 seconds to fill when facing down
▪ Increased plasma volume hand veins will take longer then 3-5 seconds
to empty when held up. Peripheral veins are engorged & clearly visible.
o 19. Neuromuscular irritability
▪ hyperflexia accelerated deep tendon reflexes
▪ FVE or FVD
o 20. Other
▪ changes in behavior, sensation fatigue level. (dehydration or overhydrated)
▪ CVP (central nervous pressure)
• Invasive monitoring
• Measurement of right ventricular preload through the superior vena cava and sits there.
• 2-8 mmHg [ want it to be higher with patients with third spacing]
• has a transducer (able to figure out what is normal atmospheric pressure, then close it off and will be able to notice difference between atm pressure and at the end of the tip. Intraabdominal, cranial, central venous pressure, etc.)
9. Discuss hyper, hypo, and isotonic IV solutions.
• Administration of IV fluids
o Replacing fluid and electrolytes
o Correcting acid base imbalance
o Administering medications, blood products and diagnostic aids, administering essential nutrients., maintaining ready access to the venous system.
• Fluids
o Intracellular fluids
▪ Is the fluid inside the cells (up to 46% of an individual’s total weight)
• Metabolic chemical reactions take place in the cell
• Usually cant access it.
o Extracellular fluid
▪ Is the fluid surrounding the cells
• Plasma, interstitial fluid & the lymph system ( blood stuff around cells )
o Over hydration
▪ Water gained exceeds the amount of water lost
• Edema occurs
o Dehydration
▪ Water loss exceeds the water gained
• Loss of more than 20% may result in death
o Osmolality
▪ Determined by the number of dissolved particles sodium, urea and glucose per kg of water.
▪ Normal serum 280-295 nOsm/ kg
▪ Go up- dehydration
▪ Go down-FVE
• Electrolytes
o Intracellular electrolytes
▪ Potassium, magnesium & phosphate
o Extracellular fluids
▪ Sodium, chloride an bicarbonate (need to know where they are)
• Thirst
o Subjective, decrease in saliva, desire to drink, less acute in older clients (when they recognize that they are thirsty, significant fluid deficits ay be present)
• IV therapy
o Evaluation of plasma sodium levels, potassium levels, serum osmolality and current disease state must be taken into account. (usually check in the morning) (potassium replacements once a day)
o Osmolality refers to the total solute concentration,
o The number of solutes determines osmotic pressure.
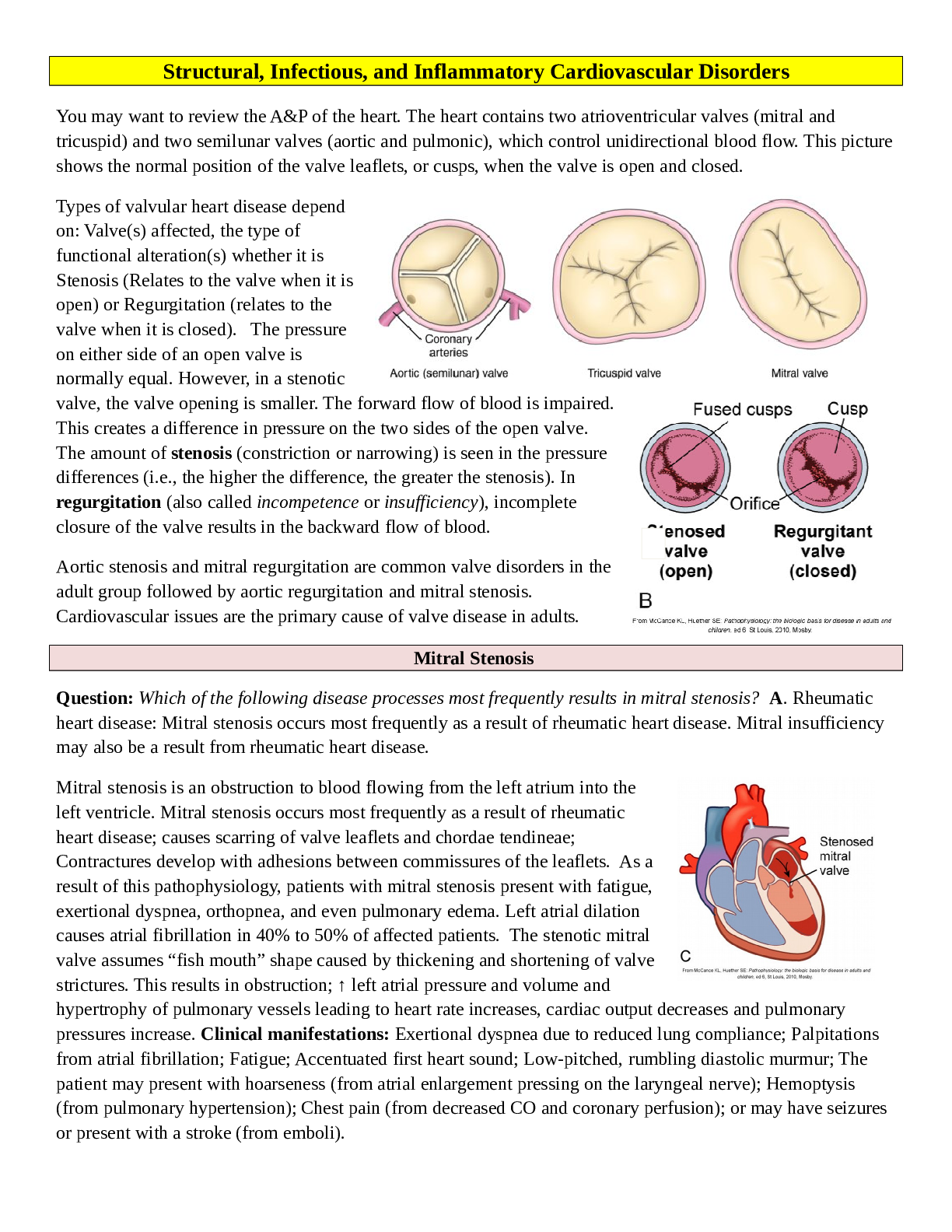
• Crystalloids
o Most commonly administered solutions. (Colloids- blood clotters)
• Isotonic crystalloids (keep things the same) #1 given most common at the hospital
o Increase total fluid volume but depending on the composition of the fluid-that is the compartment that will be affected the most
o Expands that circulating intravascular fluid
o Used to treat fluid loss such a vomiting and diarrhea and low blood pressure.
o The osmotic pressure in the intra and extra vascular compartments are equal.
▪ Normal Saline (most common given used to expand vascular fluid)
• Example –used for dehydrated clients with low BP.
• Used for administration of blood products
• Treatment for 3rd spacing
▪ Lactated ringers
• May be used for clients in metabolic acidosis (increased in carbonic acid/CO2 when acidotic)
▪ 5% dextrose in water (becomes isotonic shortly after infusion)
• provides 170 calories per liter
• 240-340 mOsm/L
▪ 5% dextrose in O2% saline (rarely give)
• Hypertonic crystalloids
o raises the osmolality of the plasma and expands plasma volume by drawing water form cells and tissues.
o Used to relieve cellular edema = esp. cerebral edema
▪ 5% dextrose in normal saline
▪ 5% dextrose in lactated ringers.
▪ (3% saline and mannitol also)
o When patients are dehydrated and have hypertonic plasma- these solutions can cause water to shift into the cells (once the dextrose is metabolized and the solutions becomes hypotonic)
• Hypotonic crystalloids
o (pushing fluid into cells and cells swell up) [half NS main one to give. ]
o simple osmosis. High to low
o Lower the serum osmolality causing water to move out of the plasma to the tissues and cells in the intracellular compartment
o These solutions are indicated for clients with hypernatremia and cellular dehydration
o Concern- not to cause problematic decrease in intravascular compartment which could lead to a drop in BP or peripheral edema.
o Suggested use for dehydrated clients with normal pressure 0.45 sodium chloride
• Plain 5% dextrose: over hydration [being used much less and less now]
o Behavior changes
▪ Older adults are more vulnerable
• Lethargy, confusion, increased tiredness, muscle twitching, nausea, weight gain.
▪ Treatment for withhold fluids until excess fluids excreted, if severe small amounts of of hypertonic solutions administered (3% NaCl)
• TABLE IN ADAMS & URBAN 36.3
• Selected Crystalloid IV solutions
• Drug • Tonicity
• Normal Saline (0.9% NaCl)* • Isotonic
• Lactated Ringer’s* • Isotonic
• Plasma-Lyte 148 • Isotonic
• Hypotonic Saline (0.45% NaCl)*
• (Half normal saline) • Hypotonic
• Plasma-Lyte 56 • Hypotonic
• Hypertonic Saline (3% NaCl) • Hypertonic
• DEXTROSE SOLUTION •
• 5% dextrose water (D5W)* • Isotonic
• 5% dextrose in 0.2% Saline • Isotonic
• 5% dextrose in Normal Saline • Hypertonic
• 5% dextrose in Lactated Ringers* • Hypertonic
• 5% dextrose in Plasma-Lyte 56 • Hypertonic
•
• Nursing considerations
o Types of fluid (prolonged administration of plain D5W)
o Tubing and bag must be changed per hospital and unit protocol
o Rate (MD order & math calculations)
o Rate per hour or per dose of medication, set the pump, manual control of IV
o Injection site
▪ Phlebitis red line streaking up arm
▪ infiltration going through the vein cool leaking
o Systemic shock
o Speed shock—absorbing too quickly
o Air embolism-air going into the line
o Pulmonary embolism –secondary to air embolism
o Pulmonary edema
o runaway IV fluids- rate can be too high
o hematoma –blood building up
o additives-what else we put in the bags
o intake and output
• Nursing implications – why is my patient taking these IV fluids
o It’s important to understand why this client is receiving this IV fluid.
o Administration of IV fluids is one of many interventions to assist our clients with alterations is fluid balance.
10. Discuss assessments for common complications associated with IV therapy. Content:
Nursing care of the client with body fluid and electrolyte disturbances.
• Distribution of body fluids
• Electrolytes: Na/K
o Hyper
o Hypo
o Medications
• Review homeostatic mechanisms regulating fluid volume
• Disturbances in fluid volume
o Dehydration
o Fluid overload
• Laboratory data
o CBC
o Chemistry
o UA
• Discontinuing IV
o Valid order, turn off IV, support catheter, remove tape-pull towards center, 2 by 2 for pressure.
o Slide catheter out and place pressure on site. Apply band aid as needed.
o Need to have order and turn IV off. Cathter in tact.
• Chloride 98-106 mEq/L
o Major extra cellular anion
o Combines to form salts
o Circulates primarily with sodium& assists to maintain cellular integrity by maintaining a balance between ICF & ECF
o Help to control osmotic pressure
o Essential in acid base balance
o Helps internal respiration
▪ Helps drop off the oxygen
• Discuss nursing interventions for a client with fluid and electrolyte imbalance and compare and contrast fluid dehydration and fluid overload
o Risk factors for fluid and electrolyte and acid base imbalance
▪ Age, acute illness, surgery, burns, respiratory disorders, head injuries, decreased intake, chronic illness, cancer, cardiac disease, renal disease, tube feedings, loss of GI fluids (Potter table 41-9)
o Changes associated with aging
▪ Loss body water
▪ Decreased renal function
▪ Skin
• Loses elasticity
▪ Cardiovascular system
• Slows down
▪ Respiratory system
▪ GI
• Not absorbing the fluid that we need
o Tube feedings
▪ Osmolality
▪ Risks
• Tolerance. Dehydration, formula is too concentrated
▪ Interventions
o Surgical patient
▪ Preop- NPO; for an extended period of time, they run the risk of dehydration. Prepping for GI procedure to cleanse their system out, it will add to their dehydration.
▪ Postop- stress, FVD (most likely immediately), FVE (not urinating after procedure and their receiving fluids), hyponatremia, shock (lack of oxygen to tissues and organs)
o Medications
▪ Any therapy or treatments that can impacts F&E (Potter BOX 41-3)
▪ Diuretics, steroids, CNS depressants (narcotics acid//base), antibiotics, nephron toxic, calcium- metabolic alkalosis, MOM, NSAID-nephro toxic (ibuprofen, check kidney function)
Note be sure and review the IV solutions listed below for the exam
0.9 NaCL
0.45 NaCl Lactated Ringers
5% Dextrose in Water
5% Dextrose in Normal Saline
5% Dextrose & 0.2% Normal Saline
5% Dextrose & 0.45 Normal Saline 5% Dextrose & Lactated Ringers Lactated Ringers
I.V. Fluids What Nurses Need to Know
http://journals.lww.com/nursing/Fulltext/2011/05000/I_V fluids_What_nurses_need_to_k now.10.aspx
[Show More]



.png)