*NURSING > EXAM > Chapter 37: The Experience of Loss,Death, and Grief Potter et al.: Fundamentals of Nursing, 9th Ed (All)
Chapter 37: The Experience of Loss,Death, and Grief Potter et al.: Fundamentals of Nursing, 9th Edition ,100% CORRECT
Document Content and Description Below
Chapter 37: The Experience of Loss,Death, and Grief Potter et al.: Fundamentals of Nursing, 9th Edition MULTIPLE CHOICE 1. A nurse encounters a family who experienced the death of ... their adult child last year. The parents are talking about the upcoming anniversary of their child’s death. The nurse spends time with them discussing their child’s life and death. Which nursing principle does the nurse’s action best demonstrate? a. Facilitation of normal mourning b. Pain-management technique c. Grief evaluation d. Palliative care ANS: A Anniversary reactions can reopen grief processes. A nurse should openly acknowledge the loss and talk about the common renewal of grief feeling around the anniversary of the individual’s death; this facilitates normal mourning. The nurse is not attempting to alleviate a physical pain. The actions are of open communication, not evaluation. Palliative care refers to comfort measures for symptom relief. DIF:Apply (application)REF:765 OBJ: Identify the nurse’s role when caring for patients who are experiencing loss, grief, or death. TOP: Implementation MSC: Psychosocial Integrity 2. A cancer patient asks the nurse what the criteria are for hospice care. Which information should the nurse share with the patient? a. It is for those needing assistance with pain management. b. It is for those having a terminal illness, such as cancer. c. It is for those with completion of an advance directive. d. It is for those expected to live less than 6 months. ANS: D Patients accepted into a hospice program usually have less than 6 months to live. Patients with a terminal illness are not eligible until that point. Palliative care provides assistance with pain management when a patient is not eligible for hospice care. An advance directive can be completed by any person, even those who are healthy. DIF:Understand (comprehension)REF:761 OBJ: Discuss the criteria for hospice care. TOP: Teaching/Learning MSC: Psychosocial Integrity 3. A terminally ill patient is experiencing constipation secondary to pain medication. Which is the best method for the nurse to improve the patient’s constipation problem? a. Contact the health care provider to discontinue pain medication. b. Administer enemas twice daily for 7 days. c. Massage the patient’s abdomen. d. Use a laxative. ANS: D Opioid medication is known to slow peristalsis, which places the patient at high risk for constipation. Laxatives are indicated for opioidinduced constipation. Massaging the patient’s abdomen may cause further discomfort. Discontinuing pain medication is inappropriate for a terminally ill patient. Enema administration twice a day is not the best step in the treatment of opioidinduced constipation. DIF:Apply (application)REF:763 OBJ: Describe interventions for symptom management in patients at the end of life. TOP: Implementation MSC: Reduction of Risk Potential 4. A severely depressed patient cannot state any positive attributes to life. The nurse patiently sits with this patient and assists the patient to identify several activities the patient is actually looking forward to in life. Which spiritual concept is the nurse trying to promote? a. Time management b. Reminiscence c. Hope d. Faith ANS: C Hope gives a person the ability to see life as enduring or having meaning or purpose. The nurse’s actions do not address time management, reminiscence, or faith. Time management is organizing and prioritizing activities to be completed in a timely manner. Reminiscence is the relationship by mentally or verbally anecdotally relieving and remembering the person and past experiences. Faith is belief in a higher power. DIF:Apply (application)REF:754 OBJ: Develop a nursing care plan for a patient and family experiencing loss and grief. TOP: Implementation MSC: Psychosocial Integrity 5. In preparation for the eventual death of a female hospice patient of the Muslim faith, the nurse organizes a meeting of all hospice caregivers. A plan of care to be followed when this patient dies is prepared. Which information will be included in the plan? a. Prepare the body for autopsy. b. Prepare the body for cremation. c. Allow male Muslims to care for the body after death has occurred. d. Allow female Muslims to care for the body after death has occurred. ANS: D Muslims of the same gender prepare the body for burial. Muslim faith discourages cremation and autopsy to preserve the sanctity of the soul of the deceased and promote burial as soon as possible after death. DIF:Apply (application)REF:767 OBJ: Develop a nursing care plan for a patient and family experiencing loss and grief. TOP lanningMSC:Management of Care 6. Family members gather in the emergency department after learning that a family member was involved in a motor vehicle accident. After learning of the family member’s unexpected death, the surviving family members begin to cry and scream in despair. Which phase does the nurse determine the family is in according to the Attachment Theory? a. Numbing b. Reorganization c. Yearning and searching d. Disorganization and despair ANS: C Yearning and searching characterize the second bereavement phase in the Attachment Theory. Emotional outbursts of tearful sobbing and acute distress are common in this phase. During the numbing phase, the family is protected from the full impact of the loss. During disorganization and despair, the reason why the loss occurred is constantly examined. Reorganization is the last stage of the Attachment Theory in which the person accepts the change and builds new relationships. DIF: Apply (application) REF: 753 OBJ: Discuss grief theories. TOP: Evaluation MSC: Psychosocial Integrity 7. A nursing assistive personnel (NAP) is caring for a dying patient. Which action by the NAP will cause the nurse to intervene? a. Elevating head of bed b. Making the patient eat c. Giving mouth care every 2 to 4 hours d. Keeping skin clean, dry, and moisturized ANS: B Patients should never be forced to eat so the nurse will intervene to correct this inappropriate behavior. Eating in the last days of life often causes the patient pain and discomfort. Equally, as the body is shutting down the nutrients in food are not able to be absorbed. Therefore, forcing patients to eat serves no beneficial purpose for the patient. All the rest are correct and do not need the nurse to intervene. Elevating the head of the bed is appropriate and will promote ease of breathing and lung expansion and facilitate postural drainage. Giving mouth care will protect membranes if dehydrated, nauseated, or vomiting. Keeping skin clean, dry, and moisturized will decrease skin discomfort and prevent skin breakdown. DIF:Apply (application)REF:763764 OBJ: Identify ways to collaborate with family members and the interdisciplinary team to provide palliative care. TOP: Implementation MSC: Management of Care 8. An Orthodox Jewish rabbi has been pronounced dead. The nursing assistive personnel respectfully ask family members to leave the room and go home as postmortem care is provided. Which statement from the supervising nurse is best? a. “I should have called a male colleague to handle the body.” b. “Family members stay with the body until burial the next day.” c. “I wish they would go home because we have work to do here.” d. “Family will quietly leave after praying and touching the rabbi’s head.” ANS: B Jewish culture calls for family members or religious officials to stay with the body until the time of burial. A male provider is unnecessary. Requesting or expecting the family to go home is not providing culturally sensitive care. Hindus and Muslims usually have persons of the same gender handle the body after death. Buddhists often say prayers while touching and standing at the head of the deceased. DIF:Apply (application)REF:767 OBJ: Describe care of the body after death. TOP: Caring MSC: Psychosocial Integrity 9. A palliative team is caring for a dying patient in severe pain. Which action is the priority? a. Provide postmortem care for the patient. b. Support the patient’s nurse in grieving. c. Teach the patient the stages of grief. d. Enhance the patient’s quality of life. ANS: D The primary goal of palliative care is to help patients and families achieve the best quality of life. Providing support for the patient’s nurse is not the primary obligation when the patient is experiencing severe pain. Not all collaborative team members on the palliative team would be able to provide postmortem care, as is the case for nutritionists, social workers, and pharmacists. Teaching about stages of grief should not be the focus when severe pain is present. DIF:Apply (application)REF:760 OBJ: Identify ways to collaborate with family members and the interdisciplinary team to provide palliative care. TOP: Implementation MSC: Psychosocial Integrity 10. A veteran is hospitalized after surgical amputation of both lower extremities owing to injuries sustained during military service. Which type of loss will the nurse focus the plan of care on for this patient? a. Perceived loss b. Situational loss c. Maturational loss d. Uncomplicated loss ANS: B Loss of a body part from injury is a situational loss. Maturational losses occur as part of normal life transitions across the life span. A perceived loss is uniquely defined by the person experiencing the loss and is less obvious to other people. Uncomplicated loss is not a type of loss; it is a description of normal grief. DIF:Apply (application)REF:751 OBJ: Describe the types of loss experienced throughout life. TOP: Planning MSC: Psychosocial Integrity 11. “I know it seems strange, but I feel guilty being pregnant after the death of my son last year,” said a woman during her routine obstetrical examination. The nurse spends extra time with this woman, helping her realize bonding with this unborn child will not mean she is replacing the one who died. Which nursing technique does this demonstrate? a. Providing curative therapy b. Promoting spirituality c. Facilitating mourning d. Eradicating grief ANS: C The nurse facilitates mourning in family members who are still surviving. By acknowledging the pregnant woman’s emotions, the nurse helps the mother bond with her fetus and recognizes the emotions that still exist for the deceased child. The nurse is not attempting to help the patient eradicate grief, which would be unrealistic. Curative therapy (curing a disease) and spiritual promotion (belief in a higher power or in the meaning of life) are not addressed by the nurse’s statement. DIF:Apply (application)REF:765 OBJ: Develop a nursing care plan for a patient and family experiencing loss and grief. TOP: Implementation MSC: Psychosocial Integrity 12. A patient has had two family members die during the past 2 days. Which coping strategy is most appropriate for the nurse to suggest to the patient? a. Writing in a journal b. Drinking alcohol to go to sleep c. Exercising vigorously rather than sleeping d. Avoiding talking with friends and family members ANS: A Coping strategies may be healthy and effective like talking, journaling, and sharing emotions with others. They may also be unhealthy and ineffective like increased use of alcohol, drugs, and violence. Although exercise is important for selfcare, sleep is also important. Shutting oneself away from friends and family by not talking about the sadness is not effective; the patient should spend time with people who are nurturing. DIF:Apply (application)REF:754 OBJ: Identify the nurse’s role when caring for patients who are experiencing loss, grief, or death. TOP: Implementation MSC: Psychosocial Integrity 13. A female nurse is called into the supervisor’s office regarding her deteriorating work performance since the loss of her spouse 2 years ago. The woman begins sobbing and says that she is “falling apart” at home as well. Which type of grief is the female nurse experiencing? a. Normal grief b. Perceived grief c. Complicated grief d. Disenfranchised grief ANS: C In complicated grief, a person has a prolonged or significantly difficult time moving forward after a loss. Normal grief is the most common reaction to death; it involves a complex range of normal coping strategies. Disenfranchised grief involves a relationship that is not socially sanctioned. Perceived grief is not a type of grief; perceived loss is a loss that is less obvious to other people. DIF: Understand (comprehension) REF: 752 OBJ: Identify types of grief. TOP: Assessment MSC: Psychosocial Integrity 14. A nurse is caring for a patient in the last stages of dying. Which finding indicates the nurse needs to prepare the family for death? a. Redness of skin b. Clear-colored urine c. Tense muscles tone d. Cheyne-Stokes breathing ANS: D Altered breathing such as CheyneStokes pattern, apnea, labored, or irregular breathing is a sign of impending death. Cyanotic, pallor, or mottling of skin occurs. Urine is decreased and a dark color. Decreased muscle tone, relaxed jaw muscles, and sagging mouth also occur. DIF:Apply (application)REF:764 OBJ: Describe interventions for symptom management in patients at the end of life. TOP: Assessment MSC: Psychosocial Integrity 15. The mother of a child who died recently keeps the child’s room intact. Family members are encouraging her to redecorate and move forward in life. Which type of grief will the home health nurse recognize the mother is experiencing? a. Normal b. End-of-life c. Abnormal d. Complicated ANS: A Family members will grieve differently. One sign of normal grief is keeping the deceased individual’s room intact as a way to keep that person alive in the minds of survivors. This is happening after the family member is deceased, so it is not endoflife grief. It is not abnormal or complicated grief; the child died recently. DIF: Apply (application) REF: 752 | 757 OBJ: Identify types of grief. TOP: Assessment MSC: Psychosocial Integrity 16. A nurse is caring for a dying patient. One of the nurse’s goals is to promote dignity and validation of the dying person’s life. Which action will the nurse take to best achieve this goal? a. Take pictures of visitors. b. Provide quiet visiting time. c. Call the organ donation coordinator. d. Listen to family stories about the person. ANS: D Listening to family members’ stories validates the importance of the dying individual’s life and reinforces the dignity of the person’s life. Taking pictures of visitors does not address the value of a person’s life. Calling organ donation and providing private visiting time are components of the dying process, but they do not validate a dying person’s life. DIF:Analyze (analysis)REF:762 OBJ: Identify ways to collaborate with family members and the interdisciplinary team to provide palliative care. TOP: Implementation MSC: Psychosocial Integrity 17. A nurse is caring for a dying patient. When is the best time for the nurse to discuss endoflife care? a. During assessment b. During planning c. During implementation d. During evaluation ANS: A Because most deaths are now “negotiated” among patients, family members, and the health care team, discuss endoflife care preferences early in the assessment phase of the nursing process. Doing so during the planning, implementation, and evaluation phases is too late. DIF:Understand (comprehension)REF:756 OBJ: Identify the nurse’s role when caring for patients who are experiencing loss, grief, or death. TOP: Caring MSC: Psychosocial Integrity 18. A nurse is providing postmortem care. Which action will the nurse take? a. Leave dentures in the mouth. b. Lower the head of the bed. c. Cover the body with a sterile sheet. d. Remove all tubes for an autopsy. ANS: A Leave dentures in the mouth to maintain facial shape. Raise the head of the bed as soon as possible after death to prevent discoloration of the face. Cover the body with a clean sheet. Autopsy often does not allow removal of tubes, equipment, and indwelling lines. DIF:Apply (application)REF:767 OBJ: Describe care of the body after death. TOP: Implementation MSC: Physiological Adaptation 19. A nurse lets the transplant coordinator make a request for organ and tissue donation from the patient’s family. What is the primary rationale for the nurse’s action? a. The nurse is not as knowledgeable as the coordinator. b. The nurse is uncomfortable asking the family. c. The nurse does not want to upset the family. d. The nurse is following a federal law. ANS: D In accordance with federal law, a specially trained professional (e.g., transplant coordinator or social worker) makes requests for organ and tissue donation at the time of every death. Given the complex and sensitive nature of such requests, only specially trained personnel make the requests. Although the nurse may be less knowledgeable than the coordinator, uncomfortable asking the family, or not wanting to upset the family, the primary rationale is to be in accordance with federal law. DIF:Apply (application)REF:765 OBJ: Identify the nurse’s role when caring for patients who are experiencing loss, grief, or death. TOP:EvaluationMSC:Management of Care 20. A patient cancels a scheduled appointment because the patient will be attending a Shivah for a family member. Which response by the nurse is best? a. “When families come together for end-of-life decisions, it provides connections.” b. “We will reschedule so the appointment does not fall on the Sabbath.” c. “Missionary outreach is so important for spiritual comfort.” d. “I’m so sorry for your loss.” ANS: D A death has occurred and saying that you are sorry for their loss is appropriate. The Jewish mourning ritual of Shivah is a time period when normal life activities come to a stop. Those mourning welcome friends into the home as a way of honoring the dead and receive support during the mourning period. Cultural variables can influence a person’s response to grief. It is not when families come together for endoflife decisions. It is not because the appointment fell on the Sabbath. It is not about missionary outreach. DIF:Apply (application)REF:751 OBJ iscuss variables that influence a person’s response to grief. TOP: Caring MSC: Psychosocial Integrity 21. During a followup visit, a female patient is describing new onset of marital discord with her terminally ill spouse to the hospice nurse. Which KüblerRoss stage of dying is the patient experiencing? a. Denial b. Anger c. Bargaining d. Depression ANS: B KüblerRoss’s traditional theory involves five stages of dying. The anger stage of adjustment to an impending death can involve resistance, anger at God, anger at people, and anger at the situation. Denial would involve failure to accept a death. Bargaining is an action to delay acceptance of death by bartering. Depression would present as withdrawal from others. DIF: Apply (application) REF: 753 OBJ: Discuss grief theories. TOP: Assessment MSC: Psychosocial Integrity 22. A previously toilet trained toddler has started wetting again. A nurse is gathering a health history from the grandparent. Which health history finding will the nurse most likely consider as the cause of the wetting? a. Dietary changes b. Recent parental death c. Playmate moved away d. Sibling was sick 2 days ANS: B A child’s stage of development and chronological age will influence grieving. Toddlers can show grief from a loss of parent(s) through changes in their eating patterns, changes in their sleeping patterns, fussiness, and changes in their bowel and bladder habits. It is common for younger children to regress when under increased stress. Siblings being sick, dietary changes, and playmates moving away are unlikely to cause wetting. DIF:Apply (application)REF:753 OBJ iscuss variables that influence a person’s response to grief. TOP: Assessment MSC: Psychosocial Integrity 23. A patient’s father died a week ago. Both the patient and the patient’s spouse talk about the death. The patient’s spouse is experiencing headaches and fatigue. The patient is having trouble sleeping, has no appetite, and gets choked up most of the time. How should the nurse interpret these findings as the basis for a followup assessment? a. The patient is dying and the spouse is angry. b. The patient is ill and the spouse is malingering. c. Both the patient and the spouse are likely in denial. d. Both the patient and the spouse are likely grieving. ANS: D Both are likely grieving from the loss of the patient’s father. Symptoms of normal grief include headache, fatigue, insomnia, appetite disturbance, and choking sensation. Different people manifest different symptoms. There is no data to support the spouse is angry or malingering. There is no data to support the patient is dying or ill. Denial is assessed when the person cannot accept the loss; both talked about the loss. DIF:Analyze (analysis)REF:757 OBJ: Describe characteristics of a person experiencing grief. TOP: Assessment MSC: Psychosocial Integrity MULTIPLE RESPONSE 1. A nurse is documenting endoflife care. Which information will the nurse include in the patient’s electronic medical record? (Select all that apply.) a. Reason for the death b. Time and date of death c. How ethically the family grieved d. Location of body identification tags e. Time of body transfer and destination ANS: B, D, E Documentation of endoflife care includes the following: time and date of death, location of body identification tags, time of body transfer and destination and personal articles left on and secured to the body. Reason for the death is not appropriate; this is a medical judgment and not a nursing judgment. How ethically the family grieved is judgmental and does not belong in the chart. We must remain open to the varying views and beliefs of grieving that are in contrast to our own in order to best support and care for our patients and their families. DIF:Understand (comprehension)REF:766 OBJ: Identify the nurse’s role when caring for patients who are experiencing loss, grief, or death. TOP:ImplementationMSC:Management of Care Chapter 36: The Experience of Loss, Death, and Grief Test Bank MULTIPLE CHOICE 1. A nurse encounters a family that experienced the death of their adult child last year. The parents are talking about the upcoming anniversary of their child’s death. The nurse spends time with them discussing their child’s life and death. The nurse’s action best demonstrates which nursing principle? a. Pain management technique b. Facilitating normal mourning c. Grief evaluation d. Palliative care ANS: B Anniversary reactions can reopen grief processes. A nurse should openly acknowledge the loss and talk about the common renewal of grief feeling around the anniversary of the individual’s death. This facilitates normal mourning. The nurse is not attempting to alleviate a physical pain. The actions are of open communication, not evaluation. Palliative care refers to comfort measures for symptom relief. DIF: Apply REF: 723 OBJ: Identify the nurse’s role when caring for patients who are experiencing loss, grief, or death. TOP: Implementation MSC: Grief 2. A cancer patient asks the nurse what the criteria are for hospice care. What should the nurse answer? a. Having a terminal illness, such as cancer b. Needing assistance with pain management c. Expected to live less than 6 to 12 more months d. Completion of an advance directive ANS: C The criterion for hospice care is being expected to live less than 6 to 12 more months. Patients with a terminal illness are not eligible until that point. Palliative care provides assistance with pain management when a patient is not eligible for hospice care. An advance directive can be completed by any person, even those who are healthy. DIF: Remember REF: 719 OBJ: Discuss the criteria for hospice care. TOP: Implementation MSC: Grief 3. A terminally ill patient is experiencing constipation secondary to pain medication. What is the best way for the nurse to improve the patient’s constipation problem? a. Massage the patient’s abdomen. b. Contact the provider to discontinue pain medication. c. Administer enemas twice daily for 7 days. d. Use a stimulant laxative and increase fluid intake. ANS: D Opioid medication is known to slow gastrointestinal transit time, which places the patient at high risk for constipation. Stimulant laxatives are indicated for opioid-induced constipation. Added water to the diet will allow water to be pulled into the GI tract, softening up stool. Massaging the patient’s abdomen may cause further discomfort. Discontinuing pain medication is inappropriate for a terminally ill patient. Enema administration is not the first step in the treatment of opioid- induced constipation. DIF: Apply REF: 721 OBJ: Describe interventions for symptom management in patients at the end of life. TOP: Implementation MSC: Grief 4. A severely depressed patient cannot state any positive attributes to his or her life. The nurse patiently sits with this patient and assists the patient to identify several activities the patient is actually looking forward to in life. The nurse is helping the patient to demonstrate which spiritual concept? a. Time management b. Hope c. Charity d. Faith ANS: B The concept of hope is vital to nursing; it enables a person to anticipate positive experiences. Being patient and friendly and creating positive relationships are key concepts in all areas of nursing, but especially with depressed patients. The nurse’s actions do not address time management, charity, or faith. DIF: Understand REF: 712 OBJ: Develop a nursing care plan for a patient and family experiencing loss and grief. TOP: Implementation MSC: Grief 5. In preparation for the eventual death of a female hospice patient of the Muslim faith, the nurse organizes a meeting of all hospice caregivers. A plan of care to be followed when this patient dies is prepared. This plan of care would include a. Male health care workers care for the body after death has occurred. b. Body preparation for autopsy. c. Body preparation for cremation. d. Female health care workers care for the body after death has occurred. ANS: D Islamic culture calls for modesty and same-sex caregivers whenever possible. Muslim faith discourages cremation and autopsy to preserve the sanctity of the soul of the deceased. DIF: Apply REF: 725 OBJ: Develop a nursing care plan for a patient and family experiencing loss and grief. TOP: Implementation MSC: Grief 6. Family members gather in the emergency department after learning that a family member was involved in a motor vehicle accident. After learning of the family member’s unexpected death, the surviving family members begin to cry and scream in despair. The nurse recognizes this as the Bowlby Attachment Theory stage of a. Numbing. b. Disorganization and despair. c. Bargaining. d. Yearning and searching. ANS: D Yearning and searching characterize the second bereavement phase in the Bowlby Attachment Theory. Emotional outbursts are common in this phase. During the numbing phase, the family may feel a sense of unreality. During disorganization and despair, the reason why the loss occurred is constantly questioned. Bargaining is part of the Kübler-Ross stages, not of the Bowlby Attachment Theory. DIF: Apply REF: 710 OBJ: Discuss grief theories. TOP: Implementation MSC: Grief 7. After the anticipated demise of a chronically ill patient, the unit nurse is found crying in the staff lounge. The best response to her crying colleague would be a. “It is normal to feel this way. Give yourself some time to mourn.” b. “Your other patients still need you, so hurry back to them.” c. “You’re being a bad role model to the unit’s nursing students.” d. “Why don’t you take a sedative to cope?” ANS: A Nurses often witness suffering on a daily basis. Nurses, as humans, also experience grief and loss when they have been intensely involved in the patient’s suffering and death. Offer comfort and understanding to colleagues, and maintain a stable patient care environment. It is inappropriate to create guilt by telling a grieving nurse to hurry back to her patients or by indicating that she is a bad role model. Suggesting that a colleague take sedative during a shift is dangerous for the safety of patients in her care. DIF: Apply REF: 725-726 OBJ: Discuss the nurse’s own grief experience when caring for dying patients. TOP: Implementation MSC: Grief 8. A family is grieving after learning of a family member’s accidental death. The transplant coordinator requests to talk with the family about possible organ and tissue donation. The nurse recognizes that a. All religions allow for organ donation. b. Life support must be removed before organ and tissue retrieval occurs. c. The best time for organ and tissue donation is immediately after the autopsy. d. The transplant coordinator is working in accordance with federal law. ANS: D It is a federal law to require facilities to develop policies about organ donation. The transplant coordinator has additional education on providing answers about organ donation. Not all religions allow for organ donation. A patient may be on life support during organ removal to preserve organ tissues. Autopsy compromises organ integrity; removal should occur prior. DIF: Apply REF: 723-725 OBJ: Describe care of the body after death. TOP: Implementation MSC: Grief 9. An Orthodox Jewish Rabbi has been pronounced dead. The nursing assistant respectfully asks family members to leave the room and go home as postmortem care is provided. Which of the following statements from the supervising nurse reflects correct knowledge of Jewish culture? a. “I wish they would go home because we have work to do here.” b. “Family members stay with the body until burial the next day.” c. “I should have called a male colleague to handle the body.” d. “I thought they would quietly leave after praying and touching the Rabbi’s head.” ANS: B Jewish culture calls for family members or religious officials to stay with the decedent’s body until the time of burial. A male provider is unnecessary. Requesting or expecting the family to go home is not providing culturally sensitive care. DIF: Apply REF: 725 OBJ: Describe care of the body after death. TOP: Implementation MSC: Grief 10. The palliative team’s primary obligation to a patient in severe pain includes which of the following? a. Supporting the patient’s nurse in her grief b. Providing postmortem care for the patient c. Teaching the patient the stages of grief d. Enhancing the patient’s quality of life ANS: D The primary goal of palliative care is to help patients and families achieve the best quality of life. Providing support for the patient’s nurse is not the primary obligation when the patient is experiencing severe pain. Not all collaborative team members would be able to provide postmortem care, as is the case for nutritionists, social workers, and pharmacists. Teaching about stages of grief should not be the focus when severe pain is present. DIF: Understand REF: 719 OBJ: Identify ways to collaborate with family members and the interdisciplinary team to provide palliative care. TOP: Implementation MSC: Grief 11. A man is hospitalized after surgery that amputated both lower extremities owing to injuries sustained during military service. The nurse should recognize his need to grieve for what type of loss? a. Maturational loss b. Situational loss c. Perceived loss d. Uncomplicated loss ANS: B Loss of a body part from injury is a situational loss. Maturational losses occur as part of normal life transitions. Perceived loss is not obvious to other people. Uncomplicated is not a type of loss; it is a description of normal grief. DIF: Understand REF: 709 OBJ: Describe the types of loss experienced throughout life. TOP: Implementation MSC: Grief 12. “I know it seems strange, but I feel guilty being pregnant after the death of my son last year,” said a woman during her routine obstetrical examination. The nurse spends extra time with this woman, helping her to better bond with her unborn child. This demonstrates which nursing technique? a. Facilitating mourning b. Providing curative therapy c. Promoting spirituality d. Eradicating grief ANS: A The nurse facilitates mourning in family members who are still surviving. By acknowledging the pregnant woman’s emotions, the nurse helps the mother bond with her fetus and recognize the emotions that still exist for the deceased child. The nurse is not attempting to help the patient eradicate grief, which would be unrealistic. Curative therapy and spiritual promotion are not addressed by the nurse’s statement. DIF: Understand REF: 723 OBJ: Develop a nursing care plan for a patient and family experiencing loss and grief. TOP: Implementation MSC: Grief 13. The nurse has had three patients die during the past 2 days. Which approach is most appropriate to manage the nurse’s sadness? a. Telling the next patients why the nurse is sad b. Talking with a colleague or writing in a journal c. Exercising vigorously rather than sleeping d. Avoiding friends until the nurse feels better ANS: B Self-care strategies for nurses include talking with a close colleague and reflecting on feelings by writing in a journal. It is inappropriate for a nurse to talk with patients to resolve the nurse’s grief. Although exercise is important for self-care, sleep is also important. Shutting oneself away from friends is not self-care; the nurse should spend time with people who are nurturing. DIF: Understand REF: 726 OBJ: Identify methods for nurse self-care in grief and loss. TOP: Implementation MSC: Grief 14. A woman is called into her supervisor’s office regarding her deteriorating work performance since the loss of her husband 2 years ago. The woman begins sobbing and saying that she is “falling apart” at home as well. The woman is escorted to the nurse’s office, where the nurse recognizes the woman’s symptoms as which of the following? a. Normal grief b. Complicated grief c. Disenfranchised grief d. Perceived grief ANS: B Complicated or dysfunctional grief occurs when an individual has a complicated grieving process that interferes with common routines of life for excessively long periods of time. Normal grief is the most common reaction to death; it involves a complex range of normal coping strategies. Disenfranchised grief involves a relationship that is not socially sanctioned. Perceived grief is not a type of grief; perceived loss is a loss that is not obvious to other people. DIF: Understand REF: 710 OBJ: Identify types of grief. TOP: Assessment MSC: Grief 15. The father has recently begun to attend his children’s school functions since the death of his wife. This would best be described as which task in the Worden Grief Tasks Model? a. Task I b. Task II c. Task III d. Task IV ANS: C The Worden Grief Tasks Model consists of four tasks. Task III is seen when the surviving family member begins to adjust to life without the deceased. Task I is accepting the reality of the loss, Task II is working through the pain of grief, and Task IV is emotionally relocating the deceased and moving on with life. DIF: Understand REF: 711 OBJ: Discuss grief theories. TOP: Assessment MSC: Grief 16. The mother of a recently murdered child keeps the child’s room intact. Family members are encouraging her to redecorate and move forward in life. The visiting nurse recognizes this behavior as grief. a. Normal b. End-of-life c. Abnormal d. Complicated ANS: A Family members will grieve differently. One sign of normal grief is keeping the deceased individual’s room intact as a way to keep that person alive in the minds of survivors. This is happening after the family member is deceased, so it is not end-of-life grief. It is not abnormal or complicated grief; the child died recently. DIF: Understand REF: 709-710| 715 OBJ: Identify types of grief. TOP: Assessment MSC: Grief 17. Validation of a dying person’s life would be demonstrated by which nursing action? a. Taking pictures of visitors b. Calling the organ donation coordinator c. Listening to family stories about the person d. Providing quiet visiting time ANS: C Listening to family members’ stories validates the importance of the dying individual’s life and reinforces the dignity of the person’s life. Taking pictures of visitors does not address the value of a person’s life. Calling organ donation and providing private visiting time are components of the dying process, but they do not validate a dying person’s life. DIF: Apply REF: 720 OBJ: Identify ways to collaborate with family members and the interdisciplinary team to provide palliative care. TOP: Implementation MSC: Grief 18. A couple is informed that their fetus’ condition is incompatible with life after birth. Nurses can best help the couple with their end-of-life decision making by offering them which of the following? a. An advance directive to complete b. Brief discussion and funeral guidance c. Time and careful explanations d. Instructions on how to proceed ANS: C Families can have limited knowledge when asked to make important ethical decisions. Nurses have the time, patience, and knowledge base to assist the family to understand their ethical situation and to help them make their own educated decision. Advance directives are completed by the person who is dying. Funeral guidance is best provided by a chaplain or a caretaker. DIF: Apply REF: 723 OBJ: Develop a nursing care plan for a patient and family experiencing loss and grief. TOP: Implementation MSC: Grief 19. A correctional facility nurse is called to the scene of a deceased inmate. The correction officer wants to quickly move the body to the funeral home because he is not comfortable with death. The inmate’s body will need to be transported where? a. Coroner’s office for an autopsy b. Police department for an investigation c. Directly to the inmate’s family d. Warden for inspection ANS: A Law often requires that an autopsy be performed if death occurred during incarceration; as the result of foul play, homicide, or suicide; or as an accidental death, as occurs in car accidents. The nurse must understand the policies that are applied in cases of foul play death and must ensure that the decedent’s body is properly cared for after death, despite the emotional feelings of individuals in close contact with the decedent. DIF: Apply REF: 724 OBJ: Describe care of the body after death. TOP: Implementation MSC: Grief 20. A dying patient with liver and renal failure requires pain medication. The nurse anticipates that the medication dose will be a. Given at appropriate milligrams per kilogram medication levels. b. A decreased dose from milligrams per kilogram levels. c. An increased dose from milligrams per kilogram levels. d. Given at midrange for dosing at recommended levels. ANS: B A dying individual will likely have a decline in renal and liver functioning. Because of reduced organ functioning, a decreased dose would be in order, so the individual does not develop toxic levels of the medications. DIF: Apply REF: 720 OBJ: Describe interventions for symptom management in patients at the end of life. TOP: Implementation MSC: Grief 21. A patient cancels a scheduled appointment because she will be attending a Shiva for a family member. Recognizing the importance of this cultural ritual, the nurse’s best comment would be which of the following? a. “Congratulations, what’s the baby’s name?” b. “I’m so sorry for your loss.” c. “Missionary church outreach is so important.” d. “Can I buy a ticket to this fundraiser?” ANS: B The Jewish mourning ritual of Shiva incorporates the community’s helping behaviors toward those experiencing death, sets expectations for behaviors of the survivor, and provides the community with sustaining traditions and rituals. An understanding of the religious and cultural significance of Shiva allows the nurse to know how to appropriately respond. DIF: Apply REF: 709 OBJ: Discuss variables that influence a person’s response to grief. TOP: Implementation MSC: Grief 22. During a follow-up visit, a woman is describing new onset of marital discord with her terminally ill spouse. Using the Kübler-Ross behavioral theory, the nurse recognizes that the spouse is in which stage of dying? a. Denial b. Bargaining c. Anger d. Depression ANS: C Kübler-Ross’ traditional theory involves five stages of dying. The anger stage of adjustment to an impending death can involve resistance, anger at God, anger at people, and anger at the situation. Denial would involve failure to accept a death. Bargaining is an action to delay acceptance of death by bartering. Depression would present as withdrawal from others. DIF: Apply REF: 710 OBJ: Discuss grief theories. TOP: Implementation MSC: Grief 23. Enuresis is reported in a previously toilet trained toddler. While gathering a health history from the grandparent, the nurse asks about which factor as the most likely cause? a. Lack of outside playtime b. Having too many toys c. Dietary changes d. Recent parental death ANS: D A child’s stage of development and chronological age will influence how he or she grieves. Toddlers can show grief through changes in their eating patterns, changes in their sleeping patterns, fussiness or irritability, and changes in their bowel and bladder habits. It is common for younger children to regress when under increased stress. Lack of outside playtime, dietary changes, and having too many toys are unlikely to cause enuresis. DIF: Apply REF: 711 OBJ: Discuss variables that influence a person’s response to grief. TOP: Implementation MSC: Grief 24. Mrs. Harrison’s father died a week ago. Mr. Harrison is experiencing headaches and fatigue, and keeps shouting at his wife to turn down the television, although he has not done so in the past. Mrs. Harrison is having trouble sleeping, has no appetite, and says she feels like she is choking all the time. How should the nurse interpret these assessment findings as the basis for a follow-up assessment? a. Mrs. Harrison is grieving and Mr. Harrison is angry. b. Mrs. Harrison is ill and Mr. Harrison is grieving. c. Both Mr. and Mrs. Harrison likely are in denial. d. Both Mr. and Mr. Harrison likely are grieving. ANS: D Symptoms of normal grief include headache, fatigue, oversensitivity to noise, insomnia, appetite disturbance, and choking sensation. Different people manifest different symptoms. Denial is assessed when the person indicates that he is not accepting that the loss happened. DIF: Apply REF: 715 OBJ: Describe characteristics of a person experiencing grief. TOP: Assessment MSC: Grief Chapter 30: The Experience of Loss, Death, and Grief Potter & Perry: Fundamentals of Nursing, 7th Edition Test Bank MULTIPLE CHOICE 1. A client has a terminal illness and is discussing future treatments with the nurse. The nurse notes that he has not been eating and his response to the nurse’s information is, “What does it matter?” The most appropriate nursing diagnosis for this client is: 1. Denial 2. Hopelessness 3. Social isolation 4. Spiritual distress ANS: 2 A defining characteristic for the nursing diagnosis of hopelessness may include the client stating, “What does it matter?” when offered choices or information concerning themselves. Also, the client’s behavior of not eating is an indicator of hopelessness. The client’s behavior and verbalization do not indicate denial. This is not an example of social isolation. The client is not avoiding or restricted from seeing others. Spiritual distress is not the most appropriate nursing diagnosis for this client. The focus needs to be on the client’s lack of hope. PTS: 1 DIF: A REF: 470 OBJ: Comprehension TOP: Nursing Process: Evaluation MSC: NCLEX® test plan designation: Safe, Effective Care Environment 2. One of the benefits of anticipatory grieving to a client or family is that it can: 1. Be done in private 2. Be discussed with others 3. Promote separation of the ill client from the family 4. Help a person progress to a healthier emotional state ANS: 4 The benefit of anticipatory grief is that it allows time for the process of grief (i.e., to say good- bye and complete life affairs). Anticipatory grief allows time to grieve in private, to discuss the anticipated loss with others, and to “let go” of the loved one. Anticipatory grief can help a person progress to a healthier emotional state of acceptance and dealing with loss. It is not most beneficial for grieving to take place only in private. It is important for grief to be acknowledged by others, and to be able to receive the support of others in the grieving process. Anticipatory grieving can be discussed with others in most circumstances. However, there may be times when anticipatory grief is disenfranchised grief as well, meaning it cannot be openly acknowledged, socially sanctioned, or publicly shared, such as a partner dying of AIDS. The benefit of anticipatory grieving is not so much that it can be discussed in most circumstances, as this discussion can also occur with normal grief when the actual loss has occurred. Anticipatory grief is the process of disengaging or “letting go” that occurs before an actual loss or death has occurred. The benefit is not the separation of the ill client from the family as much as it is the process of being able to say good-bye and to put life affairs in order, and as a result, it can help a client or family to progress to a higher emotional state. PTS: 1 DIF: A REF: 463 OBJ: Comprehension TOP: Nursing Process: Implementation MSC: NCLEX® test plan designation: Safe, Effective Care Environment 3. A newly graduated nurse is best prepared for the assignment of his first dying patient if he: 1. Completed a course dealing with death and dying 2. Is able to control his own personal emotions about death 3. Has previously experienced the death of a dear loved one 4. Has developed a personal understanding of his own feelings about death ANS: 4 When caring for clients experiencing grief, it is important for the nurse to assess his or her own emotional well-being and to understand his or her own feelings about death. The nurse who is aware of his or her own feelings will be less likely to place personal situations and values before those of the client. Although coursework on death and dying may add to the nurse’s knowledge base, it does not best prepare the nurse for caring for a dying client. The nurse needs to have an awareness of his or her own feelings about death first, as death can raise many emotions. Being able to control one’s own emotions is important; however, it is unlikely the nurse would be able to do so if he or she has not first developed a personal understanding of his or her own feelings about death. Experiencing the death of a loved one is not a prerequisite to caring for a dying client. Experiencing death may help an individual mature in dealing with loss, or it may invoke many negative emotions if there is complicated grief present. The nurse is best prepared by first developing an understanding of his or her own feelings about death. PTS: 1 DIF: C REF: 465 OBJ: Analysis TOP: Nursing Process: Implementation MSC: NCLEX® test plan designation: Safe, Effective Care Environment 4. The family of a client with a terminal illness will be able to help provide some psychological support to their family member. To assist the family to meet this outcome, the nurse plans to include in the teaching plan: 1. Demonstration of bathing techniques 2. Application of oxygen delivery devices 3. Recognition of the client’s needs and fears 4. Information on when to contact the hospice nurse ANS: 3 A dying client’s family is better prepared to provide psychological support if the nurse discusses with them ways to support the dying person and listen to needs and fears. Demonstration of bathing techniques may help the family meet the dying client’s physical needs, not in providing psychological support. Application of oxygen devices may help the family provide physical needs for the client, not in providing psychological support for the client. Information on when to contact the hospice nurse is important knowledge for the family to have and may help them feel they are being supported in caring for the dying client. However, contact information does not help the family provide psychological support to the dying client. PTS: 1 DIF: A REF: 474 OBJ: Comprehension TOP: Nursing Process: Implementation MSC: NCLEX® test plan designation: Safe, Effective Care Environment 5. A client that was recently diagnosed with a terminal illness asks his nurse about organ donation. The nurse should: 1. Have the client first discuss the subject with the family 2. Suggest the client delay making a decision at this time 3. Assist the client to obtain the necessary information to make this decision 4. Contact the client’s physician so consent can be obtained from the family ANS: 3 No topic that a dying client wishes to discuss should be avoided. The nurse should respond to questions openly and honestly. As client advocate, the nurse should assist the client to obtain the necessary information to make this decision. The nurse should provide the client with information in order to make such a decision. Although the nurse may suggest that the client discuss this option after having obtained information, it is up to the client to discuss the subject with the family. The nurse should respect the client and provide the necessary information for him or her to make a decision rather than dismissing the client’s question. It is not necessary to contact the physician or the family for consent for organ donation if the client is capable of making this decision. PTS: 1 DIF: A REF: 469-470 OBJ: Comprehension TOP: Nursing Process: Implementation MSC: NCLEX® test plan designation: Safe, Effective Care Environment 6. A client, who is receiving chemotherapy on a medical unit due to a recent diagnosis of terminal cancer of the liver, has an in-depth conversation with the nurse. The client says, “This cannot be happening to me.” The nurse identifies that this stage is associated with, according to Kübler-Ross: 1. Anxiety 2. Denial 3. Confrontation 4. Depression ANS: 2 According to Kübler-Ross, the client is in the denial stage of dying. The client may act as though nothing has happened, may refuse to believe or understand that a loss has occurred, and may seem stunned, as though it is “unreal” or difficult to believe. There is no stage of anxiety in the five stages of dying of Kübler-Ross. There is no stage of confrontation in the five stages of dying of Kübler-Ross. During depression the individual may feel overwhelmingly lonely and withdraw from interpersonal interaction. PTS: 1 DIF: A REF: 464 OBJ: Comprehension TOP: Nursing Process: Implementation MSC: NCLEX® test plan designation: Safe, Effective Care Environment 7. A client who is Chinese American has just died on the unit. The nurse is prepared to provide after-death care to the client and anticipates the probable preferences of a family from this cultural background will include: 1. Pastoral care 2. Preparation for organ donation 3. Time for the family to bathe the client 4. Preparation for quick removal out of the hospital ANS: 3 Some families of Chinese Americans will prefer to bathe the client themselves. They often believe the body should remain intact; organ donation and autopsy are uncommon. Chinese Americans do not prefer pastoral care for after-death care of a family member. Organ donation is uncommon for Chinese Americans. Chinese Americans may desire time to bathe the client. Quick removal from the hospital is not preferred. PTS: 1 DIF: A REF: 466 OBJ: Comprehension TOP: Nursing Process: Implementation MSC: NCLEX® test plan designation: Safe, Effective Care Environment 8. The nurse is providing care to a dying client. Which of the following is the primary concern? The nurse should: 1. Promote optimism in the client and be a source of encouragement 2. Promote dignity and self-esteem in as many interventions as is appropriate 3. Allow the client to be alone and expect isolation on the part of the dying person 4. Intervene in the client’s activities and promote as near normal functions as possible ANS: 2 The focus in planning nursing care is to support the client physically, emotionally, developmentally, and spiritually in the expression of grief. When caring for the dying client, it is important to devise a plan that helps a client to die with dignity and offers family members the assurance their loved one is cared for with care and compassion. Optimism should not be the primary focus when caring for the dying client. The nurse should promote the client’s self-esteem and allow the client to die with dignity. The client does not need to be left alone. The nurse’s or family’s presence may be comforting to the client by showing that he or she is being cared for and is worthy of attention. The client should be allowed to make choices and perform as many activities of daily living independently as possible. This allows the client to maintain self-esteem and dignity. PTS: 1 DIF: A REF: 481 OBJ: Comprehension TOP: Nursing Process: Implementation MSC: NCLEX® test plan designation: Safe, Effective Care Environment 9. There is a different focus for the client with hospice nursing care. The nurse is aware that client care provided through a hospice is: 1. Designed to meet the client’s individual wishes, as much as possible 2. Aimed at offering curative treatment plans intended for client recovery 3. Involved in teaching families and/or caregivers to provide postmortem care 4. Offered primarily for hospitalized clients for whom at-home care is not possible ANS: 1 The nurse’s role in hospice is to meet the primary wishes of the dying client and to be open to individual desires of each client. The nurse supports a client’s choice in maintaining comfort and dignity. Hospice care is for the terminally ill. It is not aimed at offering curative treatment, but rather the emphasis is on palliative care. Hospice care may provide bereavement follow-up for the family after a client’s death, but hospice nurses typically do not teach the family postmortem care. Hospice care is primarily for home care, but a client in a hospice may become hospitalized. PTS: 1 DIF: A REF: 475 OBJ: Comprehension TOP: Nursing Process: Implementation MSC: NCLEX® test plan designation: Safe, Effective Care Environment 10. To provide comfort for the client, while preparing to assist the client in the end stage of her life in response to anticipated symptom development, the nurse plans to: 1. Decrease the client’s fluid intake 2. Limit the use of over-the-counter analgesics 3. Provide larger meals with more appealing seasoning 4. Determine valued activities and schedule rest periods ANS: 4 To promote comfort in the terminally ill client, the nurse should help the client to identify values or desired tasks; then help the client to conserve energy for those tasks. Decreasing the client’s fluid intake may make the terminally ill client more prone to dehydration and constipation. The nurse should take measures to help maintain oral intake, such as administering antiemetics, applying topical analgesics to oral lesions, and offering ice chips. The use of analgesics should not be limited. Controlling the terminally ill client’s level of pain is a primary concern in promoting comfort. Nausea and vomiting and anorexia may increase the terminally ill client’s likelihood of inadequate nutrition. The nurse should serve smaller portions and bland foods, which may be more palatable. PTS: 1 DIF: A REF: 471 OBJ: Comprehension TOP: Nursing Process: Implementation MSC: NCLEX® test plan designation: Safe, Effective Care Environment 11. To maintain the client’s sense of self-worth during the end of life while working with a client in an inpatient hospice unit, the nurse should: 1. Leave the client alone to deal with final affairs 2. Call upon the client’s spiritual advisor to manage care 3. Include regular visits throughout the day into the client’s care plan 4. Facilitate the arrangements to have a grief counselor visit the client ANS: 3 Spending time to let clients share their life experiences, particularly what has been meaningful, enables the nurse to know clients better. Knowing clients then facilitates choice of therapies that promote client decision-making and autonomy. Planning regular visits also helps the client maintain a sense of self-worth, because it demonstrates that he or she is worthy of the nurse’s time and attention. The client should not be left alone to feel abandoned or isolated. Nurses can help clients meet spiritual needs by facilitating connections to a spiritual practice or community and supporting the expression of culturally held beliefs. A client’s spiritual advisor may also be called upon but is not the only source of spiritual support. The nurse who turns care over to the spiritual advisor is not promoting the client’s sense of self-worth, as it may imply the client is not worthy of the nurse’s time or attention. A grief counselor may be requested to visit if the client is experiencing complicated grief. Having a grief counselor visit is not an intervention that will help maintain a client’s sense of self-worth. PTS: 1 DIF: A REF: 477 OBJ: Comprehension TOP: Nursing Process: Implementation MSC: NCLEX® test plan designation: Safe, Effective Care Environment 12. A nursing intervention to assist the client with a nursing diagnosis of sleep pattern disturbance related to the loss of spouse and fear of nightmares should be to: 1. Administer sleeping medication per order 2. Refer the client to a psychologist or psychotherapist 3. Have the client complete a detailed sleep pattern assessment 4. Sit with the client while encouraging verbalization of feelings ANS: 4 A nursing intervention to facilitate grief work is to offer the client encouragement to explore and verbalize feelings of grief. This encouragement refocuses the client on current needs and minimizes dysfunctional adaptation behaviors (e.g., not sleeping) by facilitating resolution of grief through problem-solving skills. Administering sleeping medication may help the client get to sleep but does not resolve the issue of grief. Without addressing the grief, the client may develop another dysfunctional adaptation behavior. It is not necessary to refer the client to a psychologist or psychotherapist at this time. The client needs to be encouraged to verbalize his or her feelings. Having the client complete a detailed sleep pattern assessment may help the nurse identify the number of hours of sleep the client is obtaining, but it does not address the issue causing the sleep disturbance, which is grief from the loss of the spouse. PTS: 1 DIF: A REF: 468 OBJ: Comprehension TOP: Nursing Process: Implementation MSC: NCLEX® test plan designation: Safe, Effective Care Environment 13. To promote comfort for the terminally ill client specific to nausea and vomiting, the nurse should: 1. Provide mouth care 2. Offer high-protein foods 3. Increase the fluid intake 4. Offer a high-residue diet ANS: 2 To promote comfort for the terminally ill client specific to nausea and vomiting, the nurse should administer antiemetics, provide oral care at least every 2 to 4 hours, offer clear liquid diet and ice chips, avoid liquids that increase stomach acidity (such as coffee, milk, and citrus acid juices), and offer high-protein foods in smaller portions and of a bland nature. Oral care should be provided every 2 to 4 hours. Increasing the fluid intake may help prevent constipation. A low- residue diet may help prevent diarrhea. PTS: 1 DIF: A REF: 476 OBJ: Comprehension TOP: Nursing Process: Implementation MSC: NCLEX® test plan designation: Safe, Effective Care Environment 14. A nurse-initiated or independent activity for promotion of respiratory function in a terminally ill client is to: 1. Limit fluids 2. Position the client upright 3. Reduce narcotic analgesic use 4. Administer bronchodilators as needed ANS: 2 Positioning the client upright is an independent nursing intervention for the promotion of respiratory function in a terminally ill client. Limiting fluids may not promote respiratory function, and unless a client is on a fluid-restricted diet, the nurse should not do so. Reducing narcotic analgesic use is not a nurse-initiated activity to promote respiratory function. A respiratory rate should be assessed before administering narcotics to prevent further respiratory depression. Management of air hunger involves judicious administration of morphine and anxiolytics for relief of respiratory distress. The administration of bronchodilators would require a physician’s order. It is not an independent nursing activity. PTS: 1 DIF: A REF: 476 OBJ: Comprehension TOP: Nursing Process: Implementation MSC: NCLEX® test plan designation: Safe, Effective Care Environment 15. The nurse is using Bowlby’s phases of mourning as a framework for assessing the client’s response to the traumatic loss of her leg. During the “yearning and searching” phase, the nurse anticipates that the client may respond by: 1. Crying intermittently 2. Becoming angry at the nurse 3. Acting stunned by the eventual loss 4. Discussing the change in role that will occur ANS: 1 During the “yearning and searching” phase of Bowlby’s phases of mourning, the nurse anticipates the client may have outbursts of tearful sobbing and acute distress. During Bowlby’s “disorganization and despair” phase of mourning, the nurse anticipates the client may express anger at anyone who might be responsible, including the nurse. During the “numbing” phase of Bowlby’s phases of mourning, the nurse anticipates the client may act stunned by the loss. During the “reorganization” phase of Bowlby’s phases of mourning, the nurse anticipates the client may discuss the change in role that will occur. PTS: 1 DIF: A REF: 464 OBJ: Comprehension TOP: Nursing Process: Implementation MSC: NCLEX® test plan designation: Safe, Effective Care Environment 16. The nurse finds a client who has been diagnosed with terminal lung cancer quietly crying. Which of the following nursing responses most reflects a need for additional guidance regarding therapeutic communication with a dying client? 1. “If there is anything I can do to help, just ask.” 2. “Would you like some medication to help you sleep?” 3. “Do you want me to call your wife so you two can talk?” 4. “Try not to be sad; let’s find something to be thankful for.” ANS: 4 Avoid communication barriers such as denying the client’s grief, providing false reassurance, or avoiding discussion of sensitive issues. Remember that a client’s emotions are not something you can “fix.” Instead, view emotional expression as a necessary part of the client’s adjustment to significant life changes and development of effective coping skills. PTS: 1 DIF: C REF: 468 OBJ: Analysis TOP: Nursing Process: Implementation MSC: NCLEX® test plan designation: Safe, Effective Care Environment 17. A terminally ill client shares with the nurse that he, “needs to tell someone what I want when the end comes.” The nurse’s most therapeutic response is: 1. “We can talk about that now if you want to. Let me close the door and pull up a chair.” “I imagine you would like to discuss matters with your primary care provider. I’ll let him 2. know you want to talk.” “Let me finish with my client care, I’ll be back in 10 minutes, and we can talk as long as 3. you need to.” “If you haven’t discussed your feelings with your family yet, I’d suggest you do that when 4. they visit this evening.” ANS: 1 Avoid communication barriers such as denying the client’s grief, providing false reassurance, or avoiding discussion of sensitive issues. When you sense that a client wants to talk about something, make time right then, if at all possible. PTS: 1 DIF: C REF: 469-470 OBJ: Analysis TOP: Nursing Process: Implementation MSC: NCLEX® test plan designation: Safe, Effective Care Environment 18. The wife of a client recently diagnosed with end-stage renal failure shares with the nurse that, “He just accepts this; I want a second opinion.” The nurse recognizes that while the client has reached the acceptance stage of grieving, his wife is experiencing the: 1. Anger stage 2. Denial stage 3. Depression stage 4. Bargaining stage ANS: 1 In the denial stage, a person acts as though nothing has happened and refuses to accept the fact of the loss. The person shows no understanding of what has occurred. When experiencing the anger stage of adjustment to loss, a person expresses resistance and sometimes feels intense anger at God, other people, or the situation. Bargaining cushions and postpones awareness of the loss by trying to prevent it from happening. Grieving or dying people make promises to self, God, or loved ones that they will live or believe differently if they can be spared the dreaded outcome. When a person realizes the full impact of the loss, depression occurs. Some individuals feel overwhelmingly sad, hopeless, and lonely. Resigned to the bad outcome, they sometimes withdraw from relationships and life. In acceptance, the person incorporates the loss into life and finds ways to move forward. PTS: 1 DIF: A REF: 464 OBJ: Comprehension TOP: Nursing Process: Assessment MSC: NCLEX® test plan designation: Safe, Effective Care Environment 19. The mother of a child who was killed in an automobile accident is diagnosed with excessive grief. The nurse realizes that this diagnosis increases her risk of: 1. Attempting suicide 2. Developing anorexia nervosa 3. Becoming chronically depressed 4. Developing a psychiatric phobia ANS: 1 Normal grief responses, when experienced in excess, become overwhelming. People who exhibit very intense emotions and severe symptoms lose control, appear deeply traumatized, or may become suicidal, requiring medication or stabilization before they are able to begin the healing process. Depression is possible but is triggered by a variety of events. Grief is not the typical trigger for either anorexia nervosa or phobias. PTS: 1 DIF: A REF: 463 OBJ: Comprehension TOP: Nursing Process: Assessment MSC: NCLEX® test plan designation: Safe, Effective Care Environment 20. The nurse recognizes that which of the following clients is at greatest risk for complicated (dysfunctional) grief? 1. A 26-year-old who is diagnosed with rheumatoid arthritis 2. The 58-year-old only child whose mother recently died of cancer 3. A teenage parent whose child died of sudden infant death syndrome (SIDS) 4. A 50-year-old diabetic client who has experienced an above-the-knee amputation ANS: 3 Loss associated with homicide, suicide, sudden accidents, or the loss of a child has the potential to become complicated. PTS: 1 DIF: C REF: 463 OBJ: Analysis TOP: Nursing Process: Assessment MSC: NCLEX® test plan designation: Safe, Effective Care Environment 21. Experiencing normal grief over losses allows the adolescent to successfully: 1. Move past the loss 2. Regain a sense of security 3. Develop effectual coping skills 4. Deal with an actual loss later in life ANS: 3 Normal grief experiences often help persons to mature and develop coping methods for dealing with other losses in the future. The remaining options are facets of successfully coping with loss. PTS: 1 DIF: A REF: 463 OBJ: Comprehension TOP: Nursing Process: Evaluation MSC: NCLEX® test plan designation: Safe, Effective Care Environment 22. A client who recently experienced an amputation of the left thumb has a perceived loss of physical attractiveness. The nurse recognizes that such a loss is: 1. More easily assessed than actual losses 2. Much less personal than an actual loss 3. Universally experienced by all amputees 4. Capable of producing grief similar to an actual loss ANS: 4 Perceived losses are easy to overlook because they are so internally and individually experienced, although they are grieved in the same way as an actual loss. The express of grief over a loss, perceived or real, is a very individualized, personal response. PTS: 1 DIF: C REF: 463 OBJ: Analysis TOP: Nursing Process: Assessment MSC: NCLEX® test plan designation: Safe, Effective Care Environment 23. Which of the following nursing assessment data best reflects the successful achievement of the dying client’s right to be pain free? 1. Introducing the client to effective alternative pain management techniques 2. Educating the client on the appropriate use of a patient-controlled analgesia device 3. Pain rated as a 3 out of 10 after the administration of the prescribed pain medication 4. Informed the primary care provider of the client’s need for additional pain medication. ANS: 3 The client is entitled to a pain free death. The most reflective assessment data supporting such a situation is a pain rating of 3 out of 10. The remaining options are all directed toward to that end. PTS: 1 DIF: C REF: 462 OBJ: Analysis TOP: Nursing Process: Assessment MSC: NCLEX® test plan designation: Safe, Effective Care Environment 24. Which of the following interventions best reflects the nurse’s attempt to honor the terminally ill client’s cultural values? 1. Interviewing both the client and the family to identify preferred end-of-life care 2. Talking openly and without biases about the client’s end-of-life care preferences 3. Providing the family with the opportunity to realize the client’s end-of-life wishes 4. Becoming familiar with the death rituals most common among the nurse’s client population ANS: 3 Care provided at the end-of-life within the client and family’s cultural context draws on the resources of their entire lives. Honoring client and family cultural values characterizes expert end-of-life care. Actually facilitating the opportunity to have the client’s wishes fulfilled is the best reflection of expert end-of-life care. The other options are all facets of being successful at facilitating this care. PTS: 1 DIF: C REF: 475 OBJ: Analysis TOP: Nursing Process: Planning MSC: NCLEX® test plan designation: Safe, Effective Care Environment 25. Which of the following statements, made by a nurse regarding the means by which older adults usually express and manage grief, reflects a need for further instruction and clarification? 1. “The greater the loss the greater the sense of grief.” 2. “Managing depression will help the grieving adult cope.” 3. “Having lived a long, happy life makes grieving easier to deal with.” 4. “The longer you live, the more experience you have with grieving a death.” ANS: 3 There is little evidence that grief experiences differ due to age alone. Responses to loss are more likely related to the nature of the specific loss experience. Increased age increases the likelihood that older adults have faced multiple losses—loved ones, friends, valued objects, outliving a child, or declining health. Depression does make dealing with grief more difficult. PTS: 1 DIF: C REF: 478 OBJ: Analysis TOP: Nursing Process: Analysis MSC: NCLEX® test plan designation: Safe, Effective Care Environment 26. A terminally ill client is reporting a sense of anxiety and dyspnea. The nurse’s initial intervention is to: 1. Assess the client’s vital signs and administer the prescribed antianxiety medication Determine the cause of the client’s dyspnea and provide both emotional and physical 2. support Position the client in a semi-Fowler’s position and provide supplemental oxygen via nasal 3. cannula Remain with the client and encourage him to express the concerns he is experiencing 4. regarding his death ANS: 3 Position for comfort and maximal respiratory excursion, provide supplemental O2. Then provide comforting, reduce anxiety or fever; provide effective pain management as appropriate. The initial intervention when a client is experiencing respiratory difficulties, no matter what the potential cause it to facilitate breathing through appropriate positioning and administration of oxygen. PTS: 1 DIF: C REF: 463 OBJ: Analysis TOP: Nursing Process: Implementation MSC: NCLEX® test plan designation: Safe, Effective Care Environment 27. The nurse most effectively addresses the protection of a terminally ill, incontinent client’s skin from irritation and breakdown by: 1. Using adult diapers and changing them as soon as they become wet or otherwise soiled 2. Assessing the client’s bed frequently for wetness and assuring clean, dry linens and clothing Securing an order for an indwelling catheter and keeping the perineal area free of fecal 3. matter Offering the client frequent opportunities to toilet and responding promptly to requests to 4. toilet ANS: 2 Progressive disease and decreased level of consciousness can result in both urinary and fecal incontinence. The most effective means of protect skin from irritation or breakdown is by maintaining dry linens and clothing. The remaining options are not inappropriate, but a client may not be able to respond to the need to urinate or defecate. While adult diapers and an indwelling catheter are viable interventions, the client must still be provided with care that ensures that skin will be clean and dry. PTS: 1 DIF: C REF: 476 OBJ: Analysis TOP: Nursing Process: Implementation MSC: NCLEX® test plan designation: Safe, Effective Care Environment 28. In order to most effectively address the discomfort of limited oral fluid intake for a client in the latter stages of the dying process, the nurse should: 1. Provide mouth care at least every 2 hours 2. Offer ice chips each time the client is visited 3. Provide the client frequent sips of a favorite beverage 4. Moisten the client’s lips with an appropriate water based lubricant ANS: 1 Client is less willing or able to maintain oral fluid intake reduce discomfort from dehydration by providing mouth care at least every 2 to 4 hours. Lubricating the client’s lips should be included in mouth care while the other options may be impractical if the client is unable or unwilling to take fluids orally. PTS: 1 DIF: C REF: 476 OBJ: Analysis TOP: Nursing Process: Implementation MSC: NCLEX® test plan designation: Safe, Effective Care Environment 29. The son of a client in the initial stage of the dying process is concerned that, “Mom just isn’t eating much.” The nurse responds most therapeutically by answering: 1. “Her body systems are beginning to shut down and she just doesn’t need as much food.” “Her pain medication may be making her nauseated. Has she complained or been 2. vomiting?” “We can off her frequent, small portions of her favorite foods. Can you suggest some things 3. she might enjoy?” “Right now solid foods are not as important as drinking. Just be sure she continues to take 4. in plenty of fluids.” ANS: 3 Medications, depression, decreased activity, decreased blood flow to the gastrointestinal tract; nausea produces anorexia. Offer smaller portions of client preferred foods. Treat underlying cause of anorexia. Do not force food on actively dying client. While the other options are not inaccurate, the most therapeutic response offers the son an appropriate action that might encourage his mother’s eating. PTS: 1 DIF: C REF: 476 OBJ: Analysis TOP: Nursing Process: Implementation MSC: NCLEX® test plan designation: Safe, Effective Care Environment 30. The nurse is caring for a terminal ill client in the final stages of the death process when the client’s daughter asks, “Why are you putting drops in dad’s eyes?” The nurse responds more accurately by telling the daughter that: 1. “His blinking reflex is gone and these drops lubricate his corneas.” 2. “The drops will keep the corneas moist since you have donated them.” 3. “They are artificial tears that will keep his eyes from becoming dry and painful.” 4. “They were prescribed for him but I won’t instill them if you prefer that I don’t” ANS: 3 Blinking reflexes diminish near death, causing drying of the cornea. Optical lubricants or artificial tears reduce corneal drying. While the other options are accurate, they do not address the daughter’s question as thoroughly as the identification of and reasoning for the drops. PTS: 1 DIF: C REF: 476 OBJ: Analysis TOP: Nursing Process: Implementation MSC: NCLEX® test plan designation: Safe, Effective Care Environment 31. A terminal ill client’s pain is being managed with opioid analgesics. When he reports experiencing constipation, the nurse’s most therapeutic response is: 1. “It’s a side effect of the pain medication you are taking.” 2. “I’ll discuss adding some additional bulk to your diet with your wife.” 3. “Try drinking more liquids while you are awake to help soften your stool.” 4. “I’ll see about getting a prescription for a laxative in order to avoid the problem.” ANS: 4 While constipation is a common side effect of opioid analgesics, the most therapeutic nursing response to the client’s report is to offer an appropriate intervention. While the other options are appropriate, the use of a laxative is likely to produce the most effective, timely solution to the problem especially since a terminally ill client is not likely to be eating and drinking sufficiently. PTS: 1 DIF: A REF: 476 OBJ: Analysis TOP: Nursing Process: Implementation MSC: NCLEX® test plan designation: Safe, Effective Care Environment 32. Which of the following statements shows the best understanding of Kübler-Ross’s Five Stages of Dying? 1. “Crying is an expected behavior of the Depression Stage.” 2. “There are tasks the client completes as they work toward acceptance.” 3. “People grieve in the manner in which they are most culturally comfortable” 4. “Given enough time and support, most achieves acceptance of their own death.” ANS: 2 Survivors move back and forth through a series of stages and/or tasks many times, possibly extending over a long period of time. Theorists described stages of the grieving process and a series of tasks for survivors to successfully complete their bereavement and adapt to life with a loss. Why the other options are true, they do not show the best overall understanding of the Five Stages of Dying. PTS: 1 DIF: C REF: 476 OBJ: Analysis TOP: Nursing Process: Analysis MSC: NCLEX® test plan designation: Safe, Effective Care Environment MULTIPLE RESPONSE 1. The daughter of a terminally ill client is grieving the inevitable death of her parent. The expression and depth of her grieve is most likely impacted by her: (Select all that apply.) 1. Spiritual beliefs 2. Chronological age 3. Developmental stage 4. Culturally influences 5. Past experiences with loss 6. Level of formal education ANS: 1, 4, 5 Grief is the emotional response to a loss, manifested in ways unique to an individual, based on personal experiences, cultural expectations, and spiritual beliefs. The remaining options have minimal effect on individual grieving PTS: 1 DIF: A REF: 464 OBJ: Comprehension TOP: Nursing Process: Assessment MSC: NCLEX® test plan designation: Safe, Effective Care Environment Chapter 29: The Experience of Loss, Death, and Grief Potter & Perry: Fundamentals of Nursing, 6th Edition MULTIPLE CHOICE 1. The nurse is discussing future treatments with a client who has a terminal illness. The nurse notes that the client has not been eating and responds to the nurse’s information by saying, “What does it matter?” The most appropriate nursing diagnosis for this client is: a. Social isolation b. Spiritual distress c. Denial d. Hopelessness ANS: d d. A defining characteristic for the nursing diagnosis of hopelessness may include the client stating, “What does it matter?” when offered choices or information concerning him or her. The client’s behavior of not eating also is an indicator of hopelessness. a. This is not an example of social isolation. The client is not avoiding or restricted from seeing others. b. Spiritual distress is not the most appropriate nursing diagnosis for this client. The focus should be on the client’s lack of hope. c. The client’s behavior and verbalization does not indicate denial. REF: Text Reference: p. 579 2. The nurse recognizes that anticipatory grieving can be most beneficial to a client or family because it can: a. Be done in private b. Be discussed with others c. Promote separation of the ill client from the family d. Help a person progress to a healthier emotional state ANS: d d. The benefit of anticipatory grief is that it allows time for the process of grief (i.e., to say good- bye and complete life affairs). Anticipatory grief allows time to grieve in private, to discuss the anticipated loss with others, and to “let go” of the loved one. Anticipatory grief can help a person progress to a healthier emotional state of acceptance and dealing with loss. a. It is not most beneficial for grieving to take place only in private. It is important for grief to be acknowledged by others, and to be able to receive the support of others in the grieving process. b. Anticipatory grieving can be discussed with others in most circumstances. However, at times, anticipatory grief may be disenfranchised grief as well, meaning it cannot be openly acknowledged, socially sanctioned, or publicly shared, such as a partner dying of AIDS. The benefit of anticipatory grieving is not so much that it can be discussed in most circumstances, as this discussion also can occur with normal grief when the actual loss has occurred. c. Anticipatory grief is the process of disengaging or “letting go” that occurs before an actual loss or death has occurred. The benefit is not the separation of the ill client from the family as much as it is the process of being able to say good-bye, to put life affairs in order, and as a result, it can help a client or family to progress to a higher emotional state. REF: Text Reference: p. 571 3. A newly graduated nurse is assigned to his first dying patient. The nurse is best prepared to care for this client if he: a. Completed a course dealing with death and dying b. Is able to control his own emotions about death c. Experiences the death of a loved one d. Has developed a personal understanding of his own feelings about death ANS: d d. When caring for clients experiencing grief, it is important for the nurse to assess his own emotional well-being and to understand his own feelings about death. The nurse who is aware of his own feelings will be less likely to place personal situations and values before those of the client. a. Although course work on death and dying may add to the nurse’s knowledge base, it does not best prepare the nurse for caring for a dying client. The nurse needs to have an awareness of his own feelings about death first, as death can raise many emotions. b. Being able to control one’s own emotions is important; however, it is unlikely that the nurse would be able to do so if he has not first developed a personal understanding of his own feelings about death. c. Experiencing the death of a loved one is not prerequisite to caring for a dying client. Experiencing death may help an individual mature in dealing with loss, or it may bring up many negative emotions if complicated grief is present. The nurse is best prepared by first developing an understanding of his own feelings about death. REF: Text Reference: p. 578 4. An identified outcome for the family of the client with a terminal illness is that they will be able to provide psychological support to the dying client. To assist the family to meet this outcome, the nurse plans to include in the teaching plan: a. Demonstration of bathing techniques b. Application of oxygen devices c. Recognition of client needs and fears d. Information on when to contact the hospice nurse ANS: c c. A dying client’s family is better prepared to provide psychological support if the nurse discusses with them ways to support the dying person and listen to needs and fears. a. Demonstration of bathing techniques may help the family meet the dying client’s physical needs, not to providing psychological support. b. Application of oxygen devices may help the family provide physical needs for the client, not to provide psychological support for the client. d. Information on when to contact the hospice nurse is important knowledge for the family to have and may help them feel they are being supported in caring for the dying client. However, contact information does not help the family provide psychological support to the dying client. REF: Text Reference: p. 588 5. The nurse is assigned to a client who was recently diagnosed with a terminal illness. During morning care, the client asks about organ donation. The nurse should: a. Have the client first discuss the subject with the family b. Suggest the client delay making a decision at this time c. Assist the client to obtain the necessary information to make this decision d. Contact the physician so consent can be obtained from the family ANS: c c. No topic that a dying client wishes to discuss should be avoided. The nurse should respond to questions openly and honestly. As client advocate, the nurse should assist the client to obtain the necessary information to make this decision. a. The nurse should provide the client with information with which to make such a decision. Although the nurse may suggest that the client discuss this option after having obtained information, it is up to the client to discuss the subject with the family. b. The nurse should respect the client and provide the necessary information for him or her to make a decision, rather than dismissing the client’s question. d. It is not necessary to contact the physician or the family for consent for organ donation if the client is capable of making this decision. REF: Text Reference: p. 584 6. A client has been diagnosed with terminal cancer of the liver and is receiving chemotherapy on a medical unit. In an in-depth conversation with the nurse, the client states, “I wonder why this happened to me?” According to Kübler-Ross, the nurse identifies that this stage is associated with: a. Anxiety b. Denial c. Confrontation d. Depression ANS: b b. According to Kübler-Ross, the client is in the denial stage of dying. The client may act as though nothing has happened, may refuse to believe or understand that a loss has occurred and may seem stunned, as though it is “unreal” or difficult to believe. a. No stage of anxiety is found in Kübler-Ross’s five stages of dying. c. No stage of confrontation is found in Kübler-Ross’s five stages of dying. d. During depression, the individual may feel overwhelmingly lonely and withdraw from interpersonal interaction. REF: Text Reference: p. 570 7. A client who is Chinese American has just died on the unit. The nurse is prepared to provide after death care to the client and anticipates that the probable preferences of a family from this cultural background will include: a. Pastoral care b. Preparation for organ donation c. Time for the family to bathe the client d. Preparation for quick removal from the hospital ANS: c c. Some families of Chinese Americans will prefer to bathe the client themselves. They often believe the body should remain intact; organ donation and autopsy are uncommon. a. Chinese Americans do not prefer pastoral care for after-death care of a family member. b. Organ donation is uncommon for Chinese Americans. d. Chinese Americans may desire time to bathe the client. Quick removal from the hospital is not preferred. REF: Text Reference: p. 589 8. Which of the following is the primary concern of the nurse for providing care to a dying client? The nurse should: a. Promote optimism in the client and be a source of encouragement b. Intervene in the client’s activities of daily living and promote as near normal functions as possible c. Allow the client to be alone and expect isolation on the part of the dying person d. Promote dignity and self-esteem in as many interventions as possible ANS: d d. The focus in planning nursing care is to support the client physically, emotionally, developmentally, and spiritually in the expression of grief. When caring for the dying client, it is important to devise a plan that helps a client to die with dignity and offers family members the assurance that their loved one is cared for with care and compassion. a. Optimism should not be the primary focus when caring for the dying client. The nurse should promote the client’s self-esteem and allow the client to die with dignity. b. The client should be allowed to make choices and perform as many activities of daily living independently as possible. This allows the client to maintain self-esteem and dignity. c. The client does not need to be left alone. The presence of the nurse or the family may indicate to the client that he or she is being cared for and is worthy of attention. REF: Text Reference: p. 580 9. Hospice nursing care has a different focus for client. The nurse is aware that client care provided through a hospice is: a. Designed to meet the client’s individual wishes, as much as possible b. Usually aimed at offering curative treatment for the client c. Involved in teaching families to provide postmortem care d. Offered primarily for hospitalized clients ANS: a a. The nurse’s role in hospice is to meet the primary wishes of the dying client and to be open to individual desires of each client. The nurse supports a client’s choice in maintaining comfort and dignity. b. Hospice care is for the terminally ill. It is not aimed at offering curative treatment, but rather the emphasis is on palliative care. c. Hospice care may provide bereavement follow-up for the family after a client’s death, but hospice nurses typically do not teach the family postmortem care. d. Hospice care is primarily for home care, but a client in hospice may become hospitalized. REF: Text Reference: p. 588 10. The nurse is preparing to assist the client in the end stage of her life. To provide comfort for the client in response to anticipated symptom development, the nurse plans to: a. Decrease the client’s fluid intake b. Limit the use of analgesics c. Provide larger meals with more seasoning d. Determine valued activities and schedule rest periods ANS: d d. To promote comfort in the terminally ill client, the nurse should help the client to identify values or desired tasks and then help the client to conserve energy for those tasks. a. Decreasing the client’s fluid intake may make the terminally ill client more prone to dehydration and constipation. The nurse should take measures to help maintain oral intake, such as administering antiemetics, applying topical analgesics to oral lesions, and offering ice chips. b. The use of analgesics should not be limited. Controlling the terminally ill client’s level of pain is a primary concern in promoting comfort. c. Nausea, vomiting, and anorexia may increase the terminally ill client’s likelihood of inadequate nutrition. The nurse should serve smaller portions and bland foods, which may be more palatable. REF: Text Reference: p. 586 11. The nurse is working with a client on an inpatient hospice unit. To maintain the client’s sense of self-worth during the end of life, the nurse should: a. Leave the client alone to deal with final affairs b. Call on the client’s spiritual advisor to take over care c. Plan regular visits throughout the day d. Have a grief counselor visit ANS: c c. Spending time to let clients share their life experiences, particularly what has been meaningful, enables the nurse to know clients better. Knowing clients then facilitates choice of therapies that promote client decision-making and autonomy. Planning regular visits also helps the client maintain a sense of self-worth, because it demonstrates that he or she is worthy of the nurse’s time and attention. a. The client should not be left alone to feel abandoned or isolated. b. Nurses can help clients meet spiritual needs by facilitating connections to a spiritual practice or community and supporting the expression of culturally held beliefs. A client’s spiritual advisor also may be called on, but is not the only source of spiritual support. The nurse who turns care over to the spiritual advisor is not promoting the client’s sense of self-worth, as it may imply the client is not worthy of the nurse’s time or attention. d. A grief counselor may be requested to visit if the client is experiencing complicated grief. Having a grief counselor visit is not an intervention that will help maintain a client’s sense of self-worth. REF: Text Reference: p. 587 12. A nursing intervention to assist the client with a nursing diagnosis of Sleep pattern disturbance related to the loss of spouse and fear of nightmares should be to: a. Administer sleeping medication per order b. Refer the client to a psychologist or psychotherapist c. Have the client complete a detailed sleep-pattern assessment d. Sit with the client and encourage verbalization of feelings ANS: d d. A nursing intervention to facilitate grief work is to offer the client encouragement to explore and verbalize feelings of grief. This encouragement refocuses the client on current needs and minimizes dysfunctional adaptation behaviors (e.g., not sleeping) by facilitating resolution of grief through problem-solving skills. a. Administering sleeping medication may help the client get to sleep, but does not resolve the issue of grief. Without addressing the grief, the client may develop another dysfunctional adaptation behavior. b. It is not necessary to refer the client to a psychologist or psychotherapist at this time. The client needs to be encouraged to verbalize his or her feelings. c. Having the client complete a detailed sleep-pattern assessment may help the nurse identify the number of hours of sleep the client is obtaining, but it does not address the issue causing the sleep disturbance, which is grief from the loss of the spouse. REF: Text Reference: p. 583 13. To promote comfort for the terminally ill client specific to nausea and vomiting, the nurse should: a. Provide prompt mouth care b. Offer high-protein foods c. Increase the fluid intake d. Offer a high-residue diet ANS: b b. To promote comfort for the terminally ill client specific to nausea and vomiting, the nurse should administer antiemetics, provide oral care at least every 2 to 4 hours, offer clear liquid diet and ice chips, avoid liquids that increase stomach acidity such as coffee, milk, and citrus acid juices, and offer high-protein foods in smaller portions and of a bland nature. a. Oral care should be provided every 2 to 4 hours. c. Increasing the fluid intake may help prevent constipation. d. A low-residue diet may help prevent diarrhea. REF: Text Reference: p. 586 14. A nurse-initiated or independent activity for promotion of respiratory function in a terminally ill client is to: a. Limit fluids b. Position the client upright c. Reduce narcotic analgesic use d. Administer bronchodilators ANS: b b. Positioning the client upright is an independent nursing intervention for the promotion of respiratory function in a terminally ill client. a. Limiting fluids may not promote respiratory function, and unless a client is on a fluid- restricted diet, the nurse should not do so. c. Reducing narcotic analgesic use is not a nurse-initiated activity to promote respiratory function. A respiratory rate should be assessed before administering narcotics to prevent further respiratory depression. Management of air hunger involves judicious administration of morphine and anxiolytics for relief of respiratory distress. d. The administration of bronchodilators would require a physician’s order. It is not an independent nursing activity. REF: Text Reference: p. 586 15. The nurse is using Bowlby’s phases of mourning as a framework for assessing the client’s response to the traumatic loss of her leg. During the “yearning and searching” phase, the nurse anticipates that the client may respond by: a. Crying off and on b. Becoming angry at the nurse c. Acting stunned by the loss d. Discussing the change in role that will occur ANS: a a. During the “yearning and searching” phase of Bowlby’s phases of mourning, the nurse anticipates that the client may have outbursts of tearful sobbing and acute distress. b. During Bowlby’s “disorganization and despair” phase of mourning, the nurse anticipates that the client may express anger at anyone who might be responsible, including the nurse. c. During the “numbing” phase of Bowlby’s phases of mourning, the nurse anticipates that the client may act stunned by the loss. d. During the “reorganization” phase of Bowlby’s phases of mourning, the nurse anticipates that the client may discuss the change in role that will occur. REF: Text Reference: p. 570 [Show More]
Last updated: 2 years ago
Preview 1 out of 72 pages
.png)
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$16.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Mar 22, 2021
Number of pages
72
Written in
Additional information
This document has been written for:
Uploaded
Mar 22, 2021
Downloads
0
Views
138







.png)
.png)

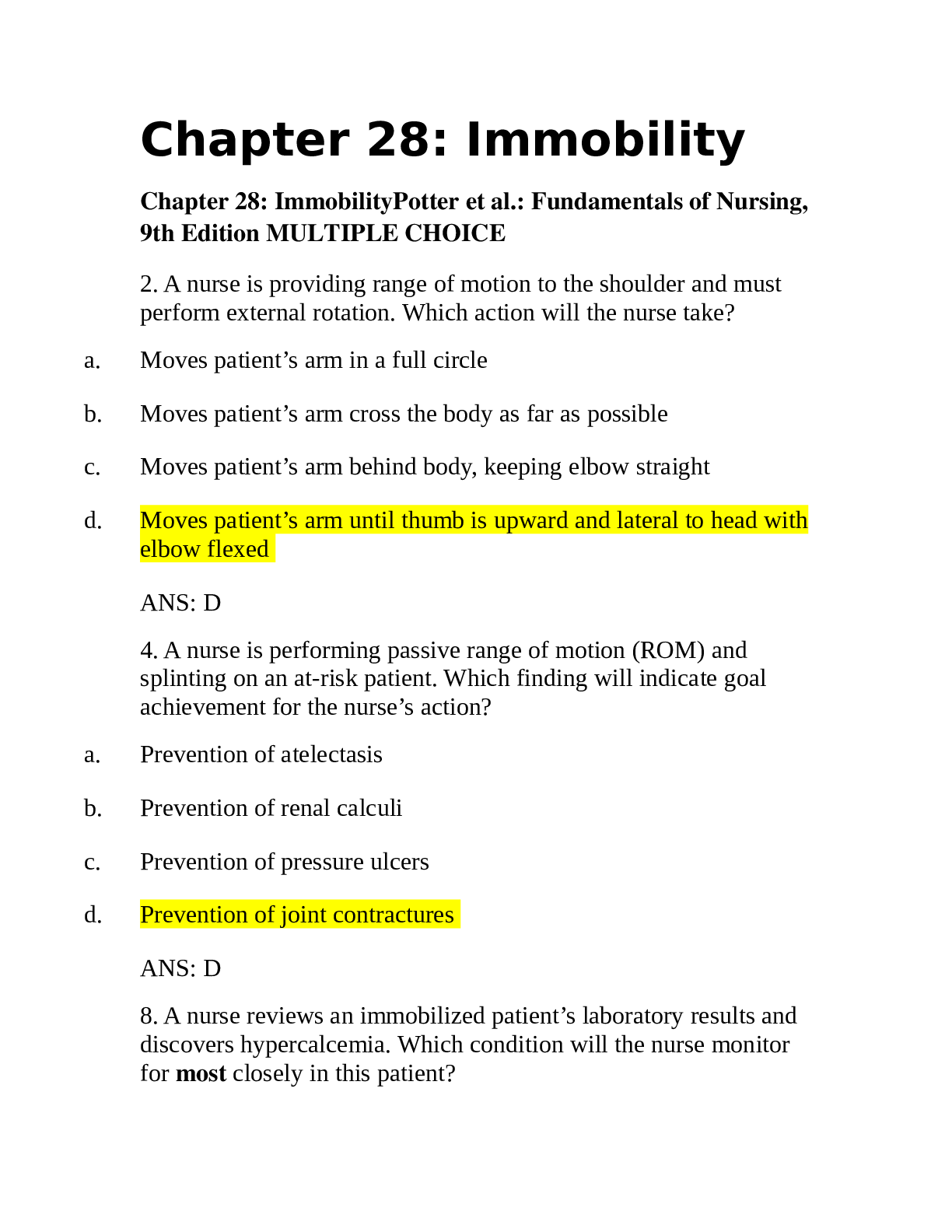
.png)
.png)
 (1).png)
.png)
.png)
.png)

