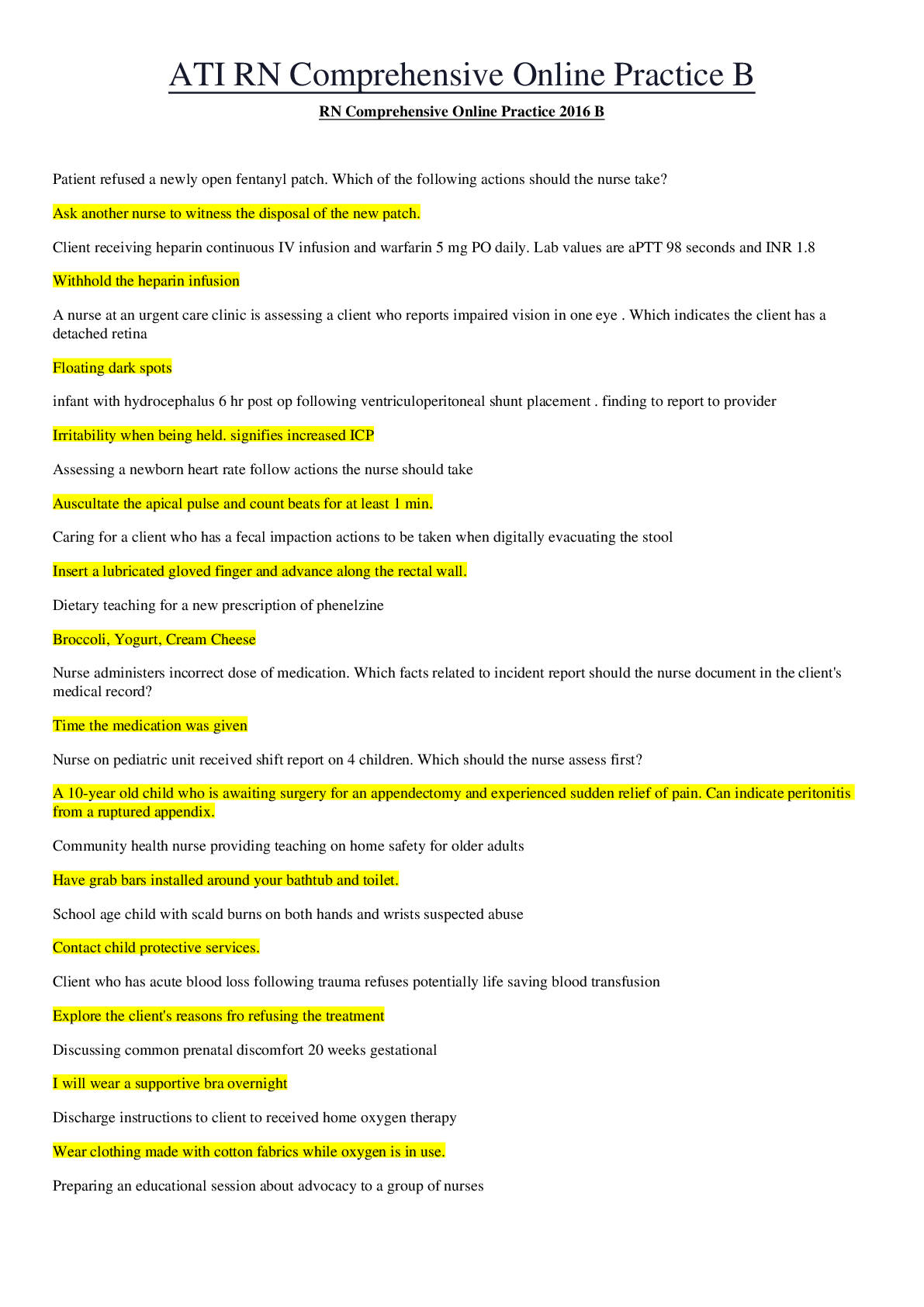
ATI RN COMPREHENSIVE EXIT EXAM
diet for chronic renal failure low protein & potassium
DM pt teaching
change shoes, wash feet w/soap & water
pulse pressure
subtract systolic value from diastolic value
lantus
...
ATI RN COMPREHENSIVE EXIT EXAM
diet for chronic renal failure low protein & potassium
DM pt teaching
change shoes, wash feet w/soap & water
pulse pressure
subtract systolic value from diastolic value
lantus
never mix, long lasting, no peak
rhogam
given @ 28 weeks & 72 hours post delivery when mom is negative & baby positive
indication of baby dehydration improving smooth fontanel
pt w/orthostatic hypotension put near nursing station
cleaning a wound clean to dirty
use bulb syringe
peripheral arterial disease cramp in leg while walking intermittent claudication
seizure precautions supine position
20 weeks gestation, having urinary frequency u/a & c/s
report to new nurse @ shift change pt @ xray
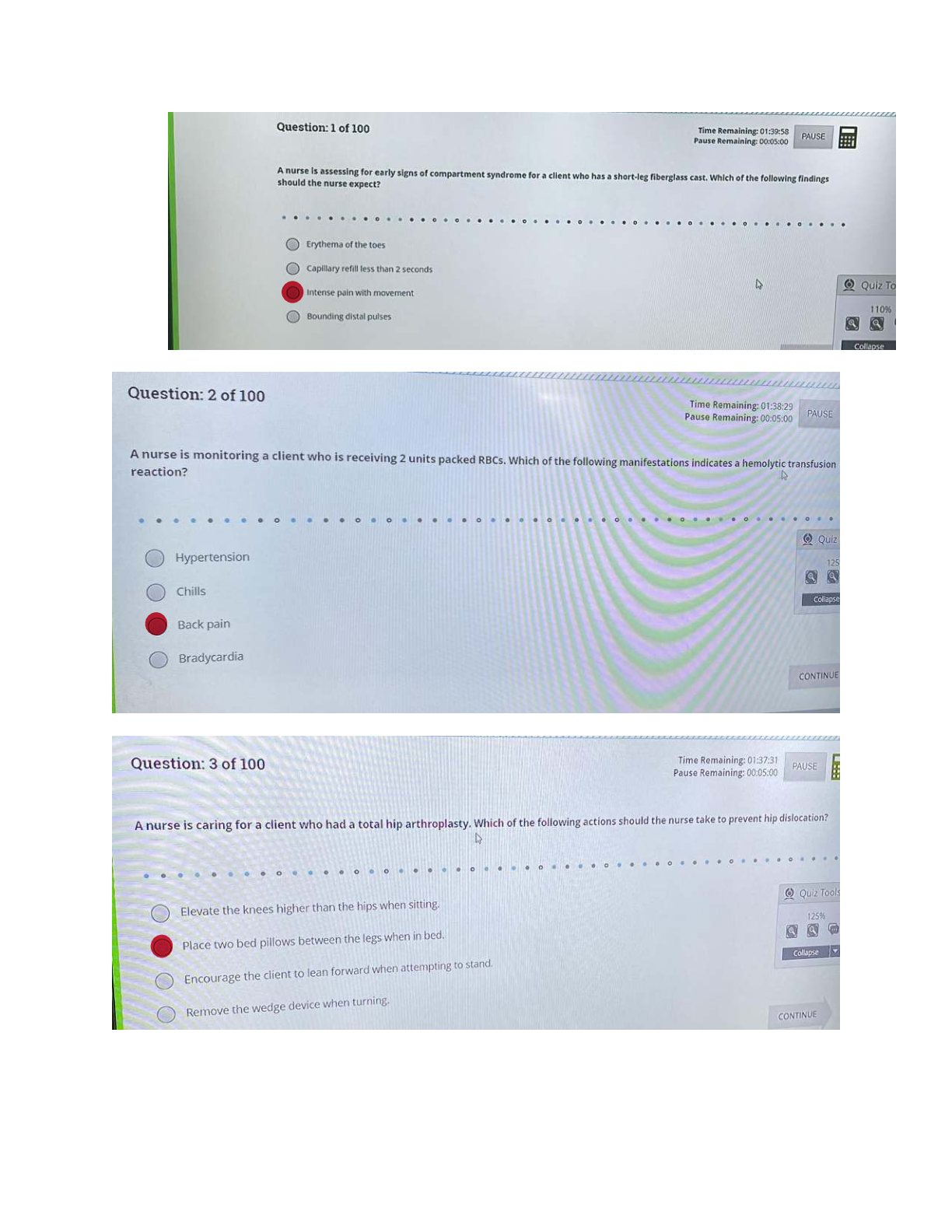
s/s of hemolytic blood transfusion flank pain
ER rape victim priority acess anxiety
nutrition
carbs 45%, protein 10-15%
latex allergy tape up cords
first ingredient on a food label most content
thoracentesis, & painful w/breathing
put pt on UNAFFECTED side for 1 hour or longer
pt w/IV sedation
check LOC if not responsive
help older brother get used to baby get a gift for big brother
early decelerations head compressions
methergine contraindication HTN
delegate to AP I & O
HF monitoring weights
location for peripheral line radial
prioritizing care for multiple pt's low flank pain
ativan
for seizures
med for diabetes insipidus desmopressin
radiation tatoo
use mild soap & water
uric acid stones eat low fat yogurt
antigout med decreases uric acid level allopurinol
non-pharm relation technique for pain management in labor hypnosis
psychotic disorder assessment finding flat affect
newborn withdrawal from heroin (opioids) hypertonicity
mitral valve location 5th intercostal
amniocentesis
go pee before procedure
total gastrectomy lack b 12
takes 30-60 meal to eat a meal
stoma color
pink or red is normal
MAOI's diet
no pepperoni, no tyramine, COTTAGE CHEESE OKJ
give iron w/?
OJ
statins contraindication Grapefruit juice
haldol
lip smacking
mag sulfate
decreased urine output decreased respirations decreased pulmonary edema
antidote for mag sulfate calcium gluconate
clozaril interventions monitor WBC
valproic acid liver function
thyroid med effectiveness weight loss
diuretics
don't skip doses
DIG adverse effects N/V & HA
prednisone take with milk
hemo/peritoneal dialysis pt teaching medical asepsis
cranial nerve 11 shoulder
peripheral catheter insertion
advance catheter when you see flash back of blood return
dispose of insulin needles @ home in coffee container
confirmation of ng placement x ray
swallowing difficulty referral speech therapy
acrabose
skip a meal, skip dose, give w/1st bite of food
sprains & strains RICE
pt DNR-CC & family asking questions related to. therapeutic communication: THERAPEUTIC RESPONSE
What did the dr tell you?
delegating to AP about skeletal traction: NEEDS MORE TEACHING AP places weight on bed
daughter feeling guilty about admitting parent into long-term facility: THERAPEUTIC RESPONSE
rephrase what daughter is feeling
how good nurse plans her day
rechecks her priorities half way through her shift
good nurse sets these when she works GOALS
pt gets bad dx, & asks you not to tell her spouse:YOUR RESPONSE you have a right to privacy
delegate to AP CPR
baby in contact precautions in a private room, what would you do to save hospital $? bring formula prn
how does a nurse properly manage her time mid-shift? reevaluates goals
which psych pt would you see first? hallucinations
dementia pt @ ER, w/marks on coccyx & wrist, suspected abuse. what do you do? ask pt. INTERVIEW HIM
psych pt yelling in front of group. very agitated, what do you do? isolate pt
charge nurse scheduling resolution between nurses nurse listens to both sides
respite care
gives family a break
pt in seclusion documentation
what happened prior to seclusion that caused for seclusion parkinson's : pt teaching
nutrition- thicken liquids
pt receiving radiation, what should you wear? lead apron
pt suffering from hyperthermia seizure precautions
pt refuses last minute for a procedure he already consented for okay to stop procedure
s/s of smallpox rash on tongue
xerostoma humidifier
vagina procedure, cervical cancer place catheter
Lyme disease report it
lice (pediculodis capitis)
can survive on surfaces for up to 48 hours
RSV
keep stethescope in room (droplet)
16 weeks gestation can get AFP test done
bacterial meningitis droplet precautions
when can kid return to school for chicken pox when lesions are crusted over
kicks a ball: developmental stage
24 months
baby w/cleft lip
untie arms & perform ROM
wrong ostomy care
changing everyday may lead to skin irritation
after male circumcision
apply petroleum jelly w/every diaper change
breastfeeding w/hep c
don't breast feed if you have cracked nipples
contraindication w/oral contraceptives HTN
combination contraceptives contraindications pt w/migraines
when percussing RUQ, what should we feel dullness
dementia pt
offer finger foods
black males @ great risk for CVA
med for alcohol withdrawal disulfiran (antabuse)
better nutririon canola oil
healthy eating 45 % carbs
to prevent neuro tube defects
folate
prevnting delays of healing protein & o2
pt raped & @ ER assess anxiety
pt reports abuse
assess pt, check for injuries
anorexia
60% refeeding-pre-albumin of 10
telemetry is used for check for dysrythmia
do not give mmr
to child bearing pt b4 pregnancy test pt w/hx of blood transfusion
diet for hf
dry spices to flavor food
TURP: closed intrermittment irrigation let it drain
Cranial nerve XI (hot spot) shoulder
Proper lifting technique (picture) bending at knees
24 month old walk up steps
Food label
greatest weight listed first
IV technique advance catheter
Refeeding syndrome 60%
Low fat diet
canola oil instead of vegetable oil
Prior to amniocentesis empty bladder
Radiation implant
limit visitors to 30 minutes
Levothyroxine
take on empty stomach, in am; increases tsh
Metformin contraindication
kidney disease, severe infection, shock, hypoxic conditions
Mastectomy
lay of affected side to promote drainage, support arm on pillow, HOB 30
Circumcision
use petroleum jelly with every diaper change
Check for NG tube placement in the jejunum X-ray
Colostomy care cut the bag
Seizure precautions saline lock IV
Ethical medical error veracity
Early decelerations head compressions
Magnesium sulfate interventions
(select all) calcium gluconate, stop infusion, UO less than 30, RR less than 12, decreased reflexes
Thoracentesis causes pneumothorax expected finding not friction rub; tracheal deviation
AP's talking in cafeteria tell them to stop talking
Safety for parkinson's clear area
Warfarin
vitamin k for toxicity; INR 2-3; PT 11-12.5
Contraindication of MMR blood transfusion
Diabetic foot care
(select all) change shoes frequently, wash feet with soap and water
Sprains
avoid warm compress
Expected finding of small pox rash in mouth
16 weeks pregnant alpha protein
Psych med lip smacking
Where to start IV first (picture) hand
PRBC need further teaching start IV on other arm
Delegate to AP CPR compressions
Delegate to LPN sterile dressing
Postural drainage
give albuterol, trendelenberg; 1 hour before meals or 2 hours after
Dumping syndrome
high protein and fat; avoid milk, sweets, and sugar; small, frequent meals
DASH diet
increase fruit, vegetables, and low fat dairy; k, mg, ca
Baby with reflux
small, frequent meals, thicken formula with rice cereal, HOB 30
Cleft palate repair periodic restraints
Nephrotic syndrome vitamin K
Pernicious anemia schilling's test
Peritoneal dialysis
report cloudy; monitor glucose; warm solution before
Gastric surgery eat 3 meals
Gastrectomy
small, frequent meals; vitamin B12, D, iron, and folate
Statin grapefruit
Preventing uric acid stones yogurt
RSV
have own stethoscope in room
Change of shift report
orthostatic hypotension by nurses station
Confused patient raise 1 side rail
Hypoglycemia
cool and clammy skin
Hyperglycemia thirst
Glycosylated blood test HbA1C
Priority for patient in seclusion document
Buddhist patient vegetarian
Positive TB
hard raised bump
Heart murmur sound blowing or swishing
Dehydration oliguria
NST
PAD
pain/cramping when walking, calf muscle atrophy, shiny cool extremities; elevate legs
Cast with white extremity compartment syndrome
Alcohol withdrawal expected finding
n&v, tachycardia, diaphoresis, tremors, seizures
Varicella scabs okay
Hyperthermia not blanket or ice
Purpose of ice decrease inflammation
Sexual assault assess anxiety
THA
avoid flexion greater than 90
Beta blocker teaching
don't stop abruptly; avoid in asthma; take with food
Combination contraceptives increase BP
Myelosuppression flu shot
Glucocorticoid
increase dose in DM; take with meals; avoid NSAIDs; Addison's crisis if stopped abruptly
Extreme focus mild anxiety
-
-
-
-
-
-
-
--
Opthalmic
Ophthalmic medications are drugs used for the eye. These medications are typically prescribed for clients who have Glaucoma, Macular Degeneration. Other ophthalmic medications are used to treat allergic conjunctivitis, inflammatory disorders, dyes to visualize the eye, and to treat infections or viruses.
Beta-Adrenergic Blocking Agents
Prescribed for clients who have open-angle glaucoma. These agents decrease the production of aqueous humor. Block beta 1and beta 2 receptors.
Common Beta-Adrenergic Ophthalmic Blocking Agents:
beta xolos ( Bet optic ) (see the form of beta in the drug names?) See optic in Betoptic? Opthalmic medication.
levo beta xolol ( Beta xon) (see the form of beta in the drug names?) levobunolol ( Beta gan) (see the form of beta in the drug name?) timolol ( Bet imol) (see the form of beta in the drug name?) Prostaglandin Analogs
First line treatment for glaucoma. Fewer side effects and just as effective as the beta-adrenergic Ophthalmic blocking agents.
These drugs lower IOP by facilitating aqueous humor outflow by relaxing the ciliary muscle. Common Prostaglandin Analogs:
latanoprost (Xal atan ) (see the suffix atan in this drug and the drug below, they are the same) Travoprost (trav atan ) (see the suffix atan in this drug and the drug above; they are the same) Alpha2-Adrenergic Agonists
These drugs lower IOP by reducing aqueous humor production and by increasing outflow. Also delays optic nerve degeneration and protects retinal neurons from death.
Common Alpha2-Adrenergic Agonists:
Brimon idine (Alphagan) (see the similarities with idine in the name of the drug)
Apraclon idine (Iop idine ) (see the similarities with idine in both of the names of the drug) Direct Acting Cholinergic Agonist/Muscarinic Agonist (parasympathomimetic agent)
These drugs stimulate the cholinergic receptors in the eye, constricts the pupil (miosis), and contraction of the ciliary muscle. IOP is reduced by the tension generated by contracting the ciliary muscle and promotes widening of the spaces within the trabecular meshwork, thereby facilitating outflow of aqueous humor.
Common Direct Acting Cholinergic Agonist Agents:
Pilocarpine
Key points of ophthalmic medications:
· Cylo plegics are drugs that cause paralysis of the ciliary muscle...plegic-like paraplegic, paralysis
· Mydriatics are drugs that dilate the pupil.
· Drug therapy for glaucoma is directed at reducing elevated IOP, by increasing aqueous humor outflow or decreasing aqueous humor production.
· Oculus Dexter: OD (right eye)
· Oculus Sinister: OS (left eye)
· Oculus Uterque: OU (both eyes)
Remember BAD POCC: Ophthalmic Medication Classes for treatment of Glaucoma B -beta adrenergic blocking agents
A -Alpha-Adrenergic Agonists
D -Direct Acting Cholinergic Agonists P -Prostaglandin Analogs
O -Osmotic Agents
C -Carbonic Anhydrase Inhibitors
C -Cholinesterase Inhibitor; An indirect acting Cholinergic Agonist
Remember BAD POCC for key points or side effects of Opthalmic Medications:
B -Blurred vision
A -Angle closure glaucoma (medications are used for this kind of glaucoma) D -Dry eyes
P -Photophobia
O -Ocular pressure (used to treat OP from glaucoma) C -Can Cause systemic effects
C -Ciliary muscle constriction
Gestational diabetes mellitus
Impaired tolerance to glucose with the first onset or recognition during pregnancy
Hyperemesis Gravidarum
Severe morning sickness with unrelenting, excessive nausea or vomiting that prevents adequate intake of food and fluids
HELLP syndrome
A variant of gestational hypertension where hematologic conditions coexist with severe preeclampsia and hepatic dysfunction.
Gestational hypertension
Hypertension beginning after the 20th week of pregnancy with no proteinuria.
Mild preeclampsia
Hypertension beginning after the 20th week of pregnancy with 1 to 2+ proteinuria and a weight gain of more than 2 kg per week in the second and third trimesters.
Eclampsia
Severe preeclampsia symptoms with seizure activity or coma
Taking in phase
24-48 hours after birth: dependent, passive; focuses on own needs; excited, talkative Taking hold phase
focuses on maternal role and care of the newborn; eager to learn; may develop blues
Letting go phase
Focuses on family and individual roles
Cephalopelvic disproportion
When the fetus has a head size, shape or position that does not allow for passage through the pelvis.
Presentation
Includes cephalic, breech and shoulder.
Longitudinal lie
The fetal long axis is parallel to the mother's long axis. The fetus is either in a breech or vertex presentation
Duration
The amount of time elapsed from the beginning of one contraction to the end of the same contraction.
Intensity
The strength of the uterine contraction.
Transverse lie
The long axis of the fetus is at a right angle to the mother's long axis. This is incompatible with a vaginal delivery if the fetus remains in this position
Frequency
The amount of time from the beginning of one contraction to the beginning of the next contraction
Regularity
The amount of consistency in the frequency and intensity of contractions.
Station
The relationship of the presenting part to the maternal ischial spines that measures the degree of descent of the fetus.
missing birth control pills...
In the event of a client missing a dose the nurse should instruct the client that if one pill is missed to take as soon as possible. If two or three pills are missed the client should follow the manufacturer's instructions and use an alternative form of contraception.
pediatric acetaminophen levels
>200 mcg/ml
pediatric carbon dioxide cord--> 14-22
premature 1 week --> 14-27
newborn --> 13-22 infant, child --> 20-28
pediatric chloride level Cord --> 96-104
Newborn --> 97-110
Child --> 98-106
Conjugated direct Bilirubin level 0.0-0.2 mg/dl
pediatric creatinine level cord --> 0.6-1.2
newborn --> 0.3-1.0
infant 0.2-0.4
child --> 0.3-0.7
adolescent --> 0.5-1.0
pediatric Digoxin toxic concentration
> 2.5 ng/ml
pediatric Glucose (Serum) Newborn, 1 day --> 40 to 60
Newborn, > 1 day --> 50 to 90
Child --> 60 to 100
pediatric Hematocrit levels 1 day --> 48-69%
2 day --> 48-75%
3 day --> 44-72 %
2 month --> 28-42 %
6- 12 year --> 37-49%
12- 18 year Male --> 37-49%
12-18 year Female --> 36-46%
Antigout Medications - What is gout?
Gout is a type of arthritis. In healthy people the body breaks down dietary purines and produces uric acid. The uric acid dissolves and is excreted via the kidneys. In individuals affected with gout the body either produces too much uric acid or is unable to excrete enough uric acid and it builds up. High uric acid levels results in urate crystals which can now collect in joints or tissues. This causes severe pain, inflammation and swelling. Treatment is both lifestyle adjustment and medication.
Medications
First Line: NSAIDs and prednisone (Deltasone)
Purpose: Used as a first line defense to treat the pain and inflammation of gout attacks. Colchicine (Colgout):
Purpose: Treat the inflammation and pain associated with gout.
Just like NSAIDs, these meds can lead to GI distress and should be taken with foods. HINT: The word gout is right in the name Colgout.
Allopurinol (Zyloprim):
Purpose:
This is the only medical preventative treatment for gout. Allopurinal prevents uric acid production. This can be an effective means of preventing gout attacks when diet alone is not effective.
HINT: Examine the name allopurinol and you can see the word PURINE in the middle of the name.
Note: There are many drug and food interactions associated with allopurinol:
Potential serious interactions with the use of saliscylates, loop diuretics, phenylbutazamines and alcohol and potential for drug interactions with Warfarin (Coumadin).
Teach client with gout to avoid the following:
· Anchovies, sardine in oil, fish roe, herring
· Yeast
· Organ meat (liver, kidneys, sweetbreads)
· Legumes (dried beans and peas)
· Meathextracts (gravies and consommé)
· Mushrooms, spinach, asparagus, cauliflower Anti-reabsorptives
What is anati-reabsorptive?
Bone is a living organ which is continually being removed (resorbed) and rebuilt. Osteoporosis develops when there is more resorption than rebuilding. Antiresorptive medications are designed to slow bone removal and or improve bone mass.
Treating and preventing osteoporosis can involve lifestyle changes and sometimes medication. Lifestyle change includes diet and exercise, and fall prevention.
Prevention and treatment of osteoporosis involve medications that work by preventing bone breakdown or promote new bone formation.
Medications
Bisphosphonates prevent the loss of bone mass Alendronate (Fosamax)
Monthly used to treat and prevent osteoporosis in menopausal women.
Facts: The benefits of Fosamax can even be seen in elderly women over 75 years of age.
Hint: Fosamax has been associated with severe esophagitis and ulcers of the esophagus. Should be avoided in clients with history of gastric ulcers.
Risedronate (Actonel): This is a newer drug and less likely to cause esophageal irritation Hint: Teach clients taking either drug to take on an empty stomach with at least 8 ounces (240
ml) of water, while sitting or standing. This minimizes the chances of the pill being lodged in the esophagus. Clients should also remain upright for at least 30 minutes after taking these pills to avoid reflux in to the esophagus.
For those clients who cannot tolerate the esophagus side effects of Fosamax, estrogen, etidronate (Didronel), and calcitonin are possible alternatives.
Teriparatide (Forteo): It acts like parathyroid hormone and stimulates osteoblasts, thus increasing their activity. Promotes bone formation.
Facts: This drug is associated with a risk of bone tumors so is only used when the benefits outweigh the risks.
Antirheumatics
What is rheumatoid arthritis?
Rheumatoid arthritis (RA) is a chronic disease that results in inflammation of the joints and surrounding tissues. RA affects the lining of the joints and the painful swelling can result in bone erosion and joint deformities. It is the small joints in hands and feet are most often affected.
Treatment is designed to provide symptom relief and some delay in progression of the disorder but not a cure.
Medications
Disease-modifying Antirheumatic drugs (DMARDs), glucocorticoids, and non-steroidal
anti-inflammatory drugs (NSAIDs) may be used individually or in combination to manage this chronic disorder.
The major categories of antirhematics are:
DMARDs I - Major Nonbiologic DMARDs
· Cytotoxic medications: Methotrexate (Rheumatrex), leflunomide (Arava)
· Antimalarial agents: Hydroxychloroquine (Plaquenil)
· Anti-inflammatory medication: Sulfasalazine (Azulfidine)
· Tetracycline antibiotic: Minocycline (Minocin) DMARDs II - Major Biologic DMARDs
· Etanercept (Enbrel)
· Infliximab (Remicade)
· Adalimumab (Humira)
· Rituximab (Rituxan)
· Abatacept (Orencia)
DMARDs III - Minor nonbiologic and biologic DMARDs
· Gold salts: Aurothioglucose (Solganal)
· Penicillamine (Cuprimine, Depen)
· Cytotoxic medications: Azathioprine (Imuran), cyclosporine (Sandimmune, Gengraf, Neoral)
· Glucocorticoids:
· Prednisone (Deltasone), prednisolone (Prelone)
● NSAIDs Hints:
DMARDs slow joint degeneration and progression of rheumatoid arthritis. Glucocorticoids and NSAIDs provide symptom relief from inflammation and pain.
Rheumatrex ( methotrexate ) is the most commonly used DMARD. This is because it has been shown to work as well or better than any other single medicine. It is also relatively inexpensive and generally safe.
Methotrexate has many food and drug interactions especially affect digoxin and phenytoin. Very difficult to absorb and should be taken on an empty stomach.
Taking folic acid helps reduce some of the side effects. Methotrexate's biggest advantage could be that it has been shown to be safe to take for long periods of time and can even be used in children.
Antineoplastics
Antineoplastics are used combat cancerous cells.
There are many kinds of anti-cancer drugs with a variety of actions. But in simple terms this category of drugs attack cells that multiply and divide. This very action which can kill cancer cells can also do the same to healthy dividing cells. This is especially true of cells that need a steady supply of new cells such as skin, hair and nails.
There are over 90 different kinds of chemotherapy agents and different drugs cause different side effects
Chemotherapy is associated with a variety of side effects:
§ Nausea and vomiting
§ Diarrhea and or constipation
§ Alopecia
§ Anorexia
§ Fatigue and exhaustion
§ Mouth sores
§ Easy bruising Medications
Fluorouracil (5-fluorouracil, 5-FU) Warning - Hazardous drug!
5-FUis one of the oldest chemotherapy drugs and is used against a variety of cancers. Following are some of the most common and important ill effects:
· Soreness of the mouth, difficulty swallowing
· Diarrhea
· Stomach pain
· Low platelets
· Anemia
· Sensitive skin (to sun exposure)
· Excessive tear formation from the eyes Nursing Hints:
Be aware of the importance of leucovorin rescue with fluorouracil therapy, if prescribed.
· The best treatment for extravasation is prevention.
· Extravasation can cause pain, reddening, or irritation on the arm with the infusion needle. In severe cases in can lead to tissue necrosis and even loss of an extremity.
· Check infusion site frequently
· Stop infusion immediately if suspected
· Slowly aspirate back blood back from the arm
· Elevate arm and rest in elevated position
· Check institution policies on how to remove catheter Oral hypoglycemics
What is diabetes?
Diabetes is a disorder that affects glucose metabolism.
Type 1 diabetes: The client either makes no insulin or not enough insulin.
Type 2 diabetes: The client makes enough insulin at least early in the disease but is unable to transport glucose from the blood into the cells.
In both cases, the individual is unable to metabolize glucose. The purpose of oral hypoglycemics is to assist with glucose metabolism.
Medications
There are four classes of hypoglycemic drugs:
· Sulfonylureas
Tolbutamide (Orin ase); glyburide; Micron ase Stimulates insulin production
Associated with weight gain
· Biguanide: Metformin
o First line drug in type 2 diabetes
o Reduces the production of glucose within the liver
o Associated with modest weight loss
o Less likely to cause hypoglycemia.
o Significant lipid-lowering activity.
· Thiazolidinediones
o Reverses insulin resistance
o Increases glucose uptake and decreased glucose production
o Associated with severe liver damage
· Alpha-glucosidaseinhibitors. o Acarbose (Precose)
o Reduces the absorption of dietary glucose
o Associated with flatulence and diarrhea Hints:
No matter which class the client will be taking there is always the risk of hypoglycemia
Be sure to teach client how to recognize early signs and symptoms of hypoglycemia as well as appropriate interventions.
Mental Status Exam
All clients should have a Mental Status Exam, which includes:
Level of consciousness Physical appearance Behavior
Cognitive and intellectual abilities
The nurse conducts the MSE as part of his or her routine and ongoing assessment of the client. Changes in Mental Status should be investigated further and the provider notified.
There are two types of mental health hospitalizations: Voluntary commitment and involuntary or civil commitment. Involuntary commitment is against the client's will. Despite that, unless proven otherwise, clients are still considered competent and have the right to refuse treatment.
Use the following communication tips when answering questions on NCLEX:
* If the client is anxious or depressed - use open-ended, supportive statements
* If the client is suicidal - use direct, yes or no questions to assess suicide risk
* If the client is panicked - use gentle guidance and direction
* If the client is confused - provide reality orientation
* If the client has delusions / hallucinations / paranoia - acknowledge these, but don't reinforce
* If the client has obsessive / compulsive behavior - communicate AFTER the compulsive behavior
* If the client has a personality or cognitive disorder - be calm and matter-of-fact
ECT
The most common type of brain stimulation therapy is electronconvulsive therapy or ECT. ECT is generally performed for major depressive disorders, schizophrenia or acute manic disorders. Most clients receive therapy three times a week for two to three weeks. Prior to ECT, carefully screen the client for any home medication use. Lithium, MAOIs and all seizure threshold medications should be discontinued two weeks prior to ECT. After therapy, reorient the client as short term memory loss is common.
Anxiety disorders
Anxiety disorders are common mental health disorders. Generalized Anxiety Disorder, Panic Disorder, Phobias, Obsessive Compulsive Disorder, and Posttraumatic stress disorder (PTSD) are all considered types of anxiety disorders. Assess the client for risk factors, triggers and responses.
Depressive disorders
A classic symptom of depression is change in sleep patterns, indecisiveness, decreased concentration, or change in body weight. Any client who shows these signs or symptoms should be asked if they have suicidal ideation. Teach clients to never discontinue anti-depressants suddenly.
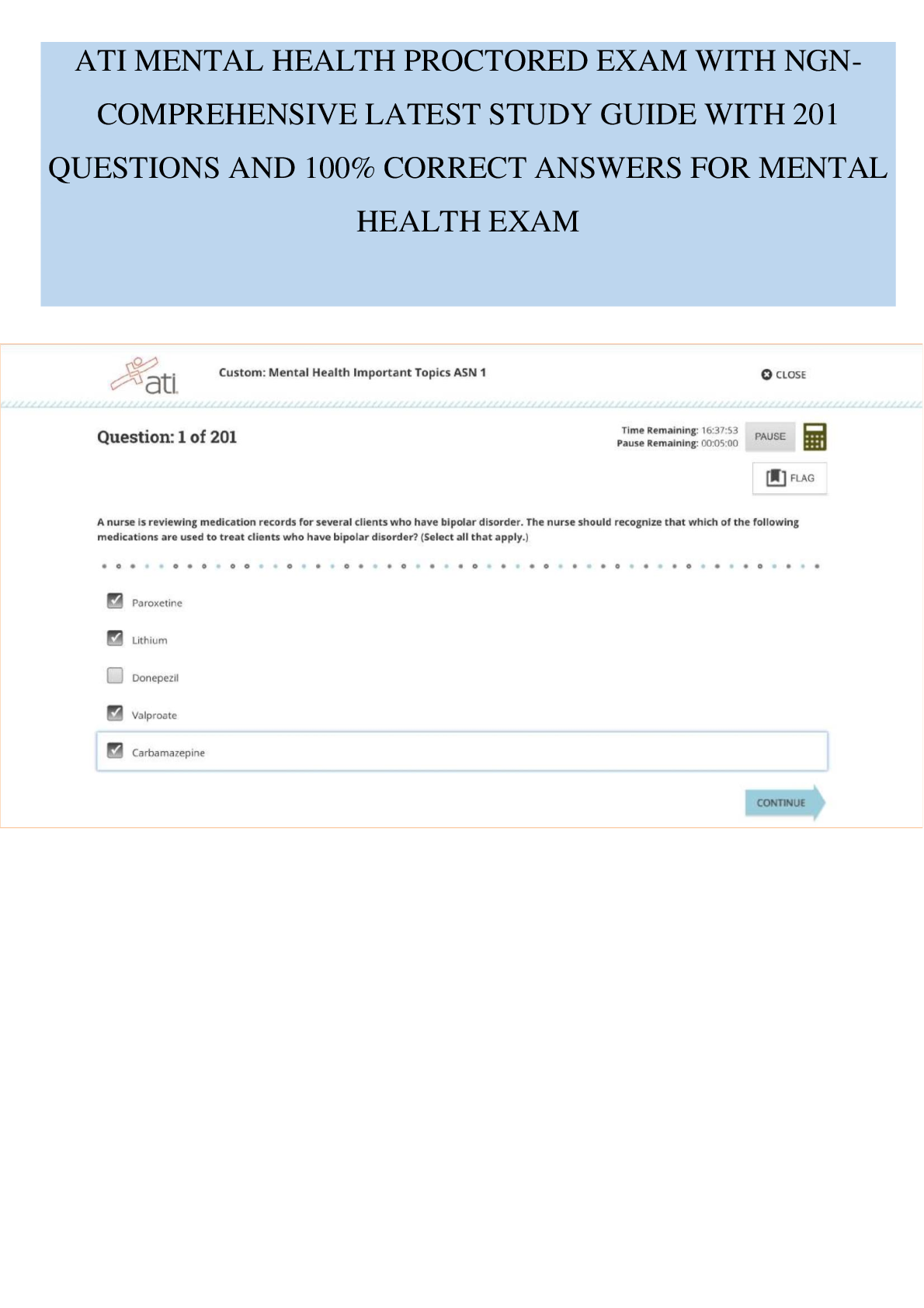
Bipolar disorders
Bipolar disorders are mood disorders with periods of depression and mania. Clients have a high risk for injury during the manic phase related to decreased sleep, feelings of grandiosity and impulsivity. Hospitalization is often required and nurses should provide for client safety.
abuse
There are several different types of abuse, including physical, sexual, or emotional. Abuse tends to be cyclic, following a pattern on tension building, battering and honeymoon phase. When test questions appear related to abuse, look for the phase to determine the correct response.
violent clients
For the aggressive or violent client, setting boundaries and limits on behavior are important. The nurse should maintain a calm approach and use short, simple sentences.
SSRI's
SSRIs: Selective Serotonin Reuptake Inhibitors. These medications include Citalopram (Celexa), Fluoxetine (Prozac), or Sertraline (Zoloft). The client should avoid using St. John's Wort with these medications, and should eat a healthy diet while on these medications.
TCAs
TCAs: Tricyclic Antidepressants. Amitriptyline (Elavil) is an example. Anticholinergic effects and orthostatic hypotension may occur.
MAOIs
MAOIs: Monoamine Oxidase Inhibitors. Phenelzine (Nardil) is an example. Hypertensive crisis may occur with tyramine food ingestion, so care must be taken to avoid these substances.
Educate the client to avoid all medications until discussed with provider.
Atypical antidepressants
Atypical antidepressants. Bupropion (Wellbutrin) is the most common example. Appetite suppression is a common side-effect. Headache and dry mouth may be severe and client should notify the provider if this occurs. Atypical antidepressants should not be used with clients with seizure disorders.
SNRI's
Serotonin Norepinephrine Reuptake Inhibitors. Common SNRIs include Venlafaxine (Effexor) and Duloxetine (Cymbalta). Adverse effects may include nausea, weight gain, and sexual dysfunction.
Antagonists
In order to understand how antagonist drugs work, you need to understand how agonist drugs produce therapeutic effects. Agonists are simply drugs that allow the body's neurotransmitters, hormones, and other regulators to perform the jobs they are supposed to perform. Morphine
sulfate, codeine, and meperidine (Demerol) are opioids agonists that act on the mu receptors to produce analgesia, respiratory depression, euphoria, and sedation. These drugs also work on kappa receptors, resulting in pain control, sedation and decreased GI motility. Antagonists, on the other hand, are drugs that prevent the body from performing a function that it would normally perform. To quote William Shakespeare & the US Army, these drug classes allow the body's functions "to be or not to be...all that they can be".
Common uses of antagonists:
· Treatment of opioids overdose, reversal of effects of opioids, or reversal of respiratory depression in an infant
· Example: a post-operative client receiving morphine sulfate for pain control experiences respiratory depression and is treated with naloxone (Narcan)
Nursing Interventions for antagonists:
· Monitor for side/adverse effects
· Tachycardia and tachypnea
· Abstinence syndrome in clients who are physically dependent on opioids agonists
· Monitor for symptoms to include cramping, hypertension, and vomiting
· Administer naloxone by IV, IM or subcutaneous routes, not orally
· Be prepared to address client's pain because naloxone will immediately stop the analgesia effect of the opioid the client had taken
· When used for respiratory depression, monitor for return to normal respiratory rate (16-20/min for adults; 40-60/min for newborns)
Antidotes
Antidotes are agents given to counteract the effects of poisoning related to toxicity of certain drugs or substances. Antidotes are extremely valuable, however most drugs do not have a specific antidote.
Atropine--> is the antidote for muscarinic agnostic and cholinesterase inhibitors: Bethanechol (Urecholine), Neostigmine (Prostigmin)
Physostigmine (Antilirium)--> is the antidote for anticholinergic drugs, atropine. Digoxin immune Fab (Digibind)--> is the antidote for digoxin, digitoxin Vitamin K--> is the antidote for Warfarin (Coumadin)
Protamine sulfate--> is the antidote for Heparin
Glucagon--> is the antidote for insulin-induced hypoglycemia Acetylcysteine (Mucomyst)--> is the antidote for acetaminophen (tylenol) Bronchodilators
Bronchodilators are used to treat the symptoms of asthma that result from inflammation of the bronchial passages, but they do not treat the inflammation. Therefore, most clients with asthma take an inhaled glucocorticoid concurrently to provide the best outcomes. The two most common classes of bronchodilators are beta2-adrenergicagonists and methylxanthines.
Beta2-adrenergic agonists : act upon the beta2-receptors in the bronchial smooth muscle to provide bronchodilation and relieve spasm of the bronchial tubes, inhibit release of histamines and increase motility of bronchial cilia. These short-acting preparations provide short-term relief during an asthma exacerbation, while the long-acting preparations provide long-term control of asthma symptoms.
The generic names for the inhaled form of these drugs end in"terol" = " T aking E ases R espiratory distress o r L abored breathing"
· Albu terol (Proventil, Ventolin)
· Formo terol (Foradil Aerolizer)
· Salme terol (Serevent)
The brand names of some drugs in this class provide a hint as well because they contain the words "vent " or " breth " referring to ventilation or breathing:
· Albuterol (Pro vent il, Vent olin)
· Salmeterol (Sere vent )
· Terbutaline ( Breth ine)
Nursing interventions and client education:
· Short-acting inhaled preparations of albuterol (Proventil, Ventolin) can cause systemic effects of tachycardia, angina, and tremors.
· Monitor client's pulse rate before, during, and after nebulizer or inhaler treatments
· Long-acting inhaled preparations can increase the risk of severe asthma or asthma-related death if used incorrectly—mainly if used without concurrent inhaled glucocorticoid use
· Oral preparations can cause angina pectoris or tachydysrhythmias with excessive use
· Instruct clients to report chest pain or changes in heart rate/rhythm to primary care provider
· Client should be taught proper procedure when using metered dose inhaler (MDI) and spacer
· If taking beta2-agonist and inhaled glucocorticoid concurrently, take the beta2-agonist first to promote bronchodilation which will enhance absorption of the glucocorticoid
· Advise client not to exceed prescribed doses
· Advise client to observe for signs of impending asthma attacks and keep log of frequency and intensity of attacks
· Instruct to notify primary care provider if there is an increase in frequency or intensity of asthma attacks
Methylxanthines: cause bronchial smooth muscle relaxation resulting in bronchodilation.
Theophylline (Theolair) is the prototype medication and is used for long-term control of chronic asthma
Nursing interventions:
· Monitor serum levels for toxicity at levels >20 mcg/mL
· Mild toxicity can cause GI distress and restlessness
· Moderate to severe toxicity can cause dysrhythmias and seizures
· Educated client regarding potential medication and food interactions that can affect serum theophylline levels
· Caffeine, cimetidine (Tagamet), and ciprofloxacin (Cipro) can increase levels
· Phenobarbital and phenytoin can decrease levels ACE inhibitors
ACE inhibitors block the production ofangiotensin II which results in vasodilation, sodium and water excretion, and potassium retention. Drugs in this class are used for treating heart failure, hypertension, myocardial infarction, and diabetic or nondiabetic nephropathy. Clients taking captopril (Capoten) should be instructed to take med at least 1 hour before meals; all other ACE inhibitors are not affected by food.
The generic names of ACE inhibitors end in "pril":
· Capto pril (Capoten)
· Enala pril (Vasotec)
· Fosino pril (Monopril)
· Lisino pril (Prinivil)
· Rami pril (Altace) Side/adverse effects include:
· Orthostatic hypotension with first dose
· Instruct client to monitor BP for at least 2 hours after first dose
· Cough, rash or altered or distorted taste (dysgeusia)
· Instruct client to notify health care provider
· Angioedema
· Treated with epinephrine and symptoms will resolve once medication is stopped
· Neutropenia is rare but serious with captopril (Capoten)
· Instruct client to report signs of infection Hyperkalemia can be life-threatening
Monitor potassium levels to maintain normal range of 3.5-5.0 mEq/L Medication/food interactions:
· Concurrent use with diuretics can lead to first-dose orthostatic hypotension
· Concurrent use with other antihypertensives can lead to increase effect resulting in hypotension
· Concurrent use with potassium supplements or potassium-sparing diuretics increases the risk of hyperkalemia
· Concurrent use with lithium can increase serum lithium levels, leading to lithium toxicity
· Concurrent use with NSAIDs can decrease the therapeutic effects of the ACE inhibitor Vasodilators
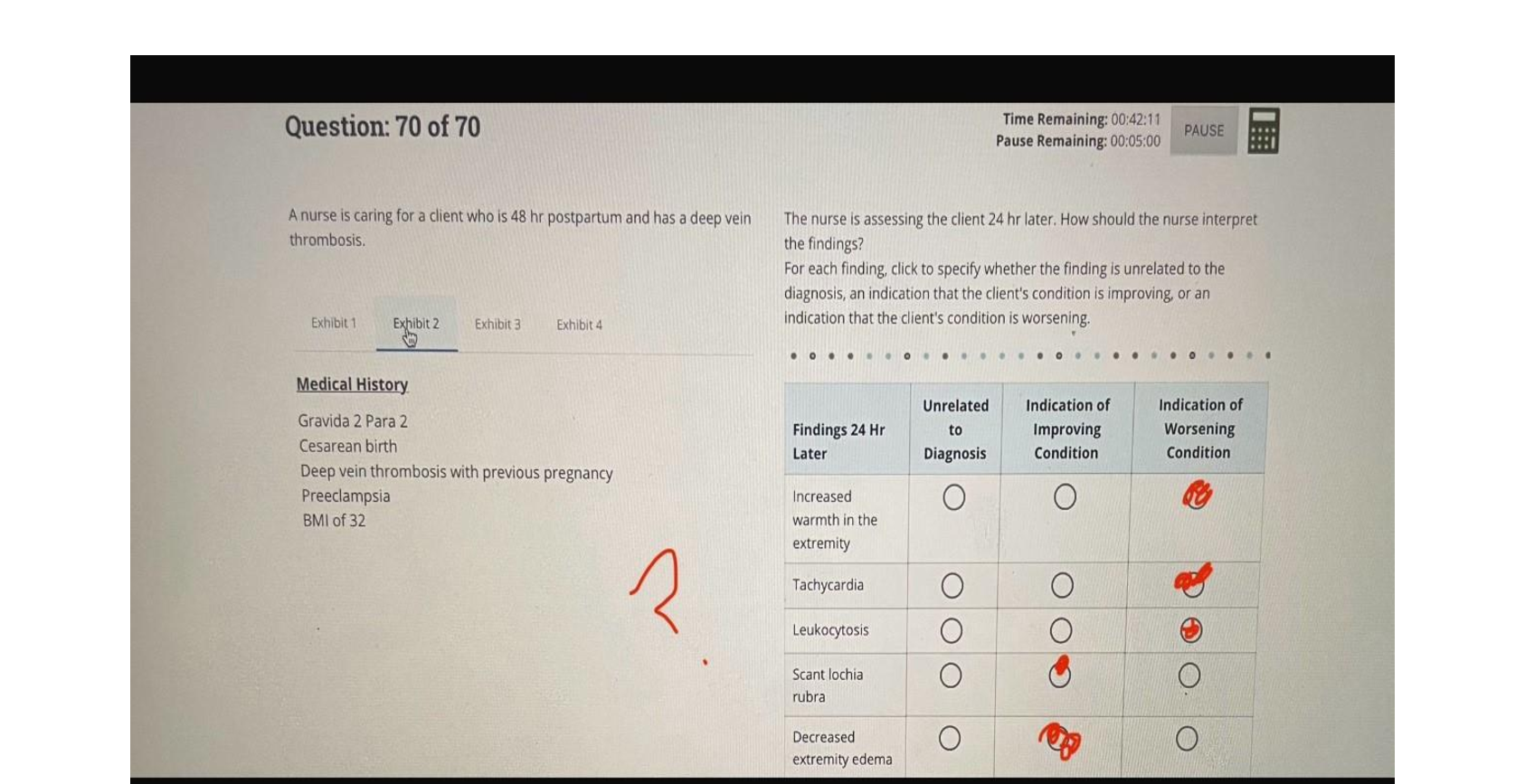
Blood Transfusion - Types of reactions and onset Acute hemolytic - immediate
Febrile - 30 min to 6 hr after transfusion Mild allergic - During or up to 24 hr after transfusion
Anaphylactic - immediate
Blood Transfusion Reaction - Medications Antipyretics (acetaminophen [Tylenol])
- febrile
Antihistamines (diphenhydramine [Benadryl]) - mild allergic
Antihistamines, corticosteroids, vasopressors - anaphylactic
Blood Transfusion - Potential Complications Circulatory overload:
Administer oxygen.
Monitor vital signs.
Slow the infusion rate.
Administer diuretics as prescribed. Notify the provider immediately
Blood Transfusion - Sepsis and septic shock Maintain patent airway.
Administer oxygen.
Administer antibiotics as prescribed. Obtain blood samples for culture.
Administer vasopressors in late phase. Elevate client's feet.
Assess for disseminated intravascular coagulation.
Digoxin - Take apical pulse for 1 min, and monitor laboratory levels for signs of toxicity. Digoxin - Instruct the client not to take medication within 2 hr of eating, and teach client how to take an apical pulse for 1 min.
Sodium polystyrene - Instruct the client to take a mild laxative if constipated, and teach how to take blood pressure
Sodium polystyrene - Monitor for hypokalemia, and restrict sodium intake.
Epoetin alfa - Instruct the client about having blood tests twice a week and how to take blood pressure.
Epoetin alfa - Administer by subcutaneous route, and monitor for hypertension.
Ferrous sulfate - Instruct the client to take medication with food and that stools will be dark in color.
Ferrous sulfate - Administer following dialysis and with a stool softener
Aluminum hydroxide gel - Avoid administering if client has gastrointestinal disorders; administer a stool softener with this medication
Aluminum hydroxide gel - Instruct the client to report constipation to the provider and to take 2 hr before or after receiving digoxin.
Furosemide - Monitor intake and output and blood pressure.
Furosemide - Instruct the client to weigh self each morning and to notify provider of light
-
-
-
-
-
-
-
-
-
-
-
Ventilator Alarms
-Low Pressure
-High Pressure
-Low: disconnection
-High: suction for possible secretions, kinks.
Glasgow Coma Scale (head injuries) (eyes, verbal, motor)
highest number 15, good. lowest number 3, severe.
Pressure Ulcer Strategies
-Reposition time (bed/chair)
-Incontinent Pt.
-Bed every 2hr, chair every hour.
-Apply barrier cream and moisture absorbing pad.
Immunization: booster every 10 years DTP
HPV vaccination doses 3 doses
How to measure Fundal Height
top of symphysis pubis to top of fundus
How to calculate due date: LMP 8/2/15
-subtract 8-3=5
-add 7 + 2= 9
May 9, 2016
Contraindicated Immunizations During Pregnancy
-Varicella
-Zoster
-MMR
True Labor vs False Labor Abdominal Discomfort true: low back and abdominal
false: abd and groin
Types of Decelerations: <120 fhr
-early
-late
-variable
-early: head compression
-late: uteroplacental insufficiency
-variable: cord compression
Nursing Interventions during late or variable deceleration left lateral position, oxygen, c-section
Normal Fetal HR 120-160
Nursing Care for Boggy Uterus
Ask pt to void; if still boggy massage top of fundus with fingers and reassess every 15 mins.
Nursing Care for Engorgement
Apply moist heat for 5 min before breastfeeding.
Ice compresses after feeding to reduce discomfort and swelling.
Nursing Care for Mastitis
Continue breastfeeding and take antibiotics as prescribed.
Narcotic antidote Naloxone (narcan)
What is wrong with the script? gentamicin 50 mg po every 4 hours #30 Drug name: Gentamicin (capital G)
Anemia lab RBC 4.20-4.87
BUN/Creatinine normal values (for kidney function)
7-20/0.8-1.4
WBC normal values (for infection)
4,000-10,000
Sodium 136-144
Potassium 3.5-5.5
Chloride 96-106
Be ready to administer for Magnesium sulfate toxicity Calcium gluconate
Sign of mag sulfate toxicity (4)
1. Absent deep tendon reflexes 2.Resp rate < 12
3. Urine output < 30 4.Mag levels above 8
Understanding Rh.
Administration of antibody and time. Mother Rh negative.
Fetus Rh positive.
Rhogam at 28 weeks, then 72 hrs after birth. Stroke eating precautions
-check gag reflex
-thickened fluids/puree
-Sit upright/flexed neck forward
Dehydration S&S (hypovolemia)
-pulse; weak and thready. hypotension
-tachy
-confused
-decreased urine output
-skin and mucous membranes dry Urine Specificity increased
Urine Specific Normal Values and Significance Decreased hypervolemia.
Increased hypovolemia.
1.001-1.029
JVD. What side of heart? Right
Adverse effect of ACE inhibitor (pril's)
ACE inhibitors,
[Show More]








 – University of the People.png)