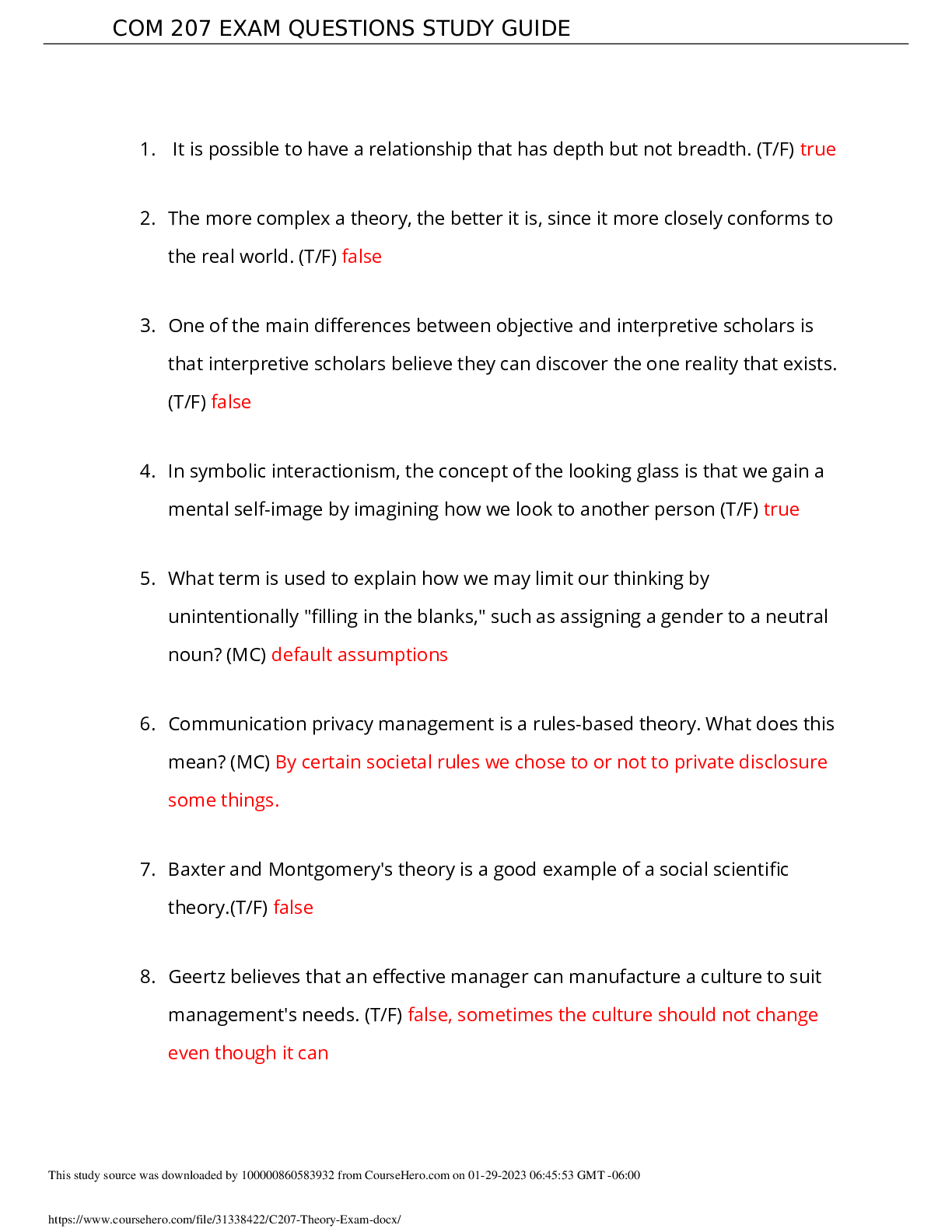
*NURSING > EXAM > NUR 204 Exam 1 TestBank Questions and Answers with Explanations Chapters 11, 19, 22, to 24 (All)
NUR 204 Exam 1 TestBank Questions and Answers with Explanations Chapters 11, 19, 22, to 24
Document Content and Description Below
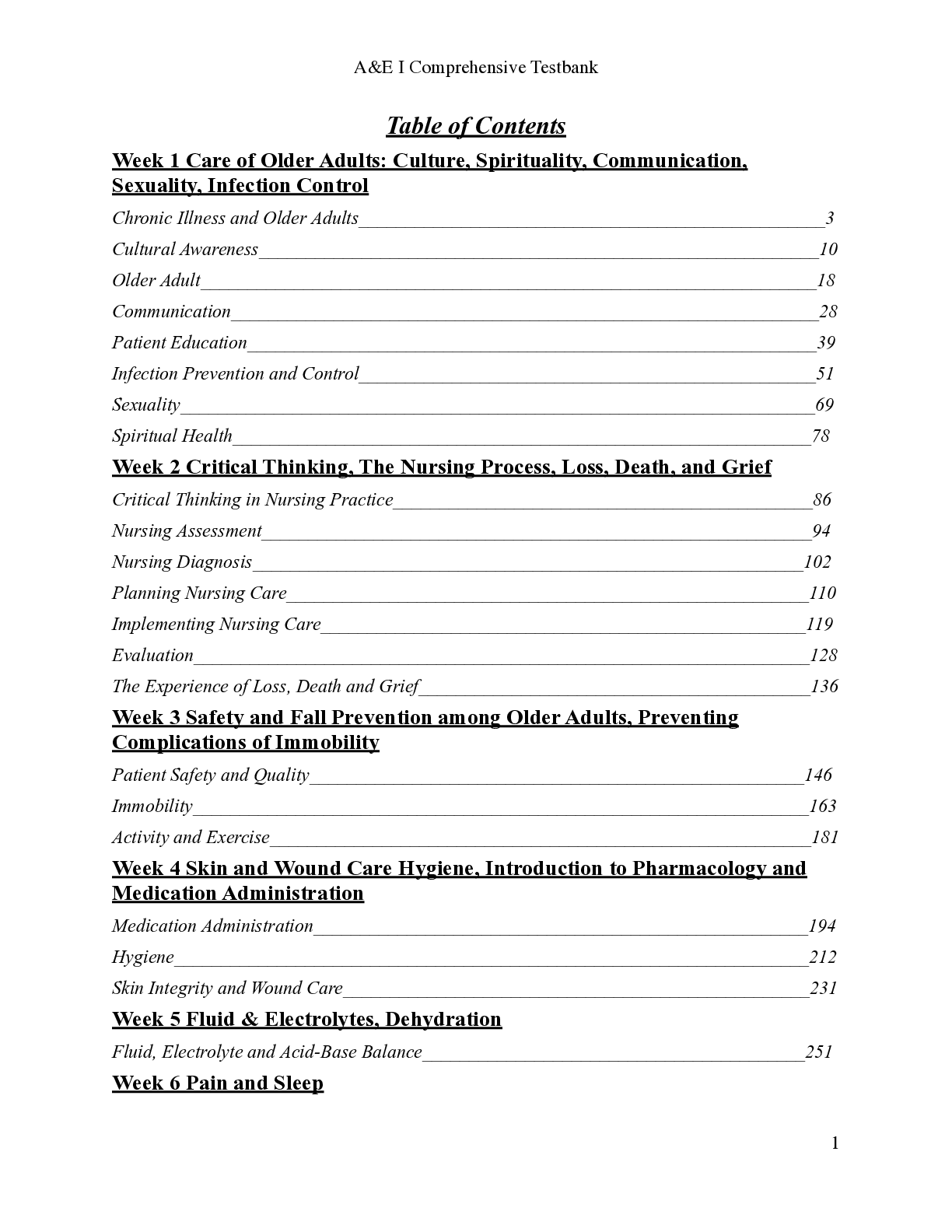
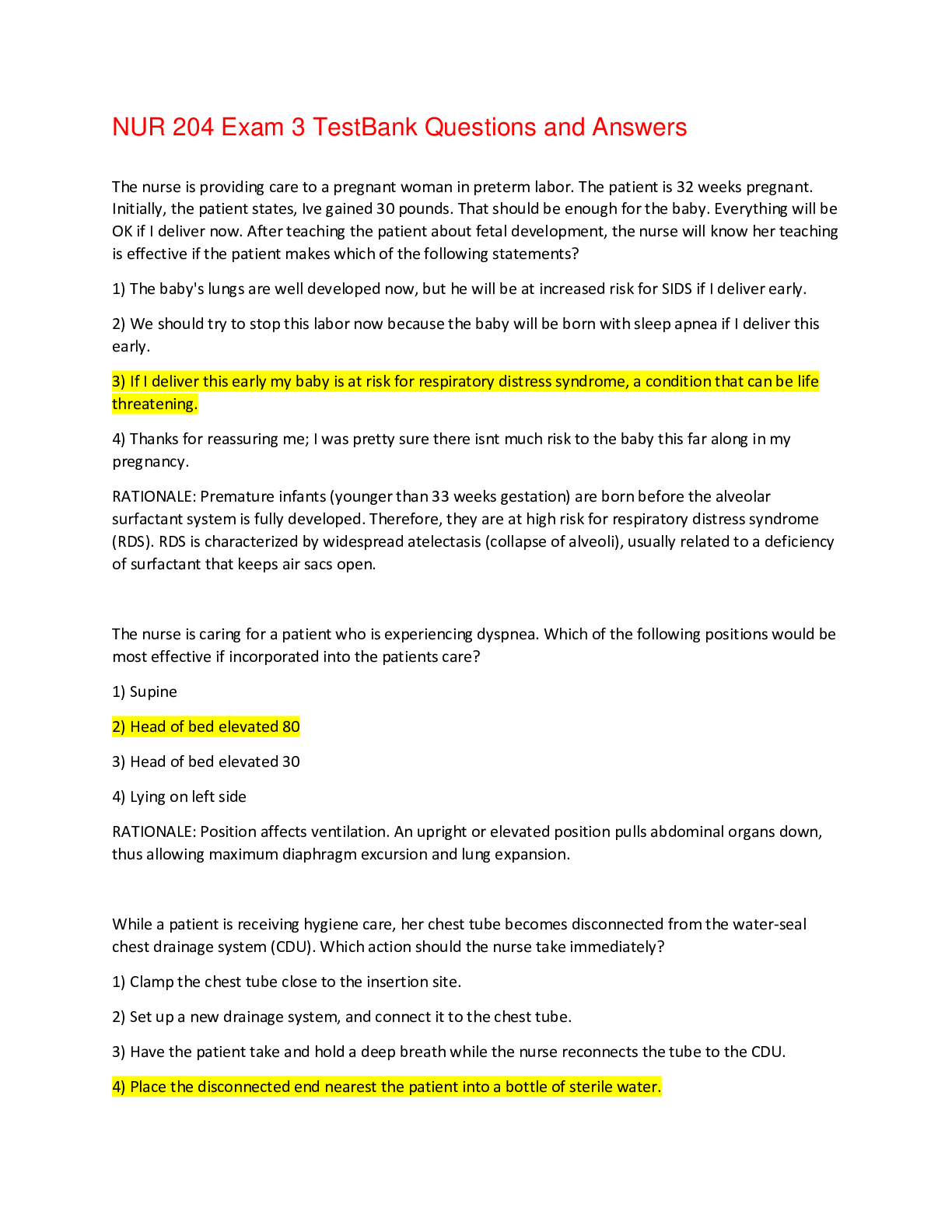
NUR 204 Exam 1 TestBank Questions and Answers with Explanations Chapters 11, 19, 22, to 24 Which area(s) should the nurse inspect when assessing for cyanosis in a dark-skinned patient? Select all tha... t apply. 1) Buccal mucosa 2) Around the lips 3) Palms 4) Tongue ANS: 1, 3, 4 In dark-skinned people, cyanosis can be best assessed by examining the palms of the hands, soles of the feet, tongue, conjunctivae, or the buccal mucosa. In light-skinned people, the nailbeds and the area around the lips can be used. In an effort to promote health, the home health nurse opens the clients bedroom windows to let in fresh air and sunlight, washes her hands often, and teaches the patient and family about the importance of hygiene and cleanliness. This most closely illustrates the ideas of which of the following people? 1) Jean Watson 2) Jurgen Moltmann 3) Florence Nightingale 4) Robert Louis Stevenson ANS: 3 Florence Nightingale believed that health was prevention of disease through the use of fresh air, pure water, efficient drainage, cleanliness, and light. Jean Watson believes that health has three elements: a high level of overall physical, mental, and social functioning; a general adaptive-maintenance level of daily functioning; and the absence of illness (or the presence of efforts that lead to its absence). Jurgen Moltmann believes that true health is the strength to live, the strength to suffer, and the strength to die. He also stated that health is not a condition of my body; it is the power of my soul to cope with the varying condition of that body. Robert Louis Stevenson wrote that health is not a matter of holding good cards; it is playing a poor hand well. The clients temperature is 101.1F. Which is the correct conversion to centigrade? 1) 38.0C 2) 38.4C 3) 38.8C 4) 39.2C ANS:2 To convert Fahrenheit to centigrade, subtract 32 from the temperature, and multiply by 5/9. Which of the following is known to be a healthy strategy for coping with stress? 1) Performing meaningful work 2) Consuming simple carbohydrates 3) Drinking three glasses of red wine each day 4) Weight training ANS: 1 Many individuals find that meaningful work is a healthy way to cope with stressors. Consuming simple carbohydrates is not a healthy way to cope with stress. Drinking more than one glass of red wine each day is considered unhealthy. Weight training has been shown to increase bone density and reduce the risk of osteoporosis and heart disease but not necessarily to reduce stress. Which family would most likely be helpful in encouraging the client to experience a high level of wellness? A family who: 1) Controls feelings in order to avoid conflict. 2) Teaches negotiation skills and independence. 3) Encourages risk-taking and adventure. 4) Views themselves as helpless victims. ANS: 2 Families who promote independence and teach good negotiation skills enable family members to experience a high level of wellness by thinking for themselves. In contrast, families who tend to squelch personal feelings to avoid conflict may not allow a high level of wellness. Families who emphasize caution in new situations are more beneficial than those who encourage risk-taking. Families who view themselves as capable and successful are more advantageous than those who view themselves as helpless victims. The client is a 76-year-old man who is experiencing chronic illness. He has a genetic-linked anemia. He says he does not eat a balanced diet, as he prefers sweets to meat and vegetables. Which of the following dimensions of health can the nurse most likely influence by teaching and counseling him? 1) Age-related changes 2) Genetic anemia 3) Eating habits 4) Gender-related issues ANS: 3 The nurse is most likely to influence the patients eating habits because those are the dimension over which he has the most control and, therefore, has the most potential for changing. Although people consider biological factors when they describe themselves as well or ill, they are not entirely within our control. Biological factors include age and developmental stage, genetic makeup, and gender. What type of loss is most common among patients who are hospitalized for complex health conditions? 1) Privacy 2) Dignity 3) Functional 4) Identity ANS: 2 Hospitalized patients commonly experience the loss of dignity. Wearing a hospital gown, having their body exposed, invasive procedures, loss of control over body functions all of these contribute to loss of dignity, and all are very common among hospitalized patients. Healthcare providers have a duty to protect privacy and confidentiality of patients, even though it is certainly threatened by some situations during hospitalization. Some patients lose functioning and identity during hospitalization, but they are not common occurrences. A 62-year-old patient is admitted to the hospital with hypertension. Which question by the nurse is most important when performing the initial assessment interview? 1) What medications do you take at home? 2) Do you have any environmental, food, or drug allergies? 3) Do you have an advance directive? 4) What is the greatest concern you are dealing with today? ANS: 4 It is most important for the nurse to ask the patient about his greatest concern. His concern can then be incorporated into the plan of care, making sure that his needs are met. Asking about medications, allergies, and an advance directive is also important but does not take priority over asking about the patients greatest conc When developing goals, which guideline should the nurse keep in mind? Goals should be: 1) Realistic so that progress is recognized by the patient 2) Developed solely by the healthcare team 3) Developed without family input, to maintain confidentiality 4) Valued by the multidisciplinary care providers ANS: 1 Goals should be realistic so that progress is recognized by the patient. They should be valued by both the patient and family. The nurse should develop goals with input from the patient and his family. Which one of the following important nursing actions is a hospitalized patient likely to experience on an emotional level and remember long after this hospitalization has ended? 1) Administering her medications according to schedule 2) Allowing flexible visitation by her family and friends 3) Explaining treatment options in terms she can understand 4) Providing a healing presence by listening and being attentive ANS: 4 The nurse can contribute meaningfully to the patients hospitalization by providing a healing presence. The nurse can do this by listening to the patient and being attentive. Administering medications according to schedule, allowing flexible visitation, and explaining treatment options are important contributions that the nurse can make, but they will not be most meaningful to the patient. Patients may be impressed, even amazed, by the healthcare technology used to diagnose and treat their illness. However, often what they remember, perhaps through the rest of their lives, is the person who connected with them in a personal way. Which statement best describes the health illness continuum? 1) Health is the absence of disease; illness is the presence of disease. 2) Health and illness are along a continuum that cannot be divided. 3) Health is remission of disease; illness is exacerbation of disease. 4) Health is not having illness; illness is not having health. ANS: 2 The health-illness continuum is best described as a graduated spectrum that cannot be divided. Which of the following helps the body release growth hormone (growth hormone assists in tissue regeneration, synthesis of bone, and formation of red blood cells)? 1) A healthy diet 2) Physical activity 3) Restful sleep 4) Comfortable room temperature ANS: 3 During sleep, our bodies release the majority of our growth hormone, which assists in tissue regeneration, synthesis of bone, and formation of red blood cells. Consuming healthy foods helps prevent disease. Physical activity reduces the risk of chronic disease and promotes longevity. Keeping the body at a comfortable temperature helps maintain health but not release of growth hormone. A client has been hospitalized for 6 weeks. All of the following interventions are good ones; but which intervention is specifically focused on helping the patient cope with the emotional responses to prolonged hospitalization? 1) Providing skin care every shift to prevent skin breakdown 2) Encouraging the patient to get up in a chair to eat meals 3) Assisting the patient to ambulate in the hallway for several minutes each day 4) Designating a corner of the patients room to display personal mementos ANS: 4 The patients environment can help nourish wellness. Helping the patient designate a corner of the room to display personal mementos can be healing and help the patient cope with the prolonged hospitalization. The other interventions might be helpful to the patient but are not as helpful in specifically dealing with hospitalization as is designating a portion of the room that is uniquely hers. Which of the following is particularly valuable in helping a patient with a terminal illness maintain a sense of self? 1) Family relationships 2) Spirituality 3) Nutrition 4) Sleep and rest ANS: 2 When patients are faced with a terminal illness, spirituality can help the patient maintain his sense of self. Family relationships can provide a loving, supportive source of comfort and reassurance, but sometimes cause the patient pain and a feeling of loneliness when faced with a terminal illness. Nutrition, sleep, and rest are healing but usually not as helpful to a patient with terminal illness as is spirituality. A client with a history of schizophrenia is diagnosed with a urinary tract infection. What is probably the most significant barrier this patient faces? 1) Chronic urinary incontinence 2) Stigma associated with mental illness 3) Risk for recurring infections 4) Auditory hallucinations (hearing things) ANS: 2 Mental illness is associated with a stigma that is usually a barrier, and even considered a debilitating handicap. Chronic urinary incontinence is not commonly associated with urinary tract infection, and nothing in the scenario suggests that the patient is incontinent. The patient is at risk for recurring urinary tract infections, but this is not considered a debilitating handicap. Auditory hallucinations are associated with schizophrenia but have not been described as the most debilitating handicap. A 76-year-old patient is admitted with an acute myocardial infarction (heart attack). The doctor tells the patient that an angioplasty is necessary. The patient agrees and signs the informed consent. This patient is experiencing which stage of illness behavior? 1) Sick-role behavior 2) Seeking professional care 3) Experiencing symptoms 4) Dependence on others ANS: 4 This patient is experiencing the dependence-on-others stage of illness behavior; he has accepted the diagnosis and treatment of the healthcare provider. The patient entered the experiencing illness stage when he began having chest pain at home. He entered the sick-role behavior phase when he admitted to family that he was experiencing chest pain. When he decided to go to the emergency department for health care intervention, he entered the seeking-professional-care stage of illness. Many health providers define illness as pathology; however, people experience, rather than define, illness. Which of the following is how most people experience illness? 1) Feeling lousy, a true sense of not being all right 2) A change in the way they feel or a disruption in their typical life 3) Something to be dreaded and avoided if at all possible 4) An experience that offers the potential for learning and spiritual growth ANS: 2 People typically describe their illness in terms of how it makes them feel or the effect it has on day-to-day life. Feeling lousy is inappropriate as many people do not feel lousy when they are ill. For example, hypertension is an illness that may have no symptoms. Similarly, patients may have chronic disease that is well managed and therefore does not make them feel ill. Something to be dreaded and avoided . . . is also not accurate. If a person has an external locus of control, he may view illness as a consequence of actions taken. From this viewpoint, he may have little control over whether he can avoid illness. Finally, although some people do grow and learn in the face of illness, most people do not hold such a positive view about illnessand the question asks how people experience illness. Dunn believes that an individuals state of health should be evaluated in the context of the persons environment. This approach illustrates that: 1) An unhealthy physical environment, characterized by poor living conditions, always has a negative effect on an individuals health. 2) Adequate income, food, and shelter create a healthful environment and always improve physical health status. 3) Physical environment, family, and social support may help or hinder the health status of an individual. 4) The environment that should always be assessed is the clients immediate surroundings; extended boundaries do not apply in an ill state. ANS: 3 The home environment, community, family, friends, and support system all influence health status. The balance among these variables has a net positive or negative effect on a clients health status. The effect of poor living conditions may be offset by the presence of loving family and friends. Poverty does not always have a negative effect on health. Similarly, the presence of food, shelter, and clothing does not always convey protective health, as loneliness and hopelessness may counteract these positive influences. When examining the clients environment, extended boundaries must be considered, especially when providing community-based care. Some people readily become ill when under stress. Others are able to deal with tremendous stress and remain physically and mentally healthy. This disparity is affected by a persons level of hardiness. How can you apply this knowledge to your nursing care? 1) You cannot use this information at all. People are innately hardy or not. This is something that you must merely recognize. 2) You should encourage all people to develop some level of hardiness in order to get through difficult physical and emotional times. 3) You should assess for your own level of hardiness: if you are hardy, you will be a better nurse; if you are not, you can learn more about hardiness. 4) You can assess for hardiness in patients; you can encourage hardy patients to learn about their illness as a means for them to be more comfortable. ANS: 4 Hardiness is a personality trait that helps many cope with stress and illness. As a personality trait, it is unlikely that you can teach or otherwise encourage this trait. Awareness of your own level of hardiness will help you understand your response to stress, but hardiness does not necessarily make you a better nurse. When preparing a room to receive a newly admitted patient, which of the following should the nursing assistive personnel (NAP) do? 1) Mop the floor with an approved disinfecting solution. 2) Fold the top bed linens back to open the bed. 3) Hook up the suction machine and check to see that it is working. 4) Position the bed in its lowest position. ANS: 2 The NAP should create an open bed. The housekeeping department is almost always responsible for cleaning the room between patients. The nurse is responsible for hooking up and checking special equipment such as suction. The nurse would need to tell the NAP whether the patient is to be admitted ambulatory, by wheelchair, or by stretcher in order to know whether to position the bed high or low. When transferring a patient from a hospital to a long-term care facility, which of the following is most helpful in facilitating the patients planning and emotional adjustment? 1) Notify the patient and family as much in advance of the transfer as possible. 2) Send a complete copy of the patients medical records to the new facility. 3) Carefully coordinate the transfer with the long-term facility to keep it smooth. 4) Help arrange for transportation and accompany the patient to the transport vehicle. ANS: 1 Notifying the patient and family well in advance of the transfer allows them time to adjust emotionally and to make any necessary plans. A copy of the records is usually sent, and the nurse does coordinate the transfer with the receiving facility; however, that does very little to assist with the patients emotional status or planning. Someone from the hospital may accompany the patient to the car; or if the transfer is by ambulance, perhaps not. Either way, that will not help the patient and family to do the necessary planning for the transfer. A 36-year-old mother of three small children has had nausea, vomiting, and extreme fatigue for the past 2 days. She calls her mother and tells her she is ill and asks if her mother can care for the children. Which stage of illness behavior is she experiencing? Choose all that apply. 1) Sick-role behavior 2) Dependence on others 3) Seeking professional care 4) Experiencing symptoms ANS: 1 The 36-year-old mother is assuming sick-role behavior because she is identifying herself as ill. She is also in the stage of experiencing symptoms; she is experiencing symptoms and realizes that illness is starting, even though she has not yet entered the stages of dependence and seeking professional care. By telling her mother of the illness, she is relieved of her normal duties, caring for her children. Dependence on others occurs when the client accepts a diagnosis and treatment from the health care provider. Seeking professional care occurs after the sick-role behavior stage. During this stage, the client makes the decision that she is ill and that professional healthcare is needed. A clients vital signs at the beginning of the shift are as follows: oral temperature 99.3F (37C), heart rate 82 beats/min, respiratory rate 14 breaths/min, and blood pressure 118/76 mm Hg. Four hours later the clients oral temperature is 102.2F (39C). Based on the temperature change, the nurse should anticipate the clients heart rate would be how many beats/min? 1) 62 2) 82 3) 102 4) 122 ANS: 3 Heart rate increases about 10 beats per minute for each degree of temperature to meet increased metabolic needs and compensate for peripheral dilation. The nurse is assessing vital signs for a client after surgical procedure on the left leg. IV fluids are infusing. It would be most important for the nurse to 1) Compare the left pedal pulse with the right pedal pulse 2) Count the clients respiratory rate for 1 full minute 3) Take the blood pressure in the arm without an IV 4) Take an oral temperature with an electronic thermometer ANS: 1 For a client having surgery on the leg, the most important data would be whether the circulation has been compromised because of the surgery. This can be done only by comparing one leg with the other. The nurse would, of course, count the respiratory rate for 1 full minute and take the BP in the arm without the IV. Oral temperatures are commonly obtained using electronic thermometers. The nurse hears rhonchi when auscultating a clients lungs. Which nursing intervention would be appropriate for the nurse to implement before reassessing lung sounds? 1) Have the client take several deep breaths. 2) Request the client take a deep breath and cough. 3) Take the clients blood pressure and apical pulse. 4) Count the clients respiratory rate for 1 minute. ANS: 2 Rhonchi are caused by secretions in the large airways and may clear with coughing. This is how you differentiate between rhonchi and other adventitious sounds. Deep breathing will not help to clear rhonchi. Taking the blood pressure and apical pulse and counting the respiratory rate are not effective for clearing rhonchi and would not be sufficient for the nurse to identify whether the sounds were, indeed, rhonchi. Which of the following sets of vital signs are all within normal limits for patients at rest? 1) Infant: T 98.8F (rectal), HR 160, RR 16, BP 120/54 2) Adolescent: T 98.2F (oral), HR 80, RR 18, BP 108/68 3) Adult: T 99.6F (oral), HR 48, RR 22, BP 130/84 4) Older adult: T 98.6F (oral), HR 110, RR 28, BP 170/95 ANS:2 All of the adolescents vital signs are within normal parameters for the age. The infants temperature is below normal for a rectal reading because the core temperature is approximately 1 degree higher than readings from other sites. The heart rate (HR) for an infant is high, the respiratory rate (RR) is low, and the blood pressure (BP) is high for the age. For the typical adult, the temperature is high, the HR is low, the RR is high, and the BP is elevated for the age. For the older adult, the temperature is high-end normal, the HR is high, the RR is high, and the BP is high for the age. The nurse assesses the following changes in a clients vital signs. Which client situation should be reported to the primary care provider? 1) Decreased blood pressure (BP) after standing up 2) Decreased temperature after a period of diaphoresis 3) Increased heart rate after walking down the hall 4) Increased respiratory rate when the heart rate increases ANS: 1 A drop in the clients blood pressure when standing indicates orthostatic hypotension, and the cause should be investigated. The changes in vital signs indicated in the other options are normal changes for the situations. The client has had a fever, ranging from 99.8F orally to 103F orally, over the last 24 hours. The clients fever would be classified as 1) Constant 2) Intermittent 3) Relapsing 4) Remittent ANS: 4 Remittent fevers fluctuate widely over a 24-hour period. Constant fevers stay above normal with only slight fluctuations. Intermittent fevers alternate between normal or subnormal temperatures with periods of fever. Relapsing fevers alternate between periods of fever and periods of normal temperature, each phase lasting 1 to 2 days. A clients vital signs 4 hours ago were temperature (oral) 101.4F (38.6C), heart rate 110 beats/min, respiratory rate 26 breaths/min, and blood pressure 124/78 mm Hg. The temperature is now 99.4F (37.4C). Based only on the expected relationship between temperature and respiratory rate, the nurse might best anticipate the clients respiratory rate to be 1) 16 2) 18 3) 20 4) 22 ANS:2 For every degree Fahrenheit (0.6C) the temperature falls, the respiratory rate may decrease up to 4 breaths per minute. The clients temperature has fallen 2 degrees; multiplied by 4, this is 8. It was 26 breaths/min: 26 8 = 18 breaths/min. Keep in mind, this is an estimate and would vary depending on the patients baseline health, current condition, age, and other factors. Which one of the following clients would probably have a higher than normal respiratory rate? A client who has 1) Had surgery and is receiving a narcotic analgesic 2) Had surgery and lost a unit of blood intraoperatively 3) Lived at a high altitude and then moved to sea level 4) Been exposed to the cold and is now hypothermic ANS: 2 A reduction in hemoglobin from blood loss would increase the respiratory rate. Narcotics and hypothermia slow the respiratory rate. Going from lower altitudes to higher altitudes inhibits oxygen binding, so going to a lower altitude would decrease the respiratory rate or have no effect. Hypothermia decreases the metabolic rate, so the respiratory rate would likely decrease. For which of the following adult clients should the nurse make follow-up observations and monitor the vital signs closely? A client whose 1) Resting morning blood pressure is 136/86 while the afternoon BP is 128/84 mm Hg 2) Oral temperature is 97.9F in the morning and 99.8F in the evening 3) Heart rate was 76 beats/min before eating and 88 beats/min after eating 4) Respiratory rate is 16 breaths/min when standing and 18 when lying down ANS: 1 Both the blood pressures would be classified as prehypertension according to the JNC 7 Express guidelines. Body temperature normally increases during the course of a day. Heart rate increases for several hours after eating. Respiratory depth decreases when lying down, so it would be normal for the rate would increase; both rates are within normal limits. A client who has been hospitalized for an infection states, The nursing assistant told me my vital signs are all within normal limits; that means Im cured. The nurses best response would be which of the following? 1) Your vital signs confirm that your infection is resolved; how do you feel? 2) I'll let your healthcare provider know so you can be discharged. 3) Your vital signs are stable, but there are other things to assess. 4) We still need to keep monitoring your temperature for a while. ANS: 3 Vital signs are one indicator of a clients physiological status, but they are not an absolute indicator of well-being from every aspect. It may be inaccurate to state that the vital signs indicate the infection is resolved; vital signs could stabilize even if the infection remains active. The healthcare providers decision regarding the clients readiness for discharge is not based exclusively on the vital signs but rather is based on a compilation of other sources of information, primarily the clients clinical status, but also cultures, complete blood counts, and various other laboratory and possibly radiologic evidence. Although the nurse will need to continue monitoring the temperature, other clinical signs must also be monitored; therefore, the statement We still need to keep monitoring your temperature . . . is incomplete and less useful than the statement that begins Your vital signs are stable, but . . . The nursing instructor asks students how they would assess the fifth vital sign. Which student would be correct? 1) I would have the client rate her pain on a scale of 0 to 10. 2) I would ask the client when she had her last bowel movement. 3) I would take the clients pulse oximetry reading. 4) I would interview the client about history of tobacco use. ANS: 1 Pain is considered to be the fifth vital sign. A clients axillary temperature is 100.8F. The nurse realizes this is outside normal range for this client and that axillary temperatures do not reflect core temperature. What should the nurse do to obtain a good estimate of the core temperature? 1) Add 1F to 100.8F to obtain an oral equivalent. 2) Add 2F to 100.8F to obtain a rectal equivalent. 3) Obtain a rectal temperature reading. 4) Obtain a tympanic membrane reading. ANS: 3 Body temperatures, from lowest to highest, are axillary, oral, rectal, and tympanic. For oral, axillary, and rectal temperatures, there is a 1F degree difference between each site and the next higher one. However, mathematical conversions between sites are not reliable and should be used only when a rough estimate is neededfor instance, to decide whether a reading needs to be validated by another site or another thermometer. Rectal temperatures are most reliable and most accurately reflect the core temperature. Tympanic membrane readings are considered by most to be the least accurate and least reliable. In caring for a client who has a fever, it would be important for the nurse to monitor for increased 1) Urine output 2) Sensitivity to pain 3) Blood pressure 4) Respiratory rate ANS: 4 The metabolic rate increases with a fever, increasing a persons respiratory rate. Urine output would more likely decrease, rather than increase, because of increased insensible loss and possible loss of intake because of loss of appetite. Change in pain sensation is not a symptom of a fever. Blood pressure is more likely to decrease with a fever because of peripheral vasodilation. The nurse is teaching a client how to use a portable blood pressure device to monitor his blood pressure at home. It would be most important for the nurse to 1) Ask the client to demonstrate the use of the blood pressure device 2) Explain the importance of frequent calibration of the device 3) Give the client a chart to record his blood pressure readings 4) Provide written instructions of the information taught ANS: 1 All are important things to include in client education, but self-monitoring of blood pressure is of little value unless it is done using proper technique. Requesting that the client demonstrate the procedure would allow the nurse to evaluate the clients technique. At last measurement, the clients vital signs were as follows: oral temperature 98F (36.7C), heart rate 76 beats/min, respiratory rate 16 breaths/min, and blood pressure (BP) 118/60 mm Hg. Four hours later, the vital signs are as follows: oral temperature 103.2F (38.5C), heart rate 76 beats/min, respiratory rate 14 breaths/min, and blood pressure 120/66 mm Hg. Which should be the nurses first intervention at this time? 1) Ask the client if he has had a warm drink in the last 30 minutes. 2) Notify the primary care provider of the clients temperature. 3) Ask the client if he is feeling chilled. 4) Take the temperature by a different route. ANS: 1 With a fever, the heart rate and respiratory rate are usually elevated. In this case, they are within normal limits, so the nurse should wonder about the accuracy of the temperature reading and validate it in some way. Because having a hot drink is a common cause of false readings, the nurse should determine whether that has occurred before retaking or otherwise validating the reading. A clients average normal temperature is 98F. Which of the following temperatures would be expected during the night in this healthy young adult client who does not have a fever, inflammatory process, or underlying health problems? 1) 97.2F 2) 98.0F 3) 98.6F 4) 99.2F ANS: 1 The lowest temperature occurs during sleep (usually at night) when the metabolic rate is lowest. Temperature normally increases throughout the day until it peaks in the early evening. The nurse is instructing a client how to appropriately dress an infant in cold weather. Which of the following instructions would be most important for the nurse to include? 1) Be sure to put mittens on the baby. 2) Layer the infants clothing. 3) Place a cap on the infants head. 4) Put warm booties on the baby. ANS: 3 All interventions are correct, but because of the many blood vessels close to the skin surface in the head, infants lose approximately one third of their body heat through the head. Therefore, to prevent heat loss, it is most important to cover the head. In evaluating a clients blood pressure for hypertension, it would be most important to 1) Use the same type of manometer each time 2) Auscultate all five Korotkoff sounds 3) Measure the blood pressure in both arms 4) Monitor the blood pressure for a pattern ANS: 4 Blood pressure fluctuates a great deal during the day and is influenced by age, sex, activity, and many other factors. Any determination of hypertension must be done after two or more BP readings taken on separate occasions. The type of manometer does not greatly influence the reliability of BP readings, although the mercury manometer is more accurate. Only the first and last Korotkoff sounds are necessary to determine a BP reading. The first time BP is assessed for a patient, the nurse should compare the reading in the left and right arm; however, this is not specific to evaluating for hypertension. Which of the following pieces of information in the clients health history might indicate a risk for primary hypertension? 1) Consumes a high-protein diet 2) Drinks three to four beers every day 3) Has a family history of kidney disease 4) Does not engage in physical exercise ANS: 2 Heavy alcohol consumption, age, race, high-sodium diet, tobacco use, family history of hypertension, and high cholesterol levels put a client at risk for primary hypertension. Kidney disease is a cause of secondary hypertension. The nurse provides client education regarding hypertension prevention and management. Which of these statements indicates that the client understands the instructions? 1) I dont have to worry if my blood pressure is high once in a while. 2) I guess I will have to make sure I dont drink too much water. 3) I can lose some weight to help lower my blood pressure. 4) I will need to reduce the amount milk and other dairy products I use. ANS: 3 A single lifestyle change, such as weight loss, can lower blood pressure (BP). Whenever the client has an elevated BP, the reading should be monitored even when it occurs just occasionally. Drinking too much alcohol is associated with hypertension, but water consumption is not unless accompanied by high sodium intake. A diet high in calcium is recommended to prevent and manage hypertension; therefore, it is not advisable to limit the intake of dietary calcium found in dairy products. For which of the following patients would it be most important to obtain an apical-radial pulse and calculate the pulse deficit? A patient who 1) Had abdominal surgery 2 hours ago 2) Suffered a fractured hip yesterday 3) Is dehydrated from vomiting 4) Has a heart or lung disease ANS: 4 Conditions that require assessment of pulse deficit include digitalis therapy and blood loss, cardiac or respiratory disease, and other conditions that affect oxygenation status. Which of the following procedure techniques has the most effect on the accuracy of an apical pulse count? 1) Counting the rate for 1 full minute 2) Exposing only the left side of the chest 3) Determining why assessment of apical pulse is indicated 4) Using your ring finger to palpate the intercostal spaces ANS: 1 Apical pulse is generally indicated for patients with cardiac conditions or who are taking cardiac medications. Often they have irregular heartbeats or slow rates. A more accurate count is obtained when such heartbeats are counted for a full minute. Exposing the chest is, of course, necessary; exposing only the left side protects the patients privacy but does not improve the accuracy. The nurse should know why an apical pulse is indicated, but this would not affect the accuracy of the count. Which finger the nurse uses to palpate depends on which hand is used. Even if the nurse failed to use the index or ring finger, this would be unlikely to affect the accuracy of the counting. Which assessment data best support a report of severe pain in an adult client whose baseline vital signs are within an average normal range? 1) Oral temperature 100F (37.8C) 2) Respiratory rate 26 breaths/min and shallow 3) Apical heart rate 56 beats/min 4) Blood pressure 124/82 mm Hg ANS: 2 Respiratory rate 26 breaths/min and shallow. Acute pain causes an increase in respiratory rate but a decrease in depth. Elevated temperature does not indicate pain. The apical pulse is lower than normal, but because the pulse increases with pain, a rate of 56 beats/min does not indicate pain. A blood pressure of 124/82 mm Hg is within normal limits. Blood pressure usually elevates temporarily with acute pain; it may decrease over time with unremitting chronic pain. During a clinic interview, a client states he has been experiencing dizziness upon standing. Which nursing action is appropriate for the nurse to implement? 1) Ask the client when in the day dizziness occurs. 2) Help the client to assume a recumbent position. 3) Measure both heart rate and blood pressure with the client standing. 4) Measure vital signs with the client supine, sitting, and standing. ANS: 4 Dizziness upon standing is a symptom of orthostatic hypotension. The nurse should obtain orthostatic vital signs (measure pulse and blood pressure with the patient supine, sitting, and standing) to assess for orthostatic hypotension. The time of day is irrelevant to the diagnosis. If the nurse observes the patient become dizzy upon standing, the first action would be to help the client lie down and then obtain orthostatic vital signs; but this is not necessary when the symptom is not present. The nurse needs to measure both the heart rate and the blood pressure but not only in the standing position. Which blood pressure has a pulse pressure within normal limits? Choose all that apply. 1) 104/50 mm Hg 2) 120/62 mm Hg 3) 120/80 mm Hg 4) 130/86 mm Hg ANS: 3, 4 The pulse pressure is the systolic blood pressure (BP) minus the diastolic BP. The pulse pressure is usually approximately one third of the systolic pressure. (120 80 = 40; 40 = 1/3 of 120) (130 86 = 44; 1/3 of 130 = 43.3) Which of the following interventions would be appropriate for a client who has a fever? Choose all that apply. 1) Put an ice pack on the clients neck and axillae. 2) Provide the client a blanket when he is shivering. 3) Offer the client fluids to drink every 1 to 2 hours. 4) Take the temperature using a tympanic thermometer. ANS: 1, 3 If ice packs are used, they are applied to the groin, neck, or axillae. A fever increases metabolic needs, so fluids are necessary to prevent dehydration. A blanket would help with heat retention. A tympanic thermometer is not appropriate when an accurate temperature is needed, as when a client has a fever. Comparing the changes in vital signs as a person ages, which statement is correct? Select all that apply. 1) Blood pressure decreases less than heart rate and respiratory rate. 2) Respiratory rate remains fairly stable throughout a persons life. 3) Blood pressure increases; heart rate and respiratory rate decline. 4) Men have higher blood pressure than women until after menopause. ANS: 3, 4 Heart rate and respiratory rate tend to decrease as people age, whereas the blood pressure increases because of increased vascular resistance. Mens blood pressure tends to be higher than womens until after menopause, when womens blood pressure typically increases. Which of these steps in taking a blood pressure is correct? Choose all that apply. 1) Use a bladder that encircles 40% of the arm. 2) Wrap the cuff snugly around the clients arm. 3) Ask the client to hold the arm at heart level. 4) Have the client sit with feet flat on the floor. ANS: 2, 4 The cuff should be wrapped snugly around the clients arm. Crossed legs or dangling legs can increase blood pressure, so feet should be flat on the floor. The bladder should encircle 80% of the arm. Holding the arm out can cause an erroneously higher blood pressure measurement; the arm should be supported. When assessing the quality of a clients pedal pulses, what is the nurse assessing? Choose all that apply. 1) Rhythm of the pulses 2) Strength of the pulses 3) Bilateral equality of pulses 4) Rate compared with apical pulse ANS: 2, 3 The quality of a pulse refers to the pulse volume (strength) and bilateral equality of the pulses. All of the following clinical signs may be present with hypoxia. However, only two are specific indicators of hypoxia (that is, if they are present, it means that the patient is probably hypoxic). Which ones are specific indicators of hypoxia? Choose all that apply. 1) Feelings of anxiety 2) Crackles in the lung bases 3) Increased heart rate 4) Improved breathing in upright position ANS: 1, 3 Apprehension, confusion, dizziness, and an increased heart rate are all specific manifestations of hypoxia. Although they are not listed in this question, cyanosis of the tongue and oral mucosa are also good indicators of hypoxia because those areas are not affected by cold or reduced circulation as are the nails, lips, and skin. Crackles and orthopnea are abnormal respiratory findings, but they do not necessarily indicate poor oxygenation. Which of the following behaviors indicates the highest potential for spreading infections among clients? The nurse: 1) disinfects dirty hands with antibacterial soap. 2) allows alcohol-based rub to dry for 10 seconds. 3) washes hands only when leaving each room. 4) uses cold water for medical asepsis. ANS: 3 Patients acquire infection by contact with other patients, family members, and healthcare equipment. But most infection among patients is spread through the hands of healthcare workers. Hand washing interrupts the transmission and should be done before and after all contact with patients, regardless of the diagnosis. When the hands are soiled, healthcare staff should use antibacterial soap with warm water to remove dirt and debris from the skin surface. When no visible dirt is present, an alcohol-based rub should be applied and allowed to dry for 10 to 15 seconds. What is the most frequent cause of the spread of infection among institutionalized patients? 1) Airborne microbes from other patients 2) Contact with contaminated equipment 3) Hands of healthcare workers 4) Exposure from family members ANS: 3 Patients are exposed to microbes by contact (direct contact, airborne, or otherwise) with other patients, family members, and contaminated healthcare equipment. Some of these are pathogenic (cause illness) and some are nonpathogenic (do not cause illness). But most microbes causing infection among patients are spread by direct contact on the hands of healthcare workers. Which of the following nursing activities is of highest priority for maintaining medical asepsis? 1) Washing hands 2) Donning gloves 3) Applying sterile drapes 4) Wearing a gown ANS: 1 Scrupulous hand washing is the most important part of medical asepsis. Donning gloves, applying sterile drapes before procedures, and wearing a protective gown may be needed to ensure asepsis, but they are not the most important aspect because microbes causing most healthcare-related infections are transmitted by lack of or ineffective hand washing. A patient infected with a virus but who does not have any outward sign of the disease is considered a: 1) pathogen. 2) fomite. 3) vector. 4) carrier. ANS: 4 Some people might harbor a pathogenic organism, such as the human immunodeficiency virus, within their bodies and yet do not acquire the disease/infection. These individuals, called carriers, have no outward sign of active disease, yet they can pass the infection to others. A pathogen is an organism capable of causing disease. A fomite is a contaminated object that transfers a pathogen, such as pens, stethoscopes, and contaminated needles. A vector is an organism that carries a pathogen to a susceptible host through a portal for entry into the body. An example of a vector is a mosquito or tick that bites or stings. A patient is admitted to the hospital with tuberculosis. Which precautions must the nurse institute when caring for this patient? 1) Droplet transmission 2) Airborne transmission 3) Direct contact 4) Indirect contact ANS: 2 The organisms responsible for measles and tuberculosis, as well as many fungal infections, are spread through airborne transmission. Neisseria meningitidis, the organism that causes meningitis, is spread through droplet transmission. Pathogens that cause diarrhea, such as Clostridium difficile, are spread by direct contact. The common cold can be spread by indirect contact or droplet transmission. A patient becomes infected with oral candidiasis (thrush) while receiving intravenous antibiotics to treat a systemic infection. Which type of infection has the patient developed? 1) Endogenous nosocomial 2) Exogenous nosocomial 3) Latent 4) Primary ANS: 1 Thrush in this patient is an example of an endogenous nosocomial infection. This type of infection arises from suppression of the patients normal floras as a result of some form of treatment, such as antibiotics. Normal floras usually keep yeast from growing in the mouth. In exogenous nosocomial infection, the pathogen arises from the healthcare environment. A latent infection causes no symptoms for long periods. An example of a latent infection is human immunodeficiency virus infection. A primary infection is the first infection that occurs in a patient. A patient admitted to the hospital with pneumonia has been receiving antibiotics for 2 days. His condition has stabilized, and his temperature has returned to normal. Which stage of infection is the patient most likely experiencing? 1) Incubation 2) Prodromal 3) Decline 4) Convalescence ANS: 3 The stage of decline occurs when the patients immune defenses, along with any medical therapies (in this case antibiotics), are successfully reducing the number of pathogenic microbes. As a result, the signs and symptoms of infection begin to fade. Incubation is the stage between the invasion by the organism and the onset of symptoms. During the incubation stage, the patient does not know he is infected and is capable of infecting others. The prodromal stage is characterized by the first appearance of vague symptoms. Convalescence is characterized by tissue repair and a return to healing as the organisms disappear. The nurse assists a surgeon with central venous catheter insertion. Which action is necessary to help maintain sterile technique? 1) Closing the patients door to limit room traffic while preparing the sterile field 2) Using clean procedure gloves to handle sterile equipment 3) Placing the nonsterile syringes containing flush solution on the sterile field 4) Remaining 6 inches away from the sterile field during the procedure ANS: 1 To maintain sterile technique, the nurse should close the patients door and limit the number of persons entering and exiting the room because air currents can carry dust and microorganisms. Sterile gloves, not clean gloves, should be used to handle sterile equipment. Placing nonsterile syringes on the sterile field contaminates the field. One foot, not 6 inches, is required between people and the sterile field to prevent contamination. A patient develops localized heat and erythema over an area on the lower leg. These findings are indicative of which secondary defense against infection? 1) Phagocytosis 2) Complement cascade 3) Inflammation 4) Immunity ANS: 3 The classic signs of inflammation, a secondary defense against infection, are erythema (redness) and localized heat. The secondary defenses phagocytosis (process by which white blood cells engulf and destroy pathogens) and the complement cascade (process by which blood proteins trigger the release of chemicals that attack the cell membranes of pathogens) do not produce visible findings. Immunity is a tertiary defense that protects the body from future infection. The patient is just beginning to feel symptoms after being exposed to an upper respiratory infection. Which antibody would most likely be found in a test of immunoglobin levels? 1) IgA 2) IgE 3) IgG 4) IgM ANS: 4 IgM are the first antibodies made in response to infection. IgE is the antibody primarily responsible for this allergic response. IgA antibodies protect the body in fighting viral and bacterial infections, and appear later. IgG antibodies also appear laterperhaps up to 10 days later. What type of immunity is provided by intravenous (IV) administration of immunoglobulin G? 1) Cell-mediated 2) Passive 3) Humoral 4) Active ANS: 2 Intravenous administration of immunoglobulin G provides the patient with passive immunity. Immunoglobulin G does not provide cell-mediated, humoral, or active immunity. Passive immunity occurs when antibodies are transferred from an immune host, such as from a placenta to a fetus. Passive immunity is short lived. Active immunity is longer lived and comes from the host. Humoral immunity occurs by secreted antibodies binding to antigens. Cell-mediated immunity does not involve antibodies but rather is a fight of infection from macrophages that kill pathogens. A patient asks the nurse why there is no vaccine available for the common cold. Which response by the nurse is correct? 1) The virus mutates too rapidly to develop a vaccine. 2) Vaccines are developed only for very serious illnesses. 3) Researchers are focusing efforts on an HIV vaccine. 4) The virus for the common cold has not been identified. ANS: 1 More than 200 viruses are known to cause the common cold. These viruses mutate too rapidly to develop a vaccine. Although some researchers are focusing efforts on a vaccine for HIV infection, others continue to research the common cold. A patient who has a temperature of 101F (38.3C) most likely requires: 1) acetaminophen (Tylenol). 2) increased fluids. 3) bedrest. 4) tepid bath. ANS: 2 Fever, a common defense against infection, increases water loss; therefore, additional fluid is needed to supplement this loss. Acetaminophen and a tepid bath are not necessary for this low-grade fever because fever is beneficial in fighting infection. Adequate rest, not necessarily bedrest, is necessary with a fever. Why is a lotion without petroleum preferred over a petroleum-based product as a skin protectant? 1) It prevents microorganisms from adhering to the skin. 2) It facilitates the absorption of latex proteins through the skin. 3) It decreases the risk of latex allergies. 4) It prevents the skin from drying and chaffing. ANS: 3 Non-petroleum-based lotion is preferred because it prevents the absorption of latex proteins through the skin, which can cause latex allergy. Both types of lotion help prevent the skin from drying and becoming chafed. Neither prevents microorganisms from adhering to the skin. For which range of time must a nurse wash her hands before working in the operating room? 1) 1 to 2 minutes 2) 2 to 4 minutes 3) 2 to 6 minutes 4) 6 to 10 minutes ANS: 3 In a surgical setting, hands should be washed for 2 to 6 minutes, depending on the type of soap used. How should the nurse dispose of the breakfast tray of a patient who requires airborne isolation? 1) Place the tray in a specially marked trash can inside the patients room. 2) Place the tray in a special isolation bag held by a second healthcare worker at the patients door. 3) Return the tray with a note to dietary services so it can be cleaned and reused for the next meal. 4) Carry the tray to an isolation trash receptacle located in the dirty utility room and dispose of it there. ANS: 2 Patients who require airborne isolation are served meals on disposable dishes and trays. To dispose of the tray, the nurse inside the room must wear protective garb and place the tray and its contents inside a special isolation bag that is held by a second healthcare worker at the patients door. The items must be placed on the inside of the bag without touching the outside of the bag. As a general rule, how much liquid soap should the nurse use for effective hand washing? At least: 1) 2 mL 2) 3 mL 3) 6 mL 4) 7 mL ANS: 2 APIC guidelines dictate that 3 to 5 mL of liquid soap is necessary for effective hand washing. To assure effectiveness, when should the nurse stop rubbing antiseptic hand solution over all surfaces of the hands? 1) When fingers feel sticky 2) After 5 to 10 seconds 3) When leaving the clients room 4) Once fingers and hands feel dry ANS: 4 The nurse should rub the antiseptic hand solution over all surfaces of the hands until the solution dries, usually 10 to 15 seconds, to ensure effectiveness. A patient is admitted to the hospital for chemotherapy and has a low white blood cell count. Which precaution should the staff take with this patient? 1) Contact 2) Protective 3) Droplet 4) Airborne ANS: 2 Protective isolation is used to protect those patients who are unusually vulnerable to organisms brought in by healthcare workers. Such patients include those with low white blood cell counts, with burns, and undergoing chemotherapy. Some hospital units, such as neonatal intensive care units and labor and delivery suites, also use forms of protective isolation. While donning sterile gloves, the nurse notices the edges of the glove package are slightly yellow. The yellow area is over 1 inch away from the gloves and only appears to be on the outside of the glove package. What is the best action for the nurse to take at this point? 1) Continue using the gloves inside the package because the package is intact. 2) Remove gloves from the sterile field and use a new pair of sterile gloves. 3) Throw all supplies away that were to be used and begin again. 4) Use the gloves and make sure the yellow edges of the package do not touch the client. ANS: 2 The gloves should be discarded because the gloves are likely to be contaminated from an outside source. The supplies do not have to be thrown away because they have not been contaminated. The nurse is removing personal protective equipment (PPE). Which item should be removed first? 1) Gown 2) Gloves 3) Face shield 4) Hair covering ANS: 2 The gloves are removed first because they are usually the most contaminated PPE and must be removed to avoid contamination of clean areas of the other PPE during their removal. The gown is removed second, then the mask or face shield, and finally, the hair covering. A nurse is splashed in the face by body fluid during a procedure. Prioritize the nurses actions, listing the most important one first. 1. Contact employee health 2. Complete an incident report 3. Wash the exposed area 4. Report to another nurse that she is leaving the immediate area. 1) 1, 2, 3, 4 2) 2, 3, 4, 1 3) 3, 4, 1, 2 4) 4, 1, 2, 3 ANS: 3 If a nurse becomes exposed to body fluid, she should first wash the area, tell another nurse she is leaving the area, contact the infection control or employee health nurse immediately, and complete an incident report. It is most important to remove the source of contamination (body fluid) as soon as possible after exposure to help prevent the nurse from becoming infected. The other activities can wait until that is done. In which situation would using standard precautions be adequate? Select all that apply. 1) While interviewing a client with a productive cough 2) While helping a client to perform his own hygiene care 3) While aiding a client to ambulate after surgery 4) While inserting a peripheral intravenous catheter ANS: 3, 4 Standard precautions should be instituted with all clients whenever there is a possibility of coming in contact with blood, body fluids (except sweat), excretions, secretions, mucous membranes, and breaks in the skin (e.g., while inserting a peripheral IV). When interviewing a client, if the disease is not spread by air or droplets, there is no likelihood of the nurses encountering body fluids. If the disease is spread by air or droplets, then droplet or airborne precautions would be needed in addition to standard precautions. If giving a complete bed bath or performing oral hygiene, the nurse would need to use standard precautions (gloves); if merely assisting a client to perform those ADLs, it is not necessary. No exposure to body fluids is likely when helping a client to ambulate after surgery Which of the following protect(s) the body against infection? Select all that apply. 1) Eating a healthy, well-balanced diet 2) Being an older adult or an infant 3) Leisure activities three times a week 4) Exercising for 30 minutes 5 days a week ANS: 1, 3, 4 Nutrition, hygiene, rest, exercise, stress reduction, and immunization protect the body against infection. Illness, injury, medical treatment, infancy or old age, frequent public contact, and various lifestyle factors can make the body more susceptible to infection. The nurse is teaching a group of newly hired nursing assistive personnel (NAP) about proper hand washing. The nurse will know that the teaching was effective if the NAP demonstrate what? Select all that apply. The NAP: 1) uses a paper towel to turn off the faucet. 2) holds fingertips above the wrists while rinsing off the soap. 3) removes all rings and watch before washing hands. 4) cleans underneath each fingernail. ANS: 1, 3, 4 Hand washing requires at least 15 seconds of washing, which includes lathering all surfaces of the hands and fingers to be effective. The fingers should be held lower than the wrists. Alcohol-based solutions for hand hygiene can be used to combat which types of organisms? Select all that apply. 1) Virus 2) Bacterial spores 3) Yeast 4) Mold ANS: 1, 3, 4 If there is potential for contact with bacterial spores, hands must be washed with soap and water; alcohol-based solutions are ineffective against bacterial spores. A patient with tuberculosis is scheduled for computed tomography (CT). How should the nurse proceed? Select all that apply. 1) Question the order because the patient must remain in isolation. 2) Place an N-95 respirator mask on the patient and transport him to the test. 3) Place a surgical mask on the patient and transport him to CT lab. 4) Notify the computed tomography department about precautions prior to transport. ANS: 3, 4 Transporting a patient who requires airborne precautions should be limited; however, when necessary the patient should wear a surgical mask (an N-95 respirator mask is not required) that covers the mouth and nose to prevent the spread of infection. Moreover, the department where the patient is being transported should be notified about the precautions before transport. The patient takes anticoagulants. Which instruction is most important for the nurse to include on the patients care plan? Teach the patient to: 1) use an electric razor for shaving. 2) apply skin moisturizer. 3) use less soap when bathing. 4) floss teeth daily. ANS: 1 The nurse should instruct the patient prescribed an anticoagulant to use an electric razor instead of a double-edge razor for shaving to prevent the risk of excess bleeding. Older adults should be encouraged to use skin moisturizers and use less soap while bathing to combat excess drying of the skin that occurs as a result of aging. However, even if this patient is an older adult, a risk for bleeding takes priority over a risk for dry skin. Everyone should be encouraged to floss their teeth daily; however, some patients with severe bleeding risk may be told not to floss. The nurse is caring for a patient admitted with a closed head injury. Which action by the nurse is appropriate when providing hygiene for this patient? 1) Avoid bathing the patient. 2) Use cool water for bathing. 3) Provide care in small intervals. 4) Rub briskly when towel drying. ANS: 3 The nurse should provide care in small intervals to avoid overstimulating the patient, thereby causing a rise in his intracranial pressure. It is not necessary to avoid bathing the patient. Using cool water to bathe the patient may cause shivering, which may elevate intracranial pressure and increase metabolic demands. Rubbing briskly when drying might also overstimulate, leading to an elevation in intracranial pressure. A patient has sustained a spinal cord injury and is no longer able to get in and out of the bathtub without assistance. Which nursing diagnosis appropriately addresses this problem? 1) Total Self-care Deficit 2) Bathing/Hygiene Self-care Deficit 3) Dressing/Grooming Self-care deficit 4) Activity Intolerance ANS: 2 The nursing diagnosis Bathing/Hygiene Self-care Deficit is most appropriate for addressing the patients inability to get in and out of the bathtub independently. There are no data to suggest that the patient is completely unable to care for himself; therefore, Total Self-care Deficit is not appropriate. There is nothing to suggest that the patient is unable to dress or groom himself. Activity Intolerance is present when a patient exhibits extreme fatigue, which is not mentioned in this scenario. Which scheduled hygiene care is usually thought of as including a back massage to help the patient relax? 1) Afternoon care 2) Early morning care 3) Morning care 4) Hour of sleep care ANS: 4 The nurse should offer a back massage during hour of sleep (HS) care to promote relaxation. During afternoon care the nurse should prepare the patient to receive visitors or for afternoon rest. Early morning care is provided after the patient awakens. It commonly prepares the patient for breakfast or procedures, such as diagnostic testing. Early morning care typically consists of assisting with toileting, face and hand washing, and mouth care. Morning care occurs after breakfast and commonly consists of toileting, bathing, and mouth, skin, and hair care. It may also include dressing and positioning or assisting the patient to the chair. For which patient can the nurse safely delegate morning care to the nursing assistive personnel (NAP)? Assume an experienced NAP, and base your decision on patient condition. Assume there are no complications other than the conditions stated. 1) 32-year-old admitted with a closed head injury 2) 76-year-old admitted with septic shock 3) 62-year-old who underwent surgical repair of a bowel obstruction 2 days ago 4) 23-year-old admitted with an exacerbation of asthma with dyspnea on exertion ANS: 3 Morning care for the patient who underwent surgical repair of a bowel 2 days ago can be safely delegated to the nursing assistive personnel because the patient should be stable. The patient who sustained a closed head injury may develop increased intracranial pressure during care. Therefore, he requires the critical thinking skills of a registered nurse to perform his morning care safely. The patient admitted with septic shock may easily become unstable with care; therefore, a registered nurse is required to provide his morning care safely. The patient admitted with an exacerbation of asthma who becomes short of breath with activity also requires the critical thinking skills of a registered nurse to detect respiratory compromise quickly. A clients epidermis has insufficient melanin. Which nursing diagnosis is appropriate? 1) Risk for Infection 2) Risk for Impaired Skin Integrity 3) Risk for Deficient Fluid Volume 4) Impaired Skin Integrity ANS: 2 The epidermis contains melanin, a pigment that protects against the suns ultraviolet rays; therefore, a person with insufficient melanin is at Risk For Impaired Skin Integrity (sunburn). There are no symptoms to indicate that the client has a sunburn (actual Impaired Skin Integrity), only that a risk factor is present. The dermis contains blood and lymphatic vessels, nerves, bases of hair follicles, and sebaceous and sweat glands; melanin does not prevent fluid loss. Fibroblasts (not melanin), also found in the dermis, produce new cells and assist in wound healing, thereby helping to prevent infection. What is the body's first line of defense against bacteria? 1) Intact skin 2) White blood cells 3) Lymph glands 4) Inflammatory response ANS: 1 Intact skin is the bodys first line of defense against bacteria. Once bacteria enter the body, the inflammatory response, white blood cells, and lymph glands play a role in fighting against the bacteria. While bathing a patient with liver dysfunction, the nurse notes yellow skin tone. The nurse should document this finding as: 1) Pallor. 2) Erythema. 3) Jaundice. 4) Cyanosis. ANS: 3 A yellow skin tone, known as jaundice, commonly occurs in patients with impaired liver function. Pallor is pale skin without underlying pink tones in the light-skinned person. Pallor occurs with anemia. Erythema, or redness of the skin, commonly occurs with inflammation or vasodilation. Cyanosis, a bluish coloring of the skin, is caused by poor peripheral circulation or decreased oxygen in the blood. A patient with diarrhea is incontinent of liquid stool. The nurse documents that he now has excoriated skin on his buttocks. Which finding by the nurse led to this documentation? 1) Skin was softened from prolonged exposure to moisture. 2) Superficial layers of skin were absent. 3) The epidermal layer of skin was rubbed away. 4) A lesion caused by tissue compression was present. ANS: 2 Excoriation is a loss of the superficial layers of the skin caused by the digestive enzymes in feces. Maceration is the softening of skin from exposure to moisture. Abrasion, a rubbing away of the epidermal layer of the skin, especially over bony areas, is often caused by friction or searing forces that occur when a patient moves in bed. Pressure ulcers are lesions caused by tissue compression and inadequate perfusion that are a result of immobility. For which patient is it most important to provide frequent perineal care? The patient: 1) with active lower gastrointestinal bleeding. 2) after an episode of diabetic ketoacidosis. 3) who has a circumcised penis. 4) with a history of acute asthma. ANS: 1 The patient admitted with active lower GI bleeding will require frequent perineal care because of the irritating effect of enzymes in the stools. The uncircumcised patient, not the circumcised patient, may require frequent perineal care. Those with diabetic ketoacidosis or who have had acute asthma do not require frequent perineal care. A patient with dementia becomes belligerent when the nurse attempts to give him a tub bath. How should the nurse proceed? 1) Call for assistance to help the patient into the bathtub. 2) Wait for the patient to calm down, and then give him a towel bath. 3) Allow the patient to go without bathing for a day or two. 4) Ask another staff member to attempt the tub bath. ANS: 2 Nurses need to individualize bathing to meet the needs of the patient. If the patient becomes belligerent, the nurse should wait until the patient calms down and then attempt a towel bath. Towel baths have been shown to reduce agitation significantly. The patient should not be forced into the tub. Having another staff member attempt the tub bath will most likely increase the patients agitation, as consistency of caregivers is important for patients with dementia. The nurse is teaching nursing assistive personnel (NAP) how to give a complete bed bath. Which instruction should the nurse include? 1) Cleanse only those areas likely to cause odor. 2) Provide the patient with warm water for washing his perineum. 3) Wash the patients back, buttocks, and perineum first. 4) Bathe the patient from head-to-toe, cleanest areas first. ANS: 4 The nurse should instruct the NAP to give a complete bed bath (a bath for patients who must remain in bed but who are able to bathe themselves), in head-to-toe fashion, beginning with the cleanest part of the body and ending with the dirtiest. The NAP should provide the patient with a basin of warm water and allow him to wash his perineum when giving an assist bath or bed bath (this is a total bed bath). During a partial bath, the NAP should cleanse only the areas that may cause odor or discomfort. The NAP should never begin the bath with the back, buttocks, and perineum because this violates the principle of clean to dirty. Which action should the nurse take when preparing a patient for a bed bath? 1) Place the nurse call device within reach for safety. 2) Cover the patient with the top linens from the bed. 3) Have the patient completely bathe himself to promote independence. 4) Wash the patients body without assistance from the patient. ANS: 1 When preparing a patient for a bed bath (a bath for patients who must remain in bed but who are able to bathe themselves), place a basin of warm water, bath linens, a clean gown, and other bathing supplies on the overbed table. Provide privacy, and place the nurse call device within reach. Remove the top linens from the bed, and cover the patient with a bath blanket. If the patient cannot bathe all areas of his body, complete the bath for him. The nurse performs at least part of a bed bath; if the patient bathes himself completely while remaining in bed, it is referred to as an assist bath. A patient admitted with an acute exacerbation of chronic obstructive pulmonary disease has a nursing diagnosis of Activity Intolerance. Which type of bath is preferred for this patient? 1) Tub bath 2) Complete bed bath 3) Towel bath 4) Bed bath ANS: 3 A towel bath is a modification of the bed bath, in which a large towel and a bath blanket are placed in a plastic bag and saturated with a commercially prepared mixture of moisturizer, nonrinse cleaning agent, and water. The bag and its contents are then placed in the microwave, and they are used to bathe the patient. This bathing method is preferred for patients who have Activity Intolerance. A tub bath, complete bed bath, and conventional bed bath may deplete this patients energy. Wearing poorly fitting shoes may result in which condition? 1) Tinea pedis 2) Plantar wart 3) Excoriation 4) Ingrown toenail ANS: 4 Wearing poorly fitting shoes and improperly trimming the toenails may cause an ingrown toenail. Tinea pedis occurs when moisture accumulates in unventilated shoes. Plantar wart is a painful growth that is caused by a virus. Excoriation occurs when digestive enzymes come in contact with skin. The school nurse is teaching a group of middle school students how to prevent tinea pedis. Which remark by a student provides evidence of learning? 1) I can contract the infection by walking barefoot in the gymnasiums showers. 2) The best way to avoid contracting the infection is to use good hand washing. 3) Wearing unventilated shoes prevents the fungus from gaining contact with my feet. 4) There is really no way to prevent its spread; its highly contagious. ANS: 1 One can contract the infection by walking barefoot in public showers, such as those in the schools gymnasium. Good hand washing does not prevent a person from contracting tinea pedis. Wearing unventilated shoes may actually aggravate the infection by allowing moisture to accumulate in the shoes. Although the infection is highly contagious, the spread of infection can be prevented by wearing special footwear in the shower. Bath water should be prepared at which temperature to prevent chilling and excess drying of the skin? 1) 99F (37.2C) 2) 102F (38.9C) 3) 103F (39.4C) 4) 105F (40.6C) ANS: 4 Bath water temperature should be 105F (40.6C) to prevent chilling, burning, and excess drying of the skin. While assessing a patient, the nurse notes that the patients nails are excessively brittle. What does this finding suggest? 1) Inadequate dietary intake 2) Normal aging process 3) Fungal infection 4) Excessive use of silver salts ANS: 1 Inadequate dietary intake or metabolic changes can cause the nails to become brittle. As a person ages, nails thicken, become ridged, and may yellow or become concave in shape. Brown or black discoloration of the nail plate may indicate a fungal infection. Bluish gray discoloration of the nail plate signals excessive intake of silver salts. A patient with a history of seizures who takes phenytoin is at risk for which oral problem? 1) Dryness of the mouth 2) Bitter taste 3) Demineralization of the tooth enamel 4) Gingival hyperplasia ANS: 4 Phenytoin causes gingival hyperplasia. Medications, such as atropine, cause dry mouth. Bitter taste can result from drugs, such as docusate sodium, a stool softener. Phenytoin does not cause demineralization of the tooth enamel. The nurse has been teaching a student how to perform mouth care for her unconscious patient. The student will show evidence of learning if she places the patient in which position for this care? 1) Supine 2) Prone 3) Semi-Fowlers 4) Side-lying ANS: 4 The nurse should position an unconscious patient in a side-lying position to provide mouth care to prevent aspiration. Supine, prone, and semi-Fowlers positions are unsafe positions for providing mouth care for the unconscious patient. Which item is best for providing mouth care for an unconscious patient? 1) Foam swabs 2) Lemon-glycerin swabs 3) Hydrogen peroxide 4) Cotton-tipped applicator soaked in mouthwash ANS: 1 Commercially packaged applicators or foam swabs are typically used to provide mouth care. Lemon-glycerin swabs are not recommended because they are drying to the oral mucosa. Hydrogen peroxide should be avoided because it is irritating to oral mucosa and may alter the balance of normal floras that occur in the mouth. Mouthwash can be used by conscious patients as part of their routine mouth care. However, cotton-tipped applicators should not be soaked in it to perform mouth care. After receiving a course of chemotherapy, a patient begins losing hair. This adverse effect of chemotherapy should be documented as: 1) pediculosis. 2) alopecia. 3) dandruff. 4) hirsutism. ANS: 2 Alopecia is abnormal hair loss that can occur as a result of chemotherapy. Pediculosis is an infestation of head lice. Dandruff is a condition in which there is excessive shedding of the epidermal layer of the scalp. Hirsutism is the excessive growth of body hair in women. Which of the following is a correct step in removing and cleaning a hearing aid? 1) Clean only the external surfaces, not the canal portion. 2) Clean the top part of the canal portion of the device. 3) Insert a wax loop or toothpick into the hearing aid. 4) Remove the battery before taking the hearing aid from the ear. ANS: 2 The nurse should clean the top part of the canal portion of the hearing aid using the wax loop and wax brush, cotton-tipped applicator, pipe cleaner, or toothpick. Nothing should be inserted into the hearing aid. The external surfaces are cleaned with a damp cloth. The hearing aid should be turned off before removing it from the ear, but the battery is not removed at that step of the procedure. It would not likely be possible to remove the battery while the device was still in the ear. The patient is sitting in a chair at the bedside. The nurse is preparing to remove the patients artificial eye. What should the nurse do to best position the patient for this procedure? Ask the patient to: 1) Lean forward and rest the arms on the overbed table. 2) Sit back in the chair and tilt the head back. 3) Move to the bed and lie down. 4) Stand up and lean over the bed. ANS: 3 The nurse should have the patient lie down so that if the eye is dropped when removing it, it will fall onto the bed instead of the floor. Sitting back in the chair would allow access to the eye but would not protect the artificial eye from falling to the floor. Leaning forward and resting the arms on an overbed table, as well as standing up and leaning over the bed, would not provide the nurse access to the eye to remove the prosthesis. Which of the following is/are a benefit of bathing? Choose all that apply. 1) Constricts blood vessels 2) Increases depth of respirations 3) Gives opportunity for assessments 4) Reduces sensory input ANS: 2, 3 Bathing presents an opportunity to perform a variety of assessments. Bathing also dilates blood vessels near the skins surface, increasing circulation. Moreover, bathing stimulates the depth of respirations and provides sensory input. For which patient(s) should the nurse avoid using back massage? One who (select all that apply): 1) underwent heart surgery 3 days ago. 2) sustained rib fractures from a fall. 3) underwent a lumbar laminectomy. 4) sustained a leg fracture in a sledding accident. ANS: 1, 2 Back massage is contraindicated with rib fractures, burns, and recent heart surgery. Massage is acceptable for the patients with lumbar laminectomy or leg fracture. The nurse is making an occupied bed. Arrange the following steps in the order in which the nurse should perform them. A. Position the patient laterally near the side rail farthest from you (that side rail is up); roll the soiled linens under him. B. Lower the side rail on the side of the bed you are working on. C. Raise the side rail on the side of the bed you are working on. D. After placing clean linens and tucking them under the soiled linens, roll the patient over the hump and position him facing you on the near side of the bed. ANS: B, A, D, C First lower the side rail on your side of the bed. This allows you to maintain good body mechanics while positioning the patient. Position the patient laterally near the far side rail, and roll soiled linens under him. Then place clean linens on the side nearest you, and tuck them under soiled linens. Next, roll the patient over the hump, and position him on his other side, facing you. Do this before raising the near side rail so you do not have to reach across the side rail to help the patient roll and turn to his other side. [Show More]
Last updated: 2 years ago
Preview 1 out of 41 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$18.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
May 14, 2021
Number of pages
41
Written in
Additional information
This document has been written for:
Uploaded
May 14, 2021
Downloads
0
Views
102

.png)