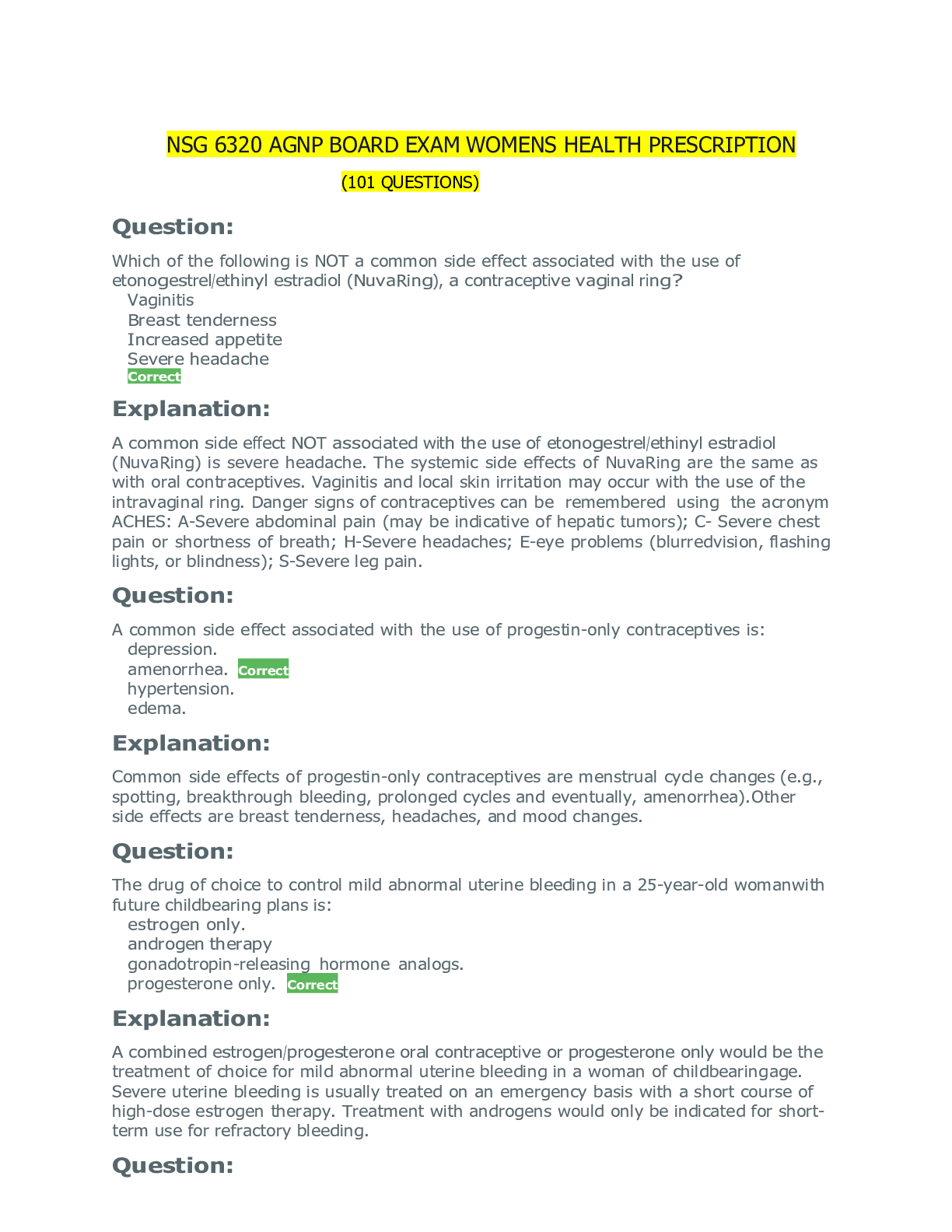
*NURSING > EXAM > AGNP BOARD EXAM QUESTIONS Womens Health Prescription (101 Questions) verified 100% A+ solution (All)
AGNP BOARD EXAM QUESTIONS Womens Health Prescription (101 Questions) verified 100% A+ solution
Document Content and Description Below
AGNP BOARD EXAM QUESTIONS Womens Health Prescription (101 Questions) Question: Which of the following is NOT a common side effect associated with the use of etonogestrel/ethinyl estradiol (NuvaR... ing), a contraceptive vaginal ring? Vaginitis Breast tenderness Increased appetite Severe headache Correct Explanation: A common side effect NOT associated with the use of etonogestrel/ethinyl estradiol (NuvaRing) is severe headache. The systemic side effects of NuvaRing are the same as with oral contraceptives. Vaginitis and local skin irritation may occur with the use of the intravaginal ring. Danger signs of contraceptives can be remembered using the acronym ACHES: A-Severe abdominal pain (may be indicative of hepatic tumors); C- Severe chest pain or shortness of breath; H-Severe headaches; E-eye problems (blurred vision, flashing lights, or blindness); S-Severe leg pain. Question: A common side effect associated with the use of progestin-only contraceptives is: depression. amenorrhea. Correct hypertension. edema. Explanation: Common side effects of progestin-only contraceptives are menstrual cycle changes (e.g., spotting, breakthrough bleeding, prolonged cycles and eventually, amenorrhea). Other side effects are breast tenderness, headaches, and mood changes. Question: The drug of choice to control mild abnormal uterine bleeding in a 25-year-old woman with future childbearing plans is: estrogen only. androgen therapy gonadotropin-releasing hormone analogs. progesterone only. Correct Explanation: A combined estrogen/progesterone oral contraceptive or progesterone only would be the treatment of choice for mild abnormal uterine bleeding in a woman of childbearing age. Severe uterine bleeding is usually treated on an emergency basis with a short course of high-dose estrogen therapy. Treatment with androgens would only be indicated for short-term use for refractory bleeding. Question: Nonhormonal treatments for menopausal symptoms include: benzodiazepines. copper intrauterine device. selective serotonin reuptake inhibitors. Correct antiepileptic/antiseizure medications. Explanation: Nonhormonal treatments for menopausal symptoms include selective serotonin reuptake inhibitors and serotonin norepinephrine reuptake inhibitors. Question: In the presence of mild hyperandrogenic symptoms related to polycystic ovarian syndrome (PCOS), the initial recommended treatment is: norethindrone/ethinyl estradiol (Lo Loestrin). Correct medroxyprogesterone (Provera). ethinyl estradiol (Estinyl). metformin (Glucophage). Explanation: In the presence of mild hyperandrogenic symptoms related to polycystic ovarian syndrome (PCOS), the initial recommended treatment is a combination oral contraceptive (i.e. norethindrone/ethinyl estradiol [Lo Loestrin]). Combined oral contraceptive therapy modestly inhibits gonadotropin secretion and thus gonadotropin- sensitive ovarian androgen production, and increases hepatic production of sex hormone binding globulin (SHBG), which further decreases free testosterone. Question: Which of the following medications would NOT be beneficial in the treatment of pain associated with fibrocystic breast disease? Spironolactone (Aldactone) Norethindrone/ethinyl estradiol (Lo Loestrin) Danazol Fluoxetine (Sarafem) Correct Explanation: Fluoxetine (Sarafem), an SSRI, is NOT recommended for the treatment of pain associated with fibrocystic breast disease. Spironolactone, a potassium-sparing diuretic; danazol, an androgen; and norethindrone/ethinyl estradiol, a combination oral contraceptive, may all be used for the treatment of pain associated with fibrocystic breast disease. Vitamin B6, vitamin E and evening primrose oil may be beneficial as well. Bromocriptine (Parlodel) may be used for more severe disease. Question: The copper component of the ParaGard intrauterine device to prevent pregnancy is thought to: thicken the endometrium and cervical mucus. decrease the movement of ovum through the fallopian tubes. interfere with estrogen uptake and decrease sperm motility. Correct suppress ovulation. Explanation: The copper component in the ParaGard intrauterine device is thought to prevent pregnancy by interfering with estrogen uptake, potentiating the local inflammatory response, and decreasing sperm motility. Question: The drug of choice to control mild abnormal uterine bleeding in a teenage patient is: estrogen only. androgen therapy. gonadotropin-releasing hormone analogs. combination estrogen/progesterone. Correct Explanation: A combined estrogen/progesterone oral contraceptive or progesterone only would be the treatment of choice for mild abnormal uterine bleeding in a teenager. Severe uterine bleeding is usually treated on an emergency basis with a short course of high-dose estrogen therapy. Treatment with androgens would only be indicated for short-term use to manage refractory bleeding. Question: A benefit associated with the use of medroxyprogesterone acetate (Depo-Provera), a progestin-only contraceptive, is: decreased risk of pelvic inflammatory disease. Correct decreased risk of cardiovascular risk factors. decreased risk of weight gain. decreased risk of osteoporosis. Explanation: Benefits associated with the use of medroxyprogesterone acetate (Depo-Provera), a progestin-only contraceptive, include decreased risk of endometrial cancer and pelvic inflammatory disease. Further benefits of Depo-Provera are decreased menstrual cramps, reduction in heavy uterine bleeding, decreased premenstrual syndrome symptoms, and decreased breast tenderness. Patients receiving Depo-Provera are at increased risk for experiencing a significant decrease in bone mineral density. Question: Progestin-only contraceptives: do not alter the quality or quantity of breast milk. Correct are not safe for use in women with cardiovascular disease. increase a patient's risk for pelvic inflammatory disease. are contraindicated in the presence of moderate hypertension. Explanation: Progestin-only contraceptives do not alter the quality or quantity of breast milk in lactating women. They may be used in women with cardiovascular risk factors. They are also safe for use in women who have an absolute or relative contraindication to estrogen and combined oral contraceptives, such as: age >45 years, breastfeeding, smoking, mild to moderate hypertension, well-controlled diabetes, or history of stroke or depression. Question: Late breakthrough bleeding or amenorrhea while taking an oral contraceptive may mean that the oral contraceptive has: not enough estrogen. too much estrogen. not enough progestin. Correct too much progestin. Explanation: Late breakthrough bleeding or amenorrhea while taking an oral contraceptive may mean that the oral contraceptive has too little progestin. Progesterone, LH and FSH are responsible for regulating endometrium shedding. If a woman is not pregnant, the corpus luteum disappears. The primary mechanism of action of hormonal contraceptives is that they suppress the secretion of gonadotropins (follicle-stimulating hormone, FSH and LH) through negative feedback inhibition. Question: In the prevention of pregnancy, medroxyprogesterone acetate (Depo-Provera) should be administered at least every: 4 weeks. 8 weeks. 10 weeks. 12 weeks. Correct Explanation: Medroxyprogesterone acetate (Depo-Provera), when used for the prevention of pregnancy, should be administered every 12-13 weeks. It has a 13-week period of effectiveness. Depo-Provera is classified as a progestin-only, injectable contraceptive. Question: Tranexamic acid (Lysteda), used in the treatment of abnormal uterine bleeding, should not be administered concomitantly with: nonsteroidal antiinflammatory drugs (NSAIDs). combination hormonal contraceptives. Correct statins. selective serotonin reuptake inhibitors. Explanation: Because tranexamic acid (Lysteda) is antifibrinolytic, concomitant use of hormonal contraception and Lysteda may further exacerbate the increased thrombotic risk associated with combination hormonal contraceptives. For this reason, concomitant use of Lysteda with combination hormonal contraceptives is contraindicated. Question: When treating hirsutism associated with polycystic ovarian syndrome, the best treatment is: norethindrone/ethinyl estradiol (Lo Loestrin). liraglutide (Victoza). metformin (Glucophage). spironolactone (Aldactone). Correct Explanation: Hirsutism associated with polycystic ovarian syndrome is more responsive to spironolactone (Aldactone). Antiandrogens are indicated if hirsutism is significant. If free testosterone and sex hormone binding globulin (SHBG) are not normalized after 3 months, the possibility of an androgen-secreting neoplasm should be considered. Antiandrogens (especially finasteride) should be avoided in pregnancy due to the potential for ambiguous genitalia in the male fetus. Question: Which of the following is NOT a steroidal progestin found in contraceptives? Drospirenone Prednisolone Correct Levonorgestrel Norethindrone Explanation: The term progestin is used for any natural or man-made substance that has properties similar to natural progesterone. All combination birth control pills contain estrogen (typically ethinyl estradiol) and one of eight kinds of progestin. These include: norethindrone, norethindrone acetate, ethynodiol diacetate, levonorgestrel, norgestrel, desogestrel, norgestimate, and drospirenone. Prednisolone is a systemic corticosteroid that has glucocorticoid and mineralocorticoid activity, but no progestational activity. Question: Danazol, classified as an androgen, is used in the treatment of abnormal uterine bleeding and endometriosis. It works by suppressing: follicle-stimulating hormone (FSH) and luteinizing hormone (LH). Correct human chorionic gonadotrophin (HCG) and luteinizing hormone (LH). gonadotrophin-releasing hormone (GnRH) and human chorionic gonadotropin (HCG). gonadotrophin-releasing hormone (GnRH) and sex binding hormone. Explanation: Danazol, an androgen, is used in the treatment of abnormal uterine bleeding and endometriosis. It works by suppressing follicle-stimulating hormone (FSH) and luteinizing hormone (LH). Question: Oral contraceptive regimens in which the estrogen and progestin both vary throughout the cycle are considered: monophasic. biphasic. triphasic. quadriphasic. Correct Explanation: Oral contraceptive regimens in which the estrogen and progestin doses both vary throughout the cycle are considered quadriphasic. Monophasic means that estrogen and progestin doses are fixed throughout the cycle. In biphasic oral contraceptive regimens, the estrogen dose remains the same for the first 21 days of the cycle, while progestin is lower in the first half and higher in the second half. When the estrogen remains consistent and the progestin varies, this is known as triphasic. Question: Uncomplicated vulvovaginal candidiasis can effectively be treated with: ketoconazole orally. itraconazole (Sporanox) orally. nystatin cream. miconazole (Monistat) vaginal suppository. Correct Explanation: Uncomplicated vulvovaginal candidiasis (VVC) can effectively be treated with miconazole (Monistat) vaginal cream/suppository. Short-course topical formulations (i.e., single dose and regimens of 1 to 3 days) effectively treat uncomplicated VVC. The topically applied azole drugs are more effective than nystatin. Treatment with azoles results in relief of symptoms and negative cultures in 80% to 90% of patients who complete therapy. Question: Patients taking oral contraceptives do NOT need to use a back-up method of contraception if taking: ampicillin. ketoconazole. phenytoin (Dilantin). metformin (Glucophage). Correct Explanation: Metformin (Glucophage) does not reduce the efficacy of oral contraceptives. Changes in glucose readings should be monitored closely. A back-up method of contraception should be used with rifampin (Rifadin), barbiturates, phenytoin (Dilantin), griseofulvin (Grifulvin), ampicillin, tetracycline (Sumycin), and carbamazepine (Tegretol). Question: Etonogestrel (Nexplanon) implant, used for contraception, is contraindicated in women: who are breastfeeding. who have migraine headaches. with a personal history of breast cancer. Correct who have coronary artery disease. Explanation: Etonogestrel (Nexplanon) implant is contraindicated as contraception in women with a current or past history of thrombosis or thromboembolic disorders, liver tumors (benign or malignant), active liver disease, undiagnosed abnormal genital bleeding, known or suspected breast cancer, personal history of breast cancer, or other progestin-sensitive cancers, now or in the past. Question: A woman who has had a hysterectomy complains of vaginal dryness, burning, and itching. A hormonal treatment is: progesterone only. oral combination contraceptives. low-dose oral estrogen. Correct implanted testosterone pellets. Explanation: A hormonal treatment for this patient is a low-dose oral estrogen. Low-dose vaginal estrogen therapy may also be considered. Genitourinary syndrome of menopause or atrophic vaginitis may cause vaginal dryness, burning, itching, atrophy, pruritus and dysuria. A progestin does not need to be added since the patient has had a hysterectomy. Question: In addition to inhibiting ovulation, combined contraceptives further prevent pregnancy by: creating a toxic environment for sperm. increasing the viscosity of cervical mucus. Correct decreasing production of sex hormone-binding globulin. thinning the uterine wall. Explanation: Combined hormonal contraceptives were developed to prevent ovulation by suppressing the release of gonadotropins. They inhibit follicular development and prevent ovulation as a primary mechanism of action. Additionally, all progestogen-containing contraceptives increase the viscosity of the cervical mucus, thereby inhibiting sperm penetration through the cervix into the upper genital tract (uterus and fallopian tubes). Etonogestrel (steroidal progestin) is approximately 32% bound to sex hormone-binding globulin (SHBG), and ethinyl estradiol induces an increase in the serum concentrations of SHBG. Question: If a patient is experiencing breast tenderness and hypertension, she may be taking an oral contraceptive with: not enough estrogen. too much estrogen. Correct not enough progestin. too much progestin. Explanation: An excess of any hormone creates an overall imbalance in the intricate endocrine system. Too much estrogen in an oral contraceptive may result in nausea, bloating, hypertension, breast tenderness and edema. Question: When using an oral contraceptive patch, the patient should be advised: that the patch can be placed anywhere on the trunk, including the breast. to tape the patch in place if it detaches and has been off less than 24 hours. Correct to remove the patch for 7 days every eighth week. to reapply the patch every 72 hours. Explanation: When using an oral contraceptive patch, the patient should be advised to apply the patch on the first Sunday after menses. The patch is worn for a week and then replaced weekly for 3 consecutive weeks. No patch is worn on the fourth week, resulting in menses. The patch should be applied to the upper arm, back, abdomen or buttocks. It should NOT be placed on the breasts. A patch that partially detaches or becomes completely removed can be reapplied or taped on as long as it has been off for less than 24 hours. Question: Which of the following medications is an aldosterone receptor antagonist and is used in the treatment of fibrocystic breast disease? Amiloride (Midamor) Chlorthalidone Indapamide Spironolactone (Aldactone) Correct Explanation: Spironolactone (Aldactone) and eplerenone (Inspra) are aldosterone receptor antagonists. The mechanism of action of spironolactone and eplerenone are to antagonize aldosterone-specific mineralocorticoid receptors, thus reducing testosterone levels. These are used in the treatment of fibrocystic breast disease and polycystic ovarian syndrome. Question: ParaGard intrauterine device should be changed every: 3 years. 5 years. 7 years. 10 years. Correct Explanation: ParaGard should be changed every 10 years. The copper component in the ParaGard intrauterine device is thought to prevent pregnancy by interfering with estrogen uptake, potentiating the local inflammatory response, and decreasing sperm motility. Question: When treating acne associated with polycystic ovarian syndrome, the best initial treatment is: norethindrone/ethinyl estradiol (Lo Loestrin). Correct liraglutide (Victoza). metformin (Glucophage). spironolactone (Aldactone). Explanation: Acne associated with polycystic ovarian syndrome (PCOS) is more responsive to oral contraceptives than other acne forms. Hirsutism associated with polycystic ovarian syndrome is more responsive to spironolactone (Aldactone). A combination with antiandrogens is usually necessary for hirsutism or severe acne. The combination targets androgen production and androgen action associated with PCOS. Question: A common side effect of medroxyprogesterone acetate (Provera), a progesterone derivative, is: dizziness. muscle cramping. breast tenderness. Correct vaginal atrophy. Explanation: Common side effects of medroxyprogesterone acetate (Provera), a progesterone derivative, are breast tenderness or discharge, hives, increased acne, spotting or breakthrough bleeding, vaginal itching or discharge, changes in appetite, bloating and insomnia. Question: The contraceptive that would be most appropriate for a lactating woman is: levonorgestrel/ethinyl estradiol transdermal (Ortho Evra). etonogestrel/ethinyl estradiol vaginal ring (NuvaRing). oral norethindrone (Jolivette). Correct levonorgestrel/ethinyl estradiol (Seasonique). Explanation: Norethindrone (Jolivette) is a progestin-only contraceptive that is safe for use during lactation. Progestin-only contraceptives do not alter the quality or quantity of breast milk in lactating women. The others are a combination of estrogen and progestin and are not recommended during lactation, regardless of the route. Question: Intrauterine devices for contraception: have no systemic effect on hormones. Correct are not safe for long-term use. may cause uncomfortable intercourse. never spontaneously expel. Explanation: Intrauterine devices for contraception are undetectable during intercourse, have no systemic effect on hormones, are cost-effective if used long term, and have no effect on milk production. Intrauterine devices are spontaneously expelled in about 2-5% of patients. Question: Medroxyprogesterone (Provera), used to provide contraception and manage abnormal uterine bleeding, does NOT exhibit: androgenic effects. anabolic effects. estrogenic activity. Correct progesterone activity. Explanation: Medroxyprogesterone (Provera) is a derivative of progesterone, a progestogen steroid hormone. It is secreted by the corpus luteum, a temporary endocrine gland that the female body produces after ovulation during the second half of the menstrual cycle. Androgenic and anabolic effects have been noted with administration of medroxyprogesterone, but the drug appears to be devoid of significant estrogenic activity. Question: Etonogestrel (Nexplanon) implant for contraception: is effective for 5 years. produces a quicker return to fertility than medroxyprogesterone (Depo- Provera). Correct is not safe for women with moderate to severe obesity. does not affect libido. Explanation: Once the etonogestrel (Nexplanon) implant is removed, hormone levels usually return to normal with 7 days. Pregnancies may occur as early as 7 to 14 days after removal. Therefore, a woman should re-start contraception immediately after removal of the implant if continued contraceptive protection is desired. The median time to conception after receiving the last dose of medroxyprogesterone (Depo-Provera) is 10 months, with a range of 4 to 31 months. Nexplanon releases etonogestrel for three years after implantation. It requires no additional attention after implant, is safe for all body weights, does not affect lactation, and has a quick return to fertility after removal. It may produce a loss of libido. Question: Combination estrogen and progesterone therapy: does not increase the risk of heart attack or stroke. increases the risk for deep vein thrombosis (DVT) and gallbladder disease. Correct only increases breast cancer risk in the presence of family history. preserves ovarian function in premenopausal women. Explanation: Combined estrogen and progesterone therapy is linked to a small increased risk for heart attack, an increased risk for stroke and deep vein thrombosis, and a small increased risk for breast cancer. This risk may be related to age, existing medical conditions, and when a woman starts taking hormone therapy. Some research suggests that for women who start combined therapy within 10 years of menopause and who are younger than 60 years, combined therapy may protect against heart attacks. A small increased risk of gallbladder disease is associated with estrogen therapy with or without progestin. The risk is greatest with forms of therapy taken by mouth. Question: Fluconazole (Diflucan), an antifungal, should not be administered concomitantly with: zolpidem (Ambien). amoxicillin (Moxatag). ethinyl estradiol/drospirenone (Yaz). erythromycin (Ery-Tab). Correct Explanation: The concomitant use of erythromycin (Ery-Tab) and fluconazole is contraindicated due to the enhancement of the QTc-prolonging effect of erythromycin. Fluconazole may increase the serum concentration of erythromycin. Question: The recommended treatment of recurrent vulvovaginal candidiasis is fluconazole administered: as a single oral dose. daily for 7 days. daily for 3 months. weekly for 6 months. Correct Explanation: Recurrent vulvovaginal candidiasis (RVVC) is usually defined as four or more episodes of symptomatic VVC within 1 year. The recommended treatment regimen is 150 mg orally weekly x 6 months. The initial therapy is 150 mg orally every 72 hours x 3 doses and then weekly. Question: For treatment of menopausal symptoms in a woman with a history of hormone-sensitive breast cancer, the nurse practitioner should consider: androgen therapy. gonadotropin-releasing hormone analogs. selective serotonin reuptake inhibitors. Correct progesterone-only therapy. Explanation: Combined estrogen and progesterone therapy is associated with a small increased risk for breast cancer. Currently, it is recommended that women with a history of hormone- sensitive breast cancer first try nonhormonal therapies, such as a selective serotonin reuptake inhibitors (i.e. paroxetine [Paxil]), for the treatment of menopausal symptoms. Question: Which of the following is NOT true about hormone replacement therapy (HRT) in menopause? Regardless of route of hormone replacement therapy, the lowest dose for the shortest amount of time should be utilized. Estrogen and progestin should be given together if the uterus is still intact. Every woman should be placed on hormone replacement therapy for at least 2 years to prevent cardiovascular effects of menopause. Correct Estrogen therapy is contraindicated with a history of breast cancer, active thrombosis or thrombophlebitis and active liver disease. Explanation: Hormone replacement therapy (HRT) should be carefully considered and individualized for each patient. The lowest dose for the shortest amount of time should be considered, regardless of route. Estrogen alone may be used if the uterus has been removed; with an intact uterus, progestin must be added to the estrogen. Estrogen therapy is contraindicated in women with a history of breast cancer, undiagnosed vaginal bleeding, active thrombosis or thrombophlebitis, endometrial adenocarcinoma and/or active liver disease. Question: A Bartholin’s gland abscess caused by Staphylococcal aureus infection is best treated with: amoxicillin-clavulanate (Augmentin). cephalexin (Keflex). clindamycin (Cleocin). Correct metronidazole (Flagyl). Explanation: A Bartholin’s gland abscess caused by Staphylococcus aureus is best treated with clindamycin (Cleocin), a lincosamide antibiotic. Due to high rates of resistance, penicillin and cephalosporins are not recommended. Metronidazole is not indicated in the treatment of staphylococcal infections. Question: Transdermal contraceptives, when compared to oral combined contraceptives,: have the same pharmacokinetics. require higher peak doses to achieve therapeutic effects. have constant plasma hormone levels, without peaks and troughs. Correct are safer in women who smoke. Explanation: Therapeutic effects of transdermal contraceptives are achieved at lower peak doses since first-pass hepatic metabolism and enzymatic degradation in the gastrointestinal tract are avoided. Therefore, plasma hormone levels remain constant (peaks and troughs do not occur). Sustained drug delivery reduces the need for frequent self- administration, and thus may improve patient compliance. The non-oral route of administration is useful for patients who have difficulty swallowing pills. Cigarette smoking increases the risk of cardiovascular effects in women receiving contraceptive therapy and should not be used. Question: A patient who is complaining of early or midcycle bleeding may need an oral contraceptive with: more estrogen. Correct less estrogen. more progestin. less progestin. Explanation: Too little estrogen in an oral contraceptive may result in early or midcycle breakthrough bleeding and increased spotting for some women. Estrogen stabilizes the endometrium. As the endometrium adjusts to a new thin state, it is fragile and atrophic. The most common cause of breakthrough bleeding is thought to be missed pills. Do not consider a change in dosing unless the breakthrough bleeding continues through at least three cycles. Question: Which of the following would NOT be an appropriate choice for the treatment of primary dysmenorrhea in an 18-year-old woman? Nonsteroidal anti-inflammatory medications Oral contraceptives Vitamin B6 Intrauterine devices Correct Explanation: The initial treatment choices for primary dysmenorrhea are nonsteroidal antiinflammatory medications (NSAIDs), oral contraceptives, vitamin B6 and omega-3 supplements. Intrauterine devices may be considered only as a last resort, due to potential complications with the device. Primary dysmenorrhea typically abates as a patient ages or has children. Question: The brand name for medroxyprogesterone acetate, a progestin-only contraceptive, is: Depo-Medrol. Depo-Provera. Correct Lupron Depot. Depo-Testosterone. Explanation: The brand name for medroxyprogesterone acetate is Depo-Provera. It is a progestin injectable and provides contraception for 13 weeks. The generic name for Depo-Medrol is methylprednisolone acetate (a systemic corticosteroid); Lupron Depot is leuprolide (a hormonal oncologic); and Depo-Testosterone is testosterone cypionate (an androgen). Question: Spironolactone (Aldactone), used in the treatment of polycystic ovarian syndrome, is highly protein bound and has a duration of: 6 hours. 12 hours. 24 hours. 48 hours. Correct Explanation: Spironolactone (Aldactone) is greater than 90% protein bound and has a half-life elimination of 1.4 hours and a duration of 48 to 72 hours. Spironolactone is used to reduce the symptoms of hirsutism and is classified as an androgen receptor blocker. It may take up to 12 months to see improvement in hirsutism. Question: A 23-year-old woman is receiving spironolactone (Aldactone) for premenstrual dysphoric disorder. At follow-up, she has a serum potassium of 5.8 mEq/L. The nurse practitioner should: discontinue spironolactone (Aldactone). discontinue the spironolactone (Aldactone) and administer kayexalate. hold spironolactone (Aldactone) until hyperkalemia is resolved. Correct discontinue spironolactone (Aldactone) and begin a thiazide diuretic. Explanation: If serum potassium increases to more than 5.5 mEq/L or renal function worsens while receiving spironolactone (Aldactone), further doses should be held until potassium is less than 5 mEq/L. Consider restarting with a reduced dose after confirming resolution of hyperkalemia/renal insufficiency for at least 72 hours. Spironolactone is an androgen receptor blocker. Question: The mechanism of action of levonorgestrel in the Mirena intrauterine device is to: thicken the endometrium and cervical mucus. Correct decrease the movement of ovum through fallopian tubes. increase estrogen uptake and decrease sperm motility. suppress gonadotropic hormones. Explanation: The levonorgestrel in Mirena intrauterine devices causes thickening of the cervical mucus and thinning of the endometrium. Other hypotheses for the mechanism of action of Mirena includes increased motility in the fallopian tubes (moving ovum through rapidly) and inflammatory effects on the endometrium interfering with sperm survival, motility and/or capacitation. Question: Danazol is indicated in the treatment of: ectopic pregnancy. endometriosis. Correct gonadal hypertrophy. ovulatory dysfunction. Explanation: Danazol, an androgen, is indicated in the treatment of endometriosis and fibrocystic breast disease. It works by suppressing follicle-stimulating hormone (FSH) and luteinizing hormone (LH). Question: Etonogestrel (Nexplanon) implant for contraception contains: estrogen only. progesterone only. Correct equal amounts of estrogen and progesterone. a higher dose of progesterone than estrogen. Explanation: Etonogestrel implant (Nexplanon) contains only progestin. It is implanted subdermally in the upper arm and releases etonogestrel for 3 years. It requires no additional attention after implant, is safe for all body weights, does not affect lactation, and has a quick return to fertility after removal. It may produce a loss of libido. Question: A 23-year-old woman complains of breakthrough bleeding 1 month after being started on a combination oral contraceptive (OC). The nurse practitioner should: advise the patient to use additional protection during intercourse, until resolved. change to a progestin-only formulation. advise the patient that breakthrough bleeding in the first 3 months is common. Correct change to a contraceptive patch for better regulation of hormones. Explanation: Breakthrough bleeding may occur in up to 50% of patients during the first 3 months of taking a combined oral contraceptive. If it does not abate after 3 months, another form of contraceptive should be considered. Breakthrough bleeding does not indicate a decrease in the pill's effectiveness. Most breakthrough bleeding is caused by missing pills. Question: Which statement is true about diaphragms in comparison to pharmacologic methods of contraception? They are as effective as oral contraceptives. They can be removed immediately after intercourse. They may cause recurrent bladder infections. Correct They are not as effective in preventing sexually transmitted diseases. Explanation: When used for contraception, diaphragms may cause recurrent bladder infections. They are helpful in the prevention of sexually transmitted diseases. Diaphragms are less effective than oral contraceptives, require dexterity to insert properly, must be left in place for at least 6 hours after intercourse, and may cause bacterial vaginosis and vaginal yeast infections. Question: Which medication is considered an estrogen for the control of abnormal uterine bleeding? Medroxyprogesterone acetate (Provera) Ethinyl estradiol (Estinyl) Correct Danazol (Danocrine) Progestin (Aygestin) Explanation: Ethinyl estradiol (EE) is an orally active estrogen and a synthetic derivative of estradiol, a steroid hormone that is the major endogenous estrogen in humans. EE is a component of almost all formulations of combined oral contraceptive pills and is the most common estrogen used for this purpose. Danazol is classified as a synthetic steroid derived from ethisterone. Medroxyprogesterone is a progestin. Progestins are synthetic progesterones. Question: Side effects of levonorgestrel (Plan B) to prevent pregnancy may include: severe abdominal bloating and cramping. nausea and vomiting. Correct breast tenderness and discharge. vaginal discharge and edema. Explanation: Side effects of levonorgestrel (Plan B) may include menstrual changes, nausea and vomiting, lower abdominal pain, fatigue, headache, dizziness, and breast tenderness. Side effects do not include bloating, breast discharge, vaginal discharge or vaginal edema. Question: A monophasic oral contraceptive: contains only ethinyl estradiol and is administered in a 21-day cycle. does not contain a placebo and is administered in a 28-day cycle. contains estrogen and progestin. Doses are fixed throughout the cycle. Correct delivers estrogen for 7 days, then progesterone for 7 days, then combined estrogen/progesterone for 7 days. Explanation: Oral contraceptives that are monophasic provide fixed estrogen and progestin doses throughout the cycle. These are typically given as 21 tablets of estrogen plus progestogen, followed by seven tablets of placebo or an iron supplement. In biphasic oral contraceptives, the estrogen dose remains the same for the first 21 days of the cycle, while progestin is lower in the first half and higher in the second half. In triphasic dosing, the estrogen remains consistent, but the progestin varies. Oral contraceptive dosing in which the estrogen and progestin doses both vary throughout the cycle are considered quadriphasic. Question: Medroxyprogesterone acetate (Provera) reduces abnormal uterine bleeding by: halting the production of estrogen. stimulating the pituitary gland to produce follicle-stimulating hormone (FSH). maintaining the corpus luteum and thus uterine thickness. preventing overgrowth of the endometrium. Correct Explanation: Medroxyprogesterone acetate (Provera) reduces abnormal uterine bleeding by preventing overgrowth of the endometrium, which prevents dysfunctional uterine bleeding. Heavy bleeding is often the product of irregular breakdown of the endometrium in teens and women who aren’t ovulating regularly. Progesterone promotes ovulation and restores a predictable cyclic monthly menstrual period. Question: Buspirone (BuSpar), used in the treatment of anxiety related to premenstrual dysphoric disorder,: requires a dosing decrease in patients with mild to moderate renal impairment. Correct is a controlled substance. may lead to physical dependence or tolerance. should not be used in patients older than 65. Explanation: Buspirone hydrochloride (BuSpar) is metabolized by the liver and excreted by the kidneys. Patients with impaired hepatic or renal function show increased plasma levels and a lengthened half-life of buspirone. Therefore, the administration of BuSpar to patients with mild to moderate impaired hepatic or renal function should be reduced. BuSpar is not a controlled substance and has not shown potential for abuse or diversion. Research shows age-related effects on the pharmacokinetics of buspirone, but greater sensitivity in older patients should be considered. Question: Fluconazole (Diflucan), an antifungal,: should be decreased in dose in the presence of renal impairment. Correct should be administered with food. is only effective against Candida albicans. is not effective in the treatment of oropharyngeal and esophageal candidiasis. Explanation: The pharmacokinetics of fluconazole (Diflucan) are markedly affected by reduction in renal function. There is an inverse relationship between the elimination half-life and creatinine clearance. The dose of fluconazole may need to be reduced in patients with impaired renal function. Fluconazole may be taken without regard to meals. It is active against most strains of Candida albicans, Candida glabrata (many strains are intermediately susceptible), Candida parapsilosis, Candida tropicalis, and Cryptococcus neoformans. Fluconazole is indicated in the treatment of oropharyngeal, esophageal and vulvovaginal candidiasis. Question: When using metformin (Glucophage) to restore ovulation/menses in polycystic ovary syndrome, full restoration may take up to: 1 month. 2 months. 3 months. 9 months. Correct Explanation: When using metformin to restore ovulation/menses in polycystic ovary syndrome, full restoration may take up to 6-9 months. Metformin can restore ovulation/menses to the point where conception is possible. Some studies suggest that metformin may be less effective in morbidly obese women. The initial and safest measure to restore ovulation is weight loss (in overweight patients). Question: A 23-year-old woman with a desire for pregnancy needs treatment for symptoms related to polycystic ovarian syndrome (PCOS). The initial choice is: liraglutide (Victoza). metformin (Glucophage). Correct spironolactone (Aldactone). finasteride (Proscar). Explanation: The first-line choice for a young woman who desires pregnancy is metformin (Glucophage). Spironolactone and finasteride are second-line therapy options. Victoza is not indicated in the treatment of PCOS. Question: Combined contraceptive patches: are replaced every 14 days. have fewer side effects than oral contraceptives. may not be as effective in women weighing more than 200 pounds. Correct are safer than oral contraceptives in patients with hypertension. Explanation: Contraceptive patches may not be as effective in women who weight >198 pounds. They have the same efficacy, contraindications and side effects as oral contraceptives. Side effects may be more pronounced or severe with the patch, since it may result in higher plasma concentrations. In addition, patches may cause skin irritation. Question: Women who have had levonorgestrel (Mirena) implanted to prevent pregnancy do NOT need to immediately report: painful intercourse. fever with vaginal discharge. string disappearance. amenorrhea. Correct Explanation: Women who have had levonorgestrel (Mirena) implanted would NOT need to immediately report amenorrhea. Although this is a potential side effect, it is expected. Women should be advised to immediately report signs and symptoms of infection, which may include: abdominal pain, fever or chills, unusual bleeding, foul-smelling discharge, fever with vaginal discharge, string disappearance and painful intercourse. Question: Medications that may be helpful in the treatment of vulvodynia include: oral contraceptives. selective serotonin reuptake inhibitors. antidepressants and anticonvulsants. Correct antibiotics and anti-inflammatories. Explanation: Vulvodynia is defined as idiopathic vulvar discomfort, most often described as burning pain occurring in the absence of relevant visible findings or a specific, clinically identifiable neurologic disorder. Discomfort may be provoked by physical contact that is sexual, nonsexual or both. Vulvodynia benefits from reduction of anxiety and stress and is treated as a chronic pain condition. Select antidepressants such amitriptyline (Elavil) and desipramine (Norpramin), and anticonvulsants such as gabapentin (Neurontin), may be helpful in treating the symptoms of vulvodynia. Question: Combined oral contraceptive use is absolutely contraindicated in patients who: are older than 35 years and smoke a pack of cigarettes/day. Correct develop migraine headaches after starting oral contraceptives. are 6-12 weeks postpartum and breastfeeding. had breast cancer more than 5 years ago. Explanation: Combined oral contraceptive use is absolutely contraindicated in patients who are older than 35 and smoke more than 15 cigarettes per day. Cigarette smoking increases the risk of cardiovascular side effects. The risk increases with age (35 years) and heavy smoking (15 or more cigarettes per day). Situations in which the benefits should outweigh the risks, but are not absolutely contraindicated, are considered "relative." Relative contraindications include: 1) smoking less than 15 cigarettes per day; 2) more than 5 years post-breast cancer; 3) first 3 weeks postpartum if not breastfeeding, and for the first month if breastfeeding. Question: Spironolactone (Aldactone), sometimes used to reduce the symptoms of hirsutism related to polycystic ovarian syndrome, is classified as a(n): androgen agonist. estrogen agonist. progesterone antagonist. androgen receptor blocker. Correct Explanation: Spironolactone (Aldactone) is an androgen receptor blocker. After treatment is initiated, it may take up to 12 months to see improvement in hirsutism. Acne is more responsive, and usually responds within 2 months. Question: Which medication is NOT the best first choice for the treatment of anxiety/mood disorders related to premenstrual dysphoric disorder? Ethinyl estradiol/drospirenone (Yaz) Fluoxetine hydrochloride (Sarafem) Paroxetine (Paxil) Clonazepam (Klonopin) Correct Explanation: Benzodiazepines such as clonazepam (Klonopin) are NOT the best choice for the treatment of anxiety/mood disorders related to premenstrual dysphoric disorder (PMDD) due to the risk for dependence. Benzodiazepines may be suitable as second-line therapy for debilitating behavior symptoms. Combined oral contraceptives (i.e. ethinyl estradiol/drospirenone [Yaz]), selective serotonin reuptake inhibitors (SSRIs; i.e. fluoxetine hydrochloride [Sarafem] and paroxetine [Paxil]) are indicated in the treatment of PMDD. SSRIs inhibit reuptake of serotonin and address the neurotransmitter deficiency believed to underlie the pathogenesis of PMDD. Combined oral contraceptives regulate menses and symptom suppression. Question: The brand name for fluconazole, an antifungal, is: Cancidas. Diflucan. Correct Micatin. Sporanox. Explanation: The brand name for fluconazole is Diflucan. Diflucan is an antifungal used in the treatment of oropharyngeal, esophageal and vulvovaginal candidiasis. The generic name for Cancidas is caspofungin; Micatin is miconazole; and Sporanox is itraconazole. These are all classified as antifungal agents. Question: The highest risk of deep vein thrombosis (DVT) is associated with combined estrogen and progesterone therapy that is administered via: the oral route. Correct transdermal patch. intravaginal cream. intravaginal ring. Explanation: Combined estrogen and progesterone therapy and estrogen-only therapy are associated with a small increased risk for stroke and deep vein thrombosis (DVT). Forms of therapy not taken by mouth (patches, sprays, rings, and others) are associated with less risk for DVT than those taken by mouth. Question: Which of the following is true about missed doses of oral contraceptives? If one dose is missed, skip it and take the next dose due. If one dose is missed, take it as soon as it is remembered. If not remembered until the next day, do NOT take two tablets at the same time. If two consecutive pills are missed, take two pills per day for the next 2 days. Correct If three consecutive pills are missed, the pack will need to be restarted. Explanation: Patients should be advised to take oral contraceptive pills at the same time daily. If one oral contraceptive pill is missed, the patient should take the missed pill as soon as remembered. If not remembered until time for next pill, the patient should take two pills. If two consecutive pills are missed, the patient should take two pills per day for the next 2 days and then resume one pill per day. Advise the patient to use vaginal spermicide and condoms for the remainder of the cycle. For three or more pills missed, it depends on the type of oral contraceptive, and at what time frame in the pack it was missed. Question: Etonogestrel/ethinyl estradiol (NuvaRing), a contraceptive vaginal ring,: contains only estrogen. contains only progestin. is replaced weekly for 3 weeks, followed by 1 week ring-free. releases higher doses of progestin steroids per day than estrogen. Correct Explanation: NuvaRing is an estrogen/progestin combination hormonal contraceptive (CHC) indicated for use by women to prevent pregnancy. It is a polymeric vaginal ring containing 11.7 mg etonogestrel (steroidal progestin) and 2.7 mg ethinyl estradiol (steroidal estrogen), which releases on average 0.12 mg/day of etonogestrel and 0.015 mg/day of ethinyl estradiol. The ring must remain in place continuously for 3 weeks, followed by a 1-week ring-free interval. Question: Prior to major surgery with prolonged immobilization, combined contraceptives should be stopped at least: 1 week before surgery. 2 weeks before surgery. 3 weeks before surgery. 4 weeks before surgery. Correct Explanation: Except for emergency surgery, all combined contraceptives should be stopped at least 4 weeks before and for 2 weeks after major surgery. The decreased mobilization associated with surgery increases the patient's risk of thromboembolism. Question: Combined oral contraceptives are NOT likely to cause: thromboembolism. hypertension. gallbladder disease. ovarian cysts. Correct Explanation: The use of combined oral contraceptives may cause life-threatening or serious complications including thrombophlebitis and thromboembolism, hepatocellular adenomas, stroke, gallbladder disease and hypertension. Taking combined oral contraceptives may reduce the development of ovarian cysts. Question: Topical creams and suppositories used in the treatment of vulvovaginal candidiasis: are water based. may weaken condoms and diaphragms. Correct have the same side effects as oral preparations. should also be used to treat sex partners to prevent recurrence. Explanation: The creams and suppositories in these regimens are oil-based and may weaken latex condoms and diaphragms. Intravaginal preparations of clotrimazole, miconazole (Monistat), and tioconazole (Monistat 1-Day) are available over the counter. Topical agents usually cause no systemic side effects, but local burning or irritation might occur. Question: Patients who have been treated with danazol for abnormal uterine bleeding should be instructed that ovulation and cyclic bleeding should resume within: 14 days. 21 days. 30 days. 90 days. Correct Explanation: Ovulation and cyclic bleeding usually return within 60 to 90 days after danazol is discontinued. Danazol, an androgen, is used in the treatment of abnormal uterine bleeding and endometriosis. It works by suppressing follicle-stimulating hormone (FSH) and luteinizing hormone (LH). Question: Combined contraceptives, whether oral, patch or intravaginal, work in the ovulatory phase by: increasing follicle-stimulating hormone and luteinizing hormone. decreasing follicle-stimulating hormone and increasing luteinizing hormone. suppressing follicle-stimulating hormone and luteinizing hormones. Correct increasing the release of follicle-stimulating hormone and luteinizing hormone. Explanation: Contraceptives, whether oral, patch or intravaginal, work in the ovulatory phase by suppressing the pituitary gonadotropins of follicle-stimulating hormone and luteinizing hormone. This inhibits ovulation. Question: A 18-year-old patient took levonorgestrel (Plan-B) 24 hours after unprotected sex. She calls the office and requests additional information. The provider should advise the patient: that plan B will protect her from becoming pregnant for 1 to 2 weeks after administration. to expect spotting or bleeding before her next period. Correct that she may experience severe abdominal pain 24 hours after taking the medication. to expect her menstrual cycle to be up to 2 weeks late. Explanation: Some women taking levonorgestrel (Plan B One-Step) will have menstrual changes such as spotting or bleeding before their next menstrual cycle. Some women may have a heavier or lighter next period, or a period that arrives earlier or later than usual. If the patient's period is more than a week late, she may be pregnant and should be tested. If the patient has severe abdominal pain, she may have an ectopic pregnancy and should receive immediate medical attention. The patient should resume her regular method of contraception or begin one, if needed. Plan B does not protect against additional acts of unprotected sex. Question: The best choice for short-term treatment of severe abnormal uterine bleeding is: estrogen only. Correct androgen therapy. gonadotropin-releasing hormone analogs. combination estrogen/progesterone. Explanation: Severe uterine bleeding is usually treated on an emergency basis with a short course of high-dose estrogen therapy. If that isn't effective (a rare occurrence), a dilation and curettage (D&C) may be done to clear the uterus of tissue. Combined oral contraceptives will require at least a 21-day course to evaluate efficacy, but improvement occurs in approximately 80% of cases within 3 days. Question: Danazol, an androgen, may cause: clitoral atrophy. breast tenderness. edema. Correct weight loss. Explanation: Danazol, an androgen, is indicated in the treatment of endometriosis and fibrocystic breast disease. Androgen-like effects include weight gain, acne and seborrhea. Mild hirsutism, edema, hair loss, or voice change may occur and may persist after cessation of therapy. Hypertrophy of the clitoris is rare. Because danazol may cause some degree of fluid retention, conditions that might be influenced by this factor (e.g., epilepsy, migraine, cardiac or renal dysfunction, polycythemia and hypertension) require careful observation. Question: Which of the following is NOT true about the administration of medroxyprogesterone acetate (Depo-Provera)? Few drug-drug interactions are associated with intramuscular Depo-Provera compared to oral contraceptives. Correct Depo-Provera must be discontinued and an alternate contraceptive considered at least 6 months before attempting pregnancy. Menses may not return for 3 to 12 months after the last Depo-Provera injection. Patients should be advised to take calcium and vitamin D while taking Depo-Provera. Explanation: Drug-drug or drug-herbal interactions have been noted between medroxyprogesterone acetate (Depo-Provera) and any product that induces the metabolic enzymes in the liver, including CYP3A4. Drugs or herbal products that induce such enzymes may decrease the effectiveness of hormonal contraceptives. Some drugs or herbal products that may decrease the effectiveness of hormonal contraceptives include barbiturates (i.e., phenobarbital), carbamazepine (Tegretol), felbamate (Felbatol), griseofulvin (Grifulvin V), oxcarbazepine (Trileptal), phenytoin (Dilantin), rifampin (Rifadin), St. John's wort and topiramate (Topamax). The average return to fertility after stopping Depo- Provera is 12-18 months. Question: Oral contraceptives in which the estrogen remains consistent, but the progestin varies throughout the cycle, is considered: monophasic. biphasic. triphasic. Correct quadriphasic. Explanation: Oral contraceptive regimens in which the estrogen remains consistent, but the progestin varies throughout the cycle, are triphasic. Monophasic means that estrogen and progestin doses are fixed throughout the cycle. In biphasic oral contraceptives, the estrogen dose remains the same for the first 21 days of the cycle, while progestin is lower in the first half and higher in the second half. When the estrogen and progestin doses both vary throughout the cycle, the regimen is quadriphasic. Question: In oral contraceptives, when the estrogen dose remains the same for the first 21 days of the cycle and progestin is lower in the first half and higher in the second half, the regimen is classified as: monophasic. biphasic. Correct triphasic. quadriphasic. Explanation: In oral contraceptives, when the estrogen dose remains the same for the first 21 days of the cycle and progestin is lower in the first half and higher in the second half, the regimen is biphasic. Monophasic means that estrogen and progestin doses are fixed throughout the cycle. Oral contraceptive dosing in which the estrogen remains consistent, but the progestin varies throughout the cycle, is considered triphasic. When the estrogen and progestin doses both vary throughout the cycle, it is quadriphasic. Question: Which of the following is NOT a mechanism of action for progestin-only contraceptives, also known as the "mini-pill"? Suppressing ovulation Creating an atrophic endometrium Thickening the cervical mucus Creating an alkaline vaginal environment Correct Explanation: Oral contraceptives containing only progestin work by suppressing ovulation, creating a thin, atrophic endometrium, and thickening the cervical mucus. This environment makes sperm penetration difficult. Progestin-only contraception is an option for women in whom an estrogen-containing contraceptive is contraindicated or causes additional health concerns. Question: Spermicides to prevent pregnancy: cannot be used in conjunction with a condom. help to prevent gonorrhea and chlamydia. Correct may affect long-term fertility. should not be use as a back-up method for other contraceptives. Explanation: Spermicides are 70-80% effective when used alone and 99% effective when used with a condom. They help prevent sexually transmitted diseases (STDs), especially gonorrhea and chlamydia. Spermicides are available without a prescription and are relatively inexpensive. The can serve as a backup method for other contraceptives, do not interfere with lactation, and do not affect fertility. They may cause irritation or burning of the vulva or the penis of the woman's partner. Question: Serious adverse reactions of progesterone therapy that warrant immediate medical attention include: breakthrough bleeding. nipple discharge. low blood pressure. calf pain and swelling. Correct Explanation: Progesterone therapy may rarely cause serious (possibly fatal) problems from blood clots (e.g., heart attack, stroke, blood clots in the lungs or legs, blindness). Patients should be advised to seek immediate medical attention if they experience signs and symptoms of a heart attack, stroke or deep vein thrombosis. While nipple discharge and breakthrough bleeding may be potential side effects and should be reported to the prescriber, they are not a reason to seek immediate medical care. This medication may increase blood pressure, especially in patients with a diagnosis of hypertension. Question: Before prescribing oral contraceptives, the nurse practitioner should check for: anemia. human papillomavirus via Pap test. sexually transmitted diseases. pregnancy. Correct Explanation: Before prescribing oral contraceptives, the nurse practitioner should always check for pregnancy. Administering oral contraceptives in pregnancy is absolutely contraindicated. Depending on the patient's risk factors, a Pap test and screening for HPV and sexually transmitted diseases may be indicated. However, these are not absolutely necessary before initiating oral contraceptives. Routine screening for anemia is not necessary prior to initiating oral contraceptives. Question: Potential side effects associated with the use of combined oral contraceptives are: cyclic weight gain and fluid retention. Correct decreased appetite and weight loss. depression and headaches. increased risk for sexually transmitted infections. Explanation: Potential side effects associated with the use of combined oral contraceptive are nausea, breast fullness and/or tenderness, cyclic weight gain and fluid retention, breakthrough bleeding, decreased menstrual flow/amenorrhea, fatigue, acne, mild headaches, and increased appetite. Question: The best treatment choice for polycystic ovarian syndrome in a 23-year-old woman with an intact uterus and history of migraine with aura is: levonorgestrel/ethinyl estradiol (Seasonique). levonorgestrel /ethinyl estradiol transdermal (Ortho Evra). levonorgestrel (Mirena) intrauterine device. medroxyprogesterone acetate (Depo-Provera). Correct Explanation: The treatment of choice for a patient with polycystic ovarian disease and a history of migraine with aura is medroxyprogesterone acetate (Depo-Provera). Combined hormones are contraindicated in patients with migraine with aura. Mirena intrauterine device is not indicated in the treatment of polycystic ovarian disease and may cause worsening of ovarian cysts. Question: When prescribing spironolactone for fibrocystic breast disease or polycystic ovarian syndrome, the nurse practitioner should provide initial and routine monitoring of: serum potassium and creatinine. Correct urine aldosterone and potassium levels. serum platelets and liver function. serum CBC and TSH. Explanation: After the initiation of spironolactone (Aldactone), serum potassium and renal function should be checked at 3 days, at 1 week, and at least monthly for the first 3 months of therapy, followed by every 3 months thereafter. If serum potassium increases to more than 5.5 mEq/L or renal function worsens, further doses should be held until potassium is less than 5 mEq/L. Consider restarting with a reduced dose after confirming resolution of hyperkalemia/renal insufficiency for at least 72 hours. Question: When a woman experiences weight gain, fatigue and changes in mood, her oral contraceptive may have too: little estrogen. much estrogen. little progestin. much progestin. Correct Explanation: Increased appetite, weight gain, fatigue and changes in mood experienced while taking an oral contraceptive may signal that the oral contraceptive has too much progestin. These side effects usually resolve after several cycles. Question: The half-life of fluconazole (Diflucan) for the treatment of vulvovaginal candidiasis is approximately: 8 hours. 12 hours. 18 hours. 30 hours. Correct Explanation: The half-life of fluconazole (Diflucan) for the treatment of vulvovaginal candidiasis is approximately 30 hours (range: 20 to 50 hours) after oral administration. Peak plasma concentrations (Cmax) in fasted normal volunteers occur between 1 and 2 hours. The recommended dosing for uncomplicated vulvovaginal candidiasis (VVC) is 150 mg orally x 1 dose; for severe cases of VVC, it is 150 mg orally every 72 hours x 2 doses. Question: Tranexamic acid (Lysteda), used in the treatment of abnormal uterine bleeding, is classified as a(n): estrogen. progesterone. androgen. antifibrinolytic. Correct Explanation: Tranexamic acid (Lysteda), used in the treatment of abnormal uterine bleeding, is classified as an antifibrinolytic. The mechanism of action of Lysteda is to competitively inhibit multiple plasminogen binding sites, decreasing plasmin formation and fibrinolysis. Antifibrinolytic agents slow the rate of blood loss and provide symptomatic control during menstruation. Antifibrinolytic agents are used when combined estrogen and progestogen therapy are contraindicated. Question: Prior to the initiation of paroxetine (Paxil) to treat mood disorder related to premenstrual dysphoric disorder in an 18-year-old woman, the nurse practitioner should check for: altered liver function tests. suicidal thinking. Correct obsessive compulsive disorder. decreased bone mineral density. Explanation: Prior to the initiation of paroxetine (Paxil) to treat mood disorder related to premenstrual dysphoric disorder in an 18-year-old woman, the nurse practitioner should check for suicidal thinking. There is no clear evidence that treating depressed patients with SSRIs increases or decreases risk of suicidality (suicidal ideation, preparatory act, attempt, or death). However, there may be an age-specific effect of antidepressants upon suicidality. Antidepressants in general may raise the risk of suicidality in patients age 18 to 24 years, have no effect upon patients aged 25 to 30 years, and may lower the risk in patients 31 years and older. It is also important to note that untreated depression may lead to suicidality. Paxil is indicated in the treatment of obsessive compulsive disorder. A decrease in bone mineral densities has been associated with the use of antidepressants and should be monitored during long-term therapy, but it is not necessary as a baseline. Question: Levonorgestrel (Plan B) for women who do not desire pregnancy: is prescription only. should be taken within 7 days of unprotected sex. is 99% effective against pregnancy. inhibits fertilization or implantation of fertilized egg. Correct Explanation: Levonorgestrel (Plan B) can be obtained without a prescription. Women who do not desire pregnancy should take Plan B within 72 hours of unprotected intercourse. It prevents pregnancy in an estimated 85% of women who would have otherwise become pregnant. It works by inhibiting or delaying ovulation and may inhibit fertilization or implantation of a fertilized egg. Question: A 53-year-old woman with an intact uterus has been receiving monophasic ethinyl estradiol for the treatment of perimenopausal symptoms. Which one of the following statements is true? Monophasic ethinyl estradiol is the recommended treatment for perimenopausal symptoms. Monophasic ethinyl estradiol may increase the risk of cervical cancer. Progesterone should be added to decrease endometrial hyperplasia risk. Correct The use of oral contraceptives is contraindicated in this patient. Explanation: Estrogen therapy causes the lining of the uterus to grow and can increase the risk for uterine cancer. Estrogen plus progesterone is recommended if the patient has an intact uterus, to protect the uterus from endometrial hyperplasia. Oral contraceptives may be used based on individual therapy and risk factors. Question: The first-line treatment for mixed somatic and behavior symptoms related to severe premenstrual syndrome (PMS) when pregnancy is desired is: metformin (Glucophage). spironolactone (Aldactone). fluoxetine hydrochloride (Sarafem). Correct ibuprofen (Motrin). Explanation: Selective serotonin reuptake inhibitors (SSRIs; i.e. fluoxetine hydrochloride [Sarafem]) are the first-line treatment for severe PMS and premenstrual dysphoric disorder (PMDD) when pregnancy is desired. SSRIs inhibit reuptake of serotonin and address the neurotransmitter deficiency believed to underlie the pathogenesis of PMS or PMDD. Adverse effects include reduced libido, jitteriness, headache, dry mouth and sleep disorders. A low starting dose is recommended. Try a different SSRI if the first one fails after three or more menstrual cycles. Prostaglandin inhibitors (i.e. ibuprofen [Motrin]) are indicated for the relief of somatic symptoms. Question: Levonorgestrel, the active ingredient in Plan B for undesired pregnancy, is also found in: Nexplanon implant. Mirena intrauterine device. Correct ParaGard intrauterine device. Depo-Provera. Explanation: Levonorgestrel, the active ingredient in Plan B, is also found in the Mirena intrauterine device. The active ingredient in Nexplanon is etonogestrel. The active ingredient in Depo-Provera is medroxyprogesterone acetate. Nexplanon, Mirena and Depo-Provera are all progestin-only devices. ParaGard intrauterine device is hormone-free, and it may be inserted for emergency contraception. Question: Progestin-only contraceptives are contraindicated in women: with moderate hypertension. who have a personal history of stroke. with pulmonary hypertension. Correct who are lactating. Explanation: Progestin-only contraceptives are absolutely contraindicated in women with known or suspected breast cancer, medical conditions that may be worsened by fluid retention (e.g., CHF, mitral stenosis, pulmonary hypertension), undiagnosed gynecological bleeding and liver disease. Progestin-only contraceptives do not alter the quality or quantity of breast milk in lactating women. Question: When initiating progestin-only contraceptives, women should be advised to: take with food anytime of the day. resume with the next dose, if one dose is missed. immediately report irregular uterine bleeding. use a backup method of contraception for the first month. Correct Explanation: Women taking progestin-only contraceptives should be advised to use a backup method of contraception for 1 month following initiation. It should be taken at the same time each day. If a pill is missed (for >3 hours), take it as soon as possible and use a back-up method for the remainder of the pill pack. Most women will experience irregular menstrual bleeding with spotting, breakthrough bleeding, prolonged cycles, and/or menorrhea. Patients should be advised that this is expected, especially during the first 3 months of progestin-only therapy. Question: Intrauterine devices should NOT be implanted in women: until they are at least 2 weeks postpartum. who have had a sexually transmitted infection in the past 3 months. Correct who have recurrent bladder infections. with a history of toxic shock syndrome. Explanation: Intrauterine devices should not be implanted in women who are pregnant; less than 4 weeks postpartum; have had a sexually transmitted infection in the past 3 months; are immediately post-septic abortion; have unexplained vaginal bleeding; have cervical, ovarian or endometrial cancer; have uterine fibroids distorting the uterine cavity; or have a current infection of cervix. Question: Levonorgestrel (Plan B), an emergency contraceptive, is absolutely contraindicated: in the presence of psychiatric illness. in the presence of known or suspected pregnancy. Correct in a woman who is breastfeeding. in women with intrauterine fibroids. Explanation: Levonorgestrel (Plan B) is absolutely contraindicated and should not be taken if a woman is already pregnant. It will not abort the pregnancy. Plan B works by inhibiting or delaying ovulation and may inhibit fertilization or implantation of a fertilized egg. It prevents pregnancy in an estimated 85% of women who would have otherwise become pregnant after unprotected sex. Levonorgestrel is a progestin-only emergency contraceptive and is safe for use while breastfeeding. Question: The brand name for spironolactone, used in the treatment of fibrocystic breast disease, is: Dyazide. Aldactone. Correct Aldomet. Sprintec. Explanation: The brand name for spironolactone is Aldactone. Spironolactone (Aldactone) is an aldosterone receptor antagonist. The generic name for Dyazide is triamterene/hydrochlorothiazide; Aldomet is methyldopa; and Sprintec is norgestimate/ethinyl estradiol. Question: The generic name of Diflucan is: fluoxetine. fluconazole. metronidazole. ketoconazole. Explanation: The generic name of Diflucan is fluconazole. Diflucan is an antifungal used in the treatment of candidiasis. The brand name for fluoxetine is Prozac (a selective serotonin reuptake inhibitor); metronidazole is Flagyl (a nitroimidazole antibiotic). Ketoconazole has no brand monographs and is classified as an antifungal. Question: An oral contraceptive known as the "mini-pill" contains: estrogen only. progesterone only. equal parts estrogen and progesterone. a higher dose of progesterone than estrogen. Explanation: Progestin-only oral contraceptives are sometimes referred to as the "mini-pill" or "progestin-only pill" (POPs). Progestin-only contraception is an option for women in whom an estrogen-containing contraceptive is either contraindicated or causes additional health concerns. There is only one progestin-only contraceptive pill in the U.S.: norethindrone (Micronor, Nor-QD). There are also progestin injections (i.e. depomedroxyprogesterone acetate [DepoProvera]); progestin implants (i.e. etonogestrel [Nexplanon]); and intrauterine progestin (i.e. levonorgestrel [Mirena]). Question: Levonorgestrel (Mirena) intrauterine device to prevent pregnancy should be changed every: 3 years. 5 years. Correct 7 years. 10 years. Explanation: Mirena should be changed every 5 years. The levonorgestrel in Mirena intrauterine devices causes thickening of the cervical mucus and thinning of the endometrium. Other hypotheses for the mechanism of action of Mirena includes increased motility in the fallopian tubes (moving ovum through rapidly) and inflammatory effects on the endometrium interfering with sperm survival, motility and/or capacitation. [Show More]
Last updated: 2 years ago
Preview 1 out of 31 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$10.50
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
May 15, 2021
Number of pages
31
Written in
Additional information
This document has been written for:
Uploaded
May 15, 2021
Downloads
0
Views
107



 Questions and Answers 100% VERIFIED.png)
 Questions and Answers 100% correct Solutions.png)






.png)

 Women’s Health Prescription (101 Questions) – South University Savannah.png)
 - South University.png)




