*NURSING > EXAM > NR 509 Advanced physical assessment quiz 3 (2020) – Chamberlain College of Nursing | NR 509 Advanc (All)
NR 509 Advanced physical assessment quiz 3 (2020) – Chamberlain College of Nursing | NR 509 Advanced physical assessment quiz 3 (2020) – Chamberlain College of Nursing
Document Content and Description Below
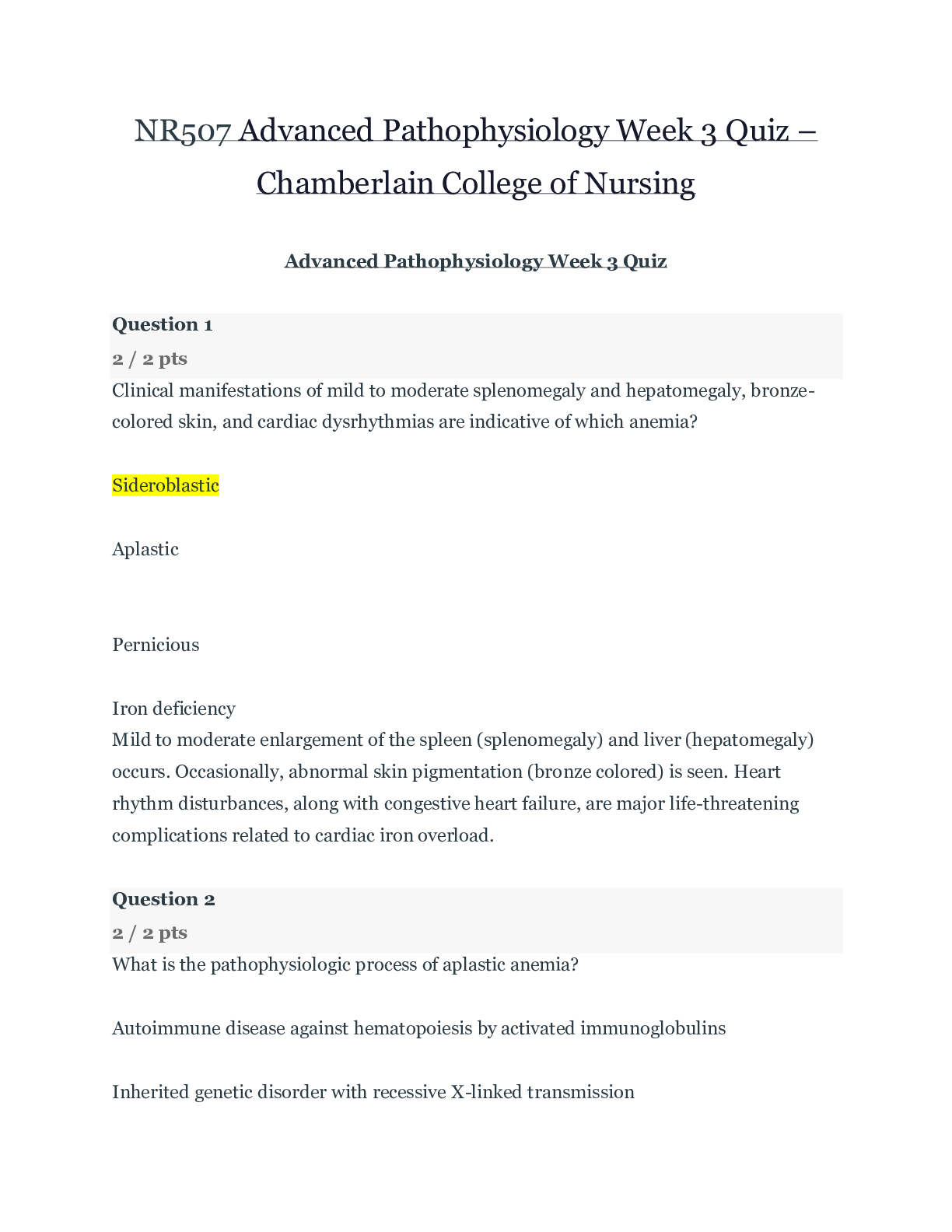
NR507 Advanced Pathophysiology Week 3 Quiz – Chamberlain College of Nursing Advanced Pathophysiology Week 3 Quiz Question 1 2 / 2 pts Clinical manifestations of mild to moderate splenomega... ly and hepatomegaly, bronze-colored skin, and cardiac dysrhythmias are indicative of which anemia? Sideroblastic Aplastic You Answered Pernicious Iron deficiency Mild to moderate enlargement of the spleen (splenomegaly) and liver (hepatomegaly) occurs. Occasionally, abnormal skin pigmentation (bronze colored) is seen. Heart rhythm disturbances, along with congestive heart failure, are major life-threatening complications related to cardiac iron overload. Question 2 2 / 2 pts What is the pathophysiologic process of aplastic anemia? Autoimmune disease against hematopoiesis by activated immunoglobulins Inherited genetic disorder with recessive X-linked transmission Malignancy of the bone marrow in which unregulated proliferation of erythrocytes crowd out other blood cells Correct! Autoimmune disease against hematopoiesis by activated cytotoxic T cells Most cases of AA result from an autoimmune disease directed against hematopoietic stem cells. Cytotoxic T cells (Tc cells) appear to be the main culprits. Question 3 2 / 2 pts Pernicious anemia generally requires continued therapy lasting 6 to 8 weeks. Correct! the rest of one’s life. until the iron level is normal. 8 to 12 months. PA cannot be cured, so maintenance therapy is lifelong. Question 4 2 / 2 pts Symptoms of polycythemia vera are mainly the result of destruction of erythrocytes. Correct! increased blood viscosity. neurologic involvement. a decreased erythrocyte count. As the disease progresses many of the symptoms are related to the increased blood cellularity and viscosity. Question 5 2 / 2 pts The body compensates for anemia by capillary vasoconstriction. kidneys release more erythropoietin. hemoglobin holds on to oxygen more firmly. Correct! increasing rate and depth of breathing. Tissue hypoxia creates additional demands and compensatory actions on the pulmonary and hematologic systems. The rate and depth of breathing increase in an attempt to increase the availability of oxygen. Question 6 2 / 2 pts In hemolytic anemia, jaundice occurs only when the patient has elevations in aspartate transaminase (AST) and alanine transaminase (ALT). Correct! heme destruction exceeds the liver’s ability to conjugate and excrete bilirubin. erythrocytes are destroyed in the spleen. the erythrocytes are coated with an immunoglobulin. Jaundice (icterus) is present when heme destruction exceeds the liver’s ability to conjugate and excrete bilirubin. Question 7 2 / 2 pts Which of the following is a description consistent with acute lymphocytic leukemia (ALL)? It is a progressive neoplasm defined by the presence of greater than 30% lymphoblasts in the bone marrow or blood. The translocation of genetic material from genes 9 and 22 create an abnormal, fused gene identified as BCR-ABL. You Answered The bone marrow and peripheral blood are characterized by leukocytosis and a predominance of blast cells. As the immature blasts increase, they replace normal myelocytic cells, megakaryocytes, and erythrocytes. There is failure of B cells to mature into plasma cells that synthesize immunoglobulins. ALL is a progressive neoplasm defined by the presence of greater than 30% lymphoblasts in the bone marrow or blood. Question 8 2 / 2 pts What change is seen in leukocytes during an allergic disorder (type I) often caused by asthma, hay fever, and drug reactions? Correct! Eosinophilia Monocytosis Neutrophilia Basophilia Allergic disorders (type I hypersensitivity) associated with asthma, hay fever, and drug reactions, as well as parasitic infections (particularly with metazoal parasites) are often cited as causes. Question 9 2 / 2 pts Heparin-induced thrombocytopenia (HIT) is described as a(n) Correct! IgG immune-mediated adverse drug reaction that reduces circulating platelets. IgE-mediated allergic drug reaction that reduces circulating platelets. hematologic reaction to heparin in which the bone marrow is unable to produce sufficient platelets to meet the body’s needs. cell-mediated drug reaction in which macrophages process the heparin and platelet complexes that are then destroyed by activated cytotoxic T cells. Heparin is a common cause of drug-induced thrombocytopenia. HIT is an immune-mediated, adverse drug reaction caused by IgG antibodies that leads to increased platelet consumption and a decrease in platelet counts. Question 10 2 / 2 pts Local signs and symptoms of Hodgkin disease–related lymphadenopathy are a result of ischemia and pressure. Correct! pressure and obstruction. obstruction and pressure. inflammation and ischemia. Local symptoms caused by pressure and obstruction of the lymph nodes are the result of lymphadenopathy. Question 11 2 / 2 pts Erythroblastosis fetalis is defined as an autoimmune disease in immature nucleated cells that are released into the bloodstream. allergic disease in which maternal blood and fetal blood are antigenically incompatible. Correct! alloimmune disease in which maternal blood and fetal blood are antigenically incompatible. autosomal dominant hereditary disease. HDN is an alloimmune disease in which maternal blood and fetal blood are antigenically incompatible, causing the mother’s immune system to produce antibodies against fetal erythrocytes. Question 12 2 / 2 pts The type of anemia that occurs as a result of thalassemia is Correct! microcytic, hypochromic. macrocytic, normochromic. macrocytic, hyperchromic. microcytic, normochromic. The anemic manifestation of thalassemia is microcytic-hypochromic hemolytic anemia. Question 13 2 / 2 pts The sickle cell trait differs from sickle cell disease in that the child with sickle cell trait has a mild form of sickle cell disease that causes sickling during fever and infection, but not during acidosis or hypoxia, whereas the child with sickle cells disease develops sickling during each of these conditions. has a milder form of the disease that is characterized by vaso-occlusive crises and is believed to result from higher hemoglobin values and viscosity. has the mildest form of the disease with normal hemoglobin and hemoglobin F, which prevents sickling. Correct! inherited normal hemoglobin A from one parent and Hb S from the other parent, whereas the child with sickle cell disease has Hb S from both parents. Sickle cell–thalassemia disease and sickle cell–Hb C disease are heterozygous forms in which the child simultaneously inherits another type of abnormal hemoglobin from one parent. Sickle cell trait, in which the child inherits Hb S from one parent and normal Hb A from the other, is a heterozygous carrier state that rarely has clinical manifestations (Table 28-3). Question 14 2 / 2 pts Polycythemia occurs in a fetus because Correct! there is increased erythropoiesis in response to the hypoxic intrauterine environment. fetal hemoglobin has a greater affinity for oxygen due to DPG. the lungs of the fetus are undeveloped and unable to adequately diffuse oxygen to the pulmonary capillaries. the fetus has a different hemoglobin structure of two α- and two γ-chains rather than two α-and two β-chains. The hypoxic intrauterine environment stimulates erythropoietin production in the fetus. Question 15 2 / 2 pts In a full-term infant, the normal erythrocyte life span is _____ days, whereas the adult is _____ days. 120 to 130; 150 Correct! 60 to 80; 120 90 to 110; 140 30 to 50; 80 In full-term infants, normal erythrocyte life span is 60 to 80 days; in premature infants it may be as short as 20 to 30 days; and in children and adolescents, it is the same as that in adults—120 days. Question 16 2 / 2 pts Hemolytic disease of the newborn can occur if the mother is Correct! Rh-negative and the fetus is Rh-positive. type A blood and the fetus has type O. type AB blood and the fetus has type B. Rh-positive and the fetus is Rh-negative. Maternal-fetal incompatibility exists if mother and fetus differ in ABO blood type or if the fetus is Rh-positive and the mother is Rh-negative. Question 17 2 / 2 pts Which of the following is a clinical manifestation of aortic stenosis? Peripheral edema Angina Bounding pulses You Answered Jugular vein distention The classic manifestations of aortic stenosis are angina, syncope, and heart failure. Question 18 2 / 2 pts The pulsus paradoxus that occurs as a result of pericardial effusion is significant because it reflects the impairment of the blood ejected from the left atria and reduction of blood volume in the left ventricle. diastolic filling pressures of the right ventricle and reduction of blood volume in both ventricles. Correct! diastolic filling pressures of the left ventricle and reduction of blood volume in all four heart chambers. blood ejected from the right atria and reduction of blood volume in the right ventricle. Pulsus paradoxus means that the arterial blood pressure during expiration exceeds arterial pressure during inspiration by more than 10 mmHg. This clinical finding reflects impairment of diastolic filling of the left ventricle plus reduction of blood volume within all four cardiac chambers. Question 19 2 / 2 pts The risk of developing coronary artery disease is increased up to threefold by high alcohol consumption. obesity. diabetes mellitus. Correct! hypertension. Hypertension is responsible for a two- to threefold increased risk of atherosclerotic cardiovascular disease. Question 20 2 / 2 pts What is the primary mechanism of atherogenesis? The release of the inflammatory cytokines interferon-beta (IFN-β), interleukin-6 (IL-6), and granulocyte colony-stimulating factor (G-CSF) The release of the inflammatory cytokines tumor necrosis factor-alpha (TNF-α), interferon-gamma (IFN-γ), and interleukin-1 (IL-1) Correct! The release of toxic oxygen radicals that oxidize low-density lipoproteins (LDLs) The release of the growth factor granulocyte-macrophage colony-stimulating factor (GM-CSF) The oxidation of LDL is an important step in atherogenesis. Inflammation with oxidative stress and activation of macrophages is the primary mechanism. Question 21 2 / 2 pts Which heart defect produces a systolic ejection murmur at the right upper sternal border that transmits to the neck and left lower sternal border with an occasional ejection click? Hypoplastic left heart syndrome Pulmonic stenosis Correct! Aortic stenosis Coarctation of the aorta A systolic ejection murmur at the right upper sternal border that transmits to the neck and left lower sternal border is produced by blood flow through the stenotic area. An ejection click may be heard with valvular arterial stenosis. Question 22 2 / 2 pts The foramen ovale is covered by a flap that creates a check valve allowing blood to flow unidirectionally from the _____ to the _____. right ventricle; left ventricle Correct! right atrium; left atrium left atrium; left ventricle right atrium; right ventricle The nonfused septum secundum and ostium secundum result in the formation of a flapped orifice known as the foramen ovale, which allows the right (atrium)-to-left (atrium) shunting necessary for fetal circulation. Question 23 2 / 2 pts When does most cardiovascular development occur? By the 28th day of gestation Correct! Between the fourth and seventh weeks of gestation Between the eighth and 10th weeks of gestation Between the 12th and 14th weeks of gestation Cardiogenesis begins at approximately 3 weeks of gestation; however, most cardiovascular development occurs between the fourth and seventh weeks. Question 24 2 / 2 pts What is the most important clinical manifestation of aortic coarctation in the neonate? Pulmonary hypertension Correct! Congestive heart failure (CHF) Cerebral hypertension Cor pulmonale The newborn usually presents with CHF symptoms. Once the ductus closes, these infants deteriorate rapidly from the development of hypotension, acidosis, and shock. Question 25 2 / 2 pts Which congenital heart defects occur in trisomy 13, trisomy 18, and Down syndrome? Atrial septal defect and dextrocardia Tetralogy of Fallot and persistent truncus arteriosus Correct! Ventricular septal defect and patent ductus arteriosus Coarctation of the aorta and pulmonary stenosis Congenital heart defects that are related to dysfunction of trisomy 13, trisomy 18, and Down syndrome include ventricular septal defect and patient ductus arteriosus (see Table 31-2). [Show More]
Last updated: 2 years ago
Preview 1 out of 14 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$12.50
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Aug 16, 2020
Number of pages
14
Written in
Additional information
This document has been written for:
Uploaded
Aug 16, 2020
Downloads
0
Views
87







 – University of the People.png)