*NURSING > STUDY GUIDE > NR507 Study Guide Quiz week 7 (All)
NR507 Study Guide Quiz week 7
Document Content and Description Below
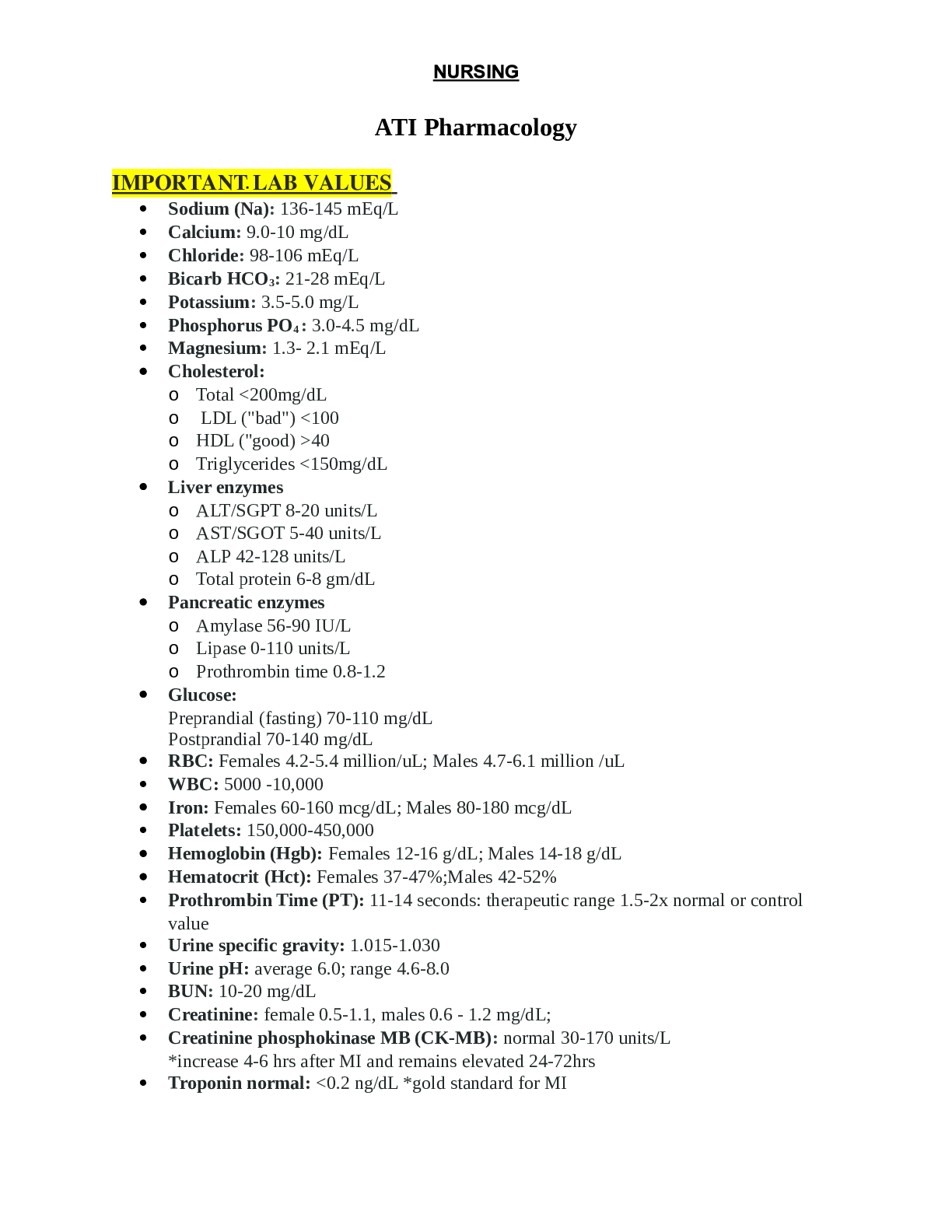
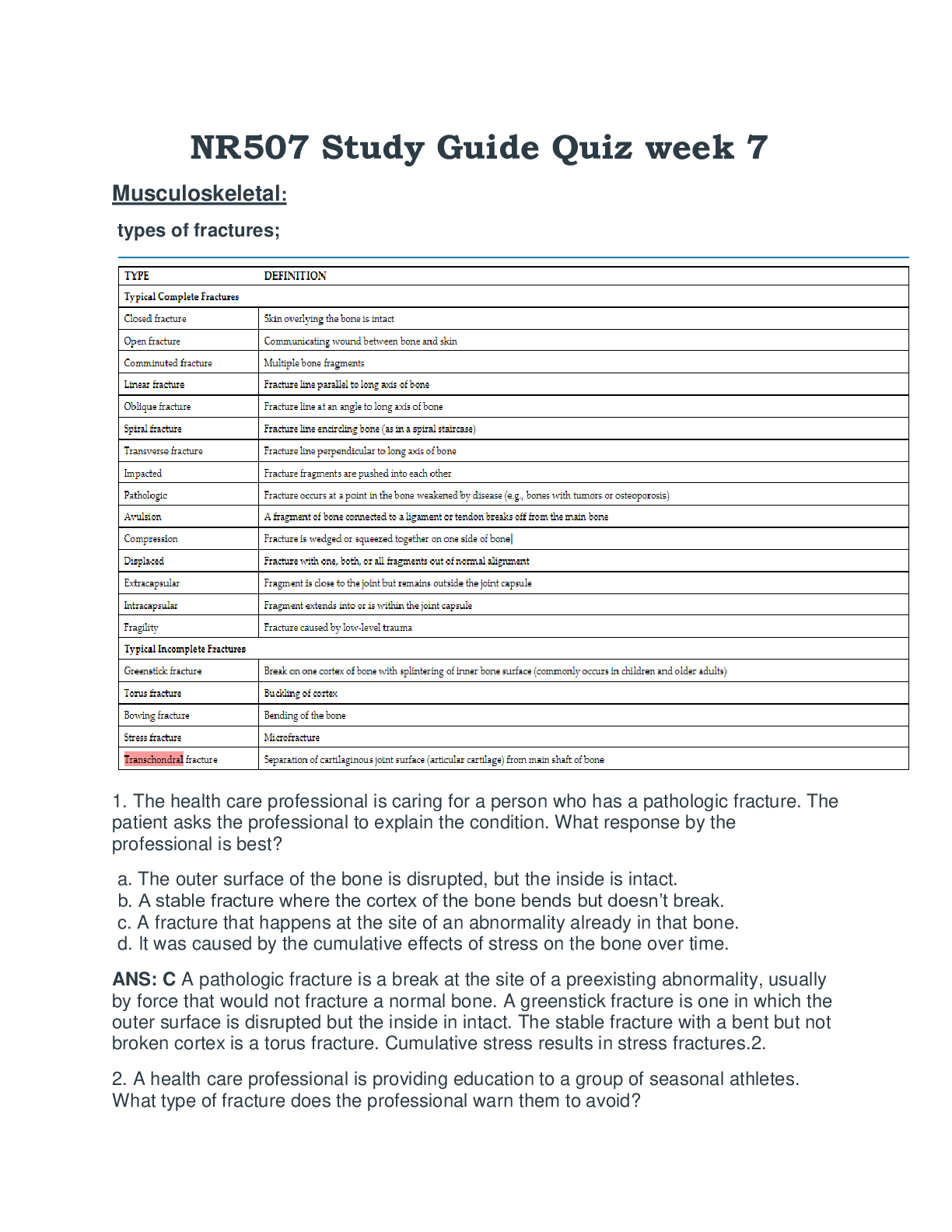
NR507 Study Guide Quiz week 7NR507 Study Guide Quiz week 7 Musculoskeletal: types of fractures; 1. The health care professional is caring for a person who has a pathologic fracture. The patient as... ks the professional to explain the condition. What response by the professional is best? a. The outer surface of the bone is disrupted, but the inside is intact. b. A stable fracture where the cortex of the bone bends but doesn’t break. c. A fracture that happens at the site of an abnormality already in that bone. d. It was caused by the cumulative effects of stress on the bone over time. ANS: C A pathologic fracture is a break at the site of a preexisting abnormality, usually by force that would not fracture a normal bone. A greenstick fracture is one in which the outer surface is disrupted but the inside in intact. The stable fracture with a bent but not broken cortex is a torus fracture. Cumulative stress results in stress fractures.2. 2. A health care professional is providing education to a group of seasonal athletes. What type of fracture does the professional warn them to avoid?a. Stress b. Greenstick c. Insufficiency d. Pathologic ANS: A A stress fracture occurs in normal or abnormal bone that is subjected to repeated stress, such as repetitive and strenuous activities that occur during athletics. A greenstick fracture is one in which the outer surface of the bone is disrupted but the interior is intact. Insufficiency fractures are seen in osteoporosis and osteomalacia. A pathologic fracture is one that occurs from force that would not usually break a bone. There is usually an underlying lesion or abnormality at the site of the fracture. 3. Improper reduction or immobilization of a fractured femur can result in which outcome after cast removal? a. The muscles around the fracture site are weak. b. The fracture requires 6 to 8 weeks of physical therapy. c. The skin under the cast is dry and flaky. d. The bone is not straight. ANS: D Improper reduction or immobilization of a fractured bone may result in nonunion, delayed union, or malunion. Malunion is the healing of a bone in a nonanatomic position that could result in the bone not being straight. The other options are normal occurrences. 4. What is the tear in a ligament referred to as? a. Fracture b. Strain c. Disunion d. Sprain ANS: D Ligament tears are commonly known as sprains. A fracture is a break in a bone. A strain is an injury to a tendon or muscle. Disunion is when bones do not heal together properly after a fracture. 5. Which type of osteoporosis would a person develop after having the left leg in a cast for 8 weeks to treat fracture of the tibia and fibula? a. Iatrogenic b. Regional c. Idiopathic d. Osteoblastic ANS: B Classic regional osteoporosis is associated with disuse or immobilization of a limb because of fractures, motor paralysis, or bone or joint inflammation. 6. A patient is brought to the Emergency Department after being found by neighbors. The patient says she has been lying on the floor in the house for 3 days. What action by the health care professional is best?a. Order a serum creatine kinase (CK) level b. Obtain an x-ray of the patient’s hips c. Arrange for the patient to have a DXA scan d. Perform the Fracture Risk Assessment ANS: A Chapter 45 - Alterations of Musculoskeletal Function 440 Pathophysiology The Biologic Basis for Disease in Adults and Children 8th Edition 97803235834 This patient is at high risk of having rhabdomyolysis. The best diagnostic test for this disorder is a serum creatine kinase level. The patient may well have a hip fracture, but other bones may be broken as well and the patient may well have rhabdomyolysis. A DXA scan and Fracture Risk Assessment are useful tools for osteoporosis. 7. The health care professional teaches a group of seniors that the most common clinical manifestation of osteoporosis is which of these? a. Bone deformity b. Bone pain c. Pathologic fracture d. Muscle strain ANS: A The most common clinical manifestation of osteoporosis is bone deformity. Pain does occur, but is often associated with fractures, which can be pathological in nature (occurring under normal stress). Muscle strain is not a component of osteoporosis. osteoporosis (types of fracture that is prevalent; screening test for osteoporosis); Hip fractures, vertebral fractures (most common osteoporotic fracture) 1. A health care professional is providing education to a group of seasonal athletes. What type of fracture does the professional warn them to avoid? a. Stress b. Greenstick c. Insufficiency d. Pathologic ANS: A A stress fracture occurs in normal or abnormal bone that is subjected to repeated stress, such as repetitive and strenuous activities that occur during athletics. A greenstick fracture is one in which the outer surface of the bone is disrupted but the interior is intact. Insufficiency fractures are seen in osteoporosis and osteomalacia. A pathologic fracture is one that occurs from force that would not usually break a bone. There is usually an underlying lesion or abnormality at the site of the fracture. 2. By the time osteoporosis is visible on an x-ray examination, up to what percent of bone has been lost? a. 30% b. 40% c. 50% d. 60%ANS: A Generally, osteoporosis is radiographically detected as increased radiolucency of bone. By the time abnormalities are detected by x-ray examination, as much as 25% to 30% of bone tissue may have been lost. 3. A patient has a bone density T score of -2.8. What diagnosis does the health care professional educate the patient on? a. Osteoplasia b. Osteoporosis c. Osteopenia d. Osteomalacia ANS: B Bone density is based on the number of standard deviations that differ from the mean bone mineral density of a young-adult reference population (a T-score). A normal T score is >-1.0. A score between -1.0 and -2.5 signifies osteopenia. A score <-2.5 indicates osteoporosis. 4. Which type of osteoporosis would a person develop after having the left leg in a cast for 8 weeks to treat fracture of the tibia and fibula? a. Iatrogenic b. Regional c. Idiopathic d. Osteoblastic ANS: B Classic regional osteoporosis is associated with disuse or immobilization of a limb because of fractures, motor paralysis, or bone or joint inflammation. 5. In osteoporosis, the receptor activator of nuclear factor κB (RANK) activates what? a. Osteoclast apoptosis b. Osteoblast survival c. Osteoprotegerin d. Osteoclast survival ANS: D RANKL activates the receptor RANK, which is expressed on osteoclasts and their precursors and suppresses apoptosis, which leads to activation and the prolongation of osteoclast survival. Apoptosis, osteoblast survival, and osteoprotegerin are not affected. 6. The health care professional teaches a group of seniors that the most common clinical manifestation of osteoporosis is which of these? a. Bone deformity b. Bone pain c. Pathologic fracture d. Muscle strain ANS: A The most common clinical manifestation of osteoporosis is bone deformity. Pain does occur, but is often associated with fractures, which can be pathological innature (occurring under normal stress). Muscle strain is not a component of osteoporosis. transchondral fractures; Separation of cartilaginous joint surface (articular cartilage) from main shaft of bone gout (cause of pain); 1. A person in the health care clinic has gout. In order to prevent a common complication, what self-care measure does the health care professional teach the person about? A. Drinking plenty of water b. Splinting affected joints c. Eating more protein d. Avoiding hot weather ANS: A Renal stones are 1000 times more prevalent in individuals with primary gout than they are in the general population. One self-care measure to prevent stones and to prevent uric acid remaining in the kidney is a large fluid intake. Splinting joints would be difficult in gout; 50% of the time the affected joint is in the big toe. The other 50% involve the heel, ankle, and instep of the foot; knee; wrist; or elbow. More protein is not related to preventing complications. Avoiding hot weather is also not a preventative measure for complications of gout. 2. What causes the crystallization within the synovial fluid of the joint affected by gouty arthritis? a. Reduced excretion of purines b. Overproduction of uric acid c. Increase in the glycosaminoglycan levels d. Overproduction of proteoglycans ANS: B When the uric acid reaches a certain concentration in fluids, it crystallizes, forming insoluble precipitates that are deposited in connective tissues throughout the body. Crystallization in synovial fluid causes acute, painful inflammation of the joint, a condition known as gouty arthritis. This selection is the only option that accurately identifies the cause of crystallization in synovial fluid associated with gouty arthritis. 3. The pathophysiologic presentation of gout is closely linked to the metabolism of which chemical? a. Purine b. Pyrimidine c. Vitamin E d. Amino acid ANS: A The pathophysiologic presentation of gout is closely linked only to purine metabolism (or cellular metabolism of purines) and kidney function. 4. A patient in the clinic has calcium crystals that are associated with chronic gout. How does the professional document this finding? a. Stonesb. Spurs c. Tophi d. Nodes ANS: C With time, crystal deposition in subcutaneous tissues causes the formation of small white nodules, or tophi, that are visible through the skin. Crystal aggregates deposited in the kidneys can form urate renal stones and lead to renal failure. Stones are precipitates that accumulate in liquid, such as kidney stones. Spurs are outgrowths of bone. Nodes are a central connecting point for some bodily structures. pathological features of degenerative joint disease; osteomalacia; epicondylopathy; hip fractures secondary to osteoporosis; Diagnosing rhabdomyolysis -Rapid breakdown of muscle that causes release of myoglobin into blood stream. S/S: muscle pain, weakness, dark urine 1. A student asks for an explanation of rhabdomyolysis. What response by the professor is best? a. Paralysis of skeletal muscles, resulting from an impaired nerve supply b. Smooth muscle degeneration, resulting from ischemia c. Lysis of skeletal muscle cells through the initiation of the complement cascade d. Release of myoglobin from damaged striated muscle cells ANS: D Rhabdomyolysis involves the release of myoglobin when muscle cells are damaged. It is not due to muscle paralysis, muscle degeneration, or from the complement cascade. 2. A patient is brought to the Emergency Department after being found by neighbors. The patient says she has been lying on the floor in the house for 3 days. What action by the health care professional is best? a. Order a serum creatine kinase (CK) level b. Obtain an x-ray of the patient’s hips c. Arrange for the patient to have a DXA scan d. Perform the Fracture Risk Assessment ANS: A Chapter 45 - Alterations of Musculoskeletal Function 440 Pathophysiology The Biologic Basis for Disease in Adults and Children 8th Edition 97803235834 This patient is at high risk of having rhabdomyolysis. The best diagnostic test for this disorder is a serum creatine kinase level. The patient may well have a hip fracture, but other bones may be broken as well and the patient may well have rhabdomyolysis. A DXA scan and Fracture Risk Assessment are useful tools for osteoporosis.3. A patient reports joint stiffness with movement and joint pain in weightbearing joints that is usually relieved by rest. What treatment option does the health care professional discuss with the patient? a. Ways to decrease serum uric acid b. Administration of oral methotrexate c. Exercise and weight reduction d. Rapid intravenous hydration ANS: C Pain and stiffness in one or more joints, usually weightbearing or load-bearing joints, are the first symptoms of osteoarthritis. The joint pain is usually relieved by rest. The standard treatment approach begins with weigh reduction and an exercise regime. Decreasing serum uric acid would be beneficial in gout. Oral methotrexate is one drug used in rheumatoid arthritis. Rapid intravenous hydrations would be appropriate for rhabdomyolysis. Gastrointestinal: reflux esophagitis; 1. A patient asks the healthcare professional to describe the cause of gastroesophageal reflux disease (GERD). What response by the professional is best? a. Excessive production of hydrochloric acid b. Zone of low pressure of the lower esophageal sphincter c. Presence of Helicobacter pylori in the esophagus d. Reverse muscular peristalsis of the esophagus ANS: B Normally, the resting tone of the lower esophageal sphincter maintains a zone of high pressure that prevents gastroesophageal reflux. In individuals who develop reflux esophagitis, this pressure tends to be lower than normal from either transient relaxation or a weakness of the sphincter. Excessive hydrochloric acid and H. pylori can lead to gastritis. Reverse peristalsis is associated with vomiting. 2. A patient has been diagnosed with reflux esophagitis (GERD). What instruction by the healthcare professional is most appropriate? a. Exercise soon after eating to increase gastric emptying. b. Try these proton-pump inhibitors for 2 weeks. c. You need to schedule an upper GI endoscopy soon. d. Over-the-counter antiemetics work well for this condition. ANS: BAbnormalities in lower esophageal sphincter function, esophageal motility, and gastric motility or emptying can cause GERD. Delayed gastric emptying contributes to reflux esophagitis by (1) lengthening the period during which reflux is possible and (2) increasing the acid content of chyme. A treatment of choice for this condition is protonpump inhibitors, so the healthcare professional would educate the patient on taking these medications. Increasing gastric motility may help GERD, but exercising soon after eating may promote vomiting and other GI distress. If GERD cannot be controlled, an endoscopy may be needed to refine the diagnosis and assess for cancerous changes. Antiemetics will not help in this condition. 3. A class of students has learned about contributing factors to duodenal ulcers. What statement indicates to the professor that the students need a review? a. Bleeding from duodenal ulcers causes hematemesis or melena. b. Gastric emptying is slowed, causing greater exposure of the mucosa to acid. c. The characteristic pain begins 30 min to 2 hours after eating d. Duodenal ulcers occur with greater frequency than other types of peptic ulcers. ANS: B Duodenal ulcers can be associated with altered mucosal defenses, rapid gastric emptying, elevated serum gastrin levels, or acid production stimulated by smoking. Slowed gastric emptying contributes to reflux esophagitis. The students making this statement need a review of the information. characteristics of gastric ulcers; Increased serum gastrin, located in upper abdomen, intermittent pain, pain-antacidrelief pattern 1. A peptic ulcer may occur in all of these areas except which? a. Stomach b. Duodenum c. Jejunum d. Esophagus ANS: C A peptic ulcer is a break, or ulceration, in the protective mucosal lining of the lower esophagus, stomach, or duodenum. This type of ulcer is not associated with the jejunum. 2. A class of students has learned about contributing factors to duodenal ulcers. What statement indicates to the professor that the students need a review? a. Bleeding from duodenal ulcers causes hematemesis or melena. b. Gastric emptying is slowed, causing greater exposure of the mucosa to acid. c. The characteristic pain begins 30 min to 2 hours after eating d. Duodenal ulcers occur with greater frequency than other types of peptic ulcers. ANS: B Duodenal ulcers can be associated with altered mucosal defenses, rapid gastric emptying, elevated serum gastrin levels, or acid production stimulated bysmoking. Slowed gastric emptying contributes to reflux esophagitis. The students making this statement need a review of the information. causes of elevated liver function tests; Increase biliary bulimia nervosa; A person has abnormally severe tooth decay and erosion of the tooth enamel. What problem should the health care professional assess the person for? a. Anorexia nervosa b. Binge eating c. Bulimia d. Refeeding syndrome ANS: C Chronic vomiting and exposure to gastric acids leads to loss of tooth enamel and decay. These are not signs of anorexia, binge eating, or refeeding syndrome. anorexia nervosa; 1. A health care professional is caring for a patient admitted to the hospital with severe anorexia. What action by the health care professional would be most important? a. Ensuring the patient is on a cardiac monitor b. Facilitating laboratory testing of electrolytes c. Arranging a psychiatry consultation d. Assessing the patient’s favorite foods ANS: A Patients with severe anorexia can have cardiac dysrhythmias, so this patient should be placed on a cardiac monitor as the priority. The other actions are appropriate; they just do not take priority. 2. A patient weighs 82 pounds and is hospitalized for anorexia. In order to prevent refeeding syndrome, how many calories should the person eat in the first two days? a. 400 b. 745 c. 936 d. 1200 ANS: B In order to prevent refeeding syndrome, feedings should start slowly at about 20 kcal/kg/day. This 82-pound person weighs 37.2727 kg, so that would be 745 calories a day. 3. A family is concerned that their most elderly member is not eating. What information about the anorexia of aging does the health care professional provide the family? (Select all that apply.) a. Usually there is a direct cause that can be treated successfully. b. Is not related to age-related changes and signifies illness c. Decreases in saliva and the sense of taste are contributing factors. d. Age-related loss of appetite is common finding. e. Social stimulation at meals might promote better eating habits.ANS: C, D, E Anorexia of aging has multiple causes that include normal age-related changes, physiologic alterations, and social/psychological factors. Decreases in saliva and the senses of smell and taste are contributory. Aging is marked by a decrease in orexigenic signals and an increase in anorexigenic signals, leading to decreased appetite. Social isolation has also been implicated in this phenomenon. interpretation of Hepatitis B vaccine serological markers (for example, results show HbsAb-what information would you provide the patient?) Endocrine: pathophysiology of Type 1 diabetes; classic signs of diabetes mellitus and their causes; kidney function in the patient with diabetes insipidus; 1. What is diabetes insipidus a result of? a. Antidiuretic hormone hyposecretion b. Antidiuretic hormone hypersecretion c. Insulin hyposecretion d. Insulin hypersecretion ANS: A Diabetes insipidus is a result of insufficient antidiuretic hormone (hyposecretion). It is not related to insulin secretion. 2. A patient who is diagnosed with a closed head injury has a urine output of 6 to 8 L/day. Electrolytes are within normal limits, but the antidiuretic hormone (ADH) level is low. Although the patient has had no intake for 4 hours, no change in the polyuria level has occurred. What treatment or diagnostic testing does the healthcare professional prepare the patient for? a. Administration of desmopressin b. Serum copeptin testing c. Insulin administration d. Renal angiogram ANS: A The stated symptoms are reflective of neurogenic diabetes insipidus (DI) which can be treated with desmopressin. Desmopressin will cause an increased ability to concentrate urine. Copeptin is a precursor of ADH and obtaining a serum level is useful in diagnosing dipsogenic DI. The patient does not need insulin or a renal angiogram. 3. Which laboratory value is consistent with diabetes insipidus (DI)?a. Low urine-specific gravity b. Low serum sodium c. Low urine protein d. High serum total protein ANS: A The basic criteria for diagnosing DI include a low urine-specific gravity while sodium levels are high. Protein levels are not considered. 4. A patient has nephrogenic diabetes insipidus (DI). What treatment does the healthcare professional anticipate for this patient? a. Exogenous ADH replacement b. Intranasal desmopressin c. Water and sodium restriction d. Loop diuretic administration ANS: A Nephrogenic DI is usually treated with administration of fluids, or intranasal (or oral) desmopressin. Neurogenic DI is treated with ADH replacement therapy. Water restriction would not be helpful. Thiazide (not loop) diuretics can improve moderate nephrogenic DI. chronic complications of diabetes mellitus; signs common to both type 1 and type 2 diabetes 1.A patient with several risk factors is concerned about developing type 2 diabetes. The healthcare professional advises the patient to lose weight, explaining that obesity is an important risk factor for type 2 diabetes mellitus because it causes what? a. Reduced insulin production by the pancreas b. Increased resistance to insulin in the cells c. Obstructed outflow of insulin from the pancreas d. Stimulation of glucose production by the liver ANS: B People with type 2 diabetes mellitus suffer from insulin resistance. Obesity causes this resistance so their cells have difficulty using insulin. Obesity does not leadto reduced insulin production, obstructed insulin outflow, or stimulation of glucose production. 2. A student asks the professor to differentiate Type 2 diabetes mellitus from Type 1. The professors’ response would be that Type 2 is best described as what? a. Resistance to insulin by insulin-sensitive tissues b. Need for lifelong insulin injections c. Increase of glucagon secretion from beta cells of the pancreas d. Presence of insulin autoantibodies that destroy beta cells in the pancreas ANS: A One of the basic pathophysiologic characteristics of type 2 diabetes is the development of insulin-resistant tissue cells. Type 1 diabetes always must be treated with insulin. Type 2 diabetes can be treated with insulin but there are other options. Pancreatic beta cells are destroyed in Type 1 diabetes. Increased glucagon is not secreted from pancreatic beta cells in Type 2 diabetes. 3. A person diagnosed with type 1 diabetes experienced an episode of hunger, lightheadedness, tachycardia, pallor, headache, and confusion. The healthcare professional teaches the person that what is the most probable cause of these symptoms? a. Hyperglycemia caused by incorrect insulin administration b. Dawn phenomenon from eating a snack before bedtime c. Hypoglycemia caused by increased exercise d. Somogyi effect from insulin sensitivity ANS: C The most likely cause of these symptoms is hypoglycemia, which is often caused by a lack of systemic glucose as a result of muscular activity or decreased food intake. Hyperglycemia is not characterized by these symptoms. The Dawn phenomenon is manifested by an early morning elevation in blood glucose. The Somogyi effect is distinguished by early morning (i.e., 4 AM) hypoglycemia followed by hyperglycemia upon arising 4. A chronic complication of diabetes mellitus is likely to result in microvascular complications in which areas? (Select all that apply.) a. Eyes b. Coronary arteries c. Renal system d. Peripheral vascular system e. Nerves ANS: A, C, E Of the options provided, the areas most often affected are the retina, kidneys, and nerves. Coronary artery disease and peripheral vascular disease are macrovascular complications. [Show More]
Last updated: 2 years ago
Preview 1 out of 12 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$5.50
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Mar 16, 2021
Number of pages
12
Written in
Additional information
This document has been written for:
Uploaded
Mar 16, 2021
Downloads
0
Views
66