*NURSING > STUDY GUIDE > NURS 624 N624 Fundamental Success Qs Exam 1 Practice Completed for 2022/2023 (All)
NURS 624 N624 Fundamental Success Qs Exam 1 Practice Completed for 2022/2023
Document Content and Description Below
NURS 624 N624 Fundamental Success Qs Exam 1 Practice TOPICS Clinical Decision making Nursing Process Medical Asepsis & Surgical Asepsis Evidence Based Practice Critical Thinking in Nursing Evidenc... e Vital Signs Med Administration Nursing Process Wound Healing Hygiene and Comfort Mobility PG 128 - 136 Communication PG 184 -194 The Nursing Process PG 219 - 233 Infection Control PG 234 - 248 Safety PG 249 - 271 Med Admin PG 297 - 312 Hygiene PG 313 - 332 Mobility PG 415 - 423 Pain, Comfort, Rest, and Sleep CHAPTER 3 COMMUNICATION 128 1. A nurse is collecting data from a client for an admission nursing history. Which question by the nurse is best to open the discussion? 1. “What brought you to the hospital?” Open-ended statement 2. “Would it help to discuss your feelings?” Yes or no 3. “Do you want to talk about your concerns?” Yes or no 4. “Would you like to talk about why you are here?” Yes or no 2. A nurse must conduct a focused interview to complete an admission history. Which interviewing technique should the nurse use?1. Probing 2. Clarification 3. Direct questions 4. Paraphrasing statements 3. Which statement about communication should the nurse consider to be accurate? 1. Verbal communication is essential for human relationships. 2. Hands are the most expressive part of the body. 3. Behavior clearly reflects feelings. 4. Communication is inevitable. All behavior has meaning 4. A client is extremely upset and mentions something about a workrelated issue that the nurse cannot understand. Which is the nurse’s best response? 1. “It’s natural to worry about your job.” 2. “Your job must be very important to you.” 3. “Calm down so that I can understand what you are saying.” 4. “I’m not quite sure I heard what you were saying about your work.” 5. Which is the purpose of the use of humor by a nurse when interacting with a client? 1. Diminish feelings of anger 2. Refocus the client’s attention 3. Maintain a balanced perspective 4. Delay dealing with the inevitable 6. A nurse is caring for a client who is blind in the left eye and visually impaired in the right eye. Which actions should the nurse employ to promote communication with this client? 1. Touch the client’s left arm before initiating a conversation. 2. Ensure that the door to the client’s room is on the client’s left side. 3. Close the window curtains and dim the lights before speaking with the client.4. Knock on the door and request permission to enter before approaching the client. 7. A client is admitted to the hospital with cirrhosis of the liver caused by long-term alcohol misuse. Which is the best response by the nurse when the client says, “I really don’t believe that my drinking a couple of beers a day has anything to do with my liver problem”? 1. “You find it hard to believe that beer can hurt the liver.” 2. “How long is it that you have been drinking several beers a day?” 3. “Each beer is equivalent to one shot of liquor, so it’s just as damaging to the liver as hard liquor.” 4. “Do you believe that beer is not harmful even though research shows that it is just as bad for you as hard liquor?” 8. Which is being communicated when the nurse leans forward during a client interview? 1. Aggression 2. Anxiety 3. Interest 4. Privacy 9. Which statement describes the following proverb? What you do speaks so loudly I cannot hear what you say. 1. Hearing ability is an important factor in communicating. 2. Nonverbal messages are often more meaningful than words. 3. Listening to what people say requires attention to what is being said. 4. When people talk too loudly, it is hard to understand what is being said. 10. A mother whose young daughter has died of leukemia is crying and is unable to talk about her feelings. Which is the best response by the nurse? 1. “Everyone will remember her because she was so cute. She was one of our favorites.”2. “As hard as this is, it is probably for the best because she was in a lot of pain.” 3. “She put up the good fight, but now she is out of pain and in heaven.” 4. “It must be hard to deal with such a precious loss.” 11. A young adult who had a leg amputated because of trauma says, “No one will ever choose to love a person with one leg.” Which is the best response by the nurse? 1. “You are a good-looking person, and you will have no trouble meeting someone who cares.” 2. “You may feel that way now, but you will feel differently as time passes.” 3. “Do you feel that no one will marry you because you have one leg?” Paraphrasing promotes communication 4. “How do you see your situation at this point?” 12. A nurse is changing a client’s dressing over an abdominal wound. Which level of space around the client is entered during the dressing change? 1. Public 2. Social 3. Intimate 4. Personal 1 ½ to 4 feet 13. Which stage of an interview establishes the relationship between the nurse and the client? 1. Preinteraction stage 2. Orientation stage 3. Examining stage 4. Working stage14. A client is exhibiting anxious behavior and states, “I just found out that I have cancer everywhere, and I don’t have very long to live. My life is over.” Which is the best response by the nurse? 1. “It might be good if your family were here right now. Shall I call them?” 2. “What might be the best way to approach this terrible news?” Client is in shock and disbelief mode of coping and will not be able to explore approaches to coping. Also, using the words “terrible news” may increase anxiety and hopelessness. 3. “That is so sad. You must feel like crying.” 4. “It sounds like you feel hopeless.” An example of reflective technique because the nurse incorporated the client’s feelings into the response. 15. Which interviewing skill is used when the nurse says, “You mentioned before that you are having a problem with your colostomy”? 1. Focusing Nurse selects one topic for further discussion from among several topics presented by the client. 2. Clarifying Not an example of clarifying which lets the client know that a message was unclear and seeks specific information to make the message clearer. 3. Paraphrasing 4. Acknowledging 16. A client says, “I am really nervous about having a spinal tap tomorrow.” Which is the best response by the nurse? 1. “I’ll ask the doctor for a little medication to help you relax.” This statement avoids the client’s feelings and fails to respond to the client’s need to talk about concerns. 2. “Clients who have had a spinal tap say it is not that uncomfortable.” This is a generalization and minimizes the client’s concern. 3. “It’s all right to be nervous, and I don’t remember anyone who wasn’t.” Recognizes the client’s feelings, gives the client permission to feel nervous and reassures client that one’s behavior is not unusual4. “Your physician is excellent and is very careful when spinal taps are done.” 17. A client with chest pain is being admitted to the emergency department. When asked about next of kin, the client states, “Don’t bother calling my daughter; she is always too busy.” Which is the best response by the nurse? 1. “Your daughter might be upset if you don’t call.” False assumption 2. “What does your daughter do that makes her so busy?” 3. “Is there someone else besides your daughter that I can call?” This lets the client know that the message has been heard and moves forward to meet the need to notify a different significant other of the client’s situation. 4. “I think that your daughter would want to know that you are sick.” False reassurance 18. Which is the nurse doing when using the interviewing technique of attentive listening? 1. Identifying the client’s concerns and exploring them with “why” questions Client may become defensive 2. Determining the content and feeling of the client’s message Attentive listening is the active use of all the senses to comprehend and appreciate the client’s verbal and nonverbal thoughts and feelings 3. Employing silence to encourage the client to talk 4. Using verbal skills to obtain information This is talking not listening 19. A client who has had postoperative complications appears upset and agitated yet withdrawn. Which is the most appropriate statement by the nurse? 1. “You seem distressed. Tell me why you are upset.” First part of statement is therapeutic, but the second part with “why” can be taken as accusation 2. “You’ve been having a pretty rough time recovering since surgery.” Therapeutic example of interviewing skill of an openended statement. It demonstrates that the nurse recognizeswhat the client is going through and the statement encourages the client’s expression of feelings. 3. “It’s not uncommon to have complications after the kind of surgery that you had.” 4. “I’m not sure that I know everything that has been happening. Tell me what has happened to you since surgery.” Nurse should already know what is happening 20. A nurse is admitting a client to the unit who was transferred from the emergency department. Which should the nurse do to facilitate communication? 1. Ensure that the client has an effective way to communicate with health-care team members. 2. Use interviewing techniques to control the direction of the client’s communication. 3. Minimize energy spent by the client on negative feelings and concerns. All feelings should be addressed 4. Refocus to the positive aspects of the client’s situation and prognosis. 21. A nurse is caring for a very confused client with a diagnosis of dementia of the Alzheimer’s type. Which should the nurse say when assisting the client to eat? 1. “Please eat your meat.” Simple words and sentences for confused clients 2. “It’s important that you eat.” Client may be confused about what “important” means 3. “What would you like to eat?” 4. “If you don’t eat, you can’t have dessert.” 22. A client states, “Do you think I could have cancer?” The nurse responds, “What did the doctor tell you?” Which interviewing approach did the nurse use? 1. Paraphrasing 2. Confrontation3. Reflective technique Reflective technique refers back to basic feelings underlying the client’s statement 4. Open-ended question 23. A nurse is developing a therapeutic relationship with a client with emotional needs. Which nursing intervention is essential during the working stage of the relationship? 1. Establish a formal or informal contract that addresses the client’s problems. Introductory (orientation) stage 2. Implement nursing actions that are designed to achieve expected client outcomes. 3. Develop rapport and trust so the client feels protected and an initial plan can be identified. Introductory (orientation) stage 4. Clearly identify the role of the nurse and establish the parameters of the professional relationship. Introductory (orientation) stage 24. A nurse uses reflective technique when communicating with an anxious client. On which does the nurse focus when using reflective technique in this situation? 1. Feelings Reflective technique requires active listening to identify the underlying emotional concerns or feelings contained in clients’ messages. These feelings are then referred back to clients to promote a clearer understanding of what they have said. 2. Content themes 3. Clarification of information 4. Summarization of the topics discussed 25. A client states, “My wife is going to be very upset that my prostate surgery probably is going to leave me impotent.” Which is the best response by the nurse? 1. “I’m sure your wife will be willing to make this sacrifice in exchange for your well-being.” 2. “The surgeons are getting great results with nerve-sparing surgery today.”3. “Your wife may not put as much emphasis on sex as you think.” 4. “Let’s talk about how you feel about this surgery.” 26. A client states, “I think that I am dying.” The nurse responds, “You believe that you are dying?” Which interviewing approach did the nurse use? 1. Focusing 2. Reflecting 3. Validating 4. Paraphrasing 27. A nurse plans to foster a therapeutic relationship with a client. Which is important for the nurse to do? 1. Sympathize with the client when the client communicates sad feelings. Empathize, not sympathize 2. Demonstrate respect when discussing emotionally charged subjects. 3. Use humor to defuse emotionally charged topics of discussion. 4. Work on establishing a friendship with the client. 28. A client appears tearful and is quiet and withdrawn. The nurse says, “You seem very sad today.” Which interviewing approach did the nurse use? 1. Examining Not an interviewing technique 2. Reflecting Reflective technique refers to feelings implied in context or verbal/nonverbal communication. 3. Clarifying 4. Orienting 29. A client is admitted to the hospital with a tentative medical diagnosis, and multiple diagnostic tests are performed. Where in the client’s medical record can the nurse find documentation about the current medical diagnosis after the diagnostic test results are reviewed by the primary health-care provider? 1. Progress Notes 2. Admission Sheet 3. History and Physical4. Social Service Record 30. Which nursing action should the nurse implement when speaking with an older adult whose hearing is impaired? Select all that apply. 1. __X__ Limit background noise. 2. __X__ Enunciate words without exaggeration. 3. __X__ Use gestures to augment communication. 4. __X__ Stand directly in front of the client when speaking. 5. __X__ Talk in a normal rate and volume when speaking with the client. 31. A client with a newly created colostomy wants to learn how to irrigate the colostomy. The nurse provides this teaching by developing a therapeutic nurse-client relationship and implementing teaching strategies. Identify the statement that is included in the working stage of this therapeutic relationship. Select all that apply. 1. “How do you feel about doing this procedure?” Orientation stage 2. “Would you like to try to insert the cone yourself today?” Working stage involves completing interventions that address expected outcomes, such as learning how to perform a colostomy irrigation. 3. “You did a great job managing the instillation of fluid today.” Working stage includes providing feedback and encouragement 4. “I am here to help you learn how to irrigate your colostomy.” Orientation stage where nurse and client make a verbal agreement to work together to assist client to achieve a goal 5. “I’ll arrange for a home-care nurse to visit you in your home when you are discharged.” Termination stage 32. A risk manager is conducting a retrospective audit of a client’s clinical record to identify the use of unacceptable abbreviations. Which abbreviation did the risk manager identify that is on The Joint Commission’s official Do Not Use List? Select all that apply.1. __X__ U 2. _____ ml 3. _____ mg 4. __X__ MS 5. __X__ QOD 6. _____ 0800 hour CLIENT’S CLINICAL RECORD 33. A nurse is attempting to develop a helping relationship with a client who was recently diagnosed with cancer. Which factor is unique to this helping relationship? Select all that apply. 1. _____ The client should always assume the dominant role. 2. _____ The nurse and the client equally share information. Focus on client not nurse 3. __X__ The interaction is specific to the client. 4. __X__ The interaction is guided by a purpose. 5. _____ The needs of both participants are met. Focus on client not nurse 35. An agitated 80-year-old client states, “I’m having trouble with my bowels.” Which response by the nurse incorporates the interviewing skill of paraphrasing? Select all that apply. 1. _____ “Tell me what you mean by having trouble.” Clarification 2. __X__ “It sounds like your bowels are causing you problems.” 3. _____ “You sound upset that your bowels are causing difficulties.” Reflection 4. _____ “It’s common to have problems with the bowels at your age.” Negates client’s concern and cuts off communication 5. _____ “When did you first notice having trouble with your bowels?” Direct question (focused assessment) 36. A client states, “I am surprised that I couldn’t even eat half my breakfast.” Which statement by the nurse uses the interviewing skill of reflection? Select all that apply. 1. _____ “Let’s talk about your inability to eat.” 2. _____ “What part of your breakfast were you able to eat?”3. __X__ “You appear startled that you did not finish your tray of food.” 4. _____ “How long have you been unable to eat most of your breakfast?” 5. __X__ “You seem surprised that you were unable to eat all your breakfast.” 37. A nurse in a subacute unit in a skilled nursing facility is caring for a client who recently had the surgical creation of a colostomy. Place the following nursing actions in the order that reflects the nurse-client therapeutic relationship, beginning with the first stage and progressing to the last stage. 1. Review all the information on the client’s clinical record. Preinteraction stage 2. Introduce self to the client. Orientation stage 3. Explore the reasons for the nurse-client interaction. Orientation stage 4. Assist the client to learn how to perform colostomy self-care. Working stage 5. Provide positive feedback to the client for successful performance of a colostomy irrigation. Working stage 6. Summarize the goals and objectives achieved. Termination stage 38. Which ability of the nurse is important to achieve effective therapeutic communication? Select all that apply. 1. __X__ Using interviewing skills 2. __X__ Remaining nonjudgmental 3. _____ Sending only verbal messages 4. _____ Being assertive when collecting data 5. _____ Displaying sympathy when communicating Empathy, not sympathy 39. A client is to have arthroscopic surgery of the knee to repair a torn tendon. The client says, “I don’t know if I’ll make it through this surgery.” Which response by the nurse may block further communication by the client? Select all that apply. 1. __X__ “The type of surgery you are having is minor.”2. _____ “Surgery often can be frightening.” Reflective 3. __X__ “Everything will be all right.” 4. __X__ “You are not going to die.” 5. _____ “You sound scared.” Reflective 40. Which should a nurse never do when documenting information on a client’s electronic medical record? Select all that apply. 1. Leave the client’s medical record open on the computer screen when entering the client’s room to administer a medication. 2. Share information verbally about a client with another nurse who is also caring for the client. 3. Document nursing care administered to a client immediately after it is completed. 4. Give a personal access code to another member of the health-care team. 5. Document exact quotes of a client’s subjective information. CHAPTER 4 THE NURSING PROCESS 185 1. A nurse makes a home-care visit for a client who had total hip replacement surgery 1 week ago. During which of the five steps in the nursing process does the nurse determine whether outcomes of care are achieved? 1. Implementation Outcomes are not determined; planned nursing care is delivered 2. Evaluation Evaluation occurs when actual outcomes are compared with expected outcomes that reflect goal achievement. If the goal is achieved the client’s needs are met3. Planning Expected outcomes are determined but their achievement is not measured yet 4. Analysis Outcomes are not determined, the nurse identifies human responses to actual or potential health problems 2. When considering the nursing process, the word “observe” is to “assess” as the word “explore” is to which of the following words? 1. Plan Observe = view something scientifically, assess = collect information 2. Analyze Explore = examine, Analyze = investigate 3. Evaluate Evaluate = come to a conclusion about a client’s response to a nursing intervention 4. Implement Implement = carry out an action 3. Which statement is related to the concept that is central to the nursing process? 1. It is dynamic rather than static. “Nursing process is a complex, interactive, five-step problem-solving process designed to meet a client’s needs.” 2. It focuses on the role of the nurse. Focuses on needs of client, not role of nurse 3. It moves from the simple to the complex. 4. It is based on the client’s medical problem. 4. Which word best describes the role of the nurse when using the nursing process to meet the needs of the client holistically? 1. Teacher 2. Advocate 3. Surrogate 4. Counselor 5. Which word is most closely associated with scientific principles? Scientific principles = established rules of action1. Data 2. Problem 3. Rationale Justification based on reasoning 4. Evaluation 6. A pebble dropped into a pond causes ripples on the surface of the water. Which part of the nursing diagnosis is directly related to this concept? 1. Defining characteristics 2. Outcome criteria 3. Etiology Also known as contributing factors includes conditions, situations or circumstances that cause the development of the human response identified in the problem statement of the nursing diagnosis 4. Goal 7. A nurse teaches a client to use visualization to cope with chronic pain. Which step of the nursing process is associated with this nursing intervention? 1. Planning In the Planning Step, identification of nursing interventions that are most likely to be effective 2. Analysis 3. Evaluation Evaluation occurs when actual outcomes are compared with expected outcomes that reflect goal achievement 4. Implementation In the Implementation step, planned nursing care is delivered 8. A nurse is caring for several clients. Which nursing action reflects the assessment step of the nursing process? 1. Taking a client’s apical pulse rate every 2 hours after the client is admitted for an episode of chest pain Implementation Nurse puts into action the plan to monitor the client’s V/S after a cardiac event is suspected 2. Scheduling a client’s fluid intake over 12 hours when the client has a fluid restriction Planning3. Examining a client for injury after a fall in the bathroom Assessment involves collecting data via observation, physical examination, and interviewing 4. Obtaining a client’s respiratory rate after a nebulizer treatment Evaluation Nurse assess the client’s RR and effort after a nebulizer treatment to determine if the treatment was effective in reducing airway resistance, thereby improving the client’s RR and reducing respiratory effort 9. A nurse is caring for a client with a fever. Which is a well-designed goal for this client? 1. “The client will have a lower temperature.” “Lower” is not specific, measurable, or objective 2. “The client will be taught how to take an accurate temperature.” Not a goal, an action the nurse plans to implement to help a client achieve a goal 3. “The client will maintain fluid intake adequate to prevent dehydration.” Goals must be client centered, specific, measurable, realistic and have a time frame in which the expected outcome is to be achieved. The words “adequate” and “dehydration” are based on generally accepted criteria against which to measure the client’s actual outcome. The word “maintain” connotes continuously, which is a time frame. 4. “The client will be given aspirin every eight hours whenever necessary.” Not a goal, an action the nurse plans to implement to help a client achieve a goal 10. Which should the nurse do during the evaluation step of the nursing process? 1. Set the time frames for goals. Part of Planning 2. Revise a plan of care. Revising a plan of care takes place in the evaluation step of the nursing process. If, during evaluation, it is determined that the goal was not met, the reasons for failure have to be identified and plan to be modified. 3. Determine priorities. Part of Planning 4. Establish outcomes. Part of Planning11. A client is admitted to a postoperative surgical unit after abdominal surgery. During which step of the nursing process does the nurse determine which actions are required to meet the needs of this client? 1. Implementation Implementation = putting plan of care into action 2. Assessment Assessment = use various skills, such as observation, interviewing, and physical examination, to collect data from various sources 3. Planning 4. Analysis Analysis = nurse identifies the client’s human responses to actual or potential health problems 12. Which information supports the appropriateness of a nursing diagnosis? 1. Defining characteristics Defining characteristics are the major and minor cues that form a cluster that supports or validates the presence of a nursing diagnosis. At least one major defining characteristic must be present for a nursing diagnosis to be considered appropriate for the client. 2. Planned interventions 3. Diagnostic statement A nursing diagnosis is made up of two parts, the diagnostic statement (aka problem statement) and the “related to” factors (aka factors that contribute to the problem or etiology) 4. Related risk factors 13. Which is the primary goal of the assessment phase of the nursing process? 1. Build trust 2. Collect data 3. Establish goals 4. Validate the medical diagnosis 14. Which most directly influences the planning step of the nursing process?1. Related factors 2. Diagnostic label 3. Secondary factors 4. Medical diagnosis 15. A nurse collects information about a client. Which should the nurse do next? 1. Plan nursing interventions. Nursing care is planned after nursing diagnoses and goals are identified, not immediately after data are collected 2. Write client-centered goals. Goals are designed after nursing diagnosis is identified, not after data collection 3. Formulate nursing diagnoses. Need to find significance before formulating any nursing diagnoses 4. Determine significance of the data. 16. When two nursing diagnoses appear closely related, which should the nurse do first to determine which diagnosis most accurately reflects the needs of the client? 1. Reassess the client. 2. Examine the related to factors. These factors are identified after the problem statement is identified 3. Analyze the secondary to factors. Secondary to factors are identified after the related to factors of the problem are identified 4. Review the defining characteristics. The first thing to do should be to differentiate b/w two closely associated nursing diagnoses is to compare the data collected to the major and minor defining characteristics. 17. Which is the primary reason why a nurse performs a physical assessment of a newly admitted client? 1. Identify if the client is at risk for falls. 2. Ensure that the client’s skin is totally intact.3. Identify important information about the client. 4. Establish a therapeutic relationship with the client. 18. A nurse evaluates a client’s response to a nebulizer treatment. To which aspect of the nursing process is this evaluation most directly related? 1. Goal To evaluate effectiveness of a nursing action, nurse must compare the actual client outcome with the expected client outcome. The expected outcomes are measurable data that reflect goal achievement and the actual outcomes are what really happened. 2. Problem 3. Etiology 4. Implementation 19. A nurse concludes that a client’s elevated temperature, pulse, and respirations are significant. Which step of the nursing process is being used when the nurse comes to this conclusion? 1. Implementation 2. Assessment 3. Evaluation 4. Analysis 20. When the nurse considers the nursing process, the word “identify” is to “recognize” as the word “do” is to which of the following words? 1. Implement 2. Evaluate 3. Analyze 4. Plan 21. A nurse is collecting subjective data associated with a client’s anxiety. Which assessment method should be used to collect this information? 1. Observing 2. Inspection3. Auscultation 4. Interviewing 22. A nurse assesses that a client has slurred speech and a retained bolus of food in the mouth. Which additional condition assessed by the nurse should be clustered with these clinical indicators? Select all that apply. 1. __X__ Hoarseness 2. _____ Dyspepsia 3. __X__ Coughing 4. __X__ Drooling 5. __X__ Gurgling 6. _____ Plaque 23. Nurses use the nursing process to provide nursing care. These statements reflect nursing care being provided to several clients. Place the statements in order as the nurse progresses through the steps of the nursing process, starting with assessment and ending with evaluation. 1. “Did you sleep last night after I gave you the sleeping medication?” 2. “The client’s clinical manifestations indicate dehydration.” 3. “The client will have a bowel movement in the morning.” 4. “What brought you to the hospital today?” 5. “I am going to give you an enema.” 4. “What brought you to the hospital today?” Assessment 2. “The client’s clinical manifestations indicate dehydration.” Analysis 3. “The client will have a bowel movement in the morning.” Planning 5. “I am going to give you an enema.” Implementation1. “Did you sleep last night after I gave you the sleeping medication?” Evaluation 24. A nurse is caring for a client with a urinary elimination problem. Which is an accurately stated goal? Select all that apply. 1. “The client will be taught how to use a bedpan while on bedrest.” Action to implement 2. “The client will experience fewer incontinence episodes at night.” “Fewer” is not specific, measurable, or objective 3. “The client will transfer from a chair to the toilet independently and safely.” Does not include time frame for expected goal 4. “The client will be assisted to the commode every 2 hours and whenever necessary.” Action to implement 5. “The client will experience one or no events of urinary incontinence daily within 6 weeks.” 25. Which human response identified by the nurse is an example of objective data? Select all that apply. 1. __X__ Irregular radial pulse of 50 beats per minute 2. __X__ Wheezing on expiration 3. __X__ Temperature of 99°F 4. __X__ Bradypnea 5. __X__ Vomiting 26. Place the following statements that reflect the analysis step of the nursing process in the order in which they should be implemented. 1. Cluster data. 2. Identify conclusions. 3. Interpret clustered data. 4. Communicate conclusion to other health team members.5. Identify when additional data are needed to further validate clustered data. 1. Cluster data 5. Identify when additional data are needed to further validate clustered data. 3. Interpret clustered data. 2. Identify conclusions. 4. Communicate conclusion to other health team members. 27. Which client statement provides subjective data? Select all that apply. 1. __X__ “I’m not sure that I am going to be able to manage at home by myself.” 2. _____ “I can call a home-care agency if I feel I need help at home.” 3. _____ “What should I do if I have uncontrollable pain at home?” 4. _____ “Will a home health aide help me with my care at home?” 5. __X__ “I’m afraid because I live alone and I’m on my own.” 28. Which nursing action reflects an activity associated with the analysis step of the nursing process? Select all that apply. 1. _____ Formulating a plan of care Planning 2. __X__ Identifying the client’s potential risks 3. __X__ Grouping data into meaningful relationships 4. _____ Designing ways to minimize a client’s stressors Planning 5. _____ Making decisions about the effectiveness of client care Evaluation 29. A nurse is interviewing a client. Which client statement is an example of objective data? Select all that apply. 1. _____ “I am hungry.” 2. _____ “I feel very warm.”3. __X__ “I ate half my lunch.” 4. __X__ “I have a rash on my arm.” 5. _____ “I have the urge to urinate.” 6. __X__ “I vomit every time I eat something.” 30. Which statement indicates that the nurse is using inductive reasoning? Select all that apply. 1. A client is admitted with a diagnosis of dehydration, and the nurse assesses the client’s skin for tenting. Deductive reasoning moves from general (client is dehydrated) to specific deduction (client will probably have tenting of skin, a sign of dehydration. 2. A nurse observes a client fall out of bed on the right hip and immediately assesses the client for right hip pain. 3. A client has an elevated white blood cell count and a fever. The nurse concludes that the client may have an infection. Inductive reasoning moves from specific to the general. 4. A client who is scheduled for surgery is crying, trembling, and has a rapid pulse. The nurse makes the inference that the client is anxious. 5. A nurse receives a call from the admission department that a client with hypoglycemia is being admitted to the unit. The nurse plans to assess the client for pale, cool, clammy skin and a low blood glucose level. 31. The following statements reflect steps in the nursing process. Place the statements in order as the nurse advances through the steps of the nursing process, beginning with assessment and ending with evaluation. 1. “The client is encouraged to attempt to defecate after meals.” 2. “The client reports not having had a bowel movement for 8 days.”3. “The client has constipation related to immobility and inadequate fluid intake.” 4. “The client will have a bowel movement within 2 days that is of soft consistency.” 5. “The client’s stool is still hard and dry 2 days after initiating an increase in fluids and activity.” 2. “The client reports not having had a bowel movement for 8 days.” Data collection that occurs in Assessment 3. “The client has constipation related to immobility and inadequate fluid intake.” Etiological factors contributing to the nursing diagnosis problem statement, which is “constipation” 4. “The client will have a bowel movement within 2 days that is of soft consistency.” Measurable goal 1. “The client is encouraged to attempt to defecate after meals.” Implementation of a planned action 5. “The client’s stool is still hard and dry 2 days after initiating an increase in fluids and activity.” Client’s response to compare with client’s actual outcome with expected outcome 32. A nurse is interviewing a client at the change of shift. Which client statement reflects subjective data? Select all that apply. 1. __X__ “When I lift my head up off the bed, I feel like vomiting.” 2. _____ “I just used the urinal, and it needs to be emptied.” 3. __X__ “My pain feels like a 5 on a scale of 0 to 5.” 4. _____ “The physician said I can go home today.” 5. _____ “I gained 10 pounds in the last month.” 34. A client is transferred from the emergency department to a medicalsurgical unit at 6:30 p.m. The nurse arriving on duty at 8 p.m. reviews theclient’s clinical record. Which information documented in the clinical record reflects the evaluation step of the nursing process? 1. Productive cough Info collected during Assessment 2. No dizziness reported by the client Client’s response to ambulation 3. Seek prescription for chest physiotherapy Planning 4. Acetaminophen 650 mg administered at 5 p.m. Implementation CLIENT’S CLINICAL RECORD 35. The nurse assesses a client and collects a variety of data. Identify the human response that is subjective data. Select all that apply. 1. __X__ Nausea 2. _____ Jaundice 3. _____ Ecchymosis 4. _____ Diaphoresis 5. _____ Hypotension CHAPTER 4 INFECTION CONTROL 219 1. Which is the primary reason why the nurse should avoid glued-on artificial nails? 1. They interfere with dexterity of the fingers. 2. They could fall off in a client’s bed. 3. They harbor microorganisms. 4. They can scratch a client. 2. A nurse working in a clinic is assessing clients of a variety of ages. Which age group should the nurse particularly assess for subtle clinical manifestations of subclinical infections? 1. Children of school age 2. Older adults 3. Adolescents4. Infants 3. Which condition places a client at the highest risk for developing an infection? 1. Implantation of a prosthetic device 2. Burns over more than 20% of the body 3. Presence of an indwelling urinary catheter 4. More than 2 puncture sites from laparoscopic surgery 4. Which does the nurse determine is a specific line of defense against infection? 1. Mucous membrane of the respiratory tract Nonspecific defense 2. Urinary tract environment Nonspecific defense 3. Integumentary system Nonspecific defense 4. Immune response 5. A nurse is concerned about a client’s ability to withstand exposure to pathogens. Which blood component should the nurse monitor? 1. Platelets Essential for blood clotting 2. Hemoglobin RBCs 3. Neutrophils WBCs are the primary defense against infection 4. Erythrocytes RBCs 6. When brushing a client’s hair, the nurse identifies white oval particles attached to the hair behind the ears. Which condition with additional clinical manifestations that support it should lead the nurse to assess the client further? 1. Pediculosis 2. Hirsutism Hirsutism is the excessive growth of hair in unusual places 3. Dandruff Dandruff is excessive shedding of dry white scales as a result of the expected exfoliation of the epidermis of the scalp4. Scabies Scabies is a communicable skin disease caused by an itch mite and is character by skin lesion with intense itching 7. A nurse educator is evaluating whether a new staff nurse understands the relationship between a fever and an infection. Which statement by the new staff nurse indicates an understanding of this relationship? 1. “Phagocytic cells release pyrogens that stimulate the hypothalamus.” 2. “Leukocyte migration precipitates the inflammatory response.” 3. “Erythema increases the flow of blood throughout the body.” Erythema does not increase flow of blood throughout the body. Increased blood flow to a localized area causes diffuse redness (erythema). 4. “Pain activates the sympathetic nervous system.” 8. A nurse is caring for a group of clients with infections. Which infection is classified as a health-care–associated infection? 1. Respiratory infection contracted from a visitor 2. Vaginal infection in a postmenopausal woman 3. Urinary tract infection in a client who is sedentary 4. Wound infection caused by unwashed hands of a caregiver Iatrogenic infection 9. A nurse is caring for a client with a high fever secondary to septicemia. The primary health-care provider prescribes a cooling blanket (hypothermia blanket). Through which mechanism does the hypothermia blanket achieve heat loss? 1. Radiation 2. Convection 3. Conduction 4. Evaporation10. Which client condition identified by a nurse is unrelated to infection? 1. Catabolism Catoblism, the destructive phase of metabolism with is resultant release of energy, is related to infection. 2. Hyperglycemia Serum glucose is increased (hyperglycemia) in the presence of an infection because of the release of glucocorticoids 3. Ketones in the urine 4. Decreased metabolic activity Metabolic activity increases, not decreases with an infection as the body mounts a defense to fight invading pathogenic microorganisms. 11. A nurse is caring for a group of hospitalized clients. Which should the nurse do first to prevent client infections? 1. Provide small bedside bags to dispose of used tissues. 2. Encourage staff to avoid coughing near clients. 3. Administer antibiotics as prescribed. 4. Identify clients at risk. 12. A client has a wound that is healing by secondary intention. Which solution to cleanse the wound and dressing should the nurse expect will be prescribed to support wound healing? 1. Normal saline and a gauze dressing Removal of dry dressing will pull recently granulated tissue off of wound bed, impeding wound healing. 2. Normal saline and a wet-to-damp dressing Wet-to-damp dressing allows epidermal cells to migrate more rapidly across wound 3. Povidone-iodine and a dry sterile dressing 4. Half peroxide and half normal saline and a wet-to-dry dressing 13. A nurse is caring for a group of clients experiencing various medical conditions. Which condition places the client at the highest risk for a wound infection? 1. Surgical creation of a colostomy Surgery is conducted using sterile technique 2. First-degree burn on the back3. Puncture of the foot by a nail 4. Paper cut on the finger 14. A school nurse is teaching a class of adolescents about the function of the integumentary system. Which fact about how the skin protects the body against infection is important to include in this discussion? 1. Cells of the skin are constantly being replaced, thereby eliminating external pathogens. 2. Epithelial cells are loosely compacted on skin, providing a barrier against pathogens. Epithelial cells on skin are closely, not loosely compacted. 3. Moisture on the skin surface prevents colonization of pathogens. Moisture on skin surface facilitates, not prevents. 4. Alkalinity of the skin limits the growth of pathogens. Acidity, not alkalinity limits growth of pathogens. 15. A client’s stool specimen is positive for Clostridium difficile. Which isolation precautions should the nurse institute for this client? 1. Droplet 2. Contact 3. Reverse 4. Airborne 16. Which should the nurse do to interrupt the transmission link in the chain of infection? 1. Wash the hands before providing care to a client. 2. Position a commode next to a client’s bed. 3. Provide education about a balanced diet. 4. Change a dressing when it is soiled. 17. Which client statement indicates that further teaching by the nurse is necessary regarding how to ensure protection from food contamination? Select all that apply.1. _____ “I should stuff a turkey immediately before putting it in the oven.” 2. __X__ “I love juicy, rare hamburgers with onion and tomato.” 3. _____ “I prefer chicken salad sandwiches with mayonnaise.” 4. _____ “I know to spit out food that does not taste good.” 5. _____ “I should defrost frozen food in the refrigerator.” 18. A client is admitted to the ambulatory surgery unit for an elective procedure. When performing a physical assessment, the nurse identifies that the client has Pediculus capitis (head lice). Place the nurse’s interventions in the order in which they should be implemented. 1. Establish contact isolation. 2. Comb the hair with a fine-toothed comb. 3. Notify the provider of the client’s condition. 4. Obtain a prescription for a pediculicidal shampoo. 5. Wash the client’s hair with a pediculicidal shampoo. 1. Establish contact isolation. 3. Notify the provider of the client’s condition. 4. Obtain a prescription for a pediculicidal shampoo. 5. Wash the client’s hair with a pediculicidal shampoo. 2. Comb the hair with a fine-toothed comb. 19. Which primary defense protects the body from infection? Select all that apply. 1. __X__ Tears in the eyes 2. __X__ Healthy, intact skin 3. __X__ Cilia of respiratory passages 4. __X__ Acidity of gastric secretions 5. __X__ Dry environment of the epidermis20. A nurse is caring for clients with a variety of wounds. Which wound will likely heal by primary intention? Select all that apply. 1. __X__ Cut in the skin from a kitchen knife Primary healing intention Wound edges are lightly pulled together (approximated) 2. _____ Excoriated perianal area 3. _____ Abrasion of the skin 4. __X__ Surgical incision 5. _____ Pressure ulcer Heals by secondary intention when wound edges are not approximated because of full-thickness tissue loss 22. A client has a wound infection. Which local human response should the nurse expect to identify? Select all that apply. 1. _____ Leukocytosis Systemic, not local 2. _____ Malaise Systemic, not local 3. __X__ Edema 4. _____ Fever Fever is a systemic, not local response 5. __X__ Pain 23. Which nursing action protects clients as susceptible hosts in the chain of infection? Select all that apply. 1. _____ Wearing personal protective equipment 2. __X__ Administering childhood immunizations 3. _____ Recapping a used needle before discarding 4. __X__ Instituting prescribed immunoglobulin therapy 5. _____ Disposing of soiled gloves in a waste container 24. From which type of isolation precaution is the N95 mask designed to protect the nurse? 1. Contact 2. Airborne 3. Standard 4. Protective25. A client tells the nurse, “I think I have an ear infection.” For which objective human response to an ear infection should the nurse assess this client? Select all that apply. 1. _____ Throbbing pain 2. __X__ Purulent drainage 3. _____ Feeling of pressure 4. _____ Dizziness when moving 5. _____ Hearing a buzzing sound 26. Which is an example of a primary defense that protects the body from infection? Select all that apply. 1. _____ Antibiotic therapy 2. __X__ Lysozymes in saliva 3. __X__ The low pH of the skin 4. __X__ The acidic environment of the vagina 5. __X__ Production of mucus by cells in the genitourinary tract 27. A nurse is caring for a client who has a prescription for shortening a Penrose drain 1 inch daily. The nurse washes the hands, removes the soiled dressing, sets a sterile field, dons sterile gloves, and cleans around the drain with sterile saline solution as prescribed. Place the following steps in the order in which they should be implemented by the nurse. 1. Complete dressing the wound. 2. Pull the drain out 1 inch, gently and steadily. 3. Grip the Penrose drain with a pair of sterile forceps. 4. Remove the pin and reattach it to the drain closer to the surface of the wound. 5. Cut off the excess drain using sterile scissors, ensuring that 2 inches remain outside the wound. 3. Grip the Penrose drain with a pair of sterile forceps. 2. Pull the drain out 1 inch, gently and steadily. 4. Remove the pin and reattach it to the drain closer to the surface of the wound.5. Cut off the excess drain using sterile scissors, ensuring that 2 inches remain outside the wound. 1. Complete dressing the wound. 28. Which nursing action protects clients from infection at the portal of entry portion of the chain of infection? Select all that apply. 1. Positioning an indwelling urine collection bag below the level of the client’s pelvis 2. Using sterile technique when administering an intramuscular injection 3. Enclosing a urine specimen in a biohazardous transport bag Controlling mode of transmission 4. Wearing clean gloves when handling a client’s excretions Controlling mode of transmission 5. Washing the hands after removal of soiled gloves Controlling mode of transmission 6. Maintaining a dressing over a surgical incision 29. The nurse is reviewing the clinical record of a newly admitted older adult male client. Which piece of information should cause the most concern? 1. Temperature 103°F 2. Abdominal cramping 3. WBC 30,000 cells/mcL 4. Blood pressure 110/86 mm Hg 30. A nurse identifies that a client has an inflammatory response. Which localized client response supports this conclusion? Select all that apply. 1. _____ Fever 2. __X__ Swelling3. __X__ Erythema 4. _____ Bradypnea 5. _____ Tachycardia 31. A nurse must collect the following specimens. Which specimen does not require the use of surgical aseptic technique? Select all that apply. 1. __X__ Stool for occult blood 2. __X__ Stool for ova and parasites 3. _____ Oropharyngeal mucus for a culture 4. _____ Urine from a retention catheter for a urinalysis 5. _____ Exudate from a wound for culture and sensitivity 32. A nurse plans to remove a client’s wound dressing. The nurse identifies the client, explains what is going to be done and why, washes the hands, collects equipment, provides for the client’s privacy, and places the client in an appropriate and comfortable position. Place the following steps in the order in which they should be implemented when removing the soiled dressing. 1. Don clean gloves. 2. Pull the tape away from the skin gently. 3. Assess the volume, color, and odor of exudate. 4. Place the soiled dressing and gloves in a biohazardous waste receptacle. 5. Remove the dressing by lifting the edge of the dressing upward and toward the center of the wound. 6. Loosen the edges of the tape around the dressing, starting from the outside and moving toward the center of the dressing. 1. Don clean gloves. 6. Loosen the edges of the tape around the dressing, starting from the outside and moving toward the center of the dressing. 2. Pull the tape away from the skin gently.5. Remove the dressing by lifting the edge of the dressing upward and toward the center of the wound. 3. Assess the volume, color, and odor of exudate. 4. Place the soiled dressing and gloves in a biohazardous waste receptacle. 33. Which client information collected by the nurse reflects a systemic response to a wound infection? Select all that apply. 1. __X__ Increased body temperature 2. __X__ Increased heart rate 3. __X__ Leukocytosis 4. __X__ Fatigue 5. __X__ Chills 34. A nurse is caring for a client who has a prescription for a vacuum-assisted closure device using black foam to facilitate wound healing. The nurse verifies the prescription, explains to the client what is to be done and why, gathers equipment, washes the hands, sets a sterile field, and dons sterile gloves. Place the following steps in the order in which they should be implemented. 1. Trim the black foam to the size of the wound cavity. 4. Place the foam in the wound cavity without overlapping onto the surrounding skin. 6. Place the suction device pad over the hole in the film and apply gentle pressure to the suction device pad. 2. Pinch and cut a 2-cm round hole in the center of the transparent film. 5. Apply the transparent film 1 to 2 inches beyond wound edges without stretching or wrinkling the transparent film.3. Connect the suction device tubing to the collection canister tubing and pump. 35. A primary health-care provider prescribes azithromycin for a client with a diagnosis of chronic bronchitis. Which should the nurse teach the client that is important to know about taking azithromycin? Select all that apply. 1. “Take this medication with food.” Azithromycin (Zithromax) should be taken 1h before or 2h after meals 2. “You can discontinue the medication as soon as you feel better.” Should finish entire regimen 3. “Take 500 mg on the first day and then 250 mg for 4 more days, for a total of 1.5 g.” 4. “The first dose should be taken after we notify you of the results of the culture and sensitivity.” Don’t wait to take 5. “Avoid taking an antacid containing aluminum or magnesium within 2 hours of taking this medication.” CHAPTER 4 SAFETY 234 1. A client brings several electronic devices to a nursing home. One of the devices has a two-pronged plug. Which rationale should the nurse provide when explaining why an electrical device must have a three-pronged plug? 1. Controls stray electrical currents 2. Promotes efficient use of electricity 3. Shuts off the appliance if there is an electrical surge 4. Divides the electricity among the appliances in the room 2. A nurse is caring for a client with Parkinson’s disease who is experiencing difficulty swallowing. For which major potential problemassociated with dysphagia should the nurse assess the client? 1. Anorexia 2. Aspiration 3. Self-care deficit 4. Inadequate intake 3. A nurse is caring for a confused client. Which should the nurse do to prevent this client from falling? 1. Encourage the client to use the corridor handrails. 2. Place the client in a room near the nurses’ station. 3. Reinforce how to use the call bell. 4. Maintain close supervision. 4. A school nurse is teaching children about fire safety procedures. Which is the first thing they should be taught to do if their clothes catch on fire? 1. Yell for help. 2. Roll on the ground. 3. Take their clothes off. 4. Pour water on their clothes. 5. A primary health-care provider prescribes a vest restraint for a client. Which should the nurse do first when applying this restraint? 1. Perform an inspection of the client’s skin where the restraint is to be placed. 2. Ensure that the back of the vest is positioned on the client’s back. 3. Permit four fingers to slide between the client and the restraint. Two fingers not four 4. Secure the restraint to the bed frame using a slipknot. Not first nursing intervention 6. An unconscious client begins vomiting. In which position should the nurse place the client?1. Supine 2. Side-lying 3. Orthopneic 4. Low-Fowler 7. A toaster is on fire in the pantry of a hospital unit. Which should the nurse do first? 1. Activate the fire alarm. Because no client is in jeopardy, the nurse’s initial action should be to activate the fire alarm. 2. Unplug the toaster from the wall. 3. Put out the fire with an extinguisher. 4. Evacuate the clients from the room next to the kitchen. 8. The risk management coordinator is preparing a program on the factors that contribute to falls in a hospital setting. Which factor that most often contributes to falls should be included in this program? 1. Wet floors 2. Frequent seizures 3. Advanced age of clients 4. Misuse of equipment by nurses 9. A nurse is assessing a client who is being admitted to the hospital. Which is the most important information that indicates whether the client is at risk for physical injury? 1. Weakness experienced during a prior admission 2. Medication that increases intestinal motility 3. Two recent falls that occurred at home 4. The need for corrective eyeglasses 10. Which should the nurse do to best prevent a client from falling? 1. Provide a cane.2. Keep walkways clear of obstacles. 3. Assist the client with ambulation. 4. Encourage the client to use hallway handrails. 11. Which is the last step in making an occupied bed that the nurse should teach a nursing assistant? 1. Elevating the head of the bed to a semi-Fowler position 2. Ensuring that the client is in a comfortable position 3. Lowering the height of the bed toward the floor 4. Raising both the upper side rails on the bed 12. A nurse is caring for a client with a nasogastric tube for gastric decompression. Which nursing action takes priority? 1. Discontinuing the wall suction when providing nursing care 2. Positioning the client in the semi-Fowler position The semi-Fowler position keeps gastric secretions in stomach via gravity (preventing reflux and aspiration) and allows the gastric contents to be suctioned out by the NG tube. 3. Instilling the tube with 30 mL of air every 2 hours Not done every 2h, but may be done to help reestablish patency of tube when clogged 4. Caring for the nares at least every 8 hours Should be done more frequently than every 8h 13. A family member brings an electric radio to a client in a longterm care facility. The client tells the nurse that an electric shock was felt while turning on the radio. Which should the nurse do first? 1. Arrange for the maintenance department to examine the radio. 2. Disconnect the radio from the source of energy. 3. Check the client’s skin for electrical burns. 4. Take the client’s apical pulse. 14. A nurse educator is teaching a group of newly hired nursing assistants. Which hospitalized client should they be taught is at the highest risk for injury?1. School-age child 2. Comatose teenager 3. Postmenopausal woman 4. Confused middle-age man 15. A nurse in the nursing education department of a community hospital is planning an in-service education class about injury prevention. Which factor that most commonly causes physical injuries in hospitalized clients should be included in the teaching plan? 1. Malfunctioning equipment 2. Failure to use restraints 3. Visitors 4. Falls 16. Which is the priority nursing intervention to prevent client problems associated with latex allergies? 1. Use nonlatex gloves. 2. Identify persons at risk. 3. Keep a latex-safe supply cart available. 4. Administer an antihistamine prophylactically. 17. Which nursing intervention enhances an older adult’s sensory perception and thereby helps prevent injury when walking from the bed to the bathroom? 1. Providing adequate lighting 2. Raising the pitch of the voice 3. Holding onto the client’s arm Doesn’t enhance sensory perception 4. Removing environmental hazards 18. A nurse is preparing a client for a physical examination. Which is most important for the nurse to do in this situation? 1. Identify the positions contraindicated for the client during the examination. 2. Explore the client’s attitude toward health-care providers.3. Inquire about other professionals caring for the client. 4. Ask when the client last had a physical examination. 19. A client has dysphagia. Which nursing action takes priority when feeding this client? 1. Ensuring that dentures are in place 2. Medicating for pain before providing meals 3. Providing verbal cueing to swallow each bite 4. Checking the mouth for emptying between every bite 20. A 3-year-old child is admitted to the pediatric unit. Which should the nurse do to maintain the safety of this preschool-age child? 1. Teach the child how to use the call bell. 2. Put the child in a crib with high side rails. 3. Ensure the child is under continuous supervision. 4. Have the child stay in the playroom most of the day. 21. A nurse is caring for a client with dementia. Which time of day is of most concern for the nurse when trying to protect this client from injury? 1. Afternoon 2. Morning 3. Evening 4. Night 22. A nurse is orienting a newly admitted client to the hospital. Which is most important for the nurse to teach the client how to do? 1. Notify the nurse when help is needed. 2. Get out of the bed to use the bathroom. 3. Raise and lower the head and foot of the bed. 4. Use the telephone system to call family members.23. Profuse smoke is coming out of the heating unit in a client’s room. Which should the nurse do first? 1. Open the window. Opening a window is contraindicated because environmental air will feed the fire. 2. Activate the fire alarm. 3. Move the client out of the room. 4. Close the door to the client’s room. 24. A nurse must apply a hospital gown that does not have snaps on the shoulders to a client receiving an IV infusion in the forearm. Which should the nurse do? 1. Put the gown on the client’s arm without the IV, drape the gown over the other shoulder, and adjust the closure behind the neck. 2. Close the clamp on the IV tubing for no more than 15 seconds while putting the gown on the client. 3. Disconnect the client’s IV at the insertion site, apply the gown, and then reconnect the IV. 4. Insert the client’s IV bag and tubing through the sleeve from inside of the gown first. 25. A nurse is planning care for a client with a wrist restraint. How often should a restraint be removed, the area massaged, and the joints moved through their full range? 1. Once a shift 2. Once an hour 3. Every 2 hours 4. Every 4 hours 26. A home-care nurse is assigned to care for an older adult living at home. Which is the first action the home-care nurse should employ to prevent falls by this older adult? 1. Conduct a comprehensive risk assessment. Assessment is first 2. Encourage the client to remove throw rugs in the home. 3. Suggest installation of adequate lighting throughout the home. 4. Discuss with the client the expected changes of aging that place one at risk.27. A nurse is preparing a bed to receive a newly admitted client to the hospital. Which action is most important? 1. Placing the client’s name on the end of the bed Name on bed violates the client’s right to privacy. An identification wristband must be worn for client identification. 2. Ensuring that the bed wheels are locked 3. Positioning the call bell in reach Should be done after positioning client in bed 4. Raising one side rail Should be done after positioning client in bed 28. Which is an appropriately worded goal for a client who is at risk for falling? Select all that apply. 1. “The client will be able to walk from a bed to a chair safely while hospitalized.” Realistic, specific, measurable, and has a time frame (“while hospitalized” reflects time frame of “continuously”). 2. “The client will be taught how to call for help to ambulate.” Planned intervention, not goal 3. “The client will be kept on bedrest when dizzy.” Maintaining a client on bedrest is a planned intervention 4. “The client will be restrained when agitated.” Planned intervention, not goal 5. “The client will be free from trauma.” Time frame of “free from” reflect “continuously” 30. Which intervention should a nurse implement when assisting a client to use a bedpan? Select all that apply. 1. Ensure that the bed rails are raised after the client is on the bedpan. 2. Position the rounded rim of the bedpan under the client’s buttocks. 3. Encourage the client to help as much as possible when using the bedpan.4. Raise the head of the bed to the semi-Fowler position once the client is placed on the bedpan. 5. Dust talcum powder on the rim of the bedpan before placing the bedpan under the client. 31. A nurse identifies the presence of smoke exiting the door to the dirty utility room. Place the nurse’s actions in order of priority using the RACE model. 1. Pull the fire alarm. 2. Close unit doors and windows. 3. Shut the door to the utility room. 4. Provide emotional support to agitated clients. 1. Pull the fire alarm. 3. Shut the door to the utility room. 2. Close unit doors and windows. 4. Provide emotional support to agitated clients. 32. Which clinical manifestation indicates that a further nursing assessment is necessary to determine if the client is having difficulty swallowing? Select all that apply. 1. __X__ Debris in the buccal cavity 2. __X__ Coughing episodes 3. __X__ Noisy breathing 4. __X__ Slurred speech 5. __X__ Drooling 33. A male client is admitted to ambulatory care for a bilateral herniorrhaphy. A nurse on the unit interviews the client, obtains the client’s vital signs, and reviews the primary health-care provider’s prescriptions. Which should the nurse do first?1. Contact the operating suite and inform them of the client’s latex allergy. Should be performed immediately after the priority intervention 2. Ensure the client’s allergy band includes the client’s identified allergies. 3. Notify the primary health-care provider of the client’s elevated vital signs. Should be documented and reported but not priority at this time 4. Share the information about the client’s anxiety with health team members. 34. A nurse is planning care for a client who requires bilateral arm restraints because the client is delirious and attempting to pull out a urinary retention catheter. Which information is important to consider when planning care for this client? Select all that apply. 1. _____ Use of restraints adequately prevents injuries. Statement is not true. Injuries and falls can occur if restraints are not applied appropriately. 2. __X__ Reasons for use of restraints must be clearly documented. 3. _____ Most clients recognize that restraints contribute to their safety. Statement is not true. Clients resist the use of restraints and are usually mentally or emotionally incompetent to understand their necessity or benefits. 4. _____ Restraints need a health-care provider’s prescription before application. 5. __X__ Laws permit the use of restraints when specific guidelines are followed. 36. An adult client consistently tries to pull out a nasogastric tube. As a last resort to maintain integrity of the tube and client safety, the nurse obtains a prescription for a restraint. Which type of restraint is appropriate in this situation? Select all that apply. 1. _____ Mummy restraint Usually for an infant or very young child during a procedure2. __X__ Elbow restraint 3. _____ Jacket restraint Usually to keep a person from falling out of bed while not immobilizing the extremities 4. __X__ Wrist restraint 5. __X__ Mitt restraint 37. A nurse uses the Get Up and Go test to assess a client for weakness, poor balance, and decreased flexibility. Place the following actions in the order in which they should be implemented when employing the Get Up and Go test. 4. Ask the client to sit in a chair. 5. Ask the client to stand. 2. Ask the client to close the eyes. 3. Ask the client to open the eyes. 1. Ask the client to walk 10 feet and then to return to the chair. 38. Which action is important when the nurse uses a stretcher? Select all that apply. 1. Raising the bed above the level of the stretcher when transferring a client from the stretcher to a bed Keep bed lower, not higher 2. Guiding the stretcher around a turn by leading with the end with the client’s head Client’s head area should not have swivel wheels 3. Ensuring that the client’s head is at the end with the swivel wheels Client’s feet should be at swivel wheels 4. Pulling the stretcher on the elevator with the client’s feet first Client should be moved into an elevator head first, not feet. 5. Pushing the stretcher from the end with the client’s head39. Which human response to illness alerts the nurse that a client is at risk for aspiration during meals? Select all that apply. 1. _____ Bulimia 2. __X__ Lethargy 3. _____ Anorexia 4. __X__ Stomatitis An inflammation of the mucous membranes of the mouth (stomatitis) may result in dysphagia and increase risk of aspiration. 5. __X__ Dysphagia CHAPTER 4 MEDICATION ADMINISTRATION 249 1. A nurse instructs a client to close the eyes gently after the administration of eyedrops. Which rationale for this instruction should the nurse explain to the client? 1. Limits corneal irritation Instilling medication into the conjunctival sac prevents trauma of drops falling on cornea. 2. Forces excess medication from the eyes 3. Disperses the medication over the eyeballs Closing eyes moves the medication over the conjunctiva and the eyeball and helps ensure an even distribution of medication. 4. Prevents medication from entering the lacrimal duct Gentle pressure over the inner canthus for 1 min after administration prevents medication from entering the lacrimal duct. 2. How often should “docusate sodium 100 mg PO bid” be given?1. Three times a day 2. Two times a day 3. Every other day 4. At bedtime 3. A nurse is preparing to reconstitute a medication in a multiple-dose vial. Which is the most essential step in the preparation of this medication? 1. Instilling an accurate amount of diluent into the vial Required amount of diluent must be followed exactly in a multiple-dose formulation to ensure accurate dosage preparation. The diluent for a single-dose formulation must also be measured exactly. 2. Using a filtered needle when drawing up the medication from the vial A filtered needle should be used when drawing up fluid from an ampule, not a vial it prevents shards of glass from entering the syringe. 3. Instilling air into the vial before withdrawing the reconstituted solution Advisable practice, but not as important as administering an accurate dose 4. Wiping the rubber seal of the vial with alcohol before and after each needle insertion Rubber seal must be wiped with alcohol before, not after, needle insertion 4. Which characteristic is associated with a subcutaneous injection of 5,000 units of heparin? 1. 3-mL syringe Most doses of heparin are less than 1-mL 2. 22-gauge needle 22-guage is too large; should be a 25- or 26- gauge needle 3. 11⁄2-inch needle length Too long 4. 90-degree angle of insertion A ½-inch-length needle inserted at a 90-degree angle will ensure that the heparin is inserted into subQ tissue. 5. A home-care nurse observes the spouse of a client inserting a rectal suppository into the client. Which behavior indicates that the nursemust provide further teaching about suppository administration? 1. Lubricates the tip of the suppository 2. Inserts the suppository while wearing a glove 3. Inserts the suppository while the client bears down Bearing down increases intra-abdominal pressure, which impedes the insertion of the suppository. The client should be instructed to relax and breathe deeply and slowly while inserting suppository. 4. Places the suppository a finger length into the rectum In an adult, a suppository should be inserted 4in to ensure it is beyond the internal sphincter. 6. A primary health-care provider prescribes a medication that must be administered via the intramuscular route. Which site should the nurse eliminate from consideration because it has the highest potential for injury when administering an intramuscular injection? 1. Vastus lateralis Preferred site for infants 7 months of age and younger 2. Rectus femoris Appropriate site for adults 3. Ventrogluteal Preferred site in adults and children 4. Dorsogluteal Highest risk for injury because of close proximity of sciatic nerve, blood vessels and bone 7. Which information about a parenteral medication indicates that the nurse should use a filtered needle when preparing the medication? 1. Has to be reconstituted Reconstitution occurs within a closed vial and does not require a filtered needle. 2. Is supplied in an ampule Top of an ampule must be snapped off at its neck to access the fluid. A filtered needle prevents glass particles from being drawn into the syringe. 3. Appears cloudy in the vial This indicates contamination 4. Is to be mixed with another medication Not necessary to use a filtered needle when mixing medications. 8. Which should the nurse use when administering a subcutaneous injection?1. 5-mL syringe SubQ injections should not exceed 1mL, but a 3-mL, not a 5-mL, syringe is acceptable for subQ injections. 2. 25-gauge needle SubQ injections should use a 25- to 29-gauge needle 3. Tuberculin syringe Volume of a tuberculin syringe is only 1mL. For most subQ injections, a syringe can accommodate up to 3mL is preferred to facilitate handling a syringe. 4. 11⁄2-inch-long needle Appropriate for IM not subQ 9. When the nurse brings a pill to a client, the client is unable to hold the paper cup with the medication. Which should the nurse do? 1. Use the cup to introduce the pill into the client’s mouth. Maintains medical asepsis while assisting client 2. Crush the pill and mix it with a small amount of applesauce. Done for dysphagia clients 3. Have the primary health-care provider prescribe the liquid form of the drug. 4. Put the pill into the client’s hand and have the client self-administer the pill. 10. Which route is inappropriate for a topical medication? 1. Intradermal An intradermal injection is inserted below, not on top of, the epidermis. 2. Bladder 3. Rectum 4. Vagina 11. A nurse holds a bottle with the label next to the palm of the hand when pouring a liquid medication. Which is the rationale for this action? 1. Prevent soiling of the label by spilled liquid 2. Conceal the label from the curiosity of others3. Ensure accuracy of the measurement of the dose 4. Guarantee the label is read before pouring the liquid 12. A primary health-care provider prescribes a medicated powder to be applied to a client’s lower leg. Which is most essential for the nurse to do when applying the medicated powder? 1. Apply a thin layer in the direction of hair growth. This action is done with lotions, creams, or ointments. 2. Protect the client’s face with a small towel. 3. Dress the area with dry sterile gauze. 4. Ensure that the skin surface is dry. Moisture harbors microorganisms 13. A nurse must administer a medication that is supplied in an ampule. Which should the nurse do first to access the ampule? 1. Break the constricted neck using a barrier. A barrier like a commercially manufactured ampule opener, gauze, or an alcohol swab, should be used to protect the nurse’s hands. 2. Wipe the constricted neck with an alcohol swab. The rubber seal of the vial should be wiped with alcohol, not the neck. 3. Insert the needle into the center of the rubber seal. Piercing a rubber seal is done with a vial, not an ampule. 4. Inject the same amount of air as the fluid to be removed. Injecting air is done with a vial not an ampule. 14. A nurse must administer a medication into the ear of an adult. Which should the nurse do to limit client discomfort when administering the eardrops? 1. Warm the solution to body temperature. 2. Place the client in a comfortable position. A comfortable position may not be the side-lying position which is required for administration of an ear drop and must be maintained for 2-3min. 3. Pull the pinna of the ear upward and backward. This action facilitates flow of medication toward eardrum in adult; not limit discomfort. 4. Instill the fluid in the center of the auditory canal. Drops should be directed along the side of the ear canal.15. A nurse instructs a client to inhale deeply and hold each breath for a second when using a hand-held nebulizer. The client asks, “Why do I have to hold my breath?” Which information should the nurse include in the response to the client’s question? 1. “It prolongs treatment.” 2. “It limits hyperventilation.” 3. “It disperses the medication.” A pause at the height of inspiration will promote distribution and absorption of the medication before exhalation begins. 4. “It prevents bronchial spasms.” Slow inhalations and exhalations with pursed lips help prevent bronchial spasms. 16. Which abbreviation indicates that the primary health-care provider wants a medication administered before meals? 1. pc After meals 2. ac Before meals 3. PO By mouth 4. OD Abbreviation for right eye 17. A home-care nurse is helping a client with short-term memory loss with how to remember to take multiple drugs throughout the day. Which should the nurse do when teaching this client? 1. Suggest that the client wear a watch with an alarm. 2. Ask a family member to call the client when medications are to be taken. 3. Design a chart of the medications the client takes each day during the week. 4. Instruct the client to put medications in a weekly organizational pill container. 18. Which action should be implemented by the nurse when a medication is delivered by the Z-track method?1. Use a special syringe designed for Z-track injections. No special syringe for Z-track. Barrel of syringe must be large enough to accommodate volume of solution to be injected (usually 1 to 3 mL) and usually 1 ½ inch needle. 2. Pull the skin laterally away from the injection site before inserting the needle. 3. Administer the injection in the muscle on the anterolateral aspect of the thigh. Vastus lateralis may cause discomfort; Ztrack injections are tolerated more when well-developed gluteal muscles are used. 4. Insert the needle in a separate spot for each dose on a Zshaped grid on the abdomen. Z represents the zig zag pattern of the needle track that results when the skin traction and needle are simultaneously removed. 19. A nurse must reconstitute a powdered medication. Which action should the nurse implement? 1. Keep the needle below the initial fluid level as the rest of the fluid is injected. This action will create excessive bubbles that can interfere with complete reconstitution or result in bubbles being drawn into the syringe. 2. Instill the solvent that is consistent with the manufacturer’s directions. 3. Score the neck of the ampule before breaking it. Reconstitution occurs in a vial not an ampule 4. Shake the vial to dissolve the powder. Vial should be rotated between the hands to facilitate reconstitution, not shaking 20. A nurse is preparing to administer a tablet to a client. When should the nurse remove the medication from its unit dose package? 1. Outside the door to the client’s room 2. When next to the client’s bed 3. In the medication room 4. At the medication cart21. A client has a prescription for an analgesic. Which nursing action is appropriate when administering this medication? 1. Reassess drug effectiveness every 8 hours. Client should be assessed every 1-2h. 2. Follow the prescription exactly for the first 24 hours. 3. Seek a new prescription after two doses that do not achieve a tolerable level of relief. Two doses provide enough time to evaluate the effectiveness of a medication for pain. 4. Ask the primary health-care provider to prescribe another medication for breakthrough pain. 22. The primary health-care provider prescribes a troche. In which part of the body should the nurse administer the troche? 1. Ear 2. Eye 3. Mouth A troche, a lozengelike tablet, dissolves slowly in the mouth in the buccal cavity to provide a localized effect. 4. Rectum 23. A nurse teaches a client about taking a sublingual nitroglycerin tablet. Which part of the body identified by the client indicates that the client understands the teaching? 1. “On my skin.” 2. “Inside my cheek.” 3. “Under my tongue.” 4. “In my eye on the lower lid.” 24. A nurse plans to administer a bolus dose of a medication via a currently running IV infusion. Which should the nurse do first? 1. Use a volume-control infusion set with microdrip tubing. Volume of fluid of a bolus dose is too small to necessitate a volume-control infusion set. 2. Ensure that it is compatible with the IV solution being infused. 3. Pinch the tubing above the infusion port while instilling the bolus. Pinching the tube is not done first. Pinching is done immediately before and while instilling the medication to ensure that the medication flows toward the client, rather than in the oppositedirection up the tubing. 4. Instill it into a 50-mL bag of normal saline and infuse it via a secondary line. This is done for an intermittent IV infusion over a 30- 90 min period rather than for an IV bolus dose administered over 1- 5min. 25. A nurse is administering an intradermal injection. At which angle should the nurse insert the needle? 1. 90-degree angle Best for IM 2. 45-degree angle Appropriate for subQ when needle is 1 inch long 3. 30-degree angle Too deep for ID, a wheal will not form 4. 15-degree angle An intradermal injection is administered by inserting a needle at a 10-15 degree angle through the skin with the bevel of the needle facing upward toward the skin. The small volume of medication instilled just below the epidermis causes the formation of a wheal. 26. A nurse plans to administer a 3-mL intramuscular injection. Which muscle is the least desirable to use for the administration of this medication? 1. Deltoid This site is most appropriate for 1-mL injection. 2. Dorsogluteal 3. Ventrogluteal Best 3-mL IM location 4. Vastus lateralis 27. A nurse is preparing to administer a subcutaneous injection of insulin. Which site should the nurse use to best promote its absorption? 1. Upper lateral arms Rate of absorption at this site is slower than at the preferred site for insulin administration. 2. Anterior thighs Thighs and buttocks have the slowest absorption rate. 3. Love handles Areas around the waist lateral to the abdomen are the preferred sites for administration of insulin.4. Upper chest 28. A client has a prescription for a vaginal cream. Which should the nurse use when placing the cream into the client’s vaginal canal? 1. A finger For suppository not cream 2. A gauze pad 3. An applicator 4. An irrigation kit 29. A primary health-care provider prescribes a medication that must be administered transdermally. Which information about the route of administration does the nurse understand is related to a drug prescribed to be administered transdermally? 1. Inhaled into the respiratory tract 2. Dissolved under the tongue 3. Absorbed through the skin 4. Inserted into the rectum 30. Which should the nurse do to limit discomfort when administering an injection to an adult? 1. Pull back on the plunger before injecting the medication. 2. Apply ice to the area before the injection. Applying ice is contraindicated because it causes vasoconstriction which limits absorption of the medication. 3. Pinch the area while inserting the needle. Pinching skin aids in needle insertion when administering a subQ injection, but does not limit discomfort of an injection. 4. Inject the medication slowly. 31. A nurse is preparing to draw up medication from a vial. Which action should the nurse implement first? 1. Ensure that the needle is firmly attached to the syringe.2. Rub vigorously back and forth over the rubber cap with an alcohol swab. Top needs to be swiped, not rubbed back and forth. 3. Inject air into the vial with the needle bevel below the surface of the medication. Injecting air below surface of solution should be avoided because it causes bubbles that may interfere with the drawing up of an accurate volume of solution 4. Instill slightly more air than the volume of medication to be withdrawn from the vial. Excess air causes bubbles 33. A primary health-care provider prescribes a medicated cream for a client to be administered topically to an area of excoriated skin. Place the following steps in the order in which they should be implemented. 1. Don clean gloves. 4. Cleanse the skin gently with soap and water and pat dry. 3. Warm the tube of medication before application. 5. Don sterile gloves and apply a thin layer of cream to the desired area. 2. Evaluate the results of the cream on the skin. 34. The instructions with a medication state to use the Z-track method of administration. Which action should the nurse implement that is specific to this procedure? Select all that apply. 1. _____ Pinch the site throughout the procedure. Skin should be pulled laterally 1 to 1 ½ inches away from injection site. 2. _____ Massage the site after the needle is removed. Massage is contraindicated because it will force medication back up the needle track which may result in tissue irritation or staining. 3. __X__ Add 0.1 to 0.3 mL of air after drawing up the correct dosage. Injection of small amount of air helps keep medication deeplyseated in the muscle 4. _____ Remove the needle immediately after the medication is injected. Removal of needle should be delayed 10 seconds to allow medication to be dispersed and absorbed. 5. _____ Inject the medication quickly, at a rate of 1 second per mL of solution. Should be injected slowly at a rate of 10 seconds per mL of solution. 35. A primary health-care provider prescribes benztropine (Cogentin)1.5 mg PO STAT. Benztropine is available in 0.5-mg scored tablets. How many tablets should the nurse administer? Record your answer using a whole number. Answer: 3 tablets. 36. Which routes are unrelated to the parenteral administration of medications? Select all that apply. 1. __X__ Buccal 2. _____ Z-track 3. __X__ Sublingual 4. _____ Intravenous 5. _____ Intradermal 37. Which intervention is uniquely related to the administration of an intradermal injection? Select all that apply. 1. _____ Using the air-bubble technique Air-bubble or air-lock technique can be used for IM 2. __X__ Circling the injection site with a pen Indicates area that must be evaluated; generally site is assessed 72h after ID injection 3. _____ Pinching the skin during needle insertion Appropriate for subQ 4. __X__ Inserting the needle with the bevel upward Used only for ID 5. _____ Massaging the area after the fluid is instilled Contraindicates dispersing medication beyond intended injection site39. A nurse is assessing a client to determine if it is appropriate to administer a prescribed medication via the oral route. Which information indicates that the nurse should ask the primary healthcare provider for a change in route? Select all that apply. 1. _____ Nausea 2. __X__ Unconsciousness Nothing that requires swallowing should ever be placed into the mouth of an unconscious client because of the risk for aspiration. 3. _____ Gastric suctioning Gastric suctioning can be interrupted for 20-30 min after medication as been instilled via a NGT 4. __X__ Emergency situation In an emergency, drug is best administered IV, rather than orally 5. _____ Difficulty swallowing Nursing interventions such as positioning, mixing a crushed medication, and dissolving a medication in a small amount of fluid can be employed to facilitate ingestion of medication. 40. A primary health-care provider prescribes a medication via a transdermal patch. Place the following steps in the order in which they should be implemented when administering this medication. 3. Wear clean gloves throughout the procedure. 1. Remove the previous patch. 2. Contain and dispose of the used patch. 6. Wash and dry the skin after removal of the used patch. 5. Apply a new patch to a different section of the skin. 4. Write the date, time, and your initials on the patch.41. A primary health-care provider prescribes an oral medication for a client. The nurse identifies that the client is having some difficulty swallowing. What should the nurse plan to do? Select all that apply. 1. Crush tablets that are crushable and mix with a small amount of applesauce. 2. Have the client hyperextend the neck slightly when swallowing. Should slight flex, not hyperextend 3. Give water before, during, and after medication administration. 4. Stroke under the chin over the larynx. Encourages laryngeal elevation, which facilitates swallowing. 5. Have the client use a straw. This increases risk of aspiration. 42. The primary health-care provider prescribes 500 mL of D5W with 10 mEq of KCl to be administered over 10 hours. The IV tubing states that each mL delivers 60 gtts. To what rate per minute should the nurse adjust the flow rate of the intravenous solution? Record your answer using a whole number. (500 total vol to be infused x 60 drop factor of IV tubing) / (60 min within an hr x 10 # of hrs prescribed) Answer: 50 gtts/min. 43. A primary health-care provider prescribes nose drops to be administered twice a day. Which should the nurse do when instilling the nose drops? Select all that apply. 1. Tell the client not to sniff the medication once administered. Avoiding sniffing the nose drops after administration allows medication to reach desired areas (ethmoid and sphenoid sinuses) via gravity. 2. Place the client in the supine position with the head tilted backward. Supine ensures gravity will promote flow of medication to the nasopharynx. Client should remain in supine for 5 minutes.3. Pinch the nares of the nose together briefly after the drops are instilled. 4. Instruct the client to blow the nose 5 minutes after the drops are instilled. 5. Insert the drop applicator 1⁄2 inch into the nose toward the base of the nasal cavity. Nose drops should be directed toward the midline of the ethmoid bone, with the dropper held ½ inch above the nares. 44. Which route is associated with the administration of a suppository? Select all that apply. 1. _____ Ear 2. _____ Nose 3. _____ Mouth 4. __X__ Vagina 5. __X__ Rectum 45. A primary health-care provider prescribes a monthly intramuscular injection of fluphenazine decanoate 37.5 mg. The medication is available as 25 mg/mL. How much solution of fluphenazine should the nurse administer? Record your answer using one decimal place. Answer: 1.5 mL. 46. A nurse is to administer an eye irrigation to a client’s right eye. Which should the nurse do? Select all that apply. 1. __X__ Direct the flow of solution from the inner to the outer canthus. 2. _____ Irrigate with a bulb syringe held several inches above the eye.3. __X__ Expose the conjunctival sac and hold open the upper lid. 4. _____ Don sterile gloves before beginning the procedure. Medical, not surgical, asepsis is required for this procedure. 5. _____ Position the client in a right lateral position. Client should be placed in a sitting or back-lying position with the head tilted toward the affected eye. 47. A primary health-care provider prescribes medicated eardrops for a client. Place the following steps in the order in which they should be implemented after cleaning the client’s ear. 5. Warm the refrigerated eardrops to room temperature by holding the container in the palm of a hand for several minutes. 4. Position the client in the side-lying position with the affected ear facing toward the ceiling. 2. Pull up and back on the cartilaginous part of the pinna gently. 3. Place the drops on the side of the ear canal without touching the canal with the dropper. 1. Release the pinna and gently press on the tragus several times. 48. A primary health-care provider prescribes a rectal suppository for an adult client. Which action should the nurse implement when administering the rectal suppository? Select all that apply. 1. __X__ Lubricate the medication before insertion. 2. _____ Warm the medication equal to body temperature. Warming medication will cause it to melt. 3. __X__ Instruct the client to take deep breaths through the mouth. 4. _____ Insert the medication just inside the rectum’s external sphincter. Rectal suppositories should be inserted 3 inches into the rectal canal past the rectum’s internal sphincter of an adult. This can be accomplished by using the full length of a lubricated, gloved index finger to place the suppository. 5. _____ Place the client in the prone position to administer the medication. Client should be placed in the left-lateral or left-Simsposition to take advantage of the anatomical curve of the rectum and sigmoid colon. 49. A primary health-care provider prescribes an IV infusion of 1,000 mL 0.9% sodium chloride to be followed by 1,000 mL D5W with 20 mEq of potassium chloride. The infusion is to be administered at 125 mL/hr. The drop factor of the IV tubing states 10 drops/mL. To how many drops per minute should the nurse set the IV infusion? Record your answer using a whole number. (Total # to be infused x drop factor) / Total time in minutes (125 vol to be infused in 1 h x 10 drop factor of IV tube) / (60 [# of min in 1h]) Answer: 21 gtts/min. 50. A primary health-care provider prescribes a liquid medication that has an unpleasant taste for a school-age child. What should the nurse do to facilitate administration of this medication? Select all that apply. 1. _____ Mix it with the child’s favorite food. 2. _____ Teach that the taste only lasts a short time. 3. __X__ Give an ice pop just before giving the medication. 4. _____ Have a parent administer the medication if present. 5. __X__ Offer the child the choice of a spoon, needleless syringe, or dropper. 52. A nurse is interviewing a newly admitted client in the process of completing a nursing admission history and physical assessment. Which information should be included in a medication reconciliation form? Select all that apply. 1. __X__ Vitamins 2. _____ Drug allergies Drug allergies are documented on a health history, not on the drug reconciliation form. 3. __X__ Food supplements 4. __X__ Over-the-counter herbs5. __X__ Prescribed medications 53. Which action should the nurse implement when administering an intramuscular injection into the ventrogluteal site? Select all that apply. 1. _____ Use a 1-inch needle. For IM, use a 1 ½ inch needle. 2. _____ Use a 25-gauge needle. A 22-gauge needle is for IM. A 25- gauge needle is generally for subQ. 3. _____ Insert the needle at a 45-degree angle. IM injection should be 90-degree. For subQ, injection with 1-inch needle at 45-degree is appropriate. 4. _____ Aspirate before instilling the medication. Aspiration is recommended before instilling the medication in the gluteus maximus site not ventrogluteal, vastus lateralis and rectus femoris. 5. __X__ Massage the insertion site after needle removal. Massage promotes dispersement of the medication. 54. A primary health-care provider prescribes a vaginal suppository for a client. The nurse obtains the suppository, pulls the curtain around the client’s bed, encourages the client to void, provides perineal care, and then dons a new pair of clean gloves. Place the following steps in the order in which they should now progress to complete the administration of the vaginal suppository. 2. Position the client in the dorsal recumbent position. 1. Drape the client, exposing only the vaginal area. 4. Lubricate the suppository and the nurse’s index finger with a water-soluble jelly. 5. Insert the suppository downward and backward using the full length of the index finger. 3. Encourage the client to remain in the supine position for 10 to 20 minutes.55. A primary health-care provider prescribes a liquid oral medication for a client. Which action should the nurse implement when administering this medication? Select all that apply. 1. Vigorously shake the liquid before pouring a dose. 2. Measure oral liquids in a calibrated medication cup at eye level. 3. Pour liquids with the label facing away from the palm of the hand. Liquids should be poured with the label against the palm of the hand to prevent the liquid from dipping on and obscuring the label 4. Place an opened top of a container on a surface with the inside lid facing up. Prevents contamination 5. Use a needleless syringe to measure an oral liquid less than 5 mL and transfer it to a medication cup. Ensures accuracy 57. A primary health-care provider prescribes two oral medications for a client with a nasogastric tube on low continuous suction. Which action should the nurse implement when administering this medication? Select all that apply. 1. Give each medication separately. If the tube used to administer a medication via a NGT becomes accidentally disconnected during administration, the nurse can identify the approximate volume of the one medication that was lost when reporting the event to the HCP. 2. Follow medication administration with 100 mL of free water. Oral medication via a NGT should be followed by 30 mL of tap water, not 100 mL of free water. 3. Crush crushable tablets into a fine powder and mix with 30 mL of warm water. Dissolves medication and prevents clogging the enteral tube 4. Shut off nasogastric tube suctioning for 30 minutes after medication administration. Enhances medication absorption in stomach 5. Ensure nasogastric tube placement by instilling 30 mL of air while auscultating over the epigastric area for a “whooshing” sound. Measuring pH of gastric aspirate is more accurate58. An older adult is transported via ambulance to the emergency department of the hospital after being found unconscious on the living room floor by a family member. The client regains consciousness and tells the nurse that everything went blank after the client stood up abruptly from a lounge chair. The client is diagnosed with dehydration and is admitted for observation and rehydration therapy. The nurse performs a routine client assessment 18 hours after initiation of the IV therapy. What should the nurse do first after reviewing the client’s clinical record and assessing the client? 1. Administer oxygen via a nasal cannula. This should be done to increase oxygen but not first priority. 2. Slow the rate of the intravenous infusion. Client is exhibiting signs of fluid volume overload and pulmonary edema. The IV infusion should be slowed to 15 to 30 mL per hour. 3. Elevate the head of the bed to the semi-Fowler position. This should be done to promote respiration but not first priority. 4. Notify the primary health-care provider of the client’s status. Should be done eventually, but client requires immediate intervention. 59. A primary health-care provider prescribes a unit of packed red blood cells for a client with a low hemoglobin level. Which action should be implemented by the nurse when administering this transfusion? Select all that apply. 1. Adjust the flow rate to 20 drops per minute for the first 15 minutes. 2. After 15 minutes, vital signs should be taken every 15 to 30 minutes. 3. Ensure that an 18-gauge needle is used for administering the blood transfusion. Standard precaution of 18-gauge needle for blood transfusions 4. Discontinue the blood transfusion if it extends beyond 4 hours after its initiation. 5. Stay with the client for 15 minutes after initiating the blood transfusion while taking vital signs every 5 minutes. Usually first 15 minutes oftransfusion reaction; clinical indicators include back pain, chills, itching, or shortness of breath. CHAPTER 5 HYGIENE 297 1. A nurse is bathing a client who has a fever. Why should the nurse use tepid bath water for this procedure? 1. Increases heat loss 2. Removes surface debris 3. Reduces surface tension of skin 4. Stimulates peripheral circulation 2. A nurse must make the decision to give a client a full or partial bed bath. Which criterion is most important for the basis of this decision? 1. Primary health-care provider’s prescription for the client’s activity2. Immediate need of the client A total client assessment with an analysis of the data identifies the needs of the client and the appropriate intervention to meet those needs. 3. Time of client’s last bath 4. Client preference 3. A client has had a nasogastric tube to decompress the stomach for 3 days and is scheduled for intestinal surgery in the morning. For which of the following is the client at the highest risk? 1. Physical injury 2. Ineffective social interaction 3. Decreased nutritional intake 4. Altered oral mucous membranes 4. A client is incontinent of urine and stool. For which client response should the nurse be most concerned? 1. Impaired skin integrity Fecal material contains enzymes that erode the skin and urine is an acidic fluid that macerates the skin. 2. Altered sexuality 3. Dehydration Incontinence is unrelated to dehydration. 4. Confusion 5. A nurse is giving a client a bed bath. Which nursing action is most important? 1. Lower the 2 side rails on the working side of the bed. 2. Ensure that the bathwater is at least 110°F. Temperature of bathwater should be between 110-115 F to promote comfort, dilate blood vessels, and prevent chilling. 3. Fold the washcloth like a mitt on the hand. 4. Raise the bed to the highest position. 6. A nurse plans to give a client a back rub. Which product should the nurse use for this intervention?1. Baby powder 2. Rubbing alcohol 3. Moisturizing lotion 4. Antimicrobial cream 7. A nurse changes the sheets and pillowcase of a bed while the client sits in a chair. Of the options presented, which is the most important nursing action when changing bed linens? 1. Ensuring the hem of the bottom sheet is facing the mattress 2. Arranging the linen in the order in which it is to be used 3. Shifting the mattress up to the headboard of the bed 4. Checking the soiled bed linens for personal items 8. A nurse is responsible for providing hair care for a client. Which should the nurse do to distribute oil evenly along hair shafts? 1. Brush the hair from the scalp toward the hair ends. 2. Lift opened fingers through the length of the hair. 3. Apply a hydrating conditioner to wet hair. 4. Comb hair with a fine-toothed comb. Fine-toothed comb should not be used for daily grooming because it can injure the scalp, damage the hair shaft and split ends of hair. 9. Which condition identified by the nurse places a client at the highest risk for impaired self-care when toileting? 1. Amputation of a foot 2. Early dementia 3. Fractured hip 4. Pregnancy 10. A client asks the nurse, “Why do I have to use mouthwash if I brush my teeth?” Which rationale about the use of all mouthwashes should the nurse include when responding to this question? 1. Reduces offensive mouth odors2. Minimizes the formation of cavities 3. Softens debris that accumulates in the mouth 4. Destroys pathogens that are found in the oral cavity 11. A nurse is planning to shampoo the hair of a client who has a prescription for bedrest. Which should the nurse do first? 1. Wet hair thoroughly before applying shampoo. 2. Encourage the use of dry shampoo. 3. Brush the hair to remove tangles. 4. Tape eye shields over both eyes. 12. A client just had perineal surgery. Which type of bath should the nurse expect to be prescribed for this client? 1. Sponge bath Sponge bath is given to reduce a client’s fever through heat loss via conduction and vaporization, but does not need HCP’s prescription. 2. Sitz bath Sitz bath immerses a client from the mid-thighs to the iliac crests or umbilicus, in a special tub, or the client sits in a basin that fits onto the toilet seat so the legs and feet remain out of water. A sitz bath requires a HCP’s prescription because it is a method of applying local heat to the perineal area. 3. Tub bath Therapeutic baths 4. Bed bath Bed bath is indicated for clients with restricted mobility or decreased energy 13. A nurse plans to assist a client who has impaired vision with a bed bath. Which is the most appropriate nursing intervention to facilitate bathing for this client? 1. Providing the client with a liquid bath gel rather than a bar of soap 2. Giving the client an adapted toothbrush to use when brushing the teeth 3. Checking the client’s ability to give self-care through a crack in the curtain 4. Ensuring the client can locate bathing supplies placed on the overbed table14. A nurse plans to meet the hygiene needs of a hospitalized client who is experiencing hemiparesis because of a brain attack (cerebrovascular accident). Which is an appropriate nursing intervention? 1. Assisting the client to bathe as needed Hemiparesis is a weakness on one side of the body that can interfere with the performance of ADLs. Encourage client to do as much as possible. 2. Giving total assistance with a complete bath 3. Providing minimal supervision during the bath 4. Encouraging a family member to bathe the client 15. A nurse is making an occupied bed. Which nursing action is most important? 1. Securing top linens under the foot of the mattress and mitering the corners 2. Ensuring that the client’s head is supported and is in functional alignment 3. Fan-folding soiled linens as close to the client’s body as possible 4. Placing the bed in the horizontal position 16. A nurse must bathe the feet of a client with diabetes. Which should the nurse do before bathing this client’s feet? 1. File the nails straight across with an emery board. 2. Teach that daily foot care is essential for adequate hygiene. 3. Ensure a provider’s prescription for hygienic foot care is obtained. 4. Assess for additional risk factors that may contribute to localized problems. 17. Which should be the nurse’s first intervention after removing a bedpan from under a debilitated client who has just had a bowel movement? 1. Document results. 2. Provide perineal care.3. Reposition the client. 4. Cover the client with the top linens. Top linens should not have been removed during this procedure. 18. Which common problem with the hair should the nurse anticipate when clients are on complete bedrest? 1. Dry hair 2. Oily hair 3. Split hair 4. Matted hair 19. A nurse is helping a client who has right hemiparesis to get dressed. Which action should the nurse implement? 1. Put the gown’s right sleeve on first. Put right sleeve of gown on weak extremity first 2. Keep the client in an open-backed gown. 3. Encourage the client to dress independently. 4. Leave the right sleeve off while adjusting the tie at the neck. 20. A cognitively impaired client is incontinent of loose stools. Which action should the nurse implement to help the client prevent skin breakdown? 1. Wash the buttocks with strong soap and water. 2. Bathe immediately after a bowel movement. 3. Apply Talcum powder after the bath. Talcum powder is unsafe because it is a respiratory irritant. 4. Put a pad under the buttocks. Placing a pad under buttocks will not keep stool off the skin. 21. A nurse covers the client with a cotton blanket during a bath. Which of the following mechanisms of heat loss is prevented by the nurse’s action? 1. Vasodilation Vasodilation increases blood flow to surface of the skin promoting heat loss 2. Conduction Conduction is the transfer of heat between two objects in physical contact3. Convection Convection is the transfer of heat by movement of air along a surface, preventing heat loss. 4. Diffusion 22. A client who has a fever experienced significant diaphoresis during the night. The client states, “I am tired, and I just want to sleep this morning.” Which should the nurse do regarding bathing the client? 1. Wait until the client feels better. 2. Postpone bathing until the afternoon. 3. Give a bed bath with complete assistance. The physical need to bath for diaphoresis needs to be explained to client and then give bed bath with complete assistance. 4. Consult with the primary health-care provider before providing care. 23. A nurse gives a bedbound client a bed bath. Which is the primary reason why the nurse provides hygiene care to this client? 1. Support a sense of well-being by increasing self-esteem. 2. Promote circulation by stimulating peripheral nerve endings. 3. Remove excess oil, perspiration, and bacteria by mechanical cleansing. 4. Exercise muscles by contraction and relaxation of muscles when bathing. 24. Which human response, identified by the nurse, best supports the concern that a client has a reduced capacity to provide for activities of daily living? 1. Presence of joint contractures 2. Inability to wash body parts Human response to ADL 3. Postoperative lethargy 4. Visual disorders 25. When giving a client a bed bath, a nurse washes the client’s extremities from distal to proximal. Which is the rationale for this nursing action?1. Decreases the chance of infection 2. Facilitates removal of dry skin 3. Stimulates venous return 4. Minimizes skin tears 26. During oral care, the nurse identifies a patch of dried food and debris adhered to the hard palate of the client’s mouth. Which word should the nurse use when documenting this condition? 1. Sordes Accumulation of food, epithelial elements, dired secretions and microorganisms 2. Plaque Invisible film that adheres to enamel surface of teeth 3. Glossitis Inflammation of tongue 4. Stomatitis Inflammation of oral mucosa 27. A nurse is teaching a client about how many times a day it is necessary to brush the teeth to achieve effective dental hygiene. According to the American Dental Association, how many times a day should the nurse teach the client to brush the teeth? 1. 6 2. 4 3. 3 4. 2 28. A nurse is providing hygiene to a client with peripheral neuropathy. Which action should the nurse implement? 1. Seek a prescription for foot care. Providing foot care is within the scope of nursing practice2. File the toenails straight across the nail. Should be provided by podiatrist for client with peripheral neuropathy 3. Wash the feet with lukewarm water and dry well. 4. Apply moisturizing lotion to the feet, especially between the toes. 29. Which nursing intervention most requires the nurse to consider the concept of intimate space? 1. Providing a bed bath 2. Obtaining the vital signs 3. Performing a health history 4. Ambulating the client down the hall 30. Which nursing action is common to both a bed bath and a tub bath? Select all that apply. 1. _____ Obtaining a prescription from the primary health-care provider 2. _____ Helping the client wash body parts that cannot be reached 3. _____ Exposing just the part of the body being washed During a tub bath or a shower the entire body is exposed 4. _____ Providing for privacy throughout the bath 5. _____ Ensuring that the call bell is in reach 31. A nurse plans to provide a client with a partial bath. Place the following steps in the order in which the nurse should proceed. 2. Face 3. Axilla 4. Both hands 6. Change water 1. Back 5. Genital area32. Which should the nurse implement when caring for a client who wears eyeglasses? Select all that apply. 1. _____ Encourage use of artificial tears while hospitalized. 2. _____ Store eyeglasses in a safe place when not being worn. 3. _____ Dry the lenses with a paper towel after they are washed. 4. _____ Limit the time that eyeglasses are worn in an effort to rest the eyes. 5. _____ Use warm water to clean the lenses of eyeglasses at least once a day. 33. When providing morning care for a client, the nurse identifies crusty debris around the client’s eyes. Which of the following should the nurse implement when cleaning the client’s eyes? Select all that apply. 1. _____ Wear sterile gloves. 2. _____ Use a tear-free baby soap. 3. __X__ Position the client on the same side as the eye to be cleaned. 4. __X__ Wash the eyes with cotton balls from the inner to outer canthus. Inner to outer moves debris from entering lacrimal duct 5. __X__ Use a separate cotton ball for each stroke when washing the eyes. 34. A nurse must make an unoccupied bed. Which nursing action is essential? Select all that apply. 1. _____ Position the call bell in reach. 2. _____ Place a pull sheet on top of the draw sheet. 3. __X__ Ensure that the bottom sheet is free of wrinkles. 4. __X__ Ensure that there is a toe pleat at the foot of the bed. 5. _____ Complete one side of the bed before completing the other side. 35. A nurse plans to administer a foot bath to a client who is sitting in a chair and has no contraindications for this intervention. Place the following steps in the order in which they should be implemented.1. Position a waterproof pad on the floor on which to place a basin half-filled with warm water (approximately 105°F to 110°F). 2. Don clean gloves and assist the client to position one foot in the water, verifying with the client that the water temperature is comfortable. 3. Soak each foot individually for 5 to 20 minutes, subject to the client’s tolerance, condition of the skin, and absence of a history of diabetes or peripheral vascular disease. 4. Wash each foot with rinse-free soap and clean under the nails with an orange stick. 5. Dry each foot gently, especially between the toes. 6. Apply lotion to each foot, avoiding between the toes. 36. A nurse teaches a client effective oral hygiene practices. Which of the following indicates that the teaching about preventing and removing dental plaque was understood by the client? Select all that apply. 1. __X__ Uses a nonabrasive toothpaste 2. __X__ Brushes the teeth with a toothbrush 3. __X__ Gargles with antiplaque mouthwash 4. __X__ Flosses the teeth with unwaxed floss 5. _X__ Has teeth cleaned regularly by a dental hygienist 37. A nurse is providing for the hygiene and grooming needs of an obese client who easily becomes short of breath when moving about. Which nursing intervention is important? Select all that apply. 1. _____ Administering oxygen during provision of care 2. _____ Maintaining the bed in a high-Fowler position Semi-Fowler position is preferred. 3. __X__ Assessing the client’s response to the activity Evaluating a client’s response to care allows nurse to alter care to meet client’s individual needs. 4. __X__ Bathing areas that the client cannot reach 5. _____ Providing rest periods every ten minutes38. A nurse plans to shave a male client’s facial hair with a safety razor. Which of the following should the nurse implement? Select all that apply. 1. _____ Hold the razor perpendicular to the skin. Safety razor should be held at 45 degree angle, not 90 degree angle to skin 2. _____ Use long, downward strokes with the razor. Short, gentle strokes should be used 3. _____ Shave in the opposite direction of hair growth. 4. __X__ Ensure that the client is not receiving an anticoagulant. Patient on anticoagulant should use electrical razor not safety razor 5. _____ Use a hot, wet washcloth to wrap the face before shaving. Use warm, not hot 40. A nurse is caring for a client with an excessively dry mouth. Which nursing action is important when providing mouth care for this client? Select all that apply. 1. Wearing clean gloves 2. Providing oral care every 2 hours 3. Rinsing frequently with mouthwash Mouthwash contains astringents that can injure sensitive, delicate, dry mucous membranes 4. Cleansing 4 times a day with a water pick 5. Swabbing with a sponge-tipped applicator of lemon and glycerin 41. A nurse is providing perineal care to a male client. Which should the nurse do? Select all that apply. 1. Wash the genital area with hot, sudsy water. Warm, not hot water should be used2. Wash the scrotum before washing the glans penis. Glans penis, foreskin and shaft of penis are cleaned before the scrotum. Scrotum is considered more soiled than penis because of its proximity to the rectum. 3. Wash the shaft of the penis while moving toward the urinary meatus When cleaning the shaft of penis, bathing should start at the glans penis and then proceed down the shaft toward the scrotum. 4. Wash the penis with one hand while holding it firmly with the other hand. 5. Wash the glans with a circular motion, starting at the tip and then proceeding down the shaft. 42. A school nurse teaches an adolescent who has dry skin and acne about skin care. Which statement by the adolescent indicates that the information is understood? Select all that apply. 1. _____ “I will scrub my face every day with a strong soap.” 2. _____ “I will break pustules carefully after washing my face.” 3. _____ “I will apply an oil-based emollient after washing my face.” 4. _____ “I will bathe my face with cool water when I shower in the morning.” Washing face once a day is inadequate 5. _____ “I will use mild soap to gently cleanse my face thoroughly twice a day.” 43. A nurse is observing a nursing assistant in a home-care setting administering a bed bath. Which issue apparent in the photograph indicates that the nursing assistant has violated the standards of care for a bed bath? Select all that apply. 1. _____ The pillows behind the client’s body should be removed before the bath. 2. __X__ The nursing assistant’s uniform is in contact with the client’s linens. 3. _____ The nursing assistant should be making eye contact with the client. 4. __X__ The client’s left leg should be covered with the bath blanket. 5. __X__ The nursing assistant is not wearing clean gloves.44. Which statement made by an older adult indicates to the nurse that additional teaching about skin care is necessary? Select all that apply. 1. _____ “I limit my baths to twice a week.” 2. _____ “I humidify my home in the winter.” 3. _____ “I apply moisturizing lotion to my body daily.” 4. __X__ “I use a bubble-bath product when I take a bath.” Bubblebaths cause irritations and dryness of the skin because they remove essential skin surface oils. Showers are preferable. 5. __X__ “I love to relax in a hot bath before going to bed.” A short shower with warm water should be encouraged instead. 45. Which of the following should the nurse implement when providing fingernail care during a client’s bath? Select all that apply. 1. __X__ Push cuticles back with a section of a soft washcloth. 2. __X__ File nails straight across, rounding corners slightly. 3. __X__ Apply a moisturizing lotion around cuticles. 4. __X__ Clean under nails with an orange stick. 5. __X__ Soak hands in warm water first. CHAPTER 5 MOBILITY 313 1. A nurse turns a client’s ankle so that the sole of the foot moves medially toward the midline. Which word should the nurse use when documenting exactly what was done during range-of-motion exercises? 1. Inversion 2. Adduction 3. Plantar flexion 4. Internal rotation2. A nurse is transferring a client from a bed to a wheelchair. Which should the nurse do to quickly assess this client’s tolerance to this activity? 1. Obtain a blood pressure. 2. Monitor for bradycardia. If client was experiencing orthostatic hypotension, the heart rate would increase, not decrease 3. Determine if the client feels dizzy. Feeling dizzy is a subjective response to orthostatic hypotension. Obtaining feedback from the client provides a quick evaluation of the client’s tolerance of the transfer. 4. Allow the client time to adjust to the change in position. 3. A nurse is transferring a client from the bed to a wheelchair using a mechanical lift. Which is a basic nursing intervention associated with this procedure? 1. Lock the base lever in the open position when moving the mechanical lift. 2. Raise the mechanical lift so that the client is six inches off the mattress. 3. Keep the wheels of the mechanical lift locked throughout the procedure. 4. Ensure the client’s feet are guarded when sitting on the mechanical lift. 4. A client has hemiplegia as a result of a brain attack (cerebrovascular accident). Which complication of immobility that may be associated with this client is a concern for the nurse? 1. Dehydration 2. Contractures 3. Incontinence 4. Hypertension 5. Which stage pressure ulcer requires the nurse to measure the extent of undermining?1. Stage 0 2. Stage I 3. Stage II 4. Stage III First sight of undermining 6. A client has a cast from the hand to above the elbow because of a fractured ulna and radius. After the cast is removed, the nurse teaches the client active range-of-motion exercises. Which client action indicates that further teaching is necessary? 1. Moves the elbow to the point of resistance 2. Keeps 90° elbow flexion after the procedure 3. Assesses the elbow’s response after this procedure 4. Puts the elbow through its full range at least 3 times 7. Which word is most closely associated with nursing care strategies to maintain functional alignment when clients are bedbound? 1. Endurance 2. Strength 3. Support 4. Balance 8. A client with impaired mobility is to be discharged from the hospital within a week. Which is an example of a discharge goal for this client? 1. The client will understand range-of-motion exercises before they are initiated. Not measurable. Understanding is not measurable unless parameters are identified. 2. The client will be taught range-of-motion exercises after they are prescribed. Nursing intervention, not measurable goal. 3. The client will transfer independently to a chair by discharge. 4. The client will be kept clean and dry at all times. Nursing goal, not client goal 9. A nurse is performing passive range-of-motion exercises for a client who is in the supine position. Which motion occurs when the nurse bends the client’s ankle so that the toes are pointed toward theceiling? 1. Adduction 2. Supination 3. Dorsal flexion 4. Plantar extension 10. A nurse is caring for a client with impaired mobility. Which position contributes most to the formation of a hip flexion contracture? 1. Low-Fowler In low-Fowler position, the hips are slightly flexed. 2. Orthopneic While in high-Fowler client is positioned leaning forward with arms resting on an over-bed table (orthopneic position). In orthopneic position, hips are extensively flexed, creating an angle of less than 90 degrees. 3. Supine Hips are extended (180 degrees), not flexed 4. Sims Hip and knee of upper leg are just slightly flexed 11. A client is diagnosed with a stage IV pressure ulcer with eschar. Which medical treatment should the nurse anticipate the primary health-care provider will prescribe for this client? 1. Heat lamp treatment three times a day Heat lamp will further dry out wound and cause burns 2. Application of a topical antibiotic Topical antibiotics only when ulcer is infected, not to treat eschar 3. Cleansing irrigations twice daily Cleansing irrigations are ineffective in removing the thick, fibrin-containing cells of eschar covering surface of the wound 4. Debridement of the wound Thick, leather like, necrotic, devitalized tissue (eschar) must be removed surgically or enzymatically before wound healing can occur 12. A nurse raises a client’s arm forward and upward over the head during range-of- motion exercises. Which word should the nurse use when documenting exactly what was done during this range-ofmotion exercise? 1. Flexion2. Supination 3. Opposition 4. Hyperextension 13. A client with a history of thrombophlebitis should not have pressure exerted on the popliteal space. In which position should the nurse avoid placing this client? 1. Prone Prone position has pressure in front of, not behind the knees 2. Supine In supine position, hips and legs are extended, which does not exert pressure on the popliteal spaces 3. Contour Contour position has head of bed and knee gatch slightly elevated putting pressure on popliteal spaces 4. Trendelenburg 14. A nurse is caring for a variety of clients, each experiencing one of the following problems. Which health problem places a client at the highest risk for complications associated with immobility? 1. Incontinence 2. Quadriplegia Paralysis of all four extremities 3. Hemiparesis Muscle weakness 4. Confusion 15. A nurse in a community center is conversing with a group of older adults who voiced fears about falling. Which is the most common consequence associated with older adults’ fear of falling that the nurse should discuss with them? 1. Impaired skin integrity 2. Occurrence of panic attacks 3. Self-imposed social isolation 4. Decreased physical conditioning Most falls occurs when ambulating 16. A nurse is evaluating an ambulating client’s balance. Which factor about the client is most important for the nurse to assess?1. Posture Helps assess client’s center of gravity and find balance for client’s base of support 2. Strength More to do with exertion of power 3. Energy level More to do with endurance 4. Respiratory rate Determines tolerance 17. A client with a prescription for bedrest has diaphoresis. Which should the nurse use to best limit the negative effects of perspiration on dependent skin surfaces of this client? 1. Ventilated heel protectors 2. Air-filled rings Tends to promote sweating 3. Air mattress Tends to promote sweating 4. Sheepskin Soft tuffs of sheepskin allow air to circulate 18. A nurse is teaching a class to nursing assistants about how to care for clients who are immobile. Which should the nurse include about why immobilized people develop contractures? 1. Muscles that flex, adduct, and internally rotate are stronger than weaker opposing muscles. Contractures occur because of muscle spasticity and shortening 2. Muscular contractures occur because of excessive muscle flaccidity. 3. Muscle mass and strength decline at a progressive rate weekly. This results in muscle atrophy not contractures 4. Muscle catabolism exceeds muscle anabolism. Disuse atrophy 19. A nurse turns the palm of a client’s hand downward when performing range-of-motion exercises. Which word should the nurse use when documenting exactly what was done? 1. Pronation 2. Lateral flexion 3. Circumduction 4. External rotation20. Which nursing action is most effective in relation to the concept Immobility can lead to occlusion of blood vessels in areas where bony prominences rest on a mattress? 1. Encouraging the client to breathe deeply 10 times per hour 2. Performing range-of-motion exercises twice a day ROM helps prevent contractures, not pressure ulcers 3. Placing a sheepskin pad under the sacrum Sheepskin pad main purpose is to allow air to circulate under client to minimize moisture and maceration of skin 4. Repositioning the client every 2 hours 21. A nurse plans to use a trochanter roll when repositioning a client. Where should the nurse place the trochanter roll? 1. Under the small of the back 2. Behind the knees when supine 3. Alongside the ilium to mid-thigh 4. In the palm of the hand with the fingers flexed 22. Which is the earliest nursing assessment that indicates damage to tissue because of compression of soft tissue between a bony prominence and a mattress? 1. Nonblanchable erythema Refers to redness of intact skin that persists when finger pressure is applied. This is a classic sign of a stage I pressure ulcer. 2. Circumoral cyanosis Indication of hypoxia 3. Tissue necrosis Necrosis occurs in stage III and IV pressure ulcers 4. Skin abrasion Stage II 23. An emaciated client is at risk for developing a pressure ulcer. In which position should the nurse avoid placing the client? 1. Thirty-degree lateral position Preferred position to prevent pressure ulcers 2. Side-lying position Majority of body weight on greater trochanter3. Supine position Occiput, scapulae, spine, elbows, sacrum and heels are at risk for pressure; however body weight is distributed more evenly 4. Prone position Ears, cheeks, acromion process, anterior-superior spinous process, knees, toes, male genitalia, and female breasts are at risk for pressure; however body weight is distributed more evenly 24. A nurse is making an occupied bed. Which is the easiest way for the nurse to prevent plantar flexion? 1. Tuck in the top linens on just the sides of the bed. 2. Place a toe pleat in the top linens over the feet. 3. Let the top linens hang off the end of the bed. 4. Position the top linens over a bed cradle. 25. A nurse identifies that a client’s pressure ulcer has just partialthickness skin loss involving the epidermis and dermis. Which stage pressure ulcer should the nurse document based on this assessment? 1. Stage I 2. Stage II Partial-thickness skin loss manifests clinically as an abrasion, blister or shallow crater 3. Stage III Full-thickness skin loss involving the subcutaneous tissue that may extend to the underlying fascia. The ulcer manifests clinically as a deep crater with or without undermining. 4. Stage IV Full-thickness skin loss with extensive destruction, tissue necrosis, or damage to muscle, bone, or supporting structures. 26. Which nursing action should be implemented when assisting a client to move from a bed to a wheelchair? 1. Lowering the height of the bed to 2 inches below the height of the client’s wheelchair2. Applying pressure under the client’s axillae areas when assisting the client to stand 3. Letting the client help as much as possible when transferring to the wheelchair 4. Keeping the client’s feet within 6 inches of each other 27. A nurse places a client in the orthopneic position. Which is the primary reason for the use of this position? 1. Facilitates breathing 2. Supports hip extension 3. Prevents pressure ulcers 4. Promotes urinary elimination 28. An immobilized bedbound client is placed on a 2-hour turning and positioning program. Which should the nurse explain to the client is the primary reason why this program is important? 1. Supports comfort 2. Promotes elimination 3. Maintains skin integrity 4. Facilitates respiratory function 29. Which do nurses sometimes do that increases their risk for injury when moving clients? 1. Use longer, rather than shorter, muscles when moving clients 2. Place their feet wide apart when transferring clients 3. Pull rather than push when turning clients 4. Rotate their backs when moving clients 30. Which systemic response in immobilized clients should nurses monitor for? Select all that apply. 1. _____ Pressure ulcer A pressure ulcer is a localized, not systemic response 2. __X__ Dependent edema Systemic response to immobility3. __X__ Hypostatic pneumonia Systemic response to immobility 4. _____ Plantar flexion contracture Localized 5. __X__ Increased cardiac workload Systemic response to immobility 32.A nurse is placing a client in the left-lateral position. Which of the following should the nurse implement when positioning this client? Select all that apply. 1. _____ Maintain the left knee flexed at ninety degrees. Left leg should be slightly flexed or extended 2. _____ Rest the right leg on top of the left leg. Right leg should be supported on a pillow in front of left leg 3. _____ Place the ankles in plantar flexion. Ankles should be maintained at 90 degrees 4. __X__ Align the shoulders with the hips. 5. __X__ Protract the left shoulder. In left-lateral (side-lying) position, the left arm is positioned in front of the body with the shoulder pulled forward (protracted). 33. A nurse places a client with a sacral pressure ulcer in the leftSims position. How should the nurse position the client’s right arm? Select all that apply. 1. __X__ On a pillow In left-Sims position, client’s right arm and leg are supported on pillows to prevent internal rotation of the shoulder and hip. 2. _____ Behind the back Right arm is positioned in front of the back 3. _____ With the palm up Right palm should be down 4. _____ In internal rotation Right arm is positioned to maintain shoulder in functional alignment 5. _____ With the elbow extended Right arm should be flexed slightly 34. A nurse concludes that a client has the potential for impaired mobility. Which of the following reflect risk factors that support this conclusion? Select all that apply. 1. __X__ Joint pain2. _____ Exertional fatigue Fatigue is associated with activity intolerance but people who are fatigued are still able to move 3. _____ Sedentary lifestyle Still able to move 4. __X__ Limited range of motion 5. _____ Increased respiratory rate Response to activity, not impaired mobility 35. A nurse enters the room of the client in the photograph. The client has right-sided weakness and is attempting to transfer out of bed without the nurse’s knowledge. What should the nurse do first? 1. Lower the height of the bed to its lowest position to the floor. 2. Reposition the client back to the semi-Fowler position. 3. Move the wheelchair parallel to the foot of the bed. 4. Put on the client’s slippers. 36. A nurse plans to teach a client with hemiparesis to use a cane. Which should the nurse teach the client to do? Select all that apply. 1. Move forward 1 step with the weak leg first, followed by the strong leg and cane. Strong leg before weak leg 2. Adjust the cane height 12 inches lower than the waist. 3. Hold the cane in the strong hand when walking. 4. Look at the feet when walking with the cane. 5. Lean over onto the cane when walking. 37. A nurse is planning to help move a client up in bed. Which of the following can the nurse implement to reduce the risk of self-strain when performing this action? Select all that apply. 1. __X__ Use the force of gravity to facilitate the move. 2. __X__ Keep the upper and lower body in alignment.3. __X__ Use the large muscles of the legs. 4. __X__ Keep the knees slightly bent. 5. __X__ Raise the bed to waist level. 38. A primary health-care provider prescribes crutches for a person who has a left lower leg injury. The nurse is teaching the person how to move from a standing to a sitting position in a chair. Place the following steps in the order in which they should be implemented. 1. While standing, back up so that the unaffected leg is against the edge of the center of the chair seat. 2. Hold the hand bars of both crutches with the left hand. 3. Grasp the arm of the chair with the right hand. 4. Lean forward slightly and flex the knees and hips. 5. Lower the body slowly into the chair. 39. A client sits for excessive lengths of time in a wheelchair. Which site should the nurse assess for skin breakdown in this client? Select all that apply. 1. __X__ Ischial tuberosities 2. __X__ Bilateral scapulae Affects also supine and Fowler positions 3. _____ Trochanters 4. _____ Malleolus Affects side-lying position 5. __X__ Sacrum Affects also supine and Fowler positions 40. A client with limited mobility has a prescription to be out of bed to a chair for 1 hour daily. The nurse plans to transfer the client using a mechanical lift. Which of the following should the nurse implement? Select all that apply. 1. Apply gentle pressure against the client’s knees while lowering the client into the chair.2. Ensure that there is a prescription to use this device to transfer the client out of bed. 3. Hook the longer straps on the end of the sling closest to the client’s feet. 4. Place a sheepskin inside the sling so that it is under the client. 5. Lead with the client’s feet when exiting the bed. 41. A primary health-care provider prescribes a standard walker for a client who has left-sided weakness and requires some assistance with balance but can bear weight on both legs. Which should the nurse teach the client about how to use the walker safely? Select all that apply. 1. __X__ Advance the strong leg last by itself. 2. _____ Lift the walker before moving it forward twelve inches. Six not twelve inches is the proper distance to advance a walker 3. __X__ Advance the walker and the weak leg ahead together first. 4. _____ Adjust the height of the walker so that it is equal with the hip joint. Hand bar should be at a height just below the client’s waist, allowing elbows to be slightly flexed 5. _____ Roll the walker a comfortable distance ahead before stepping forward. 42. A nurse is to transfer a client from a bed to a chair. After washing the hands, providing privacy, and explaining the transfer to the client, the nurse ensures that the wheels on the bed are locked and moves the bed to the lowest position. Place the following steps in the order in which they should be implemented. 1. Assess the client’s vital signs and strength while in the supine position. 2. Elevate the head of the bed to the high-Fowler position and put footwear on the client’s feet.3. Assist the client to a sitting position on the side of the bed, with the feet on the floor. 4. Verify if the client feels dizzy. 5. Support the client sitting on the side of the bed for several minutes before transferring to a chair. 43. Which action employed by the nurse indicates acceptable body mechanics to avoid self-injury? Select all that apply. 1. __X__ Keep back, neck, pelvis, and feet aligned. 2. __X__ Position oneself close to the client. 3. __X__ Keep knees and hips slightly flexed. 4. __X__ Arrange for adequate help. 5. _____ Keep feet close together. Feet should be wide apart 44. A nurse is assessing a client’s risk for thrombus formation associated with impaired mobility. Which of the following constitute Virchow’s triad? Select all that apply. 1. __X__ Compression of small vessels in the legs Compression of small vessels in the legs is one of the three factors that make up Virchow’s triad. Immobility leads to vessel compression, which can cause injury to small vessels. 2. _____ Orthostatic hypotension 3. __X__ Coagulation activation As a result of venous pooling, there is a decreased clearance of coagulation factors, resulting in activation of clotting (i.e. the blood clots faster). 4. _____ Hypostatic pneumonia 5. __X__ Venous stasis Inactive skeletal muscles of the legs do not adequately compress the peripheral vessels in the legs and therefore do not assist with the return of blood back to the heart; this results in stasis of blood in lower extremities. 45. A nurse is caring for a male client who is at risk for a pressure ulcer. After reviewing the client’s clinical record, which area of the body shouldthe nurse identify is most at risk for a pressure ulcer? 1. Greater trochanters At risk in side-lying position 2. Ischial tuberosities Ischial tuberosities are at greatest risk when a client is in the orthopneic or mid- to high-Fowler positions because the greatest weight of the body is exerted against the genital, perianal, and sacral areas of the body. 3. Medial malleolus At risk in side-lying position 4. Spinal processes At risk when client is in supine or a Fowler position CHAPTER 5 PAIN, COMFORT, REST AND SLEEP 415 1. A nurse is caring for a client who is experiencing pain. For which common psychological response to pain should the nurse assess the client? 1. Concerned about loss of control and independence 2. Withdrawing from social interactions with others 3. Asking for medication to provide for relief 4. Experiencing nausea and vomiting 2. Which is the appropriate client outcome for an adult who has disturbed sleep because of nocturia? 1. Report fewer early morning awakenings because of a wet bed. 2. Demonstrate a reduction in nighttime bathroom visits. 3. Resume sleeping immediately after voiding. 4. Use an incontinence device at night. 3. A client with a diagnosis of cancer of the ovary had her uterus and both ovaries and fallopian tubes removed (hysterectomy with bilateral salpingo-oophorectomy) and a surgical debulking via an abdominal incision 2 days ago. The client reports abdominal pain at level 5 on a 0-to-10 pain scale. After assessing the pain further, which should the nurse do first?1. Reposition the client. 2. Offer a relaxing back rub. 3. Use distraction techniques. 4. Administer the prescribed analgesic. 4. A nurse is caring for a client who is diagnosed with narcolepsy. Which is the most serious consequence of this disorder? 1. Inability to provide self-care 2. Impaired thought processes 3. Potential for injury Narcolepsy is excessive sleepiness in the daytime that can cause a person to fall asleep uncontrollably at inappropriate times 4. Excessive fatigue 5. A client is experiencing discomfort associated with gastroesophageal reflux. In which position should the nurse teach the client to sleep? 1. Right lateral 2. Semi-Fowler This limits gastroesophageal reflux because gravity allows abdominal organs to drop, which reduces pressure on stomach and results in less stomach contents flowing upward into esophagus. 3. Prone 4. Sims 6. A client is experiencing anxiety. Which aspect of sleep should the nurse expect primarily will be affected as a result of the anxiety? 1. Onset 2. Depth 3. Stage II Stage IV is affected not Stage II 4. Duration 7. A client requests pain medication for severe pain. Which should the nurse do first when responding to this client’s request? 1. Use distraction to minimize the client’s perception of pain. 2. Place the client in the most comfortable position possible.3. Administer pain medication to the client quickly. 4. Assess the various aspects of the client’s pain. All factors that affect the pain experience should be assessed, including location, intensity, quality, duration, pattern, aggravating and alleviating factors, and physical, behavioral, and attitudinal responses. Assessment must precede intervention. 8. A nurse is planning a teaching program for a client with a diagnosis of obstructive sleep apnea. Which should the nurse plan to discuss with this client? 1. Using the prescribed device that supports airway patency 2. Placing two pillows under the head when sleeping 3. Requesting a sedative to promote sleep 4. Sleeping in the supine position This increases episodes of sleep apnea 9. Which is the most important nursing intervention that supports a client’s ability to sleep in the hospital setting? 1. Providing an extra blanket 2. Limiting unnecessary noise on the unit 3. Shutting off lights in the client’s room Dim lights only 4. Pulling curtains around the client’s bed at night 10. A client has a history of severe chronic pain. Which is the most important intervention associated with providing nursing care to this client? 1. Asking what is an acceptable level of pain 2. Providing interventions that do not precipitate pain 3. Focusing on pain management intervention before pain is excessive 4. Determining the level of function that can be performed without pain11. Which concept should the nurse consider when assessing a client’s pain? 1. The expression of pain is not always congruent with the pain experienced. 2. Pain medication can significantly increase a client’s pain tolerance. 3. The majority of cultures value the concept of suffering in silence. 4. Most people experience approximately the same pain tolerance. 12. Which most common cause of sleep deprivation in the hospital should the nurse consider when planning care? 1. Fragmented sleep 2. Early awakening 3. Restless legs 4. Sleep apnea 13. A nurse is performing an admitting interview. Which client statement about pain should cause the most concern for the nurse? 1. “I try to pretend that it is not part of me, but it takes a lot of effort.” 2. “My pain medication works, but I’m afraid of becoming addicted.” 3. “At home, I take something for the pain before it gets too bad.” 4. “They say my pain may get worse, and I can’t stand it now.” 14. A client has been in the intensive care unit (ICU) for 3 days. For which common adaptation indicating ICU psychosis associated with sleep deprivation should the nurse assess the client? 1. Hypoxia 2. Delirium 3. Lethargy 4. Dementia 15. Which concept associated with sleep should the nurse consider to plan nursing care for a hospitalized client? 1. People require eight hours of uninterrupted sleep to meet energyneeds. 2. Frequency of awakenings during sleep decreases as people age. 3. Fear can interfere with the ability to relax and sleep. 4. Bedrest decreases the need for sleep. 16. A nurse is assessing a client in pain. Which word might the nurse use when documenting the pattern of a client’s pain? 1. Tenderness 2. Moderate 3. Episodic 4. Phantom 17. A nurse is obtaining a health history from a newly admitted client. Which client statement about alcohol intake is based on a common physiological response? 1. “After I go drinking, I have to urinate during the night.” 2. “When I drink, I get hungry in the middle of the night.” 3. “Falling asleep is hard, but once asleep I sleep great.” 4. “If I drink too much, I oversleep in the morning.” 18. A nurse is assessing a client experiencing acute pain. Which characteristic is more common with acute pain than with chronic pain? 1. Self-focusing 2. Sleep disturbances 3. Guarding behaviors 4. Variations in vital signs Acute pain stimulates the sympathetic nervous system, which responds by increasing pulse, respirations, and blood pressure. Chronic pain stimulates the parasympathetic nervous system, which lowers pulse and blood pressure.19. At which time does a nurse medicate a client for pain for it to be considered preemptive analgesia? 1. Before a client goes to sleep 2. At equally distant times around the clock 3. As soon as a client reports the occurrence of pain 4. Before doing a dressing change that has been painful in the past The word preemptive means preventive, anticipatory and defensive. Therefore, preemptive analgesia is administered before an activity or intervention that may precipitate pain in an attempt to limit anticipated pain. 20. A client is diagnosed with chronic fatigue syndrome. Which is most important for the nurse to explore in relation to the client’s status? 1. Ability to provide self-care 2. Physical mobility 3. Social isolation 4. Gas exchange 21. Which is most important for nurses to understand when caring for clients in pain? 1. Clients who are in pain will request pain medication. 2. Clients usually are able to describe the characteristics of their pain. 3. Clients need to know that the nurse believes what they say about their pain. Pain is a personal experience and the nurse must validate it is presence and severity as perceived by the client. 4. Clients will demonstrate vital signs that are congruent with the intensity of their pain. Acute pain increases V/S because of SNS, but chronic pain will not. 22. A client is experiencing lack of sleep because of pain. Which is the most appropriate goal for this client? 1. The client will be provided with a back massage every evening before bedtime. 2. The client will report feeling rested after awakening in the morning. 3. The client will request less pain medication during the night.4. The client will experience four hours of uninterrupted sleep. 23. A nurse is helping a client who is experiencing mild pain to get ready for bed. Which nursing action is most effective to help limit pain? 1. Assisting with relaxing imagery 2. Obtaining a prescription for an opioid 3. Encouraging the client to take a warm shower 4. Recommending that the client be more active during the day 24. During which time frame do people tend to be the sleepiest? 1. 12 noon and 2 p.m. 2. 6 a.m. and 8 a.m. 3. 2 a.m. and 4 a.m. 2 a.m. – 6 a.m. & 2 p.m. – 5 p.m. 4. 6 p.m. and 8 p.m. 25. Which client statement indicates that the client is experiencing bruxism? 1. “I walk around in my sleep almost every night, but I don’t remember it.” 2. “I annoy the whole family with the loud snoring noises I make at night.” 3. “I occasionally urinate in bed when I am sleeping, and it’s embarrassing.” 4. “I am told by my wife that I make a lot of noise grinding my teeth when I sleep.” Bruxism is clenching and grinding of teeth, a parasomnia that occurs during stage II NREM sleep.26. A nurse is caring for clients receiving a variety of interventions for pain management. Which pain relief method has the shortest duration of action? 1. Client-controlled analgesia 2. Intramuscular sedatives 3. Intravenous narcotics 4. Regional anesthesia 27. A nurse is teaching a community health education class about rest and sleep. Which concept related to sleep should the nurse include? 1. Total time sleeping in bed decreases as one ages. 2. Sleep needs remain consistent throughout the life span. 3. Alcohol intake interferes with one’s ability to fall asleep. 4. Bedtime routines are associated with an expectation of sleep. 28. A nurse is teaching a client various techniques to promote sleep. Which internal stimulus that most commonly interferes with sleep should the nurse include in the teaching? 1. Ringing in the ears 2. Bladder fullness 3. Hunger 4. Thirst 29. A nurse is giving a back rub. Which stroke is most effective in inducing relaxation at the end of the procedure? 1. Percussion Gentle tapping during middle of back massage 2. Effleurage Long, smooth strokes sliding over the skin 3. Kneading Middle of backrub 4. Circular Buttocks, lower back, and scapulae 30. When the nurse is assessing a client, the client states, “The pain moves from my chest down my left arm.” Which characteristic of pain is associated with this statement?1. Pattern 2. Duration 3. Location 4. Constancy 31. A nurse is providing health teaching for a client with the diagnosis of obstructive sleep apnea. Which aspect of sleep should the nurse explain is most often affected? 1. Amount 2. Quality 3. Depth 4. Onset 32. A client is being admitted to the hospital, and the nurse is performing a complete assessment. Which is the most therapeutic question the nurse can ask about the quality of the client’s sleep? 1. “Does your bed partner complain about your sleep behaviors?” 2. “Is the number of hours you sleep at night good for you?” This is just a yes or no question. 3. “Do you consider your sleep to be restless or restful?” 4. “How would you describe your sleep?” Open-ended question requires clients to explore topic of sleep as it relates specifically to their own experiences. 33. A nurse strains a back muscle when moving a client up in bed. Which can the nurse do at home that utilizes the gate-control theory of pain relief to minimize the discomfort? 1. Use guided imagery.2. Perform progressive muscle relaxation. 3. Apply a cold compress to the site for 20 minutes. 4. Take a nonsteroidal anti-inflammatory medication every 6 hours. 34. A client is having difficulty sleeping and may be experiencing shortened non–rapid- eye-movement (NREM) sleep. Which client assessment supports this conclusion? Select all that apply. 1. _____ Decreased pain tolerance 2. _____ Inability to concentrate 3. _____ Excessive sleepiness 4. _____ Irritability 5. _____ Confusion 35. A primary health-care provider prescribes oxycodone oral solution 15 mg every 6 hours. The drug is supplied in a 500-mL bottle that indicates 5 mg/5 mL. How much oral solution should the nurse administer? Record your answer using a whole number. Answer: 15 mL. 36. A 12-year-old boy is experiencing nocturnal enuresis. Which of the following should the nurse explore with the boy and his parents? Select all that apply. 1. __X__ Limiting fluid intake after dinner 2. __X__ Voiding immediately before going to bed 3. __X__ Eliminating caffeinated beverages from the diet 4. __X__ Thinking about waking up dry when going to bed 5. __X__ Changing the wet bed linens using a nonchalant attitude 38.Which of the following statements associated with rest and sleep must the nurse consider when planning nursing care? Select all that apply.1. _____ Energy demands increase with age. 2. _____ Metabolic rate increases during rest. 3. __X__ Sleep requirements increase during stress. 4. _____ Catabolic hormones increase during sleep. 5. __X__ Lack of awareness of the environment increases with sleep. 38. A nurse is caring for a client who is having difficulty sleeping. Which client response indicates that the client is not obtaining adequate rapid-eye-movement (REM) sleep? Select all that apply. 1. _____ Hyporesponsiveness 2. _____ Immunosuppression 3. __X__ Irritability 4. __X__ Confusion 5. _____ Vertigo 39. An older female adult explains to the nurse that she has insomnia. The nurse inter- views the client and her husband and reviews the client’s medication reconciliation form. Which of the following does the nurse conclude is associated with the client’s insomnia? Select all that apply. 1. _____ Metformin 2. __X__ Older adult 3. __X__ Female gender 4. __X__ Alcohol intake 5. _____ Diphenhydramine 6. __X__ Several naps during the day CLIENT’S CLINICAL RECORD 41. Which is important for a nurse to consider when a client reports the presence of pain? Select all that apply. 1. _____ The extent of pain is directly related to the amount of tissue damage.2. _____ Fatigue decreases the intensity of pain experienced by the client. 3. _____ Behavioral adaptations are congruent with statements about pain. 4. _____ Giving opioids to a client in pain will lead to an addiction. 5. __X__ The person feeling the pain is the authority on the pain. 42. Which statement by a client indicates a precipitating factor associated with pain? Select all that apply. 1. _____ “I usually feel a little dizzy and think I’m going to vomit when I have pain.” Physiological response 2. _____ “My pain usually comes and goes throughout the night.” Reflects pattern of pain 3. __X__ “I usually have pain after I get dressed in the morning.” Precipitating factor 4. _____ “My pain feels like a knife cutting right through me.” Quality of pain 5. __X__ “My abdominal incision hurts when I cough.” Precipitating factor 43. A nurse administers a back rub to a client after first providing for privacy and maintaining standard precautions. Place the following steps in the order in which they should be implemented. 2. Position the client in the side-lying position. 4. Arrange the gown and top linens so that the client’s back is exposed. 3. Assess the skin for color, turgor, and skin breakdown. 1. Warm lotion in your hands. 5. Use a variety of strokes to massage the muscles of the back and sacral area. 44. When assessing clients who have difficulty sleeping, the nurse assesses for which common physiological response to insomnia? Select all that apply. 1. __X__ Vertigo 2. __X__ Fatigue3. _____ Irritability 4. __X__ Headache 5. _____ Frustration 45. A nurse is assessing a client experiencing chronic pain. Which characteristic is more common with chronic pain than with acute pain? Select all that apply. 1. __X__ Gradual onset 2. __X__ Long duration 3. _____ Anticipated end Acute pain 4. __X__ Psychologically depleting 5. _____ Responds to conventional interventions [Show More]
Last updated: 2 years ago
Preview 1 out of 106 pages
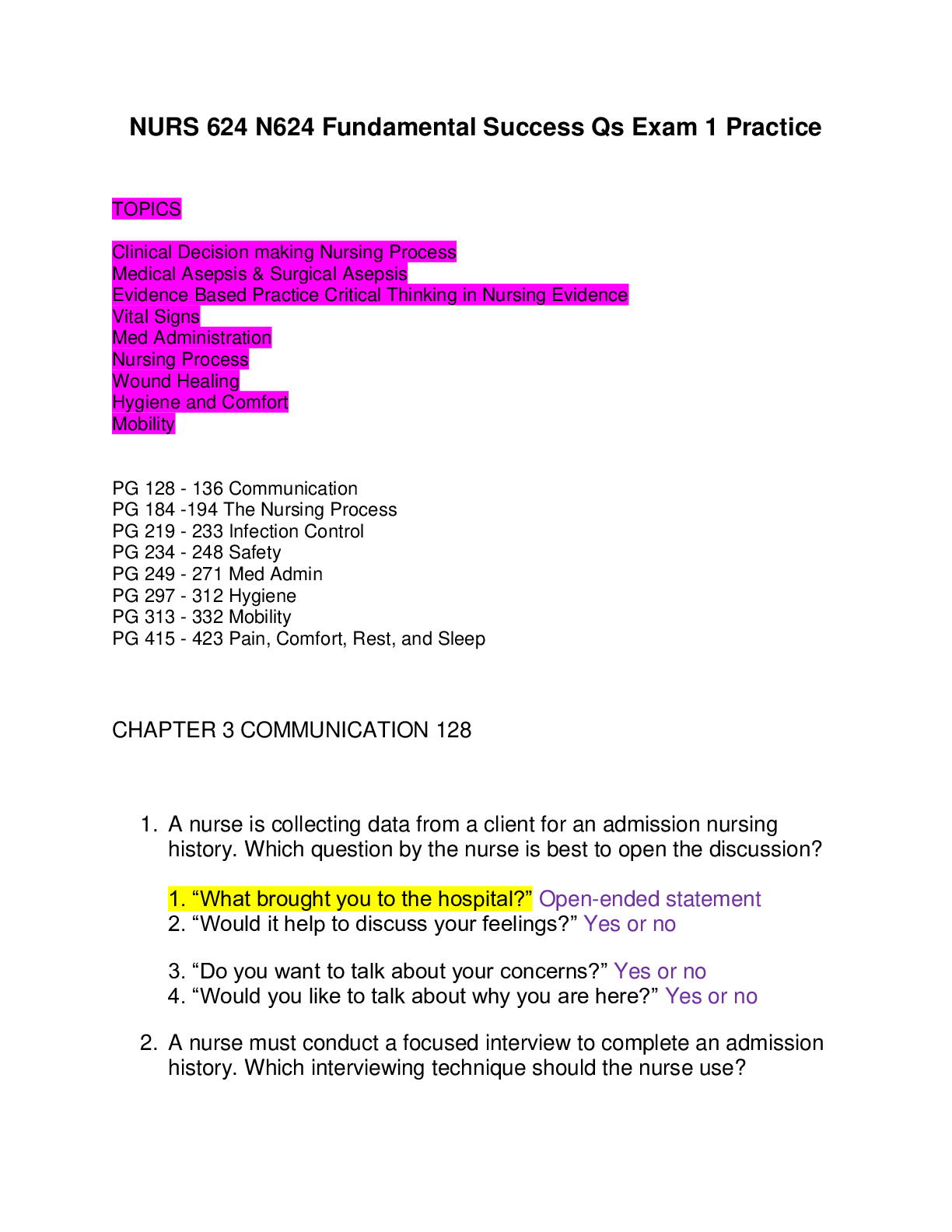
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$18.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Jan 29, 2021
Number of pages
106
Written in
Additional information
This document has been written for:
Uploaded
Jan 29, 2021
Downloads
0
Views
88