Biology > STUDY GUIDE > NSG 331 Med-Surg Final Exam Review 2019/2020 – Marian University | NSG331 Med-Surg Final Exam Revi (All)
NSG 331 Med-Surg Final Exam Review 2019/2020 – Marian University | NSG331 Med-Surg Final Exam Review 2019/2020
Document Content and Description Below
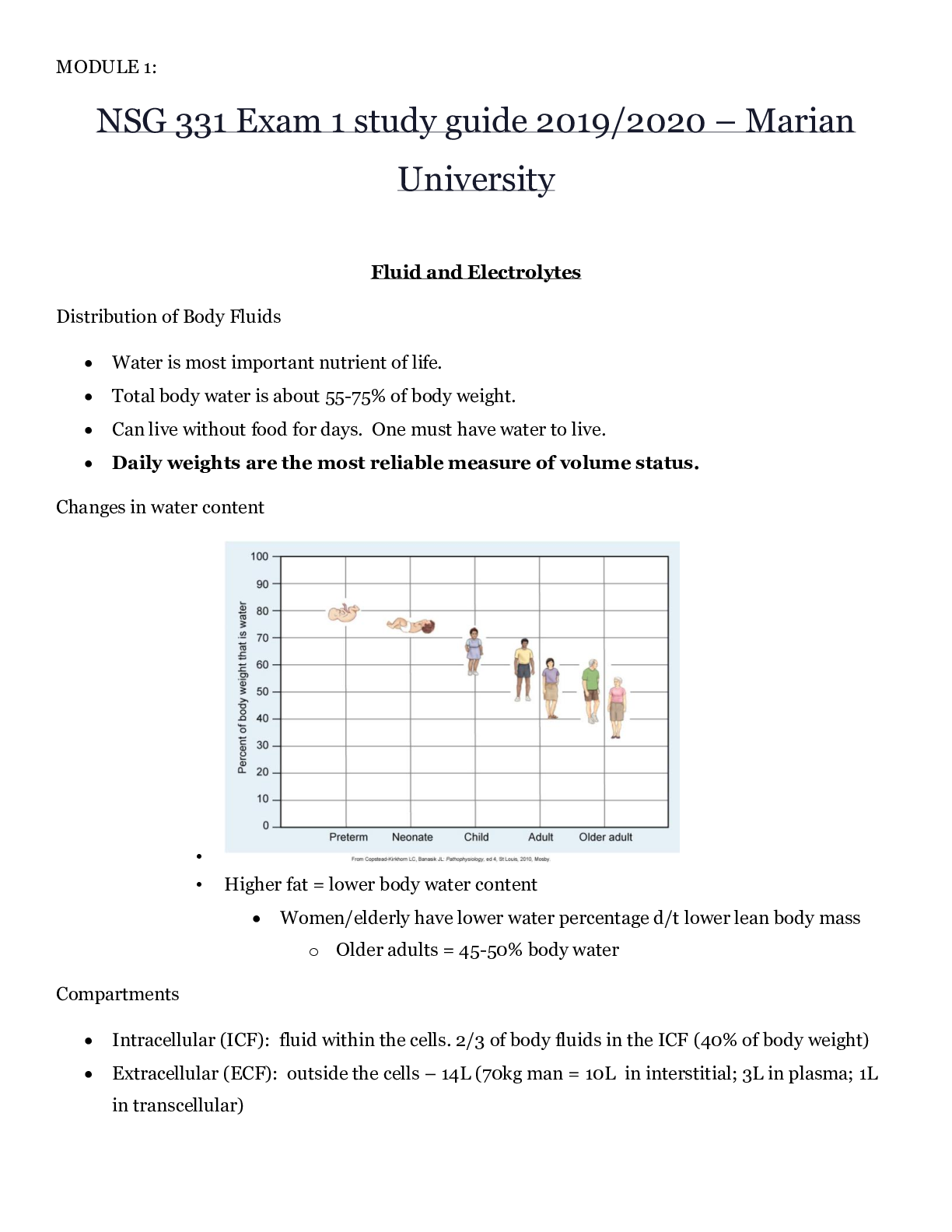
NSG 331 Med-Surg Final Exam Review 2019/2020 – Marian University MED-SURG FINAL EXAM REVIEW TOPICS CHAPTER 13 Dermatitis (p. 200) 1. Allergic contact dermatitis 2. Irritant dermatitis... 3. Nummular eczema 4. Seborrheic dermatitis 5. Stasis dermatitis 6. Atopic dermatitis • Usually called eczema • Common, chronic, relapsing • Often begins in childhood • Familial hay fever, asthma, etc. • Manifestations ⎫ Pruritus –major manifestation ⎫ Dry skin ⎫ Acute onset with red, oozing, crusting rash ⎫ Intense scratching leads to lesions, infection and scarring • Treatment ⎫ Hydrate the skin (soaks with colloidal oatmeal) ⎫ Moisturize the skin ⎫ Remove allergens ⎫ Reduce inflammation ⎫ Treat infection 7. Nursing Management of Dermatologic Problems • Wet Dressings – damaged, oozing skin – remove crust and scabs – tap water at room temp/vinegar ⎫ Relieve itching ⎫ Suppress inflammation ⎫ Debride the wound • Baths – large areas of the body – colloidal oatmeal (Aveeno) • Topical Medications – Table 23-12 – occlude with plastic wrap to increase absorption • Control Pruritus – break the itch-scratch cycle to prevent excoriation and lichenification ⎫ Lichenification – thickening of the epidermis with exaggerated markings resembling a washboard o Caused by chronic itching / rubbing of the skin • Prevention of Spread – gloves and adamant hand washing • Prevention of Secondary Infections – particularly to existing skin lesions • Specific skin care – educate patient on skin care after dermatologic procedures and hygiene ⎫ Wounds kept moist and covered heal more rapidly, leave scab/crust undisturbed CHAPTER 16 Dehydration Fluid Volume Deficit (FVD): Hypovolemia • Causes: decr intake, vomiting, fever, diarrhea, NG loss, hemorrhage, 3rd spacing, incr insensible loss, diab insipid • S&S: dry, pale cold clammy skin, wt loss, decreased turgor and cap refill, tachycardia, postural hypotension, high HCT level, low U/O, low grade temp, altered mental status, seizures, coma, restlessness, drowsiness • Treatment: underlying cause, oral/IV fluids (0.9% NS), blood (if d/t hemorrhage), rest, nutrition • Nursing measures: VS, I&O, postural hypotension (safety) Hypothalamic-pituitary regulation o Body fluid deficit / Increases in plasma osmolarity activates osmoreceptors in hypothalamus ♣ Activates thirst and release of ADH from posterior pituitary to retain water (distal tubules) ♣ Thirst mechanism major defense against dehydration - Elderly have reduced thirst mechanism o Dec BP, nausea, pain, hypoglycemia, hypoxemia all stimulate ADH release; ♣ postop stress response, receiving analgesics/anesthesia = ADH release and decreased osmolality o Dry mouth will cause a person to drink even when there is no body water deficit Renal Regulation o Kidneys regulate water balance by adjusting urinary volume and excretion of electrolytes o Avg adult = kidneys reabsorb 99% of filtrate = 1.5L urine per day ♣ Kidney issues = less ability to regulate = edema, etc. Adrenal cortical Regulation o Release of hormones to regulate water and electrolytes ♣ Glucocorticoids – cortisol – anti-inflammatory = increase serum glucose levels ♣ Mineralocorticoids – aldosterone =enhance Na retention/K+ excretion (dec Na = RAAS activation ♣ Hormones regulate amt of water is retained Cardiac Regulation o Natriuretic peptide (antagonist to RAAS) – cardiomyocytes: response to incr atrial pressure & incr Na ♣ Decrease blood volume = atrial NP (ANP) and b-type NP (BNP) – renal tubules – excrete Na/H2O ♣ Activate to decrease volume – elevated = CHF – inhibit aldosterone, renin, ADH, angiotensin II Gastrointestinal Regulation o Oral intake accounts for most water (D/V = losing fluid/electrolytes) o Secretes approximately 8000mL of digestive fluid that is reabsorbed (small amt eliminated in feces) ♣ D/V – prevents reabsorption – fluid and electrolyte loss Insensible water loss = Sweating Sensible water loss = Excessive sweating – exercise, fever, excessive environmental heat Hypo/Hypernatremia (p. 279) Hypo/hyperK+ (p. 281) Magnesium Imbalance (p. 286) Fluid Volume Excess/Overload (p. 276) Acid/Base Imbalances (p. 288) CHAPTER 21 Bacterial Conjunctivitis (p. 371) 1. Pinkeye most common infection 2. Occurs in any age group 3. Manifestations: • Discomfort • Pruritus • Redness • Mucopurulent drainage 4. Typically occurs in one eye THEN spreads 5. MEDS—besifloxacin 6. Teach—handwashing & avoid contact with infected person Cataracts (p. 373-376) 1. Def: opacity within the lens 2. Etiology & Pathophysiology • Most: age related = senile cataracts • Blunt or penetrating Trauma • Congenital factors – i.e. maternal rubella • Radiation or ultraviolet exposure - UV • Steroids – systemic or long-term corticosteroids • Ocular inflammation • Diabetes Mellitus – develops cataracts at a younger age 3. Clinical Manifestations • Decrease in vision - visual decline is gradual, rate of cataract development varies from patient to patient. • Abnormal color perception • Totally opaque lens creates the appearance of a white pupil. • Glare - result of light scatter d/t lens opacities - may be significantly worse at night when pupil dilates. 4. Diagnostic Studies - Diagnosis is based on decreased visual acuity or other complaints of visual dysfunction. • History and physical • Visual acuity measurement • Ophthalmoscopy (Direct and Indirect) – observe opacity • Appearance of white pupil • Slit lamp microscopic exam – observe opacity • Glare testing – potential acuity testing in selected patients • Keratometry / A-scan ultrasound – if Sx is planned • Visual field perimetry to determine cause of visual loss 5. Interprofessional Care • Nonsurgical ⎫ Visual aids ϖ Changing eyewear prescription ϖ Reading glasses ϖ Magnifiers ϖ Increased lighting • Surgical ⎫ Preop ϖ Dilating drops & nonsteroidal anti-inflammatory eye drop ϖ Mydriatic or cycloplegic drugs ⎫ Intraop ϖ Phacoemulsification—most common cataract surgery ϖ Extracapsular cataract extraction—for advanced cataracts ϖ IOL lens placed at end of procedure ⎫ Postop ϖ Antibiotic drops to prevent infection & corticosteroid drops ϖ Avoid bending, stooping, coughing, lifting 6. Nursing Management ⎫ A/f surgery, pt experiences little or no pain ⎫ NOTIFY—intense pain bc indicates hemorrhage, infection, or increased IOP ⎫ NOTIFY—increased or purulent drainage, redness, deceased visual acuity Glaucoma (p. 379-352) 1. Def: increased IOP and consequences of elevated pressure, optic nerve atrophy, and peripheral visual loss 2. Etiology & Pathophysiology • Primary Open-Angle Glaucoma ⎫ Most common type ⎫ Outflow of aqueous humor is decreased ⎫ Drainage channels become clogged ⎫ Damage to optic nerve can result • Primary Angle-Closure Glaucoma ⎫ Lens bulging forward as a result of the aging process ⎫ Pupil dilation 3. Clinical Manifestations • POAG ⎫ Develops slowly w/o Sx ⎫ Eventually tunnel vision • PACG ⎫ Sudden, excruciating pain in or around the eye ⎫ N/V ⎫ Seeing colored halos around lights, blurred vision and ocular redness 4. Diagnostic Studies • Elevated IOP (normal 10-21 mm) • POAG—slit lamp microscopy reveals normal angle • PACG—slit lamp microscopy reveals narrow or flat angle, edematous cornea, fixed or dilated pupil, ciliary injection 5. Interprofessional Care • Keep IOP low to prevent optic nerve damage • Chronic Open-Angle Glaucoma ⎫ Drugs, initial treatment ⎫ Argon Laser Trabeculoplasty—noninvasive option when drugs fail • Acute Angle-Closure Glaucoma ⎫ Ocular emergency ⎫ Miotics, oral/IV hyperosmotic agents, isosorbide, mannitorl solution 6. Nursing Management • Preventable • Comprehensive ophthalmic exam q2-4y for ppl 40-64, 1-2y for ppl > 65 • All β-adrenergic blocking glaucoma agents are contraindicated in the patient with bradycardia, heart block greater than first-degree heart block, cardiogenic shock, and overt cardiac failure. • AVOID anticholinergic drugs: Benadryl, Tagament, Prozac, Paxil, Oxybutynin, Topamax, Bactrim, etc. Sensorineural and Conductive Hearing Loss (p. 387-388) 1. Sensorineural Hearing Loss • Presbycusis ⎫ Hearing loss due to aging ⎫ Causes o Aging process o Injury to hair cells of organ of Corti o Atrophy to lymph-producing cells, and blood vessels in wall of cochlea interrupting nutrients ⎫ Changes o External Ear: incr. cerumen; incr. hair growth; loss of elasticity o Middle Ear: atrophy of tympanic membrane o Inner Ear: hair cell degeneration; neuron degeneration; calcification of ossicles; vestibular apparatus changes. o Brain: decline in ability to filter sounds ⎫ Assessment Findings o External Ear: impacted ear canal; visible hair; collapsed ear canal. o Middle Ear: Conductive hearing loss o Inner Ear: diminished sensitivity to high-pitched sounds; impaired speech reception; alteration is balance and body orientation. o Brain: sensitive to loud noises, inability to hear in loud environments • Sudden Hearing Loss – sudden, unexpected loss of hearing (usually in one ear) – medical emergency • Congenital • Noise-induced • Benign and Malignant Tumors • Meniere’s Disease • Vaccines – MMR – Rubella first 8 weeks of pregnancy – avoid pregnancy 3 months after vaccines, test for Abs • Ototoxic substances 2. Sensorineural vs. Conductive Hearing Loss • Sensorineural ⎫ Impaired function of inner ear or vestibulocochlear nerve (CN VIII) ⎫ Causes: hereditary, trauma, infection, immune disease, DM ⎫ Sounds are muffled – audiogram = loss of 2000-4000 dB ⎫ Hearing aid may only make sounds louder, not clearer • Conductive ⎫ Outer or middle ear conditions prevent transmission of sound via air to inner ear. ⎫ Causes: otitis media, mastoiditis, impaction, foreign bodies, otosclerosis ⎫ Presence of bone-air gap ⎫ Person speaks softly ⎫ Find cause and treat. ⎫ Hearing aid Meniere’s Disease (p. 386) 1. Usual onset 30-60 years old 2. Every 5 of 100 persons 3. Cause is unknown • Trauma • Recent viral infection • Allergies • Genetic predisposition 4. Aural: feeling of fullness in the ear 5. S&S: sudden attacks of vertigo, tinnitus, hearing loss, nausea, vomiting 6. After attack: vertigo 2-4 hrs, dizziness, unsteadiness, gait changes, depression, moody, VS WNL, hearing loss 7. Disorder that affects both vestibular and auditory function 8. Caused by excess endolymph in the vestibular and semicircular canals 9. Remission and relapses without apparent causes 10. Clinical Manifestations • Episodic incapacitating vertigo • Tinnitis or a roaring sound • Fluctuating progressive sensorineural hearing loss • Feeling pressure or fullness in the ear (aural) • Attacks increase in frequency and symptoms 11. Diagnosis • History and physical • Diagnostic testing ⎫ Audiometric tests – speech discrimination, tone decay ⎫ Vestibular tests – caloric test, positional test – Romberg ⎫ Electronystagmography ⎫ Neurologic exam ⎫ Glycerol test 12. Collaborative Care • Acute Attacks ⎫ Drug therapy o Antihistamine o Anticholinergics o Benzodiazepines o Antiemetics o Antivertigo drugs ⎫ Bedrest • Non-acute management ⎫ Diuretics ⎫ Antihistamines ⎫ Calcium channel blockers ⎫ Antivertigo drugs ⎫ Benzodiazepines ⎫ Low sodium diet, restrict caffeine, alcohol, nicotine, foods with MSG 13. Nursing Management • Safety • Potential hearing loss • Fluid and electrolyte balance • Minimize vertigo • Minimize modifiable stressors • Avoid flickering lights/watching TV • Sudden head movement 14. Surgical Intervention • Indications ⎫ Frequent attacks that incapacitate ⎫ Quality of life is affected ⎫ Possible loss of job • Options ⎫ Endolymphatic shunt ⎫ Vestibular nerve resection ⎫ Labyrinthectomy CHAPTER 23 Skin Cancer (p. 410-413) 1. Nonmelanoma Skin Cancers • Actinic Keratosis – AKA solar keratosis ⎫ Premalignant skin lesions – most common of all pre-cancerous skin lesions ⎫ Hyperkeratotic papules and plaques on sun exposed areas ⎫ Incidence: nearly all older white population ⎫ Lesion: irregularly shaped, flat, slightly erythematous papule with indistinct borders and overlying hard keratotic scale or horn ⎫ Treatment: cryosurgery, surgical removal, topicals, dermabrasion, etc. o Aggressive d/t to inability to distinguish from squamous cell carcinoma • Basal Cell Carcinoma ⎫ Locally invasive malignancy arising from epidermal basal cells ⎫ Most common, least deadly – middle aged to older adults o Occurs most likely at the site of a previous trauma – scar, thermal burns, injuries ⎫ Erythematous, pearly, sharply defined, may become nodular and ulcerative ⎫ Treatment, surgical excision, chemosurgery, electrosurgery, cryosurgery o Hard to distinguish from Melanoma – tissue biopsy needed to confirm Dx ⎫ Rarely metastasize – if left untreated can lead to massive tissue destruction • Squamous Cell Carcinoma ⎫ Malignant tumor of squamous cells of epidermis = keratinizing epidermal cells: sun exposed skin o At the base of an actinic keratosis or another lesion ⎫ Invasive, can be highly aggressive and metastasize - Less common than Basal Cell Carcinoma o Can lead to death if not treated early and/or correctly ⎫ Pipe, cigar, cigarettes – contribute to formation of SCC on mouth and lips ⎫ Immunosuppression leads to a dramatic increase in the incidence of SCC o Renal transplant Pts – 253-fold increase in the risk for SCC ⎫ Treatment: surgical excision, radiation, chemotherapy 2. Malignant Melanoma • Tumor arising in melanocytes • Cutaneous melanoma: MM that arises from the skin • Most deadly skin cancer • Ability to metastasize to any organ including brain and heart • Risk factors: ⎫ Chronic UV exposure – damages the DNA and causes mutations in genetic code ⎫ Fair skin and eyes ⎫ Genetic factors – 5-10% incidence if family member has it ⎫ Immunosuppression and dysplastic nevi (moles) – 25% of cases – continue to produce melanin • Prognosis determinants – tumor thickness at time of diagnosis ⎫ Breslow measurement – depth of tumor in mm ⎫ Clark level – depth of invasion of tumor • Nearly 100% curable if excised at stage 0 (in situ) 3. ABCDE’s of Melanoma • A. Asymmetry • B. Border irregularity • C. Color • D. Diameter • E. Evolving 4. Atypical / Dysplastic Nevus • Appearance between common nevi(mole) and melanoma • Increased risk for melanoma • Often > 5mm across, irreg. border, variegated color, freq. multiple, after puberty, on back but may be on scalp or buttocks • Excisional biopsy for suspicious lesions Psoriasis (p. 417) 1. Background • Chronic noninfectious autoimmune inflammatory disease • Occurs worldwide • Equal in both genders • 15-50 years (big range) – usually develops before age 40 • Vulgaris is Latin for “common” • Genetic system disease with immunologic basis • Frequently manifests in the skin and joints 2. Clinical Manifestations • Red raised patches/white layer • May or may not itch • Symmetrical • Distribution: scalp, elbows, knees, genital and sacral regions • May become systemic • Course unpredictable 3. Treatment • Suppress T-Cell Activation (topical steroids,intralesion injections,retinoids,keratolytic agents) • Promote Desquamation (UVL with topicals) • Systemic Treatments (Methotrexate and Cyclosporine) 4. Nursing Measures • Self-concept issues • Teaching about medications • Risk for infections • Control causative factors CHAPTER 26 Head and Neck Cancer (p. 491-496) 1. Incidence: • 2-3% of all malignancies • Men>women • May involve ⎫ Nasal cavity ⎫ Para-nasal sinuses ⎫ Nasopharynx ⎫ Oropharynx ⎫ Larynx ⎫ Oral cavity ⎫ Salivary glands • Most people have advance disease at time of diagnosis 2. Risk Factors: • Cigarette smoking (85% of cancers) • Alcohol • Occupational exposure to asbestos, wood dust, mustard gas, petroleum products • Chronic laryngitis • Voice abuse • Genetics • HPV infection • Poor oral hygiene 3. Manifestations • Early – vary with location of the tumor ⎫ Oral cavity – white (leukoplakia)/red (erythroplakia) patch in mouth, ulcer that does not heal, change in the fit of dentures ⎫ Lump in throat, change in quality of voice ⎫ Laryngeal - Hoarseness that lasts for more than 2 weeks ⎫ Sore throat (unilateral), otalgia (ear pain), swelling or lumps in the neck 4. Interprofessional Care • Diagnostic Assessment ⎫ Hx & Physical exam ⎫ Indirect pharyngoscopy and laryngoscopy ⎫ Endoscopy ⎫ Biopsy ⎫ Chest x-ray ⎫ Barium swallow ⎫ CT / MRI / PET scan • Management ⎫ Surgery o Vocal cord stripping – removal of outer layer of tissue on vocal cords (early stage) – does not change speech o Laser surgery – inserted to vaporize / remove tumor o Cordectomy – part/all vocal cords are removed (changes speech – hoarse voice(partial); loss of voice (full removal) o Partial or total laryngectomy – removal (full or partial) of larynx o Pharyngectomy – part/all of throat is removed o Lymph node removal with neck dissection o Tracheostomy – stoma / alternate pathway o Reconstructive procedures ⎫ Radiation therapy ⎫ Chemotherapy ⎫ Targeted therapy ⎫ Physical therapy ⎫ Occupational therapy ⎫ Speech therapy Laryngectomy 1. Manifestations • Hoarseness • Pain in throat • Dysphagia • Neck masses 2. Diagnosis • Visual exam of larynx • Biopsy • CT/MRI • Chest x-ray • Barium swallow study 3. Treatment • Early: partial laryngectomy, chemo, radiation, temp. trach., soft voice • Advanced cancers: total laryngectomy, radical neck, permanent trach. Stoma. No voice, unable to smell, decr. taste 4. Nursing management for laryngectomy • Watch for complications: ⎫ Airway obstruction ⎫ Hemorrhage – monitor VS ⎫ Carotid artery rupture ⎫ Fistula formation • Elevate HOB – decreases edema and reduces pressure on esophagus ⎫ NO FLAT BEDS • Flex neck forward • Trach/stoma care • Wound assessment/care • NG feedings – d/t location of surgery and complications of chemo and radiation 5. Nursing diagnosis for laryngectomy • Risk for Aspiration • Ineffective Airway Clearance • Risk for Impaired Gas Exchange • Impaired Nutrition: Less than Body Requirements • Risk for Infection - - - - - - - - - - - - - - - - - - -Metformin (Glucophage) • Biguanides • Decreases rate of hepatic glucose production • Augments glucose uptake by tissues, especially muscles • Most effective first line treatment for type 2 DM • Side effects: o Diarrhea, lactic acidosis • Nursing considerations: o MUST BE HELD 1-2 DAYS BEFORE IV CONTRAST MEDIA GIVEN AND FOR 48 HOURS AFTER • Drug Alert: o Do not use in patients with kidney disease, liver disease, or heart failure. Lactic acidosis is rare complication of metformin accumulation. o IV contrast media that contain iodine pose a risk of acute kidney injury, which could exacerbate metformin-induced lactic acidosis o To reduce risk of kidney injury, discontinue metformin a day or two before the procedure o May be resumes 48 hours after the procedure, assuming kidney function is normal o Do not use in people who drink excessive amounts of alcohol Take with food to minimize GI side effectsDiagnostics Urinalysis: pH, specific gravity, protein, glucose, nitrites, leukocyte esterase • Urinalysis PP 1024-1031 o First morning void (more concentrated/likely to contain abnormal constituents) o Examine urine within 1 hour – otherwise keep refrigerated ♣ Bacteria multiply ♣ RBC hemolyze ♣ Casts disintegrate ♣ Urine becomes alkaline (d/t urea splitting bacteria) • Creatinine clearance – 70-135 o Collect 24-hour urine specimen ♣ First specimen in morning discarded then every void collected o Must be refrigerated, iced, or some kind of preservative o Creatinine clearance closely approximates GFR o Also, good to do a blood serum creatinine test during that time period o Most accurate indicator of renal function o Measure of amount of active muscle tissue – more muscle = higher value o After age 40 – decreases every year by 1 mL/min/year • Normal urinalysis – MEMORIZE THESE! o Clear, amber o pH: acidic (4.0-8.0) o Specific gravity: 1.03-1.030 o BUN: 8-20 o Creatinine: 0.5-1.5 o GFR-Glomerular Filtration Rate: >60 o Protein: random protein (dipstick)- 0-trace, 24-hour protein (quantitative)- <150 mg/day o Glucose: none o Nitrites: none, presence indicates bacteriuria o Leukocyte: 0-5/hpf o Esterase: none, it is an enzyme present in WBCs, indicating pyuria • Dipstick urinalysis o Identify presence of ♣ Nitrites – indicates bacteria ♣ WBC’s ♣ Leukocyte esterase - enzyme present in WBC’s that indicate pyuria – pus in urine Hemoglobin A1c – PP 1115-1118, 1659 • indicates the amount of glucose linked to hemoglobin, also called glycosylated hemoglobin • Assesses long term glycemic control during the previous 3 months • Goal is below 7% • Nursing responsibility is to inform the patient that fasting is not necessary and that blood sample will be done Cystoscopy – pp1025-1030 • Inspects interior of bladder with a tubular lighted scope • UseS: insert ureteral catheters, remove calculi, obtain biopsies of bladder lesions, treat bleeding lesions • Lithotomy position is used • Procedure may be done using local or general anesthesia, depending on patient’s needs and condition • Complications include urinary retention, urinary tract hemorrhage, bladder infection and perforation of bladder • Nursing responsibility o Before: force fluids or give IV fluids if general anesthesia is to be used, ensure consent is signed, explain procedure, give preoperative medication. o After: explain that burning on urination, pink-tinged urine, and urinary frequency are expected effects. • Observe for bright red bleeding, which is not normal. Assist with ambulation because orthostatic hypotension may occur. Offer warm sitz baths, heat, & mild analgesics to relieve discomfort. • Endourologic procedures for stones • Flexible ureteroscope inserted to remove stones from renal pelvis/UUT • Endoscopic procedure – inspects interior side of the bladder – inserted through urethra • Can remove calculi, obtain biopsy specimens, treat bleeding lesions • Fluids usually given before the procedure – often give meds before as well • Burning during urination can occur after the procedure, urine can have a pink tinge, or inc frequency • Also, could have orthostatic hypotension DIAGNOSTICS [Show More]
Last updated: 2 years ago
Preview 1 out of 114 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$16.50
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Jul 04, 2020
Number of pages
114
Written in
Additional information
This document has been written for:
Uploaded
Jul 04, 2020
Downloads
0
Views
166