*NURSING > STUDY GUIDE > MATERNAL A 327 Exam 2 Study Guide complete | (Complete A guide) very helpful | Chamberlain College o (All)
MATERNAL A 327 Exam 2 Study Guide complete | (Complete A guide) very helpful | Chamberlain College of Nursing
Document Content and Description Below
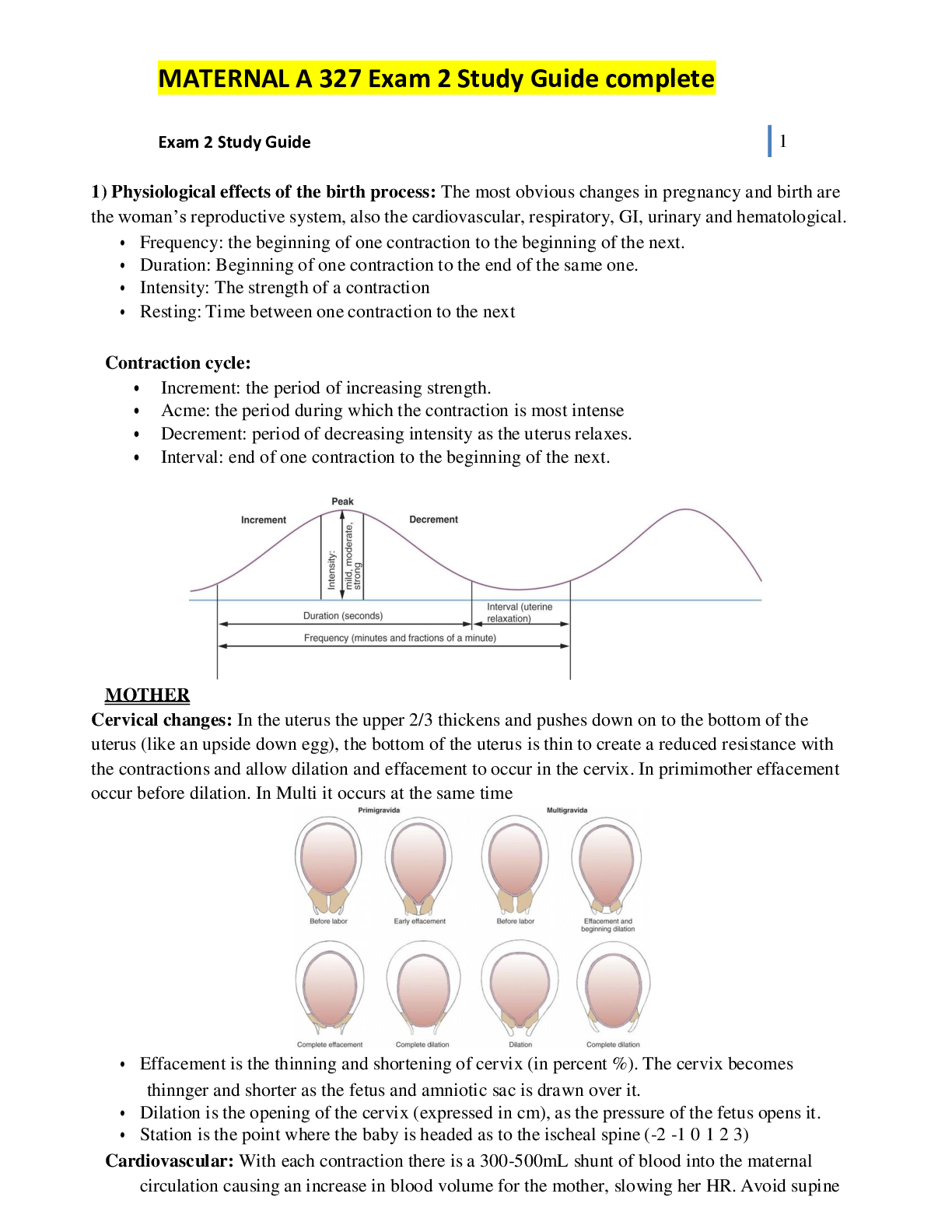
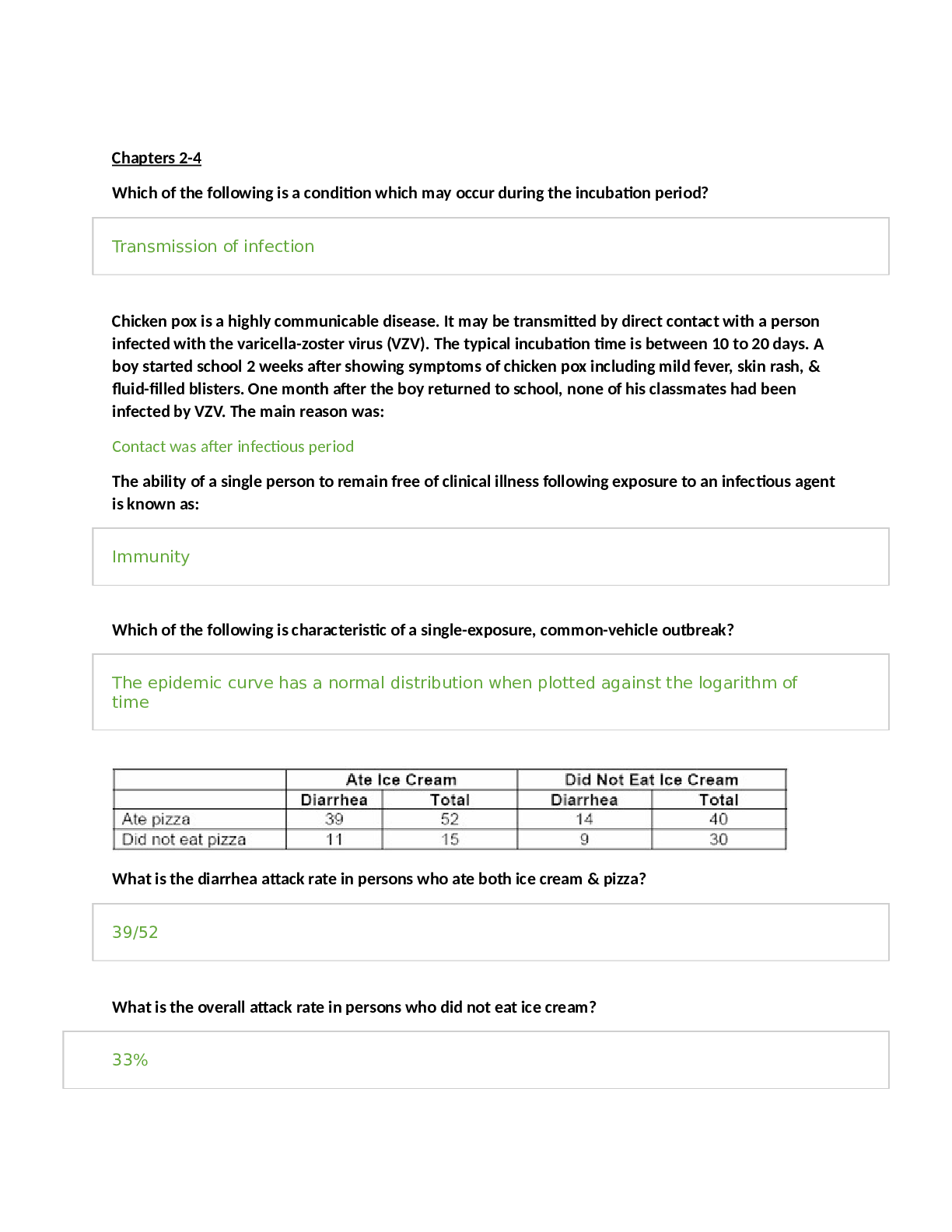
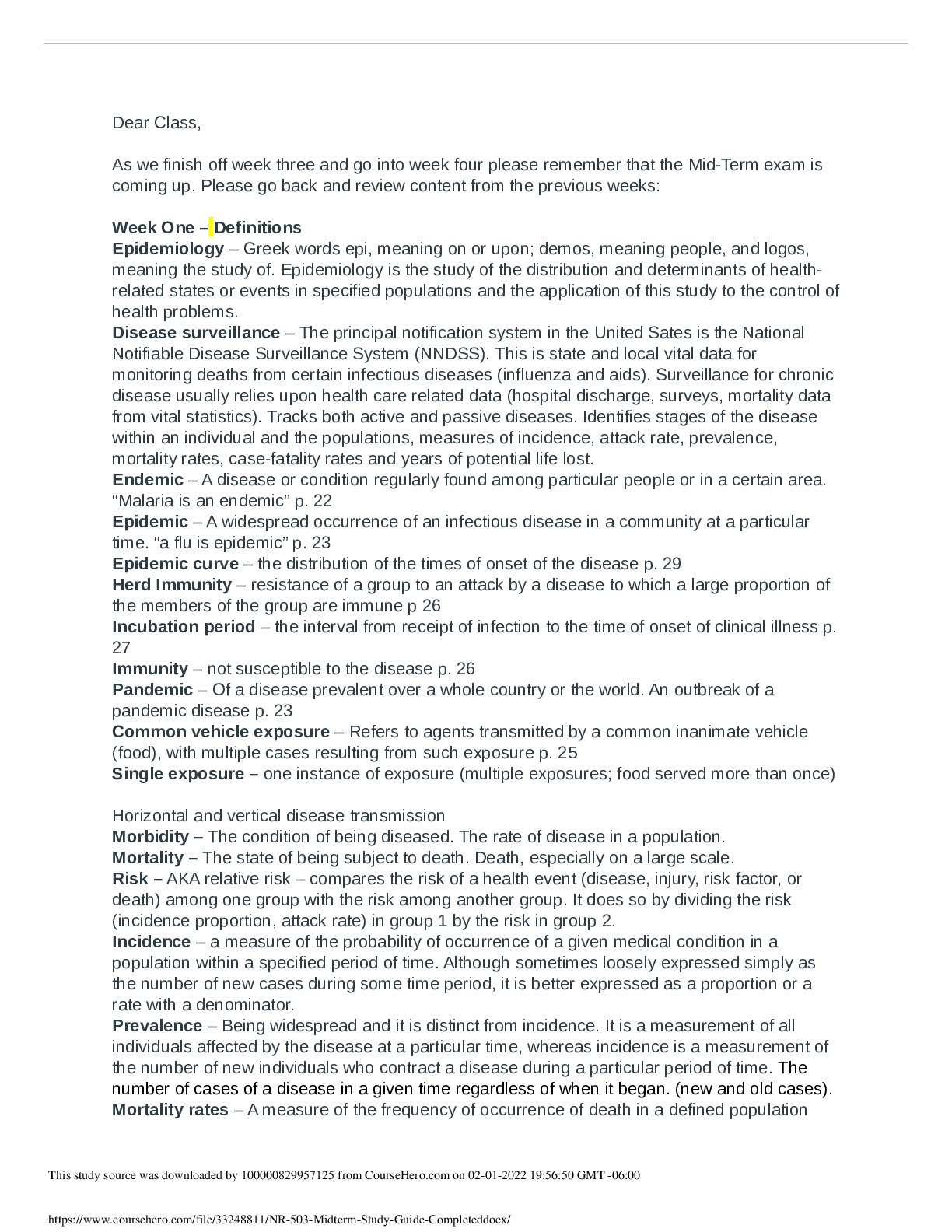
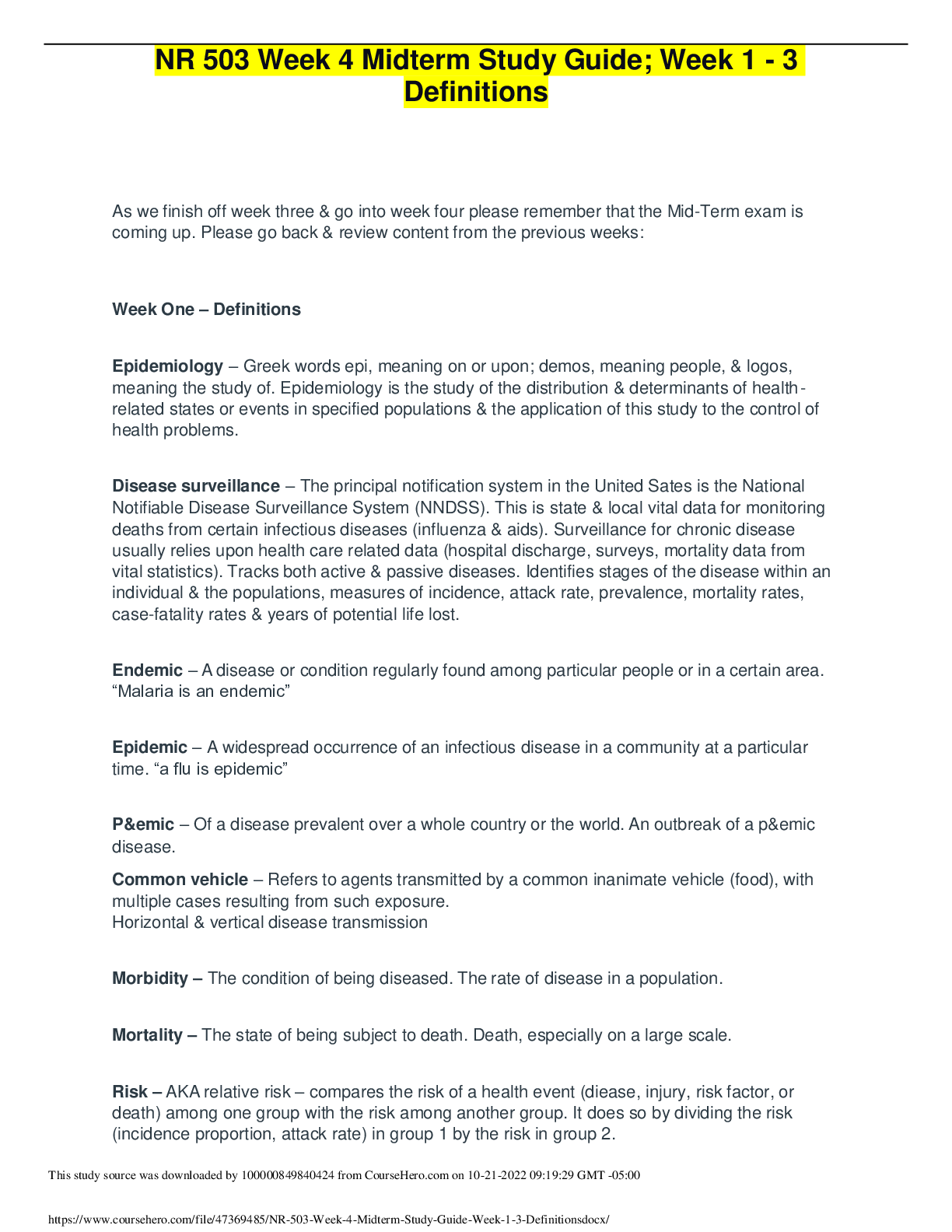
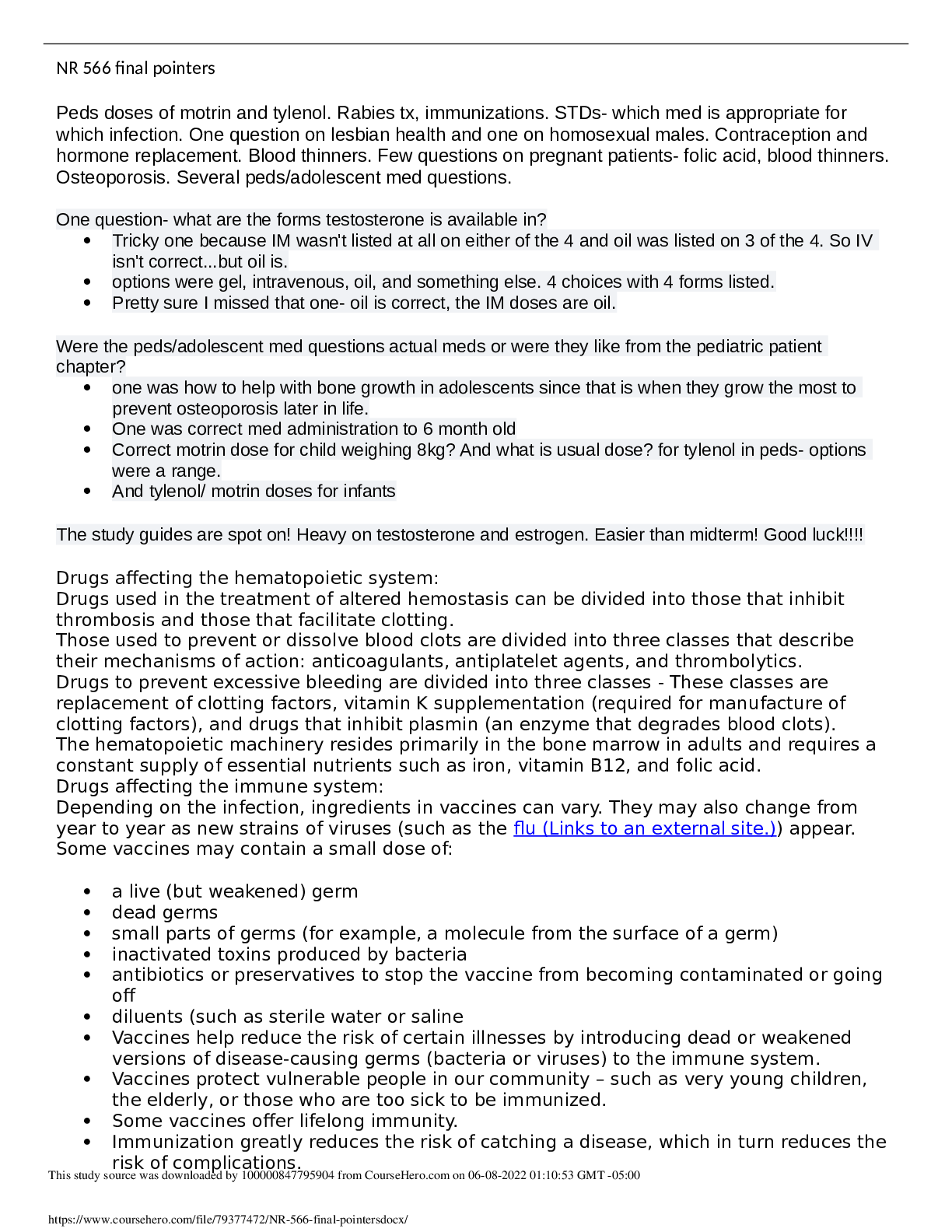
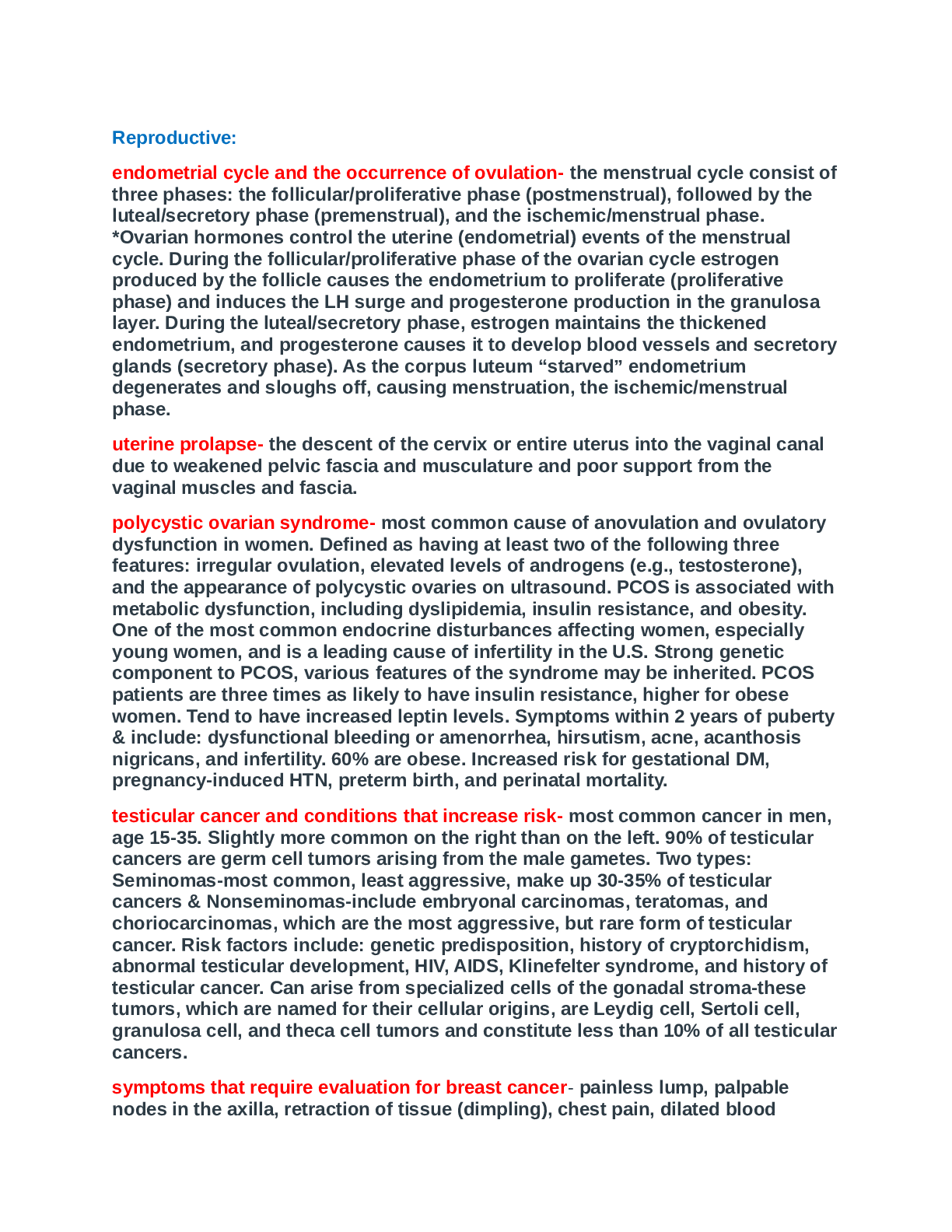
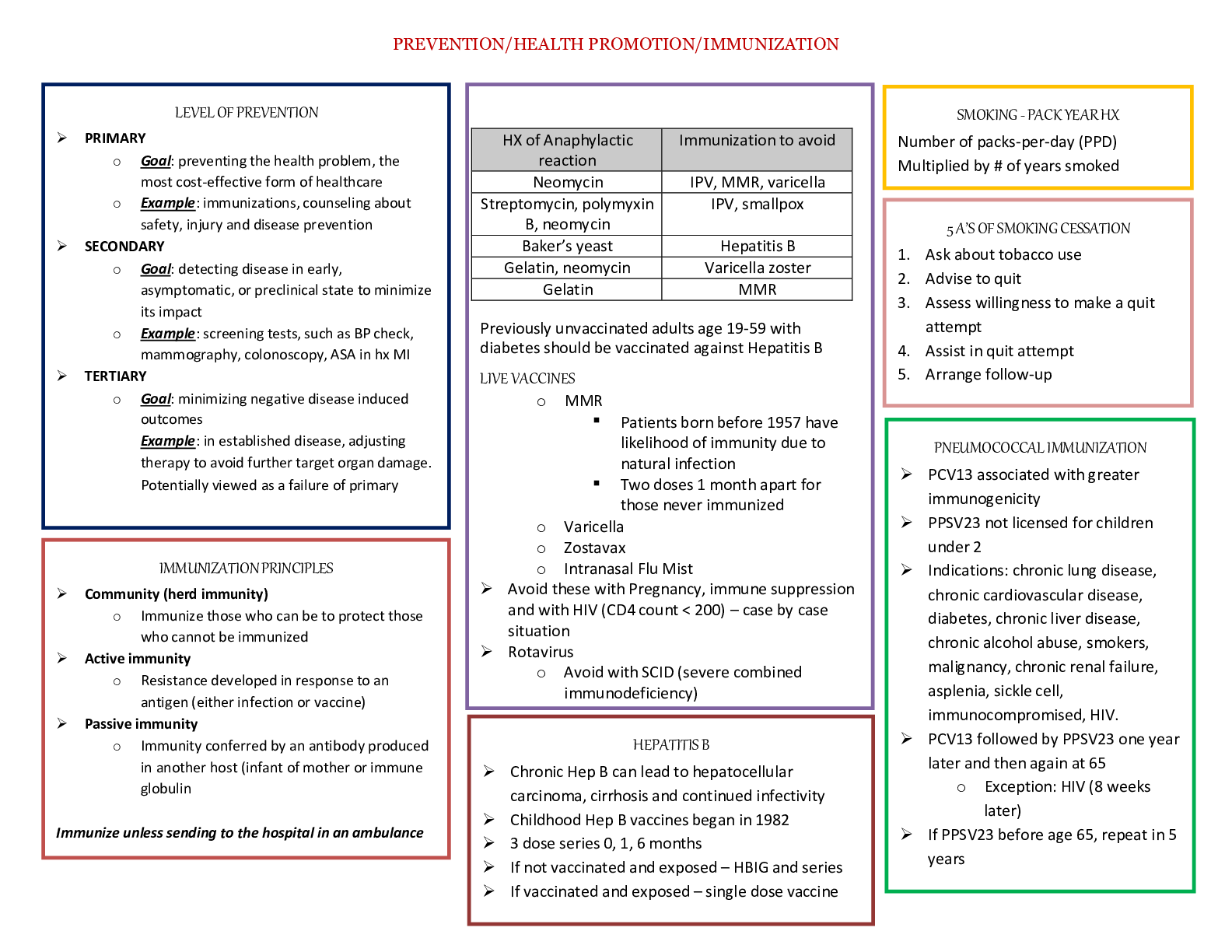
MATERNAL A 327 Exam 2 Study Guide complete Exam 2 Study Guide 1 1) Physiological effects of the birth process: The most obvious changes in pregnancy and birth are the woman’s reproductive syst... em, also the cardiovascular, respiratory, GI, urinary and hematological. • Frequency: the beginning of one contraction to the beginning of the next. • Duration: Beginning of one contraction to the end of the same one. • Intensity: The strength of a contraction • Resting: Time between one contraction to the next Contraction cycle: • Increment: the period of increasing strength. • Acme: the period during which the contraction is most intense • Decrement: period of decreasing intensity as the uterus relaxes. • Interval: end of one contraction to the beginning of the next. MOTHER Cervical changes: In the uterus the upper 2/3 thickens and pushes down on to the bottom of the uterus (like an upside down egg), the bottom of the uterus is thin to create a reduced resistance with the contractions and allow dilation and effacement to occur in the cervix. In primimother effacement occur before dilation. In Multi it occurs at the same time • Effacement is the thinning and shortening of cervix (in percent %). The cervix becomes thinnger and shorter as the fetus and amniotic sac is drawn over it. • Dilation is the opening of the cervix (expressed in cm), as the pressure of the fetus opens it. • Station is the point where the baby is headed as to the ischeal spine (-2 -1 0 1 2 3) Cardiovascular: With each contraction there is a 300-500mL shunt of blood into the maternal circulation causing an increase in blood volume for the mother, slowing her HR. Avoid supine position to prevent hypotension and position to increase blood return. Respiratory: During labor the mother is anxious, fatigue and exhausted so her RR is increased. This decrease pH and may cause Resp Alkalosis, so promote slow breathing or into a paper bag. GI: Slow motility can result in nausea and vomiting, also dry mouth. Ice chips may be used. Solid foods are not used to prevent aspiration incase general anesthesia needs to be used. Urinary system: Reduced sensation of full bladder. May be due to regional anesthesia or the contractions. Mother will not notice, and will create a discomfort, and occupies more space in the pelvis. Hematopoietic: About 500mL of blood is lost through vaginal delivery. Important to look at labs ( WBC, PLT) and also clotting factors to protect from hemorrhage and DVT. FETAL RESPONSE Placenta: During strong labor contractions, the blood supple decreases, so exchange occurs between contractions. The baby has hemoglobin F that transports more oxygen, also higher hemoglobin to carry more o2 and a higher cardiac output. With preeclampsia, GDM, or anemia these may be altered. Cardiovascular: HR should be between 110-160. Preterm babies will have higher. Pulmonary: Fetal lungs produce fluid to clear and allow normal air breathing after birth. Catecholamine’s toward term are released to help breathing. 2) Passenger is the fetus, membranes and placenta. Attitude: The relationship of fetal body parts to one another. The normal attitude is flexion to the neck, arms and legs. Fetal lie: The relationship of the longitudinal axis of the fetus to the longitudinal axis of the mother. Vertex: (head first) most common - longitudinal Breech: (buttocks first) –longitudinal. Sometimes occurs during preterm babies and babies with hydrocephalous and placenta previa (placenta in the bottom) Transverse: (laterally across uterus)\ Frank breech—This is the most common variation, occurring when the fetal legs are extended across the abdomen toward the shoulders. •Full (complete) breech—This is a reversal of the usual cephalic presentation. The head, knees, and hips are flexed, but the buttocks are presenting. •Footling breech—This occurs when one or both feet are presenting, Breech, and (3) shoulder. Exam 2 Study Guide 3 Breach’s 3) Normal labor: Should be between 37-42 weeks. Occurs when estrogen levels are higher than progesterone (progesterone relaxes), this increase in estrogen and relaxin promotes uterine sensitivity and help stimulate contractions. Then prostaglandins produced in the decidua start to prepare the uterus and cervix. Oxytocin is then released to help induce contractions. With the stretching, pressure and irritation of the uterus and cervix helps move the baby out. Brxton hicks contractions occur throughout the pregnancy, and then lightening occurs. As the womans body prepares for labor there is an increase in vaginal secretions as fetal pressure causes congestion of the vaginal mucosa. • As full term nears, the cervix softens because of the effects of the hormone relaxin and increased water content. These changes (ripening) allow the cervix to yield more easily to the forces of labor contractions. • Bloody show (mixture of cervical mucus and pink or brown blood from ruptured capillaries in the cervix; often precedes labor and increases with cervical dilation) may begin several days to a few weeks before the onset of labor, especially in the nulliparous woman, or it may not begin until labor starts. • Energy spurt occurs called “nesting” • Weight loss due to altered estrogen and progesterone ratio and causes excretion of extra fluid. 4) Stages of labor: Exam 2 Study Guide 5 Exam 2 Study Guide 7 Cardinal movement: The latent phase lasts through the first 3 cm of cervical dilation. Its length varies among women but is usually longer for the nullipara than for the multipara. The woman is usually sociable, excited, and cooperative. She is anxious as she realizes that these contractions are not Braxton Hicks contractions but the “real thing,” yet she is usually relieved that her pregnancy is finally about to end. The cervix dilates from 4 to 7 cm and at a more rapid rate than in the latent phase. The woman's behavior changes. She becomes more anxious and may feel helpless as the contractions intensify. The sociability that characterized early labor is gone and is replaced by a serious, inward focus. She is unlikely to initiate interactions unless she has specific requests. Her behaviors are typical of a person concentrating intently on a demanding task. Women who choose to take pain medication and regional analgesia usually do so during this phase. The nurse helps the woman maintain her concentration, supports her coping techniques, and helps her find alternatives for methods that do not work for her. The cervix dilates from 8 to 10 cm in this phase of the first stage, and the fetus descends further into the pelvis. The woman who does not choose epidural analgesia often finds the transition phase to be the most difficult part of her labor. She may be irritable and lose control. Her partner may be confused because actions that were helpful just a short time ago now bother her. The nurse can encourage the woman and her support person that the end of labor is near and help them use coping techniques most effectively. If premature bearing down is a problem, the nurse can help the woman blow outward with each breath until the urge passes. The second stage (expulsion) begins with complete (10 cm) dilation and full (100%) effacement of the cervix and ends with the birth of the baby. Duration of second stage labor also varies with whether the woman has an epidural. The woman often regains a feeling of control during the second stage of labor. Contractions are strong, but she may feel more in control and know that she is doing something to complete the process by pushing with the contractions. The word labor aptly describes the second stage. The woman exerts intense physical effort to push her baby out. Between contractions, she may be oblivious to her surroundings and appear to be asleep. She feels tremendous relief and excitement as the second stage ends with the birth of the baby. The third (placental) stage begins with the birth of the baby and ends with the expulsion of the placenta (Figure 12-14). This stage is the shortest, with an average length of 6 minutes). Four signs suggest placenta separation: • The uterus has a spherical shape. • • The uterus rises upward in the abdomen as the placenta descends into the vagina and pushes the fundus upward. • • The cord descends further from the vagina. • • A gush of blood appears as blood trapped behind the placenta is released. The fourth stage of labor is the stage of physical recovery for the mother and infant. It lasts from the delivery of the placenta through the first 1 to 4 hours after birth. The vaginal discharge after childbirth is called lochia (rubra, serosa, alba) Exam 2 Study Guide 9 5) Duration of labor: Differs from woman to woman. Parous mothers deliver more quickly than the nulliparous mother. Difference between true and false labor: FALSE LABOR Contractions Are inconsistent in frequency, duration, and intensity Do not change or may decrease with activity (such as walking) Discomfort Is felt in the abdomen and groin May be more annoying than truly painful TRUE LABOR Contractions Usually have a consistent pattern of increasing frequency, duration, and intensity Tend to increase with walking Begin in lower back and gradually sweep around to lower abdomen Discomfort May persist as back pain in some women Often resembles menstrual cramps during early labor 6) Issues for new nurses: Working with pain associated birth and people feeling pain. Nurses must feel compelled to relieve pain. They also must know how to feel with negative experiences maybe they had or maybe lack of personal birth. The unpredictability, intimacy especially for male nurses may make them feel uncomfortable. 7) Focused assessment: Used to determine the condition of the mother and fetus and whether the birth is imminent. • FHR is assessed and should be between 110-160bpm and regular. If electronic fetal monitoring is used then accelerations are a good sign and absence of declerations. • Important to assess for hypertension during pregnancy it is defined by greater than 140/90. • Temperature over 38C 100.4F suggest infection. • Mothers history, V/S, allergies, expected due date, last time to eat, status of membrane are all assessed and asked to the mother. • Fetal oxygenation: assessed by FHR, amniotic fluid rupture status, maternal V/S, contraction frequency, duration, intensity and resting interval. • Ask about pregnancy history, EDD, gravida/parity, allergies, membrane status, contractions, labor status, food intake, recent illness, medications, alcohol/tobacco, birth plans, support person, and cultural needs. • Labor status assessment: contractions, vag exam, membrane status, leopold maneuver, and pain assessment. • Physical assessment: general appearance, V/S, heart and lungs, abdomen, DTR, U/A • Lab test: CBC, blood type, serum test for syphilis, GBS, • Get consent signed. 8) Assessment after admission: Fetal assessment is perform to look at his well being. • FHR • Amniotomy: AROM- artificially rupture of fetal membrane. Membrane should be clear with bits of vernix. • Assess the amniotic fluid: Cloudy and yellow fluid may indicate infection. Meconium can indicate fetal distress such as hypoxia. TACO 9) Fetal oxygenation: the main assessment related to fetal well being are the following. FHR, amount and character of amniotic fluid and time, maternal v/s, and contractions (frequency, duration and intensity, resting) • Conditions associated with fetal compromise: FHR >160 <110, meconium, cloudy amniotic flui, excessive frequency or duration of contractions (reduces placenta blood flow), no uterince relaxation shorter than 30 sec, maternal hypotension/hypertension, and ever about 38/100.4. 10) Discomforts: • Provide soft indirect lighting. • Make sure that the temperature is how she likes it, they may also have a fan in the room because labor gets hot, along with cool towels. • Ensure that her room is clean; change the mothers sheets when they need to be changed (amniotic leak, vagina discharge, elimination). Also, • Mouth care, provide ice chips or hard sugar free candy to prevent dry mouth, also brushing the teeth and rinsing her mouth. • A full bladder is another discomfort, it may cause pain and will not be felt with an epidural, remind her to void. • Position her comfortably, and help her change position frequently to prevent pressure and discomforts. Also encourage her to stand up during first stage. 11) Nursing care during late intrapartum period: Nurse responsibilities include preparation of delivery table with sterile gloves, perineal cleansing, initial care and assessment of newborn. Administration of medication (pit). 12) Fetal oxygenation: 1) When there is normal maternal blood flow and volume to the placenta. 2) Normal oxygenation in maternal blood. 3) Adequate exchange of O2 and CO2 in the placenta. 4) An open circulatory path between the placenta and the fetus through vessels in the umbilical cord. 5) Normal fetal circulatory and oxygen carrying function. It is important that there is placental exchange, fetal circulation and FHR, the 5 fetal factors interact to regulate FHR: 1. Autonomic nervous system (sympathetic and parasympathetic- vagus nerve) 2. Baroreceptors (at the carotid arch- it stimulates the vagus nerve to slow) 3. Chemoreceptors (increase HR when there is low o2,pH or high o2) 4. Central nervous system (hypothalamus controls autonomic, para, sympathetic) 5. Adrenal glands (epinephrine, nonepi in response to stress and increase –sympatatetic) Exam 2 Study Guide 1 1 13) Electronic fetal monitoring and equipment: A Doppler transducer is used to detect baseline rhythm and changes in baseline. A fetoscope is reliable to detect dysrhythmias. • Advantages: shows how the fetus responds before, during and after contractions. • Limitations: Reduced mobility is a limitation of EFM. The woman is limited to her bed. Equipment: To assucultate the FHR the monitor must be place in the back of the fetus under his head. • Bedside monitor: like an ECG, may be printed and viewed. Checks FHR and mothers contractions. Also checks BP, HR, and o2 sat. • Paper strip: The data about the contractions and FHR response are printed. Uterine activity on the bottom and FHR on the top. 1 minute per blocks, 10sec per Small Square. • Remote surveillance: used at nursing station when the nurse is not at the bedside, and notes FHR, decelerations and end of paper. • Software: used and programmed to the proper use and interpretations of the FHR and uterine cx. • External fetal monitoring: secured to mothers abdomen with strap, require no membrane rupture or cervical dilation making them useful for woman who should not have devices place in the vagina or uterus such as in preterm. Slightly less accurate. • Tocotransducer: calculates changes in this signal an printes them as bells shapes on the lower grid, and FHR response on the top. However there are factors that cause changes such as fetal size, abdominal fat, maternal position, location of the transducer. • Scalp electrode monitor: detects electric signals from the fetal heart that is connected to the fetal scalp in through the vagina. It also may be put in the buttock if the baby is in breech. Places to avoid are in the face, fontanels, and genitals. it is screwed on, and taken off turning counterclockwise. • IUPC: Intrauterine pressure catheter: sense intrauterine pressure. Goes in the vagina and into the uterus and should be maintain and the kept at the same level of the transducer. 14) Evaluation of electronic fetal monitoring strips: Acceleration • An acceleration is an abrupt, temporary increase in the FHR that peaks at least 15 bpm above the baseline and lasts at least 15 seconds Accelerations are usually a reassuring sign, reflecting a responsive, nonacidotic fetus that is ≥32 weeks of gestation. Early Decelerations • Are mirror images of the contraction (lowest point in the fetal heart rate occurs with the peak of the contraction). Return to the baseline fetal heart rate by the end of the contraction. Maternal position changes usually have no effect on pattern. Are associated with fetal head compression. Are not associated with fetal compromise and require no added interventions. • Fetal head compression briefly increases intracranial pressure, causing the vagus nerve to slow the heart rate. Early decelerations are not associated with fetal compromise and require no intervention. They occur during contractions as the fetal head is pressed against the woman's pelvis or soft tissue such as the cervix. The early decelerations mirror the contraction, beginning near its onset and returning to the baseline by the end of the contraction, with the low point (nadir) of the deceleration occurring near the contraction's peak The rate at the lowest point of the deceleration is usually no lower than 30 to 40 bpm from the baseline. • Late Decelerations • Look similar to early decelerations but begin after the contraction begins (often near the peak). Nadir occurs after the peak of the contraction. Return to baseline after the end of the contraction. Reflect possible impaired placental exchange (uteroplacental insufficiency). Occasional late decelerations accompanied by moderate variability and accelerations are not ominous. Persistent late decelerations, especially with no accelerations and absent or minimal variability, should be addressed by nursing interventions to Exam 2 Study Guide 1 3 improve placental blood flow and fetal oxygen supply. The degree of fall in rate from baseline is unrelated to the amount of uteroplacental insufficiency. • Deficient exchange of oxygen and waste products in the placenta (uteroplacental insufficiency) may result in a pattern of late (delayed) decelerations. This nonreassuring pattern suggests that the fetus has reduced reserve to tolerate the recurrent reductions in oxygen supply that occur with contractions. The cause of uteroplacental insufficiency such as maternal hypotension may be acute. It may also occur with chronic conditions such as maternal hypertension and diabetes, which impair placental exchange. The FHR returns to the baseline after the contraction ends (Figure 14-12). They have a consistent appearance. The FHR may remain in the normal range and may not fall much below its baseline level. The amount of rate decrease from the baseline is not related to the amount of uteroplacental insufficiency. • Should be addressed by nursing interventions to improve placental blood flow and fetal oxygen supply. • Variable Deceleration • Conditions that reduce flow through the umbilical cord may result in variable decelerations. These decelerations do not have the uniform appearance of early and late decelerations. Variable decelerations also may be nonperiodic, occurring at times unrelated to contractions. Sharp in onset and offset. • Palpation is used to estimate contraction intensity and uterine resting tone when an external uterine activity monitor is used (see Procedure 13-2). Contraction intensity is described as mild, moderate, or strong. • Montevideo units (MVUs) may be used to describe contraction intensity in millimeters of mercury when an IUPC is used. The MVU is calculated by noting the contraction intensity in millimeters of mercury (mm Hg) above the resting tone and multiplying by the number of contractions in 10 minutes. For example, if a woman has three contractions in 10 minutes, each of which has an intensity of 110 mm Hg and a resting tone of 15 mm Hg, the result in MVUs is 285. Excess uterine activity during labor would be 400 MVUs Variability Variability denotes the fluctuations in the baseline FHR within a 10-minute window that cause the printed line to have an irregular rather than a smooth appearance 15) Nursing process in fetal oxygenation: Determine who is a low and risk woman. High risk will be assessed more frequent. (FHR, Uterine Cx, temperature, BP), think of potential problems. Promote fetal and maternal wellbeing, take corrective actions, support mom, report abnormalities, reassure mother and document 16) Nature of pain during birth: It is part of the normal birthing process, preparation time exist, it is self limiting and will end when the mother is done, the pain is not constant it is intermittent, and labor ends with the birth of a baby. 17) Adverse effects of excessive pain: Can cause fear, anxiety stimulating the sympathetic nervouse system and increasing BP and HR. this also causes vasoconstriction and increase in uterine muscle tone also raising mother BP. This may reduce blood flow to and from the placena and restrict o2 supply and waste removal. This will also reduce effectiveness of uterine contractions, slowing labor progress. Labor also increases a womans metabolic rate and her demand for O2, she will be hyperventilating so she will become alkalotic, this will result in fetal acidosis because of he turns into anaerobic metabolism cause. 18) Variables in childbirth pain: Previous childbirth experiences, anxiety and fear, culture. Other sources of pain include tissue ischemia, cerival dilation, pressure and pulling on pelvic structure, distention of the vagina, contraction intensity, fetal position, pelvic and cervical readiness, fatigue and hunger, the caregivers intervention and support system. 19) Nonpharmacologic pain management: Relaxation to reduce anxiety and fear, general comfort or using a cool cloth to relax in between contractions. Cutaneous stimulation such as self massages, or by others, counter pressure or acupuncture. Also hydrotherapy, Exam 2 Study Guide 1 5 mental stimulation such as imagery or focal pointing. Position change to decrease weight 20) Pharmacologic pain management: table 15-1 TABLE 15-1 DRUGS COMMONLY USED FOR INTRAPARTUM PAIN MANAGEMENT DRUG/DOSE COMMENTS Opioid Analgesics Meperidine (Demerol) 12.5-50 mg every 2-4 hours IV; may be given by PCA* Respiratory depression (primarily in the neonate) is the side effect. Fentanyl (Sublimaze) 50-100 mcg; may be repeated every hour; may be given by PCA Adjunct to epidural analgesia during labor (dose individualized) Onset is quick (5 minutes for IV administration), but dura action is short. Less nausea, vomiting, and respiratory depression occur with meperidine. Epidural use may cause pruritus. Butorphanol (Stadol) 1 mg every 3-4 hours; range 0.5-2 mg IV; may be given by PCA Has some narcotic antagonist effects; should not be give opiate-dependent woman (may precipitate withdrawal) o other narcotics such as meperidine (may reverse their a effects); also a respiratory depressant. Nalbuphine (Nubain) 10 mg every 3-6 hours IV; may be given by PCA Same as butorphanol. 5-10 mg may be given to relieve pruritus associated with epidural narcotics. Adjunctive Drugs Promethazine (Phenergan) 12.5-25 mg every 4-6 hours IV; dilute in 10-20 mL of 0.9% normal saline or 50 mL of normal saline; administer over 10-20 minutes Prevent and relieve nausea often associated with opioids Duration of action is longer than most narcotics; may en respiratory depressant effects of narcotics. Dilution and slow infusion into a large vein reduce risk fo necrosis. Diphenhydramine (Benadryl) 10-50 mg every 4-6 hours IV Given to relieve pruritus from epidural narcotics. Hydroxyzine (Atarax, Vistaril) 25-100 mg IM Z-track only See promethazine. Narcotic Antagonists Naloxone (Narcan) Action shorter than most narcotics it reverses; must obse recurrent respiratory depression and be prepared to give additional doses. • Some disadvantages to pain meds while labor is they may slow the contraction frequency and intensity and cause RR depresstion. • Epidurals (Marcaine/xylocaine) are popular because they black and provide anesthesia for labor and delivery without sedation of the woman. It placed between L3-L4 into epidural space. Contraindications are low platelets, allerigies, infections, scoliosis. It is important to assess for maternal hypotension, bladder distention. And may cause prolong second stage of labor. A postdural headache may occur due to leakage of CSF. It is alleviated when laying supine, blood patch or drinking caffeine. If RR depression occurs then we may give narcan. Other disadvanges are it slows the labor process, limited mobility, decrease contractions and may need IUPC. 21) Nursing care during obstetric procedure; An amniotomy is an artificial rupture of the amniotic sac, usually performed in conjunction with induction and augmentation of labor. And allows internal electronic fetal monitor. However some risk include prolapse chord, infection and abruption placente. • The nurses role is to obtain baseline v/s such as FHR. • With amniotomy place 2 or more underpads under womans buttocks. And explain procedure should not cause much pain. • Prepare disposable hook, sterile gloves, and lubricants. • Aftter amniotomy asses FHR for a full minute. • Document TACO. The quantity, color, and odor of the amniotic fluid are charted. The fluid should be clear (often with bits of vernix) and have a mild odor. A large amount of vernix in the fluid suggests that the fetus may be preterm. Greenish, meconium-stained fluid may be seen in postterm gestation or placental insufficiency. Fluid with a foul or strong odor, cloudy appearance, or yellow color suggests chorioamnionitis. Hydramnios (excessive volume of amniotic fluid) is associated with some fetal abnormalities. Oligohydramnios (abnormally small quantity of amniotic fluid) may be associated with placental insufficiency or fetal urinary tract abnormalities. • Adequate amniotic fluid is necessary for lung development throughout pregnancy. A fetus with oligohydramnios may have Resp problems. Induction of labor is performed when a continued pregnancy may jeopardize the health of the woman or fetus and labor and vaginal birth are considered safe. Labor induction is not done if the fetus must be delivered more quickly than the process permits, in which case a cesarean birth is performed. Induction is indicated in the following conditions •Conditions in which the intrauterine environment is hostile to fetal well-being (e.g., intrauterine fetal growth restriction, maternal-fetal blood incompatibility) • Spontaneous rupture of the membranes (SROM) at or near term without onset of labor, also called premature rupture of the membranes (PROM) if pregnancy is preterm, or less than 37 weeks (see Chapter 27). •Postterm pregnancy •Chorioamnionitis (inflammation of the amniotic sac) Exam 2 Study Guide 1 7 •Hypertension associated with pregnancy or chronic hypertension, both of which are associated with reduced placental blood flow •Abruptio placentae (large abruptions require immediate delivery; see Chapter 25) •Maternal medical conditions that worsen with continuation of the pregnancy (such as diabetes, hypertension, renal disease, pulmonary disease, heart disease) (seeChapters 25 and 26) •Fetal death Cervical ripening cytotec is used. But may not be used with a woman who had previod Csection because of hyperstimulation risk. Cytotec adverse reaction is hyperstimulation of uterine contractions. FHR should be closely monitored. • Indications to C section: Dystocia, cephalopelvic disproportion, hypertension, Diabetes, heart disease, or cervical cancer if labor is not advisable, genital herpes, previous csection, non reassuring FHR, prolapse umbilical chord, breech or transverse, abruption placentae. • Risk factors of Csection include infection, hemorrhage, UTI, thrombophlebitis or embolism, paralytic ileus, atelectasis, anesthesia complications. 22) Understand how each system changes during the postpartum period and why the changes occur: • Reproductive • Involution: a reduction of uterine size after delivery to its normal size. Should take up to 6 weeks. After delivery the fundus should be at the umbilicus or slightly above. Each day after it should go down 1 finger breath. • Fundus: the top portion of the uterus should be firm and contracting. A boddy uterus is soft and relaxed and is most likely due to hemorrhage. • Lochia: the discharge of blood and debri following delivery. Include Rubra (red), serosa (pinkish), Alba (white/clear). They should not contain clots. The amount may be increased by exertion or breast feeding. If increase in amount notify MD. Rubra, serosa, alba should each last 2 weeks, until 6th is gone. • Afterpains: caused by intermittent contractions following delivery. And occur in all woman, mostly in multiparous and breast feeding. • Cervix: soft and irregular, edematous, may appear bruised with multiple small lacerations. Loses 2-3cm after several days. • Vagina: low estrogen levels lead to decreased vaginal lubrication and vasocongestion for 6-10 weeks, leading to painful intercourse. • Abdominal wall: Soft and flabby with decreased muscle tone. Striae (stretch marks) are seen more in black woman. Diastisis recti separation of the rectus muscles of the abdomen may improve depending on womans activity. • Cardiovascular: Increase HR, CO, SV 1hr after delivery. The first 48hrs postpartum are the most dangerous in clients with heart Dz. Normal heart functions returns to prepregnancy in 2 weeks. • Diuresis occurs to excrete excessive fluid excess from pregnancy. • Increased fibrinogen for 1 week so risk of thrombophlebitis. • WBC may still be elevated . • H/H after labor may decrease due to loss of blood but should return normal 2 to 6 weeks after. Vaginal blood loss is about 500mL, Csection = 1000mL • At risk for orthostatic hypotension. • Temperature may be elevated the first 24hr after delivery. • Urinary: Increased bladder capacity and decreased bladder tone leads to decreased sensation and more chances of retention and infection. • Increase in diuresis 2000-3000mL accounting for about 5lb lost. • A full bladder contributes to preventing involution and uterine atony and post partal hemorrhage. • Fluids are also lost through diaphoresis. • GI: Hunger and thirst are common after birth. Constipation due to decreased peristalsis, dehydration. Give the patient stool softeners. Also risk for hemorrhoids, give tucks. • Endocrine: Estrogen and progesterone levels drop rapidly after delivery of placenta. Menstruation occurs 7-9 weeks after for nonlactating woman. Lactating woman may take up to 18 months. • Nipple stimulation leads to oxytocin release from pituitary. This stimulates the releae of prolactin from pituitary and causes production of milk. • Colostrum is produced 2-3 days after delivery , it is the first milk secreted and contains proteins and immunoglobbins. • Engorgement may occur with breast feeding, causing swollen breast , ice may be applied. • Musculoskeletal: Relaxin stops being produced so ligaments and cartilage do back to normal forms. And muscle tone gets restored. Mother may get carpal tunnel due to edema. Teach good muscle mechanics. 23) BUBBLEHE assessment: • Breast: palpate for engorgement or tenderness, symettry. Inspect nipples for redness, cracks, and erectility if nursing. If so, cold packs and cavage are appropriate. • Uterus: Palpate and determine if it is firm. Ask patient to void and position of fundus should be midline and should be at umbilicus. If it is boggy, a massage can be done. Each day fundal height drops a finger breath. Assess for incisions (edema, redness, discharge) • Bladder: ask the patient void after delivery. Assess frequency, if burning, urgency (UTI). Evaluate ability to empy bladder. Palpate for distention. A full bladder will prevent involution. Practice kegel. • Bowel: assess for passage of flatus, distention. Ask about last elimination, constipation, hemorrhoids. Auscultate BS. Encourage fluids, ambulation, fiber and stool softeners. • Lochia: Inspect type, quantity, amount and color. (Rubra, serosa, alba). Csection mother will have less. If heavy lochia, ask when was the last change and if recent notify the MD. Also if there is trickling, dribbling and oozing. Exam 2 Study Guide 1 9 • Episiotomy: Inspect for approximation, intact, redness, edema, is there bleeding? We can recommend a sitz bath, epifoam or tucks. • Homan sign: Assess for pain when dorsiflexion of the foot. Also inspect for edema, redness, warmth and pulse. If a positive finding tell patient not to walk. • Emotional: asses for pp blues, Pp depression, pyschosis by their emotions and psychological state or adjustment. 24) Nursing care after C-section: Assess pain levels, respirations and o2 sat. if the RR is between 12 and 14 notify MD, elevate HOB, administer o2. Assess abdomen for BS, distention, stools. Assess the incision site for infection, redness, edema etc. Urine output, amount, color and characteristics. And promote comfort 25) Process of becoming acquainted: Conisist of the parents and child bonding. May be 30-60mins after birth. Another process is attachment , but attachment occurs mutually and over time between the mother and the infant. Maternal touch behavior is another indication of acquaintance, when the mother strokes the baby with her fingertip, and also when she speaks to her baby in a quiet voice. And may hold the infant to her face nose to nose. Engrossment may occur in the father from the laboring experience. 26) Process of maternal adaptation: • Taking in phase: Occupied with other needs. The mother is focused primarily on her own need for fluid, food and sleep. She tells all her friends and family about her pregnancy to help her realize its all over. • Taking hold phase: Obsessed with body functions and has rapid mood wins. Guidance is needed now. The mother becomes more independent, she is concerned about managing her own body function and assumes responsibility for her own care. She also may verbalize anxiety about her competence as a mother. • Letting go phase: Mothering functions established. the parents let go of their expectations of their dream child and accept the real infant, may promote grief and may talk about it to see if feelings are mutual. 27) Major maternal concerns: • Body image may be a concern after mothers may lose their figure. Nurses need to educate that weight loss should be gradual and teach walking and gradual exercise to gain muscle tone. • Smoking: the majority of woman go back to smoking especially if stressed, have a partner who smokes or want to lose weight. They need to be educated on the hazards that smoking does to their baby. • Postpartum blues: A maternal adjustment reaction. May occur days after delivery to 2 weeks after. May be related to hormonal changes, fatigue, psychological stress related to infant dependency. The mother starts to have mood swings, anger, tearfulness, feeling of let down, anorexia and insomnia. It will resolve spontaneously. If not it can become PP depression. 28) Factors that affect family adaptation: Discomforts and fatigue and afterpains from birth. Also, insufficient knowledge such as in breast feeding, circumcision, not knowing infant signs, such as crying means hunger, cold, wetness or gentle stimulation. Also providing a safe environment. Previous experiences with other children that didn’t go so well may interfere with their child. Multipara mothers will feel more comfortbale than primis. Primis will be more fatigue from not sleeping, not spending time with her husband. However time alone with husband is sometimes needed. Another factor is lack of support system, single mothers have it hard because they have the child to take care off alone, along with the house duties. Support groups may be recommended. Other factors include mothers age, maternal and infant temperant. 29) Cultural influences on adaptation: Communication may be an issue between the nurse and mother, so an interpreter should be used. Respect for privacy, such as in middle eastern. Health beliefs play another factor such as rituals, cultural customs. For example, hygienic barriers, such as not showering, not taking medical advice, praying while bleeding, and resting after birth and allowing others to take care of the child. 30) Initiation of respirations: It is the first vital task for the newborn. At birth the infants first breath must force the remaining fetal lung fluid out of the aveoli into the interstitial space. The breathing is initiated by mechanical thermal , sensory and chemical factors that stimulate the resp center in the medulla to trigger. Diabetic mothers infatns will have slow lung maturation When the baby hits the air, they take a huge breath and lungs expand. ↓ O2, ↑Co2, ↓ pH = asphyxia sends signal to medulla to contract diaphragm. Exam 2 Study Guide 2 1 31) Cardiovascular adaptions: The clamping of the umbilical chord will increase vascular resistance and aortic blood pressure. The increased in pressure and decreased in pulmonary artery pressure because they being to dilate due to loss of placenta causes lung expansion and dilates pulmonary vessels, allow perfusion to rest of body. • Foramen ovale: connects right and left atriums. Closes 12 hours after when LA pressure is higher than RA pressure, the high pressure on the left side pushes the ovale to close. And now blood can go from RA> RV> PA>lungs> PV>LA>LV. Hoever it can take up to 3 months to close and sometimes longer. • Ductus arteriosus: the shunt between pulmonary artery and arch of aorta closes. Preventing entrance of blood from the PA, so the blood is directed to the lungs for o2. In uterus blood goes from PA Aorta.. at birth PA to lungs. Oxygen and prostaglandins help it close. When the Ductus Art senses high o2 and low prostaglandin levels (from the cutting of the placent), it closes. • Ductus venosus: the shunt that connects umbilical to IVC and bypasses liver. With the end of umbilical chord the blood flow can travel through liver as it normally would in adults. When the newborn takes his first breath the increase in oxygen causes the ductus arteriosus to close. Also fetal lung fluid moves from lung fields to interstitial and removed by lymph nodes. This helps decrease pulmonary pressure and allows for pulm dilation. However, low levels of O2 will dilate ductus arterosus and contrict pulmonary vessls and increase pressure in blood flow and lungs. Exam 2 Study Guide 2 3 32) Neurologic adaptation: Keeping the infant warm after delivery is very important. Their skin is thin, blood vessels are close to the surface. Methods of heat loss include: • Evaporation: when wet surfaces are exposed to air. It is important to dry the head thoroughly, as quickly as possible to prevent loss of heat. • Conduction: Movement of heat away from the body occurs when newborns have directed contact with objects that are cooler than the skin. For example, placing the infant on cold surface. Using warm blankets and objects help prevent this. • Convection: Is the transfer of heat from the infant to cooler surrounding air. When they are in intubators the circulating warm air helps keep them warm by convection. Provide a warm, draft free environment. • Radiation: The transfer of heat to cooler objects that are not in direct contract with the infant. Keep infants away from windows. • Nonshivering thermogenesis: The primary source of heat production in newborns is nonshiverying thermogenesis (NST), the metabolism of brown fat to produce heat. It is found around the kidney, adrenals, sternum, between scapulae , along the abdominal aorta. It begins when it detects temp of 95-96.8. It takes effect before a change occurs in core body temp. • A neutral thermal environment helps prevent heat loss or gain. And helps keep stable temp. • Hyperthermia: Infants respond poorly to hyperthermia because it increases metabolic demand (O2, glucose, energy) , vasodilation also occurs and you lose insensible fluids. • The newborn body contains 78% water. The adult contains about 60% 33) Hematologic adaptation: if the chord is not clamped for a few minutes after birth, blood from the placenta may enter the infants circulation and increase the total blood volume by 60%. • H/H is also higher in infants to enable fetal cells to transport more oxygen. • RBC have a shorter lifespan. If hemolysis occurs the RBC are broken down leaving bilirubin , and may cause jaundice. • Hematacrit above 65% may be polycythemia. It may increase the risk of jaundice and damage to the brain and other organs. Respiratory distress and hypoglycemia may occur. • WBC count could be at 15,000, then 2-3 days after drop to about 12,00. • Newborns are at risk of clotting issues due to lack of vitamin K. (that is why they receive it) (prothrombin). Vit K is synethesized in the intestines but food and normal flora are needed. If the mother took any Dilantin, phenobarbital, antitTB drugs during the pregnancy, their baby may have clotting issues. 34) GI system: The babys stomach has a capacity of 6mL/kg. The intestines are sterile while in the mother, that’s why they cannot make vit K. When their intestine are exposed to air and food, the normal flora starts to become established. Their intestine are bigger in proportion which makes them have excess fluid loss if they have diarrhea. Also they have weak cardiac spincter tone which is why they have lots of regurgitation while eating. • Enzymes: Pancreatic amylase enzymes to digest carbs are deficient for the first 4-6 months. Amylase is produced in salivary glands but little. They are also deficient in pancreatic lipase, limiting fat absorption. Lipase is however present in breast milk. And protein and lactose are also in breast milk and can easily become digested. • Stools: the first stoop excreted is called meconium. Consist of amniotic fluid, verniz, skin cells, air, bile. It is greenish-black with a thick, sticky, tarlike consistency. If meconium is not passed within 48hrs of birth, obstruction is suspected. The second stool passed by baby is called transitional stool (combination of meconium and milk stool). Then it is stools of the milk, Breast fed stools are seedy and the color and consistency of mustard with a sweet sour smell. Breastfed babies also poop more, (4- 5/day, up to 10). Formula fed babies feces will be firmer and odor like adults. 35) Hepatic system: During the 4-8 weeks of pregnancy glucose is stored as glycogen primarily in the fetal liver and skeletal muscle for after birth. Until they start become fed, they use that for energy. Glucose is also stored in the fetal for enegery during labor, breathing, heat production and movement. When it runs out, then the body uses glycogen until feedings. Many infants are at risk for hypoglycemia, if glycogen stores have been used up, poor nourishment, marcosomia and diabetic mothers, or cold temperature in the uterus. The liver is also incharge of the circulating unconjugated bilirubin (breakdown of RBC), this excess bilirubin can leave the vascular system and enter tissues (sclera, oral mucous Exam 2 Study Guide 2 5 membrane, skin) resulting in jaundice, because they mind to albumin and is eliminated in the stools. Encourage elimination , by feedings. Also a bili-mask. • Normal conjugation: Uncojugated bilirubin (bad one) is released from RBC lyse, then is converted to conjugated bilirubin by the liver and then it can be excreted. If that cannot happen then there is an increase of unconjugated bilirubin the the blood stream and body cause jaundice and brain injury. This can all start from a bruise, hematoma, RBC breakdown. • Physiological jaundice: The rate at which the bilirubin level in the blood rises and falls is important because it helps determine whether the rate for a particular infant is following the expected curve for age and birth weight. In physiologic jaundice, the bilirubin peaks at between the second and fourth days of life and falls to normal levels by 5 to 7 days. The bilirubin level rises higher and falls more slowly in Asian infants. Normal bilirubin in 3.5-5.0. newborns are at risk cause their RBC live less so there is more bilirubin due to increase RBC breakdown. • In nonphysiological jaundice, the most important difference is the time at which jaundice appears. It peaks between the second and fourth day of life and falls to normal levels by 5 to 7 days. • The most common cause of jaundice is in breastfed infants is insufficient intake. Not breastfeeding can increase bilirubin levels. Because it helps with elimination, when this does not occur the bilirubin builds up instead of being voided. • Treatment of breast milk jaundice includes close monitoring of TSB and at least 8 to 12 feedings each 24 hours. If bilirubin levels become too high, phototherapy is begun while the mother continues frequent breastfeeding. Interruption of breastfeeding is generally not recommended. Id total serum bilirubin is high, the hcp may order formula feeding for 12-48hrs whilte the mother uses a breast pump to maintain lactation. 36) Hyperbilirubinemia: Elevated bilirubin levels usually greater than 12 in a newborn. Therapy is aimed at preventing kernicterus which results in neurological damage from the bilirubin in the brain. S/s include jaundice, poor muscle tone, poor sucking reflex. Keep the newborn hydrated, facilitate early feedings, and prepare for phototherapy (the use of light to reduce serum bilirubin levels in the newborn) adverse reaction to this treatment include eye damage, dehydration. • Physiologic jaundice: is not present during the first 24hrs, it appears on the 2nd or 3rd day. • Pathological jaundice is present after birth usually within the first 24 hours. 37) Immune system: The neonate is less effective in fighting infecition. Leukocytes are delayed and are not efficient in killing invaders. Kids with infection will not display fever and leukocytosis, this occurs because the hypothalamus and inflam response are immature. The only signs may be activity, color, tone or feedings. They are susceptible to GBS, E coli. The mother passess on immunity in the last trimester and throughout breast feeding. At birth the infant may have 50-80% of the immunity. • IgG: only immunoglobin that crosses the placenta, starts in the 1st trimester. Provides immunity to bacteria, toxins, and viruses to which the mother has developed immunity. • IgM: first one produced by the body when the newborn is challenged. Protects against gram negative bacteria. Begins a few days after birth as a result to exposure to the enviorment. Does not cross placenta because its too large • IgA: important in protection of the GI and respiratory systems and newborn are particularly susceptible to infections. • IgG is the only one that crosses the placenta. The rest are passed on from breast feeding from the mother. Or actively acquired withing 4-6months of life. Breast feeding can go as long as mom wants and protects them from flu, mumps and chickenpox. 38) Psychosocial adaptation: At first infants will appear awake, alert and interested in their sorroundings. RR rate Is as high as 80, HR up to 180, crackles, retractions nasal flaring and mucous secretions may be present. Vital signs then gradually slow down after they take a deep sleep that may last several hours. When they wake up they enter the 2ns period of reactivity. V/S may increase again and may appear cyanotic with periods of apnea. • Quiet sleep state: RR is quiet , regular and slow in deep sleep, with no response to stimuli. Exam 2 Study Guide 2 7 • Active sleep state: ligher sleep, they move extremities, stretch, change facial expression, make sucking movements and fuss. REM sleep occurs. RR increases • Drowsy state: Transitional stage between sleep and waking similar to that experienced by adults as they awaken. Move slowly and lazy, and may want to go back to sleep • Quiet alert state: best time for bonding, infants focus on people and objects, respond to stimuli and enviorement. • Active alert: fussy state, restless, fast RR and HR. May have hiccups, regurgitation, seem more aware of feeling od discomfort. • Crying state: continuous and alerting cry with active body movements, does not respond to stimuli. May need comforting in order to feed or have activites. 39) Early focused assessment: Include cardiorespiratory status, thermoregulation and presence of anomalies. If the mother received narcotics late in labor , depression of the fetal CNS may interfere with RR. Preterm infants may not produce enough surfactant and may get atelectasis. • Airway: assess airway at least every 30mins until the infant has been stable for 2hrs. the normal RR is 30-60, and should be counted for a full minute. Periodic breathing (pauses in breathing lasting 5-10seconds, followed by rapid respirations for 10- 15seconds) occur in full term infants for the first few days, but is also seen in preterm. Apnea for more than 20seconds with cyanosis, and HR changes are abnormal. It is ok to hear crackles in the lungs (fetal fluid has not yet been eliminatd). Tachypnes (over 60RR) is the most common sign of resp distress, its ok for the first hour and during the second period of reactivity but not after. Occasional retractions after birth are ok, but not if it continues are the first hour. Intermittent nasal flaring is normal for the 1st hr, if longer than Resp problems. Central cyanosis is not normal. To determine diff between cyanosis and bruising apply pressure , cyanosis will blanch. Acrocyanosis is bluish color in the extremities and is normal for the first day. Cyanosis may appear while eating because of uncoordinated sucking, swallowing, and breathing. Infants that become cyanotic with exertion may have congenital heart defects. Persitant grunting may be a sign of resp difficulty. Seesaw respirations means respiratory difficulty. Chest expansion should be equal unless a pneumothorax. Assessment of choanal atresia (nasal blockage) is important because they mainly breathe through their nose, except when crying, they may become pink when crying and cyanotic when quiet. Pallor can be hypxia. Reddish color can be polycythemia and can lead to jaundice. • Heart: the heart should be assessed for a full minute, should be between 120-160. It should be assessed once every 30min until 2hrs. Murmurs are temporary and result from incomplete transition from fetal to infant circulation. Murmur are common until ductus arteriosus closes. If their femoral pulse is weaker than their brachial it can be coarctation of the aorta, a congenital heart defect. Blood pressure is taken on all extremities and unequal bp, pulse, can mean heart defects. The average bp should be 65-95/30-60, at 2 months it becomes stable for the 1st year. Cap refill is check at the chest, abdomen or extremity and should return within 3-4 seconds. • Thermoregulation: Should be assessed every 30mins until stable for 2hrs. Then again every 4hr , and then 8hr. the most common method is axillary, and should be 97.7- 99.1. • Anomalies : The head is palpatd to assess the shape and identify abnormalities. Molding are the changes in the shape of the head that allow it to pass through the birth canal. Caused by the overriding of the cranial bones at the sutures during the 2nd stage of labor. If separation of suturs are prolonged It can be due to high ICP. However a hard rigid area may indicate premature closure and may limit brain growth and head shape, craniosynostosis. The anterior fontanel is a diamond shaped area where the frontal and parietal bones meet (4-5cm) they close at about 18months of age. The anterior fontanel should be flat and soft, bulging of fontanel while crying is normal , but at rest can be high ICP. A depressed fontanel can be dehydration. Caput succedaneum is edema in the head, may occur when the vaccum is used. Cephalohematoma is bleeding between the periosteum and skull on both sides of the head. Cephalohematoma may take 6-8 weeks to resolve , because of the breakdown of RBC within the hematoma jaundice can occur. The face is examined for symmetry, facial features and movement, ear placement and maturity, eyes assessed for inflammation or edema. Neck and clavicle should be assessed to see if baby can turn head, webbing can be turner syndrome or downies. The umbilical cord should contain 3 vessels (AVA), if 2 it can be chromosomal defects or renal defects. The baby should be able to move extremities equally, they should be able to flex and resist extension, poor muscle tone can create a floppy infant can be due to poor oxygenation, assess for crepitus, lumps, swelling and lack of use. Paralysis of shoulder and neck can occur from brachial nerve plexus injury. A single crease along the base of hand down middle finger can be down syndrome. Hips are assessed for fracture or dysplasia. The use of barlow and ortolani test are used for hip instability in the newborn period. Both legs should abduct equally , hip clicking is normal but a “clunk” means the femoral head has moved into the socket. Assess the vertebrae for defects (spina bifida, meningocele). Weight can range from 2500-4000g. and lose about 10% of their weight during the first few days of life (meconium, loss of fluid, urine) then they regain weight after 14days. The length is measure from top of the head to heal , average is 45-55cm. the diameter of the head is measured around the occiput and eyebrows. The normal range is 32-38cm. the chest circumference is about 2-3cm smaller. Gonorrhea in the mother can cause infection of the infant in labor resulting in ophthalmia neonatorum blindness, all newborns get prophylactic antibiotic. Strabismus and cataracts are also assessed. Exam 2 Study Guide 2 9 • Other neuro assessment: newborn is assessed for tremors or jitterness, it can be a sign of hypoglycemia. If it is not the BG, then it can be calcium levels or prenatal exposure to drugs. Also a catlike cry is abnormal neurologically. • Billirubin: assess for jaundice every 8-12 hours and watch for it development, particularly in infants at risk for hyperbilirubin, it begins in the head and moves down, usually seen when levels are 5-7. Obtain TSB within 24 hours. • GI: check the mouth for thrush, appears 1-2 days after birth (candida) , usually if mother has yeast infection while birth, the infant is treated with nystatin suspension. Also check for cleft palate. And ability to suck and assess the feeding while breastfeeding. To decrease regurgitation of stomach, an initial formula feeding should be nomore than 1oz. assess abdomen for soft, rounded and should protrude slightly and not distended. A scaphoid abdomen can be diaphragmatic hernia (intestine are located in chest cavity instead of abdomen). Assess stools for color, type and consistency. Meconium stools are dark-green-black. A water ring should Exam 2 Study Guide 3 1 never be present around the solid part of any stool, it can mean a formula intolerance or infection. • GU: Kidneys have the most defects, its associated with with 1 umbilical chord artery. The infant should urinate 12-24 hrs after birth, if not then this may be abnormal, document it.. 6 wet diapers a day are a good sign, and uric acid crystals that cause diaper pinkish/redish may occur for first couple of days till kidney matures. Vaginal bleeding, pseudomenstruation may occur from sudden withdrawal from mothers hormones. Hymenal tags are normal . ensure meatus and vagina are present. The mal scrotum should be pendulous at term and be dark brown from hormones. • Intergumentary: their skin is fragile and sensitive, they may develop rash. The color should be pink or tan. Red is seen in preemie and/or polycythemia. Acrocyanosis can be poor peripheral circulation. Vernix may be seen in preemie and postterm may have none. • BirthMarks Mongolian spots are bluish-gray marks that resemble bruises on the sacrum, buttocks, arms, shoulders, and other areas. Mongolian spots occur most frequently in newborns with dark skin: they are seen in 96% of African- Americans, 85% of Asians, and 46% of Hispanics • A nevus simplex is also called salmon patch, stork bite, or telangiectatic nevus . It is a flat, pink discoloration from dilated capillaries that occurs on the eyelids, just above the bridge of the nose, or at the nape of the neck.. • Nevus flammeus (port-wine stain) is a permanent, flat, pink to dark reddish-purple mark that varies in size and location and does not blanch with pressure • Nevus vasculosus (strawberry hemangioma) consists of enlarged capillaries in the outer layers of skin. It is dark red and raised with a rough surface, giving a strawberry-like appearance. • Café-au-lait spots are permanent, light-brown areas that may occur anywhere on the body. • Ballard score is used to assess gestational age based on neuromuscular and physical characteristics (between week 2044), its most accurate when perform withing 12 hours of birth. 40) Early and ongoing care: Adminstration of vit K, because infants lack clotting factos without normal flora in intestines. Eye ointment (erythromycin) is used prophylactically to help prevent infection. But if mother is currently infected the prophylactic treatment is not enough, the infant will needs additional antibiotics. Also heat prevention should be ongoing, dry the wet infant quickly with warm towels to prevent heat loss, and drying the hair. When you place baby in heat warmer set the servocontrol between 96.897.7, and attach the probe to monitor temp. additionally, the infant may need extra clothing or two blankets, or warm linens. Also provide chord care, it should be checked for bleeding or oozing during early hours after birth. Should be clamped securely with no skin caught in it. Purulent drainage or redness or edema indicates infection. It becomes brownish black 23 days, and then falls off 1014 days after. Parents need to be taught that redness or discharge may be infection. Educate mothers to place babies on back to sleep to prevent SIDS. 41) Application of nursing process: If the infant needs suctioning, position him on his back with head in neutral position, use bulb syringe. Suction the mouth first because the infant may grasp when the nose is suctioned causing aspiration of mucous or fluid in the mouth. Then suction nose. Do not suction for more than 5sec at a time to avoid trauma Exam 2 Study Guide 3 3 and bradycardia. Also, important to assess for signs of hypoglycemia and maintain glucose levels. If they do not have enough glucose they may experience a drop in temperature and lead to resp distress. Also assess for jaundice, if so educate the importance of feedings to pass stools. Explain that giving water to jaundiced pateitns does not stimulate stool excretion and should be avoided. Breast feeding mothers infant should poop 4x a day, formula atleast once. 42) Commonly screened conditions: PKU – infant cannot metabolize amino acids, such as in protein foods or milk, treatment is started by the 3rd week with low PKU diet. Congenital hypothyroidism is also screen, s/s include hoarse cry, large fontanels and tongue, slow reflexes, abdominal distention, lethargy and feeding problems and lead to intellectual disabilityes. Other test are for Galactosemia, hemoglobinopathies, congenital adrenal hyperplase. 43) Latch scoring tool: 44) Assisting with the first feeding: Early breastfeeding stimulate prolactin earlier for milk production. Help move the mom to fowler position, show her how to hold breast. Observe infants response to the feeding and watch for signs of cyanosis, choking (indicates problems). Help the mom to a comfortable position, give pain meds because pain or awkward position tires the mom. Tell her to cradle or cross cradle the infant. She may use pillows to increase comfort , behing the mother head or under the child. Elevate infant to nipple to prevent him from pulling and causing soreness. The infants head and body should directly face the breast with the infants nose, cheeks, an chiin lightly touching the breast. Neck flex to make swallowing easier, ear shoulder and hip should be aligned. The mothers hand should be in “C” position or “V”. stroke nipple in babies lips till they open, and ensure baby is sucking with a kaah swallowing sign, to stop feeding use finger to insert in corner of babies mouth to prevent nipple trauma. Feedings normally are every 3 hours, for about 1015 mins on each side. Exam 2 Study Guide 3 5 45) Common breastfeeding problems: Sleep infant, nipple confusion once the mother has introduced bottle feeding, the baby confuses sucking technique or tongue movement. Suckling problems when the nipple is poorly positioned In babys mouth, engorgement may occur (swelling or fullness of breast), it peaks about 7296hrs after giving birth. It is due to congestion, increased vascularity, accumulation of milk and edema. Usually occurs when feedings are delayed, too short or infrequent. Brest become edematous, hard and tender, areola becomes hard and flat. To help with this the use of cold and heat. Cold is to control swelling and edema, and heat to promote vasodilation and milk flow. Massage them also to release oxytocin andincrease milk release. Also recommend a well fitting bra. If the pain persist they may take Tylenol, advil etc. other issues may be cracked painful nipples, flat/inverted nipples and plugged ducts, illness in the mother or drugs that interfere with milk production. 46) Circumsion care: • Observe the circumcision site at each diaper change, and check the amount of bleeding. Call the physician if more than a few drops of blood are present with diaper changes on the first day or any bleeding thereafter. • Continue to apply petroleum jelly to the penis with each diaper change for the first 4 to 7 days or as directed by your pediatrician. If a PlastiBell ring was used, do not use petroleum jelly because it might make the ring fall off too soon. • Keeping the circumcision site clean is important for healing. Squeeze warm water from a clean washcloth over the penis to wash it. Pat gently to dry the area. Fasten the diaper loosely to prevent rubbing or pressure on the incision sitE • Expect a yellow crust or scab to form over the circumcision site. This is a normal part of healing and should not be removed. The scab will fall off within 7 to 10 days. If a PlastiBell ring was used, the plastic rim will fall off in 10 to 14 days (AAP, 2011). If it does not fall off by that time or falls off sooner, notify your physician. Watch for signs of infection such as fever or drainage that smells bad or has pus in it. Call your physician if you suspect any abnormalities. The circumcision site should be fully healed in approximately 10 days. 47) Nutritional Needs of the Newborn Calories The full-term newborn needs 39 to 45 kilocalories per pound of body weight (kcal/lb) (85 to 100 kilocalories per kilogram of body weight [kcal/kg]) each day if breastfed and 45 to 50 kcal/lb (100 to 110 kcal/kg) if formula fed (Blackburn, 2013). Infants should be evaluated for feeding problems if weight loss exceeds 7%, if weight loss continues beyond 3 days of age, or if the birth weight is not regained by 10 days of age in the term infant . APGAR Exam 2 Study Guide 3 7 Scoring [Show More]
Last updated: 2 years ago
Preview 1 out of 38 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$16.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Aug 24, 2021
Number of pages
38
Written in
Additional information
This document has been written for:
Uploaded
Aug 24, 2021
Downloads
0
Views
75








.png)
.png)






