Common Infections
1. Impetigo
Impetigo is a superficial bacterial infection of the skin. It is classified into primary
impetigo when there is a direct bacterial invasion of previously normal skin or secondary
impetig
...
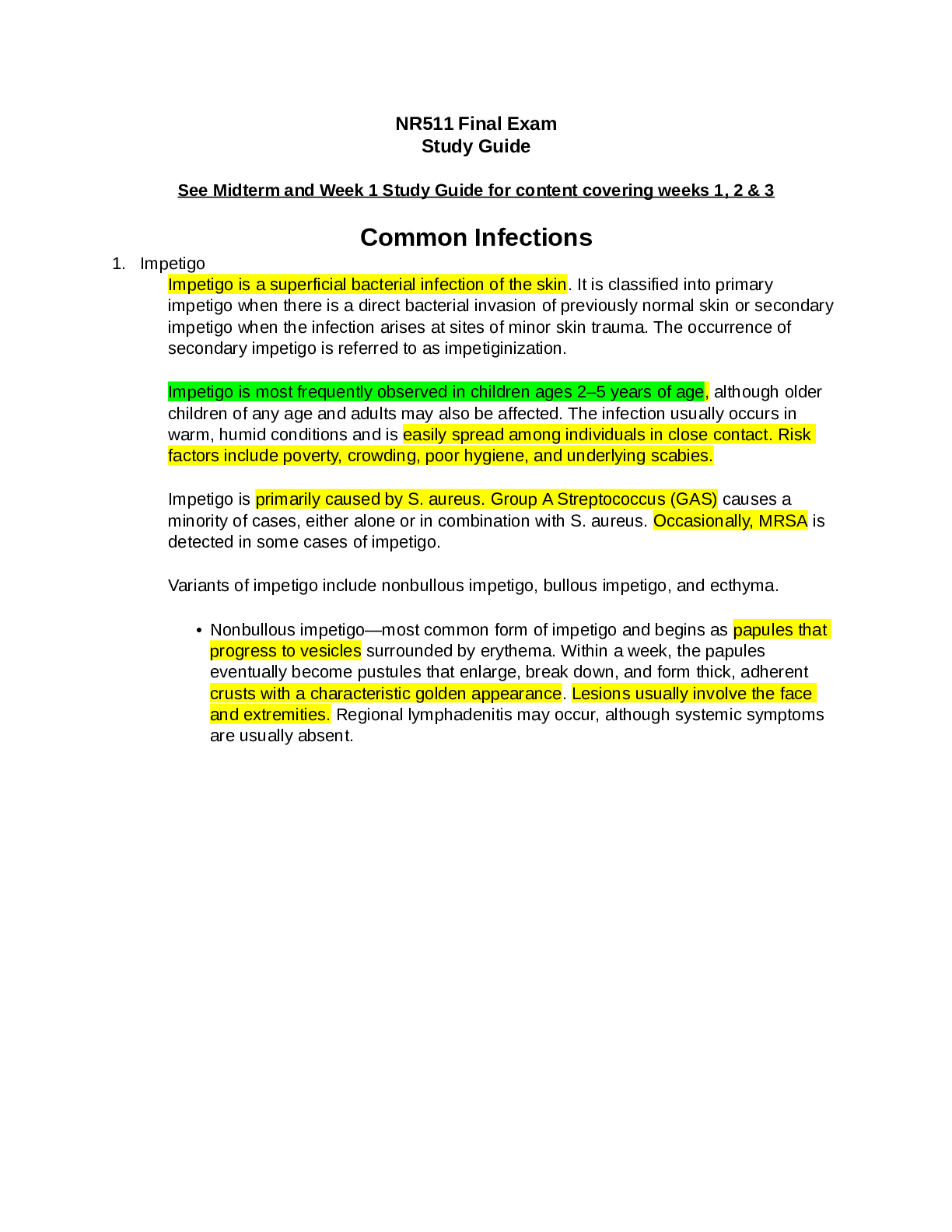
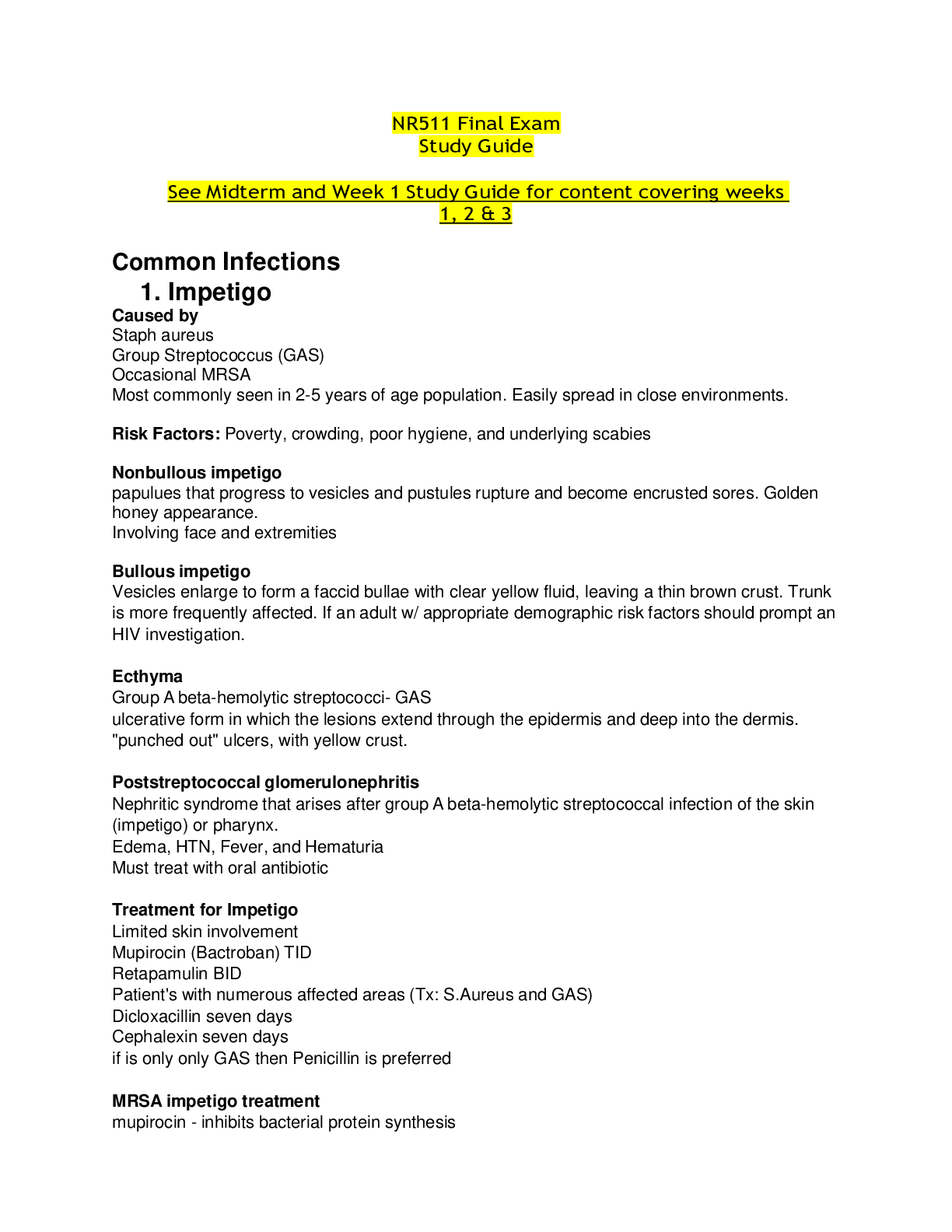
Common Infections
1. Impetigo
Impetigo is a superficial bacterial infection of the skin. It is classified into primary
impetigo when there is a direct bacterial invasion of previously normal skin or secondary
impetigo when the infection arises at sites of minor skin trauma. The occurrence of
secondary impetigo is referred to as impetiginization.
Impetigo is most frequently observed in children ages 2–5 years of age, although older
children of any age and adults may also be affected. The infection usually occurs in
warm, humid conditions and is easily spread among individuals in close contact. Risk
factors include poverty, crowding, poor hygiene, and underlying scabies.
Impetigo is primarily caused by S. aureus. Group A Streptococcus (GAS) causes a
minority of cases, either alone or in combination with S. aureus. Occasionally, MRSA is
detected in some cases of impetigo.
Variants of impetigo include nonbullous impetigo, bullous impetigo, and ecthyma.
• Nonbullous impetigo—most common form of impetigo and begins as papules that
progress to vesicles surrounded by erythema. Within a week, the papules
eventually become pustules that enlarge, break down, and form thick, adherent
crusts with a characteristic golden appearance. Lesions usually involve the face
and extremities. Regional lymphadenitis may occur, although systemic symptoms
are usually absent.
• Bullous impetigo—Bullous impetigo is seen primarily in young children in which the
vesicles enlarge to form flaccid bullae with clear yellow fluid, which later becomes
darker and ruptures, leaving a thin brown crust. The trunk is more frequently
affected. Bullous impetigo in an adult with appropriate demographic risk factors
should prompt an investigation for previously undiagnosed human
immunodeficiency virus (HIV) infection.
• Ecthyma—This form of impetigo, caused by group A, beta-hemolytic Streptococcus
(Streptococcus pyogenes), consists of an ulcerative form in which the lesions
extend through the epidermis and deep into the dermis. Ecthyma resembles
"punched-out" ulcers covered with yellow crust surrounded by raised violaceous
margins.
Poststreptococcal glomerulonephritis is a serious complication of impetigo (ecthyma).
This condition develops within 1–2 weeks following infection. Poststreptococcal
glomerulonephritis manifests with edema, hypertension, fever, and hematuria.
The diagnosis of impetigo often can be made on the basis of clinical manifestations.
A Gram stain and culture of pus or exudate is recommended to identify whether S.
aureus and/or a beta-hemolytic Streptococcus is the cause. However, treatment may be
initiated without these studies in patients with typical clinical presentations.
Bullous and nonbullous impetigo can be treated with either topical or oral therapy.
Topical therapy is used for patients with limited skin involvement whereas oral therapy is
recommended for patients with numerous lesions. Unlike impetigo, ecthyma should
always be treated with oral therapy.
Benefits of topical therapy include fewer side effects and lower risk for contributing to
bacterial resistance compared with oral therapy. Topical choices to treat impetigo include
the following medications for 5 days.
• Mupirocin three times daily
• Retapamulin twice daily
Extensive impetigo and ecthyma should be treated with an antibiotic effective for both S.
aureus and streptococcal infections unless cultures reveal only streptococci. Dicloxacillin
and cephalexin are appropriate treatments. A 7-day course of oral antibiotic treatment is
recommended. If only streptococci are detected in extensive impetigo or ecthyma, oral
penicillin is the preferred therapy.
MRSA impetigo can be treated with doxycycline, clindamycin, or trimethoprimsulfamethoxazole (Bactrim). Crusted lesions can be washed gently. Children can return
to school 24 hours after beginning an effective antimicrobial therapy. Draining lesions
should be kept covered.
Quiz: Sally, aged 25, presents with impetigo that has been diagnosed as infected
with staphylococcus. The clinical presentation is pruritic tender, red vesicles
surrounded by erythema with a rash that is ulcerating. She has not been adequately
treated recently. Which type of impetigo is this?
a. Bullous impetigo
b. Staphylococcal scalded skin syndrome (SSSS)
c. Nonbullous impetigo
d. Ecthyma
2. Staphylococcal Scalded Skin Syndrome
Caused by Staphylococcus aureus, it’s a variant of bullous impetigo:Epidermal necrosis
caused by bacterial exotoxins, resulting in the epithelial layer peeling off in large,
sheetlike pieces; mimics scalded-skin thermal burn. This serious infection is more
commonly seen in children and usually begins in the intertriginous areas.
3. Cellulitis
Cellulitis is an acute infection as a result of bacterial entry via breaches in the skin
barrier. As the bacteria enter the subcutaneous tissues, their toxins are released which
causes an inflammatory response.
Cellulitis and erysipelas is almost always a unilateral infection with the most
common site of infection being the lower extremities.
Cellulitis involves the deeper dermis and subcutaneous fat.
Cellulitis is observed most frequently among middle-aged individuals and older
adults.
The vast majority of pathogens associated with cellulitis are from either
Streptococcus or Staphlococcus bacteria. The most common are beta-hemolytic
streptococci (groups A, B, C, G, and F), and S. aureus (gram +)
Both erysipelas and cellulitis manifest with areas of skin erythema, edema,
warmth and pain. Fever may be present. Additional manifestations of cellulitis
and erysipelas include lymphangitis and inflammation of regional lymph nodes.
Edema surrounding the hair follicles may lead to dimpling in the skin, creating an
appearance reminiscent of an orange peel texture called "peau d'orange".
Cellulitis may present with or without purulence
patients with cellulitis tend to have a more indolent course with development of
localized symptoms over a few days.
Many patients with cellulitis have underlying such as tinea pedis, lymphedema,
and chronic venous insufficiency. In such patients, treatment should be directed
at both the infection and the predisposing condition if modifiable.
Patients with cellulitis or erysipelas in the absence of abscess or purulent
drainage should be managed with empiric antibiotic therapy. Patients with
drainable abscess should undergo incision and drainage.
I. Describe an appropriate empiric antibiotic treatment plan for cellulitis
should be managed with empiric therapy for infection due to beta-hemolytic
streptococci and methicillin-susceptible Staphylococcus aureus (MSSA) with:
• Cephalexin 500 mg four times daily (alternative for mild penicillin allergy)
• Clindamycin 300 mg to 450 mg four times daily (alternative for severe penicillin
allergy)
Good choices for uncomplicated cases of cellulitis that are not associated with
human or animal bites include dicloxacillin or cephalexin for 10 to 14 days.
If pt has severe PCN allergy rx erythromycin
If caused by animal or human bite: amoxicillin-clavulanic acid (augmentin) for 2
weeks
The coverage for MRSA is achieved by adding to amoxicillin one of the following:
Bactrim DS twice daily
Doxycycline 100 mg twice daily
Minocycline 200 mg orally once, then 100 mg orally every 12 hours
If clindamycin is used, no additional MRSA coverage is needed.
Risk factors for community-associated methicillin-resistant S. aureus (CA-MRSA) include the
following.
• Antibiotic use secondary to antibiotic selective pressure. Use of cephalosporins and
fluoroquinolones strongly correlates with the risk for MRSA colonization and infection.
• HIV infection
• Hemodialysis
• Long-term care facilities
Patients with drainable abscess should undergo incision and drainage. For patients undergoing
incision and drainage of a skin abscess, some experts suggest antibiotic treatment under some
conditions.
• Single abscess ≥2 cm
• Multiple lesions
• Extensive surrounding cellulitis
• Associated immunosuppression or other comorbidities
• Systemic signs of toxicity (fever >100.5° F/38° C)
• Presence of an indwelling medical device (such as prosthetic joint, vascular graft, or
pacemaker)
• High risk for transmission of aureus to others (such as in athletes or military personnel)
Quiz: Ian, age 62, presents with a wide, diffuse area of erythematous skin on his left lower leg
that is warm and tender to palpation. There is some edema involved. You suspect:
a. Necrotizing fasciitis. c. Cellulitis.
b. Kaposi's sarcoma. d. A diabetic ulcer.
4. Erysipelas
Cellulitis and erysipelas are two of the most common skin and soft tissue infections.
Erysipelas involves the upper dermis, and there is clear demarcation between
involved and uninvolved tissue.
An older name for erysipelas is “St. Anthony’s fire.” Despite the superficial nature
of this infection, erysipelas should not be taken lightly, because it can be fatal if it
is not treated promptly (especially in the very young and the elderly).
Erysipelas is sometimes seen after an episode of strep throat.
The most common sites of involvement are the face (especially the cheeks) and
the lower legs.
Erysipelas occurs in young children and older adults.
Erysipelas results almost always results from a group A strep infection.
erysipelas is non-purulent.
Patients with erysipelas tend to have acute onset of symptoms with systemic
manifestations including fever and chills
Classic descriptions of erysipelas note "butterfly" involvement of the face.
Involvement of the ear (Milian's ear sign) is a distinguishing feature for
erysipelas, since this region does not contain deeper dermis tissue.
Quiz: Which of the following types of cellulitis is a streptococcal infection of the
superficial layers of the skin which does not involve the subcutaneous layers?
a. Necrotizing fasciitis c. Erysipelas
b. Periorbital cellulitis d. "Flesh-eating" cellulitis
5. Necrotizing fasciitis
Considered as a severe case of cellulitis must refer to ER, can be a differential diagnosis
of cellulitis
Defined as deep infection that results in progressive destruction of the muscle fascia.
The affected area may be erythematous, swollen, warm, and exquisitely tender. Pain out
of proportion to exam findings may be observed.
The hallmark of this infection is its rapid progression and the severity of the
symptoms. The progress of the infection is measured in terms of hours instead of
days, and the border can be seen to literally spread in just a few hours.
This infection is caused by “flesh-eating bacteria,” and loss of life or limb is a
potential complication.
Quiz: Mark has necrotizing fasciitis of his left lower extremity. Pressure on the skin reveals
crepitus due to gas production by which anaerobic bacteria?
a. Staphylococcal aureus c. S. pyrogenes
b. Clostridium perfringens d. Streptococcus
6. Mammalian bites
Soft tissue trauma caused by animal and human bites have serious clinical implications
because of the potential for complications.
Bite wounds should be irrigated copiously with sterile saline, and grossly visible debris
should be removed. Prophylactic antibiotics are administered to patients who present for
evaluation of a bite wound who do not yet have signs or symptoms of infection in the
following circumstances.
• Deep puncture wounds (especially due to cat bites)
• Wounds requiring surgical repair
• Moderate to severe wounds with associated crush injury
• Wounds in areas of underlying venous and/or lymphatic compromise
• Wounds on the hand(s) or in close proximity to a bone or joint
• Wounds on the face or in the genital area
• Wounds in immunocompromised hosts
Amoxicillin/clavulanate 875 mg/125 mg twice daily is the agent of choice. Alternative
antibiotics include one of the following agents with activity against Pasteurella.
• Doxycycline 100 mg twice daily
• Bactrim DS twice daily
• Penicillin VK 500 mg four times daily
• Ciprofloxacin 500 mg twice daily
Plus one of the following agents with anaerobic activity.
• Metronidazole 500 mg three times daily
• Clindamycin 450 mg three times daily
First-generation cephalosporins and macrolides should be avoided. The duration of
prophylactic oral antibiotics is 3–5 days, with close follow-up. Tetanus toxoid should be
given to those who have completed a primary immunization series but who received the
most recent booster 5 or more years ago.
[Show More]