*NURSING > STUDY GUIDE > NR Pharmacology, INTRODUCTION TO PHARMACOTHERAPEUTICS (All)
NR Pharmacology, INTRODUCTION TO PHARMACOTHERAPEUTICS
Document Content and Description Below
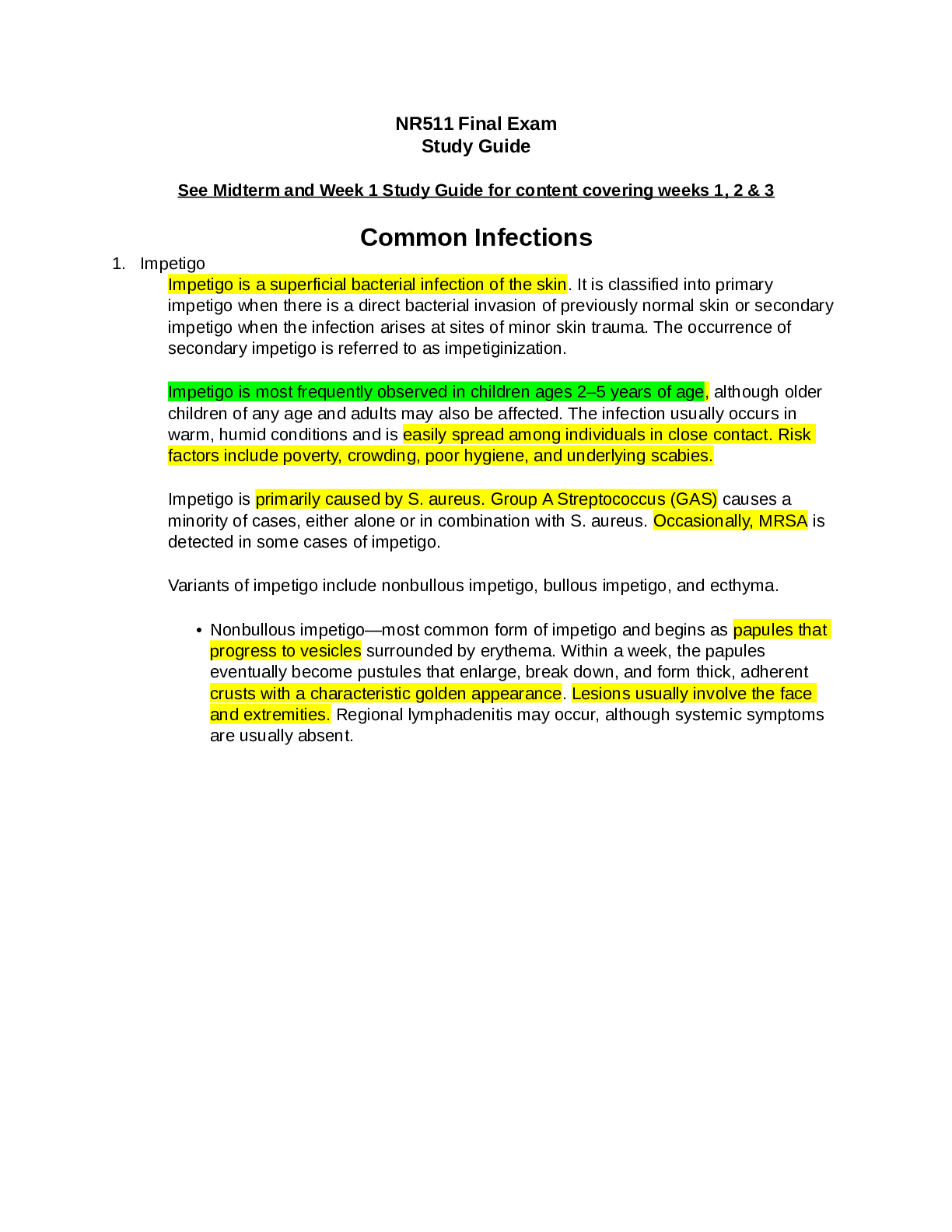
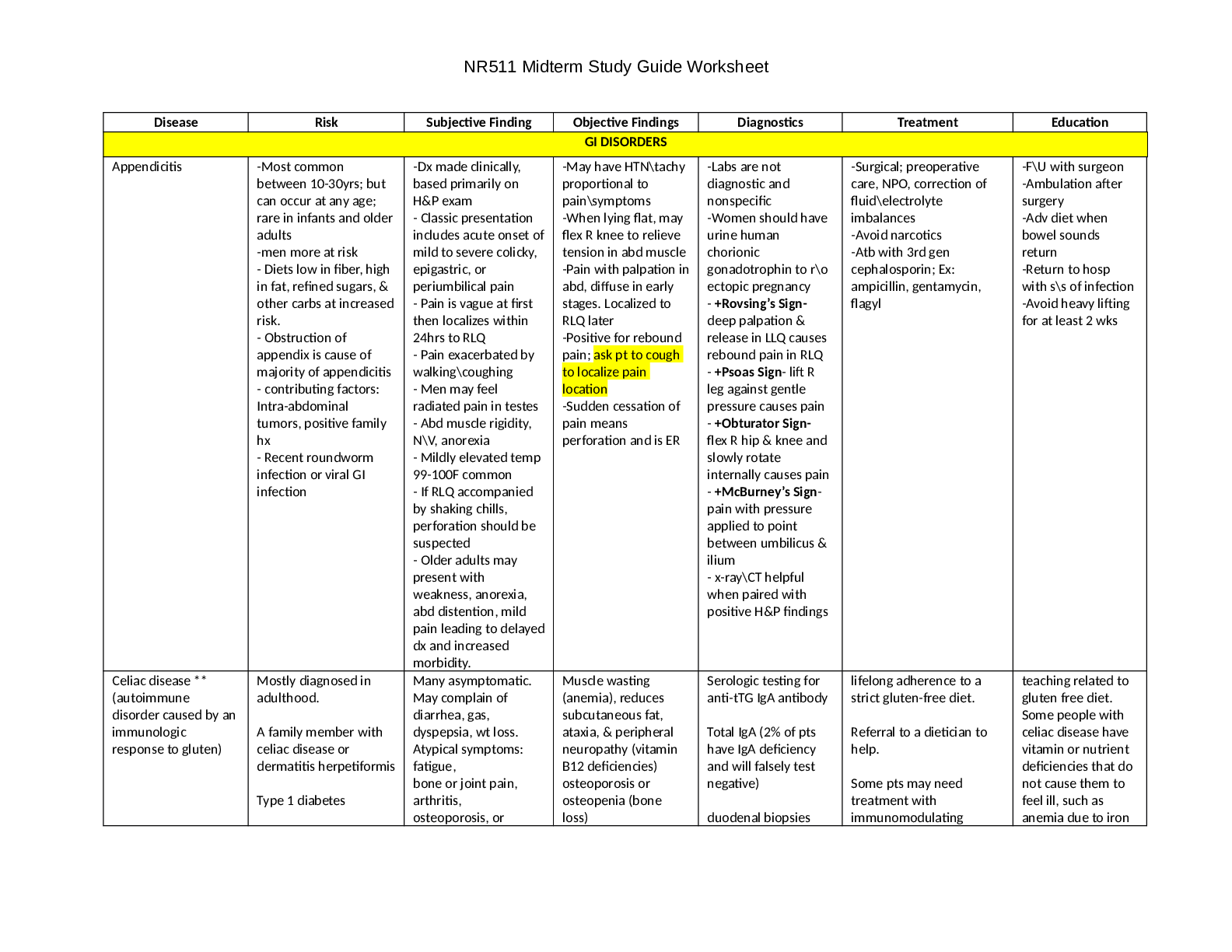
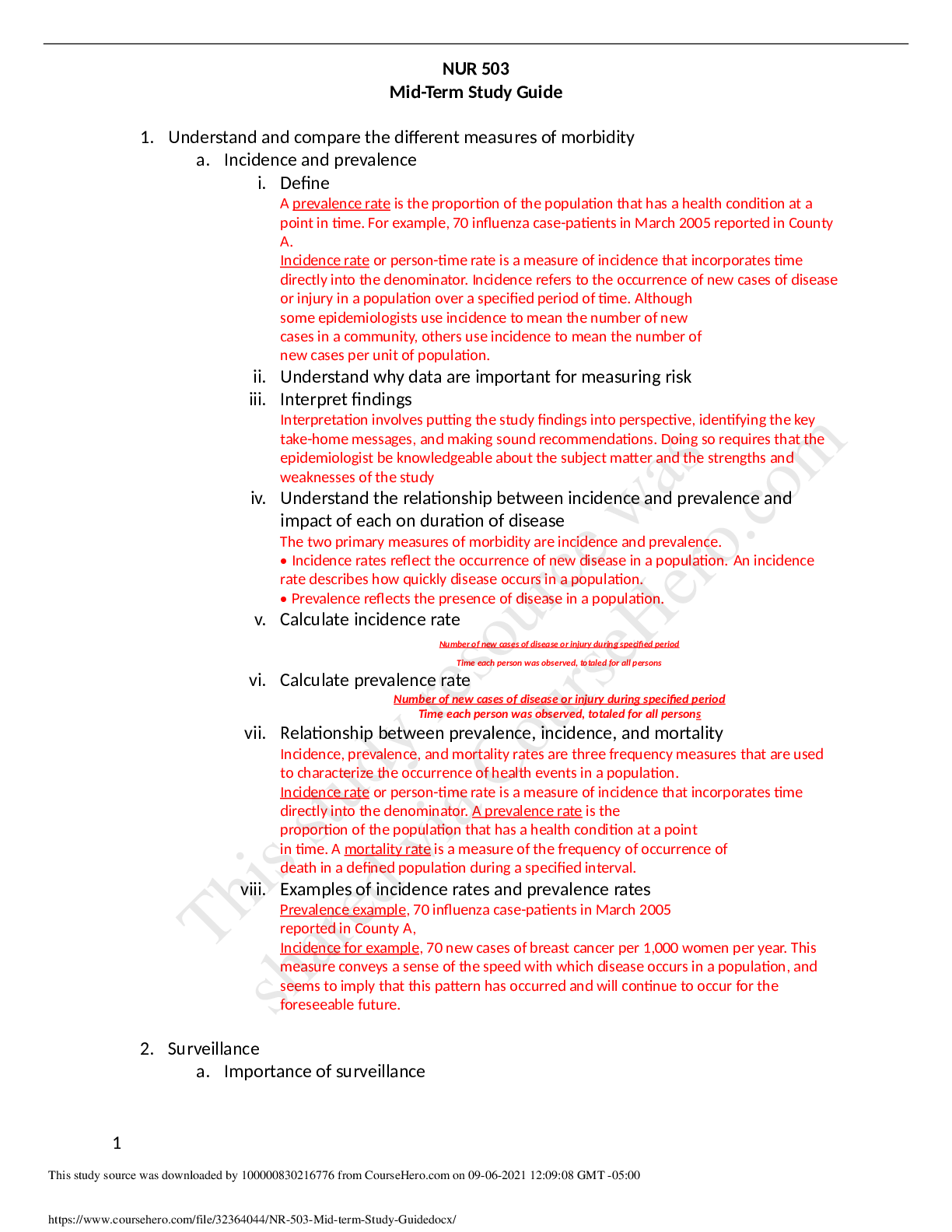
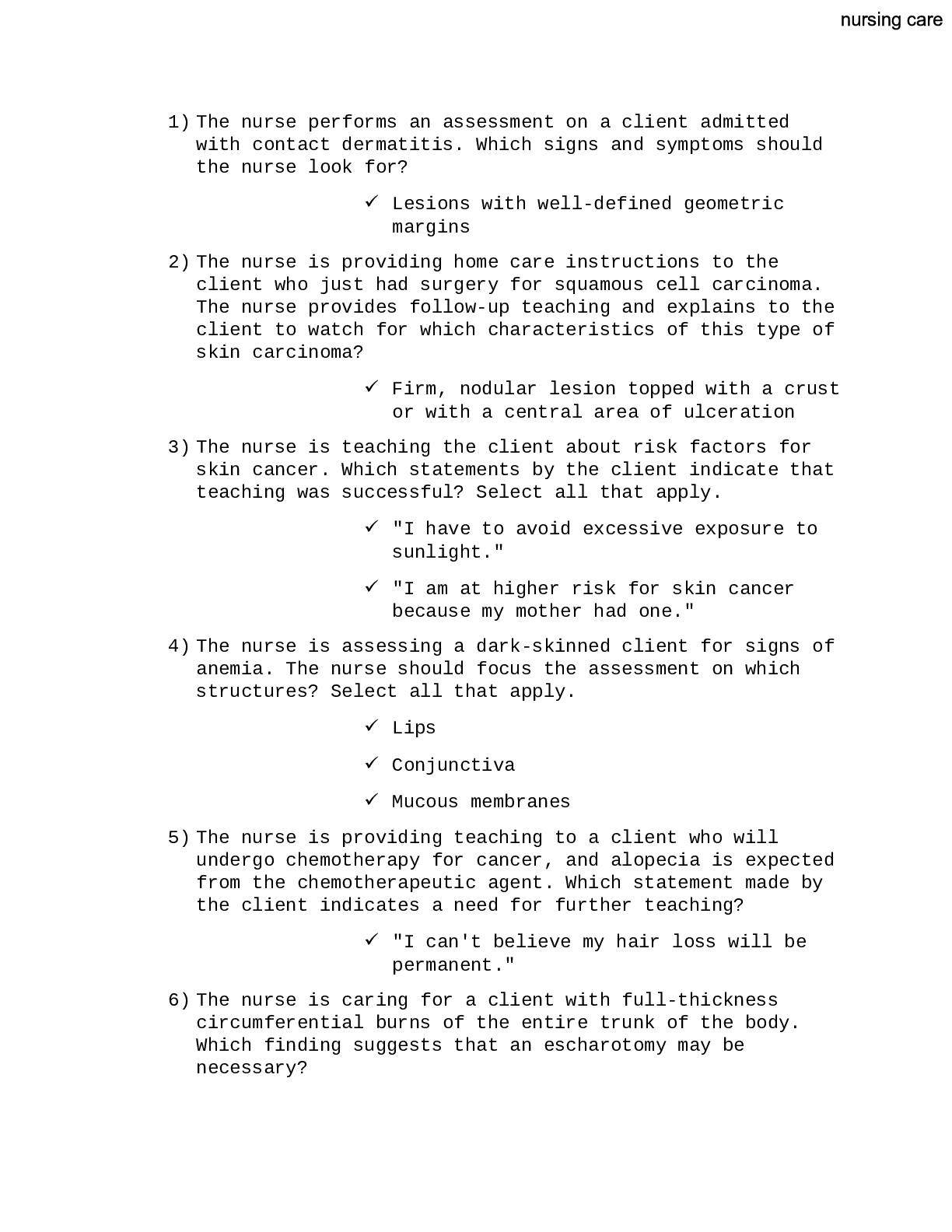
INTRO TO PHARMACOTHERAPEUTICS Prescription Writing Need at least 2 patient identifiers: Name, DOB, Address, Date of Rx, Prescriber name, address, license number, DEA number if applicable, Info for su ... pervising MD, Drug: name/strength/dose/route/QTY/refills, Signature JC “Do Not Use” List • U: write out “unit” • IU: write out “international units” • Q.D., Q.O.D.: write out daily or every other day • Trailing/leading zeros • MS, MSO4, MgSO4: write morphine sulfate or magnesium sulfate • µg: write mcg • H.S.: write half-strength or at bedtime • T.I.W.: write three times weekly or 3 times weekly • S.C. or S.Q.: write Sub-Q or subQ or subcutaneously • D/C: write discharge • c.c.: write mL • AS, AD, AU, OS, OD, OU: write out, e.g., both eyes or left ear ANTIBIOTICS Class Drug MOA Uses/Coverage ADR/DDI Education/Other PCN: 1 st Gen Pen G (IV) Inhibit cell wall synthesis, Bactericidal Pneumococcal pneumonia Benzathine penicillin (IM) Syphilis, strep throat Pen VK (PO) Gram + coverage and Treponema pallidum PCN: 2 nd Gen Nafcillin (IM/IV) Cloxacillin (PO) Antistaphylococcal, MSSA Dicloxacillin (PO) PCN: 3 rd Gen Ampicillin (PO) Extended-spectrum: G(+) PLUS some G(-); Amoxicillin (PO) OM, URI Augmentin (amox + clavulanate) Diarrhea, Good for beta-lactamase: H.Flu, M.Cat PCN: 4 th Gen Zosyn (piperacillin + tazobactam) (IV) Broad spectrum, covers Pseudomonas, many G(-) Cephalosporin: 1 st Gen Cefazolin (IM, IV) Inhibit cell wall synthesis good Gram + coverage, NO MRSA coverage Cross-sensitivity with PCNs Cephalexin (PO) Cephalosporins: 2 nd Gen Cefaclor Not as good G+ but some G(-); OM, Strep Cefuroxime (IM, IV, PO) pharyngitis Cephalosporins: 3 rd Gen Ceftriaxone (IM, IV) better G- but lower G+ coverage, High risk w/ some for ESBL resistance Ceftriaxone good for gonorrhea d/t single dose Cefotaxime (IM, IV) Cefixime (PO) Cephalosporins: 4 th Gen Cefepime (IM/IV) Good G+ and G- coverage, Covers Pseudomonas Cephalosporins: 5 th Gen Ceftaroline (IV) G- as 3rd-gen plus MRSA coverage Carbapenems Doripenem Inhibit cell wall synthesis Broader than other BL-abx All IV, IM, saved for very broad coverage May have cross-sensitivity to PCNs Ertapenem Ertapenem: not good Pseudomonas coverage Imipenem & cilastatin Meropenem Monobactam Aztreonam: IM, IV, inhale Inhibit cell wall G- ONLY, Covers Pseudomonas Never use for empiric tx, synthesis Good for PCN-allergic Vancomycin IV Inhibit cell wall synthesis Mainly for G+ and MRSA IV ADR: dose-related ototoxicity & nephrotoxicity; Red man (infusion NOT allergy) Dose for renal fxn, monitor serum levels Vancomycin PO For C. diff. colitis Telavancin Inhibit cell wall synthesis Alternative to vancomycin Covers G+ and MRSA ADR: Teratogenic and QT prolongation No drug monitoring Macrolides Erythromycin Inhibit protein synthesis, bind to 50s ribosomal subunit G+, G-, and atypicals, Often used to treat G+ in pen-allergic patients; Enzyme inhibitor: E > C >> A Must watch with: CBZ, warfarin, statins, etc. Allergic reactions are rare! Clarithromycin ADR: n/v, metallic taste Improved H.Flu vs. E-mycin Azithromycin Long 1/2 life, good for Chlamydia, other atypicals Tetracyclines Doxycycline Inhibit protein synthesis, bind to 30s ribosomal subunit Coverage very broad: G+, G-,aerobic and anaerobic, spirochetes, mycoplasmas, rickettsiae, chlamydiae, some protozoa, MRSA PO High levels of resistance CI: Avoid with chelating agents (MVI, antacid, milk, iron), Avoid in pregnancy and small children (<8) – Binds Ca and will stain teeth ADR: n/v, liver disease, phototoxicity Minocycline Tigecycline IV Derivative of minocycline MRSA, MDRSp, VRE, ESBL-producing G-, many anaerobes, NOT for Pseudomonas; for Complicated SSTIs, intraabdominal ifxn, CAP Aminoglycoside Amikacin Inhibit protein synthesis, bind to 30s ribosomal subunit G- including Pseudomonas Monitor renal function and serum drug levels! ADR: ototoxicity, nephrotoxicity Gentamicin Tobramycin Clindamycin Inhibit protein synthesis, bind to 50s ribosomal subunit Mainly for anaerobic coverage PO or IV and in some topicals, MRSA PO ADR: rashes and high rate of C.diff. Linezolid (Zyvox) Inhibit protein synthesis, bind to 50s ribosomal subunit PO & IV Use for resistant organisms: MRSA, VRSA, VRE, penicillin-resistant Strep. pneumo Caution for Serotonin Syndrome Might offer benefit when transitioning to outpatient Fluoroquinolones Ciprofloxacin Inhibit nucleic acid synthesis – inhibit topoisomerase UTI, GI, Pseudomonas broad G-, respiratory FQs with improved G+ coverage ADR: C.diff colitis!! CNS: seizure, dizziness; Cardiac: QT prolong; MS: tendon, cartilage; Endo: glycemic control; Skin: photosensitivity, rash DDI: antacids, Fe, Ca, Zn Levofloxacin UTI, GI, LRI, URI, skin Moxifloxacin LRI, URI, GI, skin (no UTI!!) Others PO, otic, ophthalmic Folate Antagonist TMP-SMX (Bactrim, Septra) Broad with G+ and G-, NO Pseudomonas Common for UTI, MRSA PO ADRs: rash (simple to SJS), photosensitivity, crystalluria (need to counsel) Dose based on TMP (more important in PO liquid) Miscellaneous Metronidazole Covers protozoa, anaerobes **DOC: C.diff. colitis Trichomoniasis; Various infections of: skin, bone, CNS, GYN, GI, LRI, endocarditis ADR: Avoid with EtOH. Metallic taste Nitrofurantoin unclear, thought to inhibit several enzyme pathways and possibly Use in simple UTI treatment and prophylaxis NOT pyelonephritis or complicated cystitis CI: ClCr <60 mL/min; Do not use in renal impairment Warnings/Caution: Hepatic disease, Elderly HARM FALL 2013 BLOCK I: DERM & EENT INTRODUCTION TO DERMATOLOGIC PRODUCTS Determinant of Pharmacologic Response 1. Permeability and penetration – hydrated > dehydrated, thin > thick, trauma > no trauma 2. Concentration gradient – greater concentration greater amount per unit time (threshold may exist) 3. Dosing – time left on skin, frequency, quantity; dermis acts as barrier and can effect duration 4. Vehicle – cream, ointment, liquid, solution 5. Occlusion – maximizes efficacy, increases absorption, protection Drug Delivery Systems Emulsions – drug particle contained w/in vehicle/base; Indication for different types of products (dry/wet, sensitivity/pain, size, location, acute/chronic) Creams – most common vehicle, no occlusion Ointments – common, good for dry lesions due to occlusive properties; NOT for intertriginous areas; can be cosmetically unpleasing Gels – clear, non-greasy, non-staining, non-occlusive, quick drying; can sting on application and be drying (due to EtOH) Solutions – evaporate quickly (drying), used in acute/weeping/oozing wounds o Tinctures – alcohol-based solution, used for extreme drying properties Aerosols – advantage for painful skin, but expensive and not efficient dosage form Lotions – good for tender areas, spreads easily, evaporates quickly, good for large areas Powders – used to absorb moisture/friction; caution w/ very wet lesions due to crusting Choosing Which Drug Delivery System to Use DRY wet lesions and WET dry lesions **more liquid agents dry better Acute inflammation (oozing/weeping/vesication/edema/pruritis) aqueous vehicles, powders, lotions, sprays, aerosols Subacute inflammation (crusting/oozing/pruritis) creams, gels Chronic inflammation (lichenification/dryness/erythema/pruritis/scaling) ointments ANDROGENIC ALOPECIA Tx goal: reduce loss and maintain existing hair **If you stop therapy, hair loss WILL return! Drug MOA Indication ADRs/DDI/CI Specific Education/Other Minoxidil Changes follicle size & growth cycle of hair to f hair & thicker/longer shaft Topical formulation only to limit and contain ADR (BP); OTC, 1st line M & F ADR: local irritation, undesirable growth if inappropriately use **well- tolerated Wash hands after application, treatment must be continuous Finasteride Type II 5-alpha-reductase inhibitor, PO (tablet) formation that only grows *CI: pregnancy Caution in women of child-bearing 4inhibits conversion of testosterone to dihydrotestosterone (reverse loss) hair at vertex/frontal scalp; first line for men, second line for women ADR: libido, erectile dysfunction, ejaculation disorder, ejaculation vol age, wash hands/gloves, treatment must be continuous SYSTEMIC ANTIFUNGALS Class Drug MOA Indication ADRs/DDI/CI Specific Education/Other Amphotericin B (“Amphoterrible”) binds to ergosterol and alters permeability; large spectrum of activity IV; only used in infectious disease with high resistance *lipid formations are less toxic, but still not good ADRs: EXTREMELY TOXIC (nephrotoxicity, infusion- related toxicity) Azoles Fluconazole (Diflucan) inhibit synthesis of ergosterol by blocking demethylation of lanosterol IV and PO; Important treatment for infections due to Candida; drug of choice for vaginal yeast infections Itraconazole IV and PO *bioavailability varies, PO solution achieves higher serum concentrations; Used for fungal nail infections Can cause liver problems – must get liver enzymes checked every 4- 6 weeks Voriconazole IV and PO; Broad spectrum triazole used for serious infections, first line for aspergillosis ADR: visual abnormality Posaconazol e PO suspension Broad-spectrum triazole, but can cause many DDIs *Enhanced w/ high-fat meal, splitting dose in fasting Echinocandins disrupts cell wall structure formation by inhibiting β- glucan synthase IV only; used to treat significant fungal infection – integral component of Aspergillus and Candida cell wall Generally well tolerated (but expensive) *more common/better tolerated/less DDIs than azole Flucytosine disrupts cell wall formation via pyrimidine analog PO only, rarely used as monotherapy due to rapid resistance development Spectrum: Cryptococcus spp, Candida spp; used to treat cryptococcal meningitis in combination w/ AmB Key Points of Systemic Antifungals Always consider hepatic function (liver disease, heavy EtOH use, etc.) Review patient’s medical history to avoid DDIs Systemic –azole agents in primary care are mainly used for skin/nail disorders, vaginal yeast infections (fluconazole) TOPICAL ANTIFUNGALS Class Drug MOA Indication Specific Education/Other Topical Azoles Block biosynthesis of ergosterol Tinea pedis/cruris/corporis, tinea versicolor, cutaneous candidiasis, vaginal candidiasis *Most effective topical antifungal for treatment of dermatophytes Topical Allylamines, Butylamine Naftifine inhibit squalene epoxidase (key enzyme in ergosterol biosynthesis pathway) Tinea pedis/cruris/corporis, tinea versicolor Terbinafine (Lamisil) **Terbinafine = tx for nail fungus Butenafine Topical Polyene Nystatin Bind to ergosterol in fungal cell membrane, changes membrane permeability cutaneous infections caused by Candida albicans, other Candida spp *not useful against dermatophytes *highly toxic systemically Other Selenium exerts a cytostatic effect of cell of epidermis tinea versicolor Lotion, Shampoo formulations OTC (well- Sulfide and follicular epithelium tolerated) Tolnaftate Distorts the hyphae and stunts mycelial growth of fungal species Tinea pedis/cruris/corporis, tinea versicolor (Tinactin) *tough-actin tinactin; Cream, solution, powder, spray, gel forumations OTC Ciclopirox alters integrity of fungal cell membrane skin, superficial nail infections; tinea pedis/cruris/corporis, tinea versicolor *activity against Candida Cream, lotion, nail laquer (Penlac) formulations Systemic Agents for Superficial Infections *Fluconazole Itraconazole Ketoconazole Terbinafine Griseofulvin Indicated for candidiasis *yeast/vaginal infections Single dose is used for treatment Indicated for candidiasis, dermatophytes (tineas), onychomycosis (nail fungus) Multiple DDIs – Inhibited CYP3A4 Indicated for candidiasis, dermatophytes Multiple DDIs, potential hepatotoxicity *only last line in life-threatening infection PO and topical available Indicated for candidiasis, dermatophytes, onychomycosis Potential hepatotoxicity – monitor liver enzymes Inhibits mitosis, rarely used Indicated for dermatophytes and onychomycosis *Pulse Therapy (Terbinafine and Itraconazole): Used in onychomycosis treatment, has some evidence for less toxicity (dosed daily 1 week, off 3 weeks) to decrease ADRs, DDIs DRUG ERUPTIONS Types of Drug Eruptions Mild rash, itching, dry skin severe, potentially life-threatening conditions) SJS, TEN, Angioedema, Vasculitis, Coagulent-induced skin necrosis General Approach to Drug Reactions (1) Recognize that problem may be drug-related Identify agent (2) STOP OFFENDING AGENT (3) Determine severity (i.e. triage situation) (4) Treat sequelae **Don’t forget to EDUCATE PATIENT Reaction Characteristics Common Offenders Acneiform Reactions Differ from true acne: no comedone, uniform appearance of lesions, location, age, recent drug exposure glucocorticoids, oral contraceptives, lithium, anabolic steroid Photosensitivity Reactions Phototoxic reactions – exaggerated sunburn or increased sensitivity to light; UVA causes alteration of drug to toxic form (>common) Photoallergic reactions – manifests in bullae, urticaria, sunburn; UVA alters drug to antigen and leads to allergic response (<common) antibiotics, antidepressants, hypoglycemics, oral contraceptives, antipsychotics, antihypertensives Allergic Contact Dermatitis Topical administration can cause localized allergic response, reaction widespread if given systemic drug after topical sensitization neomycin (Neosporin), benzocaine, diphenhydramine (Benadryl) Erythema Multiforme Lesions of various forms including Target lesions; affect mucous membranes allopurinol, barbiturates, phenothiazine, sulfonamides Stevens-Johnson Syndrome (SJS) Most common severe eruption; can be life-threatening (est. 5-20%) sulfonamides*, FQs, allopurinol, carbamazepine, pregnancy, infection, radiation, cancer, foods Topical Epidermal Necrosis (TEN) Prodrome of milder symptoms (fever, fatigue, arthralgias, sore throat); can be fatal (est. 30%) allopurinol, aminopenicillins, carbamazepine, sulfonamides*, infection, foods Erythema Nodosum Erythematous rash with tender nodules commonly on legs (usually no mucosal involvement) oral contraceptives*, analgesics, sulfonamides Drug Hypersensitivity Reaction Multiple names/varied constellation of symptoms and signs may lead to misdiagnosis; Typically start w/ fever, widespread maculopapular rash on trunk, arms, legs; organ damage may follow, fatal in 10% sulfonamides, PCNs, anticonvulsants, antimalarials Fixed Drug Eruption Erythematous lesions of various types (nodules, bullae) common on genitals, face *always in same spot Caused exclusively by drugs (antibiotics, anti-inflammatories, oral contraceptives) *generally resolve after offending drug d/c Maculopapular Typical rash, #1 drug reaction manifested in skin *classic PCN rash ampicillin, amoxicillin, allopurinol General Concepts Glucocorticoids – receptors widespread throughout body (cortisol) Mineralocorticoids – receptors in kidney, colon, salivary/sweat glands, brain (aldosterone) o Regulates water volume and concentration of electrolytes – acts on kidney tubules, collecting ducts, enhances Na+ reabsorption o Used less frequently than glucocorticoids Class MOA Indications/Management ADR/Patient Education Systemic Glucocorticoids Anti-Inflammatory Promotion of Metabolism (**DM patients sugar will increase) Increased Resistance to Stress Alteration of Blood Cell Levels in Plasma Acute Adrenal Insufficiency Dx: ACTH stimulation test; Tx: IV hydrocortisone + glucose Chronic (Addisons) Adrenal Insufficiency: Tx: PO hydrocortisone daily, prednisone or dexamethasone Some patients normalized by hydrocortisone + salt intake, many require mineralcorticoid replacement Fludrocortisone** mineral action Inflammatory/Autoimmune Disease: Provide sx relief only – do not cure!! High initial dose and taper over days to allow adrenal recovery Tablets (#1), can also be injected to minimize systemic effects Asthma Inhaler administration daily *minimizes systemic effects, ADRs Agents: Triamcinolone, Beclomethasone, Flunisolide, Fluticasone PO for severe exacerbations * chronic bronchitis and emphysema Allergic Disease Relief delayed 12-24h, appropriate for severe/long /systemic reactions PO or IV, nasal spray steroids are first choice treatment for allergic rhinitis Other: Infectious Disease: supplemented, not 1st line Blood Malignancies Traumatic Injury/Organ Transplantation: Spinal cord injury (NOT effective w/ head injury), Organ transplantation Preterm labor Chemotherapy ADRs of Corticosteroids Fluid/electrolyte imbalances Metabolic: hyperglycemia/glucosuria (close management w/ diet, insulin) Immune suppression: Increased susceptibility to infection with chronic use GI acid production: increased risk of peptic ulcer, (esp. in conjunction w/ NSAIDs) Myopathy: muscle wasting, takes high dose Osteoporosis, Osteonecrosis Cataracts Behavioral changes – “steroid psychosis” Growth suppression in children – especially systemic steroids **use of steroids in chronic asthma in children is a common concern Cushing’s Syndrome – chronic use; upper body obesity, rounded/moon face, thin arms/legs Withdrawal from Glucocorticoids: Sudden withdrawal can be life-threatening (acute adrenal insufficiency) **taper off if used > 2weeks!! Topical Corticosteroids Inflammatory skin diseases 1% hydrocortisone ointment +/- occlusive dressing, minimal systemic absorption Systemic administration for widespread/severe exacerbations (prednisone, prednisolone) Many preparations – betamethasone (most potent), triamcinolone, clobetasol Fluorinated steroids should NOT be used on face (dexamethasone, triamcinolone, betamethasone, “flu-sone,lone,rone) * DOC for skin inflammation and pruritus but avoid use in infectious etiologies (except when combined w/ antifungal) Ocular Inflammation Dexamethasone eye drops or ointment **should always be used under Aoid overuse, use lowest potency *educate patient not to exceed recommended dosing Don’t forget systemic effects: children, elderly, liver disease, thin skin, use of occlusion/high potency agents (ointments) ADRs *fewer than systemic Local – with chronic, repeated use Systemic – adrenal suppression can occur with high dose, long-term treatment [Show More]
Last updated: 3 years ago
Preview 1 out of 93 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$15.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Sep 08, 2021
Number of pages
93
Written in
All
Additional information
This document has been written for:
Uploaded
Sep 08, 2021
Downloads
0
Views
125