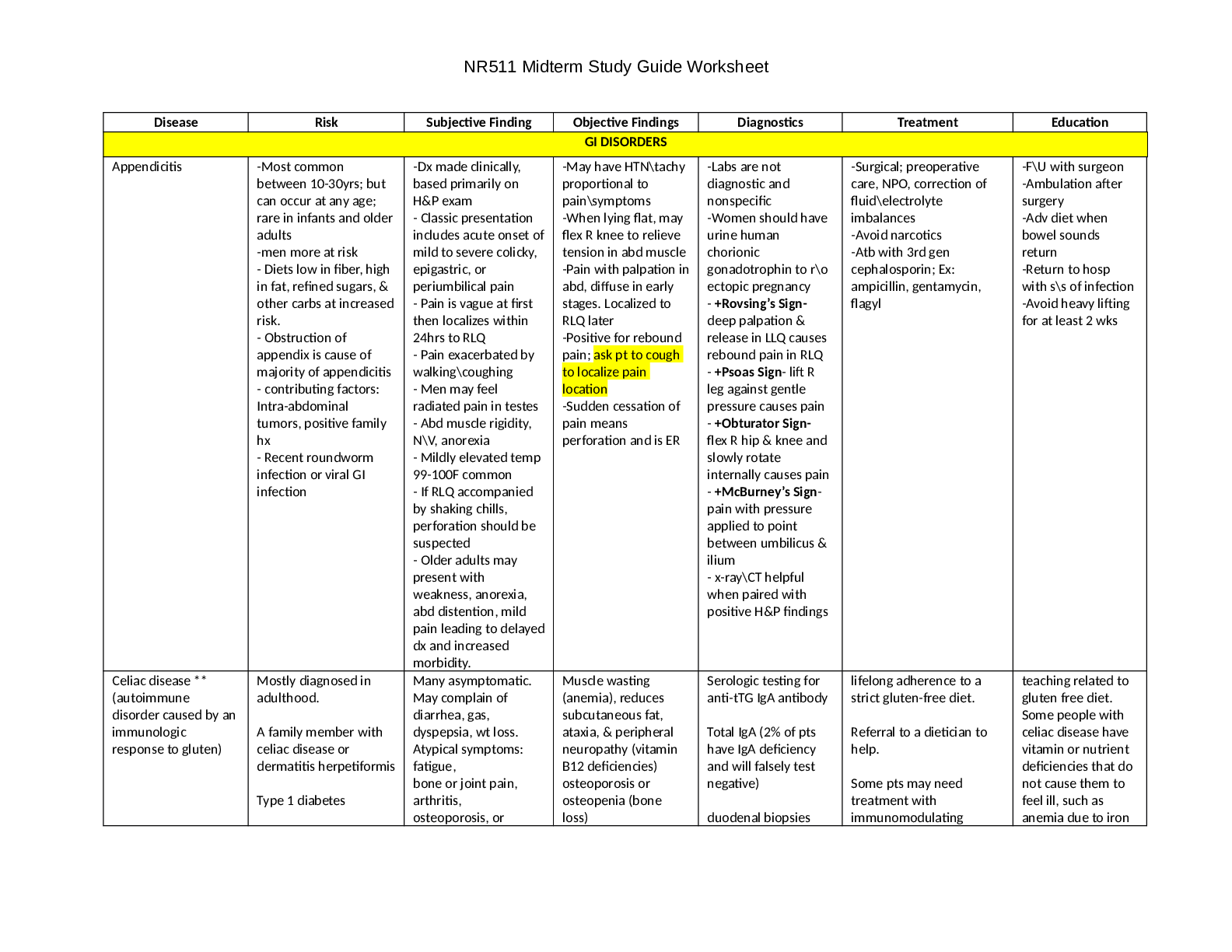
NR511 Midterm Study Guide Worksheet
Disease Risk Subjective Finding Objective Findings Diagnostics Treatment Education
GI DISORDERS
Appendicitis -Most common
between 10-30yrs; but
can occur at any age;
rare in i
...
NR511 Midterm Study Guide Worksheet
Disease Risk Subjective Finding Objective Findings Diagnostics Treatment Education
GI DISORDERS
Appendicitis -Most common
between 10-30yrs; but
can occur at any age;
rare in infants and older
adults
-men more at risk
- Diets low in fiber, high
in fat, refined sugars, &
other carbs at increased
risk.
- Obstruction of
appendix is cause of
majority of appendicitis
- contributing factors:
Intra-abdominal
tumors, positive family
hx
- Recent roundworm
infection or viral GI
infection
-Dx made clinically,
based primarily on
H&P exam
- Classic presentation
includes acute onset of
mild to severe colicky,
epigastric, or
periumbilical pain
- Pain is vague at first
then localizes within
24hrs to RLQ
- Pain exacerbated by
walking\coughing
- Men may feel
radiated pain in testes
- Abd muscle rigidity,
N\V, anorexia
- Mildly elevated temp
99-100F common
- If RLQ accompanied
by shaking chills,
perforation should be
suspected
- Older adults may
present with
weakness, anorexia,
abd distention, mild
pain leading to delayed
dx and increased
morbidity.
-May have HTN\tachy
proportional to
pain\symptoms
-When lying flat, may
flex R knee to relieve
tension in abd muscle
-Pain with palpation in
abd, diffuse in early
stages. Localized to
RLQ later
-Positive for rebound
pain; ask pt to cough
to localize pain
location
-Sudden cessation of
pain means
perforation and is ER
-Labs are not
diagnostic and
nonspecific
-Women should have
urine human
chorionic
gonadotrophin to r\o
ectopic pregnancy
- +Rovsing’s Sign-
deep palpation &
release in LLQ causes
rebound pain in RLQ
- +Psoas Sign- lift R
leg against gentle
pressure causes pain
- +Obturator Sign-
flex R hip & knee and
slowly rotate
internally causes pain
- +McBurney’s Sign-
pain with pressure
applied to point
between umbilicus &
ilium
- x-ray\CT helpful
when paired with
positive H&P findings
-Surgical; preoperative
care, NPO, correction of
fluid\electrolyte
imbalances
-Avoid narcotics
-Atb with 3rd gen
cephalosporin; Ex:
ampicillin, gentamycin,
flagyl
-F\U with surgeon
-Ambulation after
surgery
-Adv diet when
bowel sounds
return
-Return to hosp
with s\s of infection
-Avoid heavy lifting
for at least 2 wks
Celiac disease **
(autoimmune
disorder caused by an
immunologic
response to gluten)
Mostly diagnosed in
adulthood.
A family member with
celiac disease or
dermatitis herpetiformis
Type 1 diabetes
Many asymptomatic.
May complain of
diarrhea, gas,
dyspepsia, wt loss.
Atypical symptoms:
fatigue,
bone or joint pain,
arthritis,
osteoporosis, or
Muscle wasting
(anemia), reduces
subcutaneous fat,
ataxia, & peripheral
neuropathy (vitamin
B12 deficiencies)
osteoporosis or
osteopenia (bone
loss)
Serologic testing for
anti-tTG IgA antibody
Total IgA (2% of pts
have IgA deficiency
and will falsely test
negative)
duodenal biopsies
lifelong adherence to a
strict gluten-free diet.
Referral to a dietician to
help.
Some pts may need
treatment with
immunomodulating
teaching related to
gluten free diet.
Some people with
celiac disease have
vitamin or nutrient
deficiencies that do
not cause them to
feel ill, such as
anemia due to iron
NR511 Midterm Study Guide Worksheet
Down syndrome or
Turner syndrome
Autoimmune thyroid
disease
Microscopic colitis
(lymphocytic or
collagenous colitis)
Addison's disease
osteopenia (bone loss)
liver and biliary tract
disorders
(transaminitis, fatty
liver, primary
sclerosing cholangitis,
depression or anxiety
peripheral neuropathy
seizures or migraines
missed menstrual
periods
infertility or recurrent
miscarriage
canker sores inside the
mouth
dermatitis
herpetiformis (itchy
skin rash)
hypothyroidism
Pts with dermatitis
herpetiformis found
to have signs of celiac
disease on intestinal
biopsy.
Test for nutritional
deficiencies
associated with
malabsorption of C.D.
(hemoglobin, iron,
folate, vit B12,
Calcium, and Vitamin
D.)
agents. deficiency or bone
loss due to vitamin
D deficiency.
However, these
deficiencies can
cause problems
over the long term.
Untreated
celiac/developing
certain types of
gastrointestinal
cancer. This risk can
be reduced by
eating a gluten-free
diet.
Cholelithiasis is the formation of
gallstones and is found
in 90% of patients with
cholecystitis.
--Risk factors--2 types of
stones (cholesterol and
pigmented)
a. Cholesterol (most
common form): female,
obesity, pregnancy,
increased age, drug-
induced (oral
contraceptives and
clofibrates: cholesterol
lowering agent), cystic
fibrosis, rapid weight
loss, spinal cord injury,
Ileal disease with
extensive resection,
Diabetes mellitus, sickle
cell anemia.
b. Pigmented: hemolytic
diseases, increasing age,
hyperalimentation
Patient complaint of
indigestion, nausea,
vomiting (after
consuming meal high
in fat), and pain in RUG
or epigastrium that
may radiate to the
middle of the back,
infrascapular area or
right shoulder.
Right side involuntary
guarding of
abdominal muscles,
Positive Murphy's
sign, possible palpable
gallbladder, Low grade
fever between 99-101
degrees. Possible
jaundice from
common bile duct
edema and
diminished bowel
sounds.
Mild elevation of
WBC up to 15, 000
Abdominal Xray:
Quick, noninvasive,
reliable, and cost-
effective means of
identifying the
presence of
cholelithiasis.
a. Initial management--
begins with definitive
diagnosis. When
asymptomatic (normally
an incidental finding while
exploring another
problem) require no
further treatment except
teaching s/sx of
"gallbladder attack".
Nonsurgical candidate can
be treated with dissolution
therapy or lithotripsy.
Acute includes hydration
(IV fluids), antibiotics,
analgesics, GI rest.
b. Treatment of choice for
Acute cholecystitis is early
surgical intervention after
stabilization. Poor surgical
risk may benefit from
cholecystectomy
operatively or
percutaneously.
Nonsurgical
intervention: weight
loss, avoidance of
fatty foods to
decrease attacks,
alternative birth
control for persons
taking oral
contraceptives,
menopausal women
taking estrogen
informed about
alternative sources
of phytoestrogens
NR511 Midterm Study Guide Worksheet
(artificial supply of
nutrients, typically IV),
cirrhosis, biliary stasis,
chronic biliary
infections.
Crohn’s ** Ages 15-25 of onset and
then again at 50-80.
Familial tendency,
smoker
Carcinoma less common
in patients with CD due
to treatment sometimes
colectomy
Mild-Four or fewer
loose bowel
movements per day,
can have small
amounts of blood and
mucus in the stool,
and cramping in the
rectum. Moderate-4-6
loose bowel
movements per day
containing more blood
and mucus and other
sx such as tachycardia,
weight loss, fever, mild
edema. Severe-
frequent bloody bowel
movements (6-10),
abd pain and
tenderness, sx of
anemia, hypovolemia,
impaired nutrition.
Most common sx are
abd
cramping/tenderness,
fever, anorexia, wt
loss, spasm, flatulence,
RLQ pain or mass
Tenderness in LLQ or
across entire abd with
guarding and abd
distension. DRE
performed to look for
anal and perianal
inflammation, rectal
tenderness, and blood
in stool. S/Sx of
peritonitis and ileus
may be found
depending on severity
of crohns. Tender
mass in RLQ, anal
fissure, perianal
fissure, edematous
pale skin tags. Extra
intestinal finding may
be episcleritis,
erythema nodosum,
nondeforming
peripheral arthritis,
and axial arthropathy
Stool analysis to r/o
bacterial, fungal, or
parasitic infection for
cause of diarrhea.
CBC to check for
anemia, eval for
hypocalcemia, vit D
deficiency.,
hypoalbuminemia,
and steatorrhea. LFT
to screen for primary
sclerosis cholangitis,
and other liver
problems assoc with
IBD. Check fluid and
electrolytes. May
have elevated WBC
count and sed rate
and prolonged
prothrombin time.
Barium upper GI
series, colonoscopy,
and CT to determine
bowel wall thickening
or abscess formation
Glucocorticoids, there is
no cure for CD and
treatment is aimed at
suppressing inflammation
and symptomatic relief of
complications. Initially
oral prednisone 40-60
mg/d, tapered over 2-4
months, then can have
daily maintenance dose of
5-10mg/d. Sulfasalazine
for mild to moderate CD
500 mg BID, increased to
3-4 g/d. Clinical
improvement in 3-4 wks,
and then tapered to 2-3
g/d for 3-6 months, this
medication interferes with
folid acid absorption and
patient must take
supplements.
Metronidazole effective in
tx perianal disease and in
controlling crohns colitis,
other ABT’s such as Cipro,
Ampicillin, and
Tetracycline effective in
controlling CD ileitis, and
ileocolitis.
Immunosuppressive meds
when unresponsive to
other treatments.
Pt educated on
disease process,
diet and lifestyle
changes. Stress
reduction, adequate
rest to decrease
bowel motility and
promote healing.
Low residue diet
when obstructive sx
present such as
canned fruits,
vegetables and
white bread
Diverticulitis ** -Uncommon under
40yrs; risk rises after
-Rare in pediatric; equal
in men\women
-More common in
-25% develop
symptoms
-LLQ abd pain, worsens
after eating
-Pain sometimes
-LLQ abd tenderness
with possible Firm,
fixed mass may be
identified in area of
diverticula
-Abd x-ray can reveal
free air, ileus,
obstruction
-Barium studies show
sinus tracts, fistulas,
-Asymptomatic cases
managed with high fiber
diet or fiber supplement
with psyllium
-Mild symptoms managed
-Increase fiber in
diet to avoid
constipation and
straining
-H2O intake of at
NR511 Midterm Study Guide Worksheet
developed countries
-High in low fiber, high
fat\red meat diets
-Obesity, chronic
constipation, h\o
diverticulitis, & number
of diverticula which
occur in sigmoid colon.
relieved with BM or
flatus
-BM may alternate
between diarrhea\
constipation
-May present with
bleeding w\o pain or
discomfort
-Fever, chills, tachy;
LLQ with anorexia, N\V
-Fistula may form
causing dysuria,
pneumaturia, fecaluria
-May have rebound
tenderness with
guarding\rigidity
-Tender rectal exam;
stool usually + for
occult blood
obstruction
-Colonoscopy to r\o
Ca, but less sensitive
than barium for
diverticula
-CT with contrast
outpatient with clear
liquid diet and rest
-Atb should not be
routinely used but can be
with diverticula abscess
culture
-Amoxicillin\clavulanate K
(or) flagyl with bactrim
-Symptoms usually subside
quickly and diet can be
advanced slowly
-Pain managed with
antispasmotics Ex; Levsin,
Bentyl, BuSpar
-Avoid morphine
-NG for ileus or intractable
N\V
-Pt can be D\C’d from hosp
once able to maintain
adequate nutrition\
hydration if acute phase
resolved
-Colon resection may be
necessary if no
improvement or
deterioration after 72hrs
of treatment
least 8\8oz glasses
to promote bowel
regularity
-Bulk-forming
laxative may be
needed Ex: psyllium,
FiberCon,
Metamucil
GERD ** -Can occur at any age
-Risk increases with age,
then decreases after
69yrs
-Prevalence equal
across gender, ethnic,
cultural
-Obesity, alcohol,
caffeinated beverages,
chocolate, fruit, decaf
coffee, fatty foods,
onions, peppermint\
spearmint, tomato
products
Anticholinergics, beta-
-Heartburn; mild to
severe
-Regurgitation, water
brash, dysphagia, sour
taste in AM, belching,
coughing,
odynophagia (painful
swallow), hoarseness
or wheezing at night
-Substernal\
retrosternal pain
-Worsens if reclined
after eating, eating
large meals,
constrictive clothing
-H&P usually normal
-May be + for occult
blood in stool
-Usually Hx alone
diagnoses
-May manifest with
atypical symptoms
such as adult-onset
asthma, chronic
cough, chronic
laryngitis, sore throat,
noncardiac chest pain
-If pt fails to respond
to 4-8wks PPI, EGD is
ordered
-EGD warranted over
empiric treatment
when heartburn &
-8wk trial of PPI; weight
loss, avoiding triggers
-If unresponsive to once
daily dosing; can increase
to twice daily; if no relief
EGD needed
-PPI and H2-RA should not
be taken together
-Pt’s on long term therapy
should be re-eval’d q6mos
-Weight loss, med
compliance and
avoidance of
triggers
-Small frequent
meals; main meal
mid-day, avoid
eating 4hrs before
bed, avoid straining,
sleep with HOB
elevated, smoking
cessation, stress
mgmt
NR511 Midterm Study Guide Worksheet
adrenergics, CaChannel
blockers, diazepam,
Estrogen\ progesterone,
Nicotine, Theophylline
-May present with
dysphagia; dysphagia
should only occur with
first bite
dysphagia, bleeding,
anemia, weight loss,
or recurrent vomiting
-EGD with Barrett’s
esophagus q3-5yrs
Giardia Can harbor in intestine,
protozoan attaches to
mucosa of small bowel.
In US, risk in adults is
oral-anal intercourse,
children in daycare.
In third world countries,
risk of contamination
through water sources.
Bloating, flatulence,
nausea, watery
diarrhea, weight loss,
anorexia,
Malabsorption Stool testing positive
for trophozoites 50%
of the time. Duodenal
aspirate or small
bowel biopsy
Quinacrine Hydrochloride
(Atabrine) 100 mg TID
after meals for 5-7 days or
Metronidazole (Flagyl) 250
mg TID for 5-7 days
Teach good hand
washing technique,
sanitize surfaces,
and avoid swimming
in all types of water
sources to avoid
further
contamination.
H. Pylori Infection Risks: Increased age,
living in crowded
conditions, no clean
water source
(nonfiltered water),
smoking
Ache or burning pain
in abdomen.
Abdominal pain that is
worse when stomach
is empty.
Nausea/loss of
appetite/unintentional
weight loss.
Frequent
burping/bloating
Objective Findings
RUQ/LUQ tenderness
-Fecal antigen assay
-Urea breath Test
-Biopsy with
histological
examination
-Serological antibody
Standard triple drug
therapy is clarithromycin
and either amoxicillin or
metronidazole with a PPI
BID for 14 days.
Amoxicillin preferred over
metronidazole b/c there
are some resistant strands
of metronidazole.
-Complications
(PUD)
-Medication side
effects
Irritable bowel
syndrome **
Women more than
men, rate 3:1; starts in
late adolescence and
early adulthood; rare in
pts >50
-2 kinds of patients-
those with abdominal
pain and altered bowel
habits, and those with
painless diarrhea.
-Left lower quadrant
pain, sharp and
burning with cramping
or a diffuse, dull ache,
precipitated by eating,
The physical exam
tenderness in LLQ and
over the umbilicus or
epigastric area in
those with small
bowel involvement.
Digital rectal exam
may reveal
tenderness and may
exacerbate
CBC, ESR, CMP
(electrolytes, serum
amylase), urinalysis,
stools for occult
blood, ova and
parasites, and
cultures.
Labs mostly normal
and any diagnostic
clue as to the cause is
Producing IBS include
caffeine, legumes (and
other fermentable
carbohydrates), and
artificial sweeteners.
alleviate symptoms by
eating a lower-fat diet that
contains more protein.
High fiber diet is good,
introduced slowly to avoid
Recognize triggers
and avoid them.
Patients must
understand that the
goal of treatment is
to improve their
symptoms, not cure
the disease, and
that improvement
NR511 Midterm Study Guide Worksheet
stress and relieved
with a bm or flatus.
-The pain does not
interfere with sleeping,
frequent complaints of
abdominal distention,
gas, and belching,
urgency to defecate,
passage of large
volumes of mucus
within the stool.
-frequently associated
with psych dg, which
presents in the form of
anxiety, depression,
and somatoform
disorders (marital
discord, death, or
abuse)
symptoms.
-No weight loss or
deterioration in
health.
-Key to diagnosis is
the lack of fever,
leukocytosis, or
bloody stools. pg579
advanced assessment
helpful. If WBC found
in the stool =
infectious or
inflammatory process
and not IBS.
Rule out food
intolerance, lactase
deficiency (hydrogen
breath test or lactose
tolerance test). IBS is
often confused with
lactose intolerance
and can be evaluated
by removing lactose
from the diet for 2
weeks and monitoring
the symptoms.
the sensation of bloating,
8 glasses of water per day,
probiotic VSL#3 one
packet bid, Antidiarrheal
medications only
temporary.
-If diarrhea is severe,
episodic use of loperamide
(Imodium) 2 mg or
diphenoxylate (Lomotil)
2.5–5.0 mg every 6 hours
can be used as needed.
-Constipation- lactulose or
magnesium hydroxide.
-Postprandial pain-
dicyclomine 10 to 20 mg 3-
4x a day by mouth or
hyoscyamine 0.125 to 0.75
mg twice a day.
Anticholinergics avoid in
glaucoma and bph.
Tricyclic antidepressants
and ssri in some pt
a time-consuming
process. Dietary
education- fiber
intake increase
Peptic ulcer disease
** (includes gastric
ulcers and duodenal
ulcers)
3 major causes: (1)
Infection w/ H.Pylori, (2)
chronic ingestion of ASA
and other NSAIDs, (3)
acid hypersecretion
such as in Zollinger-
Ellison syndrome.
Genetics, blood type,
personality type, and
cigarette smoking may
also play a role in the
development of PUD.
Pts w/ COPD, cirrhosis,
renal failure, and renal
transplant have higher
incidence.
Hallmark: c/o burning
or gnawing (hunger)
sensation or pain
(dyspepsia) in
epigastrium, often
relieved by food or
antacids. Pts describe
pain episodic pattern
of c/o in which the
pain tends to cluster
and last for minutes,
w/ episodes separated
by periods of no sx.
Almost half w/ NSAID-
induced ulcers are
asymptomatic.
Nocturnal pain: in 2/3
of pts w/ duodenal
Pts w/ duodenal
ulcers often
demonstrate
epigastric tenderness
2.5cm to right of
midline, but this may
also be present in
cholecystitis,
pancreatitis, non-
ulcer dyspepsia, and
other GI disorders.
Reports of melena or
coffee-ground-like
emesis usually
indicate bleeding
ulcer, and perforated
ulcer may present w/
abdominal rigidity.
Routine lab tests:
normal unless
significant bleeding or
vomiting. Pt actively
bleeding à CBC w/
diff. to eval HGB levels
is paramount. Most
pts w/ upper GI
bleeding should have
restrictive strategy,
defined as transfusing
when HGB levels fall
below 7 g/dL.
Diagnostic standard à
upper GI endoscopy.
Serology test or direct
bacteriological
analysis via an
esophagogastroduode
Aim to relieve pain, heal
ulcer, & prevent
complication and
recurrences.
-PPIs: drugs of choice &
includes omeprazole,
raveprazole, lansoprazole,
esomeprazole,
dexlansoprazole,
pantoprazole. PPIs heal
duodenal ulcers in 4 wks
therapy and gastric ulcers
after 8 wks.
-H2-R
eceptor Antagonists: Used
for mild symptoms with no
complication or serious
Smoking cessation;
avoid foods that
precipitate
dyspepsia.
MUST follow
treatment regimen.
Educate about side
effects such as
change in stool
color to black with
bismuth
preparations. If
sucralfate with
antacid, PPI, H2RA
being taken, stress
that sucralfate
cannot be taken
with other meds o
[Show More]

.png)