NR 601 Week 8 Final Exam Review (Latest 2021)
Document Content and Description Below
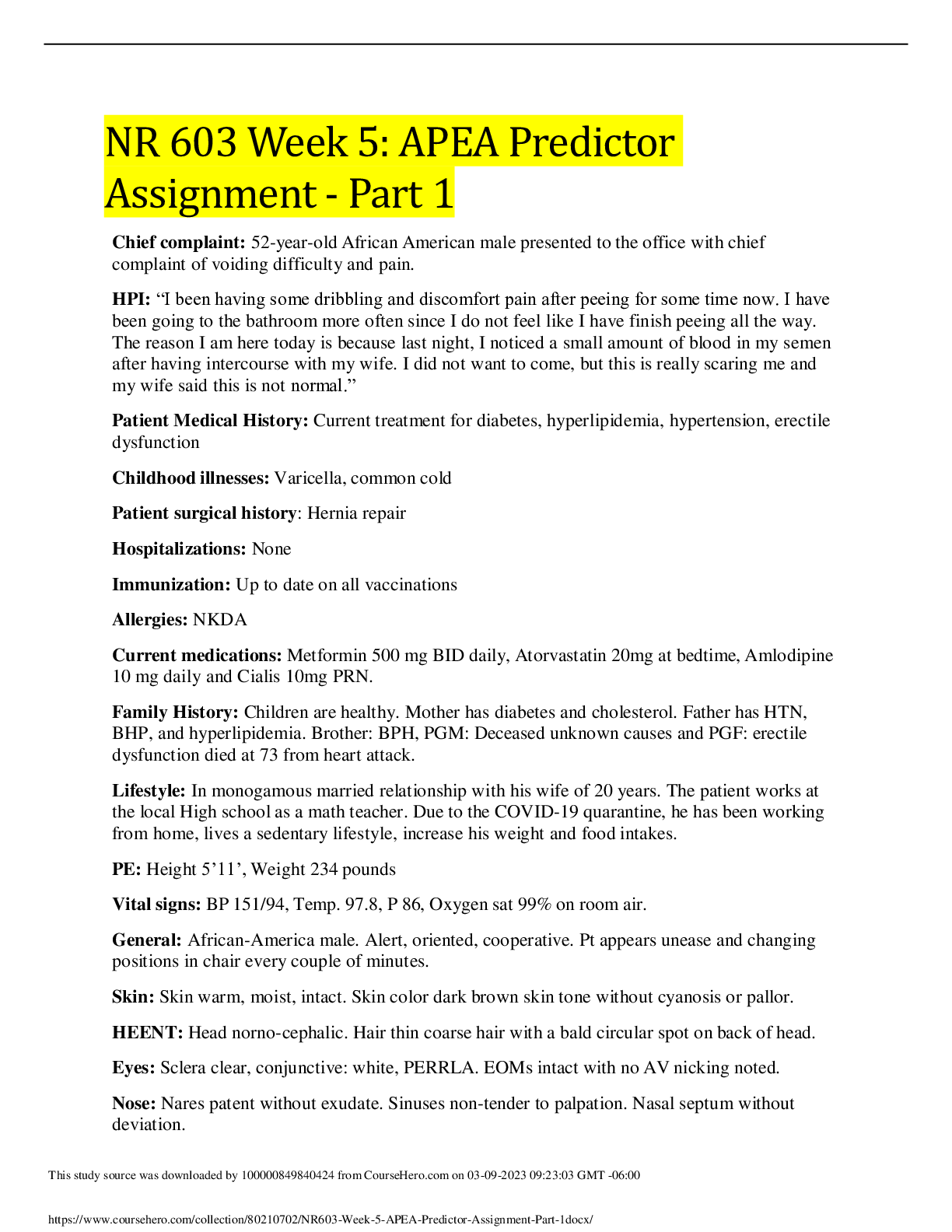
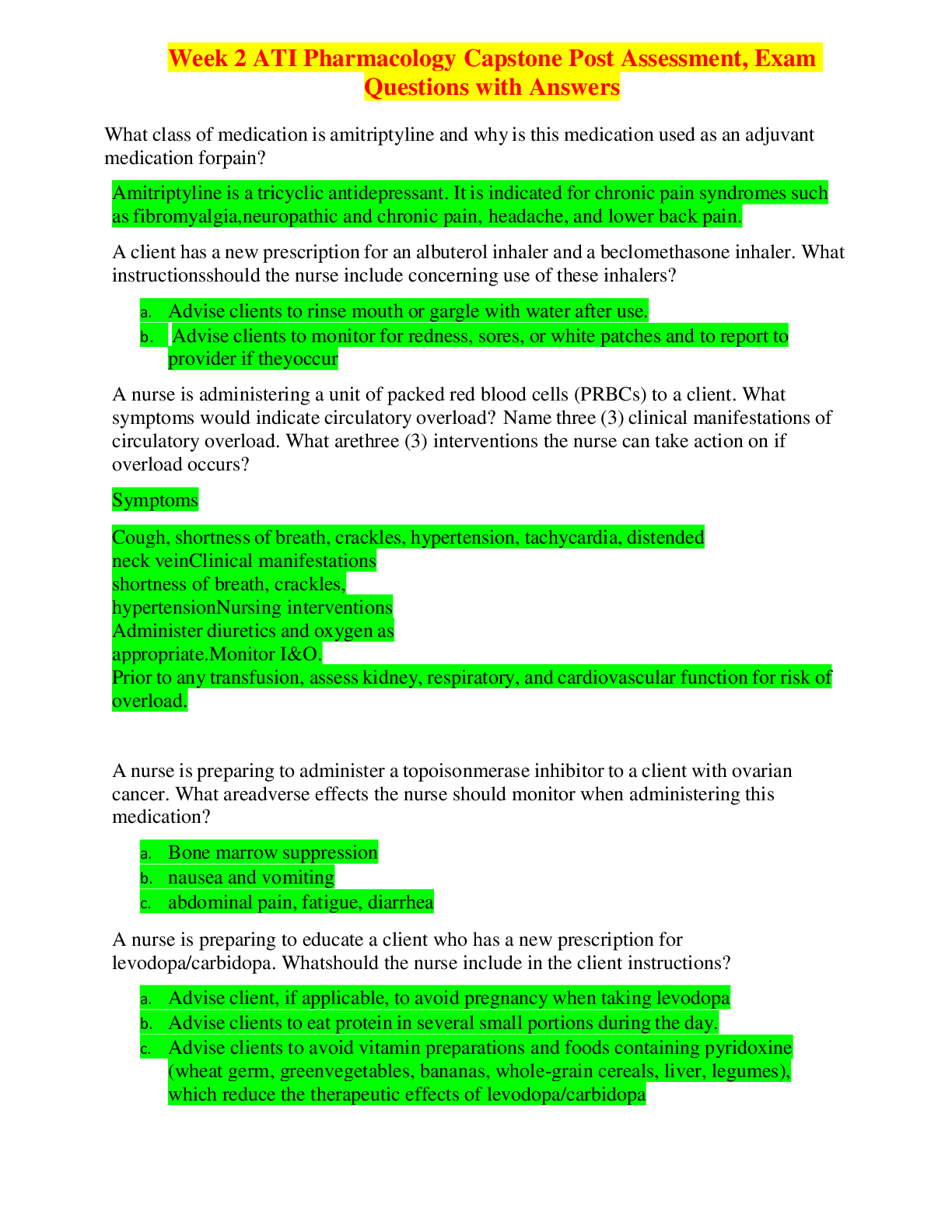
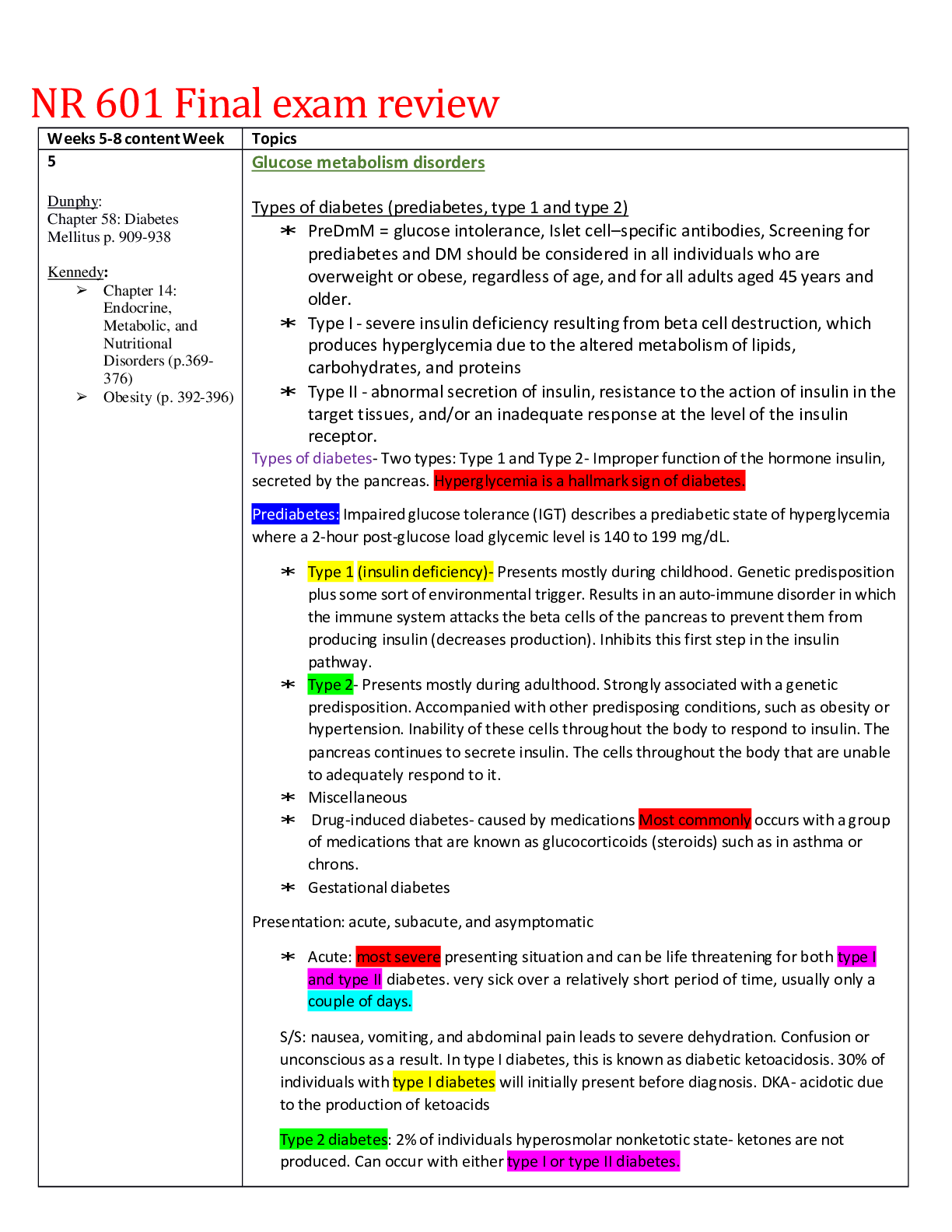
NR 601 Final exam review Weeks 5-8 content Week Topics 5 Dunphy: Chapter 58: Diabetes Mellitus p. 909-938 Kennedy: Chapter 14: Endocrine, Metabolic, and Nutritional Disorders (p.369- ... 376) Obesity (p. 392-396) Glucose metabolism disorders Types of diabetes (prediabetes, type 1 and type 2) PreDmM = glucose intolerance, Islet cell–specific antibodies, Screening for prediabetes and DM should be considered in all individuals who are overweight or obese, regardless of age, and for all adults aged 45 years and older. Type I - severe insulin deficiency resulting from beta cell destruction, which produces hyperglycemia due to the altered metabolism of lipids, carbohydrates, and proteins Type II - abnormal secretion of insulin, resistance to the action of insulin in the target tissues, and/or an inadequate response at the level of the insulin receptor. Types of diabetes- Two types: Type 1 and Type 2- Improper function of the hormone insulin, secreted by the pancreas. Hyperglycemia is a hallmark sign of diabetes. Prediabetes: Impaired glucose tolerance (IGT) describes a prediabetic state of hyperglycemia where a 2-hour post-glucose load glycemic level is 140 to 199 mg/dL. Type 1 (insulin deficiency)- Presents mostly during childhood. Genetic predisposition plus some sort of environmental trigger. Results in an auto-immune disorder in which the immune system attacks the beta cells of the pancreas to prevent them from producing insulin (decreases production). Inhibits this first step in the insulin pathway. Type 2- Presents mostly during adulthood. Strongly associated with a genetic predisposition. Accompanied with other predisposing conditions, such as obesity or hypertension. Inability of these cells throughout the body to respond to insulin. The pancreas continues to secrete insulin. The cells throughout the body that are unable to adequately respond to it. Miscellaneous Drug-induced diabetes- caused by medications Most commonly occurs with a group of medications that are known as glucocorticoids (steroids) such as in asthma or chrons. Gestational diabetes Presentation: acute, subacute, and asymptomatic Acute: most severe presenting situation and can be life threatening for both type I and type II diabetes. very sick over a relatively short period of time, usually only a couple of days. S/S: nausea, vomiting, and abdominal pain leads to severe dehydration. Confusion or unconscious as a result. In type I diabetes, this is known as diabetic ketoacidosis. 30% of individuals with type I diabetes will initially present before diagnosis. DKA- acidotic due to the production of ketoacids Type 2 diabetes: 2% of individuals hyperosmolar nonketotic state- ketones are not produced. Can occur with either type I or type II diabetes. Subacute: mild to moderate presentation that occurs over a period of weeks to months. S/S: Generally, just not feeling as well. Fatigue, increased thirst, frequent urination, or even weight loss. Most common form of presentation in Type 1 diabetes (70%). Asymptomatic screening tests: Type II diabetes affects nearly 10% of the population. Those with the risk factors of type II diabetes should be routinely screened. Most common means by which type II diabetes is diagnosed. Diagnostic criteria - ADA criteria for diagnosing DM- Random BG >200 (week 5 quiz question) 3 Ps of DM: polyphagia, polydipsia, polyuria (week 5 quiz question) FPG ≥126 mg/dL (7.0 mmol/L). Fasting is defined as no caloric intake for at least 8 hrs 2-h PG ≥200 mg/dL (11.1 mmol/L) during OGTT. The test should be performed as described by the WHO, using a glucose load containing the equivalent of 75-g anhydrous glucose load dissolved in water. A1C ≥6.5% (48 mmol/mol). The test should be performed in a laboratory using a method that is NGSP certified and standardized to the DCCT assay. In a patient with classic s/s of hyperglycemia or hyperglycemic crisis (polyuria, poly dipsia, weight loss), a random plasma glucose ≥200 mg/dL (11.1 mmol/L) Current guidelines for the diagnosis of DM include any one of the following: • Glycosylated hemoglobin (A1C) of 6.5% or higher • Symptoms of diabetes (e.g., polyuria, polydipsia, weight loss) plus a random plasma glucose level of 200 mg/dL or higher • Fasting plasma glucose level of 126 mg/dL or higher (following 8 hours of no caloric intake) • Two-hour plasma glucose level of 200 mg/dL or higher during an oral glucose tolerance test (OGTT) with a 75-g glucose load Diagnostic testing: laboratory tests. The hyperglycemia and the hemoglobin A1C are tested for in the blood to aid in the diagnosis of diabetes mellitus. Hemoglobin A1C: greater than or equal to 6.5% Blood glucose levels: greater than or equal to 200 mg/dL. Random- cannot be used to diagnose pre-diabetes. Fasting- slightly lower, then the level is 126 mg/dL. Two-hour glucose tolerance test Initial treatment recommendations If FPG is above 126, next action: order A1C (week 5 quiz question) Treatment goals for older adults (Kennedy table 14-2) Hbg A1C goals based on complications (Dunphy p.925) An A1C value of less than 7% indicates strong control; however, a value of less than 6.5% has been shown to significantly decrease the occurrence of complications, provided this can be achieved without hypoglycemia or other adverse effect. Weight loss recommendations (Kennedy) modest weight loss of 5% can improve glycemic control Risk factors (Dunphy p.922) Family history (first-degree relative) Body mass index >25 kg/m2 (lower for Asian Americans) Age >45 years Impaired fasting glucose or A1C >5.7% History of gestational diabetes Hypertension (> 140/90 mm Hg or on antihypertensive therapy) Hyperlipidemia (high-density lipoprotein <35 mg/dL, triglycerides >250 mg/dL) Women with polycystic ovarian syndrome Race/Ethnicity • African American • Latino • Native American • Asian American • Pacific Islander Complications (Dunphy p.919) Type 1 DM, the risk of development or progression of retinopathy, nephropathy, hyperlipidemia, and neuropathy Most common s/e of DM: Yeast infections (week 5 quiz question) : page 932 Dunphy • Retinopathy - Optimizing blood pressure and lipid levels can reduce the risk or slow the progression of retinopathy. • Hyperlipidemia - an annual fasting lipid profile, including serum cholesterol, triglyceride, HDL, and calculated LDL cholesterol measurements. Lifestyle management (i.e., modifications to diet and physical activity), pharmacologic therapy. The purpose of treatment is to reduce cardiovascular events. • Diabetic Kidney disease - A routine spot UACR (normal < 30 mcg albumin/mg creatinine) and eGFR should be performed annually on all diabetic patients. Maintaining normal serum glucose levels, controlling BP is the most effective method to slow or reduce the risk of diabetic kidney disease. ACEIs or ARBs are the recommended treatment for patients with DM and hypertension, abnormally high UACR, or a lower than normal eGFR. • Hypertension - Systolic blood pressure should be less than 140 mm Hg and diastolic blood pressure below 90 mm Hg. A lower blood pressure goal of 130/80 mm Hg may be appropriate for patients at high risk for cardiovascular events. Treatment can be with ACEIs, ARBs, thiazide-like diuretics, or dihydropyridine calcium channel blockers. • Macrovascular disease - Evidence of uncontrolled angina, carotid bruits, or ECG abnormalities may require advanced intervention and calls for referral to a cardiologist. Daily aspirin is recommended for cardiac prophylaxis in patients with a 10-year risk of CVD greater than 10% at a dose of 81 to 165 mg/day. Given the increased risk of bleeding due to its antiplatelet effects, aspirin is not recommended in low-risk patients with a 10-year CVD risk of less than 5%. • Neuropathy - All patients should be screened for neuropathic symptoms at the time of diagnosis and then at least annually. Patients with significant urinary symptoms or impotence should be referred to a urologist. • Pregnancy- every pregnancy in a woman with type 2 DM should be planned. Insulin is the first-line medication for the treatment of diabetes in pregnancy. • Hypoglycemia • DKA – Dunphy pg 914 table 58.2 • HHS – Dunphy pg 920 table 58.4 Treatments for complications Metformin – contraindicated in renal disease, abnormal creatinine clearance, acute MI, or septicemia (week 5 quiz question) Hypoglycemia is a medical emergency because of the seriousness of potential sequelae (e.g., seizures, coma, cardiovascular dysfunction, death). Initial testing for suspected hypoglycemia includes measurement of the blood glucose level. Hypoglycemia is typically diagnosed if the patient experiences a decrease in blood glucose concentration of greater than 100 mg/dL per hour or a blood glucose level of less than 50 mg/dL at any point during the test. The treatment of acute hypoglycemia for alert patients who can ingest by mouth is 6 to 12 ounces of orange juice or other fruit juice without additional sugar. The long-term management of hypoglycemia includes treatment of its underlying causes and dietary modifications as needed. SMBG is the cornerstone of long-term self-management of hypoglycemia. Treatment of choice for insulinoma is surgical resection Obesity o Comorbidities related to obesity type 2 diabetes, hypertension, sleep apnea, nonalcoholic fatty liver disease, hyperlipidemia, osteoarthritis, or heart disease Coronary heart disease/congestive heart failure • Hypertension • Dyslipidemia/hyperlipidemia • Type 2 diabetes mellitus/insulin resistance • Metabolic syndrome • Sleep apnea • Restrictive lung disease • Asthma • Varicose veins and venous insufficiency • Gout/hyperuricemia • Osteoarthritis • Reflux esophagitis • Gallbladder disease • Thromboembolic disease • Cancers: Endometrial, breast, prostate, colon o BMI classifications (Kennedy) Overweight is defined as a BMI of 25 to 29. Obesity is defined as a BMI >30 with morbid obesity as a BMI >40. • <18.5 Underweight • 18.5-24.9 Normal • 25.0-29.9 Overweight • 30.0-34-9 Class I obesity • 35.0-39.9 Class II obesity • >40.0 Class III extreme obesity Facts: If an individual has symptoms of diabetes, then only one positive test, either the blood glucose or the hemoglobin A1C is necessary for the diagnosis of [Show More]
Last updated: 3 years ago
Preview 1 out of 34 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$12.50
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Sep 22, 2021
Number of pages
34
Written in
All
Additional information
This document has been written for:
Uploaded
Sep 22, 2021
Downloads
0
Views
149