What leads demonstrate the ST depression?
Lorene demonstrates ST depression dispersed throughout the EKG. Specifically, the depression
is exhibited in leads I, II, V4, V5, a slight depression in aVF, and V6. There is a
...
What leads demonstrate the ST depression?
Lorene demonstrates ST depression dispersed throughout the EKG. Specifically, the depression
is exhibited in leads I, II, V4, V5, a slight depression in aVF, and V6. There is also an ST
elevation in aVR. The EKG shows signs of acute coronary syndrome (ACS). An EKG for ACS
will show ST depression in six or more leads, most significant in leads V4 to V6, particularly
when related with inverted T waves and ST elevation in lead aVR. These EKG changes should
warrant importantnce for urgent, aggressive evaluation because of the high probability of severe
angiographic coronary artery disease (Nikus et al., 2014).
Is Lorene Hypertensive per ACA 2017 Guidelines? Compare the ACA guidelines to JNC 8
guidelines and discuss what treatment you recommend for her BP and why?
According to the American College of Cardiology (ACC), Lorene’s blood pressure, which is
146/90, would place her in stage II hypertension (HTN). The ACC definitions of stage II is
systolic greater than or equal to 140 or diastolic greater than or equal to 90. Her blood pressure
numbers falls within the guidelines recommendations (Whelton, Carey, & Aronow, 2018).
The ACA and JNC 8 guidelines report the difference in opinions about the blood pressure
parameters. According to ACA normal blood pressure is systolic less than 120 mm Hg and
diastolic less than 80 mm Hg. HTN stage 1 systolic BP (SBP) is 130-139 mm Hg or diastolic BP
(DBP) 80-89 mm Hg, and HTN stage 2 SBP greater than or equal to 140 mm Hg or DBP greater
than or equal to 140 mm Hg or DBP greater than or equal to 90 mm Hg (Whelton, Carey, &
Aronow, 2018).
The JNC 8 recommendation is high blood pressure goals and to use fewer medications.
The guidelines also factor in the SBP and DBP with age and comorbidity-specific treatment. For
example, a patient who is 60 years old without diabetes (ADA) or chronic kidney disease (CKD),
the blood pressure goal is to be less than 150/90 mm Hg. In younger patients and patients who is
60 with a history of ADA and CKD, the goal for blood pressure is less than 140/90 mm Hg. The
ACA is a stricter guideline, recommending lowering numbers no matter what comorbidities that
patient has (American Family Physician, 2014).
After reviewing the two guidelines, a slower method of controlling blood pressure will be
adopted. Lorene is considered obese. She has hypertension, metabolic Syndrome, and
dyslipidemia. She also had a history of gestational diabetes, and her current A1c is elevated at
6.4%. With her current ST changes, Lorene’s blood pressure will need to be lowered. However,
starting aggressive treatment is not ideal, and she may feel the effects of lowering her BP to
quickly. Lorene needs to go back on medications. However, her belief about controlling her BP
with diet and exercise is correct and will be adopted in her treatment plan mentioned later in this
case study response.
What is the primary diagnosis causing Lorene’s chest pain? Include ICD 10 codes.
Lorene’s symptoms are consistent with Acute Coronary Syndrome (ACS), ICD 10 code
I24.9. Her report suggests having shortness of breath, discomfort that radiates back and up
between her shoulder blades. The discomfort happens on exertion and resolves with rest. She is
slightly nauseated and is diaphoretic. Symptoms of ACS consists of chest pain or discomfort, that
could include pressure, tightness or fullness; pain or discomfort unilateral or bilateral arms, neck,
the jaw, back or stomach; shortness of breath; feeling dizzy or lightheaded; nausea; and sweating.
An EKG for ACS will show ST depression in six or more leads, most significant in leads V4 to
V6 as stated before (Fuster, Kovacic, Josée, & Kravis, 2014).
What other secondary diagnoses does Lorene have that should be addressed?
Lorene’s secondary diagnoses are metabolic syndrome, hypertension (HTN), elevated
a1C, and tobacco dependence. These issues, along with being obese are indicators that Lorene
needs to make some lifestyle changes. If she can add diet, exercise and medication management
to her daily activities, she will be able to reverse some of these comorbidities.
Metabolic syndrome is defined in women as an increase in waist circumference, elevated
triglycerides higher than 175 mg/dL, low high-density lipoproteins less than 50 mg/dL, an
elevated blood pressure, and elevated glucose. Her blood pressure is significantly elevated. She
eats out at most resultants, works often, and socially drinks while having cigarettes once a week
(Wilson et al., 2018).
Design a treatment plan and discuss how each intervention applies to Lorene's case.
Consider the following interventions:
• Labs
• Durable Medical Equipment Diagnostic tests- discuss the goal/purpose
• Any consultation with outside providers/services
• Medications- discuss why you chose each specific medication
• Referrals- who and why
• Follow up- why and when
• Education- specific and measurable
• Lifestyle Changes- specific to her cultural preferences, values, and beliefs
ACS is considered one of the most common deaths for people in the United States. This
reason is why it is essential for primary care providers to diagnose and manage symptoms. ACS
is included in two clinical presentations: ST-elevation myocardial infarction (STEMI) and non–
ST elevation acute coronary syndrome (NSTE-ACS). Overall the ACC stresses the importance of
primary prevention to decrease risk factors for ACS. However, if primary preventions cannot be
achieved, then quick management must be implemented in a patient presenting with symptoms in
primary care (Swiataj, Christensen, & Brewer, 2017.
In the office, Lorenece will chew a nonenteric coasted aspirin (162to 325 mg) due to her
positive symptoms of ACS listed above. Sublingual nitroglycerin 0.3 -0.6 mg can be given every
five minutes for three doses within fifteen minutes to help with the chest pain. Her oxygen
saturation is 97%. Therefore oxygen therapy is not warranted. However, she should be attached
to pulseoximetry machine while waiting for the ambulance. Another staff member should have
called the ambulance, so Lorene can be transported quickly to the emergency room. If the
pharmacy care office can obtain labs, cardiac bio marks that include troponins will be collected.
The hospital will also collect these markers. Once at the hospital, the cardiologist will be
consulted, and they will take over to determine the method of treatment (Swiataj, Christensen, &
Brewer, 2017.
Once Lorene is treated and leaves the hospital, she will follow up with cardiology to help
reduce her risks of morbidity and mortality. The cardiologist will coordinate posthospitalization
care including a cardiac rehabilitation program, medication management, and follow-up. The
primary care provider and the cardiologist can work together creating strategies to control risk
factors, such as cholesterol levels, hypertension, and smoking (Swiataj, Christensen, & Brewer,
2017.
As the primary care provider, the goal for post-hospitalization is to create a plan to
manage, her metabolic syndrome, hypertension, elevated a1c and tobacco dependence. All these
issues lead to her to positive symptoms requiring her to be treated for ACS.
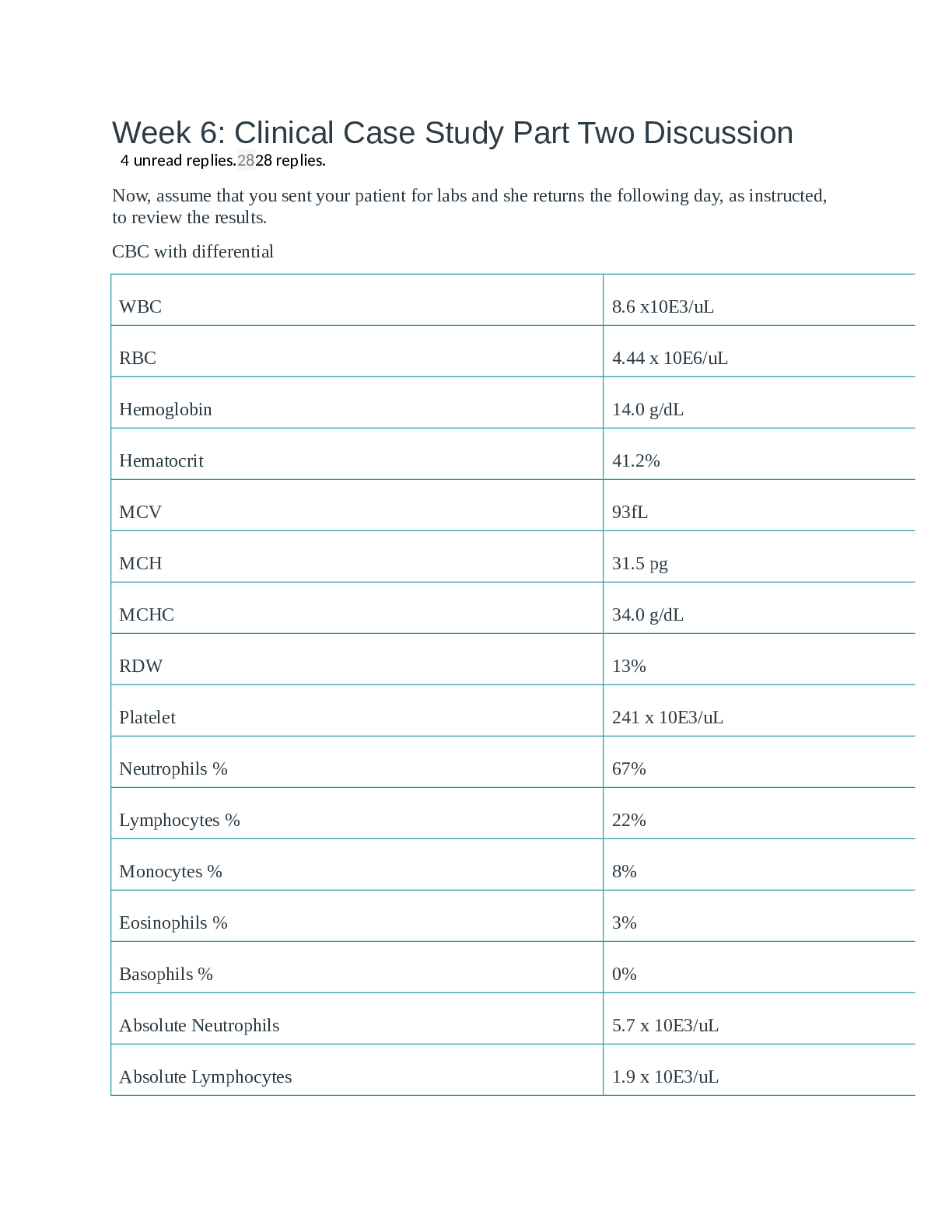
As for labs, the hospital records will be obtained, and a CMP, lipid panel, CBC, and A1C
will be collected to create a baseline. The provider will be using these labs to monitor her kidney
functions, cholesterol, and blood sugars for prediabetes management. Her labs three months ago
indicate that she is prediabetic. The A1c range for prediabetes is 5.7%-6.4%. She also has a a
high fasting glucose of 135 mg/dL. This number establishes her as a person with diabetes.
However, she would need to complete another fast blood sugar to see if the marker is elevated to
establish diabetes. The treatment plan will also include controlling her lipid panel. Her total
cholesterol ( 230 mg/dL) is borderline and needs to be lowered. Her HDL needs to increase in order
to help reduce the risk of more heart disease. Her LDL, which is 180 mg/dL, istoo high and needsto
be less than 100 mg/dL. These abnormal levels put her at higher risks for more cardiac events in the
future. She will obtain labs every three months until levels normalize. At six months to a year,
Lorene goal levels should be close to if not normal (Pippitt & Gurgle, 2016; Whelton, Carey, &
Aronow, 2018; Wilson et al., 2018).
Lorene will be on several medications to help control her complications. These
medications will control her HTN, ACS, and HDL. She will need to return in one month to
reassess these medications.
The cardiologist will most likely initiate aspirin (ASA) and other antiplatelet medications
like Clopidogrel. ASA blocks an enzyme called cyclooxygenase which is highly vasoactive and
prothrombotic. Clopidogrel is an anti-platelet medication that inhibits the adenosine diphosphate
(ADP) pathway. She will have the initial loading dose of these medications at the hospital. Daily
medications regimine is as followed. Depending on type of cardiac event, she may only be on
plavix for 12 months (Swiataj, Christensen, & Brewer, 2017).
Rx: Aspirin 81 mg
Sig: take one tablet by mouth daily.
Disp: 30 ( thirty)
Refill: 0 ( zero)
(Epocrates, 2019a)
Plavix ( clopidogrel) 75 mg
Sig: Take one tablet by mouth daily
Disp: 30 ( thirty)
Ref: 0 (zero)
(Epocrates, 2019e)
To control her blood pressure, the first medications Lorene will receive is a thiazide
diuretic. The goal is to reduce her blood pressure to less than 140/90mm Hg. If this is not
achieved after the first month, then she will be placed on a calcium channel blocker. The thiazide
controls blood pressure by inhibiting distal convoluted tubule sodium and chloride reabsorption
(American Family Physician, 2014).
Rx: Hydrochlorothiazide 25 mg
Sig: Take one tablet by mouth daily
Disp: 30 (thirty)
Ref: 0 ( zero)
(Epocrates, 2019b)
This medication will be added if blood pressure is not controlled
RX: Norvasc( amlodipine) 5 mg
Sig: Take one tablet by mouth daily
Dis: 30 ( thirty)
Ref: 0 ( zero)
(Epocrates, 2019d)
According to the ACC risk cacluator, Lorene is 40.7% risk for Atherosclerotic Coronary
Disease. (ASCVD). She should be prescribed a high-intensity statin therapy because she has
multiple ASCVD risk factor (American College of Cardiology, 2019).
Rx: Lipitor ( atorvastatin) 40 mg
Sig: Take two tablets twice daily. One tablet in the morning and one tablet in the evening.
Dis: 60 ( sixty)
Ref: 0 ( zero)
(Epocrates, 2019c)
Lorene’s cardiologist will decide when and what testsshe will need to have after a hospital
visit. Most likely she will have an EKG completed often and routine stress tests. Depending on
cardiologist recommendations, these test will be completed for the duration of her life (Swiataj,
Christensen, & Brewer, 2017.
Along with the cardiologist, a referral to a dietitian should be made to help Lorene choose
healthy options for meals. Recommendations to reduce lipid panel, prevent diabetes and reduce the
risk of cardiovascular events lifestyle changes must be made. The dietitian can help Lorene choose
healthy meals when she is eating out and also show her how to
[Show More]