AADE STUDY QUESTIONS SET 3
EXAM 2022
A 38-year-old man with type 2 diabetes and an A1C of 8.7% stopped taking
metformin 500mg twice daily due to persistent diarrhea. Which of the following is
most likely to achie
...
AADE STUDY QUESTIONS SET 3
EXAM 2022
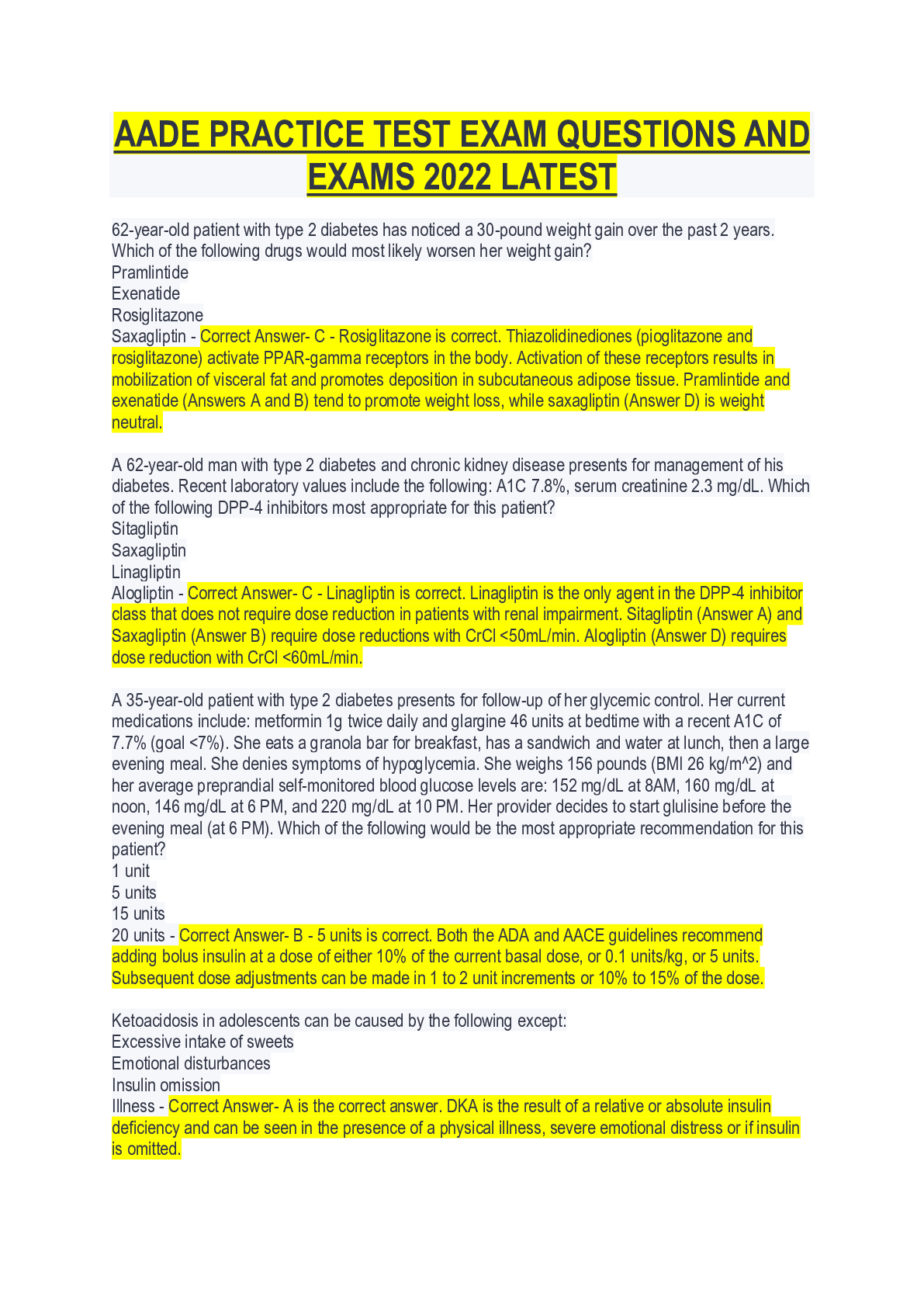
A 38-year-old man with type 2 diabetes and an A1C of 8.7% stopped taking
metformin 500mg twice daily due to persistent diarrhea. Which of the following is
most likely to achieve his A1C goal of less than 7%?
Liraglutide
Canagliflozin
Saxagliptin
Glimepiride - Correct Answer- D - Glimepiride is correct. Biguanides and
sulfonylureas lower A1C up to 2%, while other agents only lower A1C by 0.5% to
1%, including: GLP-1 receptor agonists like liraglutide (Answer A); SGLT2 inhibitors
like canagliflozin (Answer B); DPP-4 inhibitors like saxagliptin (Answer C).
A 36-year-old pregnant woman with gestational diabetes inadequately controlled with
diet and exercise presents for follow-up. She and her husband have tried to become
pregnant several times without success, and they are very concerned about the
effects of drugs on the fetus. Which of the following would be the most appropriate
addition to her regimen?
Glyburide
Metformin
Liraglutide
NPH insulin - Correct Answer- D - NPH insulin is correct. Recombinant human NPH
insulin is preferred during pregnancy due to its amino acid structure and long history.
Several meta-analyses suggest that glyburide (Answer A) is inferior to metformin and
insulin due to increased risk of neonatal hypoglycemia and macrosomia. About 50%
of the metformin dose crosses the placenta but is not associated with adverse
effects on the fetus; however, metformin may slightly increase the risk of prematurity
(Answer B). The GLP-1 receptor agonists (liraglutide, Answer D) are all FDA
Pregnancy Category C.
A 64-year-old man with type 2 diabetes, cardiovascular disease and heart failure
returns to clinic on metformin 1g twice daily plus glargine 65 units at bedtime. His
fasting glucose is 162 mg/dL with an A1C of 8.1% and eGFR 50 mL/min/1.73m2.
Which of the following would be the most appropriate recommendation for this
patient?
Increase metformin
Add empagliflozin
Add pioglitazone
Add dapagliflozin - Correct Answer- B - Add empagliflozin is correct. Based on data
from the EMPA-REG trial, adding empagliflozin to background therapy in patients
with established cardiovascular disease decreases heart failure hospitalizations by
35%, cardiovascular death by 38% and all-cause mortality by 32%. The optimal dose
of metformin is 2g per day, increasing the dose offers no additional A1C reduction
but does increase side effects (Answer A). Adding pioglitazone in this patient would
not be ideal considering his history of heart failure (Answer C). It is uncertain
whether the beneficial effects observed in EMPA-REG are restricted to empagliflozin
or represent a class effect; however, dapagliflozin (Answer D) is not recommended
in patients with an eGFR <60 mL/min/1.73m2.
Which of the following immunizations would be most appropriate for a 42-year-old
patient with type 2 diabetes who received the "pneumonia vaccine" 20 years ago?
Zostavax (zoster)
Prevnar 13 (pneumococcal 13-valent conjugate)
Pneumovax 23 (pneumococcal polysaccharide)
MenB (meningococcal B) - Correct Answer- C - Pneumovax 23 (pneumococcal
polysaccharide) is correct. Patients with diabetes are at increased risk for
pneumococcal infection with a mortality rate as high as 50%. All patients with
diabetes older than 2 years of age should initially receive Prevnar 13 prior to
pneumococcal polysaccharide vaccine 23 (PPSV23). Patients with diabetes older
than 19 years and those at high risk of infection should receive follow-up vaccination
with PPSV23. Immunocompromised patients (including people over age 65 with a
"naturally" declining immune system) mount a better response with Prevnar 13
followed by PPSV23 one year later. Zostavax (Answer A) is indicated for patients
over age 50 to prevent herpes zoster (shingles). Vaccination against meningococcal
B (Answer D) is indicated for adults less than age 25 as a 2-dose series at least one
month apart.
Which of the following best describes the onset of insulin lispro?
15 to 30 minutes
1 to 3 hours
4 to 6 hours
6 to 12 hours - Correct Answer- A - 15 to 30 minutes is correct. Rapid acting insulin
products, such as lispro, aspart and glulisine enter the bloodstream 15 to 30 minutes
after subcutaneous injection. Short-acting regular insulin has an onset of 30 to 60
minutes and lasts approximately 4 to 6 hours (Answers B and C). The intermediate
and long-acting insulin products have a 1 to 3 hour onset of action, with NPH
reaching its peak effect at 6 hours and lasting 12 hours (Answer D).
Which of the following patients with diabetes would most benefit from aspirin
therapy?
41-year-old male and no risk factors
54-year-old female and 10-yr ASCVD risk 5.6%
59-year-old male with hypertension who also smokes
61-year-old female and 10-yr ASCVD risk of 4.2% - Correct Answer- C - 59-year-old
male with hypertension who also smokes is correct. The 2016 ADA guidelines
recommend aspirin 75mg to 162mg daily for patients with type 1 or type 2 diabetes
and a 10-yr ASCVD risk >10%. This degree of risk includes most men and women >
50 with diabetes and at least 1 additional risk factor (hypertension, dyslipidemia,
smoking, albuminuria, or family history of ASCVD).
A 28-year-old woman with Type 1 diabetes for 10 years needs to re-calculate a
mealtime (insulin to carbohydrate ratio) bolus based on her new insulin regimen. Her
current total daily dose (TDD) of insulin is 60 units. Which of the following best
estimates the amount of carbohydrates matched by 1 unit of insulin?
3 g
8 g
25 g
30 g - Correct Answer- B - 8 g is correct. The Rule of 500 estimates the amount of
carbohydrates matched by 1 unit of insulin. This patient takes a total daily dose
(TDD) of 60 units (500 divided by 60 units = 8 g of carbohydrate). A general rule of
thumb is that 1 unit of insulin is necessary for every 15 g of carbohydrate.
A 25-year-old pregnant woman with gestational diabetes inadequately controlled with
diet, exercise and metformin presents for follow-up. Which of the following would be
the most appropriate addition to her regimen?
Glulisine
Glargine
Detemir
Degludec - Correct Answer- C - Detemir is correct. All insulin products are FDA
Pregnancy Category B except for glulisine, glargine and degludec which are labeled
category C
During a routine foot exam, the provider observes several signs. Which of the
following is a sign of peripheral artery disease (PAD)?
Warm, reddened skin
Diminished hair growth
Palpable dorsalis pedis pulses
Prominent metatarsal heads - Correct Answer- B - Diminished hair growth is correct.
Peripheral artery disease (PAD) is characterized by signs of inadequate perfusion
(Answer C) that may include cool skin temperature, bluish color (Answer A), and
diminished hair growth. Prominent metatarsal heads (Answer D) is related to loss of
motor nerve function that allows involuntary flexion.
Which of the following lab parameters best correlates with mental functioning during
HHS and DKA?
Plasma sodium level
Serum osmolality
Blood pH
Serum glucose - Correct Answer- B - Serum osmolality. Although disturbances in
sodium (Answer A), glucose (Answer D) and blood pH (Answer C) occur during HHS
and DKA, serum osmolality has the greatest effect on mental functioning. Increased
osmolality occurs with dehydration and overhydration may create a hypotonic state
causing cells to fill and potentially lyse.
A 78-year-old woman with type 2 diabetes (A1C 7.8%, serum creatinine 0.9 mg/dL)
presents for evaluation. She resides in an assisted living facility and is accompanied
today by her daughter. She appears in good health but reports longstanding urinary
incontinence and has been wearing adult diapers for years. She also reports
frequently skipping meals because it is "too far to walk to the dining room." Her vital
signs today are as follows: weight 110 pounds (BMI 17 kg/m^2), blood pressure
118/68 mmHg, pulse 66 BPM. Which of the following would be the LEAST
appropriate recommendation?
Metformin
Saxagliptin
Canagliflozin
Pioglitazone - Correct Answer- C - Canagliflozin is correct. The SGLT2 inhibitors
block 90% of glucose reuptake from the kidney (approximately 100 g/day). Increased
glucose excretion results in increased risk of urinary tract and genital mycotic
infections. Because of the longstanding history of urinary incontinence in this patient
and chronic use of adult diapers, she is at high risk of genitourinary infection.
Metformin, saxagliptin and pioglitazone (Answers A, B and D) would be reasonable
options for this elderly patient with good kidney function but concerns about
hypoglycemia.
Which of the following does NOT occur more commonly in children with type 1
diabetes than the general pediatric population?
Celiac disease
Hypothyroidism
Addison disease
Asthma - Correct Answer- D - Asthma is correct. Patients with type 1 diabetes are at
increased risk of other autoimmune diseases. Children with type 1 diabetes should
be screened for celiac disease and hypothyroidism soon after diagnosis. Type 1
diabetes does not increase the risk of asthma in children.
What impact does diabetes have on the development of coronary artery disease in
women compared with men?
Women have a higher risk than men
Men have a higher risk than women
The risk is minimal in both sexes
The risk is the same for both sexes - Correct Answer- A - Women have a higher risk
than men. Although premenopausal women without diabetes have a lower risk of
coronary artery disease compared with men, having diabetes eliminates the
protective effect of estrogen.
Which of the following is the most compelling reason to avoid very strict glycemic
control (A1C <6%) based on data from the ACCORD trial?
Increased mortality
Increased drug cost
Increased retinopathy
Increased nephropathy - Correct Answer- A - Increased mortality is correct. Although
intensification of therapy often increases drug cost (Answer B), patients in the
intensive therapy group (goal A1C <6% compared with an A1C goal of 7% to 7.9% in
the control group) of the ACCORD trial experienced a 22% increase in mortality. This
increased mortality risk was not associated with A1C, severe hypoglycemia or weight
gain. Intensive glycemic control reduces the risk of microvascular complications
(Answer C and D); however, these benefits are offset by the increased mortality risk.
Which of the following childhood illnesses is most associated with diabetes? CONTINUES.....
[Show More]