Computer Science > QUESTIONS & ANSWERS > Certified Coding Specialist (CCS) Exam Preparation 2022 – COMPLETE SOLUTION (All)
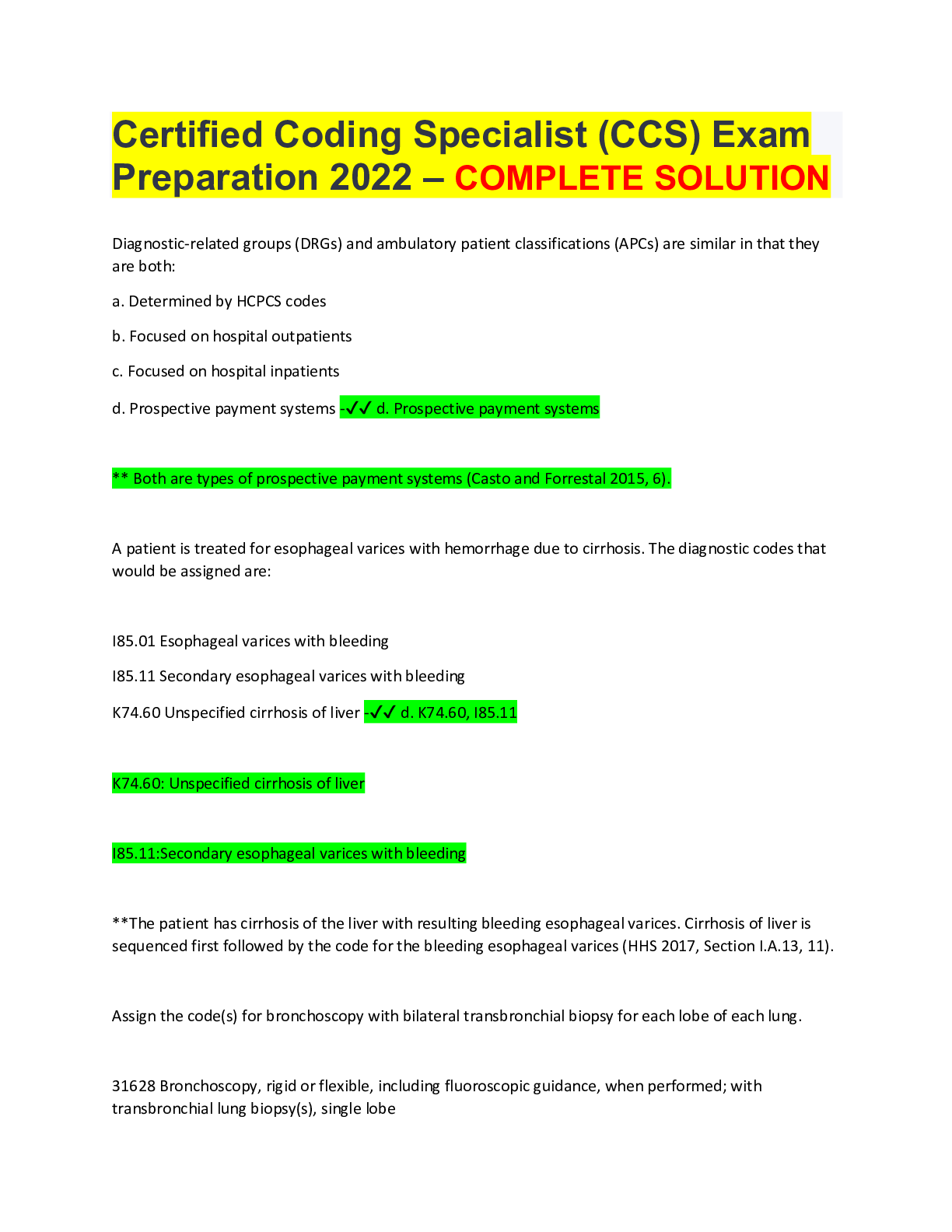
Certified Coding Specialist (CCS) Exam Preparation 2022 – COMPLETE SOLUTION Diagnostic-related groups (DRGs) and ambulatory patient classifications (APCs) are similar in that they are both: a. D ... etermined by HCPCS codes b. Focused on hospital outpatients c. Focused on hospital inpatients d. Prospective payment systems -✔✔ d. Prospective payment systems ** Both are types of prospective payment systems (Casto and Forrestal 2015, 6). A patient is treated for esophageal varices with hemorrhage due to cirrhosis. The diagnostic codes that would be assigned are: I85.01 Esophageal varices with bleeding I85.11 Secondary esophageal varices with bleeding K74.60 Unspecified cirrhosis of liver -✔✔ d. K74.60, I85.11 K74.60: Unspecified cirrhosis of liver I85.11:Secondary esophageal varices with bleeding **The patient has cirrhosis of the liver with resulting bleeding esophageal varices. Cirrhosis of liver is sequenced first followed by the code for the bleeding esophageal varices (HHS 2017, Section I.A.13, 11). Assign the code(s) for bronchoscopy with bilateral transbronchial biopsy for each lobe of each lung. 31628 Bronchoscopy, rigid or flexible, including fluoroscopic guidance, when performed; with transbronchial lung biopsy(s), single lobe31629 Bronchoscopy, rigid or flexible, including fluoroscopic guidance, when performed; with transbronchial needle aspiration biopsy(s), trachea, main stem and/or lobar bronchus(i) 31632 Bronchoscopy, rigid or flexible, including fluoroscopic guidance, when performed; with transbronchial lung biopsy(s), each additional lobe −50 Bilateral procedure -✔✔ Assign the code(s) for endoscopic sinusotomy with bilateral anterior ethmoidectomy. 31231 Nasal endoscopy, diagnostic, unilateral or bilateral (separate procedure) 31254 Nasal/sinus endoscopy, surgical; with ethmoidectomy, partial (anterior) −50 Bilateral procedurea. a. 31254 b. 31254-50 c. 31254, 31254 d. 31231 -✔✔ b. 31254-50 31254 Nasal/sinus endoscopy, surgical; with ethmoidectomy, partial (anterior) −50 Bilateral procedurea. ** A code for the anterior ethmoidectomy is assigned and to denote the bilateral procedure, a modifier of -50 is added (CPT Assistant Winter 1993, 23; Jan. 1997, 4; Sept. 1997, 10; Oct. 1997, 5; Dec. 2001, 6; May 2003, 5). The sinusotomy is not coded separately, as it is a diagnostic procedure. The most common language used for both data definition language and data manipulation language is: a. Unified modeling language b. JAVA c. Perl d. Structured query language -✔✔ d. Structured query language ** Structured query language (SQL) is used commonly for data language and data definitions (Sharp 2016, 184).An ethmoidectomy removes infected tissue and bone in the ethmoid sinuses that blocks natural drainage. The surgeon views your ethmoid sinuses with an endoscope, a thin flexible tube with a very small camera and light at the end of it. -✔✔ Documentation from the nursing or other allied health professionals' notes can be used to establish which of the following diagnoses: a. Body mass index (BMI) b. Malnutrition c. Aspiration pneumonia d. Fatigue -✔✔ a. Body mass index (BMI) ** The physician must establish the diagnosis—obesity or morbid obesity—and the additional information can be pulled from ancillary documentation to establish the correct code assignment for body mass index (BMI) (Leon-Chisen 2017, 168). A 55-year-old patient has hypertensive heart disease with congestive heart failure. What code would be assigned? a. I15.8, Other secondary hypertension b. I11.0, Hypertensive heart disease with heart failure and I50.9, Heart failure, unspecified c. I50.9, Heart failure, unspecified and I15.0, Renovascular hypertension d. N18.6, End stage renal disease -✔✔ b. I11.0, Hypertensive heart disease with heart failure and I50.9, Heart failure, unspecified ** There is a cause and effect relationship established between the hypertension and the congestive heart failure. A separate code for the congestive heart failure is assigned based on the "code also" note (HHS 2017, Section I.C.9.a., 40). A surgeon would like to undertake a research study on his patients with stage II malignant melanoma of the back, who have undergone wide excision of the melanoma. What work processes and associated software could be used to provide this information?a. Obtain a summary of the cases from the cancer registry, import them into a spreadsheet, and provide to the surgeon. b. Obtain a summary of the cases from the chart completion software, import them into a spreadsheet, and provide to the surgeon. c. Obtain a summary of the cases from the master patient index, import them into a spreadsheet, and provide to the surgeon. d. Obtain a summary of the cases from the transcription tracking software, import them into a spreadsheet, and provide to the surgeon. -✔✔ a. Obtain a summary of the cases from the cancer registry, import them into a spreadsheet, and provide to the surgeon. **The cancer registry can be used to undertake studies in addition to reporting cases to a central registry (Sharp and Madlock-Brown 2016, 173). A facility located near a national park has a significant number of snake bites, and patients receive treatment with antivenom in urgent-care settings. Sometimes a patient is admitted to the hospital after several days. Can the urgent-care setting provide the hospital with a list of names of patients treated with snake antivenom? a. Only the names of patients who are admitted to the hospital can be requested if the physician needs it for continuity of care, but an entire list of patients cannot be provided. b. A list of names could be provided. c. No information can be obtained under any circumstances. d. A list of patients may be available after consultation with the national park ranger. -✔✔ a. Only the names of patients who are admitted to the hospital can be requested if the physician needs it for continuity of care, but an entire list of patients cannot be provided. **Only records that are required for care or authorized by the patient can be released by the urgentcare facility to the acute-care facility (Brodnik 2012, 225; Rinehart-Thompson 2016b, 243-247). What diagnoses and procedures should be reported for recurrent left inguinal hernia with laparoscopic repair?K40.30 Unilateral inguinal hernia, with obstruction, without gangrene, not specified as recurrent K40.31 Unilateral inguinal hernia, with obstruction, without gangrene, recurrent K40.91 Unilateral inguinal hernia, without mention of obstruction or gangrene, recurrent 49520 Repair recurrent inguinal hernia, any age; reducible 49521 Repair recurrent inguinal hernia, any age; incarcerated or strangulated 49651 Laparoscopy, surgical; repair recurrent inguinal hernia a. K40.91, 49520 b. K40.31, 49521 c. K40.91, 49651 d. K40.30, 49520 -✔✔ c. K40.91:Unilateral inguinal hernia, without mention of obstruction or gangrene, recurrent 49651:Laparoscopy, surgical; repair recurrent inguinal hernia **The patient has a recurrent hernia without obstruction and this is captured in diagnosis code K40.91 (Leon-Chisen 2017, 253; CPT Assistant Nov. 1999, 24; March 2000, 9). .In order to accurately code a cardiac catheterization, what needs to be determined based on a review of the documentation? a. The approach and the side of the heart (chambers) into which the catheter was inserted b. The approach, the side of the heart (chambers) into which the catheter was inserted, as well as any additional procedures performed c. The duration of the procedure d. If there is documentation of the procedure in the medical record that stents are considered -✔✔ b. The approach, the side of the heart (chambers) into which the catheter was inserted, as well as any additional procedures performed A condition is present on admission when: a. It is the principal diagnosisb. It is accordance with medical staff bylaws c. A condition that occurs prior to an inpatient admission d. It is present within 3 days after admission -✔✔ c. A condition that occurs prior to an inpatient admission **It is important to understand the time frame for assigning a status code specifying that a condition is present on admission (Leon-Chisen 2017, 571-574). A patient was admitted after a fall down the steps. The patient was unconscious for approximately 45 minutes and was admitted to the emergency department (ED) within 3 hours of the fall. A CT scan was performed within an hour of admission to the ED. A cerebral contusion was diagnosed by the ED physician based on the findings in the CT scan. What conditions should be reported on the Uniform Billing form 04 (UB-04)? R40.0 Somnolence S02.91XA Unspecified fracture of skull, initial encounter for closed fracture S06.331A Contusion and laceration of cerebrum, unspecified, with loss of consciousness of 30 minutes or less, initial encounter S06.332A Contusion and laceration of cerebrum, unspecified, with loss of consciousness of 31 minutes to 59 minutes, initial encounter W10.9XXA Fall (on) (from) unspecified stairs and steps, initial encounter a. S02.91XA, W10.9XXA b. R40.0 c. S06.331A, W10.9XXA d. S06.332A, W10.9XXA -✔✔ d. S06.332A:Contusion and laceration of cerebrum, unspecified, with loss of consciousness of 31 minutes to 59 minutes, initial encounter. W10.9XXA: Fall (on) (from) unspecified stairs and steps, initial encounter**The code for the injury to the brain also includes the time of unconsciousness. The external cause code is provided here as part of the review; however, no external cause codes are used on the exam except those for poisonings and adverse effects of drugs (Leon-Chisen 2017, 487-488). Medicare reimbursement depends on all of the following, except: a. The correct designation of the principal diagnosis b. Policies and procedures of the medical staff c. The presence or absence of additional codes that represent complications, comorbidities, or major complications/comorbidities d. Procedures performed -✔✔ b. Policies and procedures of the medical staff **Policies and procedures of the medical staff are not relevant. But the presence or absence of additional codes that represent complications, comorbidities, or major complications/ comorbidities are all important to determine the MS-DRG as part of Medicare Acute Inpatient Prospective Payment System (Leon-Chisen 2017, 566; Rinehart-Thompson 2016a, 240-241). A 35-year-old woman has hypertension with acute renal failure and stage 3 chronic kidney disease. What code would be assigned? a. N17.9, Acute kidney failure, unspecified b. I13.2, Hypertensive heart and chronic kidney disease with heart failure and with stage 5 chronic kidney disease, or end stage renal disease c. I50.9, Heart failure, unspecified d. N17.9, Acute kidney failure, unspecified and I12.9, Hypertensive chronic kidney disease with stage 1 through stage 4 chronic kidney disease, or unspecified chronic kidney disease and N18.3, Chronic kidney disease, stage 3 (moderate) -✔✔ d. N17.9, Acute kidney failure, unspecified and I12.9, Hypertensive chronic kidney disease with stage 1 through stage 4 chronic kidney disease, or unspecified chronic kidney disease and N18.3, Chronic kidney disease, stage 3 (moderate) **Code the hypertension with stage 3 chronic kidney disease. In this case, both hypertension and chronic kidney disease are documented and a combination code is used. Also the code for the stage 3 chronic kidney disease must be assigned due to the "code also" note. The acute renal failure is identified with a separate code (HHS 2017, Section I.C.9.a., 40; HHS 2017, Section I.C.14.a., 53).A patient is diagnosed with infertility due to endometriosis and undergoes an outpatient laparoscopic laser destruction of pelvic endometriosis. In order to code this encounter accurately, what steps must the coder take? a. Review the operative report to determine what procedure codes to use and also to determine the site or sites of endometriosis so codes with the highest specificity may be assigned, and use infertility as a principal diagnosis. b. Review the operative report to determine where the laser was used in the pelvis so the site or sites of endometriosis can be specified, and assign a principal diagnosis of infertility. c. Review the operative report to determine where the laser was used in the pelvis so the site or sites of endometriosis can be specified as principal, and assign a secondary diagnosis of infertility. d. Review the operative report to determine what procedure codes to use and also to determine the site or sites of endometriosis so codes with the highest specificity may be assigned, and use the diagnosis of infertility as a secondary condition. -✔✔ d. Review the operative report to determine what procedure codes to use and also to determine the site or sites of endometriosis so codes with the highest specificity may be assigned, and use the diagnosis of infertility as a secondary condition. ** There may be endometrial implants throughout the pelvic cavity which may attach to various anatomic structures such as the fallopian tube, ovary, and omentum. These locations should be identified so that the appropriate diagnostic codes can be assigned and the appropriate procedure codes can be assigned based on the destruction of the endometrial implants. Therefore, the correct answer is to review the operative report to determine what procedure codes to use and determine the site or sites of endometriosis so that codes with the highest specificity may be assigned. Also, use the diagnosis of infertility as a secondary condition (Schraffenberger 2017, 455-457; Leon-Chisen 2017, 272). A patient is admitted to a psychiatric unit of an acute-care facility. The patient experienced the following symptoms almost every day for the last month: loss of interest or pleasure in most or all activities, which is a change from her prior level of functioning. She has also gained 15 lbs, has difficulty falling asleep, feels fatigued, and has difficulty making decisions. What potential diagnosis most closely fits the patient's overall symptoms? a. Insomnia b. Major depression c. Reye's syndrome d. Bipolar disorder -✔✔ b. Major depressionThe CPT definition of a surgical package contains which of the following? a. The surgical procedure(s) b. Follow-up surgery c. Preoperative tests d. Yearly follow-up visits -✔✔ a.The surgical procedure(s) **The surgical package refers to a combination of individual services provided during one surgical operation (Smith 2017, 55). A patient was admitted to the endoscopy unit for a screening colonoscopy. During the colonoscopy, polyps of the colon were found and a polypectomy was performed. What diagnostic codes should be used and how should they be sequenced? Z12.11 Encounter for screening for malignant neoplasm of colon D12.6 Benign neoplasm of colon, unspecified a. Z12.11 b. D12.6 c. Z12.11, D12.6 d. D12.6, Z12.11 -✔✔ c. Z12.11: Encounter for screening for malignant neoplasm of colon D12.6:Benign neoplasm of colon, unspecified **The circumstances of the encounter are for a screening colonoscopy. Because of this screening, colonoscopy is listed first, followed by a code for the polyps (HHS 2017, Section I.C.21, 90). A patient has a principal diagnosis of pneumonia (J18.9) (MS-DRG 195). Which of the following may legitimately change the coding of the pneumonia in accordance with the UHDDS and relevant clinical documentation?a. Sputum culture reflects growth of normal flora. b. Patient has a positive gram stain. c. Patient is found to have dysphagia with aspiration. d. Patient has nonproductive sputum. -✔✔ c. Patient is found to have dysphagia with aspiration. ** Patient is found to have dysphagia with aspiration is the correct answer because it changes the coding to aspiration pneumonia and would result in MS-DRG 179 RESPIRATORY INFECTIONS & INFLAMMATIONS W/O CC/MCC, which has a weight of 0.9325 (Medicare Grouper Version Used: 2017). This is in comparison to MS-DRG 0195, SIMPLE PNEUMONIA & PLEURISY W/O CC/MCC MDC: 04 which has a DRG weight of 0.7028 (Medicare Grouper Version Used: 2017). A method of checking the accuracy of data is to: a. Validate the purpose for the data collection b. Warehouse data on a regular basis c. Authenticate all end users d. Ensure that each record or entry within the database is correct -✔✔ d. Ensure that each record or entry within the database is correct ** A good process to ensure the data is accurate is to make certain each record or entry within the database is correct (Sharp and Madlock-Brown 2016, 195). Assign the code(s) for chest x-ray, complete. 71010 Radiologic examination, chest; single view, frontal 71020 Radiologic examination, chest, 2 views, frontal and lateral 71030 Radiologic examination, chest, complete, minimum 4 views 71035 Radiologic examination, chest, special views (eg, lateral decubitus, Bucky studies) a. 71020b. 71030 c. 71010, 71035 d. 71035 -✔✔ b. 71030 Radiologic examination, chest, complete, minimum 4 views **The code for a complete chest x-ray includes a minimum of four views and does not include computer-aided detection or fluoroscopy (CPT Assistant July 2007, 6; Dec. 2009, 14). A 45-year-old female with chronic ulcerative enterocolitis and steroid induced osteoporosis due to longterm steroid therapy. What codes should be assigned? K50.00 Crohn's disease of small intestine without complications K51.00 Ulcerative pancolitis without complications M81.0 Age-related osteoporosis without current pathological fracture M81.8 Other osteoporosis without current pathological fracture T38.0X5A Adverse effects of glucocorticoids and synthetic analogues, initial encounter Z79.52 Long term (current) use of systemic steroids Z79.899 Other long term (current) drug therapy a. K51.00, M81.8, T38.0X5A, Z79.52 b. K50.00, M81.0, T38.0X5A, Z79.52 c. K51.00, M81.0, T38.0X5A, Z79.899 d. K50.00, M81.8, T38.0X5A, Z79.52 -✔✔ a. K51.00: Ulcerative pancolitis without complications. M81.8:Other osteoporosis without current pathological fracture. T38.0X5A: Adverse effects of glucocorticoids and synthetic analogues, initial encounter. Z79.52:Long term (current) use of systemic steroids **The ulcerative colitis and osteoporosis should be coded as well as the adverse effect and long term use of the steroid (HHS 2017, Section I.C.19.e, 74).** In order to determine the correct procedure code, the lengths of the wounds repaired with the same type of closure are added together (AMA CPT Professional Edition 2017, 75, Surgery/ Integumentary Section directions). [Note: Since this is an emergency department visit, CPT codes are assigned, rather than ICD-10-PCS codes.] A patient was treated in the emergency department with lacerations of the neck and underwent a repair of two (2) wounds of the neck (2.0 cm and 1.4 cm) with layered closure. What are the diagnosis (excluding external cause codes) and procedure codes assigned? S11.91XA Laceration without foreign body of unspecified part of neck, initial encounter S11.92XA Laceration with foreign body of unspecified part of neck, initial encounter 0HQ4XZZ Repair neck skin, external approach 12041 Repair, intermediate, wounds of neck, hands, feet and/or external genitalia; 2. 5 cm or less 12042 Repair, intermediate, wounds of neck, hands, feet, and/or external genitalia; 2.6 cm to 7.5 cm a. S11.91XA, 0HQ4XZZ b. S11.92XA, 0HQ4XZZ c. S11.92XA, 12041 d. S11.91XA, 12042 -✔✔ d. S11.91XA :Laceration without foreign body of unspecified part of neck, initial encounter. 12042: Repair, intermediate, wounds of neck, hands, feet, and/or external genitalia; 2.6 cm to 7.5 cm Assign the code(s) for diagnostic left and right cardiac catheterization, left and right coronary arteriogram with low osmolar contrast and fluoroscopic guidance. 4A023N6 Measurement of cardiac sampling and pressure, right heart, percutaneous approach 4A023N7 Measurement of cardiac sampling and pressure, left heart, percutaneous approach 4A023N8 Measurement of cardiac sampling and pressure, bilateral, percutaneous approach B2141ZZ Fluoroscopy of right heart using low osmolar contrastB2151ZZ Fluoroscopy of left heart using low osmolar contrast B2161ZZ Fluoroscopy of right and left heart using low osmolar contrast B2111ZZ Fluoroscopy of Multiple Coronary Arteries using Low Osmolar Contrast a. 4A023N6, 4A023N7 b. 4A023N8, B2111ZZ c. 4A023N6 d. 4A023N7 -✔✔ b. 4A023N8: Measurement of cardiac sampling and pressure, bilateral, percutaneous approach B2111ZZ: Fluoroscopy of Multiple Coronary Arteries using Low Osmolar Contrast **There is a combination code for a left and right cardiac catheterization (4A023N8). Both the diagnostic cardiac catheterization and the cardiac angiography procedures are assigned (Leon- Chisen 2017, 412- 414). A patient is admitted with an acute exacerbation of COPD with stage 5 hypertensive kidney disease. What is the correct diagnostic code assignment? I12.0 Hypertensive chronic kidney disease with stage 5 or end-stage renal disease I12.9 Hypertensive chronic kidney disease, stage 1 through stage 4, or unspecified with chronic kidney disease J44.1 Chronic obstructive pulmonary disease with exacerbation J44.9 Chronic obstructive pulmonary disease, unspecified N18.5 Chronic kidney disease, stage 5 a. J44.9, I12.0 b. J44.1, I12.9 c. J44.9, I12.0 d. J44.1, I12.0, N18.5 -✔✔ d. J44.1, I12.0, N18.5J44.1 Chronic obstructive pulmonary disease with exacerbation. I12.0 Hypertensive chronic kidney disease with stage 5 or end-stage renal disease. N18.5 Chronic kidney disease, stage 5 **Acute exacerbation of COPD is coded as J44.1. The hypertension is present with the chronic renal disease. Because of this, a combination code for hypertension and chronic renal disease is coded. In addition, the stage of the kidney disease is also coded (HHS 2017, Section I.C.14.a, 53). A data map or crosswalk consists of: a. Terms used to describe paths between classifications and vocabularies b. A map of time frames for multiple project completion c. A descriptive list of data names d. Normalized data attributes -✔✔ a. Terms used to describe paths between classifications and vocabularies **There are several definitions of mapping and crosswalks but an important one in healthcare is that they are used to describe paths between classifications and terminologies (Palkie 2016, 164-165). The patient was admitted for breast carcinoma in the right breast at two o'clock. This was removed via lumpectomy. The patient was found to have 1 of 7 lymph nodes positive for carcinoma during axillary lymph node dissection. One of the patient's neighbors who is also a coworker at the hospital called the coding department to get the patient's diagnosis because she is a cancer survivor herself. The coder should: a. Discuss the case with the coworker b. Report the incident to hospital security c. Give the caller false informationd. Explain that discussing the case would violate the patient's right to privacy -✔✔ d. Explain that discussing the case would violate the patient's right to privacy ** Disclosing information without the patient's written consent violates the patient's right to privacy (Brodnik 2012, 231, 414; Gordon and Gordon 2016a, 615-616). The requirements for documentation and record completion (documents such as history and physicals, discharge summaries, and consultations) as well as penalties for non-adherence must be specified in: a. Hospital rules and regulations b. Conditions of nonparticipation c. Medical staff bylaws d. Nursing staff policies -✔✔ c. Medical staff bylaws **The medical staff bylaws are required by accreditation and regulatory organizations to refer to the timeline required for completion (Malmgren and Solberg 2016, 240; Brinda 2016, 166). A bronchoscopy with biopsy of the left bronchus was completed and revealed adenocarcinoma. What, if any, modifier should be added to the procedure codes? a. -50, Bilateral procedure b. -51, Multiple procedures c. -LT, Left side d. No modifiers should be reported. -✔✔ d. No modifiers should be reported. Because the lungs are paired organs, it may seem as though modifier -50 would be appropriate. However, a modifier would not be assigned because the bronchus is not a paired organ, and the bronchus is the location of the procedure, not the lungs. Similarly, it might seem as though modifier -LT would be assigned, but again, this would not be assigned as the bronchus is not a paired organ. In order to assign the correct modifier, it is important to note that paired organs include ears, eyes, nostrils, kidneys, lungs, ovaries, and such (CPT Assistant May 2003).Using the following evaluation and management map, which answers represent documentation that should be considered, when assigning an E/M example for hospital acuity points assignment? Evaluation and Management Mapping The following are the points needed to determine the level of CPT code [Show More]
Last updated: 3 years ago
Preview 1 out of 45 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Can't find what you want? Try our AI powered Search
Connected school, study & course
About the document
Uploaded On
Sep 04, 2022
Number of pages
45
Written in
All

This document has been written for:
Uploaded
Sep 04, 2022
Downloads
0
Views
142
Scholarfriends.com Online Platform by Browsegrades Inc. 651N South Broad St, Middletown DE. United States.
We're available through e-mail, Twitter, Facebook, and live chat.
FAQ
Questions? Leave a message!
Copyright © Scholarfriends · High quality services·