Chapter 8
An Introduction to Pharmacogenomics
Optimal drug treatment requires selection of the best possible agents with close
monitoring of pharmacokinetics, pharmacodynamics, adverse drug reactions, and the cost
...
Chapter 8
An Introduction to Pharmacogenomics
Optimal drug treatment requires selection of the best possible agents with close
monitoring of pharmacokinetics, pharmacodynamics, adverse drug reactions, and the cost
of different agents.
Pharmacogenomics is the branch of science concerned with the identification of the
genetic attributes of an individual that lead to variable responses to drugs. Interestingly,
the science has evolved to also consider patterns of inherited alterations in defined
populations, such as specific ethnicities, that account for variability in
pharmacotherapeutic responses.
Until recently, the ultimate goal of pharmacogenomics had been the development of
prediction models to forecast debilitating adverse events in specific individuals and, more
recently, across populations based on similarities in age, gender, or more commonly, race
or ethnicity, as contrasted with the rest of the population. However, in spite of this newer
usage, pharmacogenomics may predict the extreme deviation of some patients from
predictable pharmacokinetic and pharmacodynamic responses: the idiosyncratic response.
Pharmacogenomics seeks to identify patterns of genetic variation that are subsequently
employed to guide the design of optimal medication regimens for individual patients.
With empiric therapy, interindividual (allot pic) variation in drug response occurs—with
patient outcomes varying from a complete absence of therapeutic response to potentially
life-threatening adverse drug reactions (ADRs).
Genetic differences may account in part for some of the well-documented variability in
response to drug therapy. Obviously, many factors other than genetics—such as age, sex,
other drugs administered, and underlying disease states—also contribute to variation in
drug response. However, inherited differences in the metabolism and disposition of drugs
and genetic polymorphisms in the targets of drug therapy (e.g., metabolizing enzymes or
protein receptors) can have an even greater influence on the efficacy and toxicity of
medications. Interestingly, age, gender, and endemic geographical differences may
themselves emerge as phenotypic consequences of differential epigenetic control. This
implies that heterogeneity in the control of gene expression based upon age, gender, and
geographic location is itself a life-long changing process that is under the control of
molecular “epigenetic” switches that either activate or inhibit groups of genes as a unit.
Genetics Revisited
An individual’s genetic makeup (or genotype) is derived as a result of genetic
recombination or “mixing” of genes from that individual’s parents. All the DNA
contained in any individual cell is known as the genome of the individual, a word formed
by the combination of “gene” and “chromosome,” and thus represents all the genes that
individual can express.
The Human Genome Project has sought not only to identify and correlate SNPs with
phenotypic differences but also to record and map haplotypes as well.o The completion of the Human Genome Project, as well as the mapping of SNPs
and haplotypes, has allowed the field of pharmacogenomics to understand the
variability of drug metabolism seen across individuals and populations.
Standard adopted nomenclature is used in pharmacogenomics and pharmacogenetics. Of
the various mutant variants of a specific gene, each variant is numerically and
sequentially named starting with the “wild-type” or normal or nonmutated copy of the
gene.
o Thus, for instance, CYP2D6 written in italics refers to the normal copy of the
gene, whereas CYP2D6*1 (pronounced “star 1”) refers to the first identified
natural variant (mutant) copy of this gene.
History of Pharmacogenetics
Since 1962, the term has been used to refer to the effects of genetic differences on a
person’s response to drugs.
The rate of acetylation of a drug such as isoniazid is clinically relevant because it
determines the rate of elimination of the drug from the body. Thus, individuals known as
slow acetylates will metabolize the drug slowly, allowing greater residence time in the
body and enhanced toxicity. It is a pharmacogenomic variation, which is responsible for
slow or fast acetylates as explained below.
Pharmacogenomics
The ultimate promise of pharmacogenomics is the possibility that knowledge of the
patient’s DNA sequence might be used to enhance drug therapy to maximize efficacy, to
target drugs only to those patients who are likely to respond, and to avoid ADRs.
The long-term expected benefits of pharmacogenomics are selective and potent drugs,
more accurate methods of determining appropriate drug dosages, advanced screening for
disease, and a decrease in the overall cost to the health-care system in the United States
caused by ineffective drug therapy.
Genetic Differences in Drug Metabolism
First realized by the observation that sometimes very low or very high concentrations of
drug were found in some patients despite their having been given the same amount of
drug.
Genetic Polymorphism
o Occurs when a difference in the allele(s) responsible for the variation is a
common occurrence.
o Under such circumstances, mutant genes will exist somewhat frequently alongside
wild-type genes. The mutant genes will encode for the production of mutant
proteins in these populations. The mutant proteins will, in turn, interact with drugs
in different manners, sometimes slight, sometimes significant. Monogenic traits
by themselves cannot explain the complexity of drug metabolism.o Four different phenotypes categorize the effects that genetic polymorphisms have
on individuals: poor metabolizers (PMs) lack a working enzyme; intermediate
metabolizers (IMs) are heterogeneous for one working, wild-type allele and one
mutant allele (or two reduced-function alleles); extensive metabolizers (EMs)
have two normally functioning alleles; and ultrarapid metabolizers (UMs) have
more than one functioning copy of a certain enzyme.
Phase I and Phase II Metabolism
o Drug metabolism generally involves the conversion of lipophilic substances and
metabolites into more easily excretable water-soluble forms. Drug metabolism
takes place mostly in the liver and is divided into two major categories, phase I
(oxidation, reduction, and hydrolysis reactions) and phase II metabolism
(conjugation reactions).
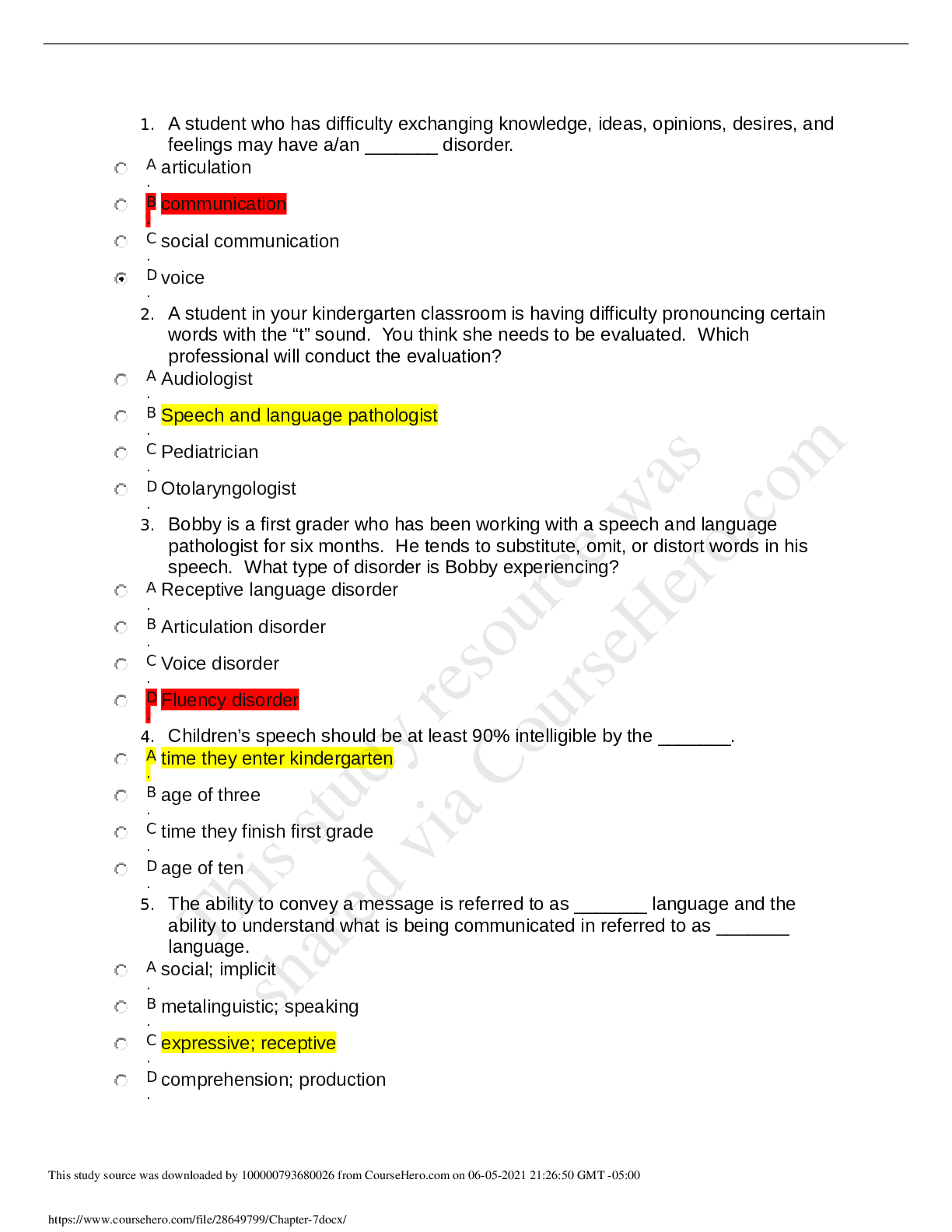
Metabolizer Phenotype Effect on Drug Metabolism Clinical Implications
Poor to intermediate
metabolizers
Slow Prodrug will be metabolized
slowly into active drug
metabolite. May have
accumulation of prodrug.
Active drug will be
metabolized slowly into
inactive metabolite. Potential
for accumulation of active
drug. Patient requires lower
dosage of medication.
Ultra rapid metabolizers Fast Prodrug rapidly metabolized
into active drug. No dosage
adjustment needed.
Active drug rapidly
metabolized into inactive
metabolites leading to
potential therapeutic failure.
Patient requires higher dosage
of active drug.
o Phase I metabolism enzymes are responsible for approximately 59% of the
adverse drug reactions.
o CYPs are generally located in the endoplasmic reticulum (ER) and the
mitochondria in human cells, of which the ER isoforms are of particular
importance to the field of drug metabolism. In terms of their organ distribution,
they are found in greater amounts in the liver and the intestine and to a somewhat
lesser extent in other organs, such as the skin, brain, lungs, and kidneys.o Hepatic, renal, and intestinal ER CYPs are involved in the biotransformation of a
plethora of drugs and endogenous substrates in humans mainly by oxygenation of
the target substrate molecule and mediated by differential oxidation states of the
central iron atom in the enzyme. Due to this oxygenation reaction, CYPs are
classified as monooxygenases.
Specific CYP450 Enzymes
o CYP2D6
Up to 25% of drugs are metabolized by this.
Exhibits polymorphism.
Acts on many xenobiotics, such as SSRI fluoxetine, TCAs, beta blockers,
CCB (diltiazem), theophylline, and tamoxifen.
Table 8-3
Research has shown that while approximately 10% of Caucasians, up to
7% of African Americans, and 4.8% of Asians have the “poor
metabolizer” (PM) phenotype, 5% of Caucasians and 4.9% of African
Americans have the “ultra rapid metabolizer” (UM) phenotype.
Table 8-2
o CYP2D6 and Tamoxifen
The role is not so much the metabolism of this drug as it is to activate it by
conversion to endoxifen inside the cell.
o CYP2D6 and Opioid Analgesics (Codeine)
Codeine relies on CYP2D6 enzymes to convert them to their active form,
morphine.
UM types may not experience the analgesic effects of the drug at normal
therapeutic doses, and PMs may not be able to convert codeine to its
active metabolite morphine, thus experiencing little or no clinical benefit.
o Genetic Testing for CYP2D6 Polymorphisms
CYP2C9
The primary route of metabolism for about a hundred different
drugs in humans.
While some CYP2C9 substrates are the more common drugs, such
as phenytoin, glipizide, and losartan, other drug substrates include
those that evince a narrow therapeutic index, such as the coumarinrelated anticoagulant agents warfarin and acenocoumarol.
CYP2D9 and Warfarin
o Warfarin is one of the most effective, cheapest, and widely
prescribed anticoagulant drugs that act by inhibiting the
enzyme vitamin K epoxide reductase, which prevents the
formation of functional vitamin K.
o This action in turn inhibits the activation of clotting factors
in the liver, causing the anticoagulant effect.
o Clinically, warfarin maintenance dosing requirements are
lower in patients with CYP2C9*2 polymorphisms andfurther reduced in patients with CYP2C9*3 variants
(Gulseth, Grice, & Dager, 2009), making these two the
most common “reduced function variants” for the CYP
gene in terms of its effect on warfarin.
o In addition, patients with homozygous presentation of a
CYP2C9 mutation appear to have a greater reduction in
dosing requirement than do heterozygotes. Approximately
one-third of the population carries at least one allele for the
slow-metabolizing form of CYP2C9
Interestingly, the nonsteroidal anti-inflammatory drugs (NSAIDs)
celecoxib and flubiprofen have received “use with caution” in PM
label warnings from the FDA owing to CYP2C9 polymorphism.
CYP3A4
Responsible for up to 50% of drug metabolism.
Examples of these classes include azole antifungals, CCBs,
antihistamines, anticonvulsants, antimicrobials, and
corticosteroids.
Predicting the onset and offset of these effects is very difficult.
The time to onset and offset of drug-drug interactions is closely
related to each drug’s half-life and the half-life of enzyme
production.
Clinically significant drug interactions in this setting may increase
the risk of toxicity.
Table 8-5
Close monitoring is required when prescribing drugs that induce or
inhibit CYP3A4 enzymes.
P-Glycoprotein
A membrane-bound, ATP-dependent transport system responsible for the efflux of a
variety of xenobiotics from cells to the extracellular fluid.
This includes the ejection of drugs from cells, usually against their concentration
gradients. Pgp, also known as multidrug resistance (MDR1) protein, is the product of the
ABCB1 and ABCB4 genes and is a member of adenosine triphosphate (ATP)-binding
family of proteins.
Differential expression of Pgp may explain tissue-specific and temporal variations in
efflux efficiency in different cells.
The more Pgp protein expressed by the cell, the greater the efflux potential of xenobiotics
such as anticancer drugs.
Over 50 SNPs within the ABCB1 gene have been identified, which may lead to variability
in drug responses.
Pharmaceutically relevant examples of this include the variation in drug response to
agents such as antiepileptic drugs, select cardiovascular agents, and so on. Interestingly, P-glycoprotein at the site of the gastrointestinal (GI) tract effluxes
hydrophilic drugs out of the cell and inhibits drug absorption through the GI tract (Howe,
2009). As drugs passively diffuse through the GI tract, Pgp pumps move drugs from
cytoplasmic areas to extracellular fluid. Some examples of substrates of P-glycoprotein
include carvedilol, diltiazem, and digoxin (Howe, 2009).
Several antiepileptic drugs such as phenytoin, carbamezapine, lamotrizine, phenobarbital,
valproic acid, and gabapentin are substrates or inhibitors of Pgp, but there is considerable
controversy in the literature regarding these.
In the case of digoxin, Pgp affects the level of digoxin available for absorption and
elimination (Howe, 2009). P-glycoprotein inhibitors include verapamil, quinidine,
cyclosporine, and ketoconazole (Howe, 2009). If an inhibitor of P-glycoprotein is
administered, then blood levels of substrates will rise, as seen if quinidine is administered
with digoxin.
Drugs can be categorized as reversible or suicidal inhibitors or P-glycoproteins.
Clinical Implications of Pharmacogenomics
Adverse Drug Reactions
o 56% of drugs cited in ADR studies are metabolized by polymorphic phase I
enzymes, of which 86% are P450s.
Warfarin
o Although genetic testing prior to prescribing has not yet been required by the
FDA, numerous warfarin dosing calculators exist on the Web where a clinician
can insert clinical information about the patient, including genetic test results and
indications, and a dosing regimen will be calculated or “individualized” for that
patient.
Pharmacogenetic Testing Prior to Prescribing
o Within the anticoagulant drug class, warfarin is a drug with a narrow therapeutic
index.
o Patients with CYP2C9 variations require more time to achieve the International
Normalized Ratio, or INR, and are at an increased risk for bleeding; they may also
require lower doses of warfarin to achieve and maintain therapeutic INR.
o Thus, if there are indications of inherited differences in these genes, the patient
should be genotyped.
o However, monitoring INR is still as much of a requirement while dosing warfarin
as before.
o Generally, cell samples are collected from the mouth or from blood.
o The pharmacogenetic tests mentioned on drug labels can be classified as “test
required,” “test recommended,” and “information only.” Currently, four drugs are
required to have pharmacogenetic testing performed before they are prescribed:
cetuximab, trastuzumab, maraviroc, and dasatinib.
o In December 2007, the FDA added a Black-Box Warning on the carbamazepine
label, recommending testing for the HLA-B*1502 allele in patients with Asian
ancestry before initiating carbamazepine therapy because these patients are athigh risk of developing carbamazepine-induced Stevens–Johnson syndrome (SJS)
or toxic epidermal necrolysis (TEN).
o Table 8-7
[Show More]