Roles and responsibilities of APRN prescribers
• The responsibility for the final decision on which drug to use and how to use it is in the hands of the APRN prescriber.
• The degree of autonomy in this role and the b
...
Roles and responsibilities of APRN prescribers
• The responsibility for the final decision on which drug to use and how to use it is in the hands of the APRN prescriber.
• The degree of autonomy in this role and the breadth of drugs that can be prescribed vary from state to state based on the nurse practice act of that state.
• All states have title protection for NPs.
• Only Oregon has mandated third-party reimbursement parity for NP services.
• In all but five states, the control of practice and licensure is within the sole authority of the state's board of nursing. These five states have joint control in the board of nursing and the board of medicine.
• Scope of practice is determined by the individual NP's license under the nurse practice act of the licensing jurisdiction. Some have a graduated scope based on experience level. New prescribers need to understand that their employment sites may restrict this legal scope of practice but cannot extend it.
• In 17 states and the District of Columbia, NPs have independent scope of practice and prescriptive authority without a requirement or attestation for physician collaboration, consultation, delegation, or supervision.
• Six states have full autonomous practice and prescriptive authority following a period of postlicensure/postcertification supervision or collaboration.
Clinical judgement in prescribing
• Prescribing a drug results from clinical judgment based on a thorough assessment of the patient and the patient's environment, the determination of medical and nursing diagnoses, a review of potential alternative therapies, and specific knowledge about the drug chosen and the disease process it is designed to treat. In general, the best therapy is the least invasive, least expensive, and least likely to cause adverse reactions. Frequently, the best choice is to have lifestyle, nonpharmacological, and pharmacological therapies working together. When the choice of treatment options is a drug, several questions arise.
• As APRNs prescribe a drug for a given pathophysiology, their nursing background leads them to place equal emphasis on understanding the impact the drug will have on the patient.
• Patient education is a central focus of nursing and APRN practice.
• Knowledge and clinical experience shared from the mingling of medical and nursing perspectives are mutually beneficial to the providers and the patient.
• The APRN can benefit from the in-depth knowledge about the drugs in the physician's specialty area. The physician can benefit from APRNs’ focus on the impact of the drug on the patient and from their patient education skills. In the age of health-care reform, increasing emphasis is being placed on these latter issues.
Collaboration with other providers
• NPs and physicians do work together very effectively on an individual basis and in collegial care teams. In an era of health-care reform, our joint concerns about patient care decisions require us to be allies.
• Physicians may offer insight or advice on pharmacological management from their experience.
• A physician's expertise related to pharmacology is based on understanding biochemistry and prescribing for a given pathophysiology. The emphasis is on the disease and the drug, with less emphasis on the impact on the patient. Patient education by physicians may be limited or left to a nurse or pharmacist.
• Collaboration with other NPs and APRNs who have prescriptive privileges has two major advantages.
o On a one-to-one basis dealing with individual patient issues, NPs and APRNs can share “clinical pearls” from their knowledge base and collaborate to improve the care of the patient.
o Collaboration on issues related to scope of practice and prescriptive privilege at the state and national level is critical to obtaining and maintaining the autonomy of practice needed to provide optimal patient care.
• Collaboration with pharmacists requires an understanding of the educational preparation for and evolution of the role of the pharmacist. The profession of pharmacy requires graduate-level preparation for all pharmacists with the granting of a practice doctorate, the Doctor of Pharmacy (PharmD). PharmDs have extensive knowledge about pathophysiology and take an active role in determining the best drug to prescribe. A PharmD can assist by offering expertise on the clinical management of patients, including available dosage forms, potential adverse reactions, and drug interactions.
• Both physicians and APRNs increasingly consult PharmDs for their knowledge of pharmacokinetics and pharmcotherapeutics when prescribing for complex patients.
Autonomy and prescriptive authority
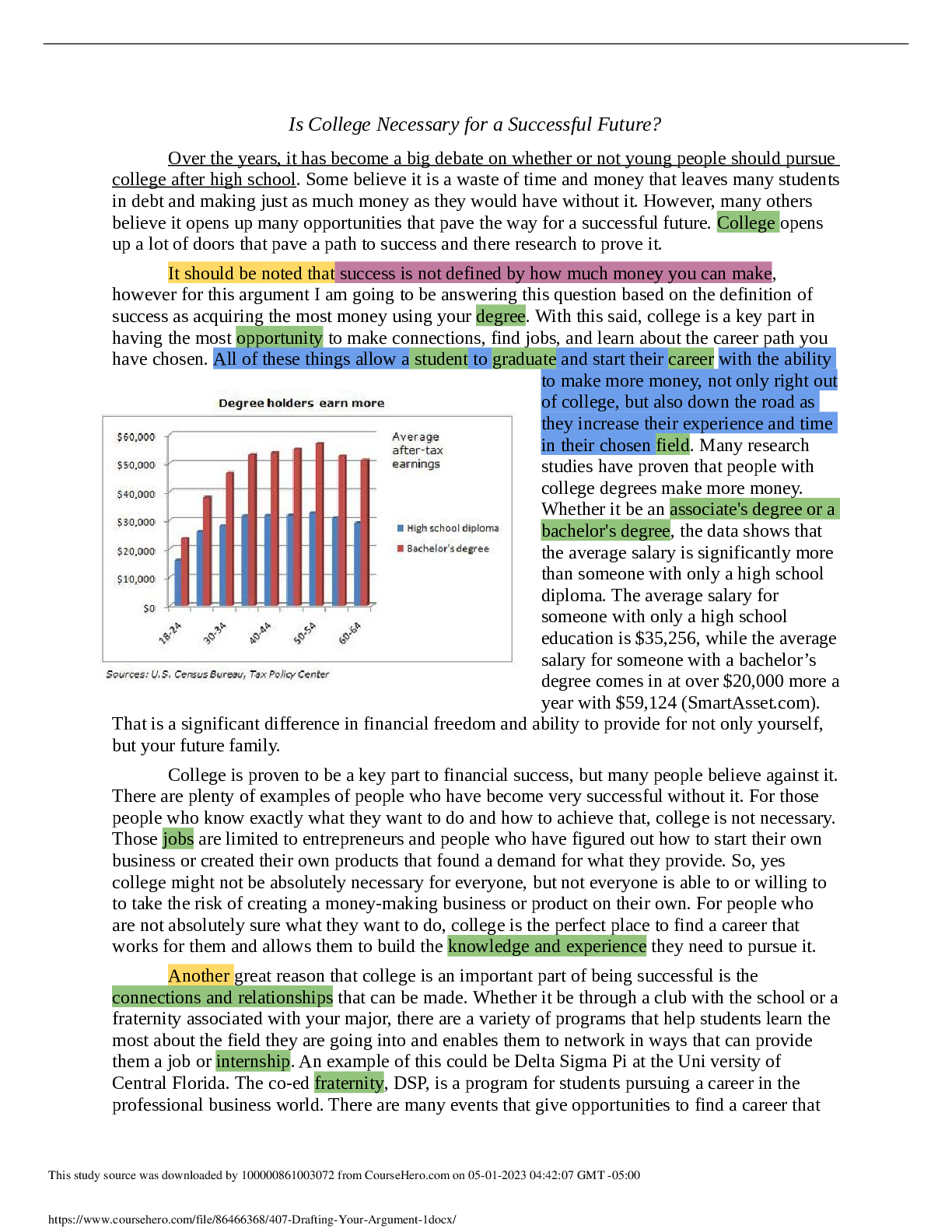
• By January 2004, all states had recognized the NP title, scope of practice, and prescriptive authority in legislation. Momentum to full autonomy is gaining, with 26 states allowing independent practice for NPs and 21 states allowing independent full prescribing as of January 2015 (National Council of State Boards of Nursing [NCSBN], 2015). APRNs in other states have also gained recognition, although the scope of practice and prescriptive authority is often more restricted.
• These gains are not written in stone, however, and can be reversed. Despite continuing research studies (Newland, 2009; Pearson, 2009; Gielen, 2013) that demonstrate the effectiveness of the role of the APRN in improving patient outcomes, barriers remain. Major concerns related to prescriptive authority must continue to be addressed. Not all states have legislation that permits APRNs to prescribe independently of any required physician involvement. Turf battles continue between APRNs and physicians at national and many state levels over physician supervision requirements and co-signatures on prescriptions. The advent of the doctorate of nursing practice (DNP) degree with its comparable level of education to that of other health-care providers and a focus on independent practice may address some of these issues about supervision. However, the American Medical Association continues to stress the need for physician supervision and final authority for the patient, even for APRNs who hold the DNP (Partin, 2008; AMA, 2010, 2013). This push for physician control occurs despite data from malpractice and malfeasance ratios that clearly show that the rationale for physician supervision is unfounded (Pearson, 2009).
Drug databases
• Nurses evaluate sources of drug information and learn which ones to trust. For an APRN, the sources of drug information expand to include the wide array of professional literature that ranges from the well-reputed journals to literature from specialty and professional organizations, the multitude of computerized drug databases (e.g., Micromedix, Lexicomp, Epocrates), information from the U.S. Food and Drug Administration, and formula programs that can be accessed via a handheld device or computer.
• The APRN prescriber needs to evaluate how reliable the drug information is. How can reliability be determined? Is the information source written by someone who may benefit from presenting biased information? Is the information source current? Today's “wonder drug” may be removed from the market tomorrow. Is the information relevant to the specific patient for whom the drug will be prescribed? If the information is a research report, what type of research design was used? Are there questions about the validity and reliability of the data? Are national or international guidelines used to inform prescribing or does the reference suggest prescribing outside established guidelines? To prescribe drugs appropriately, APRNs must be able to answer these questions; to answer them, they must master sources of information and use them on a regular basis.
Medication adherence
• Multiple national retail pharmacies have developed $4.00 prescription formularies. Awareness of what is on the local discount formulary may save the patient hundreds of dollars in prescription costs and may increase compliance.
Chapter 4: Legal and Professional Issues in Prescribing
New drug approval process including clinical phases I-IV
The process of synthesis and extraction identifies new molecules with the potential to produce a desired change in a biological system
• Phase I clinical evaluation is the first testing of a new compound in subjects, for the purpose of establishing the tolerance of healthy human subjects at different doses; defining its pharmacological effects at anticipated therapeutic levels; and studying its absorption, distribution, metabolism, and excretion patterns in humans.
• Phase II clinical evaluation is controlled studies performed on patients with the target disease or disorder to determine a compound's potential usefulness and short-term risks. A relatively small number of patients, usually no more than several hundred subjects, are enrolled in phase II studies.
• Phase III trials are controlled and uncontrolled clinical trials of a drug's safety and efficacy in hospital and outpatient settings. Phase III studies gather precise information on the drug's efficacy for specific indications, determine whether the drug produces a broader range of adverse effects than those exhibited in the small study populations of phases I and II studies, and identify the best way of administering and using the drug for the purpose intended. If the drug is approved, this information forms the basis for deciding the content of the product label. Phase III trials verify that the acceptable risk/benefit ratio seen in phase II persists under conditions of anticipated usage and in groups of patients large enough to identify statistically and clinically significant responses.
U.S. FDA regulatory jurisdiction: Official labelling vs off-label use of drugs
• The FDA's jurisdiction over the uses of marketed drugs and doses extends only to what the manufacturer may recommend and must disclose in its labeling.
• The FDA is not charged with dictating how a prescriber should practice.
• The FDA is concerned with the marketing and availability of drugs that have demonstrated substantial evidence of an acceptable risk/benefit ratio for labeled indications. The proper and efficacious therapeutic use of these drugs is the responsibility of the prescriber.
• Official labeling:
o a prescription drug, the manufacturer's directions or FDA-approved labeling (the package insert) is intended for the prescriber, pharmacist, or nurse and provides a summary of information about the chemical and physical nature of the product, pharmacological indications and contraindications, means of administration, dosages, side effects and adverse reactions, how the drug is supplied, and any other information pertinent to safe and effective use. This summary, or official labeling, is developed through discussion between the FDA and the drug manufacturer. The material in the Physician's Desk Reference (PDR) is a verbatim presentation of the official labeling.
• Off label use:
o The prescription of an FDA-approved drug for an off-label (unlabeled) indication may be initiated by patient need. Off-label use includes use of an FDA-approved drug in a dose or route for which it was not approved or for a clinical indication other than the FDA-approved use. Clinical support can be demonstrated for off-label use if the proposed use is based on rational scientific theory or controlled clinical studies. The FDA has made it clear that it neither has nor wants the authority to compel prescribes to adhere to FDA-approved use in all clinical situations. An example of off-label use is that of trazodone, which is an antidepressant, for sleep. In this example, a side effect of the medication (drowsiness) has been shown to have clinical efficacy for patients with difficulty sleeping whether or not they are clinically depressed. Although not FDA approved for insomnia, trazodone is commonly prescribed for this indication.
o Nurse practitioners (NPs) are responsible for knowing the FDA indication and approval status of any drug they prescribe. However, a prescribing decision on how to use a drug must be based on what is best for the patient and then supported by available evidence. In professional liability suits, FDA-approved drug labeling may have evidentiary weight, but drug labeling is not intended to set the sole standard for what is good clinical practice. NPs must also be aware that Medicare and other insurers rarely cover off-label prescriptions and that consequently the patient may bear greater cost. Off-label prescribing can also result in increased or unknown risk to the patient
Controlled substance laws
• Every person who manufactures, distributes, prescribes, procures, or dispenses any controlled substance must register and obtain a registration number with the U.S. Drug Enforcement Administration (DEA).
• Must maintain and keep on file for a minimum of 2 years accurate records of controlled drugs they purchase, distribute, administer, and dispense.
[Show More]