*NURSING > STUDY GUIDE > NU249/NUR2488- Assess Your Knowledge- Exam 1/NUR 2488 Mental Health 1 exam answers (All)
NU249/NUR2488- Assess Your Knowledge- Exam 1/NUR 2488 Mental Health 1 exam answers
Document Content and Description Below
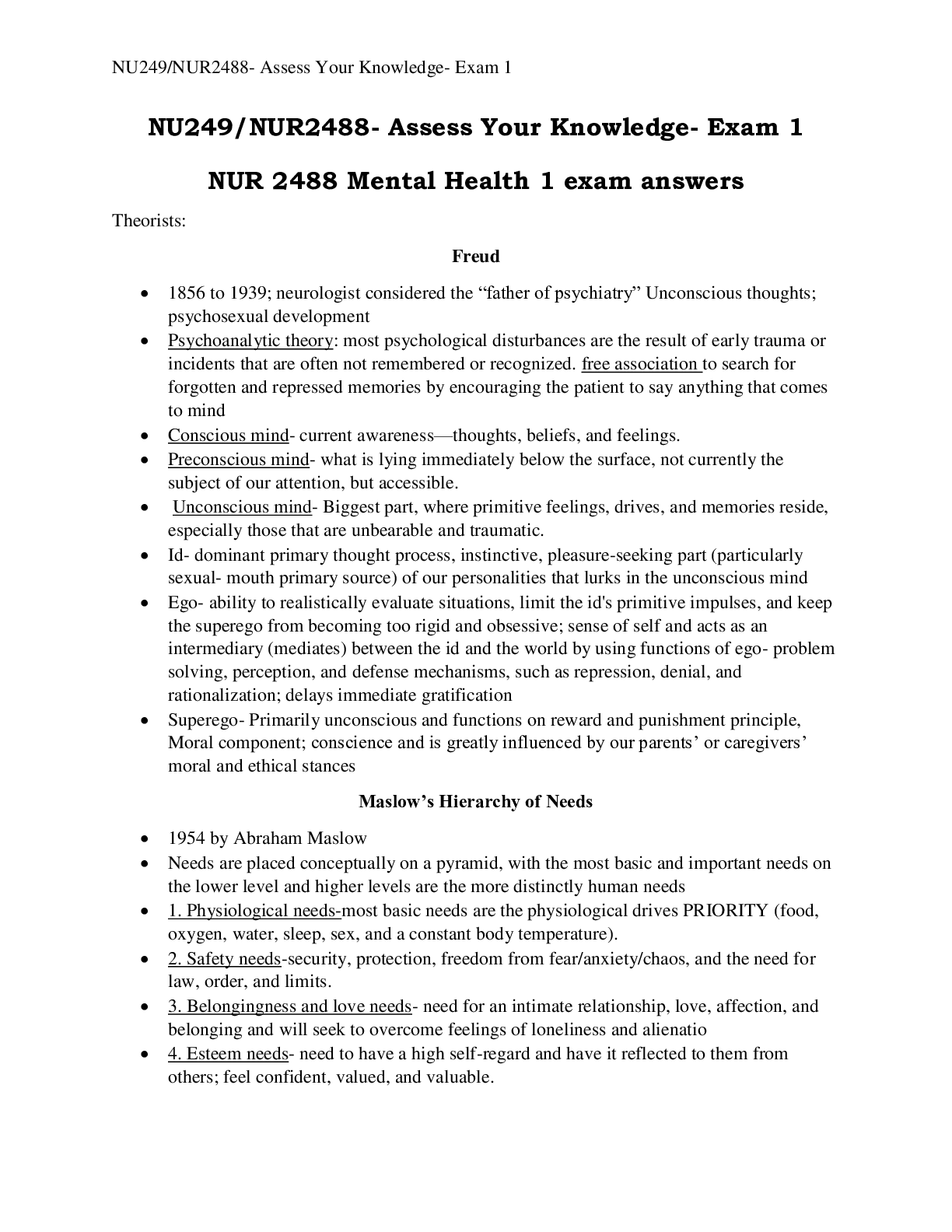
NU249/NUR2488- Assess Your Knowledge- Exam 1 NU249/NUR2488- Assess Your Knowledge- Exam 1 NUR 2488 Mental Health 1 exam answers Theorists: Freud 1856 to 1939; neurologist considered the “fa... ther of psychiatry” Unconscious thoughts; psychosexual development Psychoanalytic theory: most psychological disturbances are the result of early trauma or incidents that are often not remembered or recognized. free association to search for forgotten and repressed memories by encouraging the patient to say anything that comes to mind Conscious mind- current awareness—thoughts, beliefs, and feelings. Preconscious mind- what is lying immediately below the surface, not currently the subject of our attention, but accessible. Unconscious mind- Biggest part, where primitive feelings, drives, and memories reside, especially those that are unbearable and traumatic. Id- dominant primary thought process, instinctive, pleasure-seeking part (particularly sexual- mouth primary source) of our personalities that lurks in the unconscious mind Ego- ability to realistically evaluate situations, limit the id's primitive impulses, and keep the superego from becoming too rigid and obsessive; sense of self and acts as an intermediary (mediates) between the id and the world by using functions of ego- problem solving, perception, and defense mechanisms, such as repression, denial, and rationalization; delays immediate gratification Superego- Primarily unconscious and functions on reward and punishment principle, Moral component; conscience and is greatly influenced by our parents’ or caregivers’ moral and ethical stances Maslow’s Hierarchy of Needs 1954 by Abraham Maslow Needs are placed conceptually on a pyramid, with the most basic and important needs on the lower level and higher levels are the more distinctly human needs 1. Physiological needs-most basic needs are the physiological drives PRIORITY (food, oxygen, water, sleep, sex, and a constant body temperature). 2. Safety needs-security, protection, freedom from fear/anxiety/chaos, and the need for law, order, and limits. 3. Belongingness and love needs- need for an intimate relationship, love, affection, and belonging and will seek to overcome feelings of loneliness and alienatio 4. Esteem needs- need to have a high self-regard and have it reflected to them from others; feel confident, valued, and valuable.NU249/NUR2488- Assess Your Knowledge- Exam 1 5. Self-actualization- choose a path that will result in inner peace and fulfillment; We are preset to strive to be everything that we are capable of becoming; highly individual; drive is restlessness, a sense that something is missing. Erikson’s Stages of Development Infancy—birth to 1½ years; Trust vs. mistrust, Egocentric; Task- develop a basic sense of trust that leads to hope, requires a feeling of physical comfort and a minimal experience of fear or uncertainty Early childhood—1½ to 3 years; Autonomy vs. shame/doubt, Task- gain self-control of and independence within the environment Preschooler- 3-6 years, Initiative vs. Guilt, Task—achieve a sense of purpose and develop a sense of mastery over tasks School age—6 to 12 years; Industry vs. inferiority; Task- gain a sense of self-confidence and recognition through learning, competing, and performing successfully Adolescence—12 to 20 years; Identity vs. role confusion; Task- integrate all the tasks previously mastered into a secure sense of self Young adulthood—20 to 30 years; Intimacy and solidarity vs. isolation; Task- form intense long-term relationships and commit to another person, cause, institution, or creative effort Adulthood—30 to 65 years; Generativity vs. self-absorption; Task- achieve life goals and obtain concern and awareness of future generations Senescence—65 years to death; Integrity vs. despair; Task- derive meaning from one's whole life and obtain/maintain a sense of self-worth Understand the role of neurotransmitters as related to disorders Dopamine- controls emotional responses and the brain's reward and pleasure centers, stimulates the heart, and increases blood flow to vital organs. Decreased: Parkinson disease, depression; Increased: Schizophrenia, mania Serotonin- helps regulate mood, arousal, attention, behavior, and body temperature; Decreased: Depression; Increased: Anxiety states Norepinephrine- noradrenergic, major role in regulating mood; Decreased: Depression; Increased: Anxiety states GABA- modulates neuronal excitability and is associated with the regulation of anxiety; Decrease: Anxiety disorders, schizophrenia, mania; Increase: Reduction of anxiety, schizophrenia, mania Nurse-Client RelationshipNU249/NUR2488- Assess Your Knowledge- Exam 1 Orientation- first time the nurse and the patient meet; create environment of trust, gather data, patient may begin to express thoughts and feelings, identify problems, and discuss realistic goals. Working- introduction; allow the patient to experience increased levels of anxiety and demonstrate dysfunctional behaviors in a safe setting while trying out new and more adaptive coping behaviors; maintain trust, promote insight, identify strengths; work toward goal Termination phase- date of the termination phase should be clear from the beginning; therapeutic conclusion; progress toward clothes; feeling explored Difference between a Nurse-client- patient centered; Nurse maximizes communication skills, understanding of human behaviors, and personal strengths to enhance patient’s growth; Patient needs are addressed; Language is straightforward; Focus is on the patient’s idea) and a Social relationship- Includes friendship and socialization; Mutual needs are met; May include giving advice; Basic needs are met; Content is superficial; Roles may shift; little evaluation of interaction occurs. Boundaries with clients- Self disclosure- only if therapeutic to client; Gift giving- never financial, only if gift is shared among ALL staff; Touch- caring touch only if no physical need is present and if provides therapeutic comfort; Friendship/romantic associationNever appropriate; No favoring, secrets, special attention or time, personal info sharing, and thinking about client when not at work The role of the psych RN- •Completing comprehensive data collection that includes the patient, family, and other health care workers •Developing, implementing, and evaluating plans of care •Assisting or supervising mental health care workers •Maintaining a safe and therapeutic environment •Facilitating health promotion through teaching •Monitoring behavior, affect, and mood •Maintaining oversight of restraint and seclusion •Coordinating care by the treatment team Nursing Process Describe the nursing process when developing plan of care- Assessment- gather data; Diagnosis-identify problem, construct NANDA, and proritize; Outcome Identificationexpected outcome; Planning- intervention, EPB, and document; Implementationtherapies; Evaluation- Goal met? Developing a goal/outcome includes?- Safe- must be safe for the patient as well as for other patients, staff, and family; Appropriate- must be compatible with other therapies and with the patient's personal goals and cultural values, as well as with institutional rules; Individualized- should be realistic (1) within the patient's capabilities given the patient's age, physical strength, condition, and willingness to change; (2) based on the number of staff available; (3) reflective of the actual available community resources; and (4) within the student's or nurse's capabilities; Evidence based- They should be based on scientific principles when available.NU249/NUR2488- Assess Your Knowledge- Exam 1 Understanding the difference between mental health- state of well-being in which every individual realizes his or her own potential, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to her or his community, without illness; Mental health is fundamental to health. ; and mental illness- wide range of mental health condition- disorders that affect your mood, thinking and behavior; Mental disorders are real health conditions that have an immense impact on individuals and families. The Interview Sections of the psychiatric assessment- 1. Establish rapport 2. Obtain an understanding of the current problem or chief complaint 3. Review physical status and obtain baseline vital signs 4. Assess for risk factors affecting the safety of the patient or others 5. Perform a mental status examination (MSE) 6. Assess psychosocial status 7. Identify mutual goals for treatment 8. Formulate a plan of care Sections of the MSE 10- observes the patient's physical behavior, nonverbal communication, appearance, speech patterns, mood and affect, thought content, perceptions, cognitive ability, and insight and judgment Attention- performance on serial sevens, digit span tests Abstraction: performance on tests involving similarities, proverbs Insight- recognition that one has a mental illness, compliance with treatment, and the ability to re-label unusual mental events Judgement- patient's capacity to make sound, reasoned and responsible decisions What considerations should be evaluated during an interview?- H Home environment (e.g., relations with parents and siblings); E Education and employment (e.g., school performance); A Activities (e.g., sports participation, afterschool activities, peer relations); D Drug, alcohol, or tobacco use; S Sexuality (e.g., whether the patient is sexually active, practices safe sex, uses contraception, or practices alternative sexual lifestyles); S Suicide risk or symptoms of depression or other mental disorder; S “Savagery” (e.g., violence or abuse in home environment or in neighborhood) Communication Empathetic vs. sympathetic responses: sympathy is feeling compassion, sorrow, or pity for the hardships that another person encounters, while empathy is putting yourself in the shoes of another. Therapeutic Communication Techniques- 1. Silence—allows the client to take control of the discussion, if he or she so desires. 2. Accepting—conveys positive regard 3. Giving recognition—acknowledging; indicating awareness 4. Offering self—making oneself available 5. Giving broad openings—allows client to select the topicNU249/NUR2488- Assess Your Knowledge- Exam 1 6. Offering general leads—encourages client to continue 7. Placing the event in time or sequence—clarifying the relationship of events in time 8. Making observations—verbalizing what is observed or perceived 9. Encouraging description of perceptions—asking the client to verbalize what is being perceived 10. Encouraging comparison—asking the client to compare similarities and differences in ideas, experiences, or interpersonal relationships 11. Restating—lets the client know whether an expressed statement has been understood or not 12. Reflecting—questions or feelings are referred back to the client so that they may be recognized and accepted 13. Focusing—taking notice of a single idea or even a single word 14. Exploring—delving further into a subject, idea, experience, or relationship 15. Seeking clarification and validation—striving to explain that which is vague and searching for mutual understanding 16. Presenting reality—clarifying misperceptions that the client may be expressing 17. Voicing doubt—expressing uncertainty as to the reality of the client’s perceptions 18. Verbalizing the implied—putting into words what the client has only implied 19. Attempting to translate words into feelings—putting into words the feelings that client has expressed only indirectly 20. Formulating a plan of action—strives to prevent anger or anxiety from escalating to an unmanageable level the next time the stressor occurs Non-Therapeutic Communication Techniques- 1. Giving reassurance—may discourage the client from further expression of feelings if he or she believes they will only be belittled 2. Rejecting—refusing to consider the client’s ideas or behavior 3. Giving approval or disapproval—implies that the nurse has the right to pass judgment on the “goodness” or “badness” of the client’s behavior 4. Agreeing or disagreeing—implies that the nurse has the right to pass judgment or whether the client’s ideas or opinions are “right” or “wrong” 5. Giving advice—implies that the nurse knows what is best for the client, and that the client is incapable of any self-direction 6. Probing—pushing for answers to issues the client does not wish to discuss, causing the client to feel used and valued only for what is shared with the nurse 7. Defending (what the client has criticized)—implies that he or she has no right to express ideas, opinions, or feelings 8. Requesting an explanation—implies that the client must defend his or her behavior or feelings 9. Belittling feelings expressed—causes the client to feel insignificant or unimportant 10. Making stereotypical comments (clichés and trite expressions)—is meaningless in a nurse-client relationshipNU249/NUR2488- Assess Your Knowledge- Exam 1 11. Using denial—blocks discussion with the client and avoids helping the client identify and explore areas of difficulty 12. Interpreting—results in the therapist telling the client the meaning of his or her experience (which may or may not be correct) 13. Introducing an unrelated topic—causes the nurse to take over the direction of the discussion 14. Indicating the existence of an external source of power—encourages the client to project blame for his or her thoughts or behaviors on others Cultural Considerations An ethnic group or ethnicity is a population group whose members identify with each other on the basis of common nationality or shared cultural traditions. EX: they can be as broad as "Native American" or as narrow as "Cherokee" Culture is defined and understood in several ways. Culture may be seen as a group's acceptance of a set of attitudes, ideologies, values, beliefs, and behaviors that influence the way the members of the group express themselves; EX: language; spirituality; works of art; group customs and traditions; food preferences; response to illness, stress, pain Apply the impact of culture to patient care- expected that nurses from one culture should be able to give culturally competent care to individuals from any other culture; culturally competent when health-care providers and institutions are able to provide care for clients that meet the clients’ cultural needs. Ultimately, cultural competency leads to highquality care to every client regardless of language, race, or ethnic background. Ethics Define and give examples for (pg. 81): Beneficence: The duty to act so as to benefit or promote the good of others. Spending extra time to help calm an extremely anxious patient is a beneficent act. Autonomy: Respecting the rights of others to make their own decisions. Acknowledging the patient's right to refuse medication is an example of promoting autonomy. Justice: The duty to distribute resources or care equally, regardless of personal attributes. intensive care unit (ICU) nurse devotes equal attention both to a patient who has attempted suicide and to another patient who suffered a brain aneurysm. Fidelity (nonmaleficence): Maintaining loyalty and commitment to the patient and doing no wrong to the patient. Maintaining expertise in nursing skill through nursing education demonstrates fidelity to patient care. Veracity: One's duty to communicate truthfully. Describing the purpose and side effects of psychotropic medications in a truthful and nonmisleading way Negligence or malpractice is an act or an omission to act that breaches the duty of due care and results in or is responsible for a person's injuries. Person apprehensive (assault) of harmful or offensive touching (battery)NU249/NUR2488- Assess Your Knowledge- Exam 1 What rights do all patients have?- Right to Treatment; Right to Refuse Treatment; Right to Informed Consent; Right to Privacy; What rights are limited to involuntarily admitted clients?- Prepare an advance psychiatric directive document that will express their treatment choices. The advance directive for mental health decision making should be followed by health care providers when patients are not competent to make informed decisions for themselves. This document can clarify the patient's choice of a surrogate decision maker and instructions about hospital choices, medications, treatment options, and emergency interventions Duty to Warn-duty to warn a patient's potential victim of potential harm. How it is used in psychiatric nursing-Assessing and predicting the patient's danger of violence toward another; Identifying the specific individual(s) being threatened; Taking appropriate action to protect the identified victims HIPPA- Health Insurance Portability and Accountability Act (HIPAA), you may not, without the patient's consent, disclose information obtained from the patient or information in the medical record to anyone except those individuals for whom it is necessary for implementation of the patient's treatment plan. Describe when it is appropriate to use restraints/seclusion- When the particular behavior is physically harmful to the patient or a third party; When alternative or less restrictive measures are insufficient in protecting the patient or others from harm; When a decrease in sensory overstimulation (purpose of seclusion only) is needed; When the patient anticipates that a controlled environment would be helpful and requests seclusion Important keys to restraints- Written order of a physician; Confined to specific, time-limited periods (e.g., 2 to 4 hours); Patient’s condition is reviewed and documented regularly (e.g., every 15 minutes). Psychopharmacology: Identify the classes of medications used to treat psychiatric disorders Antidepressants: SSRIs- identify medications in class, common side effects, and teaching points Tricyclics- identify medications in class, common side effects, and teaching points MAOIs- identify medications in class, common side effects, and teaching points Recognize serotonin syndrome- S/S, nursing implications Anxiolytics: Benzodiazepines- identify medications in class, common side effects, and teaching pointsNU249/NUR2488- Assess Your Knowledge- Exam 1 Concerns for client taking benzo? Antipsychotics Typical- identify medications in class, common side effects, and teaching points Atypical- identify medications in class, common side effects, and teaching points Identify potentially fatal side effects- recognize S/S [Show More]
Last updated: 2 years ago
Preview 1 out of 8 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$6.50
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Jan 27, 2021
Number of pages
8
Written in
Additional information
This document has been written for:
Uploaded
Jan 27, 2021
Downloads
0
Views
86