*NURSING > EXAM > NR 601 Midterm Exam Study Guide Weeks 1- 4 Content- Download Paper To Score A High Grade ( A ) (All)
NR 601 Midterm Exam Study Guide Weeks 1- 4 Content- Download Paper To Score A High Grade ( A )
Document Content and Description Below
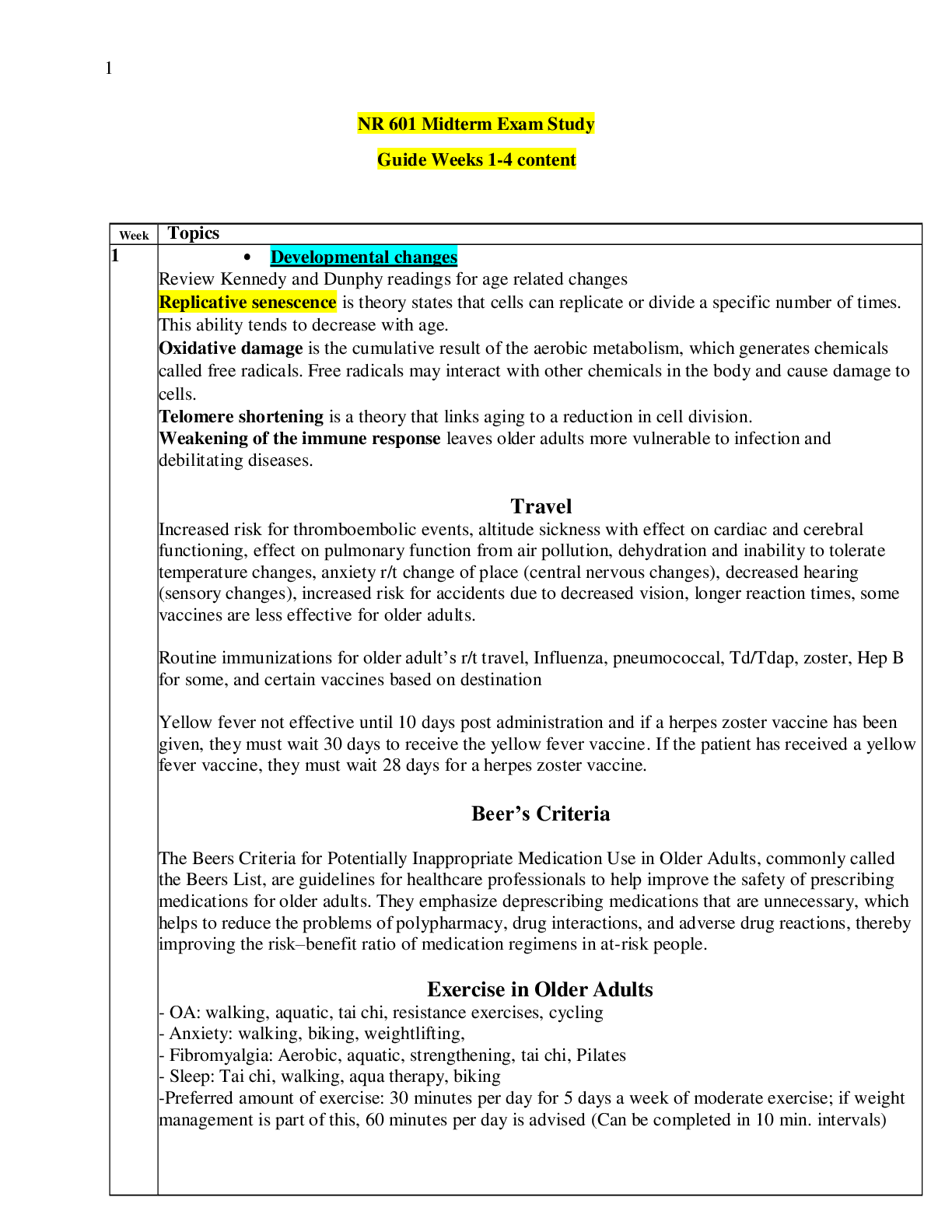
Week Topics 1 • Developmental changes Review Kennedy and Dunphy readings for age related changes Replicative senescence is theory states that cells can replicate or divide a specific number of ti... mes. This ability tends to decrease with age. Oxidative damage is the cumulative result of the aerobic metabolism, which generates chemicals called free radicals. Free radicals may interact with other chemicals in the body and cause damage to cells. Telomere shortening is a theory that links aging to a reduction in cell division. Weakening of the immune response leaves older adults more vulnerable to infection and debilitating diseases. Travel Increased risk for thromboembolic events, altitude sickness with effect on cardiac and cerebral functioning, effect on pulmonary function from air pollution, dehydration and inability to tolerate temperature changes, anxiety r/t change of place (central nervous changes), decreased hearing (sensory changes), increased risk for accidents due to decreased vision, longer reaction times, some vaccines are less effective for older adults. Routine immunizations for older adult’s r/t travel, Influenza, pneumococcal, Td/Tdap, zoster, Hep B for some, and certain vaccines based on destination Yellow fever not effective until 10 days post administration and if a herpes zoster vaccine has been given, they must wait 30 days to receive the yellow fever vaccine. If the patient has received a yellow fever vaccine, they must wait 28 days for a herpes zoster vaccine. Beer’s Criteria The Beers Criteria for Potentially Inappropriate Medication Use in Older Adults, commonly called the Beers List, are guidelines for healthcare professionals to help improve the safety of prescribing medications for older adults. They emphasize deprescribing medications that are unnecessary, which helps to reduce the problems of polypharmacy, drug interactions, and adverse drug reactions, thereby improving the risk–benefit ratio of medication regimens in at-risk people. Exercise in Older Adults - OA: walking, aquatic, tai chi, resistance exercises, cycling - Anxiety: walking, biking, weightlifting, - Fibromyalgia: Aerobic, aquatic, strengthening, tai chi, Pilates - Sleep: Tai chi, walking, aqua therapy, biking -Preferred amount of exercise: 30 minutes per day for 5 days a week of moderate exercise; if weight management is part of this, 60 minutes per day is advised (Can be completed in 10 min. intervals) Laboratory Changes in Older Adults • Protein rises slightly renal pathology, UTI, aging kidney changes • Specific gravity: lower maximum in elderly: 1.016-1.022-decline in nephrons ability to concentrate urine • ESR: increases-not sensitive/nor specific in the aging adult • Iron binding-decreases • Hgb: decreases-anemia is common in the elderly • HCT: slight decrease-decline in hematopoiesis • Leukocytes: drop-drugs/sepsis • Lymphocytes-T and B cell fall-risk for infection is higher-immunization encouraged • Platelets: no change in number • Albumin-decline-smaller liver-and enzymes-protein energy malnutrition • Globulin: slight increase • Total serum protein: decreases indicate malnutrition, infection and liver disease • BUN: increases and decline in GFR-decreased cardiac output • CR: increases-r/t lean body mass decrease • CR clearance: decreases-10% per 10 years after 40-careful prescribing drugs that are excreted by kidneys • Glucose tolerance: increase of 10 mg/dL/decade after 30-diabetes more prevalent-drugs can cause glucose intolerance • Alk phosp: increase-elevations> 2 Geriatric Syndromes • Sleep Disturbances • Problems with eating or feeding • Incontinence • Confusion • Evidence of falls • Skin breakdown Categories for Aging • Young – old = 65–74 years • Old = 75–84 • Oldest-old = 85 and older Comprehensive Geriatric Assessment Physical Health -Beers Criteria: avoid Polypharmacy & Potentially Inappropriate Medication the elderly/ADR -STOPP Screening Tool of Older Persons Prescriptions: medications that might likely need to be stopped for the older adult -START Screening Tool to Alert Doctors to Right Treatment: includes medications that need to be added. -MINI Nutritional Assessment Instrument: identifies older adults who have or at risk of malnutrition -Nutrition Health Checklist: identifies older adults who have or at risk of malnutrition Functional Health - KATZ : Activities of Daily Living Scale - Lawton and Brody Scale: Instrumentals activities of daily living - Hendrich II Fall Risk Model: assessment of falls, useful in acute care, ambulatory, assisted living, and long-term care. - Timed Get up and Go Test: mobility screen - Tinetti’s Performance Oriented Mobility Assessment is a task-oriented test that measures gait and balance abilities Physiological Health - DSM-5: describes the characteristics of delirium and mild to moderate neurocognitive mental disorders - MMSE Mini Mental Status Examination: - GDS: SF Geriatric Depression Scale -Short form: consists of 15 questions requiring yes or no response. Can be completed in any healthcare setting. -PHQ-9 Patient Health Questionnaire Socioenvironmental Supports -Lubben Social Network Scale -6 item version • Important contribution to family and friendship • Helps identify patients at risk for social isolation who can benefit from intervention • Include the following geriatric assessment to help improves patient’s social support ■ Is there any one special person you could call or contact if you need help? (If yes, identify.) ■ In general, other than your children, how many relatives do you feel close to and have contact with at least once a month? (Number.) ■ In general, how many friends do you feel close to and have contact with at least once a month? (Number.) Additional social and economic resources are assessed by exploring the following: MIDTERM STUDY GUIDE FOR NR 601-AGING ADULT 66 ■ Living situation ■ Housing ■ Transportation ■ Income ■ Assets ■ Degree of financial burden resulting from health concerns Quality of Life Measures: -Medical Outcomes Study-Short Form 36: • looks at physical, mental, and social domains ➢ GOLD standard for quality of life instruments because of its longevity, applicability, and ease of administration and analysis. • Lab results- Dunphy Table 77.2 Lab Test Normal Changes with age Comments UA Protein 0-5mg/100ml Rises slightly May be due to kidney changes with age, urinary tract infection, renal pathology Specific Gravity 1.005-1.020 Lower max in elderly 1.016-1.022 Decline in nephrons impairs ability to concentrate urine Hematology ESR Men: 0-20 Women: 0-30 Significant increase Neither sensitive nor specific in aged Iron Binding 50-160mcg/dl 230-410mcg/dl Slight decrease Decrease Hemoglobin Men: 13- 18g/100ml Women: 12-16g Men: 10-17g Women: None noted Anemia common in the elderly Hematocrit Men: 45-52% Women 37-48% Slight decreased speculated Decline in hematopoiesisLeu Leukocytes 4,300–10,800/mm3 Drop to 3,100– 9,000/mm3 Decrease may be due to drugs or sepsis and should not be attributed immediately to age Lymphocytes 00–2,400 T T-cell and B-cell Infection risk higher; cells/mm3 50–200 B cells/mm3 levels fall immunization encouraged Platelet 150,000–350,000/ No change in number Blood Chemistry Albumin 3.5–5.0 Decline Related to decrease in liver size and enzymes; protein-energy malnutrition common Globulin 2.3–3.5 Slight increase Total serum protein 6.0–8.4 g No change Decreases may indicate malnutrition, infection, liver disease Blood urea nitrogen Men: 10–25 Women: 8–20 mg Increases significantly up to 69 mg Increases significantly up to 69 mg Creatinine 0.6–1.5 mg Increases to 1.9 mg Related to lean body mass decrease Creatinine clearance 104–124 mL/min Decreases 10%/decade after age 40 years Used for prescribing medications for drugs excreted by kidney Glucose tolerance 62–110 mg/dL after fasting; >120 mg/dL after 2 hours postprandial Slight increase of 10 mg/dL/decade after 30 years of age Diabetes increasingly prevalent; drugs may cause glucose intolerance Alkaline phosphatase 13–39 IU/L Increase by 8–10 IU/L Elevations >20% usually due to disease; elevations may be found with bone abnormalities, drugs (e.g., narcotics), and eating a fatty meal • Atypical disease presentations Erroneously associating aging with disease, disuse, and disability, older adults perceive this change as inevitable and either fail to present to the health-care provider or, if they do, fail to challenge the assumption that this represents normal aging. At times an acute symptom such as pain or dyspnea is superimposed on a chronic symptom, and the older adult may not recognize that it represents a new or exacerbated pathology TABLE 1-1 Presentation of Illness in Older Adults ILLNESS ATYPICAL PRESENTATIONS Acute abdomen Absence of symptoms or vague symptoms Acute confusion Mild discomfort and constipation Some tachypnea and possibly vague respiratory symptoms Appendicitis pain may begin in right lower quadrant and become diffuse Depression Anorexia, vague abdominal complaints, new onset of constipation, insomnia, hype lack of sadness Hyperthyroidism Hyperthyroidism presenting as “apathetic thyrotoxicosis,” i.e., fatigue and weakne weight loss may result instead of weight gain; patients report palpitations, tachyca onset of atrial fibrillation, and heart failure may occur with undiagnosed hyperthyr Hypothyroidism Hypothyroidism often presents with confusion and agitation; new onset of anore weight loss, and arthralgias may occur Malignancy New or worsening back pain secondary to metastases from slow growing breast m Silent masses of the bowel Myocardial Absence of chest pain infarction (MI) Vague symptoms of fatigue, nausea, and a decrease in functional and cognitive sta classic presentations: dyspnea, epigastric discomfort, weakness, vomiting; history previous cardiac failure Higher prevalence in females versus males Non-Q-wave MI Overall infectious diseases process Absence of fever or low-grade fever Malaise Sepsis without usual leukocytosis and fever Falls, anorexia, new onset of confusio alteration in change in mental status, decrease in usual functional status Peptic ulcer disease Absence of abdominal pain, dyspepsia, early satiety Painless, bloodless New onset of confusion, unexplained tachycardia, and/or hypotension Pneumonia Absence of fever; mild coughing without copious sputum, especially in dehydrate patients; tachycardia and tachypnea; anorexia and malaise are common; alteration cognition. Pulmonary edema Lack of paroxysmal nocturnal dyspnea or coughing; insidious onset with changes function, food or fluid intake, or confusion Tuberculosis (TB) Atypical signs of TB in older adults include hepatosplenomegaly, abnormalities in function tests, and anemia Urinary tract infection Absence of fever, worsening mental or functional status, dizziness, anorexia, fatig weakness • Geriatric syndromes • Sleep Disturbances • Problems with eating or feeding • Incontinence • Confusion • Evidence of falls • Skin breakdown • Categories of aging- know age ranges for old, young old, old-old, etc. • Young – old = 65–74 years • Old = 75–84 • Oldest-old = 85 and older TABLE 1-2 Select Bimodal Presentations of Illness in Younger Adults versus Older Adults TYPE OF CONDITION YOUNGER ADULTS OLDER ADULTS Dermatological Psoriasis Late teens to 20s Irregular course which tends to generalize Hereditary factors 50s—males 60s—females Sporadic onset Gastrointestinal Inflammatory bowel disease Ulcerative colitis (UC) Crohn’s disease (CD) 20–40 years old Right lower UC Insidious onset >60–75 years old a secon occurs More often older women Proctitis Left-sided UC Higher rates of anemia May present as chronic di Fistula development Increased cases of associa malnutrition Extraintestinal manifestat including: arthritis spond uveitis, and erythema nod More comorbid condition May be confused with oth of colitis Malignancies Hodgkin’s lymphoma 20–30 years old Possible infectious etiology >50 years old Increased mortality Neurodegenerative Women 20–40 years old Men—50–70 years old Heated pool, gentle stretches, counsel about possible increased pain initially Chronic obstructive pulmonary disease Cycle ergometer, treadmill walking; individualize Supervised program—consider pulmonary rehabilitation program Chronic venous insufficiency Walking, standing exercises Supervised program Osteoporosis Weight-bearing exercises, weight training Assess balance and risk for falls before beginning Parkinson’s disease Walking, treadmill walking, stationary bike, dancing, tai chi, Pilates, boxing Assess balance and risk for falls before beginning; American Parkinson’s Disease Association resources Peripheral arterial disease Lower extremity exercises, treadmill walking, walking Very short intervals initially, progress as tolerated Age-related sleep disorders Tai chi, walking, aquatherapy, biking Assess balance and risk for falls before beginning Dementia Walking, recreational activities Provide safe environment, assess fall risk and ability to participate. ⟶ Testing prior to exercise initiation ⟶ Recommended testing prior to exercise initiation ⟶ Barriers, facilitators and contraindications to exercise Barriers ■ Lack of time ■ Perceived need for equipment ■ Perceived barrier to beginning exercise/physical activity ■ Disability or functional limitation ■ Unsafe neighborhood or weather conditions ■ No parks or walking trails ■ Depression ■ High body mass index (BMI) ■ Lack of motivation ■ Interpersonal loss or significant life event ■ Ignorance of what to do Patient Facilitators ■ Social support ■ Positive self-efficacy ■ Motivation to engage in physical activity ■ Good health, no functional limitations ■ Frequent contact with prescriber ■ Regular schedule, planned program ■ Satisfaction with program ■ Insurance incentive ■ Improvement in mobility or health condition ■ Staff Contraindications ■ Unstable angina ■ Uncompensated heart failure ■ Severe anemia ■ Uncontrolled blood glucose ■ Unstable aortic aneurysm ■ Uncontrolled hypertension or tachycardia ■ Severe dehydration or heat stroke ■ Low oxygen saturation ⟶ Health promotion (Dunphy and Kennedy) ⟶ Immunizations Shingrix is a new vaccine for zoster and is recommended over Zostavax. It is administered in two doses. The second dose can be given from 2 to 6 months after the initial one. Persons who have had Zostavax should now be immunized with Shingrix. Those who have had a prior episode of zoster should be vaccinated (CDC, Adult Immunization Schedule) ⟶ Travel (Kennedy) Risks related to travel: Patients with chronic disease that is well managed at home may decompensate in foreign environments because of heat, humidity, altitude, fatigue, changes in diet, and exposure to infectious diseases.Fever is not always a reliable indicator of illness in the older adult. Seroconversion rates decrease with age, rendering some vaccines less effective for older travelers. Immunizations for travel: all immunizations should be current. influenza, pneumococcal, Td/Tdap (tetanus, diphtheria, and acellular pertussis), zoster, and for some, hepatitis B vaccination. Yellow fever and herpes zoster vaccine are the only live virus vaccines that people over age 50 receive. Immune response can be impaired if live virus vaccines are given within a 28- to 30-day interval of each other. Yellow fever vaccine is not effective until 10 days after administration. If the NP gives a patient a herpes zoster vaccine, that patient cannot receive a yellow fever vaccine for 30 days. If the patient is required to have a yellow fever vaccine for travel, he or she cannot enter a yellow fever country until 10 days after receiving the yellow fever vaccine. If a patient receives a yellow fever vaccine, he or she cannot receive a herpes zoster vaccine for 28 days. The patient may receive both vaccines on the same day with no decrease in immune response The most common vaccines used for protecting travelers are hepatitis A, hepatitis B, typhoid fever, yellow fever, adult booster polio, Japanese encephalitis, meningococcal, and rabies. Comprehensive Geriatric Assessment Physical Health Screening Tools -Beers Criteria: avoid Polypharmacy & Potentially Inappropriate Medication the elderly/ADR -STOPP Screening Tool of Older Persons Prescriptions: medications that might likely need to be stopped for the older adult -START Screening Tool to Alert Doctors to Right Treatment: includes medications that need to be added. -MINI Nutritional Assessment Instrument: identifies older adults who have or at risk of malnutrition -Nutrition Health Checklist: identifies older adults who have or at risk of malnutrition Functional Health Screening Tools - KATZ : Activities of Daily Living Scale - Lawton and Brody Scale: Instrumentals activities of daily living - Hendrich II Fall Risk Model: assessment of falls, useful in acute care, ambulatory, assisted living, and long-term care. - Timed Get up and Go Test: mobility screen - Tinetti’s Performance Oriented Mobility Assessment is a task-oriented test that measures gait and balance abilities Physiological Health Screening Tools - DSM-5: describes the characteristics of delirium and mild to moderate neurocognitive mental disorders - MMSE Mini Mental Status Examination: - GDS: SF Geriatric Depression Scale -Short form: consists of 15 questions requiring yes or no response. Can be completed in any healthcare setting. -PHQ-9 Patient Health Questionnaire Socioenvironmental Supports Screening Tools -Lubben Social Network Scale -6 item version • Important contribution to family and friendship • Helps identify patients at risk for social isolation who can benefit from intervention • Include the following geriatric assessment to help improves patient’s social support ■ Is there any one special person you could call or contact if you need help? (If yes, identify.) ■ In general, other than your children, how many relatives do you feel close to and have contact with at least once a month? (Number.) ■ In general, how many friends do you feel close to and have contact with at least once a month? (Number.) Polypharmacy (Kennedy) Multiple definitions (review discussion) o Prescribing many drugs, prescribing 5 or more drugs, or prescribing potentially inappropriate medications. o The use of multiple pharmacies (providers & self-prescribers) o Providers should routinely evaluate medication appropriateness to avoid the risk of polypharmacy Prevention strategies o Have new patients bring in all medications to their first visit o Review med list at every visit o Ask if any other provider has changed or added any meds o Update med list at every visit Screening tools o Three available tools to evaluate patient’s prescriptions ▪ STOPP (screening tool of older persons’ potentially inappropriate prescriptions ▪ MAI (Medication Appropriateness Index) ▪ ARMOR (Assess, Review, Minimize, Optimize, Reassess) COPD (Dunphy and Kennedy) 2 Risk Factors: The most significant cant risk factor for COPD is cigarette smoking and occupational/industrial gases or fumes, and indoor/outdoor air pollution Cardinal symptoms: of COPD include dyspnea, chronic cough, and/or sputum production Physical examination: with advancing disease may reveal decreased breath sounds, hyperinflation (e.g., resonance to percussion), use of accessory muscles of respiration, wheezes, crackles in the lung bases, pursed lip breathing, and/or distant heart sounds Diagnostic Tests: Spirometry is the gold standard for measuring airflow limitation. Airflow limitation that is not fully reversible is evident if post-bronchodilator FEV 1 /FVC is less than 0.70 and FEV 1 is less than 80% predicted X-Ray: Abnormalities associated with COPD may be present on a chest x-ray, such as lung hyperinflation, hyperlucency of the lungs, or tapering of vascular markings Laboratory tests: should include a complete blood count (CBC) with differential to rule out anemia, polycythemia, and Serum alpha 1 -antitrypsin levels are recommended for individuals presenting with COPD at early ages (less than 45 years of age), in non-tobacco users with clinical emphysema, and individuals with a family history of COPD at a young onset. Non-Rx Treatment: No smoking (smoking cessation), Pulmonary rehabilitation is recommended in patients with high symptom, influenza vaccines, pneumococcal polysaccharide vaccine (PPSV23) is recommended for all patients at age 65 years and adults 19 to 64 years of age at high risk are recommended to have the PPSV23. Rx Treatment: COPD exacerbations are classified as mild, moderate, or severe. Interventions aligned with severity include: MILD (short-acting bronchodilator [SABDs]; treatment only; MODERATE (SABDs and/or oral corticosteroids); or SEVERE (emergency department visit or hospitalization required). Inhaled Beta 2 -Agonist Bronchodilators: Bronchodilators are widely used in the treatment of COPD to reverse bronchoconstriction by relaxing smooth muscles in the airways. There are two types of beta 2 -agonists: SABAs and LABAs. * SABAs, known as “rescue” inhalers, are prescribed for intermittent symptoms on an as-needed basis. * SABAs include medications such as Albuterol or Levalbuterol. LABAs in COPD are used for maintenance therapy to prevent acute bronchospasms and not for relief of acute symptoms. The duration of LABAs is about 12 hours. ⟶ Asthma (Dunphy) Risk Factors: Exposure to allergens, respiratory infections, family history/genetic predisposition, atopy, occupational irritants, tobacco smoke, high levels of indoor and outdoor pollution, and obesity; rhinitis is a specific factor in older adults Cardinal symptoms: Wheezing, shortness of breath, cough (especially at night), chest tightness. Diagnostic Tests: Methacholine test can be done with spirometry (used in asthma diagnosis) it causes bronchoconstriction. Spirometry or pulmonary function testing, particularly forced expiratory volume in 1 second (FEV 1), FEV 6, forced vital capacity (FVC), and FEV 1 /FVC ratio before and after bronchodilator challenge, showing an improvement of 12% and 200 mL, indicates reversible airway obstruction. This is helpful in differentiating asthma from COPD, particularly in an older adult with a prior smoking history. If spirometry is near normal, bronchoprovocation such as a Methacholine challenge test may help to differentiate other conditions. Laboratory tests: In a patient with dyspnea, measurement of brain natriuretic peptide, also known as B-type natriuretic peptide (BNP), and a chest x-ray may be needed to eliminate other conditions. Treatment: Nitric Oxide, dilates the airway by relaxing the smooth muscle and confirms that a corticosteroid therapy will most likely work as well Medications for each severity class (Dunphy p. 401) Step 1: Intermittent: PEF normal, FEV1>80% predicted, PFT variability > 20% (SABA-PRN and less than twice a week) no daily med needed SABA Albuterol Step 2: Mild persistent: FEV1>80% predicted, PFT variability 20-30% symptoms > 2 days a week, several times at night per month (SABA PRN and not to exceed 3-4 times a day) Corticosteroid (ICS) Fluticasone Step 3: Moderate Persistent: FEV1 60-80% predicted, PFT variability > 30%-daily symptoms, exacerbations affect sleep/activity (not nightly) SABA PRN no to exceed 3-4 times per day. Daily low dose ICS+LABA or medium dose ICS or low dose ICS +LTRA, theophylline or zileuton ICS or Combination Fulticasone/salmeterol, Budesonide/formoterol, or Momentasone/formoterol Step 4: Severe persistent: FEV1 30% continuous daily symptoms, frequent nighttime symptoms. PRN SABA not to exceed 3-4 times per day. Short course of oral corticosteroid (systemic) Daily regimen: Medium dose ICS+LABA/alternative: medium dose ICA+LTRA, theophylline or zileuton ICS & LABA Community Acquired Pneumonia (CAP) (Dunphy) ⟶ Signs and symptoms: Typical symptoms include fever, chills, cough, and rusty or thick sputum, with associated gastrointestinal upset or anorexia, malaise, and diaphoresis; pleuritic chest pain may also be present, crackles. Older patient - mental status changes, falls, inc. resp. rate, hypotension, anorexia, new onset of urinary incontinence. ⟶ Diagnostic criteria: CURB -65 (each criteria worth 1 pt) C - Confusion U - BUN >19 ng/dL R - Respiratory rate ≥ 30 breaths/min B - BP: Systolic <90 mm Hg OR Diastolic <60 mm Hg ⟶ Radiographic findings: chest x-ray is considered the gold standard for the diagnosis of pneumonia; C-reactive protein (CRP) and/or urine specific antigen when there is a question about when, or if, to start antibiotic therapy ; CT scan of the chest is often ordered and is more accurate than a chest x-ray; Pulmonary infiltrate, lobular consolidation, or opacities found on chest x-ray, CT scan, or ultrasound confirm the diagnosis of pneumonia. ⟶ Treatment standards (Dunphy p. 383): Antimicrobial therapy represents the mainstay of treatment for patients with suspected or confirmed pneumonia. Additional management is supportive and includes the use of analgesics for relief of chest pain and myalgia, antipyretics to control fever, increased fluid intake (typically at least 3 L over 24 hours), restricted activity or bedrest, a position of comfort (usually upright) to facilitate breathing, and humidified air to relieve irritated nares and pharynx. Expectorants may be indicated to decrease sputum viscosity and clear airways if a productive cough is present. ⟶ Treatment: Uncomplicated CAP, Azithromycin (Zithromax) or Clarithromycin (Biaxin) or Doxycycline Treatment Standards/Guidelines: Empiric Antimicrobial Choices for Community-Acquired Pneumonia (CAP) PATIENT PROFILE ANTIMICROBIAL AGENT Uncomplicated CAP Without recent antibiotic therapy (ATBX)* Azithromycin (Zithromax) or clarithromycin (Biaxin) or doxycycline (Vibramycin) With recent ATBX† Respiratory fluoroquinolone moxifloxacin (Avelox) or levofloxacin (Levaquin) OR Azithromycin or clarithromycin PLUS High-dose amoxicillin (Amoxil) OR Azithromycin or clarithromycin PLUS High-dose amoxicillin– clavulanate (Augmentin) Patient with CAP plus comorbidities: alcoholism; diabetes mellitus; lung/liver/renal diseases Respiratory fluoroquinolone OR Beta-lactam IV/intramuscular ceftriaxone (Rocephin) or Cefuroxime (Ceftin) PLUS Macrolide Patient with community-acquired methicillin-resistant S . aureus pneumonia Vancomycin (Vancocin) OR Linezolid (Zyvox) ⟶ Scoring 0-1 : Low risk; consider outpatient treatment 2: Brief hospitalization or closely monitored outpatient treatment ≥ 3: Severe, hospitalize and possible ICU Obstructive & Restrictive Airway Disease (Kahn Academy video and Dunphy ⟶ Understand the PFT interpretation for both (Kahn Academy video): https://www.alphanetbfrg.org/pdfs/Understanding-PFT.pdf ⟶ PFT: Normal FEV 1 /FVC ratio but decreased FVC and FEV 1 ; decreased total lung capacity, residual volume, and functional residual capacity. Residual volume–to–total lung capacity ratio is normal to low. ⟶ Know which airway diseases are reversible and irreversible: FEV 1 /FVC ratio before and after bronchodilator challenge, showing an improvement of 12% and 200 mL, indicates reversible airway obstruction ⟶ Obstructive pattern: An FEV1/FVC <70/80% suggests obstructive lung disease. o Decreased FEV1, normal or decreased FVC, and decreased FEV1/FVC o Classically, these are the patients with asthma, chronic bronchitis, or emphysema ▪ PFTs can help further distinguish between the above three: ▪ Bronchodilator responsiveness - an increase in the FEV1 by 12% following bronchodilator use suggests asthma ▪ Bronchial provocation - inducing asthmatic obstruction of reactive lower airways by administering methacholine, histamine, or adenosine monophosphate ▪ DLCO will be decreased in patients with emphysema, and can be normal or increased in patients with asthma o Lower airway obstruction vs. upper airway obstruction ▪ Lower airway obstruction typically displays impaired expiratory capacity (see image below), while upper airway obstruction has impaired inspiratory capacity, which can be evident on the flow volume loop (seen as flattening of the inspiratory arm). ⟶ Restrictive pattern restrictive lung disease typically has normal or increased FEV1/FVC o Decreased TLC, FEV1, and FVC with a normal FEV1/FVC, and a low DLCO o Typically these are patients with interstitial lung disease, severe skeletal abnormalities, or diaphragmatic paralysis o The flow volume loop is generally normal in appearance, but has low lung volumes Spirometry (Kahn Academy video and readings) ⟶ Know definitions for each spirometry criteria: Spirometry measures two key factors: expiratory forced vital capacity (FVC) and forced expiratory volume in one second (FEV1). Your doctor also looks at these as a combined number known as the FEV1/FVC ratio. If you have obstructed airways, the amount of air you’re able to quickly blow out of your lungs will be reduced. This translates to a lower FEV1 and FEV1/FVC ratio. Forced vital capacity (FVC). This is the largest amount of air that you can forcefully exhale after breathing in as deeply as you can. A lower than normal FVC reading indicates restricted breathing. Forced expiratory volume (FEV). This is how much air you can force from your lungs in one second. This reading helps your doctor assess the severity of your breathing problems. Lower FEV-1 readings indicate more significant obstruction. Spirometry ⟶ PFTs can be used in a variety of settings, and they are generally ordered to: o Look for evidence of respiratory disease when patients present with respiratory symptoms (e.g. dyspnea, cough, cyanosis, wheezing, etc.); o Assess for any progression of lung disease; o Monitor the efficacy of a given treatment; o Evaluate patients pre-operatively; and o Monitor for potentially toxic side effects of certain drugs (e.g. amiodarone) ⟶ The components of PFTs include: o Lung volumes o Spirometry and flow volume loops o Diffusing capacity ⟶ Sleep Apnea ⟶ Signal Symptoms: OSA should be suspected whenever hypersomnia and snoring coexist or even with new onset or poorly controlled hypertension. Patient report of not sleeping, excessive daytime sleepiness, loud snoring (sleep apnea), restless legs, difficulty falling asleep and staying asleep, irritability, difficulty concentrating, sleep that is not refreshing and restful. Diagnose: the gold standard for identifying the presence, type, and severity of sleep apnea is overnight Polysomnogram OSA Treatment: Although CPAP machine is the preferred method for treatment of OSA, BPAP or APAP ⟶ Diagnostic criteria (includes risk factors) Sleep apnea is defined as a temporary pause in breathing during sleep that lasts at least 10 seconds. For a confirmed diagnosis, this should occur a minimum of five times an hour. The predominant physical examination findings of OSA reflect the risk factors: obesity (particularly of the upper body), increased neck size, crowded oropharynx (tonsillar hypertrophy and enlargement of soft palate [uvula] and tongue). ⟶ Signs and symptoms & Hypersomnolence signs and symptoms: Hypersomnolence is the single most important presenting symptom of sleep apnea. Daytime symptoms include a morning headache (from hypercapnia) and neuropsychological disturbances, including falling asleep while performing purposeful activities. The patient may complain of nocturnal restlessness, frequent urination or enuresis, and choking. Patients also may report impaired intellectual performance, such as decreased concentration, ambition, and memory loss. 3 Mood disord ers Anxiety ⟶ Signs and symptoms, prevalence, risk factors: Excessive worrying that is difficult to control and interferes with daily life; can also manifest with somatic symptoms such as chest tightness, shortness of breath, upset stomach. Predictors of late- onset anxiety include female gender, recent adverse life events, illness, cognitive impairment, and mental illness comorbidities, while poverty and poor psychological support during earlier years also contribute (Zhang et al., 2015). Comorbid dementia or depression are not uncommon in older patients experiencing anxiety Signs and Symptoms: May include a sense of impending doom, trembling, breathlessness, and tachycardia. Anxiety may impair working memory, attention, and problem-solving skills (Andreescu & Varon, 2015). In older adults, somatic complaints are more common, such as constipation, nausea, and sleep disturbance. Worries about health, disability, and finances are also common. One is more likely to learn of a patient’s anxiety by asking the question, “How do you feel when you are under stress?” than by asking, “Are you anxious?” Patients with specific phobias may have an irrational fear to something that poses little danger, such as fear of crowds or natural phenomena (heights, lightening). Specific phobias may occur following a traumatic event, such as falling. Symptoms of anxiety in older adults often overlap with symptoms of physical disorders, depression, and dementia. Generalized anxiety disorder (GAD), social anxiety, specific phobia, and anxiety disorder related to substance use, medication, or another medical condition. Panic disorder and agoraphobia are less common in older adults Diagnose: Excessive anxiety and worry for at least for 6 months with intensity/duration/frequency out of proportion for feared event. Presence of physiological symptoms • Presence of mood related symptoms such as depression, loss of interest in activities • 3 of the following 6 symptoms (only 1required in children) Muscle tension, sleep disturbance, restlessness, easily fatigued, difficulty concentrating, irritability Diagnostic Tests: Complete a history and physical examination. Laboratory tests can rule out medical conditions with anxiety symptoms, including complete blood count (CBC), CMP, and TSH. Order additional tests based on the findings of the history and physical examination. Valid assessment scales to help diagnosis and assess older adults for anxiety include the Geriatric Anxiety Inventory (GAI) and the Geriatric Assessment Scales. Treatment: 1st Line is SSRI: Sertraline (Zoloft), Escitalopram (Lexapro), Citalopram, and Paxil are commonly used in older adults and SNRI: Venlafaxine (Effexor) and anxiolytic Buspar to treat acute symptoms and Response should be noted in 8 weeks First-line treatment includes the selective serotonin reuptake inhibitors (SSRIs) because they have the least risk of drug interactions, side effects, or worsening existing medical conditions. Escitalopram, sertraline, and citalopram are commonly used in older adults, although citalopram should not be used routinely in doses above 20 mg daily due to prolongation of QT interval precautions. GI disturbances, sexual dysfunction, and altered mental status due to hyponatremia may occur. Buspirone and gabapentin are also used as secondary agents when first-line therapy fails and anxiolytic therapy is warranted. ⟶ Medication management Maintenance SSRI use has been shown to reduce relapse of anxiety in older adults. SSRIs can increase anxiety if started at higher doses. It may take several weeks for full effect to occur. Unipolar Depression (Kennedy and Dunphy) Signs and symptoms: Depression is a pervasive feeling of sadness or a lack of interest or pleasure in previously enjoyed or usual activities. Feelings of guilt, self-hate, loss of motivation, low self-esteem, sleep and appetite disturbances, low energy, and poor concentration are common. Risk factors: Aging adults are at increased risk of depression, vascular risk factors, and the association of ischemic cerebral lesions with distinctive behavioral symptoms supports the “vascular depression”, Alcohol, substance abuse, family or personal history of psychiatric illness or depression Diagnose: PHQ2 an PHQ9 – At least one of the symptoms is either (1) depressed mood or (2) anhedonia (no pleasure), five (or more) symptoms have been present during the same 2-week period causing change from previous functioning. minimal depression 0-4, mild to moderate depression 10-14, moderately severe 15-19, severe 20-27 PHQ9: scoring 1-4=minimal 5-9=mild 10-14=moderate 15-19=moderately/severe 20-27=severe The Geriatric Depression Scale (GDS) is a screening test, 5 or more indicates depression for patients >60 Diagnostic criteria: CBC, CMP, Lipid Panel, TSH, Vit B and Vit D Treatment: 1 st line treatment (mild, moderate, severe) Medication management – SSRI: Sertraline (Zoloft) Citalopram (Celexa), Escitalopram (Lexapro), Fluoxetine (Prozac), Paroxetine (Paxil) SNRI: Duloxetine (Cymbalta), Venlafaxine (Effexor) ⟶ 1st line treatment (mild, moderate, severe) ⟶ Medication management ⟶ Bipolar Depression Signal Symptoms: 1. Bipolar I disorder requires an individual to have experienced at least one manic episode. A manic episode involves a change in mood that may be expansive, euphoric, or irritable, and accompanied by an increase in energy level. Most patients also have depressive episodes, but this is not a required component. 2. Bipolar II disorder requires at least one prior episode of major depression and at least one hypomanic episode, a milder form of mania. Diagnosis: Mood Disorder Questionnaire (MDQ) is a validated screening tool for BD-MDQ can identify 70% of persons with BD while eliminating the diagnosis for 90% of persons without it, GDS for elderly with depressive symptoms Elevated mood, presenting as euphoria or irritability. According to the DSM-5, the individual must also experience increased energy while having these symptoms ■ Distractibility ■ Insomnia ■ Grandiosity ■ Flight of ideas ■ Activities (hyperactive, does not require rest) ■ Speech (rapid, can be garbled) ■ Thoughtlessness (impulsivity) Symptoms during the depressive phase are similar to those of major depression. Use the acronym SIGECAPS: ■ Sleep disturbance ■ Interest/pleasure reduction ■ Guilt feelings, thoughts of worthlessness ■ Energy changes/fatigue ■ Concentration/attention impairment ■ Appetite/weight changes ■ Psychomotor disturbances First-line treatment for late-life mania includes • Mood stabilizers lithium and valproic acid • antipsychotics, quetiapine and olanzapine • Treatment: Lithium, Lamotrigine, Valproate, Carbamazepine Bipolar Mania U.S. Food and Drug Administration (FDA)-Approved Drugs ■ Anticonvulsant mood stabilizers: Lithium, valproic acid, divalproex, or carbamazepine (second line) ■ Antipsychotics: Olanzapine, risperidone, quetiapine, ziprasidone, aripiprazole, asenapine Bipolar Acute Depression FDA-Approved Drugs ■ Anticonvulsants: Lithium ■ Antipsychotics: Quetiapine, lurasidone, olanzapine-fluoxetine combination. ⟶ Medication metabolic side effects. Valproic acid: • drug levels, liver function tests (LFTs), and CBC. Adverse effects include weight gain, hepatotoxicity, pancreatitis, and thrombocytopenia. ⟶ Sleep/ Wake Disorders (Dunphy) ⟶ Underlying medical causes ⟶ Underlying psychological causes ⟶ Most common sleep disorder (Dunphy) Insomnia Signs and symptoms: Psychiatric disorder, hot flashes, OSAH (obstructive sleep apnea hypopnea), RLS (restless leg syndrome) GERN, Arthritis, Fibromyalgia, Delirium, Dementia, Thyroid, Obesity, Pregnancy, Nocturia, Rx side effects Signs and symptoms: reports not sleeping, excessive daytime sleepiness, loud snoring (sleep apnea), restless legs, difficulty falling asleep and staying asleep, irritability, difficulty concentrating, sleep that is not refreshing and restful, daytime fatigue, an older adult may spend 10 to 12 hours in bed at night trying to sleep Diagnostic criteria: Epworth Sleepiness Scale or Stanford Sleepiness Scale, sleep diary, interrogate sleep partner (if any) 1st line treatment for chronic insomnia Treatment: Cognitive Behavioral Therapy CBT-1 st line tx for chronic insomnia, OTC melatonin or prescription ramelteon can be tried. If ineffective, initiate a short-acting sedative-hypnotic, such as Zolpidem (Ambien) or Zaleplon (Sonata), at lowest dosage before desired bedtime for 1 week or less. Suggest spacing dosing to every other day to avoid side effects. If a benzodiazepine is used, Temazepam (Restoril) is relatively short-acting. If this is ineffective, reevaluate the diagnosis and restructure the treatment modalities. Benzo’s not for the elderly. Transient insomnia avoid caffeine 12 before bedtime, D/C ETOH and sleep-interrupting drugs, OTC melatonin, if ineffective, a short-acting sedative-hypnotic, such as zolpidem (Ambien) or zaleplon (Sonata), at lowest dosage before desired bedtime for 1 week or less (space to avoid S/E), 4 Osteoarthritis (Kennedy, Dunphy, Kahn Academy) Morning joint stiffness lasting less than 30 minutes; joint stiffness that improves with mild activity. gel phenomenon, Weight-bearing joints such as the knees and hips are most affected by OA, Persistent pain and limitation of motion in the affected joint. Signs and symptoms: gradual development of upper or midthoracic back pain associated with activity or long periods of sitting or standing, which is relieved with rest in the recumbent position, Acute vertebral compression fractures generally occur in the thoracic or high lumbar region, with the patient experiencing a more sudden, severe onset of pain Radiographic findings: joint space narrowing due to loss of cartilage, later finding Asymmetrical joint space narrowing. Ultrasound and MRI may be used to detect damage to cartilage, ligaments, and tendons, which cannot be seen on x-ray Treatment: In noninflammatory OA, Acetaminophen is the medication of choice in doses of 2 to 3 g per day, For patients who are not getting relief from acetaminophen and exercise, the cyclooxygenase type 2 (COX-2) selective agents: celecoxib 50 to 100 mg PO twice daily, NSAIDS should be avoided in older adults with a calculated creatinine clearance less than 35 ml/min, Topical capsaicin nonpharmacological therapies, such as walking NSAIDs- cyclooxygenase type 2(COX-2) such as celecoxib (Celebrex) 50- 100mg BID. In patients who can not afford COX-2 may try, nonacetylated salicylates such as Magnesium trisalycylate 500-750mg BID-TID. Tramadol can be given at 50mg Q 4 -6 hours Opiates such as codeine and oxycodone can be used for severe OA Glucosamine and chondroitin Topical diclofenac sodium Osteoporosis • Osteoporosis is the most common bone disease in humans. Signs and symptoms: Kyphosis, decreased height, vertebral fractures, severe back pain. All patients more than 50 years old should be screened for fracture risk. The U.S. Prevention Task Force (USPTF) recommends osteoporosis screening in women 65 years and older and in younger women whose fracture risk is equal to or greater than that of a 65-year-old white woman who has no additional risk factors (Grade B). Diagnosis: A bone mineral density (BMD) can be measured by several methods, including dual-energy x-ray absorptiometry (DEXA or DXA), quantitative computed tomography (QCT), and quantitative ultrasound (QUS). DEXA Results: DEXA are reported as T- and Z- scores. T-score of -1.0 or above = normal bone density T-score between -1.0 and -2.5 = low bone density, or Osteopenia T-score of -2.5 or lower = osteoporosis Who Diagnostic Criteria: T Score o Medication management Tramadol can be given at 50mg Q • Osteoporosis Medication management Treatment: 1 st line: Bisphoshonates are now the first line treatment Alendronate, Risedronate, Zoledronic Acid, or Denosumab to reduce the risk for hip and vertebral fractures in women who have Calcium and Vitamin D • Post-menopausal women who are getting adequate calcium from dietary intake alone (approximately 1,200 mg daily) do not need supplementation • Women with inadequate dietary intake should take supplemental elemental calcium (generally 500–1,000 mg/day), in divided doses at mealtime, so that their total calcium intake (diet plus supplements) approximates 1,200 mg/day • Women should also ingest a total of 800 international units of vitamin D daily. TABLE 55.4 Recommended Daily Calcium Intake Women 50 years and younger 1,000 mg daily 51 years and older 1,200 mg daily Men 70 years and younger 1,000 mg daily 71 years and older 1,200 mg daily Rheumatoid Arthritis (Kennedy, Dunphy, Kahn Academy) Rheumatoid Arthritis is an incurable autoimmune condition that affects synovial joints in the body. Signs and symptoms: morning stiffness, joint swelling & pain (small joints of hands, wrists, & feet), symmetrical inflammatory polyarthritis, decreased physical function. Clinical Joint Findings: hyperflexion of the (middle joints of the fingers) PIP Proximal interphalangeal joints, flexion of the DIP joints (swan neck deformities), flexion of the PIP joints and extension of the DIP joints (boutonniere deformity). Clinical joint findings hyperflexion of the PIP joints flexion of the DIP joints (swan neck deformities) flexion of the PIP joints and extension of the DIP joints (boutonniere deformity) Diagnosis: A bone mineral density (BMD) can be measured by several methods, including dual-energy x-ray absorptiometry (DEXA or DXA), quantitative computed tomography (QCT), and quantitative ultrasound (QUS). *** Erosions at the joints may take several years to occur • Radiographs of the hands and feet are needed to look for early signs of erosions • Additional radiographic findings in RA include soft tissue swelling, symmetrical joint space narrowing, and joint subluxations Diagnostic criteria: rheumatoid factor (RF), CRP, ESR, anti-citrullinated peptide antibodies (when accompanied by high RF titer), anti-CCP antibodies, CBC may show normochromic, normocytic anemia, mild leukocytosis, and thrombocytosis Treatment: Corticosteroids, Analgesia, NSAIDs Disease-modifying antirheumatic drugs (DMARD) as a single therapy or a combination of two or more DMARDs. DMARDs suppress the immune response and prevent joint damage, although they may take up to 3 months to have an effect. Traditional DMARDs include: Methotrexate, Sulfasalazine, Leflunomide, Hydroxychloroquine [Show More]
Last updated: 2 years ago
Preview 1 out of 31 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$13.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Feb 10, 2023
Number of pages
31
Written in
Additional information
This document has been written for:
Uploaded
Feb 10, 2023
Downloads
0
Views
115





.png)




