1
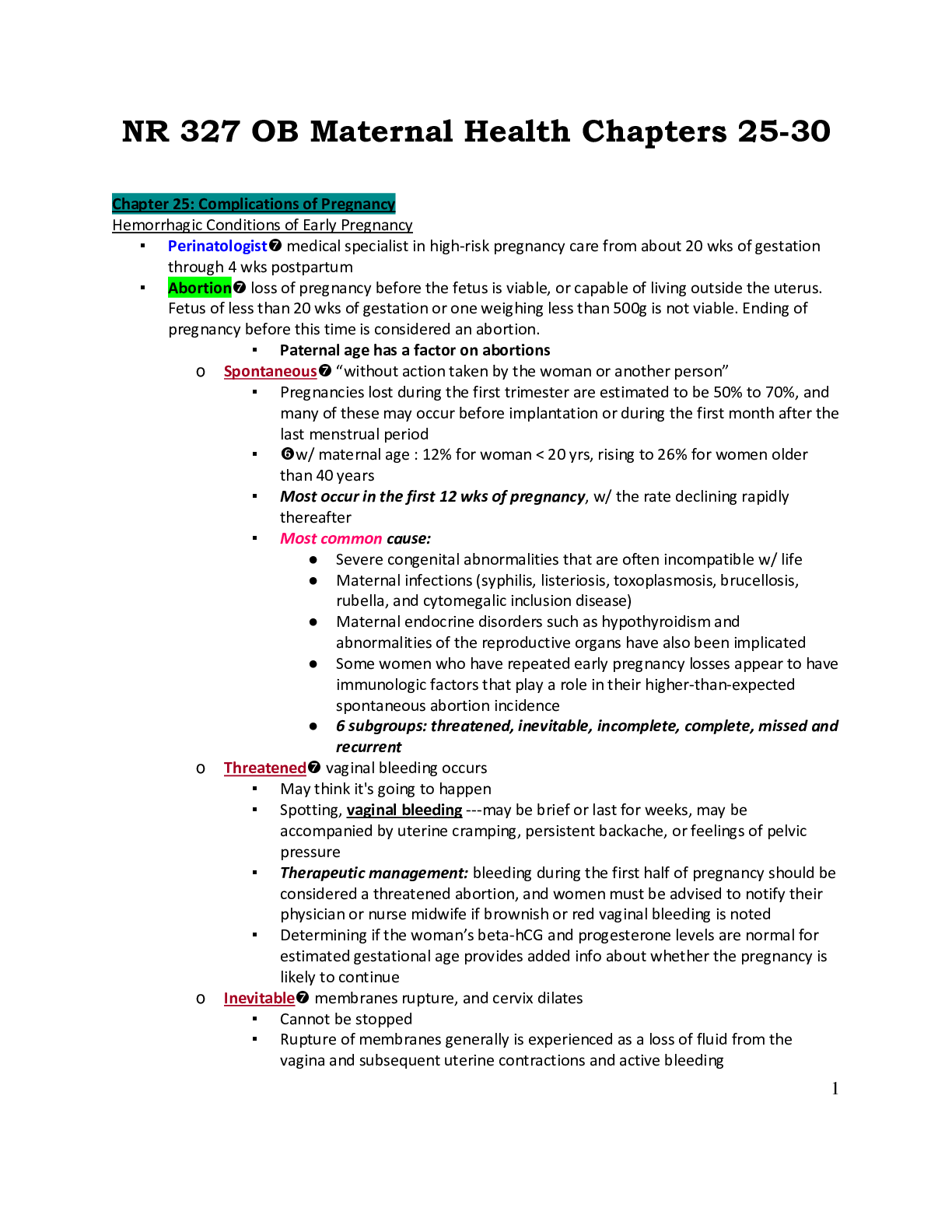
NR 327 OB Maternal Health Chapters 25-30
Chapter 25: Complications of Pregnancy
Hemorrhagic Conditions of Early Pregnancy
▪ Perinatologist medical specialist in high-risk pregnancy care from about 20 wks of gestat
...
1
NR 327 OB Maternal Health Chapters 25-30
Chapter 25: Complications of Pregnancy
Hemorrhagic Conditions of Early Pregnancy
▪ Perinatologist medical specialist in high-risk pregnancy care from about 20 wks of gestation
through 4 wks postpartum
▪ Abortion loss of pregnancy before the fetus is viable, or capable of living outside the uterus.
Fetus of less than 20 wks of gestation or one weighing less than 500g is not viable. Ending of
pregnancy before this time is considered an abortion.
▪ Paternal age has a factor on abortions
o Spontaneous “without action taken by the woman or another person”
▪ Pregnancies lost during the first trimester are estimated to be 50% to 70%, and
many of these may occur before implantation or during the first month after the
last menstrual period
▪ w/ maternal age : 12% for woman < 20 yrs, rising to 26% for women older
than 40 years
▪ Most occur in the first 12 wks of pregnancy, w/ the rate declining rapidly
thereafter
▪ Most common cause:
● Severe congenital abnormalities that are often incompatible w/ life
● Maternal infections (syphilis, listeriosis, toxoplasmosis, brucellosis,
rubella, and cytomegalic inclusion disease)
● Maternal endocrine disorders such as hypothyroidism and
abnormalities of the reproductive organs have also been implicated
● Some women who have repeated early pregnancy losses appear to have
immunologic factors that play a role in their higher-than-expected
spontaneous abortion incidence
● 6 subgroups: threatened, inevitable, incomplete, complete, missed and
recurrent
o Threatened vaginal bleeding occurs
▪ May think it's going to happen
▪ Spotting, vaginal bleeding ---may be brief or last for weeks, may be
accompanied by uterine cramping, persistent backache, or feelings of pelvic
pressure
▪ Therapeutic management: bleeding during the first half of pregnancy should be
considered a threatened abortion, and women must be advised to notify their
physician or nurse midwife if brownish or red vaginal bleeding is noted
▪ Determining if the woman’s beta-hCG and progesterone levels are normal for
estimated gestational age provides added info about whether the pregnancy is
likely to continue
o Inevitable membranes rupture, and cervix dilates
▪ Cannot be stopped
▪ Rupture of membranes generally is experienced as a loss of fluid from the
vagina and subsequent uterine contractions and active bleeding2
▪ Incomplete evacuation of the products on conception can result in excessive
bleeding or infection can occur
▪ Therapeutic management:
● Vacuum curettage (removal of uterine contents w/ a vacuum curette) is
used to clear the uterus if the natural process is ineffective or
incomplete
● Dilation and curettage (D&C) (stretching the cervical os to permit
suctioning or scraping the uterine walls) may be needed if the
pregnancy is more advanced or if bleeding is excessive
o Incomplete some products of conception have been expelled, but some remain
▪ Active uterine bleeding and severe abdominal cramping
▪ Cervix is open and fetal and placental tissues are passed
▪ Products of conception may have been expelled from the uterus but remain in
the vagina because of their small size, often no larger than a ping-pong ball, in
the very early gestation period
▪ Therapeutic management:
● Retained tissue prevents the uterus from contracting firmly, thereby
allowing profuse bleeding from uterine blood vessels
● Initial tx: focus on stabilizing the woman’s cardiovascular state
● Blood specimen is drawn for blood type and screen or crossmatch, and
an IV line is inserted for fluid replacement and drug administration
● D&C usually performed to remove the remaining tissue when the
woman’s condition is stable
● Later pregnancy and a larger amount of fetal tissue may require a
greater cervical dilation and evacuation (D&E) with removal of fetal
tissue, followed by vacuum or surgical curettage
o May be followed by IV administration of oxytocin or IM
administration of methylergonovine (methergine) to contract
the uterus and control bleeding
● D&C may not be performed if the pregnancy has advanced beyond 14
wks because of the danger of excessive bleeding
o In this case… oxytocin or prostaglandin is administered to
stimulate uterine contractions until all products of conception
(fetus, membranes, placenta, and amniotic fluid) are expelled
o Complete
▪ All products have been expelled from the uterus
▪ After passage of all products of conception, uterine contractions and bleeding
subside, and the cervix closes
▪ Uterus feels smaller than the length of gestation would suggest
▪ Symptoms of pregnancy are no longer present, and the pregnancy test becomes
negative as hormone levels fall
▪ Therapeutic management:
● No additional intervention is required once complete abortion is
confirmed unless excessive bleeding or infection develops
● Rest and watch for further bleeding, pain, or fever3
● Not have sexual intercourse until after a follow-up visit w/ her health
care provider
o Missed
▪ Fetus dies during first have a pregnancy but is retained in the uterus
▪ May/ not have vaginal bleeding (red or brownish color)
▪ Uterus stops growing and decreases in size
▪ Amniotic fluid starts to get absorbed and tissue of fetus starts degenerating
▪ Macerationdiscoloration, softening, and eventual tissue degeneration
▪ Therapeutic management:
● For a first-trimester missed abortion, a D&C usually can be done. If the
missed abortion occurs during the second trimester, when the fetus is
larger, a D&E may be done, or vaginal prostaglandin E2 (PGE2) or
misoprostol (Cytotec) may be needed to induce uterine contractions
that expel the fetus. A D&C may be needed to remove the placenta.
● 2 major complications of missed abortion are infection and
disseminated intravascular coagulation (DIC)
o Signs such as elevation in temp, vaginal discharge w/ a foul
odor, and abdominal pain indicate uterine infection, and
evacuation of the uterus is delayed until cultures are obtained
and antimicrobial therapy is initiated
o Recurrent spontaneous
▪ Usually defined as 3 or more spontaneous abortions, although some authorities
now use two or more pregnancy losses as the definition
▪ Primary cause of recurrent abortion are believed to be genetic or chromosomal
abnormalities and anomalies of the reproductive tract, such as bicornuate
uterus (uterus w/ 2 horns) or incompetent cervix.
▪ Additional causes include:
● An inadequate luteal phase w/ insufficient secretion of progesterone
and immunologic factors that involve increased sharing of human
leukocyte antigens by the sperm of the man and the ovum of the
woman who conceived
● Woman’s immunologic system is not stimulated to produce blocking
antibodies that protect the embryo from maternal immune cells or
other damaging antibodies
● Systemic diseases such as lupus and diabetes mellitus have been
implicated in recurrent abortions
▪ May be caused by cervical incompetence, and anatomic defect that results in
painless dilation of the cervix in the second trimester… in this situation, a
cerclage procedure—suturing of the cervix to prevent early dilation—may be
performed
● Cerclage is most likely to be successful if done before much cervical
dilation or bulging of the membranes through the cervix has occurred
● Sutures may be removed near term in preparation for vaginal deliver
▪ RhoGAM is given to unsensitized Rho(D)-negative woman to prevent dev of
anti-Rh antibodies4
▪ Microdose (50mcg) is given to woman whose fetus is less than 13 wks of
gestational age at the time of the abortion
▪ Disseminated intravascular coagulation**
o DIC, also called consumptive coagulopathy
o Life-threatening defect in coagulation that may occur w/ several complications of
pregnancy such as abruptio placentae or hypertension
o Inappropriate coagulation
o Tiny clots form in the tiny blood vessels, blocking blood flow to organs causing ischemia
o Clotting mechanisms defect
▪ Diseases that cause DIC (3 major groups)
a. Infusion of tissue thromboplastin into the circulation and uses up clotting factors such
as fibrinogen and platelets:
i. Abruptio placentae (premature separation)
ii. Retention of a dead fetus
b. Conditions that cause endothelial damage (inner lining of blood vessels)
i. Severe preeclampsia
ii. HELLP (hemolysis, elevated levels of liver enzymes, and low platelet levels)
c. Nonspecific effect of some diseases
i. Maternal sepsis
ii. Amniotic fluid embolism
▪ Nursing assessment
o Assess for bleeding for unexpected sites: IV sites, nosebleeds, spontaneous bruising
o Report findings
o Coagulation studies
o No epidurals ( if patient is at risk)
o Monitor clients who may be at risk
▪ DIC treatment
o Blood labs confirm dx:
▪ Decrease fibrinogen and platelets
▪ Prolonged PT and a PTT
▪ Increase fibrin degradation products
o The D-dimer serum assay, which normally has negative results, confirms fibrin split
products (FSP) and is presumptive for DIC when results are positive
o Correct the cause if known
o Blood products
▪ Such as whole blood, packed red blood cells, and cryoprecipitate, are
administered as needed, to maintain the circulating volume and to transport
oxygen to body cells
o Administer oxygen
▪ Ectopic pregnancy
o Implantation of a fertilized ovum outside of uterus
o More than 98% of ectopic pregnancies occur in the fallopian tube
o “disaster of reproduction”
o Remains a significant cause of maternal death from hemorrhage
o Tubal damage caused by ectopic pregnancy reduced the woman’s changes of
subsequent pregnancies5
o Incidence and Etiology
▪ Increase in incidence is attributed to the growing number of women of
childbearing age who experience scarring of the fallopian tubes because of
pelvic infection, inflammation, or surgery
▪ Pelvic infxn often is caused by chlamydia or Neisseria gonorrhoeae
▪ Greater incidences of ectopic pregnancies occur in women who conceived w/
assisted reproduction, most likely r/t the tubal factors that contributed to
infertility
▪ Contraception such as intrauterine contraceptive devices or low-dose
progesterone agents is associated w/ increased risk of ectopic pregnancy
▪ Additional causes of ectopic pregnancy are delayed or premature ovulation, w/
the tendency of the fertilized ovum to implant before arrival in the uterus, and
altered tubal motility in response to changes in estrogen and progesterone
levels that occur w/ conception
▪ Multiple induced abortions increase the risk for tubal pregnancy, possibly
because of salpingitia (infxn of the fallopian tube) that occurred after induced
abortion
▪ Signs and symptoms
o Missed menstrual period
o Positive pregnancy test
o Abdominal pain
o Vaginal “spotting”
o Deep, severe pelvic pain= ruptured ectopic pregnancy
▪ If implantation occurs in the distal end of the fallopian tube, which can contain the growing
embryo longer, the woman may at first exhibit the usual early signs of pregnancy and consider
herself to be normally pregnant. Several weeks into the pregnancy, intermittent abdominal pain
and small amounts of vaginal bleeding occur, and initially this could be mistaken for threatened
abortion. Because routine ultrasound examination in early pregnancy is common, however, it is
not unusual to diagnose an ectopic pregnancy before onset of symptoms.
▪ If implantation has occurred in the proximal end of the fallopian tube, rupture of the tube may
occur within 2 to 3 weeks of the missed period because the tube is narrow in this area.
Symptoms include sudden, severe pain in one of the lower quadrants of the abdomen as the
tube tears open and the embryo is expelled into the pelvic cavity, often with profuse abdominal
hemorrhage.
▪ Radiating pain under the scapula may indicate bleeding into the abdomen caused by phrenic
nerve irritation. Hypovolemic shock (acute peripheral circulatory failure from loss of circulating
blood) is a major concern because systemic signs of shock may be rapid and extensive without
external bleeding.
▪ Laparoscopy (examination of the peritoneal cavity by means of a laparoscope) occasionally may
be necessary to diagnose rupture of an ectopic pregnancy
o Characteristic bluish swelling within the tube is the most common finding
▪ Methotrexate (a folic acid antagonist) is used to inhibit cell division in the developing embryo
▪ Surgical management of a tubal pregnancy that is unruptured may involve a linear
salpingostomy (incision along the length of a fallopian tube to remove an ectopic pregnancy
and preserve the tube) to salvage the tube
▪ If fallopian tube ruptures, goal is to control the bleeding and prevent hypovolemic shock6
▪ Gestational trophoblastic disease (hydatidiform mole)
o Hydatidiform mole is one form of gestational trophoblastic disease, which occurs when
trophoblasts (peripheral cells that attach the fertilized ovum to the uterine wall)
o Abnormality of placenta develops, and, if present, a fetus has a fatal chromosome
defect
o The condition is characterized by proliferation and edema of the chorionic villi.
o Fluid-filled villi form grapelike clusters of tissue that can rapidly grow large enough to
fill the uterus to the size of an advanced pregnancy
o Form of a molar pregnancy
▪ Can be complete or partial
● Complete= no fetus
● Partial= fetal tissue or membranes are present
o Risk in maternal age over 35 yrs of age
o Incidence is higher among Asian women
o Previous molar pregnancies also is a risk
o May become cancerous ---- choriocarcinoma- and may metastasize to sites such as the
lung, vagina, liver, and brain
o Complete mole is thought to occur when the ovum is fertilized by a sperm that
duplicates its own chromosomes while the maternal chromosomes in the ovum are
inactivated
▪ Composed only of enlarged villi but contains no fetal tissue or membranes
o Partial mole, the maternal contribution is usually present but the paternal contribution
is doubled, and therefore the karyotype is triploid (69, XXY or 69XYY).
▪ Includes some fetal tissue and membranes
▪ If fetus is identified with the partial mole, it is grossly abnormal because of the
abnormal chromosomal composition
▪ Clinical manifestations:
o Higher levels of beta-hCG than expected
o Snowstorm ultrasound pattern—shows vesicles and the absence of a fetal sac or fetal
heart activity in a complete molar pregnancy
o Larger uterus than expected
o Vaginal bleeding
o Excessive N/V
o Early development of preeclampsia (before 24 wks)
▪ Therapeutic management
o Medical management includes two phases:
1) Evacuation of the trophoblastic tissue of the mole
2) Continuous follow-up of the woman to detect malignant changes of any
remaining trophoblastic tissue
o Radiology studies to determine metastatic disease
o Lab studies (CBC, coagulation cross & match, liver enzymes)
o Vacuum aspiration followed by curettage(D and E)
▪ Pitocin following evacuation---to contract the uterus7
● Uterine contractions can cause trophoblastic tissue to be pulled into the
large venous sinusoids in the uterus, resulting in embolization of the
tissue and respiratory distress
▪ Beta hcg repeated in 6 wks
▪ Pregnancy should be avoided for 1 year
Application of the Nursing Process: Hemorrhagic Conditions in Early Pregnancy
▪ Assessment (how, where, color, ect.)
▪ Nursing diagnoses
▪ Expected outcomes
▪ Interventions
o Provide info about tests and procedures
o Teach measures to prevent infection
o Provide dietary info
o Teach signs of infection to report
o Reinforce follow up care
▪ Evaluation
Hemorrhagic Conditions of Late Pregnancy: Placenta Previa
▪ After 20 wks of pregnancy, the 2 major causes of hemorrhage are the disorders of the placenta
called placenta previa and abruptio placentae
▪ Abnormal implantation of the placenta in the lower uterus at or very near the cervical os
(opening)
o The placenta is closer to the internal cervical os than to the presenting part (usually the
head) of the fetus
o 3 classifications of placenta previa (total, partial, and marginal) depend on how much of
the internal cervical os is covered by the placenta
o Marginal (sometimes called low-lying): the placenta is implanted in the lower uterus,
but its lower border is more than 3 cm from the internal cervical os
▪ Common is early ultrasound examination and often appears to move upward
and away from the internal cervical os (placental migration) as the fetus grows,
and the upper uterus develops more than the lower uterus
o Partial: the lower border of the placenta is within 3 cm of the internal cervical os but
does not completely cover the os
o Total: the placenta completely covers the internal cervical os
o Marginal placenta previa is common in early ultrasound examinations and often appears
to move upward and away from the internal cervical os as the fetus grows, and the
upper uterus develops more than the lower uterus
▪ Incidence and etiology
o 1 in 300 births--- evidence indicates that rate is increasing
o More common in older women, multiparas, women who have had cesarean births,
and women who have had suction curettage for induced or spontaneous abortion
o African or Asian ethnicity also increases the risk
o Cigarette smoking and cocaine use are personal habits that add to a woman’s risk for
previa
o Previa more likely if the fetus is male
▪ Clinical manifestations
o Painless--- d/t happening in the lower part of the uterus8
o Sudden onset of painless uterine bleeding in the last half of pregnancy
o Bleeding results from tearing of the placental villi from the uterine wall as the lower
uterine segment thins and the internal os begins dilation near term
o Bleeding is painless because it does not occur in a closed cavity and does not cause
pressure on adjacent tissue
▪ Therapeutic management
▪ Home and inpatient care
Hemorrhagic Conditions of Late Pregnancy: Abruptio Placentae
▪ Premature separation of a normally implanted placenta --- occurs in cases of bleeding and
formation of a hematoma (clot) on the maternal side of the placenta
▪ Hemorrhage may be apparent (vaginal bleeding) or concealed
o Major dangers for the women:
▪ Hemorrhage
▪ Consequent hypovolemic shock
▪ Clotting abnormalities
o Major dangers for the fetus:
▪ Asphyxia
▪ Excessive blood loss
▪ Prematurity
▪ Incidence and etiology (pg.515**)
o Accounts for 10% to 15% of perinatal deaths
o Varies but it about 0.5 to 1% of pregnancies
o Cause is unknown, but several factors increase the risk
▪ Maternal use of cocaine, which causes vasoconstriction (narrowing of blood
vessel lumen) in the endometrial arteries, is a leading cause of abruptio
placentae
▪ Maternal HTN, cigarette smoking
▪ Multigravida status
▪ Short umbilical cord
▪ Abdominal trauma
▪ Premature rupture of the membranes
▪ History of previous premature separation of the placenta
▪ AMA (advanced maternal age)
▪ Clinical manifestations
1) Bleeding, which may be evident vaginally or may be concealed behind the placenta
2) Uterine tenderness that may be localized at the site of the abruption
3) Uterine irritability w/ frequent low-intensity contractions and poor relaxation between
contractions
4) Abdominal or low back pain that may be described as aching or dull
5) High uterine resting tone identified w/ use of an intrauterine pressure catheter
▪ Additional signs include, back pain, nonreassuring FHR patterns, signs of
hypovolemic shock, or fetal death
▪ Therapeutic management
▪ Nursing considerations
Application of the Nursing Process: Hemorrhagic Conditions of Late Pregnancy (pg.516**)
▪ Assessment9
o Amount of bleeding
o What time did the bleeding start?
o Pain?
o VS—check for SHOCK
▪ Increased HR
▪ Low BP
o Condition of the fetus
o Uterine contractions
o Obstetric history
o Length of gestation
o Lab data
▪ Nursing diagnoses
▪ Expected outcomes
▪ Interventions
o Monitor for signs of hypovolemic shock
▪ Early signs:
● Fetal tachycardia (often first sign of either maternal or fetal
hypovolemia)
● Maternal tachycardia, weak peripheral pulses
● Normal or slightly decreased blood pressure
● Increased resp. rate
● Low oxygen saturation
● Cool, pale skin and mucous membranes
▪ Late signs:
● Falling blood pressure and oxygen saturation levels
● Pallor; skin becomes cold and clammy
● Urine output less than 30 mL/hr
● Restlessness, agitation, decreased mentation
▪ Evaluation
Hyperemesis Gravidarum
▪ Persistent, uncontrollable vomiting that begins in the first wks of pregnancy and may continue
throughout pregnancy
▪ HEG may continue throughout pregnancy, although its severity usually lessens
▪ Associated with loss of 5% or more of prepregnancy weight, dehydration, acidosis from
starvation, elevated levels of blood and urine ketones, alkalosis from loss of hydrochloric acid in
the gastric fluids and hypokalemia
▪ Short-term hepatic dysfunction w/ elevated liver enzymes may occur
▪ Deficiency of vit. K may cause coagulation disorders, and deficiency of thiamine can cause
encephalopathy
▪ Etiology
o Unknown - reaction to fetal proteins (?)
o More common among unmarried white women, during first pregnancies, and in
multifetal pregnancies
o Other possible causes include possible allergy to fetal proteins
o Elevated levels of pregnancy-related hormones such as estrogen and beta-hCG are
considered a possible cause, as is maternal thyroid dysfunction10
▪ Therapeutic management
o Promethazine (Phenergan)
o Diphenhydramine (Benadryl)
o Histamine-receptor antagonists
o Gastric acid inhibitors
o Metoclopramide (Reglan)
o Ondansetron (Zofran)
▪ Nursing considerations
o levels of Hgb and Hct may occur as a result of dehydration
o Concentrations of sodium, potassium, and chloride may be reduced, resulting in
hypokalemia and alkalosis
o Weight loss and the presence of ketones in the urine suggest that fat stores and protein
are being metabolized to meet energy needs
o Dehydration= increased urine specific gravity ( more than 1.025)
Hypertensive Disorders of Pregnancy
▪ Gestational hypertension
o BP elevation (140/90) after 20 wks of pregnancy that is not accompanied by
proteinuria
o Must be considered a working diagnosis because it may progress to preeclampsia
o If gestational HTN persists after birth, chronic HTN is diagnosed
▪ Preeclampsia
o Systolic BP of 140 or greater or a diastolic blood pressure of 90 or greater occurring
after 20 wks of pregnancy that is accompanied by significant proteinuria (1+ urine dip, >
3+ if 24 hr. urine), & have edema
▪ Eclampsia
o Progression of preeclampsia to generalized seizures that cannot be attributed to other
causes
o Seizures may occur postpartum
▪ Chronic hypertension
o Elevated BP was known to exist before pregnancy or before 20 wks of gestation
o Unrecognized chronic HTN may not be diagnosed until well after the end of pregnancy
when the BP remains high
Hypertensive Disorders of Pregnancy: Preeclampsia
▪ Condition in which HTN develops during the last half of pregnancy in a woman who previously
had normal BP
o In addition to HTN, renal involvement may cause proteinuria
o Edema
o Only known cure is birth of the fetus
▪ Incidence and risk factors
o Affecting 5%-10% of all pregnancies
o Often associated w/ intrauterine fetal growth restriction (IUGR)
o Most likely to occur in a first pregnancy, women older than 35 years , African Americans,
those w/ a positive family history and those w/ chronic HTN or renal disease
o Women w/ diabetes or multifetal gestations are also more likely to have preeclampsia
o Presence of immunologic or genetic disorders such as lupus or clotting disorders adds to
the risk for preeclampsia11
▪ Pathophysiology (p.520*)
o Result of generalized vasospasm
▪ Preventive measures
o Prenatal care
o Attempts at prevention in women at high risk for recurrence have included low-dose
aspirin, calcium and magnesium supplements, and fish oil supplements
▪ Clinical manifestations
o Classic signs:
▪ HTN---BP should be measured uniformly at each office visit (woman seated and
her arm supported)
▪ Proteinuria can be identified by using a clean-catch specimen of urine to
prevent contamination of the specimen by vaginal secretions or blood
▪ Women w/ a UTI often have erythrocytes and leukocytes in urine, which would
elevate urine protein level in the absence of preeclampsia
▪ HA & blurred vision
o Additional signs:
▪ When retina is examined, vascular constriction and narrowing of the small
arteries are obvious in most women w/ preeclampsia
▪ Vasoconstriction that can be seen in the retina is occurring throughout the body
▪ DTRs may be very brisk (hyperreflexia)
▪ Coagulation may be impaired
▪ Therapeutic management of mild preeclampsia
▪ Inpatient management of severe preeclampsia
o Severe if systolic BP is 160 or greater, the diastolic bp is 110 or greater, or evidence of
multisystem involvement is present
▪ Ante/intra/postpartum management
o Antihypertensive meds
▪ Hydralazine
▪ Nifedipine
▪ Labetalol
o Anticonvulsant (p.523**)
▪ Magnesium sulfate (Antidote: Calcium Gluconate 1-2g)
● Adm. By IV infusion, which allows for immediate onset of action and
does not cause the discomfort associated with IM adm.
● Administered through a secondary line
● Therapeutic serum level is 4 to 8 mg/dL
▪ DTR rating scale:
● 0= reflex absent
● +1= reflex present, hypoactive
● +2= normal reflex
● +3= brisker than avg. reflex
● +4= hyperactive reflex; clonus may also be present
**Eclampsia stimulates uterine irritability
Application of the Nursing Process: Preeclampsia
▪ Assessment
o Weigh woman on admission and daily12
o Check VS and auscultate the chest at least every 4 hrs for moist breath sounds that
indicate pulmonary edema
▪ Assess location and severity of edema at least every 4 hrs
o Check urine for protein every 4 hrs, strict I/Os
o Client symptoms
o Magnesium toxicity
o Psychosocial assessment
▪ Nursing diagnoses
▪ Expected outcomes
▪ Interventions
o Monitor for signs of impending seizures:
▪ Hyperreflexia, possibly accompanied by clonus
▪ Increasing signs of cerebral irritability (headache, visual disturbances)
▪ Epigastric or right upper quadrant pain, N/V
o Monitor signs of Magnesium toxicity
▪ RR less than 12
▪ Maternal pulse ox < 95%
▪ Absence of DTR’s
▪ Sweating, flushing
▪ Altered sensorium
▪ Hypotension
▪ Serum magnesium value above the therapeutic range of 4-8mg/dL
▪ STOP MAG IF…..RR < 12, pulse <95% or DTR’s are absent
▪ Evaluation
HELLP Syndrome
o Hemolysis
▪ Believed to occur as a result of the fragmentation and distortion of erythrocytes
during passage through small damaged blood vessels
o Elevated
o Liver enzymes
▪ Liver enzymes increased when hepatic blood flow is obstructed by fibrin
deposits
▪ Hyperbilirubinemia and jaundice may occur as a result of liver impairment
o Low
o Platelets
▪ Low platelet levels are caused by vascular damage resulting from vasospasm;
platelets aggregate at sites of damage, resulting in thrombocytopenia, which
increases the risk for bleeding, usually in the liver
▪ Life-threatening
▪ Complicates about 10% of pregnancies
▪ Half of the women affected by HELLP also have severe preeclampsia, although HTN may be
present
▪ May occur during the postpartum period
▪ Symptoms
o Pain in the right upper quadrant, the lower right chest, or the midepigastric area
o May be tenderness because of liver distention13
o N/V
o Severe edema
▪ Therapeutic management
o Avoid traumatizing the liver by abdominal palpation (RUQ)
o Sudden increase in intraabdominal pressure---- could lead to rupture of a subcapsular
hematoma, resulting in internal bleeding and hypovolemic shock
o Tx: magnesium sulfate to control seizures and hydralazine to control BP
Chronic Hypertension
▪ Diagnosis
o Evidence suggests that hypertension preceded the pregnancy
o When a woman is hypertensive before 20 weeks of gestation
▪ Seen most often in older women, obese, and those w/ diabetes
▪ More common in African Americans at any age than in people of other races
▪ Therapeutic management
o Antihypertensive medications should be initiated if the diastolic pressure remains higher
than 90 in early pregnancy
o Methyldopa (aldomet) is the drug of choice because of its record of safety and
effectiveness in pregnancy
o Beta-blockers and CCB may be used if methyldopa is not effective
Incompatibility between Maternal and Fetal Blood
▪ Rh incompatibility
o Risk factors
o Pathophysiology
o Fetal/neonatal implications
▪ Kernicterus (staining of brain tissue)---leading to bilirubin encephalopathy
▪ Erythroblastosis fetalisAgglutination and hemolysis of fetal erythrocytes
resulting from incompatibility between maternal and fetal blood. In most cases,
the fetus is Rh-positive, and the mother is Rh-negative.
o Prenatal assessment/management
▪ Rh-negative women should have an indirect Coombs’ test to determine
whether they are sensitized (have developed antibodies) as a result of
previous exposure to Rh-positive blood)
● If Coombs’ test is negative, it is repeated at 28 wks of gestation to
identify if they have developed subsequent sensitization
▪ RhoGAM is administered to unsensitized Rh-negative woman at 28 wks of
gestation to prevent sensitization, which may occur from small leaks of fetal
blood across the placenta, & 72 hrs after delivery
o Postpartum management
▪ ABO incompatibility
o People with type O blood develop anti-A or anti-B antibodies naturally as a result of
exposure to antigens in the foods that they eat or to infection by gram-negative bacteria
o The antibodies may either be IgG or IgM ….IgG antibodies may cross the placental
barrier and cause hemolysis of fetal RBC’s
Chapter 26: Concurrent Disorders During Pregnancy
Diabetes Mellitus: Etiology14
▪ Complex disorder of carbohydrate metabolism caused primarily by a partial or complete lack
of insulin secretion by the beta cells of the pancreas
▪ Without insulin, glucose accumulates in the blood (hyperglycemia)
▪ Classic symptoms of diabetes
o Polydipsia -- thirst
o Polyuria-- excretion of urine
o Polyphagia -- hunger
▪ Because the body cannot metabolize glucose, it begins to metabolize protein and fat to meet
energy needs
▪ Metabolism of protein produces a negative nitrogen balance, and the metabolism of fat results
in the buildup of ketone bodies (such as acetone, acetoacetic acid, or beta hydroxybutyric acid)
or ketosis (accumulation of acids in the body)
▪ Fluctuating periods of hyper/hypoglycemia damage small blood vessels throughout the body
o Can cause serious impairment, especially in the kidneys, eyes, and heart
Diabetes Mellitus: Effect of Pregnancy on Fuel Metabolism
▪ Early pregnancy (1-20wks gestation)
o Small change in maternal metabolic need
o Insulin release in response to serum glucose levels accelerates.
o May experience hypoglycemia
o Lipogenic substance such as insulin that stimulates the production of fat ----
accumulation of fat prepares the mother for the rise in energy use by the growing fetus
during the second half of pregnancy
▪ Late pregnancy (20 -40 wks gestation)
o Fetal growth accelerates
o Rise in placental hormone levels
▪ Estrogen, progesterone, and human placental lactogen (hPL)
o Hormones create resistance to insulin.---which allows an abundant supply of glucose to
be available for the fetus
▪ However… the hormones have a diabetogenic effect in that they may leave the
woman w/ insufficient insulin and episodes of hyperglycemia
o Gluconeogenesis (formation of glycogen from noncarbohydrate sources such as
proteins and fat)
▪ Birth
o Maintenance of normal maternal glucose levels is essential during birth to reduce
neonatal hypoglycemia.
▪ Postpartum
o The need for additional insulin falls.
o Breastfeeding is encouraged.
▪ The added calorie intake by the mother helps lower the amount of insulin
needed in women with types 1 and 2 diabetes mellitus.
o The woman with gestational diabetes mellitus (GDM) usually needs no insulin after
birth.
Diabetes Mellitus: Classification
▪ Type 1
o Insulin deficient (IV insulin)
▪ Type 215
o Insulin resistant/deficient (can give oral medications for hypoglycemia)
▪ GDM
o The onset of glucose intolerance during pregnancy (A1-diet control, A2- diet & insulin)
Diabetes Mellitus: Incidence
▪ Diabetes mellitus is a common medical condition.
▪ About 90% to 95% of diagnoses are type 2----Type 1 accounts for 5% to 10% of diagnoses.
▪ Up to 10% of all pregnancies are affected by GDM.
▪ Women who have GDM in pregnancy have a 35% to 60% chance of developing diabetes in the
next 10 to 20 years.
Diabetes Mellitus: Preexisting
▪ Maternal effects
o During first trimester
▪ Hypoglycemia, hyperglycemia, ketosis
▪ Increased incidence of spontaneous abortion or major fetal malformations
o Preeclampsia is two to three times more likely to develop.
o Premature rupture of the membranes (PROM)
o Hydramnios—which may result from fetal hyperglycemia and consequent fetal diuresis,
and premature rupture of membranes, which may be caused by overdistention of the
uterus by hydramnios or a large fetus
o Macrosomia---baby weighs more than 8.8lb (4000g)
o Shoulder dystocia---delayed or difficult birth of fetal shoulders after the head is born
▪ Fetal effects
o Congenital malformation
▪ Most common major congenital malformations associated w/ preexisting
diabetes are neural tube defects, caudal regression syndrome (failure of
sacrum, lumbar spine, and lower extremities to develop), and cardiac defects
o Variations in fetal size
▪ Fetal growth is related to maternal vascular integrity
▪ Although maternal insulin does not cross the placental barrier, the fetus
produces insulin by the tenth week of gestation
▪ Fetal macrosomia results when elevated levels of blood glucose stimulate
excessive production of fetal insulin, which acts as a powerful growth hormone
(LGA)
▪ If vascular impairment occurs, placental perfusion may be decreased
▪ Small for gestational age (SGA)----likely d/t impaired placental perfusion which
decreases supplies of glucose and oxygen delivered to the fetus
● Intrauterine growth restriction (IUGR)
▪ Neonatal effects
o Hypoglycemia
▪ Neonate is at higher risk for hypoglycemia b/c fetal insulin production would
have been accelerated during pregnancy to metabolize the excessive glucose
received from the mother
▪ When the maternal glucose supply is abruptly withdrawn at birth, the level of
neonatal insulin exceeds the available glucose, and hypoglycemia develops
rapidly
o Hypocalcemia16
▪ During last half of pregnancy, large amts of calcium are transported across the
placenta from the mother to the fetus
▪ At time of birth, this transfer is abruptly stopped, leading to a dramatic decrease
in the amt of total and ionized calcium defined as a calcium concentration less
than 7 mg/dL, most often occurs within the first 3 days of life
▪ Associated w/ preterm birth and perinatal asphyxia, which are more likely to
occur w/ poor maternal glycemic control
o Hyperbilirubinemia
▪ Fetus experiencing recurrent hypoxia compensates by production of additional
erythrocytes (polycythemia) to carry oxygen supplied by the mother
▪ At birth, excess erythrocytes are broken down, which releases large amounts of
bilirubin into the neonate’s circulation
o Respiratory distress syndrome
▪ Fetal hyperinsulinemia retards cortisol production, which is necessary for the
synthesis of surfactant needed to keep the newborn’s alveoli open after birth,
thereby increasing the risk for RDS
▪ Reduced lung fluid clearance and delayed thinning of lung connective tissue may
also play a part
▪ RDS is more likely to occur if the mother’s glycemic control is poor because wide
fluctuations in her insulin and glucose levels have slowed lung maturation
Diabetes Mellitus: Maternal Assessment
▪ History
o Onset and management of diabetic condition
o May need insulin to control (no oral agent)
▪ Via injection—even if the oral agent had been effective in the woman w/ type 2
diabetes
▪ Physical exam
o Baseline electrocardiogram (ECG)
o Ophthalmology referral
o Height, weight, and blood pressure (BP)---d/t increased risk for preeclampsia
o Fundal height—noting any abnormal increase in size that may indicate macrosomia or
hydramnios, which may occur as a result of diuresis by the hyperglycemic fetus
▪ Laboratory tests
o 24 hour urine---for total protein excretion and creatinine clearance
o Urine should be checked by using a dipstick for the presence of glucose, ketones, and
protien
o Hemoglobin A1c (HbA1c)
Diabetes Mellitus: Fetal Surveillance
▪ Surveillance should begin early for women with preexisting diabetes to look at fetal well being.
▪ Testing for anomalies
▪ Frequent ultrasound
▪ Fetal echocardiogram (ECG)
▪ Fetal kick count
Diabetes Mellitus: Therapeutic Management
▪ Maintain normal blood glucose levels. (70-140)
▪ Facilitate the birth of a healthy baby.17
▪ Avoid accelerated impairment of blood vessels and other major organs.
▪ Preconception care
▪ Diet:
o 40-45% of the calories should be from carbohydrates
o 12-20% from protein
o 40% from fat
o Should be distributed among 3 meals or 2 or more snacks
o Bedtime snack should include a complex carb and a protein
▪ Self-monitoring of glucose
▪ Insulin therapy
Gestational Diabetes Mellitus: Risk Factors
▪ Overweight
▪ Maternal age older than 25 years
▪ Previous birth outcome often associated with GDM
▪ GDM in previous pregnancy
▪ History of abnormal glucose tolerance
▪ Family history of diabetes
▪ Member of a high-risk ethnic group (African American, Hispanic or Latino, American Indian,
Asian American, or pacific islanders)
Gestational Diabetes Mellitus: Screening
▪ Glucose challenge test
o Administered between 24 to 28 wks of gestation, often to both low- and high- risk
antepartum patients
o 1 hour test, 50g of oral glucose solution
▪ If blood glucose concentration is 140 mg/dL or greater, a 3 hours oral glucose
tolerance test is recommended
o If abnormal: 3 hour oral glucose tolerance test (OGTT) 100g of glucose solution
▪ Oral glucose challenge test—must fast from midnight on the day of the test—ingest 100g of
oral glucose solution--- GDM is the diagnosis if the fasting blood glucose level is abnormal or if
two or more of the following values occur on the OGTT.
o Fasting, greater than 95 mg/dL
o 1 hour, greater than 180 mg/dL
o 2 hours, greater than 155 mg/dL
o 3 hours, greater than 140 mg/dL
Gestational Diabetes Mellitus: Therapeutic Management
▪ Diet:
o Registered dietitian, registered dietary technician, or diabetes educator
o Nonobese prepregnancy weight, an average of 30 kcal/kg/day is recommended
o Obese: 25 kcal/kg/day
▪ Exercise---slowly ease into it
▪ Blood glucose monitoring ---depending on how frequent the doctor wants it
▪ Fetal surveillance
Gestational Diabetes Mellitus: Nursing Considerations
▪ Increase effective communication.
▪ Provide opportunities for control.
▪ Provide normal pregnancy care.18
Application of the Nursing Process: Pregnant Woman with Diabetes
▪ Assessment
o History
▪ Onset and management of diabetic condition
▪ May need insulin to control (no oral agent)
o Physical exam
▪ Baseline ECG
▪ Ophthalmology referral
▪ Height, weight, and BP
o Laboratory tests
▪ 24 hour urine
▪ HbA1c
▪ Intervention
o Teaching self-care skills
▪ Home blood glucose monitoring
▪ Insulin administration
● 90 degree angle
● Injected slowly
● Aspirating is not necessary
● Withdrawal needle quickly
▪ Continuous subcutaneous insulin infusion (NOT FOR GDM)
o Teaching dietary management
o Recognizing and correcting hypoglycemia and hyperglycemia
o Explaining procedures, tests, and plan of care
Cardiac Disease
▪ Plasma volume, venous return, and cardiac output all increases
▪ Heart rate and stroke volume, the components of cardiac output, increase during pregnancy
▪ Congestive heart failure condition resulting from failure of the heart to maintain adequate
circulation; characterized by weakness, dyspnea, and edema in body parts that are lower than
the heart
Cardiac Disease: Incidence (pg. 546**)
▪ Heart disease complicates about 1% of pregnancies.
▪ It remains a significant cause of maternal mortality.
▪ The two major categories of heart disease are rheumatic heart disease and congenital heart
disease.
▪ Congenital heart disease being the major cause of heart disease in a childbearing woman
▪ Third category--- mitral valve prolapse
o Common but benign condition that usually does not cause problems during pregnancy
o Myocardial infarction and conduction defects also may occur in women of childbearing
age, especially w/ the increase in obesity
▪ Cardiomyopathy--- rare and often fatal disorder of the muscle structure of the heart and may
be considered a diagnosis of exclusion
o May occur during late pregnancy to 5 months postpartum with no identifiable cause and
no known previous heart disease
o Left ventricular systolic dysfunction is demonstrated by echocardiographic criteria19
▪ CHF may be secondary to underlying heart disease or damage or may occur secondary to tx for
other conditions
▪ Risk of recurrence w/ another pregnancy is high
Cardiac Disease: Classification
▪ Rheumatic heart disease
o Sometimes follows a streptococcal pharyngitis “strep throat”
o May cause scarring of the heart valves---resulting in stenosis (narrowing) of the
openings b/w the chambers of the heart
o The mitral valve is the most common site of stenosis.
▪ Obstructs free flow of blood from the left atrium to the left ventricle
▪ LA becomes dilated and as a result, pressure in the LA, pulmonary veins, and
pulmonary capillaries is chronically elevated
o May lead to pulmonary hypertension, pulmonary edema, or congestive heart failure
o First warnings of heart failure include persistent rales at the base of the lungs, dyspnea
on exertion, cough, and hemoptysis
o Progressive edema and tachycardia are additional signs of heart failure
▪ Congenital heart disease
o Left-to-right shunt
▪ Atrial septal defect
● Pressure in the left side of the heart is higher than that in the right side
● Pulmonary HTN occasionally develops
▪ Ventricular septal defect
● Often close w/ no surgical closure needed
● Pulmonary congestion may occur
▪ Patent ductus arteriosus
● Shunt b/w the pulmonary artery and aorta
● Antibiotic prophylaxis before labor is recommended
o Right-to-left shunt
▪ Tetralogy of Fallot
● Obvious signs of heart disease: cyanosis, clubbing of the fingers
indicating proliferation of capillaries to transport blood to the
extremities; and inability to tolerate activity
▪ Eisenmenger’s syndrome
● Cyanotic heart condition that develops when pulmonary resistance
equals or exceeds systemic resistance to blood flow and a right-to-left
shunt develops
● Late surgical correction often results in the woman’s death
o Mitral valve prolapse
▪ Can be associated with ASD and Marfan syndrome ( involved weakness in
connective tissue, bones, and muscles; the vascular system is affected,
particularly the aorta )
▪ Peripartum and postpartum cardiomyopathy
o Signs & Symptoms: SOB edema, weakness, hart palp., chest pains - partial
recovery/transplant
o Readmission to the ICU
o Shows up latent pregnancy or 5 months postpartum20
Cardiac Disease: Diagnosis and Classification
▪ Assessment for specific signs and symptoms of heart disease is part of every initial prenatal visit.
▪ Signs and symptoms
o Dyspnea, syncope (fainting) with exertion
o Hemoptysis
o Paroxysmal nocturnal dyspnea
o Chest pain with exertion
o Additional signs
▪ The severity of the disease is determined by ability to endure physical activity
Cardiac Disease: Therapeutic Management (pg. 548-549)
▪ Class I or II heart disease (less severe)
o Limited activity & prevent anemia, infection, weight gain
▪ Class III or IV heart disease (more severe)
o Cardiac decompensation, CHF, bedrest
▪ Drug therapy
o Anticoagulants (Heparin/Lovenox)
▪ Heparin/Lovenox is withheld during labor and resumed 6 hours after vaginal
birth and 18 to 24 hours after cesarean birth
o Antidysrhythmics (BB & CCB)
o Antiinfectives (gentamicin, amoxicillin, penicillin)
o Drugs for heart failure
Cardiac Disease: Intrapartum Management
▪ 300 to 500 mL of blood is shifted from the uterus and placenta into the central circulation.
o Extra fluid causes a sharp rise in cardiac workload.
▪ Vaginal delivery is recommended for a woman with heart disease unless there are specific
indications for cesarean birth.
▪ Minimize maternal pushing and use of the valsalva maneuver.
▪ Limit prolonged labor.
▪ 4th stage of labor is associated w/ special risks--- after delivery of the placenta, about 500 ml of
blood is returned to the intravascular volume
Cardiac Disease: Postpartum Management
▪ Although no evidence of distress during pregnancy, labor, and childbirth, women may have
cardiac decompensation during the postpartum period
o Blood from the placenta and uterus increases the workload on the heart.
▪ Close observation for signs of infection, hemorrhage, and thromboembolism
o Conditions can act together to precipitate postpartum heart failure.
▪ Signs and symptoms of congestive heart failure include:
o Cough (frequent, productive, hemoptysis)
o Progressive dyspnea with exertion
o Orthopnea
o Pitting edema of legs and feet or generalized edema of face, hands, or sacral area
o Heart palpitations
o Progressive fatigue or syncope with exertion
o Moist rales in lower lobes, indicating pulmonary edema
Application of the Nursing Process: Pregnant Woman with Heart Disease
▪ Assessment21
o Vital signs
o Fatigue
o Signs of congestive heart failure
o Weight
o Mother’s knowledge base
▪ Intervention
o Teach about increased cardiac workload.
▪ Excessive weight gain and edema
▪ Exertion
▪ Exposure
▪ Emotional stress
o Help the family accept restrictions on activity.
o Provide postpartum care.
kidney infections can lead to preterm labor
Anemias
▪ Decline in circulating RBC mass reduces the capacity to carry oxygen to the vital organs of the
mother or the fetus
o Significant maternal anemia is associated w/ preterm birth and low birth weight
o Pregnant woman considered anemic if her Hgb level is less than 10.5 or 11
▪ Iron-deficiency anemia (Pica)
o Foods high in iron or supplements
▪ Folic acid deficiency anemia (megaloblastic)
o Folic acid—essential for cell duplication and fetal and placental growth. Also an essential
nutrient for the formation of RBCs
▪ Sickle cell disease
o Autosomal recessive genetic disorder
o Occurs when the gene for the production of hemoglobin S is inherited from both
parents
o Low oxygen concentration usually causes the sickling, with acidosis and dehydration
worsening the process
▪ Thalassemia
o Genetic disorder that involves the abnormal synthesis of alpha or beta chains of
hemoglobin
o This abnormal synthesis leads to alterations in the RBC membrane and decreased life
span of RBCs
o DO NOT give large doses of iron, they can not absorb it
Medical Conditions
▪ Immune-complex diseases
o Systemic lupus erythematosus
▪ Chronic, inflammatory, autoimmune disease that can affect any organ or system
in the body
▪ Body attacks its own tissues as it would foreign antigens that enter
o Antiphospholipid syndrome
▪ Autoimmune condition characterized by the production of antiphospholipid
antibodies combined w/ certain clinical features22
▪ unexplained fetal deaths less than 10 wks, 3+ spontaneous abortions
o Hashimoto’s thyroiditis
▪ antithyroid antibodies, causes most cases of hypothyroidism in women
▪ hypothyroidism in pregnancy increases risk for miscarriage, preterm birth, and
preeclampsia
▪ fetal developmental issues
o Rheumatoid arthritis (IMPROVES DURING PREGNANCIES)
▪ Neurologic disorders
o Seizure disorders (medication complications/stillbirths)
o Bell’s palsy (3x more likely to develop during pregnancy- increased estrogen)
▪ Sudden unilateral neuropathy of the 7th cranial nerve that causes facial paralysis
weakness of the forehead and lower face
Infections during Pregnancy: Viral
▪ Cytomegalovirus (CMV)
o Isolated from urine, saliva, blood, cervical mucus, semen, breast milk, and stool
o Transmission may occur from contamination w/ any of these fluids, although close
personal contact is required
o Seroconversion (change in blood test from negative to positive indicating development
of antibodies in response to infection or immunization)
o Polymerase chain reaction (PCR)---rapid analysis of gene sequence for in vitro diagnosis
of infections
▪ Rubella
o Caused by a virus transmitted from person to person through droplets or through direct
contract w/ articles contaminated by nasopharyngeal secretions
o Rubella virus from the mother can cross the placental barrier and infect the fetus at any
time during pregnancy
o Greatest risk to the fetus is during the first trimester, when fetal organs are developing
o Rubella titer of 1:8 or greater provides evidence of immunity
▪ Varicella-zoster
o need to not be around until completely scabbed over
▪ Herpes simplex
o No vaginal delivery (bright light exam), lesions on the baby
▪ Parvovirus B19
o Erythema infectiosum (also called fifth disease), is an acute, communicable disease
characterized by a highly distinctive rash - DEADLY TO FETUS
o “slapped –cheeks” appearance
▪ Hepatitis B---baby gets an additional injection of this after birth (12 hrs of life)
o
▪ Human immunodeficiency virus (HIV)
o No breastfeeding, remain HAART therapy compliant
o give baby AZT prophylactically
Infections during Pregnancy: Nonviral
▪ Toxoplasmosis
o Protozoan infection caused by toxoplasma gondii23
o Transmitted through organisms in raw and undercooked meat, through contact w/
infected cat feces or soil, and across the placental barrier to the fetus if the expectant
mother acquires the infection during pregnancy
▪ Group B streptococci
o Leading cause of life-threatening perinatal infections in the US, screened around 37
weeks (2 doses of IV antibiotics before delivery, or continuous if active labor) -
PROTECTS babies from meningitis, 48 hr stay
o Colonizes the rectum, vagina, cervix, and urethra of pregnant as well as nonpregnant
woman
o 15%-40% pregnant women are colonized by GBS in the vaginal or rectal area, but
isolating the organism is often possible only intermittently
▪ Tuberculosis
o Fetus has failure to thrive, enlarged spleen, lymph nodes, & liver
o Droplet transmission
o Mycobacterium tuberculosis
Chapter 27: Intrapartum Complications
Dysfunctional Labor
▪ Problems of the powers
o Ineffective contractions
▪ Maternal fatigue
▪ Maternal inactivity
▪ Fluid and electrolyte imbalance
▪ Hypoglycemia
▪ Excessive analgesia or anesthesia
▪ Maternal catecholamines secreted in response to stress or pain
▪ Disproportion b/w the maternal pelvis and fetal presenting part
▪ Uterine over distention such as w/ multiple gestation or hydramnios (excess
volume of amniotic fluid)
o Hypotonic dysfunction (secondary arrest)
▪ Contractions are coordinated but too weak to be effective –they are infrequent
and brief and can be indented easily w/ fingertip pressure at the peak
▪ Usually occurs during the active phase of labor (4-7cm)
▪ Uterine distention is associated w/ hypotonic dysfunction b/c the stretched
uterine muscle contracts poorly
▪ Tx: amniotomy, oxytocin infusion, pain management, IV fluids, maternal
position change
o Hypertonic dysfunction
▪ Less common than hypotonic and more often affects women in early labor w/
their first baby
▪ Contractions are uncoordinated and erratic in their frequency, duration, and
intensity ---contractions are painful but ineffective
▪ Usually occurs during the latent phase of labor
▪ Basal intrauterine pressure is usually high
▪ Uterine resting tone b/w contractions is higher than normal, reducing uterine
blood flow24
▪ This uterine ischemia decreases fetal oxygen supply and caused the woman to
have almost constant cramping pain
▪ Oxytocin is NOT usually given because it can intensify the already high uterine
resting tone
▪ Tocolytic drugs may be ordered to reduce uterine resting tone and improve
placental blood flow
o Ineffective maternal pushing
▪ Use on non-physiologic pushing techniques and positions
▪ Fear of injury b/c of pain and tearing sensations felt by the mother when she
pushes
▪ Decreased or absent urge to push
▪ Maternal exhaustion
▪ Analgesia or anesthesia that suppresses the woman’s urge to push
▪ Psychological unreadiness to “let go” of her baby
▪ Problems with the passenger
o Fetal size
o Fetal presentation or position
o Multifetal pregnancy
o Fetal anomalies
▪ Problems with the passenger
o Fetal size
▪ Macrosomia—infant weighs more than 8lb 13 oz (4000g) at birth
● head or shoulders may not be able to adapt to the pelvis if they are too
large (cephalopelvic disproportion)
▪ Shoulder dystocia ---urgent situation because the umbilical cord can be
compressed between the fetal body and the maternal pelvis
● Delayed or difficult birth of the shoulders may occur as they become
impacted above the maternal symphysis pubis
● After head is born, it retracts against the perineum, much like a turtle's
head drawing into its shell (“turtle sign”)
● More likely to occur when the fetus is large or the mother has diabetes,
but many cases occur in pregnancies w/ no identifiable risk factors
● Fundal pressure should be avoided so that the shoulders are not pushed
even harder against the symphysis
● Infants clavicles should be checked for crepitus, deformity, and bruising,
each of which suggests fracture
o Abnormal fetal presentation or position
▪ Rotation Abnormalities
● Persistence of the fetus in the OP or OT position can contribute to
dysfunctional labor
● These positions prevent the mechanisms of labor (cardinal movements)
from occurring normally
● Labor usually is longer and more uncomfortable when the fetus remains
in the OP or OT position.
o Intense back or leg pain that may be poorly relieved w/
analgesia makes coping w/ labor difficult for the woman25
● Maternal position changes promote fetal head rotation to the OA
position and descent-Ex:
o Hands and knees
o Side-lying
o Lunge
o Squatting
o Sitting, kneeling, or standing while leaning forward
● Upright maternal positions promote descent, which usually is
accompanied by fetal head rotation
▪ Deflexion abnormalities
● Poorly flexed fetal head presents a larger diameter to the pelvis than if
flexed with the chin on the chest
▪ Breech presentation
● Cervical dilation and effacement often are slower when the fetus is in
breech presentation because the buttocks or feet do not form a
smooth, round dilating wedge like the head
● Greatest fetal risk is that the head--- the largest fetal part--- is the last to
be born
● May experience: (even with a C-section)
o Fetal injury, particularly w/ a difficult vaginal birth
o Prolapsed umbilical cord
o Low birth weight as a result of preterm gestation, multifetal
pregnancy, or intrauterine growth restriction
o Fetal anomalies contributing to breech presentation, such as
hydrocephalus
o Complications secondary to placenta previa or cesarean birth
● Can be performed (trial of labor):
o The maternal pelvis is of normal size and shape
o The estimated fetal weight is 4.4 to 8.4 (2000 to 3800g)
o The fetus is in either frank or complete breech presentation
o Fetal head is well flexed
o Multifetal pregnancy---woman is carrying two or more fetuses
▪ May result in dysfunctional labor because of uterine overdistention, which
contributes to hypotonic dysfunction, and abnormal presentation of one or both
fetuses
▪ Greater risk for postpartum hemorrhage resulting from uterine atony because of
uterine overdistention
▪ If 3 or more fetuses are involved, the birth is almost always by cesarean section
o Fetal anomalies
▪ Hydrocephalus or a large tumor may prevent normal descent of the fetus
▪ Breech or transverse lie also are associated w/ fetal anomalies
▪ C-section is scheduled if vaginal birth is not possible or is inadvisable
▪ Problems of the passage
o Pelvis
▪ Danger of uterine rupture (tear in uterine wall) is greater with thinning of the
lower uterine segment, especially if contractions remain strong26
o Soft tissue obstructions
▪ During labor, a full bladder is a common soft tissue obstruction
▪ Encouraged to void every 1-2 hours
▪ Problems of the psyche
o Increased glucose consumption reduces the energy supply available to the contracting
uterus
o Secretion of catecholamines
o Adrenal secretion of catecholamines diverts blood supply from the uterus and placenta
to the woman’s skeletal muscles
▪ Abnormal labor duration
o Prolonged
▪ Maternal infection, intrapartum or postpartum
▪ Neonatal infection, which may be severe or fatal
▪ Maternal exhaustion
▪ Higher levels of anxiety and fear during a subsequent labor
▪ Cervical dilation should proceed--- 1.2cm/hour (nullipara) and 1.5cm/hour is the
parous woman
▪ Descend---1cm/hr in nullipara and 2cm/hr in the parous woman
o Precipitate labor
▪ Birth occurs within 3 hours of its onset
▪ Intense contractions often begin abruptly rather than gradually increasing in
frequency, duration, and intensity, as is typical of most labors
o Precipitate birth
▪ Occurs after a labor of any length, in or out of the hospital or birth center, when
a trained attendant is not present to assist
Application of the Nursing Process: Intrauterine Infection
▪ Assessment
o Fetal tachycardia (>160 bpm ); a rising baseline FHR often is the first sign of intrauterine
infection
o Maternal temperature; assess every 2-4 hours in normal labor and every 2 hours after
membranes rupture; assess hourly if elevated or other signs of infection are present
▪ Nursing diagnoses
o Risk for infection r/t presence of favorable conditions for development
▪ Expected outcomes
▪ Interventions
o Reduce risk of infection (hand hygiene, limited SVE, keep her clean)
o Identify infection
▪ Evaluation
Application of the Nursing Process: Maternal Exhaustion
▪ Assessment (ask, behavior, emotions, changes in VS)
▪ Nursing diagnoses
o Activity intolerance r/t depletion of maternal energy reserves
▪ Expected outcomes
▪ Interventions
o Conserving maternal energy (dark, quiet, calm)
o Promote coping skills, rest, nutrition/fluids27
▪ Evaluation
Premature Rupture of the Membranes (PROM)
▪ PROM--- before the onset of labor in a term (37 weeks), unknown cause- but etiology maybe a
risk
▪ PPROM--- refers to the rupture of membranes <37 wks with or without contractions (preterm)
▪ Etiology (risk that put pt. at risk)
o Chorioamnionitis (intraamniotic infection), or inflammation of the membranes, which
may be associated w/ group B streptococci, Neisseria gonorrhoeae, etc.
o Infections, possibly asymptomatic, of the vagina or cervix
o Amniotic sac w/ a weak structure
o Previous preterm birth, especially if preceded by PPROM
o Fetal abnormalities or malpresentation
o Incompetent cervix or a short cervical length
o Overdistention of the uterus
o Maternal hormonal changes
o Recent sexual intercourse
o Maternal stress or low socioeconomic status
o Maternal nutritional deficiencies
▪ Complications
o Organisms that cause chorioamnionitis weaken the amniotic membrane, leading to the
rupture--- mother is at higher risk for postpartum infection, and the newborn is
vulnerable to neonatal sepsis
o GBS is often associated w/ PPROM
o Chorioamnionitis, characterized by maternal fever and uterine tenderness is most likely
to precede preterm birth in the infant born before 34 wks of gestation
o If chorioamnionitis does not precede PROM, it is more likely to occur if a long time
elapses b/w membrane rupture and birth because vaginal organisms can readily enter
the uterus
o Membranes that rupture before term may form a seal, stopping the fluid leak and
allowing the amniotic fluid cushion to become established
o Umbilical cord compression, reduced lung volume, and deformities resulting from
compression may occur, particularly if rupture occurs near the age of fetal viability,
about 23 wks of gestation, possibly extending the duration of amniotic fluid loss
▪ Therapeutic management
o Depends on gestation. Risk for infection or preterm birth complications are weighed
against labor induction or c/sec
▪ Confirm PPROM
▪ Fetal lung maturity
▪ Cervix readiness
o Near term: if cervix is favorable and fetal lungs are mature= labor induction
▪ induction may be delayed 24 hrs if cervix is not favorable and no signs of
infection
▪ Prophylactic antibiotics given for unknown GBS
▪ May require C-section
o Preterm: risk of maternal fetal infection weighed against newborn complications due to
prematurity28
▪ Cerclage (suture encircling the cervix) may have been placed earlier in the
pregnancy to prevent premature cervical dilation
● If infection is not already present, the physician must consider whether
leaving the cerclage in place is likely in increase the risk for infection
o No signs of infection and fetal lungs are immature, then mom is admitted for
ongoing observation
1) Daily NSTs
2) BPP several times a week
3) Antibiotics and steroids given
4) Avoid delivery before 25 wks gestation
▪ Nursing considerations
o Client may be hospitalized until delivery or monitored at home after staying in hospital
few days. Teaching is crucial
▪ Avoid sexual intercourse (prostaglandin released in semen to thin uterus)
▪ Avoid breath stimulation (promotes contractions)
▪ Take temp 4 times / day (call if above 100)
▪ Follow activity restrictions
▪ Call if contracting or if foul vaginal odor noted
Preterm Labor
▪ Begins after the 20th wk but before the ends of the 37th wk of pregnancy
▪ Physical risks to the mother are no greater than labor at term unless complications such as
infection, hemorrhage, or the need for a cesarean delivery also exist
▪ Particularity if earlier than 32 wks of gestation
▪ Adverse effects of prematurely:
o Cerebral palsy
o Developmental delay
o Vision and hearing impairment
▪ Associated Factors:
o Some possible causes of preterm labor are the following:
▪ Maternal medical conditions, including infxns of the urinary tract, reproductive
organs, or system organs
▪ Conceptions enhanced by assisted reproductive technology
▪ Present and past obstetric conditions such as short cervical length
▪ Fetal conditions (IUGR-growth retardation, inadequate amniotic fluid volume,
etc)
▪ Social and environmental factors such as inadequate or absent prenatal or
dental care
▪ Demographic factors
▪ Signs and symptoms
o Uterine contractions that may/not be painful
o Sensation that the baby is frequently “balling up”
o Cramps similar to menstrual cramps
o Constant low backache; irregular or intermittent low back pain
o Sensation of pelvic pressure or a feeling that the baby is pushing down
o Pain, discomfort, or pressure in the vagina or thighs
o Change or increase in vaginal discharge29
o Sense of “just feeling bad” or “coming down w/ something”
▪ Preventing preterm birth
o Community education
o Improving access to care
o Identifying risk factors
o Promoting adequate nutrition
o Progesterone supplementation
▪ Therapeutic management
o Predicting
▪ Short cervix—which allows vaginal organisms easier access to the uterus, where
they weaken the membranes and cause premature rupture
▪ Previous PPROM
▪ Fetal fibronectin: protein present in fetal tissues
● Normally found in cervical and vaginal secretions until 16-20 wks of
gestation and again at or near term
● If it appears too early, it suggests that labor may begin early
▪ Infections
o Identifying preterm labor
▪ Frequent prenatal visits
o Stopping
▪ Management focuses on stopping uterine activity before the point of no
return—usually after about 3-cm dilation
▪ Tocolytics (terbutaline/brethine) given SubQ
● Goes home on
▪ If still contracting give mag sulfate 1-2 grams loading dose and given for 24
hours (no longer than 2 weeks)
▪ If doesn't work then deliver in 24 hours after betamethasone given then get in
trendelenburg position
o Accelerating fetal lung maturity
▪ Physician may order corticosteroids to speed fetal lung maturation if birth
before 34 wks seems inevitable
▪ Adm the steroid as late as 37 wks of gestation may be chosen if fetal lung
maturity studies demonstrate immature lungs later than 34 wks
▪ Betamethasone or dexamethasone may be used!!
Application of the Nursing Process: Preterm Labor
▪ Psychosocial concerns
o Assessment
o Nursing diagnoses
o Expected outcomes
o Interventions
o Evaluation
▪ Home care
o Assessment
▪ Compliance
▪ Activity around the house
▪ Who's there hindering or helping?30
▪ bed rest w/ bathroom privileges
o Nursing diagnoses
o Expected outcomes
o Interventions
o Evaluation
▪ Boredom
o Assessment
o Nursing diagnoses
o Expected outcomes
o Interventions
o Evaluation
Tocolytics
● Magnesium sulfate, Nifedipine, terbutaline, corticosteroids (betamethasone, dexamethasone)
● Dosage/Route/indications
o Magnesium sulfate:
▪ IV loading dose, 4-6g over 30 minutes, maintenance dose 1-4g
▪ Indications: inhibit preterm labor b/c added effect of quieting uterine activity,
anticonvulsant, smooth muscle relaxer
o Nifedipine (calcium channel blocker):
▪ PO, 10-20mg, Q3-6Hrs, long acting formulations 30-60mg Q8-12Hrs
▪ Indications: block calcium reduces muscular contractions
o Terbutaline:
▪ Don’t use beyond 48-72 hours, IV, 0.01-0.05mg, increase 0.01 at 10-30min until
max dose 0.08 reached, SubQ intermittent injections 0.25mg Q4 Hrs makes
mom really crabby and increased her HR
▪ Indications: stimulates uterine contractions
Prolonged Pregnancy----anything greater than 42 wks
▪ Complications
o Insufficiency of the placental function secondary to aging and infarction reduces transfer
of oxygen and nutrients to the fetus and removal of waste
▪ Therapeutic management
▪ Nursing considerations
o Late decelerations & variables on FHR monitor, meconium delivery most likely
Intrapartum Emergencies
▪ Placental abnormalities
o Placenta previa—abnormal implantation of the placenta in lower uterus
o Placenta accreta—abnormally adherent placenta into the muscle
▪ Strongest risk for placenta accreta is prior uterine surgery, usually 1 or more
cesarean births
▪ May cause immediate intrapartum hemorrhage
o Placenta increta---placenta penetrates into uterine muscle itself
o Placenta percreta --- placenta penetrates all the way through the uterus31
▪ Prolapsed umbilical cord---slips downward after the membranes rupture, subjecting it to
compression b/w the fetus and pelvis
o More likely if:
▪ Fetus remains at a high station
▪ Very small fetus
▪ Breech presentation
▪ Transverse lie
▪ Hydramnios
o Signs of prolapse:
▪ May not be visible but may be palpated on vaginal examination as it pulsates
synchronously w/ the fetal heart
● Occult prolapse: one in which the cord slips alongside the fetal head or
shoulders
o Prolapse cannot be palpated or seen but is suspected b/c of the
changes in the FHR, such as sustained bradycardia or variable
decelerations
o Priority: relieve pressure on the cord to improve blood flow through it until delivery
and prompt delivery, push the call light to summon help, others should call the
physician and prepare for birth while the nurse caring for the woman relieves pressure
on the cord (Trendelenburg)
o Emergency interventions:
▪ Position the woman’s hips higher than her head to shift the fetal presenting part
toward her diaphragm using either knee-chest, trendelenburg position or hips
elevated with pillows with side lying position maintained
▪ Maintain vaginal elevation of the presenting part using a gloved hand while the
woman is transferred to the OR until the physician orders cessation of vaginal
elevation
▪ Avoid or minimize manual palpation or handling of the cord as much as possible
to minimize cord vessel vasospasm
▪ Ultrasound exam may be used to confirm presence of fetal heart activity before
C-section
▪ Give the woman 8-10 liters per min by face mask to increase maternal blood
oxygen saturation making more available for the fetus
▪ Uterine rupture
o Complete rupture--- direct communication b/w the uterine and peritoneal cavities
o Incomplete rupture---rupture into the peritoneum covering the uterus or into the broad
ligament but not the peritoneal cavity
o Dehiscence –partial separation of an old uterine scar. Little or no bleeding may occur
o Possible signs and symptoms:
▪ Abdominal pain and tenderness
▪ Chest pain
▪ Hypovolemic shock
▪ Signs associated w/ impaired fetal oxygenation
▪ Absent fetal heart sounds32
▪ Cessation of uterine contractions
▪ Palpation of the fetus outside the uterus
▪ Uterine inversion
o Occurs when the uterus completely or partly turns inside out, usually during the 3rd
stage of labor
o Causes:
▪ Pulling on umbilical cord before the placenta detached from the uterine wall
spontaneously
▪ Fundal pressure during birth
▪ Fundal pressure on an incompletely contracted uterus after birth
▪ Increased intraabdominal pressure
▪ An abnormally adherent placenta
▪ Congenital weakness of the uterine wall
▪ Fundal placenta implantation
o Management:
▪ Physician tries to replace the uterus through the vagina into a normal position…
if that is not possible, a laparotomy is used to replace the uterus
▪ Anaphylactoid syndrome
o Often called amniotic fluid embolism
o Occurs when the amniotic fluid is drawn into the maternal circulation and carried to the
woman’s lungs
▪ Trauma
o Decrease to lower levels of maternal fibrinogen is associated with abruptio placentae
Application of the Nursing Process: Intrapartum Emergencies
▪ Assessment
▪ Nursing diagnoses
▪ Expected outcomes
▪ Interventions
▪ Evaluation
Chapter 28: Postpartum Maternal Complications
Postpartum Hemorrhage
blood loss of more than 500 ml after vag birth or 1000 ml after cesarean birth, a decrease in hct of
10% or more since admission or the need for a blood transfusion & continued bleeding even with the
“usual treatment”
▪ Early postpartum hemorrhage (within the 1st 24 hours)—complicates 1-5% of births
1) Uterine atony
▪ Relaxed uterine muscles
▪ Atony refers to lack of muscle tone that results in failure of the uterine muscle
fibers to contract firmly around blood vessels when the placenta separates
▪ Bleeding continues until the uterine muscle fibers contract to stop the flow of
blood
▪ Methergine and hemabate may be given IM to help with uterine atony
● Do not give methergine to somebody with high blood pressure
▪ Hysterectomy is the last resort to save the life of a woman w/ uncontrollable
postpartum hemorrhage33
2) Trauma
▪ Includes vaginal, cervical, or perineal lacerations and hematomas
▪ Late postpartum hemorrhage (AKA secondary postpartum hemorrhage) (greater than 24 hrs
and up to 6-12wks after birth)
o Subinvolution
▪ Delayed return of the uterus to its nonpregnant size and consistency
o Retained placental fragments
▪ That remain attached to the myometrium when the placenta is delivered
▪ Clots form around the retained fragments, and excessive bleeding can occur
when the clots slough away several days after delivery
▪ If bleeding continues or recurs, dilation and curettage (stretching of the cervical
os to permit suctioning or scraping of the walls of the uterus) may be necessary
to remove fragments
Placenta accreta= Abnormal adherence of the placenta to the uterine wall
Meds to give for postpartum hemorrhage:
1) Pitocin
2) Methergine –don’t give w/ history of high BP
3) Hemabate –don’t give w/ history of asthma
4) Cytotec
Hypovolemic Shock
▪ Acute peripheral circulatory failure resulting from loss of circulating blood volume
▪ If hematocrit is lower after delivery, the woman lost the amt of blood added during pregnancy
and an additional 500ml for each 3% drop in the Hct value
▪ Pathophysiology
o As shock worsens, the compensatory mechanisms fail and physiologic insults spiral
o Inadequate organ perfusion and decreased cellular oxygen for metabolism result in a
buildup of lactic acid and the development of metabolic acidosis
o Acidosis results in vasodilation, which further increases bleeding
▪ Clinical signs and symptoms
o Tachycardia ---body trying to compensate for the blood loss (may not appear until 20-
25% of the woman’s blood volume has been lost)
o Decrease in BP and narrowing of pulse pressure occur when the circulating volume of
blood is sufficiently decreased
o RR increases
o Skin changes – vasoconstriction causes it to become pale and cool to the touch
o As shock progresses, changes also occur in the CNS--- mother becomes anxious, then
confused, and finally lethargic as blood loss increases
o Urine output decreases and eventually stops
▪ Therapeutic management
o Control the bleeding is the main focus
o Second IV line w/ a large bore catheter capable of carrying whole blood
o May need to give vasopressors to bring BP back up34
o VS about every 3 minutes
o Oxygen
o Check fundus and bleeding
▪ Nursing considerations
Application of the Nursing Process: Woman with Excessive Bleeding
▪ Assessment
o Uterine atony or trauma
o Weigh pads--- 1 gram = 1mL
▪ Nursing diagnoses
▪ Expected outcomes
▪ Intervention
o Prevent hemorrhage
o Collaborating w/ the health care provider
o Providing support for the family
o Posthemorrhagic care
o Home care
▪ Evaluation
Subinvolution of the Uterus
▪ Definition
o Slower-than-expected return of the uterus to its nonpregnant size after childbirth
▪ The endometrial lining has sloughed off as part of the lochia, and the site of placental
attachment is well healed by 6 wks after childbirth if involution progresses as expected
▪ Causes
o Retained placental fragments
o Pelvic infection
▪ Signs of subinvolution:
o Prolonged discharge of lochia
o Irregular or excessive uterine bleeding
o Profuse hemorrhage
o Pelvic or fundal pain
o Backache
o Feelings of pelvic pressure or fullness
▪ Therapeutic management
o Give Methergine (PO) and an antibiotic
▪ Nursing considerations
o Demonstrate how to locate and palpate the fundus and how to estimate fundal height
in relation to the umbilicus
o Uterus should become smaller each day
o Instruct mother to report any deviation from the expected pattern or duration of lochia
Thromboembolic Disorders
▪ Thrombus—collection of blood factors, primarily platelets and fibrin, on a vessel wall
▪ Thrombophlebitis--- occurs when the vessel wall develops an inflammatory response to the
thrombus—this further occludes the vessel
▪ Embolus--- mass that may be composed of a thrombus or amniotic fluid released into the
bloodstream that may cause obstruction of capillary beds in another part of the body,
frequently the lungs35
▪ Pulmonary embolus—potentially fatal complication that occurs when the pulmonary artery is
obstructed by a blood clot that was swept into circulation from a vein or by amniotic fluid
▪ Three most common thromboembolic disorders encountered during pregnancy and the
postpartum period are SVT (confined to the lower legs), DVT and occasionally pulmonary
embolism
▪ Incidence and etiology
o Leading cause of maternal mortality
o 3 major causes of thrombosis are venous stasis, hypercoagulable blood, and injury to
the endothelial surface (innermost layer) of the blood vessel
o Venous stasis and hypercoagulable blood are present in all pregnancies
o Blood vessel injury is likely to occur during birth
▪ Venous stasis
● During pregnancy, compression of the large vessels of the legs and
pelvis by the enlarging uterus causes venous stasis
● Most pronounced when the pregnant woman stands for prolonged
periods of time---which increases the potential for continued pooling of
blood postpartum
▪ Hypercoagulation
● During pregnancy the levels of many coagulation factors are elevated
● The fibrinolytic system, which causes clots to disintegrate (lyse), is
suppressed
● Result: factors that promote clot formation are increased and factors
that prevent clot formation are decreased to prevent maternal
hemorrhage, resulting in a higher risk for thrombus formation during
pregnancy and the postpartum period
▪ Blood vessel injury
● Lower extremity trauma, operative delivery, and prolonged labor can
cause vascular damage
● C-section significantly increases the risk for thromboembolic disease
▪ Additional predisposing factors
Superficial Venous Thrombosis
▪ Clinical signs and symptoms
o Most often associated w/ varicose veins and limited to the calf area
o Can also occur in the arms as a result of IV therapy
o Swelling of the involved extremity
o Redness, tenderness and warmth
o May be possible to palpate an enlarged, hardened, cordlike vein
▪ Therapeutic management
o Analgesics
o Rest
o Elastic stockings
o Elevation of lower extremities
Deep Venous Thrombosis
▪ Signs and symptoms
o Swelling in one leg over the other—typically the left leg
o May report pain in the leg, groin, lower back or right lower quadrant36
o Erythema, heat, and tenderness over the affected area are the most common signs
o Positive Homan’s sign
▪ Diagnosis
o Doppler
o Magnetic resonance imaging (MRI)
▪ Therapeutic management
o Prevention of thrombus formation
o Heparin or lovenox
o 36 wks gestation--- switch from lovenox back to heparin
o 24 hrs after last dose of heparin—and epidural can be given
▪ Resumed 6-12 hrs after birth
o Encourage early ambulation
o Compression socks
o Coumadin may come in postpartum period
▪ Coumadin is started before heparin is stopped to provide continuous
anticoagulation
o Pg.607 (be familiar with initial treatment and subsequent treatment)
o Treatment can continue up to 6 months after birth
Application of the Nursing Process: Deep Venous Thrombosis
▪ Assessment
o Usually unilateral
o Mark and measure affected leg
o Assess leg pain
o Evaluate her labs
o Warmth and redness indicates inflammation
o Coolness or cyanosis indicates venous obstruction
▪ Nursing diagnoses
▪ Expected outcomes
▪ Intervention
o Monitor signs of bleeding
o Explain continued therapy
o Help the family adapt to home care
▪ Evaluation
Pulmonary Embolism
▪ Pathophysiology
o Serious complication of DVT and a leading cause of maternal mortality
o 70% of patients w/ PE also have symptoms of DVT
o PE occurs when fragments of a blood clot dislodge and are carried to the lungs
o Embolus can also consist of amniotic fluid and its debris, condition called anaphylactoid
syndrome
o Embolus lodges in a vessel and partially or completely obstructs the flow of blood into
the lungs
o Death may occur is pulmonary circulation is severely compromised
▪ Clinical signs and symptoms
o Dyspnea, chest pain, tachycardia, and tachypnea
o Pulmonary rales, cough37
o Hemoptysis (expectoration of blood or bloody sputum)
o Abdominal pain
o Low-grade fever
o Syncope is uncommon and may indicate massive emboli
▪ Therapeutic management
o Tx is aimed at dissolving the clot and maintaining pulmonary circulation
o Oxygen is used to decrease hypoxia, and narcotic analgesics are given to reduce pain
and apprehension
o Be rest w/ head of bed elevated is used to help reduce dyspnea
o Heparin therapy is initiated and is continues throughout pregnancy if the embolism
occurs prior to birth
o Dopamine may be used to support falling BP
o Streptokinase, urokinase, or tissue-type plasminogen activator, may be used for lifethreatening pulmonary emboli but are associated w/ bleeding
▪ Nursing considerations
o Monitoring for signs
o Facilitating oxygenation
o Seeking assistance
Puerperal Infection
▪ Definition
o Temperature of 38° C (100.4° F) or higher after the first 24 hours and occurring on at
least 2 of the first 10 days following childbirth
o Bacterial infections after childbirth
▪ Causes:
o Endometritis (infection of inner lining of the uterus)
o Wound infections
o UTI
o Mastitis
o Septic pelvic thrombophlebitis
o Endomyometritis—infection of the muscle and inner lining of the uterus
▪ Effects
▪ Risk factors (table 28-2)
Endometritis
▪ Infection of the inner lining of the uterus
▪ Etiology
o Occurs in 1-3% of women following vaginal birth and 5-15% of women after scheduled
c-section
o Of extended labor and rupture of membranes precede c-section birth, infection occurs
in 30% to 35% of women who have no prophylactic antibiotics and 15% to 20% of those
who receive prophylactic antibiotics
▪ Clinical signs and symptoms
o Looks “sick”
o Temp of 38 (100.4) or higher within 36 hours of birth, chills, malaise, anorexia,
abdominal pain and cramping, uterine tenderness and purulent, foul-smelling lochia
o Tachycardia, and subinvolution
o Usually occur within the 36 hours after birth38
▪ Therapeutic management
o Broad spectrum antibiotics (IV)
▪ Cephalosporins, clindamycin plus gentamicin, or ampicillin plus aminoglycoside
▪ Metronidazole w/ penicillin may also be given
o Antibiotics are continues until the woman has been afebrile and asymptomatic for
about 24 hours
o To decrease the incidence of endometritis and wound infections, many physicians give a
single prophylactic IV dose of an antibiotic to any woman who is having a c-section or
who is at an increased risk for infection
▪ Complications
o May affect the fallopian tubes (salpingitis) or the ovaries (oophoritis)
o Peritonitis (inflammation of the membrane lining the walls of the abdominal and pelvic
cavities) may occur and lead to formation of a pelvic abscess
▪ Nursing considerations
o Place women in fowlers position to promote drainage of lochia
o Assess vital signs every 2 hours while fever is present and every 4 hours afterward
o Foods high in Vit. C and protein to aid healing
Wound Infection
▪ Approximately 3% to 5% of c-sections sites become infected
▪ Risk factors:
o Obesity
o Diabetes
o Hemorrhage
o Anemia
o Chorioamnionitis
o Corticosteroid therapy
o Multiple vaginal examinations
▪ Clinical signs and symptoms
o Edema
o Warmth
o Redness
o Tenderness and pain
o Edges of wound may pull apart and seropurulent drainage may be present
▪ Therapeutic management
o Culture the wound—would may need to be debrided
o Broad spectrum antibiotics
o Incision and drainage of the affected area may be necessary
o Analgesics are often necessary, and warm compresses or sitz baths may be used to
provide comfort and to promote healing by increasing circulation to the area
▪ Nursing consideration
Urinary Tract Infections
▪ Etiology
o Bladder and urethra are traumatized by pressure during childbirth, from the descending
fetus
o Most often caused by coliform bacteria, such as E.coli
▪ Clinical signs and symptoms39
o Typically begin on the first or second postpartum day
o Dysuria
o Urgency
o Frequency
o Suprapubic pain
o Chills
o Spiking fever
o Costovertebral angle tenderness
o Flank pain
o n/v
▪ Therapeutic management
▪ Nursing considerations
o Take medication for the entire time
o Drink at least 2500 to 3000ml of fluid each day to help dilute the bacterial count and
flush the infection from the bladder
Mastitis
▪ Etiology
o Infection of the breast---occurs most often 2-4 wks after childbirth
o 2%–10% of lactating women are affected
o Usually affects only one breast
o Often caused by Staph aureus, E. coli or streptococci
▪ Clinical signs and symptoms
o Initial symptoms may be flu-like w/ fatigue and aching muscles
o Temp of 39 C (102.2F) or higher
o Chills
o Malaise and headache
o Localized lump or wedge-shaped area of pain
o Redness, heat, inflammation, and enlarged axillary lymph nodes
o Hard, tender area may be palpated
▪ Therapeutic management
o With early antibiotic tx, mastitis usually resolves within 24 to 48 hours
o Antibiotics should be continued for a full 7 days
o 10% of women with mastitis develop a breast abscess
o Application of moist heat or ice packs, breast support, bed rest, fluids, analgesics
o Continue to breastfeed from both breasts----regular and through emptying of the breast
is important in preventing abscess formation
▪ Nursing considerations
Septic Pelvic Thrombophlebitis
▪ Incidence and etiology:
o usually not seen until 2-4 days after childbirth
o occurs when infection spreads along the venous system and thrombophlebitis develops
o develops more often in women w/ wound infection and usually involves one or both
ovarian veins, called ovarian vein syndrome
▪ Clinical signs and symptoms
o Pain in the groin, abdomen, or flank
o Fever40
o Tachycardia
o N/V
o Bloating
o GI distress and decreased bowel sounds
▪ Therapeutic management
o Readmission to the hospital is usually necessary
o Anticoagulation therapy w/ IV heparin and IV antibiotics
o Warfarin may be given when heparin is discontinued
o Improvement usually occurs within 2-3 days of anticoagulation therapy
Application of the Nursing Process: Infection
▪ Assessment
o Assess for fever, tachycardia, pain or unusual amount, color, or odor of lochia
o Generalized symptoms of malaise and muscle aching may also be significant
o Examine all wounds each shift for signs of localized infection
▪ Redness, edema, tenderness, discharge, or pulling apart of incisions or sutured
lacerations
▪ Nursing diagnoses
▪ Expected outcomes
▪ Interventions
o Preventing infection
▪ Promoting hygiene
▪ Preventing urinary stasis
▪ Teaching breastfeeding techniques
▪ Providing information
▪ Evaluations
Postpartum Mood Disorders
▪ Postpartum depression (onset during pregnancy, or within 4 wks after childbirth that lasts at
least 2wks)
▪ Changed in appetite or weight, sleep, and psychomotor activity; decreased
energy; feelings of worthlessness or guilt; difficulty thinking, concentrating or
making decisions; recurrent thoughts of death of suicide; or death or suicide
plans or attempts
o Incidence
▪ Affecting 10-15% of postpartum women
▪ Usually develops during the first 3 months but may occur at any time during the
first year postpartum
o Predictors (pg. 616 Box 28-3)
▪ More likely to occur in primigravidas but can develop after any pregnancy
▪ Cause is unknown
o Clinical signs and symptoms
▪ Depressed mood w/ loss of interest in her usual activities and a loss of her usual
emotional response toward her family
▪ Sees the infant as demanding and herself as inept at mothering
▪ Anxiety
▪ Unworthiness
▪ Guild41
▪ Agitation and shame
o Impact on the family
o Therapeutic management
o Cultural aspects
Application of the Nursing Process: Postpartum Depression
▪ Assessment
▪ Nursing diagnoses
▪ Expected outcomes
▪ Interventions
▪ Evaluations
Postpartum Mood Disorders (Cont.)
▪ Bipolar II disorder
▪ Postpartum psychosis
Postpartum Anxiety Disorders
▪ Panic disorder
▪ Postpartum obsessive compulsive disorder
▪ Post-traumatic stress disorder
Chapter 29: High-Risk Newborn: Complications Associated with Gestational Age and Development
Care of High-Risk Newborns
▪ Multidisciplinary approach
▪ Case management and clinical pathways
Late Preterm Infants
▪ Infants born between 34 0/7 and 36 6/7 weeks of gestation
▪ Incidence and etiology
▪ Characteristics of late preterm infants
o Appearance
o Behavior
Late Preterm Infants: Assessment and Care of Common Problems
▪ Thermoregulation
o VS should be checked every 3-4 hours for the first 24 hours and then every shift,
depending on need and agency policy
o Kangaroo care---a method of providing skin to skin contact between infants and their
parents, is often used to keep infants warm
▪ Feedings
o Are at risk for hypoglycemia, and blood glucose measurements should be performed
according to hospital protocol, especially during the first 24 hours
o Supplemental feedings by bottle, gavage, or use of a supplemental nursing system may
be necessary if the infant's weight loss is greater than 10% total or more than 3% per
day
▪ Discharge
o Should not be discharged earlier than 48 hrs after birth
o Must have had normal VS for at least 24 hours before discharge
o Bilirubin levels should also be assessed before
Preterm Infants
▪ Born before the beginning of the 38th week of gestation42
▪ Low birth weight--- 5lb 8 oz or less
▪ Very- low birth weight---3lb 5 oz or less at birth
▪ Extremely low birth weight---infants weigh 2lb 3 oz or less
▪ Incidence and etiology
▪ Causes
▪ Prevention
o Provision of adequate prenatal care for every pregnant woman to identify and treat risk
factors as early as possible
▪ Characteristics of preterm infants
Preterm Infants: Assessment and Care of Common Problems
▪ Respiration
o Assessment
o Nursing interventions
▪ Working with equipment
▪ Positioning
▪ Suctioning
▪ Hydration
▪ Problems with thermoregulation
o Assessment
▪ Abdominal skin temp is usually maintained at 96.8 to 97.7 (36 to 36.5)
▪ Temp should be recorded every 30-60 minutes initially and every 1-3 hours
when infant is stable
o Nursing interventions
▪ Neutral thermal environment
▪ Weaning to open crib
▪ Problems with fluid and electrolyte balance
o Assessment
o Nursing interventions
▪ Problems with the skin
▪ Problems with infection
▪ Problems with pain
Application of the Nursing Process: Preterm Infant
▪ Environmentally caused stress
o Assessment
o Nursing diagnosis
o Expected outcomes
o Interventions
o Evaluation
▪ Nutrition
o Assessment
o Nursing diagnoses
o Expected outcomes
o Interventions
▪ Parenteral feedings
▪ Enteral feedings
▪ Gavage feedings43
▪ Oral feedings
▪ Facilitate breastfeeding
o Evaluation
▪ Parenting
o Assessment
▪ Attachment
▪ Bonding
o Analysis
o Planning
▪ Parenting
o Interventions
▪ Advanced preparations
▪ Assist at birth
▪ Support
▪ Information
▪ Kangaroo care
o Evaluation
▪ Interaction
▪ Increase decision making
▪ Alleviate concerns
▪ Ongoing problems
▪ Discharge
Respiratory Distress Syndrome
▪ Caused by insufficient production of surfactant in the lungs
▪ Most often occurs in preterm infants under 28 wks of gestation and increases as the gestation
age decreases
▪ Occurs in birth asphyxia, c-section, multiple births, male gender, cold stress, and maternal
diabetes b/c these conditions interfere w/ surfactant production
▪ Pathophysiology
o Enough surfactant is usually produced beginning at 34 wks to 36 wks of gestation to
prevent RDS
o As fewer alveoli expand, atelectasis, hypoxia, and hypercapnia (increased carbon
dioxide) occur
o Causes pulmonary vasoconstriction and decreased blood flow to the lungs b/c of high
resistance within the pulmonary blood vessels
▪ Manifestations
o Tachypnea
o Tachycardia
o Nasal flaring
o Xiphoid and intercostal retractions
o Cyanosis
o Audible grunting on expiration
o Acidosis develops as a result of hypoxemia
o “ground glass” appearance of the lungs
o Areas of atelectasis are present
▪ Therapeutic management44
o Surfactant is instilled into the infant's trachea shortly after birth or as soon as signs of
RDS become apparent
▪ Nursing considerations
Bronchopulmonary Dysplasia---AKA as chronic lung disease
▪ Chronic condition in which damage to the infant’s lungs requires prolonged dependence on
supplemental oxygen.
▪ Occurs most often in infants less than 32 wks gestational age and in one third of VLBW infants
▪ Infants generally continue to require oxygen at 36 wks postmenstrual age or at 28 days after
birth
▪ Pathophysiology
o BPD results from a combination of factors such as high levels of oxygen, oxygen free
radicals and pressure of mechanical ventilation that injure bronchial epithelium and
interfere w/ alveolar development
o Result is inflammation, atelectasis, edema, and airway hyperreactivity w/ loss of cilia,
thickening of the walls of the alveoli, and fibrotic changes
▪ Manifestations
o Increased need for or an inability to be weaned from resp support and oxygen
o Tachycardia
o Tachypnea
o Retractions
o Crackles
o Wheezing
o Resp. acidosis
o Cyanosis
o Increased secretions
o Bronchospasm
o Pulmonary edema may occur
▪ Therapeutic management
o Prevention includes use of maternal steroids to reduce prematurity and RDS, minimizing
exposure to oxygen and pressure w/ ventilation as much as possible, avoidance of fluid
overload, and increased nutrition
o Tx is supportive, w/ antibiotics and bronchodilators are necessary, and gradual
decreases in the amount of oxygen
o Diuretics are given and fluids are restricted as infants are prone to fluid overload
o Increased calories and protein are important
Intraventricular Hemorrhage---AKA germinal matrix hemorrhage and periventricular- intraventricular
hemorrhage
▪ Bleeding into and around the ventricles of the brain
▪ Approx.. 30% of preterm infants weighing less than 1500 g develop intraventricular hemorrhage
▪ First few days days of life are the most common times for hemorrhage to occur
▪ Pathophysiology
o Results from rupture of the fragile blood vessels in the germinal matrix, located around
the ventricles of the brain
o Associated w/ increased or decreased BP, asphyxia or resp. distress requiring
mechanical ventilation, and increased or fluctuating cerebral blood flow45
o Rapid blood volume expansion, hypercarbia, anemia, and hypoglycemia are other
causes
o Hemorrhage is graded 1 through 4
o 1= very small bleed at the germinal matrix, producing few if any clinical changes
o 2= hemorrhage extends into the lateral ventricles
o 3= causes distention on ventricles
o 4= causes ventricular dilation and extends into surrounding brain tissue
o Condition is diagnosed by cranial ultrasound through the anterior fontanel
▪ Manifestations
o Determined by the severity of the hemorrhage
o May have no signs or lethargy, poor muscle tone, deterioration of respiratory status w.
cyanosis or apnea, drop in hct, acidosis, hyperglycemia, decreased reflexed, tense
fontanel and seizures
o Mild aberrations of eye position or movement may occur
▪ Therapeutic management
o Tx is supportive and focuses on maintaining respiratory function and dealing w/ other
complications
o Hydrocephalus may develop from blockage of cerebrospinal fluid flow
o Ventriculoperitoneal shunt may be necessary to drain the fluid
▪ Nursing considerations
Retinopathy of Prematurity
▪ Injury to the blood vessels in the eye --May result in visual impairment or blindness in preterm
infants
▪ Occurs more often in preterm infants weighing less than 1000g and less than 29 wks of
gestational age
▪ Pathophysiology
o Exact cause is unknown
o High level of oxygen is a risk factor.
o Immature blood vessels in the eye are injured
▪ Therapeutic management
o Laser surgery to destroy abnormal blood vessels is the current treatment of choice
o Intravitreal bevacizumab has been used in some cases and will have more study to
determine its use in the future
o Cryosurgery or reattachment of the retina also may be necessary
▪ Nursing considerations
o Mydriatic eye drops given to dilate the eyes may cause HTN, bradycardia, and apnea
o Ice packs may be used for edema, and pain medication should be given
Necrotizing Enterocolitis
▪ Serious inflammatory condition of the intestinal tract that may lead to cellular death of areas
of intestinal mucosa
▪ Occurs in 1-5% of infants admitted to NICUs
▪ Ileum and proximal colon are the area’s most often affected
▪ Pathophysiology
o Exact cause is unknown
o Rate of NEC increases with decreasing gestational age
o Previous hypoxia of the intestines may be a causative factor46
o Incidence of NEC is much higher after infants have received feedings
▪ Manifestations
o Increased abdominal girth caused by distention
o Increased gastric residuals
o Decreased or absent bowel sounds
o Loops of bowel seen through the abdominal wall
o Vomiting
o Bile-stained residuals or emesis
o Abdominal tenderness
o Signs of infection
o Occult blood in the stools
o Resp difficulty may occur because of pressure from the distended abdomen on the
diaphragm
o Apnea, bradycardia, temp instability, lethargy, hypotension, and shock also may be
present
o Presence of air within the intestinal wall is characteristic of the condition
▪ Therapeutic management
o Mothers should be encourage to breastfeed
o Tx includes antibiotics, discontinuation of oral feedings, continuous or intermittent
gastric suction, and use of parenteral nutrition to rest the intestines
o Surgery may be necessary if perforation or continued lack of improvement occurs
o Necrotic area is removed and an ostomy may be performed
Short Bowel Syndrome
▪ A bowel that is shorter than normal---Caused by congenital malformations or surgical
resection
▪ Pathophysiology
o Decreased mucosal surface area causes inadequate absorption of fluids, electrolytes,
and nutrients
o Loss of greater than 50% of the small bowel may result in symptoms of generalized
malabsorption or deficiencies of certain nutrients related to the region of bowel that
have been removed
▪ Manifestations
o Malabsorption
o Diarrhea
o Failure to thrive
o If the small bowel is 40 cm or more, malabsorption may improve in time because the
remaining bowel continues to grow and adapt in function
▪ Therapeutic management
o TPN is begun as the primary source of nutrition
o Formulated to meet the child’s nutritional needs as well as promote weight gain and
growth
o Enteral nutrition is begun as soon as possible following surgery to allow the intestines to
adapt to food
Post-Term Infants
▪ Born after the 42nd week of gestation
▪ Scope of the problem47
o Postmaturity syndrome (dysmaturity syndrome) ---hypoxia and malnourishment in the
fetus
▪ Assessment
o May have an apprehensive look associated w/ hypoxia
o Infant may be thin with loose skin and little subq fat
o Little or no vernix caseosa, but infant generally has abundant hair on the head and long
nails
o Skin is wrinkled, cracked, and peeling
▪ Therapeutic management
o Apgar scores less than 7 are more likely in postterm infants
o In cases of asphyxia or meconium aspiration, respiratory support is needed at birth
▪ Nursing considerations
Small-for-Gestational Age Infants
▪ Those who fall below the tenth percentile in size on growth charts
▪ May be preterm, full-term, or postterm
▪ Approx. 1/3 of all low-birth-weight infants are SGA
▪ Causes
o Congenital malformations
o Chromosomal anomalies
o Genetic factors
o Multiple gestations
o Fetal infections such as rubles or cytomegalovirus may cause FGR
▪ Scope of problem
o Low apgar scores, meconium aspiration, and polycythemia are increased in the SGA
infant
o Hypoglycemia is common because of inadequate storage of glycogen in the liver
o SGA infants are prone to inadequate thermoregulation because subq white fat and
brown fat stores have been used to survive in utero
▪ Characteristics
o Approximately 20% of SGA infants have symmetric growth restriction
o Abdominal circumference is decreased because the liver, spleen, and adrenals are
smaller than normal
o Infant appears long, thin, and wasted
o Facial appearance of being elderly
▪ Therapeutic management
▪ Nursing considerations
Large-for-Gestational Age Infants
▪ Infants who are above the 90th percentile for gestational age on intrauterine growth charts
▪ May have macrosomia (weigh more than 8 lb 13oz to 9lb 15 oz (4000 to 4500g) and are usually
born at term, although they may be preterm or postterm
▪ Causes
o Born to multiparas
o Large parents
o Mothers who are obese
o Diabetes in the mother may also cause increased size, as may erythroblastosis fetalis
▪ Scope of problem48
o More likely to go through longer labor, suffer injury during birth or need a c-section
o Shoulder dystocia may occur b/c the shoulders are too large to fit through the pelvis
o Congenital heart defects and a higher mortality rate also are more common
▪ Therapeutic management
▪ Nursing considerations
Chapter 30: High-Risk Newborn: Acquired and Congenital Conditions
Respiratory Complications
▪ Asphyxia
▪ Transient tachypnea of the newborn
o Develop rapid respirations soon after birth from inadequate absorption of fetal lung
fluid
o Usually resolves within 24 to 48 hours
o Risk factors:
▪ Cesarean birth w/ or w/out labor, macrosomia, multiple gestation, excessive
maternal sedation, prolonged or precipitous labor, male gender, and maternal
diabetes or asthma
▪ Mild immaturity of surfactant production also may be a factor
o Cause:
▪ Unknown
▪ Thought to result from a delay in absorption of fetal lung fluid by pulmonary
capillaries and lymph vessels
● This leads to decreased lung compliance and air trapping and produces
signs similar to those of RDS
o Manifestations:
▪ Tachypnea develops within 6 hours of birth
▪ Grunting, retractions, nasal flaring, and mild cyanosis also are present
o Therapeutic management:
▪ Supportive and may include oxygen for cyanosis
▪ Gavage feeding may be given when the respiratory rate is high to prevent
aspiration and conserve energy
▪ Antibiotics may be given until sepsis is ruled out
▪ Meconium aspiration syndrome
o Condition in which there is obstruction, chemical pneumonitis, and air trapping caused
by meconium in the lungs
o Develops in 5% of those infants
o Occurs most often in infants who are post term, small for gestational age, and are
compromised before birth by placental insufficiency w/ decreased amniotic fluid and
cord compression
o Causes:
▪ Occurs most often when hypoxia causes increased peristalsis of the intestines
and relaxation of the anal sphincter before or during labor
▪ MAS develops when meconium in the amniotic fluid enters the lungs during
fetal like or at birth
▪ Persistent pulmonary hypertension of the newborn49
o Condition in which pulmonary vasoconstriction occurs after birth and elevates vascular
resistance of the lungs
o Normal changes to neonatal circulation are impaired as a result
o Causes:
▪ Occurs most often in infants who are term or postterm
▪ Can be caused by abnormal lung development or maternal use of nonsteroidal
anti-inflammatory drugs or selective serotonin reuptake inhibitors
▪ Often associated w/ hypoxemia and acidosis from conditions such as asphyxia,
MAS, sepsis, polycythemia, diaphragmatic hernia, and RDS
o Manifestations:
▪ Signs within the first 12 hours after birth
▪ Tachypnea
▪ Resp. distress
▪ Progressive cyanosis often become worse w/ handling
▪ O2 sat and partial pressure of oxygen in arterial blood are decreased
▪ PaCO2 is increased and acidosis is present
o Therapeutic management:
▪ Treat underlying cause of poor oxygenation and relieving pulmonary
vasoconstriction
▪ Arterial pH may be increased w/ resp therapy and drug therapy to cause
pulmonary vasodilation
▪ Sedation, high-frequency ventilation, and surfactant therapy may be necessary
▪ Inhaled nitric oxide may be given to dilate pulmonary vessels
Hyperbilirubinemia (Pathologic Jaundice)
▪ Definition
o May be seen in the first 24 hours of life
▪ Causes
o Hemolytic disease of the newborn from incompatibility b/w the blood of the mother
and that of the fetus
o Rh incompatibility, in which the Rh-negative mother forms antibodies when blood from
an Rh-positive fetus enters her circulation
o Erythroblastosis fetalis---agglutination and hemolysis of fetal erythrocytes resulting
from incompatibility b/w maternal and fetal blood
o Hydrops fetalis---severe anemia that results in heart failure and generalized edema
▪ Therapeutic management
o Phototherapy
o Exchange transfusions
Application of the Nursing Process: Hyperbilirubinemia
▪ Assessment
▪ Analysis
▪ Nursing diagnosis
▪ Expected outcomes
▪ Evaluation
Infection
▪ Transmission of infections
▪ Sepsis neonatorum---systemic infection from bacteria in the bloodstream50
o Causes
▪ Bacteria such as GBS, Escherichia coli, coagulase-negative Staph, Staph aureus,
Haemophilus influenzae and fungi such as Candida albicans
▪ Early onset--- acquired during birth, often from complications of labor
▪ Late onset--- occurs from 8-90 days after birth in healthy term infants or after
72 hours of life in a very-low-birth weight infants
o Therapeutic management
o Nursing considerations
o Nursing interventions
Infant of a Diabetic Mother
▪ Scope of problem
o Cardiac , urinary tract, and GI anomalies, neural tube anomalies, sacral agenesis are
most frequent
o Cardiomegaly is common and may lead to heart failure
▪ Characteristics
▪ Therapeutic management
▪ Nursing considerations
▪ Nursing interventions
Polycythemia
▪ Hemoglobin level greater than 22 g/dL and a hematocrit greater than 65%
▪ Causes
o May occur when poor intrauterine oxygenation causes the fetus to compensate
producing more erythrocytes than normal
o More common in infant who are post term, LGA, or SGA or have fetal growth restriction
(FGR)
o Also occurs in infants of mothers who smoke or have HTN or diabetes
o Delayed cord clamping or a transfusion from one twin to another may also cause the
condition
▪ Manifestations
o Plethoric color
o Lethargy
o Irritability
o Poor tone
o Tremors
o Abdominal distention
o Decreased bowel sounds
o Poor feeding
o Hypoglycemia
o Resp. distress may also be present
▪ Therapeutic management
o Supportive
o Partial exchange transfusion may be performed if the hct is above 70%
o Blood is replaced w/ normal saline to decrease the total number of RBCs
▪ Nursing considerations
Hypocalcemia
▪ A total serum calcium concentration of less than 7 mg/dL.51
o Early-onset (in the first 72 hours of age)
o Late-onset (1 week of age)
▪ Causes
o Occurs most often in IDMs, and infants w/ asphyxia, prematurity, maternal
anticonvulsant therapy, and delayed nutrition
o Late-onset is caused by hyperparathyroidism, malabsorption, low magnesium levels,
diuretic therapy and rickets
▪ Manifestations
o Irritability
o Jitteriness
o Poor feeding
o High-pitched cry
o Muscle twitching
o Apnea
o Seizures
o Electrocardiographic changes
▪ Therapeutic management
o IV calcium gluconate is given if feeding alone does not raise the calcium level
▪ Nursing considerations
Prenatal Drug Exposure
▪ Neonatal abstinence syndrome ---disorder in which infants exposed to maternal drugs before
birth demonstrate signs of drug withdrawal
▪ Identification
▪ Therapeutic management
▪ Nursing considerations
o Feeding
o Rest
o Bonding
Phenylketonuria
▪ Genetic disorder that causes central nervous system injury from toxic levels of the amino acid
phenylalanine in blood
▪ Cause:
o Caused by a deficiency of the liver enzyme phenylalanine hydrolase, which is necessary
to convert phenylalanine to tyrosine for use
o Autosomal recessive disorder
▪ Manifestations
o Digestive problems and vomiting and later progress to seizures, musty odor of the urine,
and severe cognitive impairment
o Older children have eczema, hypertonia, hyperactive behavior, cognitive impairment,
and hypopigmentation of the hair, skin, and irises
▪ Therapeutic management
o Low-phenylalanine diet that should start no later than 3 wks after birth and continue
throughout life to avoid irreversible neuro damages
o Low-protein foods are introduced when solids are started
▪ Nursing considerations52
o Screening before 24 hrs of age should be repeated because the infant may not yet have
consumed enough protein for the test to be accurate
Congenital Cardiac Defects: Classifications
▪ Acyanotic defects
o Obstruction of blood flow from the ventricles or a defect that causes increased flow of
blood to the lung occurs
o Both increase the work of the heart
o Growth is slowed, and the infant fatigues easily
▪ Cyanotic defects
o Blood flow to the lung decreases, or venous blood and oxygenated blood are mixed in
the systemic circulation, or both, decreasing the oxygen carried to the tissues and
resulting in cyanosis
▪ Left-to-right shunting
o Increases blood flow to the lungs
o Allow blood to flow from the higher pressure of the left side of the heart to the right
side or from the aorta to the pulmonary artery
▪ Ex: ventricular septal defects and patent foramen ovale
▪ Defects with obstruction of blood flow
o Decrease in the blood flow through a vessel or valve occurs because of stenosis
(narrowing)
o Adds to the work of the heart, causes hypertrophy of the heart or major blood vessels—
and may lead to heart failure
▪ Ex: coarctation of the aorta and stenosis of pulmonary or aortic valves fit into
this classification
▪ Defects with decreased pulmonary blood flow
o Impairment in the flow of blood from the right side to the lungs
o Combined w/ abnormal openings b/w pulmonary and systemic circulations, occurs in
defects w/ decreased pulmonary blood flow
▪ Ex: tet of flow
▪ Cyanotic defects with increased pulmonary blood flow
o Defects allow survival only if a mixing of venous and oxygenated blood in the systemic
circulation
▪ Ex: transposition of the great vessels
Congenital Cardiac Defects
▪ Manifestations
o Cyanosis
o Heart murmurs
o Tachycardia and tachypnea
o Other signs
▪ Therapeutic management
▪ Nursing considerations53
Which assessment finding would convince the nurse to "hold" the next dose of magnesium sulfate?
a) Absence of deep tendon reflexes
• Because absence of deep tendon reflexes is a sign of magnesium toxicity, the next
scheduled dose should not be administered. Calcium gluconate is the antidote that
should be administered. An hourly output of less than 30 mL could indicate toxicity. A
respiratory rate of less than 12 breaths/min could indicate toxicity. Decrease in blood
pressure is an expected side effect of magnesium sulfate.
b) Urinary output of 100 mL total for the previous 2 hours
c) Respiratory rate of 14 breaths/minute
d) Decrease in blood pressure from 160/100 to 140/85
Glucose metabolism is profoundly affected during pregnancy because:
▪ Pancreatic function in the islets of Langerhans is affected by pregnancy.
▪ A pregnant woman uses glucose at a more rapid rate than a nonpregnant woman.
▪ A pregnant woman increases her dietary intake significantly.
▪ Placental hormones are antagonistic to insulin, resulting in insulin resistance.
o Placental hormones, estrogen, progesterone, and human placental lactogen (HPL),
create insulin resistance. Insulin also is broken down more quickly by the enzyme
placental insulinase. Pancreatic functioning is not affected by pregnancy. The glucose
requirements differ because of the growing fetus. The pregnant woman should increase
her intake by 200 calories a day.
In neonatal resuscitation, which should be done first?
a) Suction the mouth and nose
b) Stimulate the infant by rubbing the back
c) Perform the Apgar test
d) Dry the infant and position the head
o Drying the infant to prevent heat loss is the first action. It is followed by positioning to
open the airway. The neonate is not breathing, so drying the neonate to prevent heat
loss and positioning the neonate would take priority over the suctioning. Stimulating the
infant is a step in the process, but not the first action. The Apgar can be delayed until
steps have been taken to initiate breathing. By assessing the lack of breathing, some of
the Apgar has already been completed.
Fran delivered a 9 lb, 10 oz baby 1 hour ago. When you arrive to perform her 15-minute assessment,
she tells you that she "feels all wet underneath." You discover that both pads are completely
saturated and that she is lying in a 6-inch diameter puddle of blood. What is your first action?54
a) Call for help
b) Assess the fundus for firmness
o Firmness of the uterus is necessary to control bleeding from the placental site. The
nurse should first assess for firmness and massage the fundus as indicated. The first
action should be to assess the fundus. Assessing blood pressure is an important
assessment with a bleeding client, but the top priority is to control the bleeding. This is
done by first assessing the fundus for firmness. If bleeding continues in the presence of
a firm fundus, lacerations may be the cause.
c) Take her blood pressure
d) Check the perineum for lacerations
What action should be initiated to limit hypovolemic shock when uterine inversion occurs?
a) Administer oxygen at 3 L/minute by nasal cannula.
b) Administer an oxytocic drug by intravenous push.
c) Monitor the fetal heart rate every 5 minutes.
d) Restore circulating blood volume by increasing the intravenous infusion rate.
o Intravenous fluids are necessary to replace the lost blood volume that occurs in uterine
inversion. Administering oxygen will not prevent hypovolemic shock. Oxytocin drugs
should not be given until the uterus is repositioned. A uterine inversion occurs during
the third stage of labor.
The most important reason to protect the preterm infant from cold stress is that:
a) It could make respiratory distress syndrome worse.
o Cold stress may interfere with production of surfactant, making respiratory distress
syndrome worse. Preterm infants do not shiver to produce heat. Cold stress does
interfere with the ability to eat, but does not make the infant less able to digest the
nutrients. Decreased circulation is not the top priority in caring for an infant with cold
stress.
b) Shivering to produce heat may use up too many calories.
c) A low temperature may make the infant less able to digest nutrients.
d) Cold decreases circulation to the extremities.
[Show More]