1
NR 327 OB Maternal Health Chapters 12-22
Chapter 12: Processes of Birth
Physiologic Effects of the Birth Process: Maternal Response
Most obvious changes of pregnancy and birth occur in the woman’s reproductive sys
...
1
NR 327 OB Maternal Health Chapters 12-22
Chapter 12: Processes of Birth
Physiologic Effects of the Birth Process: Maternal Response
Most obvious changes of pregnancy and birth occur in the woman’s reproductive system, but significant changes also occur during
labor in her cardiovascular, resp, GI, urinary, and hematopoietic systems
Reproductive System: Characteristics of Contractions
▪ Coordinated
o Uterus can contract and relax in a coordinated way
o If not coordinated=not effective
o Frequency (beginning of one uterine contraction to the beginning of the next)
▪ Frequency be assessed as the # of contractions in 10 minutes, averaged over 30 minutes
o Duration (beginning of a uterine contraction to the end of the same contraction)
▪ Usually expressed in seconds
o Intensity (strength of a contraction)
▪ Mild, moderate, and strong describe contraction intensity as palpated by the nurse
▪ Different descriptions of intensity apply when an internal fetal monitor is used to record contractions
o Coordinated labor contractions begin in the uterine fundus and spread downward toward the cervix to propel the
fetus through the pelvis
▪ Involuntary
o Uterine contractions are involuntary and are not under conscious control
o Anxiety and excessive stress can diminish contractions, whereas relaxation can facilitate the natural process
▪ Intermittent (come &go)
o Are intermittent rather than sustained, allowing relaxation of the uterine muscle and resumption of blood flow to
and from the placenta
▪ Contractions last 60-90 seconds, 2-3 minutes apart
▪ Coordinated contractions from the top thin and dilate the cervix
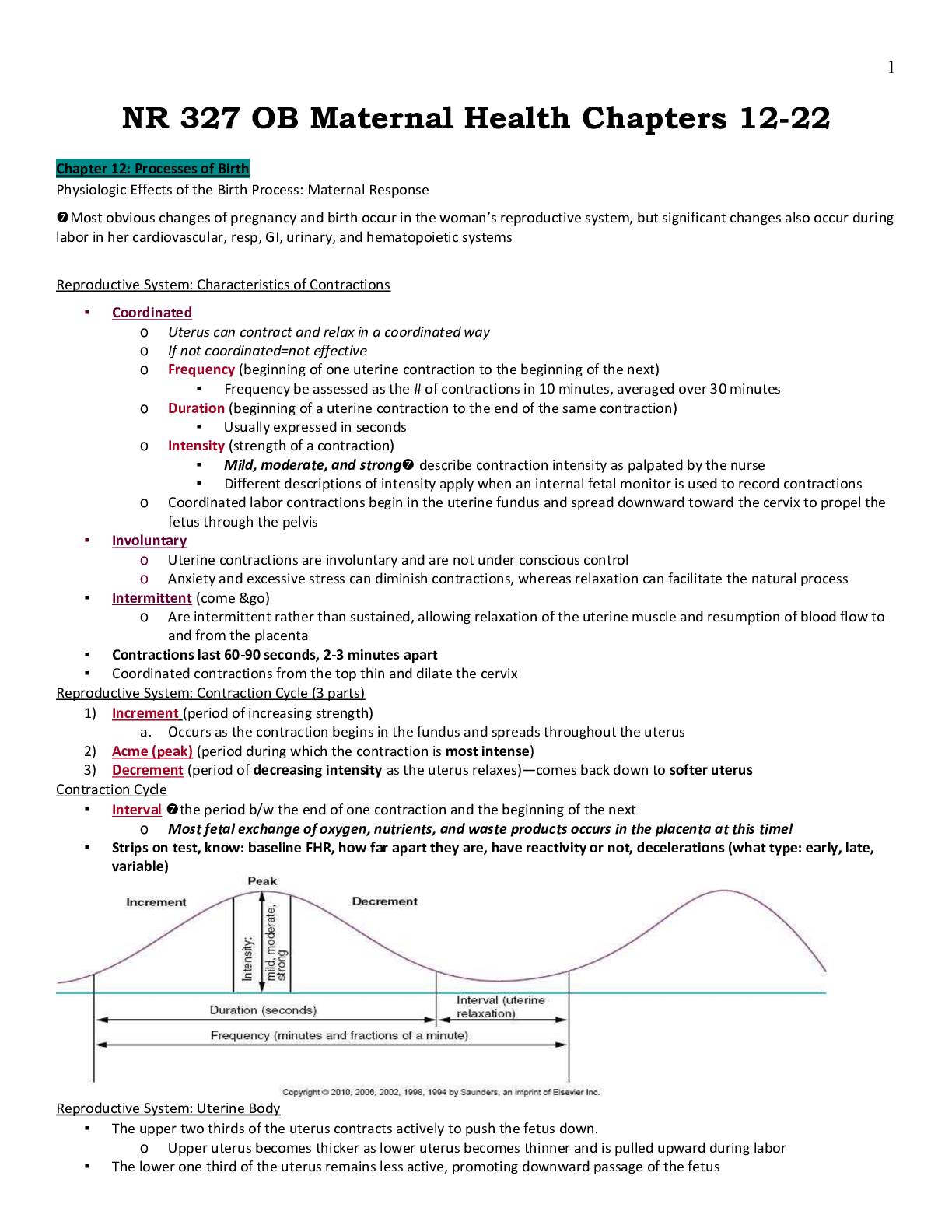
Reproductive System: Contraction Cycle (3 parts)
1) Increment (period of increasing strength)
a. Occurs as the contraction begins in the fundus and spreads throughout the uterus
2) Acme (peak) (period during which the contraction is most intense)
3) Decrement (period of decreasing intensity as the uterus relaxes)—comes back down to softer uterus
Contraction Cycle
▪ Interval the period b/w the end of one contraction and the beginning of the next
o Most fetal exchange of oxygen, nutrients, and waste products occurs in the placenta at this time!
▪ Strips on test, know: baseline FHR, how far apart they are, have reactivity or not, decelerations (what type: early, late,
variable)
Reproductive System: Uterine Body
▪ The upper two thirds of the uterus contracts actively to push the fetus down.
o Upper uterus becomes thicker as lower uterus becomes thinner and is pulled upward during labor
▪ The lower one third of the uterus remains less active, promoting downward passage of the fetus2
▪ The cervix is also passive.
▪ Myometrial (pertaining to the uterine muscle) cells in the upper uterus remain shorter at the end of each contraction
rather than returning to their original length
o Myometrial cells in the lower uterus become longer w/ each contraction
o These 2 characteristics enable the upper uterus to maintain tension b/w contractions to preserve the cervical
changes and downward fetal progress made w/ each contraction
▪ The physiologic retraction ring marks the division b/w the upper and lower segments of the uterus
o Segments change the shape of the uterine cavity, which becomes more elongated and narrow as labor progresses
o This change in uterine shape straightens the fetal body and efficiently directs it downward in the pelvis
Reproductive System: Cervical Changes
▪ Effacement (thinning and shortening)
o Creates a thin mucus discharge/ lubricates vaginal canal to deliver baby
o Primigravida (Nulliparas): Efface first then dilate
o b/f labor: the cervix is a cylindric structure about 2 cm long at the lower end of the uterus
o labor contractions push the fetus downward against the cervix while pulling the cervix upward
▪ if membranes are intact, hydrostatic (fluid) pressure of the amniotic sac adds to the force of the
presenting part on the cervix
▪ cervix becomes shorter and thinner as it is drawn over the fetus and amniotic sac
▪ Dilation (opening)
o Multiparas: dilate first then efface
o As the cervix is pulled upward and the fetus is pushed downward, the cervix dilates
o Expressed in centimeters
▪ Effacement and dilation occur concurrently during labor but at different rates.
▪ Nullipara
o Woman who has not completed a pregnancy to at least 20 weeks of gestation
o Completes most cervical effacement early in the process of cervical dilation
▪ Para (AKA a parous woman)
o Woman who has given birth after a pregnancy of at least 20 weeks gestation
o Also designates the number of pregnancies that end after at least 20 wks of gestation
o Cervix is usually thicker than that of a nullipara at any point during labor.
Maternal Cardiovascular System
▪ Blood flow to the placenta decreases during a contraction*
o The muscle fibers of the uterus constrict around the maternal spiral arteries, which supply the placenta.
o Temporarily shunts 300-500 mL of blood back into maternal systemic circulation, leading to a relative increase in
the woman’s blood volume.
o This temporary change increases her blood pressure slightly and slows her pulse rate.
▪ Vital signs are best assessed during the interval between contractions. (DON’T take VS during
contractions!)
o Pain meds give at onset of contractions because of blood flow to fetus
▪ Supine hypotension may occur during labor if the woman lies on her back.
o The woman should be encouraged to rest in positions other than supine to promote blood return to her heart and
thus enhance blood flow to the placenta and promote fetal oxygenation
Maternal Respiratory System
▪ Increase depth and rate of respirations ---↑during labor, especially if woman is anxious or in pain
▪ Hyperventilation
o It may occur with rapid and deep breathing.
▪ Use brown paper bag to get CO2 back
o Respiratory alkalosis occurs as she exhales too much carbon dioxide.
▪ She may feel tingling of her hands and feet, numbness, and dizziness.
▪ The nurse should help her slow her breathing and breathe into a paper bag or her cupped hands to restore normal blood
levels of carbon dioxide and relieve these symptoms.
Maternal Gastrointestinal System
▪ Decreased gastric motility ---can result in N/V
▪ Most women are not hungry but are thirsty and have dry mouths.
o Ice chips are commonly provided.
o Small amounts of other clear liquids may be allowed.3
▪ Solid food is usually withheld to prevent vomiting and aspiration in the event that general anesthesia is required.
Maternal Urinary System
▪ Reduced sensation of a full bladder ---b/c of intense contractions and the effects of regional anesthesia, the woman may be
unaware that her bladder is full, yet it may contribute to discomfort, especially that which persists after regional anesthesia
▪ Full bladder can inhibit fetal descent b/c is occupies space in the pelvis
Maternal Hematopoietic System
▪ 500 mL normal blood loss for vaginal delivery
o Women can tolerate profuse blood loss during the birthing process because of the ↑ blood volume during
pregnancy by 30%-40%
▪ Woman who is anemic at the beginning of labor has less reserve for normal blood loss and poor tolerance for excess
bleeding
▪ Levels of several clotting factors, especially fibrinogen, are elevated during pregnancy and continue to be higher during
labor and after delivery.
o Provides protection from hemorrhage
o Increases the mother’s risk for a venous thrombosis during pregnancy and after birth
▪ DVT ↑ w/ bed rest
Physiologic Effects of the Birth Process: Fetal Response
▪ Placental circulation
o Exchange of oxygen, nutrients, and waste products b/w the mother and fetus occurs in the intervillous spaces
without the mixing of maternal and fetal blood
o During strong labor contractions, the maternal blood supply to the placenta and eventually stops temporarily as
the spiral arteries supplying the intervillous spaces are compressed by the uterine muscle
o Most placental exchange occurs during the interval between contractions
o Fetal protective mechanisms include:
▪ Fetal hGB, which more readily takes on oxygen and releases carbon dioxide
▪ High hGB and Hct levels than can carry more oxygen than adult hGB
▪ A high cardiac output
▪ Cardiovascular system responds to stress
o Heart rate ranges from 110 to 160 beats per minute (BPM)
▪ Pulmonary system
o The fetal lungs produce fluid to allow normal development of the airways.
o As term nears, production of fetal lung fluid decreases to about 65% of its maximum production and its absorption
into the interstitium of the lungs ↑
o Labor speeds the absorption of lung fluid, so about 35% of the maximum amount remains in the airways at birth
▪ Some fluid is expelled from the upper airways as the fetal head and thorax are compressed during
passage through the birth canal
▪ Most remaining lung fluid is absorbed into the interstitial spaces of the newborn’s lungs and then into the
circulatory system
o Catecholamines produced by the fetal adrenal glands in response to the stress of labor appear to contribute to
the infant’s adaptation to extrauterine life
▪ Stimulate cardiac contraction and breathing
▪ Quicken the clearance of remaining lung fluid
▪ Aid in temperature regulation
o Infants born by c-section are more likely to have transient breathing difficulty
▪ Transient tachypnea of the newborn (retained lung fluid)
Components of the Birth Process
▪ Four major factors interact during normal childbirth: 4 Ps
o Powers:
▪ Contractions 2-3 minutes apart lasting 60-90 seconds
o Passage:
▪ Pelvis has to be large enough/right shape
o Passenger:
▪ Fetus-right position
o Psyche: moms mind
▪ Moms mind has to be prepared4
▪ If she’s fighting it will make it harder to dilate, if scared and not relaxing will made hard to efface and
dilate
▪ Interrelationship of these components
Components of the Birth Process: Powers
▪ Uterine contractions (1st stage of labor)
o Primary force that moves the fetus through the maternal pelvis
▪ Maternal pushing efforts (2nd stage of labor) accelerate movements
o Full cervical dilation to birth of the baby
o Uterine contractions continue to propel the fetus through the pelvis
o Woman feels an urge to push and bear down as the fetus distends her vagina and puts pressure on her rectum.
Components of the Birth Process: Passage
▪ The bony pelvis
o Usually more important to the outcome of labor than the soft tissue b/c the bones and joints do not readily yield
to the forces of labor.
o However, softening of the cartilage linking the pelvic bones occurs near term b/c in ↑levels of the hormone relaxin
▪ The linea terminalis (pelvic brim) divides the bony pelvis into the:
o False pelvis (top) above linea terminalis
o True pelvis (bottom) below linea terminalis
▪ Most important in childbirth (has 3 subdivisions):
1) Inlet (upper pelvic opening)
2) Midpelvis (pelvic cavity) (zero station= even w/ the ischial spin)
3) Outlet (lower pelvic opening) (coming out of pelvis)
Components of the Birth Process: Passenger
▪ The passenger is the fetus, membranes, and placenta.
▪ Several fetal anatomic and positional variables influence the course of labor.
▪ Fetal head
o Cephalic presentation (96% of the time)
o The bones of the fetal head involved in the birth process are:
▪ The two frontal bones on the forehead
▪ Two parietal bones at the crown of the head
▪ Occipital bone at the back of the head
● The five major bones are not fused but are connected by sutures which are narrow areas of
flexible tissue that connect fetal skull bones, permitting slight movement during labor
o Fontanels
▪ Wider spaces at the intersections of the sutures connecting fetal or infant skull bones
▪ Anterior fontanel diamond shape
● Formed by the intersection of four sutures:
o Two coronal, frontal, and sagittal, which connect the 2 frontal and 2 parietal bones
▪ Posterior fontanel triangular shape
● Formed by the intersection of 3 sutures
o One sagittal and two lambdoid, which connect the two parietal bones and occipital bone
● Very small, and often looks more like a slight indentation in the skull
The sutures and different shapes of the fontanels provide important landmarks to determine fetal position (relation of a fixed
reference point on the fetus to the quadrants of the maternal pelvis) and head flexion during vaginal examination
o Fetal head diameters
▪ 9.5cm
▪ Components of the Birth Process: Passenger (Cont.)5
Components of the Birth Process: Variations in the Passenger
▪ Fetal lie
o Orientation of the long axis of the fetus to the long axis of the woman
o In more than 99% of pregnancies, the lie is longitudinal and parallel to the long axis of the
woman
o Longitudinal
▪ Head down in pelvis, fetus laying vertical
o Transverse
▪ Exists when the long axis of the fetus is at a right angle to the woman’s
long axis
▪ Fetus laying horizontal
o Oblique
▪ At some angle b/w the longitudinal lie and the transverse lie
▪ Attitude
o Relationship of fetal body parts to one another
o Flexion
▪ Head flexed toward the chest and the arms and legs flexed over the
thorax
▪ Back is curved in a convex “C” shape
▪ Head down in pelvis, fetus laying vertical
o Extension
▪ Not in fetal position- cephalic brow/ face position
▪ Presentation
o Fetal part that first enters the pelvis
o Cephalic
1) Vertex
● Most common type of cephalic presentation, in which the fetal head is fully flexed
● Called vertex or occiput presentation & is the most favorable for normal progress of labor b/c the
smallest suboccipitobregmatic diameter is presenting
2) Military
● Head is in a neutral position, neither flexed nor extended. Longer occipitofrontal diameter is
presenting
3) Brow
● Fetal head is partly extended. Brow presentation is unstable, usually converting to a vertex
presentation if it extends. Longest supraoccipitomental diameter is presenting
4) Face
● Head is extended and the fetal occiput is near the fetal spine. The submentobregmatic diameter
is presenting
o Breech
▪ Occurs when the fetal buttocks enter the pelvis first6
▪ More common in preterm births and when a fetal abnormality such as hydrocephalus prevents the head
from entering the pelvis during the later weeks of pregnancy or with abnormalities of the maternal uterus
and pelvis with placenta previa (placenta in the lower uterus)
▪ Disadvantages:
● Buttocks are not smooth and firm like the head and are less effective at dilating the cervix
● Fetal head is the last part to be born, by the time the fetal head is deep in the pelvis, the umbilical
cord is outside the mother’s body and is subject to compression b/w the fetal head and the
maternal pelvis
● Head must be delivered quickly to allow infant to breathe
▪ Frank: most common variation, occurring when the fetal legs are extended across the abdomen toward
the shoulders
▪ Full: (complete breech) Indian style/ bottom down—head, knees, and hips are flexed, but the buttocks
are presenting
▪ Footling: one foot or both feet are out
o Shoulder
▪ Cesarean birth is necessary when the fetus is viable
▪ Occurs more often w/ preterm birth, high parity, prematurely ruptured membranes, hydramnios, and
placenta previa
Cephalic Presentation
Breech Presentation7
Components of the Birth Process:Variations in the Passenger (Cont.)
▪ Position
o Location of fixed reference point on the presenting part in relation to the four quadrants of the maternal pelvis
o Right or left
▪ First letter of the abbreviation describes whether the fetal reference point is to the right or left of the
mother’s pelvis. If the fetal reference point is neither to the right nor to the left of the pelvis, this letter is
omitted
o Occiput (O) (the back of the head or skull) used in vertex presentation
▪ Anterior:
▪ Posterior: harder to deliver baby
o Mentum (M) / (chin) reference point in a face presentation
o Sacrum (S) (BREACH) used for breech presentations
➔ Letter may also designated the less common brow (F for fronto) and shoulder (Sc for scapula) presentations
o Anterior (A)
o Posterior (P)
o Transverse (T)
▪ If the fetal reference point is in neither an anterior nor a posterior quadrant
▪ Don’t feel baby presenting parts= deliver C-section
o LOA,ROA,LOP,ROP,LSA,RSA8
Components of the Birth Process: Psychepsychological response to labor
▪ Anxiety
o Maternal catecholamine’s secreted in response to anxiety and fear can inhibit uterine contractility and placental
blood flow
▪ Culture and expectations
▪ Birth as an experience
▪ Support (during pregnancy/ after/ before)
▪ Impact of technology (pay attention to mom not just monitor)
Components of the Birth Process: Interrelationship of the Four Ps
▪ The four Ps are actually an interrelated whole.
▪ The nurse can act as an advocate for the laboring woman and her support person to increase their sense of control and
mastery of labor, which often reduces anxiety and fear and helps them achieve their desired birth.
Normal Labor: Theories of Onset
▪ Factors that appear to have a role in starting labor include:
o Progesterone withdrawal
o Increase release of prostaglandins
o Increased secretion of natural oxytocin
o Increased oxytocin receptors in the uterus
o Increased stretching and pressure of the uterus and cervix
Indications of labor (when to go to hospital) - CONTRACTIONS are COORDINATED
Normal Labor: Premonitory Signs (labors approaching)
▪ Braxton Hicks contractions (NOT coordinated)
o Irregular and mild uterine contractions that occur throughout pregnancy and become stronger in the last trimester
▪ Lightening (dropped)
o Fetus descends toward the pelvis inlet (“dropping”), the woman notices that she breathes more easily b/c upward
pressure on her diaphragm is reduced9
o ↑ pressure on her bladder causes her to urinate more frequently
o Pressure of the fetal head in the pelvis may also cause leg cramps and edema
o Happens 2-3 wks before the natural onset of labor
▪ Increased vaginal mucus secretion (lubricates)
o ↑ in clear and nonirritating vaginal secretions occurs as fetal pressure causes congestion of the vaginal mucosa
▪ Cervical changes
o Softening (ripening)—d/t the hormone relaxin and ↑ water content on the connective tissue of the cervix
▪ As the fetal head descends w/ lightening, it puts pressure on the cervix, starting the process of effacement
and dilation
● Effacement and dilation cause expulsion of the mucus plug that sealed the cervix during
pregnancy, rupturing small cervical capillaries in the process
o Possible dilation
o Bloody show
▪ Mixture of cervical mucus and pink or brown blood from ruptured capillaries in the cervix; often precedes
labor and ↑ with cervical dilation
▪ Energy spurt (nesting) and weight loss (1-3lbs; may occur b/c the altered estrogen to progesterone ratio causes excretion of
some of the extra fluid that accumulates during pregnancy)
o Right before labor
▪ Contractions are coordinated
Normal Labor: True Labor and False Labor
▪ True Labor
o Increased contractions
o Increased discomfort
o ***Cervical change: progressive effacement and dilation most important
▪ DILATION
▪ False labor (prodromal labor or prelabor)
o Contractions inconsistent/ uncoordinated
o Discomfort is more annoying than truly painful
o Cervix does not change
▪ NO dilation
Normal Labor: Labor Mechanisms
▪ Descent
o Movement of fetus through the birth canal
▪ Abdomen-pelvis- birth canal
o Inhibiting factors:
▪ Full bladder can inhibit fetal descent b/c it occupies space in
pelvis= UTERINE ATONY causing HEMORRHAGE!
▪ Small pelvis, position of baby (brow/face/ shoulder) large
baby, ineffective contractions
▪ Engagement
o Occurs when the largest diameter of the fetal presenting part
(normally the head) pas passed the pelvic inlet and entered the
pelvic cavity
o Fetal presenting part reaches 0 station
▪ Ears at ischial spine
▪ Internal rotation
o Rotates head at different position – to allow the largest fetal head
diameters to align w/ the largest maternal pelvic diameters
o The fetus enters the pelvic inlet w/ the sagittal suture in a
transverse or oblique orientation to the maternal pelvis b/c that is the widest inlet diameter
o Internal rotation allows the longest fetal head diameter (the anteroposterior) to conform to the longest diameter
of the maternal pelvis
▪ Flexion
o Of the fetal head, allowing the smallest head diameters to align w/ the smaller diameters of the midpelvis as the
fetus descends
▪ Extension10
o Extending up, start to see crowning (HAIR)
▪ External rotation
o Head is out an rotates to one side
o Aligning the head w/ the shoulders during expulsion
▪ Expulsion
o Head is completely out- should deliver
Normal Labor: Stages of Labor
▪ First stage of labor (0-10) onset of true labor
o Latent phase---(7.3-8.6hrs)(O-3cm)
▪ Cervical dilation and effacement
▪ Educate** , FHR
▪ Cervical effacement and fetal positional change occur during the latent phase, preparing for the more
rapid changes of active labor
▪ Happy
▪ Transfers from latent to active when she needs an epidural
▪ Start of dilation
▪ Contractions usually begin irregularly
▪ 4.1- 5.3 hrs for multiparas
o Active phase (4-7cm)
▪ Dilates at a more rapid rate than in the latent phase
▪ Effacement of the cervix is completed
▪ Fetus descends in the pelvis and internal rotation begins
▪ Durations of active and transition phases usually vary w/ whether the woman had epidural analgesia
● Nulliparas w/ no epidural—duration of these two phases within the 1st stage is about 7.7 to 13.3
hours
● Multiparas w/ no epidural- 5.7-7.5 hours
▪ Contractions are about 2 to 5 minutes apart, with a duration of about 40 to 60 seconds and an intensity
that ranges from moderate to strong
▪ Active labor contractions reach their peak intensity quickly and stay at the peak longer than during the
latent phase
o Transition (8-10cm)
▪ Fetus descends further into the pelvis
▪ Bloody show often increases w/ the completion of cervical dilation
▪ DON’T PUSH IF NOT AT 10CM
▪ Anxiety ↑fear of losing control helplessness “I can’t do this”
▪ Contractions every 1.5-2 minutes lasting 60-90 seconds- strong intensity
▪ Averaging 3.6 hours in the nullipara and having a variable length in the multipara
▪ Second stage of labor
o Expulsion of the fetus
o “expulsion” begins w/ complete (10cm) dilation and full (100%) effacement of the cervix and ends w/ the birth of
the baby
o The word “labor” aptly describes the second stage
o Pushing & Delivery of the baby
o May think she needs to have a bowel movement or “the baby is coming”/ “I have to push”
o DON’T PUSH IF NOT AT 10 CM---otherwise cervix will swell and not be able to deliver
o *pushing techniques
▪ Bare down as if you’re having a bowel movement
▪ Can push even w/ epidural
o Contractions may diminish slightly or even pause briefly as the second stage begins
▪ They are still strong, about 2 to 3 minutes apart, with a duration of 40-60 seconds
▪ Third stage of labor (shortest stage)
o Expulsion of the placenta
o Begins with the birth of the baby and ends with the expulsion of the placenta
o Shortest stage, with an avg length of 6 minths
o When the infant is born, the uterine cavity becomes much smaller
o The reduced size decreases the size of the placenta site, causing it to separate from the uterine wall11
o Four signs suggest placenta separation:****
1) Uterus has a spherical shape
2) Uterus rises upward in the abdomen as the placenta descends into the vagina and pushed the fundus
upward
3) Cord descends further from the vagina
4) A gush of blood appears as blood trapped behind the placenta is released
o Mechanisms:
▪ Schultze: placenta is expelled with the shiny fetal side presenting first
▪ Duncan: rough maternal side presents first
o Delivery of placenta (avg 6 mins)
o The uterus must contract firmly and remain contracted after the placenta is expelled to compress open vessels at
the implantation site
o Monitor for hemorrhage
▪ Soft boggy uterus (uterine atony)
● Massage uterus supporting suprapubic area
● Encourage to pee Q3Hrs
▪ Fourth stage of labor (recovery period---1-4hrs after birth)
o Maternal physiologic stabilization and parent—infant bonding
o Immediately after birth, the firmly contracted uterus can be palpated through the abdominal wall as a firm,
rounded mass about 10-15 cm in diameter at or below the level of the umbilicus
o Monitor for hemorrhage
o Educate (reinforce)
o Hydrate
o Assessments essential (VS)
▪ If multipara contractions 10 minutes apart in an hour, come to hospital
▪ If primipara 5 minutes apart in an hour, come to hospital
▪ If ferning present, that means ROM (rupture of membranes)
Stages of Labor
Normal Labor:
● FHR Q30min
● Contractions Q30min
● Active phase:
o FHR Q15min
o Contractions Q30min
o B/P Q1hour
o AROM/SROM (artificial/ spontaneous rupture of membranes): Temp Q1 otherwise Q4
Friedman Curve
● Used to Plot Labor Progress
● Shows: Multipara will delivery faster than nullipara woman
o a women that’s delivered before will labor faster than a none pregnant woman before
Vaginal Exams
● Limit vaginal exams because increase risk for infection
● Don’t want gel in vagina if doing ferning test b/c it will mess up test give it a false negative
● Purpose: determines cervical dilation/effacement, fetal presentation, position, station, bloody show, and status of
membranes
● Sterile vaginal exam (SVE): determines where woman is in phases of labor & limit d/t risk of infection
Chapter 13: Nursing Care During Labor and Birth
Issues for New Nurses
▪ Pain associated with birth
▪ Inexperience and negative experiences
▪ Unpredictability
▪ Intimacy
Admission to Birth Facility
▪ Decision to go to the birth facility
o Number and duration of any previous labors
o Distance from the hospital12
o Available transportation
o Childcare needs
o Risk status
Admission to Birth Facility: Nursing Responsibility during Admission
2 nursing priorities when the woman arrives at the birth center are to:
-establish a therapeutic relationship
-assess the condition of the mother and fetus
Priority nursing actions w/ admission during labor
▪ Maternal readiness
▪ FHT
▪ Maternal VS
▪ Establish a therapeutic relationship
o Make family feel welcome
o Determine family expectations
o Convey confidence
o Assign a primary nurse
o Use touch for comfort
o Respect cultural values
▪ Focus assessment
o Fetal heart rate (FHR)
▪ FHR 110 to 160
▪ Regular rhythm: presence of acceleration; absence of deceleration
o Maternal vital signs
▪ Identify signs of hypertension and infection (100.4 or higher)
● HTN during pregnancy is defined as a sustained BP ↑ to 140 mm Hg systolic or 90 mm Hg
diastolic of higher
▪ Impending birth (crowning/ head of baby)
▪ Grunting sounds
▪ Bearing down
▪ Urgency to push
▪ Database assessment
o Obtain essential information from the client
o Fetal assessment
▪ FHR is assessed by intermittent auscultation, electronic monitoring or both
▪ Nurse documents the color and odor of the amniotic fluid and the time of rupture if the membranes
ruptured before admission
o Labor status
▪ Determines by assessing her contraction pattern
▪ Contractions are assessed by palpation, the electronic monitor, or both
▪ Establish if rupture of membrane
▪ Vaginal examination is not performed if the woman has active bleeding (other than bloody show) b/c
the procedure can ↑ bleeding
▪ Speculum rather than vaginal examination may be done if the gestation is preterm or with active bleeding
o Physical exam
▪ Presence and location of edema and abdominal scars and the height of the fundus
▪ Determine presentation and position of the fetus and aid in location of fetal heart sounds
Leopold Maneuvers
Determine presentation and position of the fetus and aid in location of fetal heart sounds
Have women empty bladder, lie on her back knees flexed w/ pillow under hips
Maneuver if fetus is breech presentation13
▪ Admission procedure
o Notify the birth attendant
▪ Give report
▪ Obtain orders
o Consent forms
o Laboratory tests
▪ Hematocrit obtained by finger stick
▪ Midstream urine specimen to assess protein and glucose levels--- usually obtained before notifying the
birth attendant
o Intravenous (IV) access
▪ IV solutions containing electrolytes, such as lactated Ringer solution, are most common
Admission to Birth Facility: Nursing Responsibility after Admission
▪ Fetal assessment
o FHR assessed using either intermittent auscultation or electronic fetal monitoring
o A spontaneous rupture of membranes (SROM) may occur, or the birth attendant may perform an amniotomy
(AROM- artificial rupture of the fetal membranes)
▪ FHR is assessed for at least 1 minute when the membranes rupture
▪ Umbilical cord could be displaced in a large fluid gush, resulting in compression and interruption of blood
flow through it
● Charting r/t to membrane rupture includes the time, FHR, and character and amount of the fluid
o Amniotic fluid: spontaneous rupture of membranes (SROM) or artificial rupture of membranes (AROM)
▪ Should be clear and may include bits of vernix, the creamy white fetal skin lubricant
▪ Cloudy, yellow, and foul-smelling amniotic fluid suggests infection
▪ Green fluid indicates that the fetus passed meconium before birth
● Meconium passage may have been in response to transient hypoxia, although the cause is often
unknown
▪ Fluid:
● Large: > 1000ml
● Moderate: 500-1000ml
● Scant: trickle, barely enough to detect
▪ Maternal assessment
o Vital Signs
o Contractions
o Labor progress
o Intake and output
o Response to labor
▪ Support person’s response
Application of Nursing Process: False or Early Labor
▪ Assessment
o Evaluate status of labor
o Discharge or admit
▪ Analysis
▪ Planning
1) Promote normal placental function
2) Observe for and report problems to the physician or nurse-midwife
▪ Interventions14
o Reassurance
o Teaching
▪ Evaluation
Application of Nursing Process: Fetal Oxygenation
▪ Assess at frequent intervals
o FHR evaluation
o Characteristics, amount, and time of amniotic fluid rupture
o Maternal vital signs
o Pattern of contractions: frequency, duration, intensity, and resting interval
▪ Analysis
▪ Planning
▪ Interventions
o Promote placental function
o Observe for conditions associated with fetal compromise
▪ Evaluation
Discomfort
▪ Assessment
▪ Analysis
o Provide choices to enhance client control
o Determine whether anxiety is contributing to discomfort
▪ Planning
o Pain relief is NOT a realistic goal
o Goal is for positive birth experience
▪ Interventions
o Comfort measures
▪ Lighting
▪ Temperature
▪ Cleanliness
▪ Mouth care
▪ Bladder
▪ Positioning (movement and frequent position changes help with):
1) Decrease pain
2) Improve maternal-fetal circulation
3) Improve the strength and effectiveness of contractions
4) Decrease the length of labor
5) Facilitate fetal descent
6) Decrease perineal trauma and episiotomies
▪ Water:
● Bath may slow labor if used in latent labor
o Should be used in active labor or id persistent, nonproductive contractions during early labor
have caused the woman to become very fatigued
● Breast stimulation by a shower or whirlpool often provokes contractions by secretion of natural
oxytocin
Positions for First Stage
▪ Sitting upright
▪ Standing
▪ sitting leaning forward w/ support
▪ semi sitting
▪ side lying
▪ kneeling, leaning forward w/ support
▪ Interventions
o Teaching
▪ First stage
▪ Second stage
▪ Laboring down (the technique of delaying pushing until the reflex urge to push occurs)15
● Allowing uterine contractions to cause most fetal internal rotation and descent after full dilation
naturally
▪ Positions for second stage
Positions for Pushing Second Stage
▪ Head and knees
▪ Squatting
▪ Semi-sitting pushing
▪ Side lying pushing
▪ Interventions
o Encouragement
o Giving of self
o Pharmacologic measures
o Caring for the birth partner
▪ Evaluation
Preventing Injury
▪ Assessment
o Anticipate birth time to prepare for delivery
o Preparations are usually completed when crowning in the nullipara reaches a diameter or about 3-4 cm
▪ Analysis
o Client is vulnerable before/after delivery
▪ Planning
o Prevent or minimize injuries
▪ Interventions
o Transfer to a delivery room
o Positioning for birth
o Observe the perineum
▪ Evaluation
Nursing Care During the Late Intrapartum Period
▪ Responsibilities during birth
o Preparation of a delivery table with sterile gowns, gloves, drapes, solutions, and instruments
o Perineal cleansing preparation
o Supporting the woman and partner with final pushing efforts
o Initial care and assessment of the newborn
o Administration of medications (usually oxytocin) to contract the uterus and to control blood loss
Nursing Care During the Late Intrapartum Period
▪ Responsibilities after birth
o Care of the infant
▪ Maintaining cardiopulmonary function (Apgar)
● Assess the infants Apgar score at 1 and 5 minutes (& 10 minutes if response is poor)
▪ Support thermoregulation
▪ Identify infant
o Care of the mother
▪ Observe for hemorrhage
▪ Vital signs
● BP, pulse and respirations should be assessed every 15 minutes during the first hour
● A rising pulse rate is an early sign of excessive blood loss because the heart pumps faster to
compensate for reduced blood volume
● BP falls as the blood volume diminished, but this is a last sign of hypovolemia---a rising pulse rate
may also reflect medications administered
▪ Promote comfort
▪ Fundus
● Most common reason for excessive postpartum bleeding is that the uterus does not firmly
contract and compress open vessels at the placental site
● Fundus should be firm, in the midline, and below the umbilicus (about the size of a large
grapefruit)16
o If the fundus is firm, no massage is needed but if it is soft (boggy), it should be massaged
until its firm
o Promote early family attachment
Chapter 14: Intrapartum Fetal Surveillance
Intrapartum Fetal Assessment
▪ The process of fetal surveillance to identify signs associated with well-being and with compromise
▪ At a minimum, intrapartum fetal assessment includes evaluation of the FHR and the mother’s uterine activity
▪ Purposes: to evaluate how the fetus tolerates labor and to identify hypoxic insult
Fetal Oxygenation
▪ Five factors for adequate fetal oxygenation
1) Normal maternal blood flow and volume to
the placenta
2) Normal oxygen saturation in maternal blood
3) Adequate exchange of oxygen and carbon dioxide in the placenta
4) An open circulatory path between the placenta and the fetus through vessels in the umbilical cord
5) Normal fetal circulatory and oxygen-carrying functions
▪ Uteroplacental exchange
o Oxygen-rich and nutrient blood from the mother enters the intervillous spaces and the placenta via the spiral
arteries
o Oxygen and nutrients in the maternal blood pass into the fetal blood that circulated within capillaries inside the
chorionic villi in the intervillous spaces
o Carbon dioxide and other waster products pass from the fetal blood into the maternal blood at the same time
o Maternal blood carrying fetal waste products drains from the intervillous spaces through endometrial veins and
returns to the mother’s circulation for elimination by her body
▪ Substances pass back and forth between mother and fetus without mixing of maternal and fetal blood
o During labor, contractions gradually compress the spiral arteries, temporarily stopping maternal blood flow into
the intervillous spaces at the peak of strong contractions
▪ During contractions, the fetus depends on the oxygen supply already present in body cells, fetal
erythrocytes, and the intervillous spaces
● Oxygen supply in these areas is enough for about 1-2 minutes
▪ Fetal circulation
o Fetal heart circulates oxygenated blood from the placenta throughout the body and returns deoxygenated blood
to the placenta
o Umbilical vein carries oxygenated blood to the fetus, and the two umbilical arteries carry deoxygenated blood
from the fetus to the placenta
▪ Regulation of fetal heart rate
1) Autonomic nervous system the sympathetic and parasympathetic branches of the autonomic nervous system
are balance forces that regulate FHR
▪ Sympathetic stimulation ↑ the heart rate and strengthens myocardial contractions through release of
epinephrine and norepinephrine
▪ The net result of sympathetic stimulation is an ↑ in CO
▪ Parasympathetic nervous system, through stimulation of the vagus nerve, reduces the FHR and
maintains variability
● Parasympathetic branch gradually exerts greater influence as the fetus matures, beginning
between 28 to 32 wks. of gestation
2) Baroreceptors cells that are sensitive to blood pressure changes
▪ located in the carotid arch and major arteries respond to stretching when the fetal BP ↑
▪ the baroreceptors stimulate the vagus nerve to slow the FHR and decrease the BP, thus lowering CO
3) Chemoreceptors cells that are sensitive to chemical changes in the blood, specifically changes in oxygen and
carbon dioxide levels, and changes in acid-base balance
▪ Found in the medulla oblongata and in the aortic and carotid bodies
▪ Decreased oxygen concentration, ↑ carbon dioxide content, or a lower pH in blood or cerebrospinal fluid
triggers an ↑ in the heart rate
● However, prolonged hypoxia, hypercapnia (excess carbon dioxide in the blood), and acidosis or
depletion of base depress the FHR17
4) Adrenal glandssecrete epinephrine and norepinephrine in response to stress, which causes a sympathetic
response that accelerates the FHR
▪ The adrenal cortex responds to a fall in the fetal blood pressure w/ release of aldosterone and retention
of sodium and water, resulting in an ↑ in the circulating fetal blood volume
5) Central nervous system responsible for the variations we see, along with the FHR when the baby is awake or
asleep
▪ The fetal cerebral cortex causes the heart rate to ↑ during fetal movement and decrease when the fetus is
quiet
▪ The hypothalamus coordinates the 2 branches of the autonomic nervous system: the sympathetic and
parasympathetic systems
▪ The medulla oblongata maintains the balance b/w stimuli that speed and slow the heart rate
Pathologic Influences on Fetal Oxygenation
▪ Maternal cardiopulmonary alterations (all of these effects the placental blood flow)
o Hemorrhage causes an actual in the mother’s blood volume
o Aortocaval compression can occur when the pregnant woman lies in the supine position and the weight of the
uterus compresses the aorta and the inferior vena cava
▪ It reduces blood return to her heart, lowers her CO (supine position), and can reduce placental perfusion
o Maternal hypertensionmay reduce blood flow to the placenta b/c of vasospasm and narrowing of the spiral
arteris
▪ HTN may be pregnancy induced or chronic or may result from ingestion of drugs such as cocaine
o Lowered oxygen level in the mother’s blood redcues the amt available to the fetus
▪ Maternal acid-base alterations that accompany resp. problems also can compromise exchange in the
placenta
▪ A lower maternal oxygen tension may result from resp. disorders such as asthma or from smoking
▪ Uterine activity
o Hypertonic uterine activity
▪ Reduces the time available for exchange of oxygen and waster products in the placenta
▪ Contractions may be too long or too frequent or have too short an interval
▪ Can occur spontaneously or with uterine stimulants such as oxytocin (Pitocin), prostaglandins, or
misoprostol (Cytotec)
o Placental disruptions
▪ Abruptio placentae partial separation before birth
o Interruptions in umbilical flow
▪ Nuchal cord or knot umbilical cord around the fetal body, often the neck
▪ Oligohydramnios inadequate amount of amniotic fluid--- may cause nuchal cord or knot d/t
inadequate fluid to cushion the cord
▪ Entangled between fetal body parts
▪ Inadequate Wharton’s jelly for cushioning
o Fetal alterations
▪ CNS or cardiac abnormalities may cause an abnormal rate or rhythm
▪ Risk factors
Auscultation and Palpation: Advantages
▪ Mobility
▪ Likely to change positions more often
▪ Water-based methods of pain management can be used more freely.
▪ Atmosphere more natural than technologic
▪ Less invasive
▪ Possible cost advantage
Auscultation and Palpation: Limitations
▪ Fetal heart rate (FHR) and uterine activity are assessed for a small percentage of the total labor.
▪ No continuous printed or computer-archived record
▪ Interruptions for auscultation may be distracting.
▪ Maternal obesity or large amniotic fluid volume may create difficulties.
▪ Staff-intensive
Auscultation and Palpation: Auscultation Equipment
▪ Fetoscope18
▪ Doppler ultrasound transducer (device that translates fetal heart motion into an electrical signal)
Auscultation and Palpation: Evaluation of Auscultated Fetal Heart Rate Data
▪ Fetoscope detects actual fetal heart sounds.
o Reliable for detecting fetal dysrhythmias
▪ Doppler transducer also used to detect baseline, rhythm, and changes in the baseline.
o Cannot be used to reliably detect dysrhythmias
Electronic Fetal Monitoring: Advantages
▪ Supplies more data about the fetus than auscultation
▪ Archives a permanent record on paper, computer media, or both
▪ Continuous electronic fetal monitoring (EFM) shows how the fetus responds before, during, and after each contraction.
▪ Allows one nurse to observe two laboring women
Electronic Fetal Monitoring: Limitations
▪ Reduced mobility
o Telemetry (wireless transmission) or intermittent monitoring gives the woman more freedom of movement than
continuous electronic monitoring without telemetry---otherwise, the woman is limited to her bed or a nearby chair
if EFM is continuous
▪ Frequent maternal position changes or an active fetus often requires constant equipment adjustment.
o Belts or stockinette bands, used to keep sensors positioned properly for external monitoring, are uncomfortable
for some woman
o Woman may concentrate on maintaining a good tracing rather than making herself comfortable or changing
positions that might enhance fetal descent
▪ The high-tech atmosphere created by the electronic fetal monitor may be objectionable to a woman and her partner
EFM, though used in more than 80% of births in the US, has not proved to be consistently reliable at identifying the fetus who is
truly in trouble
EFM best identifies the well-oxygenated fetus, but it does not as reliably identify the compromised fetus.. therefore, EFM
must be considered a screening tool, rather than a diagnostic tool
Electronic Fetal Monitoring: Equipment
▪ Bedside monitor unit
o Uses information form the fetal heart rate and uterine activity sensors to provide a visual output in the form of a
numeric displace and a graphic strip
▪ Paper strip
o Range of rates if from 30-240 bpm
▪ Data entry devices and computer software
▪ Remote surveillance
▪ Devices for external fetal monitoring
▪ Devices for internal fetal monitoring
o Use requires ruptured membranes and about 2 cm of cervical dilation
o Devices are invasive and risk of infection is slightly ↑
o Fetal scalp electrode (or spiral electrode) detects electric signals from the fetal heart
▪ Monitor unit generates a beeping sound w/ each fetal heartbeat
▪ This device may also be applied to the buttocks in a breech presentation
▪ Areas to avoid for electrode application are the fetal face, fontanels, and genitals
▪ Electrode wire protrudes from the mother’s vagina and is attached to a leg place on her thigh---a cord
from the leg plate connects to the bedside unit
▪ Because it barely penetrates the fetal skin (about 1mm), the electrode is easily displaced
o 2 kinds of intrauterine pressure catheters (IUPCs) can be used to measure uterine activity, including contraction
intensity and resting tone:
1) A solid catheter w/ a pressure transducer in its tip, which may have an additional lumen for
amnioinfusion ( infusion of a sterile isotonic solution into the uterine cavity during labor to reduce
umbilical cord compression; may also be done to dilute meconium in amniotic fluid and reduce the risk
that the infant will aspirate thick meconium at birth)
2) A hollow, fluid-filled catheter that connects to a pressure transducer on the bedside monitor unit
Evaluating Intermittent Auscultation and Palpation Data
▪ Evaluate in orderly fashion19
▪ FHR evaluated for
o Rate, counting the FHR for at least 30 seconds b/w contractions
o Regularity of rhythm
o Absence of decrease from baseline
▪ Contractions evaluated for
o Frequency: beginning of one contraction to the beginning of next
o Duration: beginning to end of one contraction
o Intensity (really gauged by IUPC/ palpating)
▪ Strength by PALPATION if monitoring external TOCO
● Nose (mild)
● Chin (moderate)
● Forehead (Hard)
▪ Strength by monitoring INTERNAL (IUPC)
o Resting interval (how far apart are contractions)
o Resting tone (when contraction went away, it went away completely, fundus =soft)
Evaluation of Electronic Fetal Monitoring Strips
▪ FHR baseline is the average heart rate, rounded to 5bpm, measured over 2 minutes of clear tracing within a 10-minute
window—during this 2 or more minutes, the uterus must be at rest, and episodes of significant ↑ or in rate must not
occur
o Normal:
▪ Rate that averages from 110-160 bpm. The preterm fetus at 26-28 wks often averages a rate at the upper
end of this range because the parasympathetic nervous system, which slows the rate, is immature. Some
healthy full-term fetuses have a rate that averages 100-110bpm
o Bradycardia:
▪ Less than 11- bpm, persisting for at least 10 minutes
o Tachycardia:
▪ More than 160 bpm, persisting for at least 10 minutes
▪ FHR variability
o Variability denotes the fluctuations in the baseline FHR within a 10-minute window that cause the printed line to
have an irregular rather than a smooth appearance
▪ 2 types of variability, short-term and long-term
o Variability occurs b/c multiple factors constantly speed and slow the fetal hear in a push- and –pull manner
▪ Adequate oxygenation promotes normal function of the autonomic nervous system and helps the fetus
adapt to the stress of labor
▪ Variability evaluates the function of the fetal autonomic nervous system, especially the parasympathetic
branch
o Factors that decrease
o Classification of variability
▪ Absent- undetectable
▪ Minimal- undetectable to ≤5 bpm
▪ Moderate- 6 to 25 bpm
▪ Marked - >25bmp
▪ Periodic patterns in FHR
o Accelerations an abrupt, temporary ↑ in the FHR that peaks at least
15 bpm above the baseline and lasts at least 15 seconds
▪ Often occur w/ fetal movement- may or may not have relation
to contractions
▪ Before 32 wks of gestation, temporary ↑ in the FHR that
peaks at least 10 bpm above the baseline and lasts at least
10 seconds is considered an acceleration
▪ Prolonged accelerations: accelerations lasting longer than 2
minutes but less than 10 minutes
o Decelerations
▪ Early (head compression)20
● Fetal head compression briefly ↑ intracranial pressure, causing the vagus nerve to slow the heart
rate
● Early decels are not associated w/ fetal compromise and require no intervention
● Occur during contractions as the fetal head is pressed against the woman’s pelvis or soft tissue
such as the cervix
● Have a gradual, rather than abrupt, decrease from the baseline
● Mirror the contraction, beginning near its onset and returning to the baseline by the end of the
contraction
● Usually no lower than 30-40 bpm
▪ Late (uteroplacental insufficiency)
● May be from deficient exchange of oxygen and waste products in the placenta
● This non-reassuring pattern suggests that the fetus has reduced reserve to tolerate the recurrent
reductions in oxygen supply that occur with contractions
● Lowest rate (30 to 40 bpm) but are shifted to the right in relation to the contraction
● Often begin after the peak of the contraction
● FHR returns to the baseline after the contraction ends
▪ Variable (cord compression)
● Conditions that reduce flow through the umbilical cord
● These decelerations do not have the uniform appearance of early and late decels
● Shape, duration and degree of fall below baseline vary
● They fall and rise abruptly (within 30 seconds) w/ the onset and relief of cord compression,
unlike the gradual fall and rise of early and late decels
● in FHR is at least 15 bpm and lasts at least 15 seconds but led than 2 minutes
▪ VEAL CHOP
o Variable Cord compression
Early Decels Head compression
Accelerations O2/OK
Late decels Poor placental perfusion
o Variable decelerations: cord compression=change moms position
o Early decelerations: head compression=change position
o Late decelerations: BAD= potential C-section
▪ O2 non-rebreather 8-10L, reposition
▪ STOP Pitocin if on it
▪ Vag exam
▪ PROLONGED LATE DECELS ARE BAD! Need baby to come back up to baseline
● Otherwise EMERGENCY C-section, baby needs O2
o Absent variability=BAD
o Marked variability=BAD
o Sinusoidal heart rate pattern=BAD/ EMERGENCY C-section
▪ Uterine activity
o Frequency: may be measure with the electronic monitor as w/ palpation or from peak to peak
o Duration: calculated from the beginning to end of each contraction
o Intensity of the contractions and Uterine resting tone palpitation is used to estimate contraction intensity and
uterine resting tone when an external uterine activity monitor is used
▪ Described as mild, moderate, or strong
▪ Intensity usually increases as labor progresses. Uterine contraction intensity with the IUPC is about 50 to
75 mm Hg during labor, although it may reach 110mm Hg w/ pushing during the second stage
● Average resting tone is 5-15 mm Hg
Significance of FHR Patterns
▪ Category 1: Normal (reassuring)
o Such as normal rate and accelerations and absence of nonreassuring decelerations are associated w/ fetal wellbeing21
o NO intervention is required---pattern suggests that the fetus has adequate reserves to tolerate intrapartum
stressors
▪ Category 2: indeterminate (often described as equivocal or ambiguous data)
o Often referred to as equivocal or ambiguous
o Describe patterns that have elements of reassuring characteristics but also data that may be nonreassuring
▪ Examples:
● Tachycardia
● Bradycardia w/ presence of variability
● Minimal or marked baseline variability
● Absent variability w/ no recurrent decelerations
▪ Category 3: abnormal (nonreassuring)
o If favorable signs are absent or if signs that are associated with fetal hypoxia or acidosis are present
o Does not necessarily indicate that fetal hypoxia or acidosis has occurred
o Indicate that steps should be taken to identify possible causes for these patterns
o More significant if they occur together and are persistent
o Clarification of data
▪ 2 methods are used during the intrapartum period: VAS and fetal scalp stimulation
▪ Analysis of umbilical cord blood gases and pH is used immediately after birth
▪ Fetal scalp blood sampling for blood gases is < common
▪ Fetal oxygen saturation monitoring had a brief trail w/ disappointing results and is no longer being done
o Vibroacoustic stimulation
▪ VAS- stimulation may be used by the nurse, physician, or nurse-midwife as the initial method to stimulate
the fetus or to supplement fetal scalp stimulation, or it may be used if scalp stimulation is contraindicated
▪ An artificial larynx or vibroacoustic stimulator is applied to the mother’s lower abdomen, and it is
turned on for up to 3 seconds. A reassuring response is an acceleration that peaks at 15 bpm for 15
seconds or more
▪ An absent response, however, does not necessarily mean that the fetus is suffering from hypoxia or
acidosis
o Fetal scalp stimulation “tickle” the top of babies head- see if you can get an↑ in FHR
▪ Scalp stimulation is used to evaluate the response of the fetus to tactile stimulation
▪ Nurse, physician, or nurse-midwife may perform this procedure
▪ Examiner applies pressure to the scalp (or other presenting part) w/ a gloved finger (or fingers) & sweeps
the fingers in a circular motion
▪ An FHR acceleration, as in VAS, is reassuring response that suggests the fetus is in normal oxygen and
acid-base balance
▪ Fetal scalp stimulation is NOT done in some cases:
● Preterm fetus (may cause contractions)
● Prolonged rupture of membranes (higher risk of infection)
● Chorioamnionitis (intrauterine infection)
● Placenta previa (placenta overlies ther cervix, and hemorrhage is likely)
● Maternal fever of unknown origin (possibility of introducing microorganisms into the uterus)
o Fetal scalp blood sample
▪ Normal scalp pH is 7.25 to 7.35
▪ Scalp sampling is less common b/c it is invasive and the results are not available immediately
o Fetal oxygen saturation monitor
o Cord blood gasses and pH (p.269)
▪ Umbilical cord blood analysis is used to assess the infant’s oxygenation and acid-base balance
immediately after birth
▪ Arterial cord blood best reflects fetal oxygenation b/c this blood is leaving the fetus on its way to the
placenta
▪ Cord is promptly double-clamped and cut to isolate a 10-30-cm segment
▪ Blood samples from an umbilical artery provide the most accurate info about the newborns acid-base
status
▪ Blood drawn into heparinized syringed to prevent coagulation, and the syringes are capped to avoid
altering values by exposure to room air22
Interventions for Category 3 Patterns
▪ Identify cause
▪ Improve fetal oxygenation
o Tocolytic drug--- such as “terbutaline” may be given to reduce uterine activity
▪ Increase maternal blood oxygen saturation
o 100% oxygen through a snug face mask makes more oxygen available for transfer to the fetus
o Common suggested rate is 8-10 liters per min (L/min)
▪ Reduce cord compression
o Amnioinfusion increases the fluid around the fetus and cushions the cord
▪ Lactated ringers solution or normal saline is infused into the uterus through an IUPC
Application of the Nursing Process: Intermittent Auscultation and Electronic Fetal Monitoring
▪ Learning needs
o Assessment
o Analysis
o Planning
o Interventions
o Evaluation
▪ Fetal oxygenation
o Assessment
▪ Evaluate the fetal monitoring strip systematically for the elements noted previously
▪ Following are recommended assessment and documentation intervals for both IA and EFM, although
facility policies may be diff.
● Low-risk women--- every 30 minutes during the active phase and every 15 minutes during the
second stage
● High-risk women----every 15 minutes during the active phase and every 5 minutes during the
second stage
▪ According to the American college of Obstetricians & Gynecologists:
● Active first-stage labor--- every 15 minutes
● Second-stage labor---every 5 minutes
▪ Take the woman’s temp every 4 hours (every 2 hours after membranes rupture)
▪ Asses pulse, RR and BP hourly
o Analysis
o Planning
o Interventions
o Evaluation
Chapter 15: Pain Management During Childbirth
Unique Nature of Pain During Birth
▪ Components of pain process
o A physiologic component, which includes reception by sensory nerves and transmission to the CNS
o A psychological component, which involves recognizing the sensation, interpreting it as painful, and reacting to
the interpretation
▪ Pain is subjective and personal.
▪ Differs from other types of pain
o Part of a normal process
o Preparation time exists.
o It is self-limiting there is an end in site
o Labor pain is not constant, but intermittent.
o Labor ends with the birth of a baby.
Adverse Effects of Excessive Pain
▪ Physiologic effects
o Fear and anxiety—which stimulates sympathetic nervous system activity and results in ↑ secretion of
catecholamines (epinephrine and norepinephrine)
▪ Catecholamines stimulate alpha and beta receptors-causing effects on the blood vessels and uterine
muscles
▪ Epinephrine stimulates both alpha and beta receptors, whereas norepinephrine stimulates primarily
alpha receptors23
▪ Stimulation of the alpha receptors cause uterine and generalized vasoconstriction and an ↑ in the uterine
muscle tone--- these effects reduce blood flow as they raise the maternal BP
▪ Stimulation of the beta receptors relaxes the uterine muscle and causes vasodilation
● However… the uterine vessels are already dilated in pregnancy, so dilation of other maternal
vessels allows the woman’s blood to pool in them. The pooling of blood reduces the amt of blood
available to perfuse the placenta
▪ Effects of excessive catecholamine secretion:
● Reduced blood flow to and from the placenta, restricting the fetal oxygen supply and waste
removal
● Reduced effectiveness of uterine contractions, slowing labor process
o Increases maternal metabolic and respiratory rate (demand for oxygen)
▪ Fetus may have < oxygen available for uptake and have less ability to unload carbon dioxide to the mother
▪ Net result is that the fetus shifts to anaerobic metabolism, w/ buildup of hydrogen ions (acidosis)
● This type of acidosis is metabolic, and does not resolve as quickly after birth as resp. acidosis,
which results from shorter periods of hypoxia
▪ Psychologic effects
o Poorly relived pain lessens the pleasure of this life event
o Mother may find it difficult to interact w/ her infant b/c she is depleted from a painful labor
Variables in Childbirth Pain: Physical Factors
▪ Childbirth pain is of 2 types: visceral and somatic
o Visceral slow, deep, poorly localized pain that is often described as dull or aching. Dominates during first-stage
labor as the uterus contracts and the cervix dilates
o Somatic quick, sharp pain that can be precisely localized. Most prominent during late first-stage labor and
during second-stage labor as the descending fetus puts direct pressure on maternal tissues
▪ Sources of pain
o Tissue ischemia blood supply to the uterus during contractions, leading to tissue hypoxia and anaerobic
metabolism. Ischemic uterine pain has been likeded to ischemic heart pain
o Cervical dilation dilation and stretching of the cervix and lower uterus are a major source of pain
▪ Pain stimuli from cervical dilation travel through the hypogastric plexus, entering the spinal cord at the
T10, T11, T12, and L1 levels
o Pressure and pulling on pelvic structures some pain results from pressure and pulling on pelvic structures such
as ligaments, fallopian tubes, ovaries, bladder and peritoneum
▪ Pain is visceral pain; a woman may feel it as referred pain in her back and legs
o Distention of the vagina and perineum marked distention of the vagina and perineum occurs w/ fetal descent,
especially during the second stage
▪ Woman may describe a sensation of burning, tearing, or splitting (somatic pain). Pain from vaginal and
perineal distention and pressure and pulling on adjacent structures enters the spinal cord @ S2, S3, and
S4 levels
▪ Tolerance or perception of pain
o Labor intensity may differ depending on the length of labor
o Cervical readiness if prelabor cervical changes (softening, w/ some dilation and effacement) are incomplete, the
cervix does not open as easily as it does when it is soft and dilation and effacement have begun
▪ More contractions are needed to achieve dilation and effacement, resulting in a longer labor and greater
fatigue in the laboring woman
o Fetal position labor Is likely to be longer and more uncomfortable when the fetus is in an unfavorable position
▪ An occiput posterior position is a common variant seen in otherwise normal labors--- this position, each
contraction pushes the fetal occiput against the woman’s sacrum
▪ She experiences intense back discomfort (back labor) that persists b/w contractions
● May not be able to deliver her baby until it rotates to the occiput anterior position
o Pelvic readiness size and shape of a woman’s pelvis influence the course and length of her labor
▪ Abnormalities may contribute to fetal malpresentation or malposition, resulting in a difficult and longer
labor
o Fatigue and hunger
o Caregiver interventions IV lines can cause pain when inserted, fetal monitoring is uncomfortable to some
woman, but others want to hear the sounds, a woman whose labor is induced or augmented often reports more
pain and ↑ difficulty coping w/ it b/c contractions reach peak intensity quickly24
Variables in Childbirth Pain: Psychosocial Factors
▪ Culture
▪ Anxiety and fear
▪ Previous experiences
▪ Preparation
▪ Support system
Nonpharmacologic Pain Management: Advantages
▪ Does not slow labor
▪ No side effects or risk of allergy
▪ Some pharmacologic methods may not eliminate labor pain.
▪ May be the only realistic option in advanced, rapid labor
Nonpharmacologic Pain Management: Limitations
▪ Desired level of pain control is not always achieved
▪ Even a well-prepared and highly motivated woman may have a difficult labor and need analgesia or anesthesia.
Nonpharmacologic Pain Management: Gate Control Theory
▪ Transmission of nerve impulses controlled by a neural mechanism in the dorsal horn of the spinal cord that acts like a gate
to control impulses transmitted to the brain
▪ Pain is transmitted through small-diameter sensory nerve fibers.
▪ Stimulation of large-diameter fibers in the skin blocks conduction of pain through small-diameter fibers, thereby “closing
the gate” and decreasing the amount of pain felt.
Nonpharmacologic Pain Management: Preparation for Pain Management
▪ Childbirth classes
▪ The ideal time to prepare is before labor.
▪ The support person learns specific methods to encourage and support.
▪ The nurse can teach or reinforce.
▪ The latent phase of labor is the best time for intrapartum teaching.
Nonpharmacologic Pain Management: Application of Techniques
▪ Relaxation
o Promotes uterine blood flow, improving fetal oxygenation
o Promotes efficient uterine contractions
o Reduces tension that ↑ pain perception and pain tolerance (maximum pain one is willing to endure)
o Reduces tension that can inhibit fetal descent
▪ Cutaneous stimulation
o Self-massage
o Massage by others
o counterpressure
▪ sacral pressure may help when the woman has back pain, usually most intense when her fetus is in an
occiput posterior position
o Touch
o Thermal stimulation
▪ Warmth applied to back, abdomen, or perineum during labor
▪ Warmth ↑ local blood flow, relaxes muscles, and raised the pain threshold
o Acupressure
▪ Directed form of massage in which the support person applied pressure to specific pressure points using
hands, rollers, balls, or other equipment
▪ Hydrotherapy
o Water therapy can supplement any relaxation technique
o Buoyancy supports body, equalizing pressure, aids in muscle relacation
o Fluid shifts from the extravascular space to the intravascular space, reducing edema as the excess fluid is excreted
by the kidneys
▪ Mental stimulation
o Imagery
o Focal point
▪ Breathing techniques
o First-stage breathing
▪ Taking a cleansing breath (each contraction begins and ends with a deep inspiration and expiration)25
▪ Slow-paced breathing
▪ Modified paced breathing
▪ Patterned-paced breathing (AKA paint-blow breathing)
▪ Breathing to prevent pushing
▪ Overcoming common problems
o Second stage breathing
Pharmacologic Pain Management
▪ Effect on the fetus
▪ Maternal physiologic alterations
o Cardiovascular changes
o Respiratory changes
▪ Full uterus reduces her respiratory capacity
o GI changes
▪ Pregnant woman’s stomach is displaced upward by her large uterus and has a higher internal pressure
▪ Progesterone slows peristalsis and reduces the tone of the sphincter at the junction of the stomach and
esophagus--- these changes make a pregnant woman vulnerable to regurgitation and aspiration
(inhalation) of gastric contents during general anesthesia
o Nervous system changes
▪ Circulating levels of endorphins (substance similar to opioids that occurs naturally in the CNS and modifies
pain sensations; r/t enkephalins) and enkephalins (same as endorphins) are high--- these substances
modify pain perception and reduce requirements for analgesia and anesthesia
▪ Epidural and subarachnoid spaces b/w the arachnoid mater and pia mater are smaller during pregnancy,
enhancing the spread of anesthetic agents used for epidural blocks or subarachnoid blocks
▪ Effects on the course of labor
▪ Effects of complications
▪ Interactions with other substances
Combined spinal epidural (CSE) analgesia allows subarachnoid injection of opioids via a spinal needle followed by ongoing pain
relief from anesthetics injected through the epidural catheter
Regional Pain Management: Epidural Block
▪ Injecting a local anesthetic agent, often combined with an opioid, into epidural space
o Epidural space outside the dura mater, b/w the dura and the spinal canal—it is loosely filled w/ fat, connective
tissue, and epidural veins that are dilated during pregnancy
▪ Provides substantial relief of pain from contractions and birth canal distention
▪ Can be extended upward
▪ Analgesia, rather than full anesthesia
▪ Adequate pain relief without complete motor block
▪ Exact time to being an epidural block is individualized: started just before a scheduled cesarean birth, and for labor, the
best time to start the block is when the woman is in active labor, to avoid slowing progress
▪ Epidural space: entered at about L3-L4 interspace (below the end of the spinal cord) and a catheter is passes through the
needle into the epidural space
o Catheter allows continuous infusion or intermittent injection of medication to maintain pain relief during labor and
vaginal or cesarean birth
▪ ALL DRUGS INJECTED INTO THE EPIDURAL OR SUBARACHNOID SPACES MUST BE PRESERVATIVE FREE
o Fentanyl (Sublimaze)
o Sufentanil (Sufenta)
o Ropivacaine (Naropin)
o Morphine (Duramorph, Astramoprh)
▪ Adverse effects of epidural opioids
o N/V
o Pruritus
▪ Itching of the face and neck
o Delayed respiratory depression
Regional Pain Management: Intrathecal Opioid Analgesics
▪ Injected into the subarachnoid space where it binds to opiate receptors, allowing much smaller doses than would be
adequate if given systemically26
▪ Advantages:
o Rapid onset of pain relief without sedation
o No motor block, enabling the woman to ambulate during labor
o No sympathetic block, with its hypotensive effects
▪ Disadvantages:
o Limited duration of action, possibly requiring another procedure for continued pain relief
o Inadequate pain relief for late labor and the birth, requiring added measures to manage pain at these times
▪ Much smaller doses than if given systemically
▪ Woman can feel her contractions
▪ Rapid onset of pain relief without sedation
▪ Can ambulate during labor
▪ No sympathetic block
▪ Limited duration of action
▪ Inadequate pain relief for late labor and the birth
Regional Pain Management: Subarachnoid Block (SAB)
▪ Simpler procedure than the epidural block
▪ May be performed when a quick cesarean birth is
necessary
▪ Performed just before birth, providing no pain relief
during most of labor
▪ Adverse effects:
o Maternal hypotension
o Bladder distention
o Postdural puncture headache
Subarachnoid Block
Level of Anesthesia
Blood Patch
Regional Pain Management: Systemic Drugs
▪ Nitrous Oxide27
o “laughing gas”
o Gas is delivered as 50 percent nitrous oxide and 50 percent oxygen
o Woman controls when she takes breaths of the 50-50 combination
▪ Parenteral analgesia (opioid analgesics) most common parenteral medication given to reduce perception of pain w/out
loss of consciousness
o Demerol (meperidine) often produces a dysphoric rather than an analgesic effect in the woman
▪ Half-life of 3 to 6 hours in the woman but 3 days or longer in the newborn
▪ Infrequently used for labor
▪ Pure opioid agonists
▪ Used to shut the gate (gate control therapy)--- stopping the sensation where it is not getting to the
neurons so we are able to stop the process of pain
o Sublimaze (fentanyl) pure opioid agonists (or substances that cause a physiologic effect)
o Stadol (butorphanol) mixed opioid agonist and antagonist (substance that blocks another substance or body
secretion)
o Nalbuphine (Nubain) mixed opioid agonist and antagonist
▪ Duration 3-6 hrs (pg.291)
▪ Opioid antagonists
o Naloxone (Narcan)
▪ Reverses opioid-induced resp. depression, although it is seldom used in obstetrics
▪ Does not reverse resp. depression from other causes such as barbiturates, anesthetics, nonopioid drugs,
or pathologic conditions
▪ Has a shorter duration of action than most of the opioids it reverses, and resp. depression may recur
▪ Can induce withdrawal symptoms in an opiate-dependent woman or newborn
▪ Naltrexone (Trexan) may be given for pruritus relief (opioid antagonist)
▪ Adjunctive drugs (given during the intrapartum period include those w/ antiemetic and tranquilizing effects and sedatives)--
- given to reduce nausea and anxiety to promote rest
o Phenergan (promethazine)
▪ IV from must be very diluted
▪ IM (preferred but painful)
o Vistaril (Hydroxyzine)
▪ Antihistamine w/ antiemetic effects
● IM, w/ deep Z-track technique
● NOT GIVEN BY IV ROUTE
▪ Sedatives
Regional Pain Management: Local Infiltration Anesthesia
▪ Local anesthetic
▪ Just prior to episiotomy or suture of laceration
▪ Does not alter pain from uterine contractions or distention of the vagina
▪ Rarely has adverse effects on either mother or infant
Regional Pain Management: Pudendal Block
▪ Anesthetizes the lower vagina and part of the perineum
▪ Provides anesthesia for an episiotomy and vaginal birth
▪ Does not block pain from uterine contractions
▪ Mother feels pressure.
Local Anesthesia
Pudendal Block
Regional Pain Management: General Anesthesia
▪ Systemic pain control
▪ Loss of consciousness
▪ Rarely used for vaginal births
▪ Still has a place in cesarean birth
▪ May be needed unexpectedly and quickly for emergency procedures at any stage of pregnancy
▪ Before induction of anesthesia, a woman breathes oxygen for 3-5 minutes, or at least 4 deep breaths, to ↑ her oxygen
stores and those of her fetus for the short period of apnea during rapid anesthesia induction
▪ Adverse Effects:
o Maternal aspiration of gastric contents28
▪ Aspiration pneumonitis: chemical injury to the lungs that may occur w/ regurgitation and aspiration of
acidic gastric secretions
o Respiratory depression
o Uterine relaxation
Chapter 16: Nursing Care During Obstetric Procedures
Amniotomy: Artificial Rupture of Membrane
▪ Indications
o Induce labor scheduled event—come in to hospital and start the process
▪ Artificial initiation
o Augment labor patient already in labor, but may not be progressing the way they want
▪ Artificial stimulation of ineffective uterine contractions
▪ Augmentation with oxytocin is considered when labor has begun spontaneously but progress has slowed
or stopped, even if contractions seem to be adequate
o Allow internal fetal monitoring
▪ Risks
o Prolapse cord primary risk that the umbilical cord will slip down in the gush of fluid
▪ Cord can be compressed b/w the fetal presenting part and the woman’s pelvis, obstructing blood flow to
and from the placenta and reducing fetal gas exchange
o Infection with interruption of the membrane barrier, vaginal organisms have free access to the uterine cavity
and may cause chorioamnionitis (inflammation of the amniotic sac, usually caused by bacterial and viral
infections )
▪ Risk is low at first but ↑ as the interval b/w membrane rupture and birth ↑
▪ Birth within 24 hours of membrane rupture is desirable, although infection does not occur at any absolute
time
o Abruptio placenta (premature separation of a normally implanted placenta) can occur if the uterus is
distended w/ excessive amniotic fluid when the membranes rupture
▪ As the uterus collapses w/ discharge of the amniotic fluid, the area of placental attachement shrinks
▪ Placenta then no longer fits its implantation site and partially separates
▪ Large area of placental disruption can significantly reduce fetal oxygenation, nutrition, and waste disposal
▪ Technique
o Done by physician or nurse-midwife
o Amnihook snags membrane
o Amniotomy is often deferred if the fetal presenting part is high or the presentation is not cephalic
o Risk of a prolapsed cord is higher is these situations because more room is available for the cord to slip down
o Noncephalic= more likely to be cesarean birth & amniotomy is done at the time of surgery through the
abdominal and uterine incisions
▪ Nursing considerations
o Obtain baseline information
▪ Fetal heart rate (FHR) 20 to 30 minutes before procedure
o Assist with procedure
▪ Place absorbent pads
▪ Equipment
o Provide care after procedure
▪ Identify complications
● The FHR is assessed for at least 1 full minute after amniotomy
● Cord compression is usually accompanied by a rate less than 100 bpm
● Large amt of vernix in the fluid suggests that the fetus may be preterm
● Greenish, meconium stained fluid may be seen in postterm gestation or placental insufficiency
● fluid with a foul or strong odor, cloudy appearance, or yellow color suggests chorioamnionitis
● fetus w/ prolonged oligohydramnios may have respiratory problems after birth b/c the lungs
cannot expand normally
● women’s temp should be assessed at least every 2-4 hours after the membranes rupture (>100.4
should be reported)
▪ Promote comfort
Induction and Augmentation of Labor
▪ Artificial methods to stimulate uterine contractions29
Induction and Augmentation of Labor: Indications
▪ Hostile intrauterine environment
▪ Spontaneous rupture of the membranes (SROM)
▪ Post-term pregnancy
▪ Chorioamnionitis (inflammation of the amniotic sac)
▪ Hypertension
▪ Abruptio placentae
▪ Maternal medical conditions that worsen with continuation of the pregnancy
▪ Fetal death
Induction and Augmentation of Labor: Contraindications
▪ Placenta previa placental implantation of the lower uterus, which would result in hemorrhage during labor
▪ Vasa previa fetal umbilical cord vessels branch over the amniotic sac rather than inserting into the placenta; fetal
hemorrhage Is a possibility if the membranes rupture
▪ Umbilical cord prolapse b/c immediate cesarean is indicated to stop cord compression
▪ Abnormal fetal presentation for which vaginal birth is often more hazardous
▪ ▪
Fetal presenting part above the pelvic inlet which may be associated w/ cephalopelvic disproportion (fetal head that is
too large to fit through the mother’s pelvis) or a preterm fetus
▪ Previous surgery in the upper uterussuch as a previous classical cesarean incision or extensive surgery for uterine
fibroids
Induction and Augmentation of Labor: Risks (**pg.306)
▪ Hypertonic uterine activity (excessive frequency, duration, or intensity of contractions) can reduce placental perfusion
and fetal oxygenation
o Contraction duration longer than 90-120 seconds
o Contractions occurring less than 2 minutes apart or relaxation of less than 30 seconds b/w contractions
o Montevideo units exceeding 400
▪ Uterine rupture
▪ Maternal water intoxication
▪ Greater risk for chorioamnionitis
▪ Greater risk for cesarean birth
Induction and Augmentation of Labor: Techniques
▪ Determining whether induction is indicated
o Gestational age
o Cervical assessment (Bishop Score) don’t worry about this! Will NOT cover
▪ Cervical ripening
o Procedures to ripen (soften) the cervix and make it more likely to dilate w/ the forces of labor are a common
adjunct to induction
o Medical methods
▪ Prostaglandin may be used to cause cervical ripening
● Prostaglandin E2
▪ Misoprostol (Cytotec) is a prostaglandin E1 analog usually given for gastric ulcers
● Can be used for both cervical ripening and induction of labor
o Mechanical methods
▪ Hydrophilic (moisture- attracting) inserts into the cervical canal, where they absorb water and swell,
gradually dilating the cervix
● Ex:
o Dilapan- synthetic material
o Lamicel- synthetic sponge containing 450 mg of magnesium sulfate
o Laminaria tents- sterile, cone-shaped preparations of dried seaweed
Induction and Augmentation of Labor: Techniques (Cont.)
▪ Oxytocin administration
o Dilute in an isotonic solution
o Secondary (piggyback) infusion --- so it can be stopped quickly if complications develop
o Insert oxytocin line into the primary intravenous line---as close as possible to the venipuncture site to limit the
amount of drug infused after changing to the nonaddictive fluid
o Start slowly, increase gradually30
o Monitor uterine activity, FHR, and fetal heart patterns frequently (before induction for a baseline, when it’s started
and throughout labor)
o Woman’s uterus becomes more sensitive to oxytocin as labor progresses
o WHEN LABOR IS AUGMENTED W/ OXYTOCIN, A LOWER TOTAL DOSE USUALLY IS NEEDED TO ACHIEVE
ADEQUATE CONTRACTIONS
▪ Serial induction of labor (p.308)
o May be performed when the woman’s cervix is not favorable and she has an indication for induction but same-day
birth is not imperative
o Oxytocin solution is given over a 2-3 day period for about 8-10 hours each day
o If woman’s labor has not made progress during the day, the oxytocin is stopped, she is given a light mean, and the
infusion is resumed the next morning
o At the end of the third day, the woman is reevaluated if she is not yet in labor
Induction and Augmentation of Labor: Nursing Considerations (**pg. 308)
▪ Observe fetal response
o Oxytocin stimulated uterine contractions, and they may become too strong (tachysystole)
▪ Tachysystole may reduce placental blood flow (uteroplacental insufficiency), which decreases exchange of
fetal oxygen and waste products
o Hypertonic contractions reduce uteroplacental blood flow.
o Assess FHR pattern
o Reduce or stop infusion for nonreassuring FHR.
o Sidelying position
o Oxygen by facemask
o Physician may order a drug such as terbutaline (Brethine) or magnesium sulfate to reduce uterine activity
Induction and Augmentation of Labor: Nursing Considerations (Cont.)
▪ Observe maternal response
o Assess uterine activity
o Assess blood pressure and pulse
o Be aware of pain management techniques
o Record intake and output
o Observe for signs of water intoxication
▪ Headache, blurred vision, behavioral changes, increased BP and RR, decreased pulse, rales, wheezing, and
coughing
o Assess for uterine atony in postpartum periodmore likely if she has received oxytocin for a long time b/c the
uterine muscle becomes fatigues and does not contract effectively to compress vessels at the placental site
▪ Manifested by a soft uterine fundus and excess amounts of lochia, usually w/ large
clots
▪ Prolonged uterine relaxation may cause postpartum hemorrhage
o Observe for postpartum hemorrhage caused by uterine relaxation
o Woman’s BP and pulse rate are taken every 30 minutes or w/ each oxytocin dose change
increase to identify changes from her baseline
o Temp is checked every 2-4 hours to identify infection
Version: Indications
▪ External version
o Change the fetal position from a breech, shoulder (transverse lie), or oblique presentation to
cephalic
o Successful version may allow the woman to avoid a cesarean birth by increasing her change for vaginal birth
▪ Internal version
o Change the position of a second twin in a vaginal birth
Version: Contraindications
▪ Usually not done if a woman is likely to deliver vaginally
▪ Uterine malformations
▪ Previous cesarean
▪ Fetal size ≥4000 g
▪ Cephalopelvic disproportion
▪ Placenta previa placental implantation of the lower uterus31
▪ Multifetal gestation
▪ Oligohydramnios
▪ Ruptured membranes
▪ Cord around the fetal body or neck (nuchal cord) (C.A.N.)
▪ Uteroplacental insufficiency
▪ Engagement of the fetal head
▪ Placenta previa
Version: Risks
▪ Few risks to the woman are present.
▪ Few serious fetal risks exist.
▪ Fetus may become entangled in the umbilical cord---compressing its vessels and resulting in hypoxia
▪ Abruptio placentae may occur---if fetal manipulation disrupts the placental site
▪ Mixing of fetal and maternal blood--- could become mixed within placental vessels, possibly resulting in maternal
sensitization to the fetal blood time
Version: Techniques
▪ External version
o Nonstress test (NST) or BPP is done to evaluate fetal well-being
o If nonreassuring fetal signs are present, the version is not performed
o Determine gestational age beyond 37 weeks
o ECV usually attempted after 37-39 wks of gestation but before the woman is in labor for following reasons:
▪ As term nears, the fetus may spontaneously turn to cephalic presentation
▪ Fetus more likely to return to an abnormal presentation if version is attempted before 37 wks of gestation
▪ Fetal compromise and onset of labor occur, a fetus born after 37 wks of gestation is not likely to have
major problems associated w/ preterm birth, such as resp. distress syndrome
o Administer tocolytic (terbutaline) drug to relax uterus while version is performed
▪ Onset of action is 6 to 15 minutes after subcutaneous injection
o Epidural or spinal block may be given to reduce the mother’s discomfort as the physician manipulates the fetus
o Use ultrasound to guide manipulations
o Rho(D) immune globulin (RhoGAM) given if indicated
▪ Internal version
o Uncommon procedure, most often for the second twin after the first delivers in the cephalic presentation
Version: Nursing Considerations
▪ Provide information
▪ Promote maternal and fetal health
o Woman should have nothing by mouth 4 hours before and during this short procedure in case a cesarean is
needed quickly
o An IV line is placed for possible drug administration of fluid resuscitation if the FHR is not reassuring (category
III)
▪ Maternal vital signs are taken every 15- 30 minutes until they return to her baseline level---pulse rate should be no higher
than 120bpm
▪ Reduce anxiety
Operative Vaginal Birth
▪ Also called “forceps or vacuum extraction”---may be used by the physician to apply traction to the fetal head during birth,
aiding the woman’s expulsive efforts
▪ Vacuum extractor used suction to grasp the fetal head while traction is applied (used more than forceps)
o Not used for the fetus of 34 wks or less gestation b/c the suction is more likely to injure the head, scalp, and
intracranial vessels
o NO MORE THAN 3 “POP-OFFS” of the vacuum extractor should be allowed, and they should not be followed by
attempts to deliver w/ forceps
o May create scalp edema called a chignon at the application area
▪ Forceps curved, metal instruments w/ 2 curved blades that can be locked in the center
o blades may be closed or open and are shaped to grasp the fetal head
o Foam pads are available to cushion the fetal head from the blades
o Piper forceps are a special type used to assist birth of the head, as it is born last in a vaginal breech birth
Operative Vaginal Birth: Indications
▪ Shortened second stage of labor---- for the well-being of the woman, fetus, or both32
▪ Maternal indications
o Exhaustion
o Inability to push effectively
o Cardiac and pulmonary disease
▪ Fetal indications
o Nonreassuring FHR patterns
o Failure of the fetal presenting part to fully rotate and descend in the pelvis
o Partial separation of the placenta
o Nonreassuring FHR patterns near the time of birth
Operative Vaginal Birth: Contraindications
▪ Cesarean birth preferable
o Severe fetal compromise
o Acute maternal conditions
o High fetal station
o Cephalopelvic disproportion
Operative Vaginal Birth: Risk
▪ Trauma to maternal and fetal tissues
▪ Maternal risks include laceration and hematoma of the vagina
▪ Infant may have ecchymoses, facial and scalp lacerations and abrasions, facial nerve injury, cephalhematoma, subgaleal
hemorrhage, and intracranial hemorrhage
Operative Vaginal Birth: Technique
▪ Preparation of woman
o Empty bladder
o Cervix completely dilated and membrane ruptured
o Adequate anesthesia usually a regional block such as an epidural
▪ Classification of techniques
o Outlet: fetal head on perineum
o Low: leading edge of fetal skull at station +2
o Mid: leading edge of fetal skull between 0 and +2
▪ Forceps: locking blades applied to fetal head
▪ Vacuum extraction: cup attached to fetal head and traction applied
▪ An episiotomy (surgical incision of the perineum to enlarge the vaginal opening) may be performed as the fetal head
distends the perineum
Operative Vaginal Birth: Nursing Considerations
▪ Observe mother for trauma after birth.
o Bright red bleeding with firm fundus
▪ Observe neonate for trauma after birth.
o Facial asymmetry
Episiotomy
▪ Incision of the perineum just before birth
Episiotomy: Indications
▪ Shoulder dystocia in which the shoulder of a fetus becomes lodged under the mother’s symphysis during birth
▪ Vacuum or forceps-assisted births
▪ Face presentation—occiput posterior
▪ Preterm fetus--- an episiotomy will help reduce pressure on the preterm fetuses head
Episiotomy: Risks
▪ Infection
▪ Perineal pain
▪ Midline episiotomies--- increase a woman’s risk of the more extensive 3rd degree (into the anal sphincter) or fourth-degree
(through the rectal sphincter) tear
▪ Spontaneous lacerations are more likely to occur if a woman has an episiotomy w/ a previous pregnancy
Episiotomy: Technique
▪ Done when the fetal presenting part has crowned to a diameter of about 3-4 cm
▪ 2 types:
o Median (midline33
o Mediolateral
Episiotomy: Nursing Considerations
▪ Promote gradual stretching of perineum during second stage
o Perineum massage
▪ Delay pushing until the urge is felt
▪ Push with an open glottis
▪ Observe for hematoma and edema
Cesarean Birth: Indications
▪ Dystocia difficult or prolonged labor; often associated w/ abnormal uterine activity and cephalopelvic disproportion
▪ Cephalopelvic (fetopelvic) disproportion
▪ Hypertension
▪ Maternal diseases
▪ Active genital herpes
▪ Some previous uterine surgical procedures
o Classic cesarean incision
o Removal of fibroid tumors
▪ Persistent nonreassuring FHR patterns
▪ Prolapsed umbilical cord
▪ Fetal malpresentations
▪ Hemorrhagic conditions
Cesarean Birth: Contraindications
▪ Fetal death
▪ Immature fetus
▪ Maternal coagulation defects
Cesarean Birth: Maternal Risks
▪ Infection
▪ Hemorrhage
▪ Urinary tract trauma or infection
▪ Thrombophlebitis, thromboembolism
▪ Paralytic ileus (lack of movement in the intestines)
▪ Atelectasis
▪ Anesthesia complications
Cesarean Birth: Fetal Risks
▪ Lung immaturity is the greatest risk if the fetus is delivered preterm.
▪ Inadvertent preterm birth
▪ Transient tachypnea
▪ Persistent pulmonary hypertension of
the newborn
▪ Traumatic injury
Cesarean Birth: Technique
▪ Preparation
o Anesthesia
o Medication
▪ Famotidine (Pepcid) or
sodium citrate w/ citric
acid (Bicitra) is given to
reduce gastric acidity
b/f surgery
o Laboratory studies
o Prophylactic antibiotics
o Skin prep
o Foley catheter
▪ Incision (**pg. 318**)
o Low transverse (Pfannenstiel)**
▪ Preferred because of
its low risk for rupture34
in subsequent pregnancies
o Low vertical
o Classical vertical incision into the upper uterus
▪ Must be used when the other 2 incisions are not possible, such as when a placenta previa is located in the
lower anterior uterus
▪ More likely to rupture during later pregnancies
o Skin Incisions
Cesarean Birth: Nursing Considerations
▪ Provide emotional support
▪ Teach
▪ Promote safety
▪ Provide postoperative care
o Assessments are done q15 minutes during the first 1-2hrs and progress to q30 minutes to 1hr until she is
transferred to her postpartum room
Chapter 17: Postpartum Physiologic Adaptations
Reproductive System Changes
AFTER 14 DAYS… YOU SHOULDN’T BE ABLE TO FEEL THE FUNDUS ANYMORE
▪ Involution of uterus
o Refers to the changes the reproductive organs, particularly the uterus, undergo after childbirth to return to their
nonpregnant size and condition
▪ Involves 3 processes:
1) Contraction of muscle fibers
2) Catabolism (the process of converting cells into simpler compounds)
3) Regeneration of the uterine epithelium
o Involution begins immediately after delivery of the placenta, when uterine muscle fibers contract firmly around
maternal blood vessels at the area where the placenta was attached
o The contraction controls bleeding from the area left denuded when the placenta separated
o The uterus decreased in size as muscle fibers, which have been stretched for many months, contract and gradually
regain their former contour and size
o Regeneration of the uterine epithelial lining begins soon after childbirth
▪ Outer portion of the endometrial layer is expelled w/ the placenta
▪ Within 2-3 days, the remaining decidua (endometrium during pregnancy) separates into 2 layers
1) Superficial and is shed in the lochia
2) The basal layer containing the residual endometrial glands remains to provide the source of new
endometrium
▪ Regeneration of the endometrium, except at the site of placental attachment, occurs by 2-3 wks after
birth
▪ Exfoliation (scaling off of dead tissue)--- healing process after birth
▪ Descent of uterine fundus
o Location of the uterine fundus helps determine whether involution is progressing normally
o Immediately after delivery, the uterus is about the size of a large grapefruit or softball and weighs approximately
1000g
o Fundus can be palpated midway b/w the symphysis pubis and umbilicus and in the midline of the abdomen
o Within 12 hours the fundus rises to approximately the level of the umbilicus
o Fundus descends by approx.. 1 cm, or one fingerbreadth, per day
o By the 14th day, it has descended into the pelvic cavity and cannot be palpated abdominally
o Subinvolution delayed return of the uterus to its nonpregnant size and consistency
▪ Can cause postpartum hemorrhage
o Within 1 wk, the weight of the uterus decreases to about 500g; at 4 wks, the uterus weighs 100g or less
▪ Afterpains
o Intermittent uterine contractions
o Oxytocin, released from the posterior pituitary to stimulate the milk-ejection reflex, causes strong contractions of
uterine muscles
▪ Lochia bleeding following the delivery- asses how much
o lochia rubra: 1-3 days dark red/ or reddish brown that occurs immediately after childbirth; composed mostly of
blood ---with small particles of decidua and mucus35
▪ amount of blood when leukocytes begin to invade the area
o Lochia serosa: 3-10 days color changes from red to pink or brown-tinged
▪ Composed of serous exudate, erythrocytes, leukocytes, and cervical mucus
▪ By about the 10th day, the erythrocyte component decreases
o Lochia alba: 10- 14 days/ or persist until the end of the 3rd to 6th week
▪ discharge becomes white, cream, or light yellow in color
▪ Contains leukocytes, decidual cells, epithelial cells, fat, cervical mucus, and bacteria
▪ Cervix
o Immediately after childbirth the cervix is dilated, edematous, and bruised
o Small tears or lacerations may be present
o Rapid healing takes place, and by the end of the first week the external cervical os is 1cm in diameter
o May be some edema for as long as 3-4 months
o Shape of the external os is permanently changed
o Remains slightly open and appears slitlike rather than round, as in the nulliparous woman
▪ Vagina
o Vaginal rugae (folds) reappear by 3-4 wks, 6 to 10 wks are needed for the vaginal epithelium to be restored
o During the postpartum period, vaginal mucosa becomes atrophic and vaginal walls do not regain their thickness
until estrogen production by the ovaries is reestablished
o Lactating mothers may experience vaginal dryness (resulting from inadequate estrogen) and may experience
dyspareunia (discomfort during intercourse)
▪ Perineum
o After childbirth, the perineum may be edematous and bruised. If the woman has an episiotmy, a surgical incision
of the perineal area, it will begin to heal in 2-3 wks . Complete healing of the episiotomy site may take 4-6 months
o The episiotomy may be a median or midline incision, extending straight back from the lower edge of the introitus
toward the anus
Reproductive System Changes: Involution of Uterus
▪ Contraction of muscle
o Controls bleeding from site of placental attachment
o Decreases size of uterus
▪ Catabolism
o Reduction in cell size
o Byproducts are excreted in urine
▪ Regeneration of uterine epithelium
o First layer: decidua
o Basal layer
o Endometrial layer
Reproductive System Changes: Descent of Uterine Fundus
▪ Assess fundal height
▪ Document in relation to umbilicus
Reproductive System Changes: After Pains
▪ Etiology
o More acute for multiparas
o More severe with overdistention
o More severe during breastfeeding caused by release of oxytocin
▪ Nursing considerations
o Analgesic frequently used
o Medicate before breastfeeding
o Enhance comfort and relaxation to facilitate letdown of milk
o Prone position may provide relief
Reproductive System Changes: Lochia
▪ Changes in color
o Lochia rubra: first 3 days
o Lochia serosa: days 4 through 10
o Lochia alba: after day 10
▪ Amount difficult to quantify36
o Scant: less than a 2.5-cm (1-inch) stain on the peripad
o Light: less than 10-cm (4-inch) stain
o Moderate: less than 15-cm (6-inch) stain
o Heavy: saturated peripad in 1 hour
o Excessive: saturated peripad in 15 minutes
Reproductive System Changes: Cervix
▪ Dilated, edematous, and bruised
▪ Small tears or lacerations may be present.
▪ Rapid healing takes place.
Reproductive System Changes: Vagina
▪ Greatly stretched
▪ Walls appear edematous
▪ May have multiple small lacerations
▪ Few vaginal rugae (folds) are present
o Rugae begin to reappear by 3 to 4 weeks
o Vaginal epithelium restored 6 to 10 weeks
▪ Vaginal wall regains thickness.
▪ Dyspareunia (discomfort during intercourse)
Reproductive System Changes: Perineum
▪ Pelvic floor muscles stretch and thin.
▪ May be edematous and bruised
▪ Laceration and episiotomy
▪ Discomfort
▪ Nursing considerations
o Relief of perineal discomfort
o Teaching self-care measures
Cardiovascular System Changes: Cardiac Output
▪ Hypervolemia, which produces an average 30% to 45% ↑ in blood volume at term, allows the woman to tolerate a
substantial blood loss during childbirth
o Up to 500mL of blood is lost in vaginal deliveries
o Up to 1000mL is lost in cesarean births
▪ Despite the blood loss, a transient ↑ in maternal CO occurs after childbirth--- ↑ caused by:
1) Increased flow of blood back to the heart when blood from the uteroplacental unit returns to the central circulation
2) Decreased pressure from the pregnant uterus on the vessels
3) Mobilization of excess extracellular fluid into the vascular compartment
▪ Rise in CO returns to prelabor values within an hour after delivery
▪ Cardiac output returns to prepregnancy levels in most women by 6 to 12 weeks.
Cardiovascular System Changes: Plasma Volume
▪ Body rids itself of excess fluid
o Diuresis (increased excretion of urine)
▪ Facilitated by a decline in the adrenal hormone aldosterone, which is increased during pregnancy to
counteract the salt-wasting effect of progesterone
● Aldosterone production decreases, sodium retention declines and fluid excretion accelerates
o Diaphoresis (profuse perspiration)
Cardiovascular System Changes: Blood Values
▪ White blood cell count increased
▪ An ↑ of over 30% within 6 hours may indicate infection
o The WBC falls to normal values by 6 days after birth
▪ Hemoglobin and hematocrit difficult to interpret
o Remobilization and rapid excretion of excess body fluid
o Hematocrit is low when plasma ↑ and dilutes the concentration of blood cells and other substances carried by the
plasma
▪ As excess fluid is excreted, the dilution is gradually reduced
o Hematocrit should return to normal within 4 to 8 weeks unless excessive blood loss has occurred
Cardiovascular System Changes: Coagulation
▪ During pregnancy, plasma fibrinogen and other factors necessary for coagulation increase37
o Fibrinolytic activity (ability to break down clots) is decreased during pregnancy
▪ At risk for thrombus formation during pregnancy and postpartum period
▪ Takes 4-6 wks before the hemostasis returns to normal nonpregnant levels
▪ Decreased risk for thrombophlebitis with early ambulation
▪ Monitor high-risk clients carefully.
Gastrointestinal System Changes
▪ Digestion
o Begins to be active soon after childbirth (hunger and thirst)
▪ Constipation
o Common problem during the postpartum period
o Bowel tone and motility, which were diminished during pregnancy as a result of progesterone, remain sluggish for
several days
o In addition, relaxation of the abdominal muscles increases constipation and distention w/ gas
o Decreased food and fluid intake during labor often results in small, hard stools
o Women who are taking iron have an added cause of constipation
▪ Stool softeners
o Often prescribed
o First stool usually occurs within 2-3 days postpartum
o Normal patterns of bowel elimination generally resume by 8-14 days after birth
Urinary System Changes
▪ Physical changes
o Kidneys return to normal function by 4 wks after delivery
o Dilation of the renal pelvis and the ureters that occurs during pregnancy ends within 2-8 wks
o Acetone in urine
▪ Acetone suggest dehydration that often occurs during the exertion of labor
o Proteinuria
▪ Mild proteinuria usually is the result of the catabolic processes involved in uterine involution
o Lost muscle tone in bladder
o Traumatized meatus
o Diminished sensitivity to fluid pressure
o Diuresis
o Overdistended bladder
▪ Urinary retention
▪ Hemorrhage (uterine atony( absence or lack of usual muscle tone))
o Uterus is displace upward and laterally by the full bladder. The displacement results in decreased contraction of
the uterine muscles, a primary cause of excessive bleeding
Musculoskeletal System Changes: Muscles and Joints
▪ Muscle fatigue
▪ Relaxin levels subside
▪ Hip or joint pain
▪ Body mechanics and posture
Musculoskeletal System Changes: Abdominal Wall
▪ Tone and strength
▪ Exercises
▪ Diastasis recti (separation usually 2 to 4 cm)
o Longitudinal muscles of the abdomen separate.
▪ Usually returns to normal position by 6 weeks after birth
Integumentary System Changes
▪ Skin changes gradually disappear. (estrogen, progesterone, and melanocyte-stimulating hormone decline after birth)
o Melasma, the “mask of pregnancy”
o Linea nigra
o Spider nevi
o Palmar erythema
▪ Striae gravidarum (stretch marks)
o Fade to silvery lines but do not disappear
▪ Hair loss:38
o Begins at 4 to 20 wks after delivery and is regrown in 4-6 months for 2/3s of women and by 15 months for the
remainder of women
Neurologic System Changes
▪ Anesthesia and/or analgesia may produce temporary changes.
o Anesthesia:
▪ May produce temporary neurologic changes
● Can be lack of feeling in legs, dizziness
▪ Prevention of injury, especially falling, is a priority.
▪ Carefully assess headaches.
▪ Frontal and bilateral headaches are common in the first week postpartum and may be a result of changes in fluid and
electrolyte balance
o Headaches:
▪ Severe
▪ Could be d/t post-puncture H/A
▪ May be most severe when the woman is in an upright position/ relieved by assuming a supine position
▪ Corrected w/ blood patch
▪ Unable to sit upright
▪ Should be reported to anesthesiologist
▪ Headache along w/ blurred vision, proteinuria, epigastric/ abdominal pain may indicate development
or worsening of preeclampsia
Endocrine System Changes
▪ Resumption of ovulation and menstruation
o Menses 6 to 8 weeks
o Breastfeeding delays return
▪ May resume as early as 12 wks or as late as 18 months during lactation
o Menses may resume as early as 12 wks or as late as 18 months during lactation
▪ Lactation
o Estrogen & Progesterone prepare the breasts for lactation
▪ After expulsion of the placenta, estrogen and progesterone levels decline rapidly, and prolactin initiated
milk production within 2-3 days after childbirth
o Prolactin---returns to nonpregnant levels in 14 days if mother is not breastfeeding
o Oxytocin---necessary for milk ejection or “let-down”.
▪ Causes milk to be expressed from the alveoli into the lactiferous ducts during suckling
▪ Weight Loss
o Approximately 4.5 to 5.8kg are lost during childbirth
▪ Includes:
● Weight of the fetus, placenta, and amniotic fluid and blood lost during the birth
▪ Additional 2.3 - 3.6kg are lost as a result of diuresis and 0.9 – 1.4kg from involution and lochia by the
end of the first week
o Loss of blood and diuresis
o Adipose tissue gained during pregnancy lost slowly
o Provide information about diet and exercise
o Conserve energy and promote health of mother
Postpartum Assessment: Initial Assessments (begin during the 4th stage of labor---first 1-2 hrs after childbirth)
▪ Vital signs
▪ Skin color
▪ Location and firmness of the fundus
▪ Amount and color of lochia
▪ Perineum
o Edema
o Episiotomy
o Lacerations
o Hematoma
▪ Presence, degree, and location of pain
▪ Intravenous (IV) infusions
o Type of fluid39
o Rate of administration
o Type and amount of added medications
o Patency of the IV line
o Redness, pain, or edema of the site
▪ Urinary output
o Time and amount
o Presence of a catheter
o Color and character of urine
▪ Status of abdominal incision and dressing
▪ Level of feeling and ability to move if regional anesthesia was administered
Postpartum Assessment: Chart Review
▪ Gravida, para
▪ Time and type of delivery
▪ Presence and degree of episiotomy or lacerations
▪ Anesthesia or medications administered
▪ Significant medical and surgical history
▪ Medications
▪ Food and drug allergies
▪ Chosen method of infant feeding
▪ Condition of the baby
▪ Laboratory data
Need for Rho(D) immune globulin (RhoGAM)
▪ May be necessary if the mother is Rh-negative, the newborn is Rh-positive, and the mother is not already sensitized
▪ Rho (D) immune globulin should be administered within 72 hours after childbirth to prevent the development of
maternal antibodies that would affect subsequent pregnancies
Need for rubella vaccine
▪ If pregnant women is not immune, rubella vaccine is recommended after childbirth to prevent her from acquiring rubella
during subsequent pregnancies, when it can cause serious fetal anomalies
▪ Not recommended during pregnancy d/t it being a live vaccine
▪ Women are advised not to become pregnant for at least 28 days after receiving the vaccine
Need for pertussis vaccine
▪ may be offered to women during pregnancy or before hospital discharge after childbirth
Need for varicella vaccine
▪ varicella in pregnant women can cause infection and serious complications in the fetus and newborn
▪ recommended that women who are not immune to varicella should receive the first dose of varicella vaccine after delivery
and before discharge from the birth facility
▪ should be advised not to become pregnant for 1 month after receiving the vaccine
Risk factors for hemorrhage and infection
▪ two most common complications of puerperium (period from end of childbirth until involution of the reproductive organs
is complete; approx. 6 wks)
o hemorrhage
o infection
Postpartum Assessment: Focused Assessments after Vaginal Birth
▪ Every 15 minutes for the first hour
▪ Every 30 minutes for the second hour
▪ Every 4 hours for the first 24 hours
▪ Every 8 to 12 hours thereafter
Postpartum Assessment: Vital Signs
▪ Blood pressure---- if 140/90 or higher, preeclampsia may be present---decrease may indicate dehydration or hypovolemia
resulting from excessive bleeding
▪ Pulse
o If tachycardia is noted, additional assessments should include degree of pain, BP, location and firmness of the
uterus, amount of lochia, estimated blood loss at delivery, and hemoglobin and hematocrit values
▪ Respiration
▪ Temperature40
▪ Pain
Postpartum Assessment: Fundus
▪ Firm and near level of umbilicus
▪ Recheck after voiding.
▪ Clots interfere with uterine contraction.
▪ Support uterus when expelling clots to prevent inversion
o Nondominant hand must support and anchor the lower uterine segment during palpation and massage
▪ Drugs may be necessary to maintain contraction.
o Oxytocin can be used to maintain contraction of the uterus and thus prevent postpartum hemorrhage
Postpartum Assessment: Lochia
▪ Amount
o Constant trickle, dribble, or oozing of lochia indicates excessive bleeding and requires immediate attention
o Excessive lochia in the presence of a contracted uterus suggests lacerations of the birth canal
▪ Color
▪ Odor
o Usually described as fleshy, earthy, or musty
o Foul odor suggests endometrial infection, and assessments should be made for additional signs of infection
▪ Signs include:
● Maternal fever, tachycardia, uterine tenderness and pain
Postpartum Assessment: Perineum
▪ REEDA
o (R) Redness
o (E) Edema
o (E) Ecchymosis (bruising)
o (D) Discharge
o (A) Approximation (edges of the wound should be close, as though stuck or glued together)
Postpartum Assessment: Bladder Elimination
▪ Assess for
o Distention
o Displacement of uterus
o Fundus after emptying bladder
Postpartum Assessment: Breasts
▪ Should be soft and nontender days 1 and 2
▪ Examine whether or not mother is breastfeeding.
▪ Observe size, symmetry, and shape.
▪ Assess for flat or retracted nipples.
▪ Assess for signs of nipple trauma if breastfeeding.
▪ Palpate for firmness or tenderness.
Postpartum Assessment: Lower Extremities
▪ Examine for signs or symptoms of thrombophlebitis(occurs when the vessel wall develops an
inflammatory response to the thrombus… this further occludes the vessel)
o Palpate pedal pulses.
o Assess Homan sign.
▪ Discomfort in the calf w/ passive dorsiflexion of the foot is a positive
Homan’s sign and may indicate DVT
o Assess for edema.
▪ Diuresis is highest b/w the 2nd and 5th days after birth
▪ Fluid and electrolyte balance should return to nonpregnant status by 21
days
o Assess deep tendon reflexes.
▪ Should be 1+ to 2+
▪ Report brisker-than-average and hyperactive reflexes (3+to 4+), which suggests preeclampsia
Care in Immediate Postpartum Period: Providing Comfort Measures
▪ Ice packs
o Causes vasoconstriction and is most effective if applied soon after the birth to prevent edema and to numb the
area41
o Removed for 10 minutes before a fresh pack is applied
o Condensation from ice may dilute lochia and make it appear heavier than it actually is
▪ Sitz baths
o Cool water reduces pain caused by edema and may be most effective within the first 24 hours
o Warm water increases circulation, promotes healing, and may be most effective after 24 hours
▪ Perineal care
o Consists of squirting warm water over the perineum after each voiding or bowel movement
▪ Topical medications
o Hold nozzle of the spray 6-12 inches from her body and direct it toward the perineum
o Used after perineal care and before clean pads are applied
▪ Sitting measures
o Should be advised to squeeze her buttocks together before sitting and to lower her weight slowly onto her
buttocks ---this prevents stretching of the perineal tissue and avoids sharp impact to the traumatized area
▪ Analgesics
o Woman should receive no more than 4g of acetaminophen in a 24 hr period
o Ibuprofen (NSAIDs) are often prescribed b/c of their anti-inflammatory effects
Care in Immediate Postpartum Period: Promoting Bladder Elimination
▪ Medicate the woman for pain to help her relax.
▪ Run water in the sink or shower, place the
mother’s hands in warm water, and pour water over the vulva.
▪ Encourage urination in the shower or sitz bath.
▪ Provide hot tea or fluids of choice.
▪ Ask the mother to blow bubbles through a straw.
▪ Help the woman into the shower or sitz bath and instruct her to void there.
▪ Catheterized if:
o She is unable to void.
o The amount voided is less than 150 mL, and the bladder can be palpated.
o The fundus is elevated or displaced from the midline.
Care in Immediate Postpartum Period: Providing Fluid and Food
▪ Encourage to drink 2500 mL per day
▪ Offer fluids culturally appropriate
▪ IV fluids may be necessary if unable to tolerate by mouth (PO)
▪ Culturally appropriate meals and snacks should be available at all times.
Care in Immediate Postpartum Period: Preventing Thrombophlebitis
▪ Early ambulation
▪ Frequent trips to the bathroom
Nursing Care Following Cesarean Birth: Assessment
▪ Pain relief
o Side effects of some narcotics PCA use:
▪ Respiratory depression, itching (pruritus), N/V, and urinary retention
▪ Respirations
o Capnography (end-tidal carbon dioxide monitoring) may also be used to detect opioid-related respiratory changes
▪ Abdomen
o Paralytic ileus (lack of movement in the intestines)----signs: abdominal distention, absent or decreased bowel
sounds, and failure to pass flatus or stool
▪ Intake and output
Nursing Care Following Cesarean Birth: Interventions: The First 24 Hours
▪ Pain relief
o Offer pain medication if not on patient-controlled analgesia (PCA)
o Assess respiratory status if had epidural
▪ Overcoming effects of immobility
o New mother is on bed rest for the first 8-12 hours
o To prevent pooling of secretions in the airways, she must be assisted to turn, cough, and expand the lungs by
breathing deeply at least every 2 hours while she is awake
o Incentive spirometers help expand the lungs to prevent hypostatic pneumonia that can result from immobility
and shallow, slow respirations42
▪ Provide comfort.
Nursing Care Following Cesarean Birth: Interventions: After 24 Hours
▪ Resume normal activities.
▪ Assist mother with infant feeding.
▪ Prevent abdominal distention.
o Early, frequent ambulation
o Tightening and relaxing the abdominal muscles
o Avoidance of carbonated beverages and the use of straws, which increase the accumulation of intestinal gas
o Pelvic lifts
o Rectal suppositories, as ordered, to help stimulate peristalsis and passage of flatus
▪ Teaching for discharge
Application of the Nursing Process: Knowledge of Self-Care
▪ Assessment
o Provide health education before discharge.
o Determine learning needs and major concerns of family.
o Be aware of common barriers to learning.
▪ Analysis
o Most nursing care is wellness-oriented.
o Identify need for education related to self-care.
o Common nursing diagnosis
▪ Planning
o Verbalize or demonstrate understanding of self-care instructions.
o Verbalize understanding of practices that promote maternal health by discharge.
o Describe plans for follow-up care.
▪ Interventions
o Teach the process of involution.
o Teach self-care.
▪ Breast care for lactating mothers:
● Avoid soap on her nipples b/c it will remove the natural lubrication secreted by Montgomery’s
glands
● Keeping nipples dry b/w feedings will help prevent tissue damage, and wearing a good bra
provides necessary support as breast size increases
▪ Measures to suppress lactation:
● Instruct the woman to wear a sports bra or other well-fitting bra 24 hrs a day until the breasts
become soft
● Manage breast discomfort by application of ice, which reduces vasocongestion, and
administration of analgesics
● Advise the woman to refrain from allowing warm water to fall directly on the breasts during
showers and pumping or massaging the breasts, as these actions will stimulate milk production
● Tenderness and engorgement should return to normal in 48-72 hours
o Kegel exercises
▪ These movements strengthen the muscles that surround the vagina and urinary meatus
▪ This exercise helps prevent the loss of muscle tone that can occur after childbirth and may decrease
urinary incontinence
▪ Involves contracting muscles around the vagina, holding tightly for 10 seconds, and then relaxing for 10
seconds---women should work up to 30 contraction-relaxation cycles or more each day
o Promote rest and sleep.
o Provide nourishment and nutrition counseling.
o Promote regular bowel elimination.
o Promote good body mechanics.
o Counsel about sexual activity.
o Instruct about follow-up appointment.
▪ Often 4-6 wks after vaginal birth and 2 wks after cesarean birth
o Teach about signs and symptoms that should be reported:
▪ Fever
▪ Localized area of redness, swelling, or pain in either breast43
▪ Persistent abdominal tenderness
▪ Feelings of pelvic fullness or pelvic pressure
▪ Persistent perineal pain
▪ Frequency, urgency, or burning on urination
▪ Abnormal change in character of lochia
▪ Localized tenderness, redness, edema, or warmth of the legs
▪ Redness, separation or edema of, or foul drainage from an abdominal incision
o Ensure thorough education.
▪ Evaluation
Postpartum Discharge and Community-Based Care
▪ Criteria for discharge
o The mother has no complications, and assessments (including vital signs, pain level, lochia, fundus, urinary
output, incisions, ambulation, ability to eat and drink, and emotional status) are normal.
o Pertinent laboratory data including blood type and hemoglobin or hematocrit have been reviewed, and Rho(D)
immune globulin has been administered, if necessary.
o The mother has received instructions on self-care, deviations from normal, and proper response to danger signs
and symptoms.
o The mother demonstrates knowledge, ability, and confidence to care for herself and her baby.
o The mother has received instructions on postpartum activity, exercises, and relief measures for common
postpartum discomforts.
o Arrangements have been made for postpartum follow-up care.
o Family members or other support persons are available to the mother for the first few days after discharge.
▪ Community-based care
o Information lines
o Telephone follow-up
o Home visits
o Outpatient clinics
Chapter 18: Postpartum Psychosocial Adaptations
Process of Becoming Acquainted: Bonding
▪ Initial attraction for the neonate by the parents
▪ Enhanced when parent and infant touch and interact
▪ Delay procedures that interfere with this time
Process of Becoming Acquainted: Attachment
▪ A bond develops through satisfying interaction.
▪ The process begins in pregnancy.
▪ Both the parent and child benefit.
▪ Important concepts
▪ Reciprocal attachment behaviors repertoire of infant actions that promotes attachment b/w the parent and newborn
Process of Becoming Acquainted: Maternal Touch
▪ Maternal behavior changes rapidly as the mother discovers the infant.
▪ Initially holds baby in a face-to-face position
▪ Mother gently explores the infant with her fingertips.
▪ May stroke with palm of her hand
▪ Gradually enfolds infant
▪ Claiming or binding in as she identifies specific features
Process of Becoming Acquainted: Verbal Behaviors
▪ Speak in high-pitched voice
▪ Provide clues to early psychologic relationship to infant
▪ Nurses must observe interactions to foster early attachment.
Process of Maternal Adaptation: Puerperal Phases
▪ Taking-in phase
o Focused on own need for fluid, food, and sleep
o Allows others to make decisions
o Mother is integrating her birth experience into reality.
o May be prolonged if complications occur
▪ Taking-hold phase44
o Mother becomes more independent.
o Assumes responsibility for own self-care
o Begins to shift attention to infant
o Welcomes information about newborn behavior
o May verbalize anxiety about her competence as a mother
o Ideal time to provide instructions and demonstrations
o Teachable, reachable, referable moment
▪ Letting-go phase
o Couple relinquishes role as a childless couple
o Gives up idealized expectations of birth experience
o Relinquishes infant of their fantasy, accepts real infant
o Allow to verbalize feelings of grief
Process of Maternal Adaptation: Maternal Role Attainment
▪ Mother achieves confidence in her ability and identity as a mother.
▪ Stages of transition
o The anticipatory stage begins during pregnancy.
o The formal stage begins with the birth of th444444444444e infant and lasts for 4 to 6 weeks.
o The informal stage begins when parents learn to respond to the infant's cues.
o The personal stage is attained when a parent feels comfortable in parental role.
Process of Maternal Adaptation: Heading Toward a New Normal
▪ Appreciating the body
▪ Settling in
▪ Becoming a new family
Process of Maternal Adaptation: Redefining Roles
▪ Focuses on maintaining a strong relationship with partner
▪ New parents must share tasks and responsibilities.
▪ Lack of flexibility can lead to tension and frustration.
▪ Assists family to express concerns and feelings
Process of Maternal Adaptation: Role Conflict
▪ When perception of role differs from reality
▪ Parental role may conflict with need for employment.
▪ Help mother acknowledge feelings and recognize them as normal
▪ Develop a schedule that allows maximum time with infant
▪ Negotiate with other family members to take over household tasks
Process of Maternal Adaptation: Major Maternal Concerns
▪ Body image
▪ Concerns about regaining normal figure
▪ May have unrealistic expectations
▪ Needs adequate calories to supply energy and produce milk
▪ Participates in activities to regain muscle tone
▪ Smoking---women who breastfeed their infants are less likely to resume smoking by 26 wks postpartum
Process of Maternal Adaptation: Postpartum Blues
▪ Mild depression is a frequently expressed concern
o Condition has an early onset---begins in the first week, peaks around day 5, and ends within 2 wks
o Usually lasts no longer than 2 weeks (if it lasts longer than 2 wks, may be a more serious condition)
▪ Characterized by fatigue, insomnia, irritability, tearfulness, weeping, mood instability, and anxiety
▪ Does not usually affect ability of mother to care for infant (baby blues)
▪ Direct cause unknown
▪ Self-limiting
The Process of Family Adaptation: Father
▪ Develop bond to newborn (engrossment)
▪ Intense interest in infant
▪ Desire to touch and hold baby
▪ Experience strong attraction to infant
▪ Looks forward to parenting but lacks confidence
▪ Wants to be included in learning about infant care45
▪ Needs information about child care
The Process of Family Adaptation: Siblings
▪ Response to new baby depends on age and developmental level
o Toddlers are not usually aware of impending birth
o May view infant as competition
o Negative behaviors may surface and indicate stress.
o Jealousy and frustration may manifest as hostile behaviors toward mother.
▪ Preschoolers engage in more looking than touching.
▪ Parents need to affirm their continued love and affection.
▪ Parents and visitors must pay attention to the sibling.
The Process of Family Adaptation: Grandparents
▪ Grandparents living nearby develop a strong attachment.
▪ May live many miles away, and it is difficult to form a close attachment
▪ Expectations of the role of grandparents differ.
▪ Often are a major part of the support system of the new parents
Factors Affecting Family Adaptation
▪ Discomfort and fatigue
o May make it difficult to focus on needs of newborn
o Remain a problem since infant's schedule is erratic
▪ Knowledge of infant needs
o May become anxious if unable to console crying infant
o Have many concerns about specific procedures
o Want to know if infant is adequately nourished
o Concerns about spoiling the infant
▪ Previous experience with newborns affects family adjustment.
▪ Expectations for the newborn
o Unprepared for normal characteristics of newborn's appearance
o Nurses need to teach normal growth and development.
o Parent may be disappointed with the sex of the child.
▪ Maternal age
o Parenthood is a challenge for teenager
o Teenagers need special assistance to develop necessary parenting skills.
▪ Maternal temperament
o Personality traits are a major influence on attachment
▪ Temperament of the infant
o An infant who is calm and easily consoled increases parental confidence.
o Irritable infants who do not respond to cuddling increase parental frustration.
▪ Availability of a strong support system is a major factor in maternal adjustment.
▪ Unanticipated events
o Cesarean birth can make parental adjustment more difficult.
o Preterm or ill infant
o Birth of multiple infants
Cultural Influences on Adaptation
▪ Provide care that is culture specific.
▪ Communication
▪ Health beliefs
▪ Dietary practices
Home and Community-Based Care
▪ Assessments and interventions occur in the home.
▪ May leave facility while still in taking-in phase
▪ Communication between nurses in home and hospital
Application of the Nursing Process: Maternal Adaptation
▪ Assessment
o Several factors affect adaptation to the birth
o Table 18-1
▪ Analysis46
o Determine the parents’ ability to create or continue a nurturing environment.
o Risk for altered parenting can be related to many factors (see Box 18-1).
▪ Planning (expected outcomes)
o Verbalize feeling of comfort and support.
o Demonstrate progressive attachment behaviors.
o Participate in care of the newborn.
▪ Interventions
o Assist mother
o Monitor and protect
o Listen
o Foster independence
o Promote bonding
▪ Mother-baby care
▪ Couplet care
▪ Dyad care
o All of these mean the infants remain in the room with the parent
o Involve parents in care
▪ Evaluation
Application of the Nursing Process: Family Adaptation
▪ Assessment : fathers
o Assess father's emotional status and interaction with infant.
o Assess father's role as the primary support person.
o Help the father develop realistic expectations of newborn behavior.
o Provide information about the mother's needs during the recovery period.
o Observe reactions of siblings to the newborn.
o Observe involvement of other family members.
o Assess nonverbal behavior.
▪ Analysis
o Table 18-2
▪ Planning
o Family will verbalize understanding of infant
needs and behaviors.
o Family will identify methods for reducing stress.
o Family will describe measures to reduce sibling rivalry.
o Family will identify external resources and
support systems.
▪ Intervention
o Teach about newborns
o Help family adapt
o Help father co-parent
o Help reduce sibling rivalry
o Identify support
▪ Evaluation
Chapter 22: Infant Feeding
Nutritional Needs of the Newborn
▪ Calories
o Breastfed: 39 to 45 kcal/lb (85 to 100 kcal/kg) daily
o Formula fed: 45 to 50 kcal/lb (100 to 110 kcal/kg) daily
o May lose less than 10% of birth weight
▪ Loss is a result of normal excretion of extracellular water and meconium and newborns consuming
fewer calories than needed
▪ Nutrients
o Carbohydrates (complex)
▪ And fats… are less well digested because of the lack of pancreatic amylase and lipase in the newborn
o Proteins47
o Fats
o Vitamins/minerals
▪ Water
o Needs approx., 27-45 milliliters per pound during the first 3-5 days of life
▪ Any extra than this can cause brain damage
Breast Milk: Composition
▪ Lactogenesis I
o Begins during pregnancy and continues during the early days after giving birth
o Colostrum—thick, yellow substance
▪ Higher in protein and come vitamins and minerals compared w/ mature milk
▪ Lower in carbohydrates, fat, lactose, and some vitamins
▪ Rich in immunoglobulins, especially IgA, which helps protect the infant’s GI tract from infection
▪ Helps establish the normal flora in the intestines
● Bifidus factor, leukocytes, lysozymes, lactoferrin, and immunoglobulins
▪ Lactogenesis II
o Beings 2-3 days after birth
o Transitional milk--- milk that gradually changes from colostrum to mature milk, appears over about 10 days
o Immunoglobulins and proteins decrease and lactose, fat, and calories increase
▪ Lactogenesis III
o Mature milk replaces transitional milk
o Usually bluish and thin
o Continues to provide immunoglobulin’s and antibacterial components
o Mature milk contains approximately 20kcal/oz and nutrient sufficient to meet the infant’s needs
o Breast milk contains: maternal immunoglobulin’s, leukocytes, antioxidants, enzymes, and hormones important
for growth are present in breast milk
Breast Milk: Nutrients
▪ Protein
o Breast milk is high in taurine, which is important for bile conjugation and brain development
o Tyrosine and phenylalanine levels are low in breast milk to correspond to the infant’s low levels of enzymes to
digest them
o Casein and whey--- are the proteins in milk
▪ Carbohydrates
o Lactose is the major carbohydrate in breast milk--- it improves absorption of calcium and provides energy for brain
growth
▪ Fat
o Provides 50% of the calories in breast milk
o Hindmilk---the milk produced at the end of the feeding, produces satiety and helps the infant gain weight
o Triglycerides form the majority of fat content
▪ Vitamins
o A,E, and C are high in breast milk
o Vit. D content of breast milk is low and daily supplementation w/ 400 IU is recommended w/in the first few days
▪ Minerals
▪ Enzymes
o Breast milk contains enzymes that aid in digestion
o Amylase--- necessary for digestion (present in breast milk)
o Breast milk also includes lipase to increase fat digestion
Breast Milk: Infection-Preventing Components
▪ Bifidus factor promotes the growth of Lactobacillus bifidus—an important part of intestinal flora that helps produce an acid
environment in the GI tract
▪ Protects against common intestinal pathogens
▪ Leukocytes --- also help protect against infection
▪ Lysozyme is a bacteriolytic enzyme that acts against gram-positive and enteric bacteria
▪ Lactoferrin is a protein that beings iron in iron-dependent bacteria, preventing their growth
▪ Immunoglobulins high in colostrum—but present throughout the lactation
Breast Milk: Effect of Maternal Diet48
▪ Fatty acid content influenced by maternal diet
▪ Protein, carbohydrates, and mineral content same in malnourished mother
▪ Vitamin levels are affected by maternal intake and stores.
▪ Balanced diet important for breastfeeding woman
Formulas
▪ Modify cow’s milk to compare with breast milk
o Reduce protein content
o Remove saturated fat--- and replaced with vegetable fat
o Other nutrients
▪ Formulas for infants with special needs
o Soy/protein hydrolysate
o Casein hydrolysate
▪ Preterm infant’s formula
o Higher calorie--- 22-24 calories rahter than the 20 calories
Considerations in Choosing a Feeding Method
▪ Nursing role
▪ Breastfeeding (look at box 22-2. Pg 439)
o Advantages
o Reasons for not breastfeeding
▪ Formula
o Reasons for formula feeding
▪ Combination feeding
Factors Influencing Choice
▪ Support from others
▪ Cultural influences
▪ Employment
▪ Other factors
Normal Breastfeeding
▪ Breast changes during pregnancy
▪ Milk production
o Supply and demand
o How often is baby latching
▪ Hormonal changes at birth
o Prolactin---- loss of placental hormones results in increasing levels and effectiveness of prolactin and activates
milk production
▪ The tactile stimulation of suckling and the removal of colostrum or milk cause continued increased
levels or prolactin
o Oxytocin--- increases in response to nipple stimulation and causes the milk-ejection reflex or let-down reflex,
the release of milk from the alveoli into the ducts
▪ Continued milk production
▪ Preparation of breasts
Application of the Nursing Process: Breastfeeding
▪ Assessment
o Maternal assessment
▪ Breasts and nipples
▪ Knowledge
o Infant feeding behaviors
▪ Assess the infant’s readiness for feeding
▪ Nursing diagnosis
▪ Expected outcomes
Application of the Nursing Process: Breastfeeding (Cont.)
▪ Interventions
o Assist with first feeding
o Teaching
o Position of mother’s hands
o Latching-on49
o Suckling pattern
o Removal from breast
o Frequency and length of feeding
▪ Usually breastfed every 1.5 to 3 hours w/ 8-12 feedings in 24 hours
▪ At first… feedings can last 10-15 minutes on each side
▪ Feeding time increases as needed by the infant over the next few days
▪ Foremilk the watery first milk that quenches the infant’s thirst
▪ Hindmilk comes at the end of the feeding
o Preventing problems
▪ Avoid use of formula supplements of any kind during the first 72 hours
▪ Evaluation
Common Breastfeeding Concerns: Infant Problems
▪ Sleepy
▪ Nipple confusion
▪ Suckling problems
o When infants suck from a bottle, they must push the tongue against the nipple to slow the flow of milk
o When they suckle at the breast, they position the nipple far into the mouth so that the gums compress the areola
▪ Infant complications
o Jaundice
▪ Insensible water loss from the skin is increased as a result of the heat and lights used in treatment and
could lead to dehydration
▪ Infants receiving phototherapy (temp should be 97.6/97.7 or higher) should not be given water, which
may decrease the intake of breast milk
▪ Decreased intestinal motility from insufficient milk intake allows reabsorption of bilirubin through the
intestinal wall into the bloodstream, increasing the work of the immature liver
▪ Physiologic jaundice becomes visible when the serum bilirubin reaches 5 to 7 mg/dL, which occurs when
the baby is approximately 3 days old. This finding is within normal limits for the newborn. Pathologic
jaundice occurs during the first 24 hours of life. Pathologic jaundice is caused by blood incompatibilities,
causing excessive destruction of erythrocytes, and must be investigated. Breast milk jaundice occurs in
one third of breastfed infants at 2 weeks and is caused by an insufficient intake of fluids.
o Prematurity
o Illness and congenital defects
Common Breastfeeding Concerns: Maternal Concerns
▪ Breast problems
o Mastitis (infection of the breast)
o Engorgement
o Nipple pain
o Flat and inverted nipples
o Plugged ducts
▪ Illness in mother
▪ Medications
▪ Breast surgery
▪ Employment
▪ Milk expression
▪ Storing milk
▪ Multiple births
▪ Weaning
▪ Home care
Chapter 19: Normal Newborn: Processes of Adaptation
Initiation of Respirations: Development of the Lungs
▪ Fetal lung fluid ---produced by the alveoli
o Fluid is continuously produced at a rate of 4-5 ml/kg/hr
▪ Surfactant is produced as lungs mature.
o Reduces surface tension within alveoli
o Detectable by 24-25 wks gestation
o Surfactant usually sufficient by 34 to 36 weeks of gestation50
Initiation of Respirations: Causes of Respirations
▪ First breath must force fluid into interstitial spaces
▪ Requires negative pressure
▪ Initiation of respirations
o Chemical factors
▪ Chemoreceptors in the carotid arteries and the aorta respond to changes in blood chemistry caused by
the hypoxia that occurs w/ normal birth
▪ A decrease in the partial pressure of oxygen (PO2) and pH and an increase in the partial pressure of
carbon dioxide (PCO2) in the blood cause impulses from these receptors to stimulate the resp center in
the medulla
o Mechanical factors
▪ Approximately one third of the fetal lung fluid is forced out of the lungs into the upper air passages
during birth. The fluid passes out of the mouth or nose or is suctioned as the head emerges from the
vagina. When the pressure against the chest is released at birth, recoil of the chest draws a small
amount of air into the lungs and helps remove some of the viscous fluid in the airways.
▪ As the infant cries, pressure within the lungs increases, causing remaining fetal lung fluid to move into
the interstitial spaces, where it is absorbed by the pulmonary circulatory and lymphatic system
o Thermal factors
▪ Sensors in the skin respond to this sudden changes in temp by sending impulses to the medulla that
stimulate the resp center and breathing
o Sensory factors
o Continuation of respirations
Initiation of Respirations
Cardiovascular Adaptation: Ductus Venosus
▪ Oxygenated blood from the placenta enters the fetal circulation through the umbilical vein
▪ Directs blood away from liver into the ductus venosus (DV) which connects to the inferior vena cava during fetal life
▪ Rest of the umbilical vein flow goes through the liver before entering the IVC
▪ As blood flows into the RA, a flap of tissue directs the blood from the more highly oxygenated stream across the atrium to
the foramen ovale
▪ Blood flow diminishes when umbilical cord vessels are occluded at birth.
▪ Fibrosis of ductus venosus occurs by 1 to 2 weeks of life.
Cardiovascular Adaptation: Foramen Ovale (pg.370)***
▪ A flap valve in the septum between the right and left atria of the fetal heart
▪ As blood flows into the RA, 50-60% crosses the foramen ovale to the LA
▪ In LA.. it mixes w/ the small amount of blood entering from the pulmonary veins, flows to the left ventricle, and leaves
through the aorta
▪ Majority of blood in the ascending aorta flows to the coronary, left carotid, and subclavian arteries
▪ Resistance to pulmonary blood flow
▪ Blood from left ventricle travels to placental vessels.
▪ Pressures reverse as blood flows into dilated pulmonary vessels.
▪ Pressure in left ventricle builds, causing foramen ovale to close.
▪ Closure of foramen ovale prevents blood flow from right to left.
▪ Blood flow through heart and lungs changes to neonatal circulation.
▪ Becomes permanently closed within several months---- closes when the pressure in the left atrium is higher than that in
the right atrium
Cardiovascular Adaptation: Pulmonary Blood Vessels
▪ Blood from the superior vena cava and inferior vena cava flow into the right atrium, to the right ventricle, and into the
pulmonary artery.
▪ Most of the blood passes through the ductus arteriosus, while 10% to 12% of the blood goes to the lungs.
▪ After 30 weeks gestation, the amount of blood to the lungs increases.
▪ Blood flow to the lungs is limited because the pulmonary artery and other blood vessels are constricted, causing high
pulmonary vascular resistance
▪ Blood perfusing the lungs returns to the left atrium by the pulmonary veins.
Cardiovascular Adaptation: Ductus Arteriosus
▪ Connects the pulmonary artery and the descending aorta during fetal life
▪ Dilation is maintained by prostaglandins from the placenta and low oxygen content of the blood51
▪ May cause a murmur for the newborn—eventually goes away
▪ Closes gradually as oxygenation improves and prostaglandins, which helped keep it open, are metabolized
Cardiovascular Adaptation: Changes at Birth
▪ Alterations occur simultaneously within the first few minutes after birth.
▪ Pressures between the right and left sides of the heart are reversed.
▪ At birth shunts close, and the pulmonary vessels dilate.
▪ The foramen ovale’s flap valve closes.
▪ As the newborn takes the first breaths at birth, the rise in oxygen concentration causes the ductus arteriosus to constrict,
preventing entry of blood from the pulmonary artery
▪ Clamping of the umbilical cord closes the ductus venosus and further decreases pressure in the right side of the heart
▪ Asphyxia (insufficient oxygen and excess carbon dioxide in the blood and tissue) and persistent pulmonary HTN may
reverse the pressures in the heart and cause the foramen ovale to reopen
Neurologic Adaptation: Thermoregulation (maintenance of body temp)
▪ Newborn characteristics leading to heat loss
o Healthy full-term infant remains in a position of flexion, reducing the amount of skin surface exposed to the
surrounding temps and decreasing heat loss
▪ Methods of heat loss
o Evaporation
▪ Air drying of the skin that results in cooling
▪ Drying the infant, especially the head, as quickly as possible helps prevent loss of heat by evaporation
▪ Insensible water loss from the skin and respiratory tract increases heat loss from evaporation
o Conduction
▪ Movement of heat away from the body occurs when newborns have direct contact w/ objects that are
cooler than their skin
▪ Placing infants on cold surfaces and touching them w/ cool objects increases body heat by conduction
▪ Warming objects that will tough the infant or placing the unclothed infant against the mother’s skin (“skin
to skin”) helps prevent conductive heat loss
o Convection
▪ Transfer of heat from the infant to cooler surrounding air occurs in convection
▪ Incubators—circulating warm air helps keep them warm by convection
▪ Providing a warm, draft-free environment avoids convective heat loss
o Radiation
▪ Transfer of heat to cooler objects that are not in direct contact w/ the infant
▪ Infants in incubators transfer heat to the walls of the incubator
▪ If the walls of the incubator are cold, the infant is cooled, even when the temp of air inside the incubator
is warm
▪ Placing cribs and incubators away from windows and outside walls minimize radiant heat loss
Sites of Brown Fat
▪ Located primarily around the back of the neck; in the axillae; around the heart, kidneys, and adrenals; between the
scapulae; and along the abdominal aorta
▪ Brown fat--- generates more heat than white subcutaneous fat
Neurologic Adaptation: Thermoregulation (Cont.)
▪ Nonshivering thermogenesis
o Thermogenesis (heat production)
o Newborns rarely shiver when they are cold---instead they become restless and cry
o Acrocyanosis (bluish discoloration of the hands and feet) may occur if they are cold
o Drop in temp increases the metabolic rate, causing above-normal oxygen and glucose use
o Nonshivering thermogenesis process of heat production, without shivering, by oxidation of brown fat
▪ Begins when thermal receptors in the skin detect a skin temp of 35 C to 36C (95F to 96.8F)
o Brown fat highly vascular specialized fat that provides more heat than other fat when metabolized
▪ contains an abundant supply of blood vessels, which cause the brown color
▪ as brown fat is metabolized, it generates more heat than white subcutaneous fat
▪ blood passing through brown fat is warmed and carries heat to the rest of the body
▪ hypoxia, hypoglycemia, and acidosis may interfere w/ the infant’s ability to use brown fat to generate
heat
▪ Effects of cold stress52
▪ Neutral thermal environment
o Environment in which body temperature is maintained w/ out an increase in metabolic rate or oxygen use
▪ Hyperthermia
Hematologic Adaptation
▪ Factors affecting the blood
o Preterm infants have a greater blood volume per kilogram than term infants
o Blood volume of a term newborn is 80-100 mL.kg, but this varies according to the time of cord clamping,
gestational age of the infant, and the position of the infant when the cord is clamped
▪ Blood values
o Erythrocytes and hemoglobin
▪ Birth—infant has comparatively more erythrocytes and higher hemoglobin levels than the adult
▪ Difference is necessary because the partial pressure of oxygen in fetal blood is much lower than the
normal adult level
▪ Adequate oxygenation of the cells is possible b/c fetal hemoglobin carries 20%-50% more oxygen than
adult hemoglobin
o Hematocrit
▪ Normal newborns: 44% to 70% for the first month
▪ A level above 65% from a central side indicates polycythemia (abnormally high erythrocyte count)
● Polycythemia increases the risk of jaundice and injury to the brain and other organs as a result of
blood stasis
● Resp. distress and hypoglycemia are more common in these infants
o Leukocyte
▪ Count at birth is 9100/mm to 34,000/mm
▪ Average WBC count is 15000 in term infants
▪ WBC count falls to 12,000 by 4 to 5 days after birth
▪ WBC count may decrease in infections
▪ Increased numbers of immature leukocytes are a sign of infection or sepsis in the neonate
▪ # of platelets (thrombocytes) may also decrease as a result of infections
▪ Risk of clotting deficiency
o At birth, platelet count ranges from 84000 to 478,000
o After the first week platelet levels are the same as in the adult--- 150,000 to 400,000
Gastrointestinal System: Stomach
▪ The newborns stomach capacity is about 6mL/kg at birth
▪ Capacity expands within first few days of life.
▪ Peristalsis is rapid.
▪ Gastrocolic reflex is stimulated when the stomach fills, causing increased intestinal peristalsis
▪ Cardiac sphincter is relaxed, leading to regurgitation.
Gastrointestinal System: Intestines
▪ Long in proportion to infant's size: more surface area for absorption
▪ Infants are more prone to rapid water loss with diarrhea.
▪ Bowel sounds are present within the first hour. (as early as 15 minutes after birth)
▪ The digestive tract is sterile until feeding begins.
▪ Normal intestinal flora are established within the first few days of life
Gastrointestinal System: Digestive Enzymes
▪ Cannot digest complex carbohydrates d/t not have pancreatic amylase---deficient for the first 4-6 mos after birth
▪ Amylase is also produced by the salivary glands, but it low amounts until about the 3rd month of life
o Amylase is present in breast milk
▪ Newborn is also deficient in pancreatic lipase, limiting fat absorption significantly
o Lipase present in the mouth and stomach helps w/ some digestion of fat
o Lipase is present in breast milk, which may make it more digestible for the newborn than formula
▪ Ingredients in breast milk more easily digested
o Protein and lactose
Gastrointestinal System: Stools
▪ Meconium is the first stool excreted.
o Greenish black with a thick, sticky, tarlike consistency53
▪ Consists of particles from amniotic fluid such as vernix, skin cells, and hair, along w/ the cells shed from
the intestinal tract, bile and other intestinal secretions
o First stool is usually passed within 12 hours.
o Consists of particles from amniotic fluid
▪ Transitional stool is the second type.
o Combination of meconium and milk stools
o Greenish brown and of a looser consistency than meconium
▪ Breastfed infant
o Stools are seedy and mustard colored.
o Stools are more frequent than with formula.
o Stools have a sweet-sour smell.
▪ Formula-fed infant
o Stools are pale yellow to light brown.
o Stools are firmer in consistency.
o Stools have the characteristic odor of stools.
Hepatic System: Conjugation of Bilirubin
▪ Source and effect of bilirubin
o Hemolysis of erythrocytes (principle source of bilirubin)
o Bilirubin is a toxic substance.
o Liver must convert to a soluble form (conjugated)
o Unconjugated bilirubin causes jaundice and kernicterus (permanent neurologic injury)
▪ Unconjugated bilirubin (indirect bilirubin) is soluble in fat but not in water
o Bilirubin encephalopathyacute manifestation of bilirubin toxicity occurring in the first wks after birth
▪ Glucuronyl transferase converts unconjugated bilirubin.
▪ Excreted into duodenum
▪ Eliminated in the stool
▪ Beta-glucuronidase can convert conjugated back to unconjugated bilirubin.
▪ Factors in increased bilirubin
o Excess production
▪ Approximately 8-10 mg/kg of bilirubin is produced in newborns each day, a rate twice that in adults
▪ Rate of production remains higher for 3-6 wks
▪ Newborns have more RBCs per kilogram than adults
o Red blood cell life
▪ Fetal RBC’s break down more quickly than adult erythrocytes
▪ Last 80-100 days in term infants and 60-80 days in preterm infants
● Compared with RBCs in adults, which have a typical life span of 120 days
o Liver immaturity
o Intestinal factors
o Delayed feeding
o Trauma can result in increased hemolysis of red blood cells.
o Fatty acids are released when brown fat is used.
Hepatic System: Hyperbilirubinemia
▪ Physiologic jaundice---also called nonpathologic or developmental jaundice
o Caused by transient hyperbilirubinemia
o Never present during first 24 hours of life
o Jaundice is visible when bilirubin level is greater than 5 mg/dL
o Rate of rise and fall of bilirubin level is important.
▪ Nonphysiologic/ pathologic jaundice
o May occur in the first 24 hours
o Caused by abnormalities causing excessive destruction of erythrocytes
neonates use glucose rapidly and is at risk for hypoglycemia
Hepatic System: Jaundice Associated with Breastfeeding
▪ Breastfeeding jaundice
o Inadequate intake
o Sleepy infant with poor suck
o Delay in elimination of meconium54
o Lack of adequate suckling
▪ True breast milk jaundice
o Bilirubin levels rise after the first 3 to 5 days.
o Substances in breast milk may interfere with conjugation of bilirubin.
o Closely monitor bilirubin levels.
o Treat with phototherapy; may discontinue breastfeeding.
Hepatic System
▪ Blood coagulation
▪ Iron storage
o Iron is stored in the fetal liver and spleen during the last weeks of pregnancy
o Full-term infants who are breastfeeding usually do not need added iron until 6 months of age
▪ Metabolism of drugs
Urinary System
▪ Kidney development
o By 34-36 wks gestation, the fetal kidneys have as many nephrons as an adult
o Blood flow to the kidneys increases after birth, and resistance in the renal vessels decreases
▪ Kidney function
o GFR does not reach adult levels until 1-2 years of age--- therefore infants have a decreased ability to remove waste
products from the blood
▪ Fluid balance
o To maintain fluid balance, full-term infants need 60 to 100 mL/kg daily during the first 3 to 5 days of life and 150 to
175 mL/kg a day by 7 days of age
o Newborns body is composed of a greater percentage of water, with more located in the extracellular
compartment, and fluid is more easily lost
▪ Water distribution
o 78% of newborns body is composed of water
o Intracellular= 34% of body
o Extracellular= 44% of body
▪ Insensible water loss
▪ Urine dilution and concentration
▪ Acid-base and electrolyte balance
Immune System
▪ Less effective at fighting off infection
▪ Immunoglobulin G (IgG)
o Crosses placenta and provides temporary immunity to bacteria, bacterial toxins, and viruses to which the mother
has developed immunity
o Significant production of IgG is delayed until after 6 months of age
▪ Immunoglobulin M (IgM)
o First immunoglobulin produced when exposed to infection
o Helps protect against gram negative bacteria
o Rapid production of IgM begins a few days after birth as a result of exposure to environmental antigens
o If IgM is found in cord blood, then exposure to infection in utero has occurred
▪ Immunoglobulin A (IgA)
o Receive some from colostrum and breast milk
o Must be produced by the infant
o Does not cross the placenta
o Important in protection of the GI and resp systems, and newborns are particularly susceptible to infections of
those systems
Psychosocial Adaptation
▪ Periods of reactivity
o First period of reactivity
▪ Begins at birth and lasts for 30 minutes
o Period of sleep
o Second period of reactivity
▪ Lasts 4-6 hours
▪ Behavioral states55
o Quiet sleep state
o Active sleep state
o Drowsy state
o Quiet alert state
o Active alert state
o Crying state
Chapter 20: Assessment of the Normal Newborn
Early Focused Assessment
▪ Cardiorespiratory status
▪ Thermoregulation
▪ Presence of anomalies
▪ The nurse determines whether resuscitation or other immediate interventions are necessary.
Early Focused Assessment: History
▪ Review data about pregnancy, labor, and delivery
▪ Review the maternal age, health problems, and complications
▪ Narcotic analgesics late in labor affect respirations.
▪ Preterm infants may have inadequate amounts of surfactant.
Early Focused Assessment: Assessment of Cardiorespiratory Status
▪ Airway
o Respiratory rate
▪ Assessed at least once every 30 minutes until the infant has been stable for 2 hours after birth
▪ Normal RR is 30-60 breaths per minute
▪ Average rate is 40-49 breaths per minute
▪ Periodic breathing---pauses in breathing lasting 5-to seconds without other changes followed by rapid
respirations for 10-15 seconds
▪ Apnea---pause in breathing lasting 20 seconds or more, or accompanied by cyanosis, pallor, bradycardia,
or decreased muscle tone
o Breath sounds
o Signs of respiratory distress
▪ Tachypnea (> 60 breaths per minute)
▪ Retractions soft tissue around the bones of the chest is drawn in w/ the effort of pulling air into the
lungs
▪ Flaring of the nares
▪ Cyanosis
▪ Grunting
▪ Seesaw or paradoxical respirations
▪ asymmetry
o Choanal atresia blockage or narrowing of one or both nasal passages by bone or tissue
▪ Color
o Ruddy color--- a ruddy or reddish skin color (plethora) may indicate polycythemia, an excessive number of RBC’s
o Hematocrit value above 65% confirms polycythemia
o Infants w/ elevated hematocrit levels are at increased risk for jaundice from the normal destruction of excessive
red blood cells that occurs after birth
▪ Heart sounds
o FHR should range b/w 120 and 160 bpm
o May elevate to 180 bpm when infants are crying and drop 100 bpm when they are in deep sleep
o Once stable the heart rate is checked once every 8-12 hours or according to hospital policy
▪ Brachial and femoral pulses
▪ Blood pressure
o Average BP for full-term newborns is 65-95 systolic/ 30-60 diastolic
o Varies according to the infants age, weight, and gestational age
o Hypotension may occur in the sick infant
▪ Capillary refill
Early Focused Assessment: Thermoregulation
▪ Take temperature soon after birth.
▪ Set warmer controls to regulate the amount of heat produced.56
▪ Reassess every 30 minutes until stable for 2 hours after birth
▪ Often checked again at 4 hours and then once every 8-12 hours
▪ Normal range: 97.7F to 99.5F
Early Focused Assessment: Assessment for Anomalies
▪ Head
o Craniosynostosis premature closure of the sutures of the infant’s head
o Molding changes in the shape of the head that allow it to pass through the birth canal
o Fontanels
▪ Anterior—diamond- shaped area where the frontal and parietal bones meet
● Measure 4-6 cm from bone to bone
● Should be soft and flat or only slightly sunken
● Depressed fontanel may be a sign of dehydration
● Bulging may indicate increased intracranial pressure
▪ Posterior---triangular area where the occipital and parietal bones meet
● Much smaller than anterior fontanel, measuring 0.5 to 1 cm
● Feels like a dimple at the juncture of the occipital and parietal bones
o Caput succedaneum area of localized edema that appears over the vertex of the newborns head as a result of
pressure against the mother’s cervix during labor
▪ Pressure interferes w/ blood flow from the area, causing localized edema at birth
▪ Generally disappears within 12-48 hours after birth
▪ Crosses suture line, is soft, and varies in size
o Cephalohematoma bleeding between the periosteum and the skull, is the result of pressure during birth
▪ Occurs on one or both sides of the head, usually over the parietal bones
▪ Swelling may not be present at birth, but may develop within the frist 24-48 hours
▪ Does NOT cross the suture lines---b/c the bleeding is held b/w the bone and its covering, the periosteum
▪ Reabsorbs slowly and may take 2-3 months to compleely resolve
▪ Face
▪ Neck and clavicles
o Webbing may indicate turners syndrome or down syndrome
o Unusually large fat pad b/w the occiput and the shoulders may indicate a chromosomal anomaly
o No masses should be present
▪ Cord
o Should contrain 3 vessels
o 2 arteries are small and may stand up at the cut end
o Single vein is larger than the arteries and resembles a slit because its walls are more easily compressed
▪ Extremities
▪ Hands and feet
o Polydactyly (extra digits)
o Syndactyly (webbing between digits)
▪ Hips
▪ Vertebral column
▪ Measurements
o Weight
▪ Lose up to 10% of their birth weight during the first week of life
▪ Infants normally regain or exceed their birth weight by 14 days of life
▪ Thereafter they gain approximately 30g per day during the early months
o Length
▪ Average length of a full-term newborn is 48 to 53 cm (19 to 21 inches)
o Head
▪ Normal range of head circumference for the term newborn is 32 to 38 cm (13 to 15 inches)
o Chest
▪ Usually 2-3 cm smaller than the head
▪ Normal is 30 to 36 cm (12 to 14 inches)
Early Focused Assessment: Neurologic System
▪ Reflexes
▪ Sensory assessment57
o Ears, eyes (may change color by 6 mo of age), and sense of smell and taste
▪ Other neurologic signs
o Jitteriness (tremors)
o Seizures
o Irritability
▪ Reflexes
▪ Reflexes (Cont.)
Early Focused Assessment: Hepatic System
▪ Blood glucose
o At-risk newborns
▪ Gestational diabetes
o Signs
o Screening
▪ Bilirubin
o At-risk newborns
o Jaundice
▪ Nurse assess at least every 8 to 12 hours
▪ Becomes visible when the bilirubin is > than 5mg/dL
o Phototherapy
Early Focused Assessment: Gastrointestinal System
▪ Mouth
▪ Suck
▪ Initial feeding
▪ Abdomen
▪ Stools
Early Focused Assessment: Genitourinary System
▪ Kidney
▪ Urine
o Average number of wet diapers
o Urate crystals
▪ Genitalia
o Female
o Male
▪ Cryptorchidism failure of one or both testes to descend into the scrotum
▪ Hypospadiasabnormal placement of the urinary meatus on the ventral side of the penis
▪ Epispadias meatus on the dorsal side of the penis
▪ Chordee condition in which fibrotic tissue causes the penis to curve downward
Early Focused Assessment: Integumentary System
▪ Skin
o Color
▪ Harlequin color change clear color division over the body w/ one side deep pink or red and the other
half pale or of normal color
● Cause: vasomotor instability and it is usually transient and benign
o Vernix caseosa
▪ Thick, white substance that resembles cream cheese, provides a protective covering for the fetal skin in
utero
o Lanugo
▪ Fine, soft hair that covers the fetus during intrauterine life
o Milia
▪ White cysts, 1 to 2 mm in size, that disappear w/ out treatment
▪ Occur on the face over the forehead, nose, cheeks and chin
o Erythema toxicum
▪ Red, blotchy areas with white or yellow papules or vesicles in the center
▪ Appears during the first 24-48 hours after birth and can continue for several days to several months
▪ Most common over the face, back, shoulders, and chest
o Birthmarks58
▪ Mongolian spots
● Bluish-gray marks that resemble bruises on the sacrum, buttocks, arms, shoulders, and other
areas
● Usually disappear after the first few years of life—some may continue into adulthood
▪ Nevus simplex
● A flat, pink discoloration from dilated capillaries that occurs on the eyelids, just above the bridge
of the nose, or at the nape of the neck
● Color blanches when the area is pressed and is more prominent during crying
● Lesions disappear by 2 years of age, although those at the nape of the neck may persist
▪ Nevus flammeus
● Permanent, flat, pink to dark reddish purple mark that varies in size and location and does not
blanch w/ pressure
● Lesion may darken and may become nodular as the child gets older
● If it gets large and in a visible area, it can be lightened by laser surgery, which is often begun in
infancy
● Located over the forehead and upper eyelid may be associated w/ Sturge-Weber syndrome, a
serious neurologic condition
▪ Nevus Vasculosus (strawberry hemangioma)
● Consists of enlarged capillaries in the outer layers of skin
● Dark red and raised w/ rough surface, giving a strawberry-like appearance
● Usually located on the head
● May be present at birth or develop by 6 months of age
● After growing larger for 6 months, the hemangioma regresses over several years and disappears
● No Tx is necessary unless it becomes infected or ulcerated
▪ Café-au-lait spots
● Permanent, light brown areas that may occur anywhere on the body
● Six or more spots or spots larger than 0.5cm are associated w/ neurofibromatosis, a genetic
condition of neural tissue
o Marks from delivery
o Other skin assessments
▪ Breasts
▪ Hair and nails
▪ Documentation
Assessment of Gestational Age: Ballard Score
▪ Neuromuscular
o Posture
o Square window
o Arm recoil
o Popliteal angle
o Scarf sign
o Heel to ear
▪ Physical characteristics
o Skin
o Lanugo
▪ Appears 20 wks of gestation and increased in amount until 28 wks when it begins to disapper
▪ Most is shed by 32 to 36 wks
▪ Small amount may remain over the upper back and shoulders, on the ears, or on the sides of the forehead
▪ Infant receives a score based on the amount of lanugo present on the back
o Plantar surface
▪ Being to appear at 28 to 32 wks of gestation and cover the entire foot by term
▪ Creases appear more prominent as the infant’s skin begins to dry
o Breasts
o Eyes and ears
▪ Eyelids fused until 26-28 wks of gestation
▪ About 34 wks, the upper pinnae (ear) which have been flat, begin to curve over
● The incurving continues around the ear until it reaches neat the earlobe at 40 wks of gestation59
o Genitals
▪ Testes orginate in the abdominal cavity and begin to descend at 28 wks or gestation
▪ By 37 wks of gestation, they are located high in the scrotal sac, and generally completely descended by
term
▪ Rugae cover the surface of the scrotum by 40 wks of gestation
Assessment of Gestational Age: Ballard Score
▪ Scoring
▪ Gestational age and infant size
o Small for gestational age
o Large for gestational age
o Appropriate for gestational age
▪ Monitor for complications common to age and size of infant.
Assessment of Behavior
▪ Periods of reactivity
▪ Behavioral changes
o Orientation
o Habituation
o Self-consoling activities
o Parents’ response
Chapter 21: Care of the Normal Newborn
Early Care
▪ Vitamin K (Phytonadione)
o Given to neonates because they cannot synthesize it in the intestines w/ out bacterial flora
▪ Which places them at risk for hemorrhagic disease of the newborn (vit. K-deficiency disease)
o Administer within 1 hour of birth
o Give intramuscularly
o One dose prevents bleeding problems until the infant is able to produce vit. K in sufficient amounts
▪ Eye treatment
o Prophylactic treatment to prevent ophthalmia neonatorum incase mother is infected w/ gonorrhea
o Administer within 1 hour of birth
o Erythromycin ophthalmic ointment
o Tetracycline
o Mild inflammation
o Remove drainage with sterile saline and cotton
o May delay treatment during initial bonding
Application of the Nursing Process: Cardiorespiratory Status
▪ Assessment
o Signs of difficult transition
o Note heartbeat respiration and breath sounds
o Observe for signs of respiratory distress including: tachypnea, retractions, flaring of the nares, pallor or cyanosis,
grunting, seesaw respirations and asymmetry of chest movements
▪ Expected outcome
▪ Interventions
o Positioning (on the back w/ the head in a neutral position or to the side)
o Suctioning (use the bulb syringe, as necessary, to suction secretions as they drain into the infant’s mouth or nose
▪ Suction the mouth first, cuz infant may gasp when the nose is suctioned, causing aspiration of mucus or
fluid in the mouth
▪ Then suction the nose gently and ONLY if necessary
▪ Mechanical suctioning---Suction than no more than 5 seconds at a time, using minimal negative pressure
to avoid trauma, laryngospasm, and bradycardia
o Continued care
▪ Evaluation
▪ Bulb Suctioning
Application of the Nursing Process: Thermoregulation
▪ Assessment
o Temperature shortly after birth60
o Assess every 30 min. until stable for 2 hours
▪ Checked again at 4 hours and then every 8-12 hours or according to agency policy
o More frequent if abnormal temperature
▪ Expected outcome
o Temp: 97.7 F to 99.5 F (36.5 C to 37.5 C)
o Pulse: 120-160 bpm (100 sleeping, 180 crying)
o Respirations: 30-60 breaths/ min
▪ Interventions
o Prevent heat loss
o Provide immediate care
o Provide ongoing prevention
o Restore thermoregulation
▪ Increasing the temp to rapidly can cause complications such as apnea
o Perform expanded assessment
▪ Ingestion of warm colostrum or breast milk helps warm the infant
▪ Evaluation
Application of the Nursing Process: Hepatic Function - Blood Glucose
▪ Assessment
o Risk factors
o Signs of hypoglycemia
▪ Nursing diagnosis
▪ Expected outcomes
▪ Interventions
o Maintain safe glucose levels
▪ Feed the newborn if the glucose screening shows 40-45 mg/dL or less to prevent further depletion of
glucose
▪ Glucose water alone is not recommended for newborns because the rapid rise in glucose results in
increased insulin production, causing a further drop in blood glucose
▪ Milk provides a longer-lasting supply of glucose
o Repeating glucose tests
o Provide other care
▪ Infants who do not have enough glucose may experience a drop in temp that could lead to respiratory
distress as oxygen is used for non-shivering thermogenesis
▪ Evaluation
Applications of the Nursing Process: Hepatic Function - Bilirubin
▪ Assessment
o Assess for jaundice by blanching the infant’s skin on the nose or sternum
o Assess for jaundice every 8-12 hours along w/ vital signs
▪ Nursing diagnosis
o Hyperbilirubinemia may not occur until after discharge
▪ Expected outcomes
▪ Interventions
o Identify infants at risk for hyperbilirubinemia.
o Explain importance of adequate feedings to stimulate passage of stools and prevent high levels of bilirubin
▪ Giving water to jaundiced infants does not stimulate stool excretion and should be avoided
o Explain significance of skin color changes.
▪ Transcutaneous or serum bilirubin levels may be used to determine the degree of jaundice
o Continue to monitor during home or clinic visits.
▪ Tell the care provider if the infant is not eating well, voiding at least 6 times daily by the fourth day, and
producing stools appropriately (at least one stool per day for formula-fed infants and at least 4 stools
daily for breastfeeding infants)
▪ Evaluation
Ongoing Assessments and Care
▪ Assess every 8 hours
▪ Provide skin care
▪ Bathing61
▪ Cord care
o Becomes brownish black within 2 to 3 days and falls off within approximately 10-14 days
o Cord clamp is removed about 24 hours after birth if the end of the cord is dry---no danger of bleeding if the end is
dry and crisp
▪ Cleansing the diaper area
▪ Feedings
▪ Positioning
o Plagiocephaly flattening or asymmetry of the back of the head
▪ Protecting the infant
Circumcision
▪ Reasons for choosing circumcision
o Benefits:
▪ Reduces penile cancer, UTI’s for first year of life, HIV infection, and transmission of other sexually
transmitted diseases
o Phimosis tightening of the prepuce ---- which prevents retraction and thus requires circumcision
▪ Reasons for rejecting circumcision
o Less often practiced by families from Europe, Asia, South and Central America, Canada, and Australia
o Parents may be concerned about removing the prepuce, which serves to protect the glans
▪ Pain relief
o Dorsal penile nerve block (anesthetic injected into the dorsal penile nerve) is a safe method to eliminate pain
during circumcision
▪ Methods
▪ Nursing considerations
Application of the Nursing Process: Parents’ Knowledge of Newborn Care
▪ Assessment
o Parents’ learning needs.
o Mother’s and infant’s physical conditions
o Any special concerns
▪ Nursing diagnosis
▪ Expected outcomes
▪ Interventions
o Determining who teaches
o Setting priorities
o Using various teaching methods
o Modeling behavior
o Teaching intermittently
o Including the father
o Documenting teaching
o Providing for follow-up care
o Incorporating cultural considerations
▪ Evaluation
Immunization
▪ Hepatitis B
o Included with routine childhood vaccinations
o Immunize infant of mother who has acute or chronic infection
▪ Give vaccine---promotes antibody formation to protect infants from further exposure to the disease
▪ Give hepatitis B immune globulin
▪ Give globulin within 12 hours of birth
Newborn Screening Tests
▪ Hearing
▪ Phenylketonuria
o Genetic condition in which the infant cannot metabolize the amino acid phenylalanine, which is common in protein
foods such as milk
▪ Tx should be started by the 3rd week of life
▪ Tx with a special low-phenylalanine diet, in which the amount of amino acid is carefully regulated
▪ Hypothyroidism62
o S/S: hoarse cry, large fontanel and tongue, slow reflexes, abdominal distention, lethargy, and feeding problems,
and can lead to intellectual disability
▪ Galactosemia
o Absence of the enzyme necessary for the conversion of the milk sugar galactose to glucose causes galactosemia
o Condition results in damage to the liver, increased susceptibility to infection, intellectual disability, and other
developmental problems
o Tx: diet free of lactose and galactose
o Long erm complications such as delayed growth and neurologic impairment may occur even w/ treatment
▪ Hemoglobinopathies
o Include sickle cell anemia, thalassemia, and other disorders
o Most often found in infants of African, Mediterranean, Indian, or South and Central American background
o Cause chronic anemia’s, sepsis, and other serious conditions
▪ Congenital adrenal hyperplasia
o Refers to a group of disorders w/ an enzyme defect that prevents adequate adrenal corticosteroid and aldosterone
production and increases production of androgens
o Infant may have ambiguous genitalia or masculinization of female infants at birth
o Salt-wasting crisis w/ low sodium and glucose and high potassium levels may occur w/ in the first wk of life
o Tx: administration of corticosteroids and mineralocorticoids for the remainder of the child’s life
Tests performed within the frist 24 hours of life are less sensitive than those performed after 24 hours
Infants texted before age 12-24 hours should have repeat tests at age 1 to 2 wks so that disorders are not missed because
testing was done to early
Discharge and Newborn Follow-Up Care
▪ Early discharge
o Appropriate for gestational age
o Vital signs within normal limits---- for the 12 hours before discharge
o Feeding successfully---at least twice
o Making transition from fetal to neonatal life
o Passed urine and stool
o No excessive bleeding at the circumcision site for at least 2 hours
o Mother able to care for infant
▪ Follow-up care
o Professional follow-up care recommended with early discharge
▪ Recommends that follow up care be provided within 48 hours for all newborns who are taken home from
the birth facility less than 48 hours after birth
▪ Any infant who is breastfeeding or has other risk factors should be seen within the first wee and usually
within 2-3 days discharge
o Can be provided in a number of ways
Which occurrence is associated with cervical dilation and effacement?
a) Bloody show
▪ As the cervix begins to soften, dilate, and efface, expulsion of the mucus plug that sealed the cervix during
pregnancy occurs. This causes rupture of small cervical capillaries. Cervical dilation and effacement do not
occur with false labor. Lightening is the descent of the fetus toward the pelvic inlet before labor. Bladder
distension occurs when the bladder is emptied frequently. It may slow down the decent of the fetus
during labor.
b) False labor
c) Lightening
d) Bladder distention
A laboring woman is lying in the supine position. The most appropriate nursing action is to:
a) Ask her to turn to one side.63
▪ The woman's supine position may cause the heavy uterus to compress her inferior vena cava, reducing
blood return to her heart and reducing placental blood flow. This problem is relieved by having her turn
onto her side. Elevating her legs will not relieve the pressure from the inferior vena cava. This position
may produce hypotension in the woman, but the action should be to prevent this from happening, not to
assess for the problem. If the woman is allowed to stay in the supine position, and blood flow to the
placental is reduced significantly, fetal tachycardia may occur. The most appropriate nursing action is to
prevent this from occurring by turning the woman to her side.
b) Elevate her feet and legs.
c) Take her blood pressure.
d) Determine whether there is fetal tachycardia.
The nurse notes a pattern of late decelerations on the fetal monitor. The most appropriate action is to:
a) Continue observation of this reassuring pattern.
b) Notify the physician or nurse-midwife.
c) Give the woman oxygen by face mask.
o Late decelerations are associated with reduced placental perfusion. Giving the laboring woman oxygen
increases the oxygen saturation in her blood, making more oxygen available to the fetus. Late
decelerations are not a reassuring pattern; interventions are needed. Nursing interventions should be
initiated before notifying the health care provider. The Trendelenburg position will not increase the
placental perfusion.
d) Place the woman in a Trendelenburg position.
The most important nursing intervention after the injection of epidural anesthesia is monitoring:
a) Urinary output.
b) Contractions.
c) Maternal blood pressure.
o Epidural anesthesia may produce maternal hypotension due to vasodilation. The mother is prone to
bladder distention and this needs to be monitored. However, this does not become a problem until 1 to 3
hours later. Continuing monitoring of the contractions is important because they may be altered by the
epidural. However, this is not the most important nursing intervention after the epidural is administered.
The intravenous infusion needs to be maintained before, during, and after the epidural. However, it is not
the most important nursing intervention at this point.
d) Intravenous infusion rate.
The primary risk associated with an amniotomy is:
a) Maternal infection.
b) Maternal hemorrhage.
c) Prolapse of the umbilical cord.
▪ When the membranes are ruptured, the umbilical cord may come downward with the flow of amniotic
fluid and become trapped in front of the presenting part. Infection is a risk of amniotomy, but not the
primary concern. Maternal hemorrhage is not associated with amniotomy. This may occur if the uterus is
overdistended before the amniotomy, but it is not the major concern.
d) Separation of the placenta.
Which nursing action is most appropriate to correct a boggy uterus that is displaced above and to the right of the umbilicus?
a) Notify the physician of an impending hemorrhage.
b) Assess the blood pressure and pulse.
c) Evaluate the lochia.
d) Assist the client in emptying her bladder.
▪ Urinary retention can cause overdistention of the urinary bladder, which lifts and displaces the uterus.
Nursing actions need to be implemented before notifying the physician. This is an important assessment if
the bleeding continues. However, the focus should be on controlling the bleeding.
The best way for the nurse to promote and support the maternal-infant bonding process is to:
a) Help the mother identify her positive feelings toward the newborn.
b) Encourage the mother to provide all newborn care.
c) Assist the family with rooming-in.
▪ Close and frequent interaction between mother and infant, which is facilitated by rooming-in, is
important in the bonding process. Having the mother express her feelings is important, but it is not the
best way to promote bonding. The mother needs time to rest and recuperate; she should not be expected64
to do all of the care. The mother needs to observe the infant during all stages so she will be aware of what
to expect when they go home.
d) Return the newborn to the nursery during sleep periods.
How can the nurse help the mother who is breastfeeding and has engorged breasts?
a) Suggest that she switch to bottled formula just for today
b) Assist her to remove her bra, making her more comfortable
c) Apply heat to her breasts between feeding and cold to the breasts just before feedings
d) Instruct and assist the mother to massage her breasts
▪ Massage of the breasts causes release of oxytocin and increases the speed of milk release. Engorgement
is more likely to increase if breastfeeding is delayed or infrequent. A well-fitting bra should be worn both
day and night to support the breasts. Cold applications are used between feedings to reduce edema and
pain. Heat is applied just before feedings to increase vasodilation.
A first-time father is concerned that his 3-day-old daughter's skin looks "yellow." In the nurse's explanation of physiologic
jaundice, which point should be included?
a) Physiologic jaundice occurs during the first 24 hours of life.
b) Physiologic jaundice is caused by blood incompatibilities between the mother and infant blood types.
c) The bilirubin levels of physiologic jaundice peak at 5 to 7 mg/dL between the second and fourth days of life.
▪ Physiologic jaundice becomes visible when the serum bilirubin reaches 5 to 7 mg/dL, which occurs when
the baby is approximately 3 days old. This finding is within normal limits for the newborn. Pathologic
jaundice occurs during the first 24 hours of life. Pathologic jaundice is caused by blood incompatibilities,
causing excessive destruction of erythrocytes, and must be investigated. Breast milk jaundice occurs in
one third of breastfed infants at 2 weeks and is caused by an insufficient intake of fluids.
d) This condition is also known as breast milk jaundice.
Plantar creases need to be evaluated within a few hours of birth because:
a) The newborn has to be footprinted.
b) As the skin dries, the creases will become more prominent.
▪ As the infant's skin begins to dry, the creases will appear more prominent, and the infant's gestation could
be misinterpreted. Footprinting will not interfere with the creases. Heel sticks will not interfere with the
creases. The creases will appear more prominent after 24 hours.
c) Heel sticks may be required.
d) Creases will be less prominent after 24 hours.
The nurse's initial action when caring for an infant with a slightly decreased temperature is to:
a) Notify the physician immediately.
b) Wrap the infant in two warmed blankets and place a cap on his or her head.
▪ A cap will prevent further heat loss from the head, and having the mother place the infant skin-to-skin
should increase the infant's temperature. Nursing actions are needed first to correct the problem. If the
problem persists after interventions, notification may then be necessary. A slightly decreased
temperature can be treated in the mother's room. This would be an excellent time for parent teaching on
prevention of cold stress. Mild temperature instability is an expected deviation from normal during the
first days as the infant adapts to external life.
c) Tell the mother that the infant must be kept in the nursery and observed for the next 4 hours.
d) Change the formula because this is a sign of formula intolerance.
[Show More]