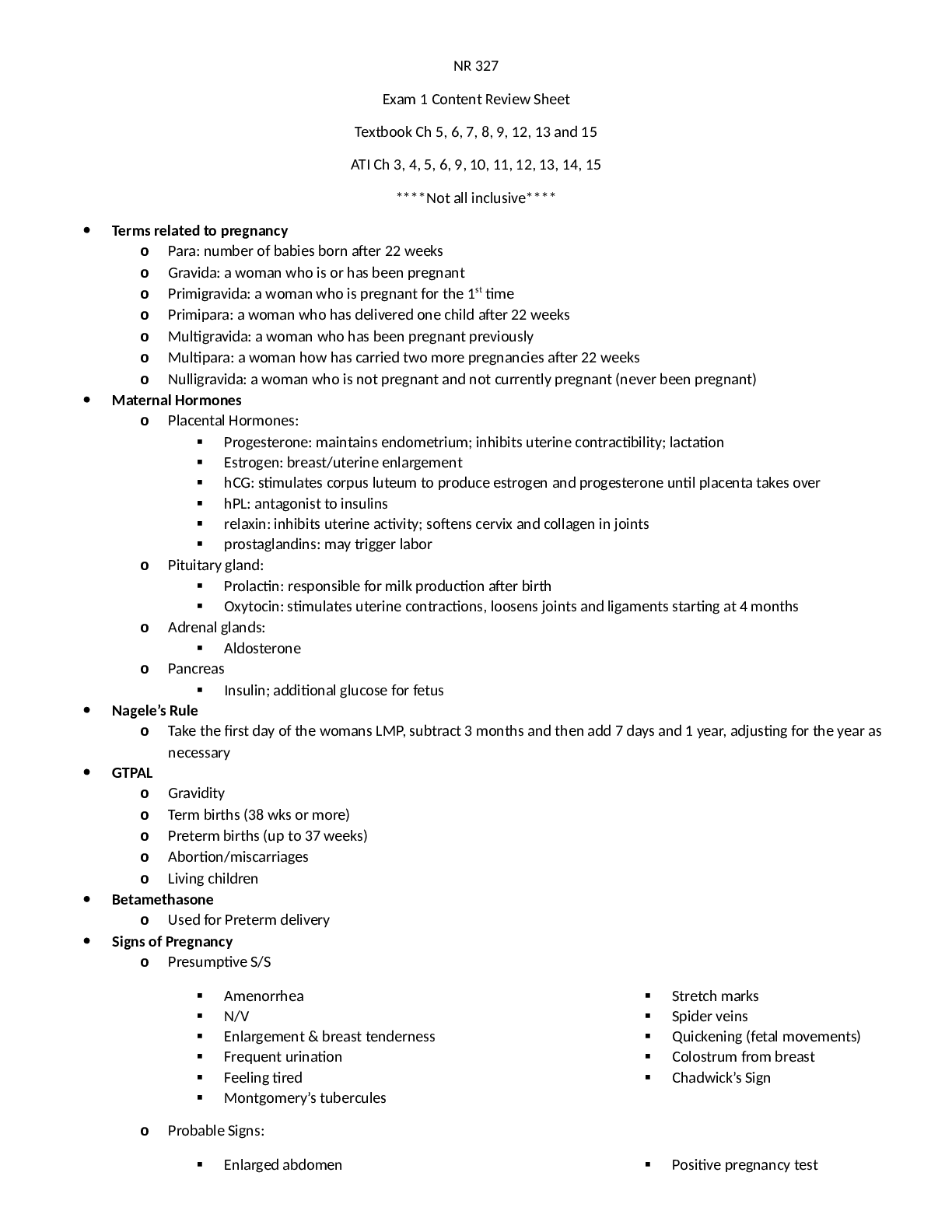
NR 327
Exam 1 Content Review Sheet
Textbook Ch 5, 6, 7, 8, 9, 12, 13 and 15
ATI Ch 3, 4, 5, 6, 9, 10, 11, 12, 13, 14, 15
****Not all inclusive****
Terms related to pregnancy
o Para: number of babies born after 22
...
NR 327
Exam 1 Content Review Sheet
Textbook Ch 5, 6, 7, 8, 9, 12, 13 and 15
ATI Ch 3, 4, 5, 6, 9, 10, 11, 12, 13, 14, 15
****Not all inclusive****
Terms related to pregnancy
o Para: number of babies born after 22 weeks
o Gravida: a woman who is or has been pregnant
o Primigravida: a woman who is pregnant for the 1st time
o Primipara: a woman who has delivered one child after 22 weeks
o Multigravida: a woman who has been pregnant previously
o Multipara: a woman how has carried two more pregnancies after 22 weeks
o Nulligravida: a woman who is not pregnant and not currently pregnant (never been pregnant)
Maternal Hormones
o Placental Hormones:
Progesterone: maintains endometrium; inhibits uterine contractibility; lactation
Estrogen: breast/uterine enlargement
hCG: stimulates corpus luteum to produce estrogen and progesterone until placenta takes over
hPL: antagonist to insulins
relaxin: inhibits uterine activity; softens cervix and collagen in joints
prostaglandins: may trigger labor
o Pituitary gland:
Prolactin: responsible for milk production after birth
Oxytocin: stimulates uterine contractions, loosens joints and ligaments starting at 4 months
o Adrenal glands:
Aldosterone
o Pancreas
Insulin; additional glucose for fetus
Nagele’s Rule
o Take the first day of the womans LMP, subtract 3 months and then add 7 days and 1 year, adjusting for the year as
necessary
GTPAL
o Gravidity
o Term births (38 wks or more)
o Preterm births (up to 37 weeks)
o Abortion/miscarriages
o Living children
Betamethasone
o Used for Preterm delivery
Signs of Pregnancy
o Presumptive S/S
Amenorrhea
N/V
Enlargement & breast tenderness
Frequent urination
Feeling tired
Montgomery’s tubercules
Stretch marks
Spider veins
Quickening (fetal movements)
Colostrum from breast
Chadwick’s Sign
o Probable Signs:
Enlarged abdomen Positive pregnancy test Changes in uterine shape
Softening of the cervix (Goodell’s
sign)
Enlarging uterus
Braxton hick’s contraction
Hegar’s sign
Palpation of the baby
Ballottement
o Positive Signs
Fetal heart sounds
X-ray
Actual delivery of infants
Reproduction (ovulation)
Emotional Response/ Psychological tasks of Pregnancy
o Emotional Response
Ambivalence
Grief
Self-centered; feels needs to
protect body
Introversion or extroversion
Body image changes
Stress
Mood changes
Sexual desire changes
Couvade syndrome
o Psychological tasks of pregnancy
1st trimester: accept pregnancy
2nd trimester: accept baby
3rd trimester: preparing for baby, nesting, attachment with baby
Prenatal Care/ Appointments, Prenatal Tests
o Prenatal Care
Ultrasound and hcG confirms pregnancy
Complete H&H
Genetic disorders, chronic illness, meds, obstetrical hx, personal habits
Complete physical exam
VS, wt/ht, pelvic exam, assess size/shape of boney pelvis
Subsequent visits
Physical assessment
Measure fundal ht
o Fundal ht=wks of gestation
Ht larger than wks means too much amniotic fluid or multiple babies
Ht smaller than weeks means intrauterine growth restriction
Urinalysis
Teaching
Fetal heart tones
Fetoscope: 16 wks, and always by 19-20 wks
Routine Lab Test:
Blood type, Rh factor, and presence of irregular antibodies
CBC w/ differential, hgb, and Hct
Hgb electrolytes
GBS
Vaginal/cervical culture
Maternal Nutrition
o Maternal wt gain depends on BMI and pre pregnant nutrition state
Underwt. Woman: 28-40 lbs.
Normal: 25-35
Overweight: 15-27 lbs.
Obese: at least 15 lbs.
Gain of 3.5 lbs. during 1st trimester
Gain about 1lb weekly rest of pregnancy
o Heart burn: take tums and small frequent meals
o Calorie Intake:
Increase 340 kcal/day during second and 452 kcal/day during third trimester Considerations: nutrition for prego adolescent, postpartum nutritional support, breastfeeding woman,
non-nursing woman
Patient teaching (pain management)
Changes in Pregnant Body
o Reproductive: uterus increases in size and changes shape and position. Ovulation and menses cease during
pregnancy
o Cardiovascular:
Cardiac output increases (30-50%) and blood volume increases (30-45% at term)
HR increases during pregnancy beginning around week 5 and reaches a peak (10-15/min) around 32
weeks
First trimester: no change
2nd trimester: systolic and diastolic decreases 5-10 mmHg
3rd trimester: Returns to first trimester levels
Supine hypotension syndrome can occur in the 2nd half of pregnancy (vertigo, decreased BP)
Palpitations and murmurs can cause an issue for these issues
o Respiratory:
Maternal oxygen needs increase
Last trimester size of chest might enlarge, allow for lung expansion, as the uterus pushes upward
Respiratory rate increases and total lung capacity decreases
Respiratory rate 18-20
Nasal stuffiness (1st trimester)
SOB (2nd trimester)
Dyspnea: Estrogen causes URT to become vascular, capillaries fill edema develops in the nose
Interventions: use cool air vaporizer
NO SPRAYS
Proper position; semi-Fowlers when sleeping
o Musculoskeletal:
Calcium and phosphorous needs increase
Changes in gravity
Gradual softening of pelvic ligaments and joints (pelvic joints relax)
Lordosis:
Caused by relaxin and progesterone
Leg cramps and backache (late pregnancy)
o Good nutrition, rest with legs elevated, wear warm clothing
o During leg cramp, pull toes up toward the leg while pressing down on the ankle
o Use proper body mechanics; avoid high heels
o GI:
N/V (1st trimester)
Constipation
Gingivitis
Increased saliva
Increased gastric acid (heartburn/pyrosis)
Interventions: avoid greasy, highly seasoned food, eat small meals frequently, eat dry toast or
crackers before arising, warm sprite and ginger ale
Sit upright 1 hour after eating
Sodium bi carb after eating
6-8 glasses of water every day
o Integumentary System:
Linea Nigra: hormone induced pigmentation, dark line that runs from the umbilicus to the symphysis
pubis and may extend as high as the sternum
Chloasma (mask of pregnancy): brownish hyperpigmentation of the skin over the face and forehead
It begins about the 16th week of pregnancy and gradually increases then it usually fades after delivery
Straie Gravidarum: stretch marks, due to action of adrencorticosteroids
Separation within underlying connective tissue of the skin Occurs over areas of maximal stretch-the abdomen thighs and breast
May never completely disappear
o Renal:
Filtration rate increases secondary to the influence of pregnancy hormones and increase in blood volume
and metabolic demands, amount of urine produced remains same
Urinary frequency is common
o Endocrine: hormones are very active during pregnancy to maintain pregnancy and function to maintain pregnancy
and prepare body for delivery
Umbilical cord/ Amniotic Fluid/ Placenta
o Placenta:
It is completely formed by the third month of pregnancy.
The umbilical cord connects the fetus to the placenta and is normally 20 inches in length and 3/4 inch in
diameter.
Adequate perfusion cause Vascular volume increase in mother 40-60%
Transports oxygen, nutrients, and antibodies to the fetus by means of the umbilical vein
Removes carbon dioxide and metabolic wastes from the fetus by the two umbilical arteries
Serves as a protective barrier against harmful effects of certain drugs and microorganisms
Acts as a partial barrier between the mother and fetus to prevent fetal and maternal blood from mixing
Produces hormones essential for maintaining the pregnancy. (estrogen, progesterone, and human
chorionic gonadotropin (HCG)).
After birth of the placenta Prolactin is responsible for milk production
o Umbilical Cord:
Lifeline to mom
Baby gets oxygen to breathe from umbilical vein
Wharton jelly: prevent obstruction resulting from pressure
o Amniotic Fluid:
The fetus floats and moves in the amniotic cavity.
It is filled with amniotic fluid
At full term, this cavity normally contains 500 cc to 1000 cc of fluid (water).
Protect the fetus from direct trauma.
Separate the fetus from the fetal membranes.
Allow freedom of fetal movement (buoyancy) and permits musculoskeletal development.
Facilitate symmetric growth and development of the fetus.
Protect the fetus from the loss of heat and maintains a relative, constant fetal body temperature.
Serve as a source of oral fluid for the fetus.
Act as an excretion and collection system.
Fetal Development
o First Trimester:
First three months of pregnancy: fertilized ovum to an embryo.
All organs are formed.
The fetus becomes less vulnerable to the effects of most drugs, most infections, and radiation.
Facial features are forming, and the fetus becomes human in appearance.
External sex organs are visible, but positive sex identification is difficult.
Well-defined neck, nail beds beginning, and tooth buds form.
Rudimentary kidneys excrete small amounts of urine into the amniotic sac.
There is movement but just not strong enough to be felt.
The fetus is about 2.9 inches long and weighs about 14 grams.
4 weeks
The nervous system (brain and spinal cord) has begun to form.
The heart begins to form.
Arm and leg buds begin to develop.
Your baby is now an embryo and 1⁄25 of an inch long.
8 weeks
All major organs have begun to form.
The baby's heart begins to beat. The arms and legs grow longer.
Fingers and toes have begun to form.
Sex organs begin to form.
The face begins to develop features.
The umbilical cord is clearly visible.
At the end of 8 weeks, your baby is a fetus, and is nearly 1 inch long, weighing less than ⅛ of an
ounce.
12 weeks
The nerves and muscles begin to work together. Your baby can make a fist.
The external sex organs show if your baby is a boy or girl.
Eyelids close to protect the developing eyes. They will not open again until week 28.
Head growth has slowed, and your baby is about 3 inches long, and weighs almost an ounce.
o 2nd Trimester:
During these months (4th, 5th, and 6th) the fetus grows fast. At the end of the second trimester, the
fetus…
Fetal heart tone (FHT) can be heard with a stethoscope.
Skin is wrinkled, translucent, and appears pink.
Sex is obvious.
Looks like a miniature baby.
Skeleton is calcified.
Birth survival is possible, but the fetus is seriously at risk.
16 wks
The musculoskeletal system continues to form.
Skin begins to form and is nearly translucent.
Meconium develops in your baby's intestinal tract. This will be your baby's first bowel
movement.
Your baby begins sucking motions with the mouth (sucking reflex).
Your baby is about 4 to 5 inches long and weighs almost 3 ounces.
20 wks
Your baby is covered by fine, feathery hair called lanugo and a waxy protective coating called
vernix.
Eyebrows, eyelashes, fingernails, and toenails have formed. Your baby can even scratch itself.
Your baby can hear and swallow.
Now halfway through your pregnancy, your baby is about 6 inches long and weighs about 9
ounces.
24 wks
The baby's bone marrow begins to make blood cells.
Taste buds form on your baby's tongue.
Footprints and fingerprints have formed.
Hair begins to grow on your baby's head.
The lungs are formed, but do not yet work.
Your baby has a regular sleep cycle.
If your baby is a boy, his testicles begin to descend into the scrotum. If your baby is a girl, her
uterus and ovaries are in place, and a lifetime supply of eggs has formed in the ovaries.
Your baby stores fat and weighs about 1½ pounds and is 12 inches long.
o 3rd Trimester:
At the end of the third trimester (7th, 8th, and 9th month), the fetus:
Skin is whitish pink.
Hair in single strands.
Testes are in the scrotum, if a male child.
Bones of the skull are firmer, comes closer at the suture lines.
Lightening occurs.
Fetus is about 20 inches long and weighs about 3300 grams.
36 wks
The protective waxy coating (vernix) thickens.
Body fat increases. Your baby is getting bigger and has less space to move around. Movements are less forceful, but
you will still feel them.
Your baby is about 16 to 19 inches long and weighs about 6 to 6½ pounds.
37-40 wks
By the end of 37 weeks, your baby is considered full term.
Your baby's organs are capable of functioning on their own.
As you near your due date, your baby may turn into a head-down position for birth.
Average birth weight is between 6 pounds, 2 ounces to 9 pounds, 2 ounces and average length is
19 to 21 inches long. Most full-term babies fall within these ranges, but healthy babies come in
many different weights and sizes.
o Cardiovascular
Heartbeat heard at 10 weeks by Doppler
Heard at 16 weeks via fetoscope
o Respiratory
Surfactant matures by 36th week
Surfactant permits expansion of the lungs
o GI system
Meconium (tarry stool)
o Urinary system
By 5th month, fetus urinates into amniotic fluid
2nd half of pregnancy: urine makes up major part of amniotic fluid
o Sexual
Can identify male/female by 16th week
o
Tests for Fetal well Being
o Ultrasound: dx procedure using high frequency sound waves to visualize development
Indications: confirm pregnancy, site of implantation, assess fetal growth, development, movement
Preparation: have patient drink 1 quart of water
o Biophysical profile: combines FHR monitoring (nonstress test) and fetal ultrasound
Measures 5 variables with a score of 2 for each normal finding, and 0 for abnormal
FHR
Fetal Breathing movements: 1 or more episodes > 30 seconds=2, absent of <30 sec=0
Gross body movements: 3 or more body/limb extensions with return to flexions=2, less than 3
episodes=0
Fetal tone: 1 or more episodes of extension with return to flexion=2, lack of flexion or absent
movement=0
Qualitative amniotic fluid volume: 1 pocket>= 2cm in 2 perpendicular planes=2. Absent of <2cm
pockets=0
Normal: 8 to 10, low risk
Abnormal: 4 to 6, suspect chronic fetal asphyxia
Abnormal: < 4, strongly suspect chronic fetal asphyxia
o Nonstress test identifies an increase in the FHR when the fetus moves
Indicating adequate oxygenation
Healthy neural pathway
Ability for fetal heart to respond to stimuli
During 3rd trimester, mom pushes button attached to monitor when she feels fetal movement
Results: reactive 2 FHR acceleration in 20 min
Nonreactive (nonreassuring), FHR does not accelerate sufficiently with fetal movement
o Contraction stress Test
Nipple stimulated: lightly brushing palm across nipple for 2 minutes, oxytocin is released
Stop when contraction begins and repeated after 5 min rest period
Determines how fetus will tolerate stress of labor
Oxytocin-stimulated contraction test: used when nipple stimulation fails and consist of IV admin of
oxytocin to induce uterine contraction
Hyperstimulation occurs monitor contractions lasting longer than 90 seconds Admin tocolytics
Maintain bed rest
Observe pt for 30 min afterward to see if contractions have ceased
Results:
Normal: no late decelerations of FHR with 3 contractions in 10 min
Abnormal: late decelerations present in 50% or more of contractions, indicative of uteroplacental
insufficiency
Complications:
Pre-term labor
Amniocentesis: amniotic fluid is aspirated under ultrasound guidance, performed after 14 weeks
Assess fetal lung maturity and well being
Chromosome analysis of cell can determine abnormalities
Measurement of alpha-fetoprotein
o High: neural tube defects
o Low: chromosomal disorders (down syndrome)
Patient care: empty bladder prior to procedure, post-procedure administer RhoGAM to Rhnegative moms, encourage rest and plenty of fluids for 24 hours, rest for 30 minutes, and
monitor vital signs, FHR, and uterine contractions through and 30 minutes following
Gestational Diabetes (general)
o Impaired tolerance to glucose with the first onset or recognition during pregnancy
Ideal level: 70-110
o Increased risk to fetus:
Spontaneous abortion
Infections
Hydramnios
Ketoacidosis
Hypoglycemia
hyperglycemia
Medications (Pitocin, magnesium sulfate, Zofran, etc)
Signs of impending labor, True vs. False labor
o True labor
Progressive dilation & effacement of the cervix, regular and increase in frequency duration & intensity,
showing, cervix becomes effaced and dilates progressively, no significant change
o False labor:
no progressive dilatation & effacement, irregular, no increase in frequency, duration, intensity, no
showing, cervix: uneffaced and closed, fetal movement may intensify for a short period or it many remain
the same
Fetal Descent Stations (Engagement)
o How far the baby is “down” in the pelvis, measure by the relationship of the fetal head to the ischial spine
o Measure in (-) & (+) numbers (cm), ischial spine is in (0) station
o If presenting part is higher than ischial spine the state has a (-) negative #
o Positive= presenting part is passed the ischial spine, positive (+) 4 is at the outlet
Signs of Fetal Distress
o Normal Fetal HR: 110 to 160 bpm
o Ominous FHR pattern
o Fetal acidosis
o Meconium-stained amniotic fluid
o Decrease or cessation of fetal movement
o Nursing Interventions:
Monitor FHR, fetal activity, and fetal heart variability
Identify and correct the cause if possible
Position patient on the side to enhance uteroplacental blood flow
Admin oxygen via face mask as order (usually 8-10L/min)
Increase nonadditive IV fluids Discontinue oxytocin infusion if in use
Assist with AROM (artificial rupture of membranes) and placement of internal fetal electrode
Notify MD immediately if no improvement
Prepare for c-section
Preoperative education and informed consent
Tx. Depends on underlying cause
Non-pharmacologic and Pharmacologic Pain Management
o Non-pharmacologic: Lamaze
o Pharmacologic:
Analgesics
Anesthetics
Epidural or Spinal
Local
Side effects of Narcotics
Stages of Labor
o The first stage of labor is referred to as the "dilating" stage.
o It is the period from the first true labor contractions to complete dilatation of the cervix (10cm)
o The forces involved are uterine contractions.
o The first stage of labor is divided into three phases:
Latent phase : 0-3 cm dilated
Active phase: 4-7 cm dilated
Transitional phase: 8-10 cm dilated
o Latent:
Ends when cervix is dilated 4 cm.
Contractions more frequent.
The duration becomes longer.
Intensity - moderate.
Mother is usually alert and talkative, can walk
Contractions last from 30 to 45 seconds The frequency of contractions is from 5 to 20 minutes.
True labor is considered to be at 4 cm.
Duration varies, sometimes as long as 24 hours.
o Active:
Begins when cervix is dilated 4 cm, ends when the cervix is dilated 8 cm.
Contractions occur every 3 to 5 minutes with a duration of 40 to 60 seconds.
Intensity progresses to strong.
The client focuses more on breathing techniques in contractions, less talkative.
Unable to walk
This phase is considered the onset of true labor.
o Transition Phase
Begins when cervix is dilated 8 cm, ends when cervix is dilated 10 cm.
Contractions occur every 2 to 3 minutes
Duration of 60 to 90 seconds.
The intensity of contractions is strong.
Completion of this phase marks the end of the first stage of labor.
Urge to push or to have a BM
o Nursing Care:
Establish a rapport with the patient and significant others.
Explain all procedures or routines, which will be carried out prior to performing them. These include:
NPO except ice chips while in labor.
Use of fetal monitors.
Progress reports.
Visitation policies.
Where patient's personal belongings will be maintained.
o 2nd Stage:
Begins when cervical dilatation is complete and ends with birth of the baby.
Impending Signs:
Bulging of the perineum. Dilatation of the anal orifice.
Nausea, Irritability and uncooperativeness.
Complaints of severe discomfort.
Dilatation and effacement – complete - patient is instructed to push with each contraction to bring the
presenting part down into the pelvis
Nursing Care:
Patient to rest between contractions
Push with contractions
One person should coach.
Verbal encouragement and physical contact help reassure and encourage the patient.
Monitor the patient's BP and the FHR every 5 minutes and after each contraction.
o 3rd Stage:
The period from birth of the baby through delivery of the placenta.
Dangerous time because of the possibility of hemorrhaging.
Signs of the placental separation
The uterus becomes globular in shape and firmer.
The uterus rises in the abdomen.
The umbilical cord descends three inches or more further out of the vagina.
Sudden gush of blood.
Nursing Care:
Following delivery of the placenta:
Observation of the fundus.
Retention of the tissues in the uterus can lead to uterine atony and cause hemorrhage.
Massaging the fundus gently will ensure that it remains contracted.
Allow the mother to bond with the infant. Show the infant to the mother and allow her to hold
the infant
o 4th Stage:
Period from the delivery of the placenta until the uterus remains firm on its own.
Uterus makes its initial readjustment to the non-pregnant state.
The primary goal is to prevent hemorrhage from the uterine atony and the cervical or vaginal lacerations.
Atony is the lack of normal muscle tone. Uterine atony is failure of the uterus to contract.
Referred as the Recovery Stage
First 4 hours after the birth.
Blood loss is usually between 250 mL and 500 mL.
Uterus should remain contracted to control bleeding, positioned in the midline of the abdomen, level with
the umbilicus.
Mother may experience shaking chills
Nursing Care:
An ice pack may be applied to the perineum to reduce swelling from episiotomy especially
Vital signs
Evaluated the fundal height and firmness
Evaluated the lochia.
Suction and oxygen in case patient becomes eclamptic.
Pitocin® is available in the event of hemorrhage.
Reasons for Augmentation/Induction of Labor
o Induction:
Preeclampsia, eclampsia, or chronic HTN
IUGR: not getting nutrients needed
ROM without spontaneous onset of labor
Nonreassuring fetal status
Post term gestation
Elective induction for the convenience of mother or practitioner is not recommended
Contraindications for Augmentation/Induction of Labor
o Contraindications for Induction of Labor
Uterine surgery
Placenta previa
Macrosomia, hydrocephalus Mal presentations
Non reassuring fetal status
Cephalon pelvic disproportion
Maternal active genital herpes
C-section birth, Forcep/Vacuum assisted birth
o C-Birth
Birth of an infant through an incision in the abdomen and uterus.
Scheduled or unscheduled.
When C/Section is unscheduled: the nurse needs to review with the client events before the C/Section to
ensure the client understands what happened
o Forceps-Assisted Birth
Forceps are metal instruments used on fetal head to assist in delivery.
Cervix must be completely dilated, and membranes must be ruptured.
Position and station of fetal head must be known.
Newborn possible facial bruising, edema.
o Vacuum-Assisted Birth
Indications are same as for forceps-assisted birth.
Maternal risks include vaginal and rectal lacerations.
Fetal risks: cephalhematoma, brachial plexus palsy, retinal and intracranial hemorrhage
Factor that may extend or influence the duration of labor- 4 P’s
o Passage: if baby is too big and cannot come through passage
o Passenger: breeched
o Powers: quality, force and frequency of uterine
o Psyche: mother’s attitude toward labor and her preparation for labor. Culture, anxiety/fear
[Show More]