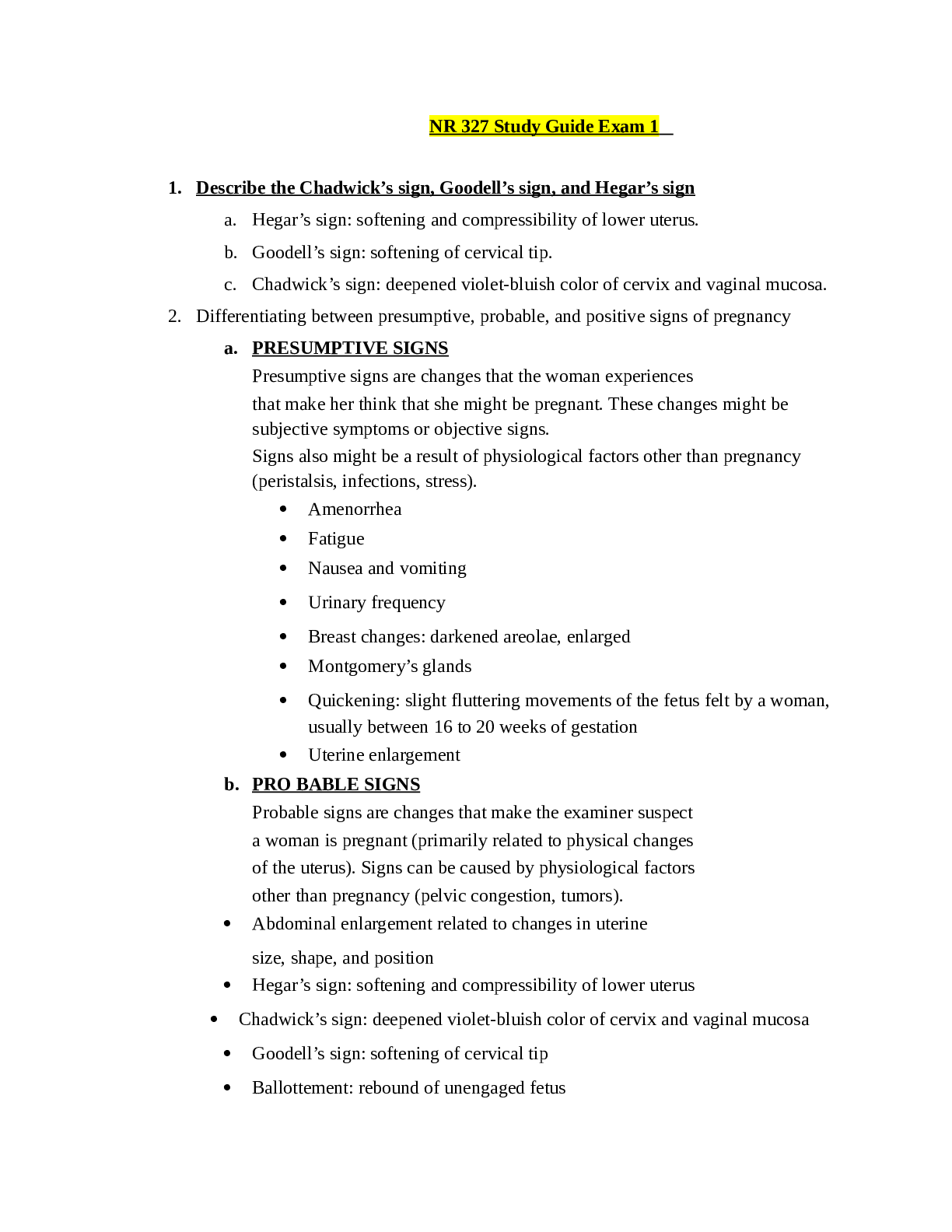
NR 327 Study Guide Exam 1
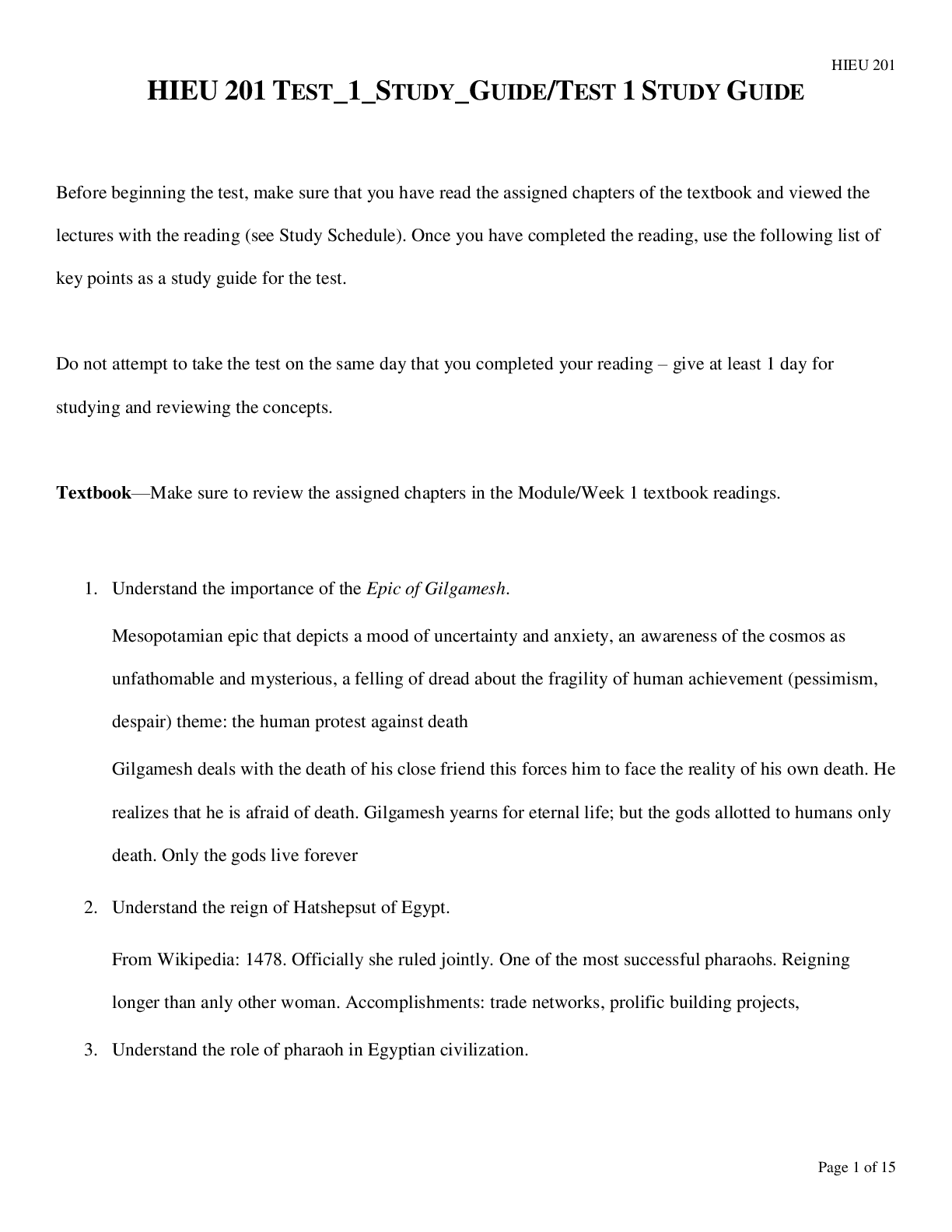
1. Describe the Chadwick’s sign, Goodell’s sign, and Hegar’s sign
a. Hegar’s sign: softening and compressibility of lower uterus.
b. Goodell’s sign: softening of cervical tip.
c. Chadwick’s
...
NR 327 Study Guide Exam 1
1. Describe the Chadwick’s sign, Goodell’s sign, and Hegar’s sign
a. Hegar’s sign: softening and compressibility of lower uterus.
b. Goodell’s sign: softening of cervical tip.
c. Chadwick’s sign: deepened violet-bluish color of cervix and vaginal mucosa.
2. Differentiating between presumptive, probable, and positive signs of pregnancy
a. PRESUMPTIVE SIGNS
Presumptive signs are changes that the woman experiences
that make her think that she might be pregnant. These changes might be
subjective symptoms or objective signs.
Signs also might be a result of physiological factors other than pregnancy
(peristalsis, infections, stress).
Amenorrhea
Fatigue
Nausea and vomiting
Urinary frequency
Breast changes: darkened areolae, enlarged
Montgomery’s glands
Quickening: slight fluttering movements of the fetus felt by a woman,
usually between 16 to 20 weeks of gestation
Uterine enlargement
b. PRO BABLE SIGNS
Probable signs are changes that make the examiner suspect
a woman is pregnant (primarily related to physical changes
of the uterus). Signs can be caused by physiological factors
other than pregnancy (pelvic congestion, tumors).
Abdominal enlargement related to changes in uterine
size, shape, and position
Hegar’s sign: softening and compressibility of lower uterus
Chadwick’s sign: deepened violet-bluish color of cervix and vaginal mucosa
Goodell’s sign: softening of cervical tip
Ballottement: rebound of unengaged fetus
Braxton Hicks contractions: false contractions that are painless, irregular, and
usually relieved by walking
Positive pregnancy test
Fetal outline felt by examiner
c. POSITIVE SIGNSPositive signs are those that can be explained only by pregnancy.
Fetal heart sounds
Visualization of fetus by ultrasound
Fetal movement palpated by an experienced examiner
3. Identify the physiologic changes of the pregnant women to the various systems.
Cardiovascular
Cardiac output increases (30% to 50%) and blood volume increases (30% to 45%
at term) to meet the greater metabolic needs. Heart rate increases during
pregnancy beginning around week 5 and reaches a peak (10 to 15/min above
pre-pregnancy rate) around 32 weeks of pregnancy.
GI
Nausea and vomiting might occur due to hormonal changes and/or an increase of
pressure within the abdominal cavity as the pregnant client’s stomach and intestines
are displaced within the abdomen. Constipation might occur due to increased
transit time of food through the gastrointestinal tract and, thus, increased water
absorption.
Respiratory
Maternal oxygen needs increase. During the last trimester, the size of the chest
might enlarge, allowing for lung expansion, as the uterus pushes upward. Respiratory rate
increases and total lung capacity decreases.
Skin
Chloasma: an increase of pigmentation on the face
Linea nigra: dark line of pigmentation from the
umbilicus extending to the pubic area
Striae gravidarum: stretch marks most notably found on the abdomen and thighs
Urinary frequency
Musculoskeletal
Body alterations and weight increase necessitate an adjustment in posture. Pelvic
joints relax. Posture changes due to the weight of the growing uterus (Lordosis)
Relaxation of the bones of the pelvis occur
Round ligament pain occurs as the uterus becomes more gavid.
Uterus
grows up & out of the pelvic floor to accommodate the fetal growth
Palpated at 12 weeks week of pregnancy
16 weeks can be found midway between the symphysis pubis & the
umbilicus
20 weeks can be found at the umbilicus
36 weeks reaches the highest near the xyphoid process pushing up on the
diaphragm (this makes it difficult to breath especially lying down).
38 weeks the fetal head descends into the birth canal & drops the fundal
height.
Braxton hicks contractions throughout pregnancy as uterus grows
10-13% of maternal cardiac output goes to the uterus
RenalUterine position causes urinary frequency.
Progesterone causes hypertrophy & hyperplasia (smooth muscle)
Bladder capacity doubles by the last trimester & tone is decreased leading to
stress incontinence.
Nocturia is common
Kegel exercises after childbirth reduce urinary incontinence by strengthening the
pelvic floor.
5. Identify the essential reasons for balanced nutrition and increase in caloric needs of
the pregnant woman, appropriate weight gain per trimester. Exercise in pregnancy.
a. Normal BMI: 25-35 lbs
b. Above lbs: 15-25 lbs
c. Obese lbs: 11-20 lbs
d. Below: 28-40 lbs
e. 2/3 weight gained in the second and third trimester.
f. Too little weight gain is associated with low birth weight and SGA infants.
(SGA is small for gestational age, below the 10th percentile)
g. Too much weight gain: gestational diabetes, macrosomia (Large for
Gestational age), prolonged labor, birth trauma, and preeclampsia.
h. Nutrition: Increase caloric 340 calories per day, should get a minimum of
2200 calories per day.
i. Adequate rest
ii. Exercise, do not overdo it, exercise 30 minutes a day for gestational
diabetes. The safest and productive exercises is swimming, brisk
walking, indoor stationary cycling, and low-impact aerobics.
iii. Avoid caffeine
iv. Increase intake 8-10 cups/day
v. Vitamin supplements include iron & folic acid for oxygenation and
neuro development, (Too much Vitamin A is toxic to the fetus).
sources include fatty fish, egg yolks, butter, cream, and dark
yellow/orange fruits and vegetables (carrots, yams, apricots, squash,
cantaloupe)
vi. Avoid sodium rich canned foods, large fish due to mercury content
and contain bacteria and parasites. No soft cheese unless
pasteurized. No unpasteurized products. (raw meat, raw eggs,
wine, raw fish, processed meats.)
6. Identify the most common discomforts experienced by many women in all three of
the trimesters of pregnancy and interventions for each.
a. Nausea & vomiting: small more frequent meals
b. Heartburn: sitting up after eating, smaller meals
c. Backache: support devicesd. Round ligament pain: slowly change positions from sitting and standing,
support devices
e. Urinary Frequency/UTI’s: void q 2 hours, void before and after sex, wipe
front and back.
f. Varicosities: support hose
g. Constipation: increase water intake, exercise, fiber
h. Leg cramps
i. Candida Albicans: (thick creamy white discharge that can cause vulvar
redness, white patches on vaginal wall.)
7. Patient teaching as it relates to each trimester
a. First Trimester:
i. Visits 4 weeks apart
ii. Fundal height and fetal heart tones, V.S. bleeding, fetal growth; 11 to
14 weeks: optional genetic testing performed
b. Second Trimester: same as bullet point i. and ii from first trimester
i. 15 to 20 weeks: Quad screening (HcG, MSAFP) which screens for
genetic & Spinal cord abnormalities)
ii. 18 and 20 weeks: Ultrasound
iii. 27 to 28 weeks: glucose screening & hemoglobin check
c. Third Trimester: same as bullet point i. and ii. From first trimester
i. 28-36 weeks: visits are about 2-3 weeks apart.
ii. 28 week: Rhogam if needed
iii. 36 weeks: GBS & STI screening performed, pelvic exam for
dilation, assessment of the fetal position.
iv. 36 to 40 weeks: visits typically 1-2 weeks pelvic exam for dilation.
8. Education on smoking and the effects it can have in the developing fetus.
a. Smoking can cause many risk factors such as
i. Low birth weight
ii. Prematurity
iii. Still births, fetal death, infant death
iv. Respiratory complications
v. Congenital heart defects
vi. CNS effects
vii. Placental insufficiency; hypoxia (late decelerations)
viii. Congenital anomalies (cleft lip, palate)
9. True vs false labor. Danger signs to report
a. True Labor
i. Lightening: the drop of the fetus allowing the mother to take a deeper
breath.
ii. Contractions1. Regular, rhythmic, consistent, stronger and come closer
together.
iii. Bloody show: normal bleeding that occurs with cervical dilation.
iv. Loss of mucous plug: white/clear mucous
v. Rupture of membranes: gush or consistent leak of amniotic fluid
vi. Cervix Dilated!!!
b. False Labor
i. Contractions
1. Not consistent, often go away with activity, can have brownish
show
ii. No Dilation!!!
c. Dangers to Report
i. Bradycardia
ii. Late decelerations
iii. Tetanic contractions
iv. Hard ridged uterus
v. Bright red bleeding
vi. Blood pressure (varies)
vii. Fever
viii. Dizziness
10. Compare the differences between ultrasonography and trans-vaginal ultrasonography
and the nursing care associated with preparation for the procedure.
a. Two-dimensional and three dimensional
b. Use of soundwaves to create images
i. Does not cause discomfort-very safe
ii. MUST HAVE BLADDER FULL FOR PROCEDURE!
iii. External Ultrasound (US) and transvaginal (internal)
1. BEST WAY TO DETERMINE APPROXIMATE
GESTATIONAL AGE!!!
2. More accurate estimation in the early gestational period
3. Determines
a. Fetal position
b. Multiple babies
c. Location of pregnancy
d. Placenta
e. Sex
f. Viability
g. Abnormalities (congenital or otherwise)
iv. Clean patient after procedure, care, and explain the procedure,
ALWAYS to the patient.11. Fetal Testing: MSAFP why is it done, when is it done?
a. A screening tool (only) that is used in the Quad marker screening, Maternal
serum Alpha-fetoprotein; High: neural tube defects (spina bifida and
anencephaly); Low: Down Syndrome
i. High: >2.5 MoM
ii. Low: <0.4 MoM
b. HCG; High: Down Syndrome; Low: miscarriage; helps determine
chromosomal abnormalities
c. Unconjugated estriol: helps determine chromosomal abnormalities
d. Placental hormone inhibin A: helps figure out trisomy 18 in women <35 y/o
age; serum is drawn 16-18 weeks gestation.
12. Pre and post nursing care for a patient undergoing an amniocentesis.
a. Needle aspiration of amniotic fluid from the amniotic sac performed under
ultrasound guidance for examination.
b. Usually performed 15-20 weeks, determine also in the third trimester for fetal
lung maturity.
c. Need to have an empty bladder
d. Strenuous activity should be avoided for 24 hours.
e. Woman may feel cramping during or after the procedure.
f. Search for
i. Trisomy 21
ii. Intrauterine infections
iii. Rh positive fetus to Rh negative mother
iv. Fetal hemolytic disease
v. Fetal lung maturity
g. Pre-care: explain procedure, prep the patient, assist the MD, baseline strip
h. Post-care: Since it is invasive you must assess for labor and bleeding
following.
13. Describe how to calculate an EDC/EDD/EDB Nageles Rule?
a. In order to use this rule you will need LMP date
b. (-3) months (+7) days 1 year from LMP.
14. Describe Gravida and Para and its significance to the nurse with the health
assessment of the woman.
a. Gravida: a woman who is or was pregnant (number of pregnancies)
i. Nulligravida: never been pregnant
ii. Primigravida: 1st pregnancy
iii. Multigravida: more than 1 pregnancy
b. Parity: the number of pregnancies that reached 20 weeks of gestation
regardless of live birth.i. Nullipara: never been pregnant or has not reached completed 20 weeks
of gestation.
ii. Primipara: has 1 pregnancy and has reached 20 weeks of gestation.
iii. Multipara: has had 2 or more pregnancies of at least 20 weeks of
gestation.
15. GTPAL classification
a. It is a system used to clarify pregnancy history
b. GRAVIDA: a woman who is pregnant or was pregnant.
c. TERM: term pregnancies delivered 37 weeks or more.
d. PRETERM: pregnancies that reached 20 weeks of gestation regardless if
the infant was born alive but delivered before 39 weeks.
e. ABORTIONS: spontaneous or elective
f. LIVING CHILDREN
16. Describe the major milestones in each of the trimester with the growth and
development of the fetus.
a. First Trimester: (1-12)
i. By week 12 the fetus has developed all of these:
1. Eyes (9th week eyes closed) & ears.
2. Mouth, lips, tooth buds
3. Arms, hands, fingers, legs, toes
4. Kidneys, gall bladder, stomach
5. Heart (can hear heart beat by 10-12th week)
6. Sex
7. Placenta fully functioning
8. CRL is determined in ultrasound imagery from head to trunk
@ 45 grams by the end of the trimester.
b. Second Trimester (13-27)
i. Quickening manifested; face is more human-like at 16 week
ii. Fingerprints @ 20 week
iii. Viable & can hear 24 weeks
iv. CRL 820 g by the end of the trimester
c. Third Trimester (28-40)
i. Surfactant is formed, eyelids are open, greatest fetal weight gain, testes
descend @ 28 weeks
ii. Brown fat deposited, begin storing Fe, Ca, Phosphorus @ 32 weeks
iii. Maternal antibodies transferred @ 36 weeks
iv. Lightening: backaches increase; Braxton hicks (+) @ 36-40 weeks
17. Evaluation of fetal heart tones with Doppler.
a. Not continuous this allows for the clinician to hear FHR for a few seconds to a
few minutes.b. Used in the MD offices.
c. Used when having difficulty locating fetus.
18. When completing a NST, CST or the interpretation the results of a BPP, be able to
explain and teach to patient why, and how these tests are completed.
a. NST: mother is placed on a fetal monitor.
i. Increased FHR w/ movement= fetal w/ adequate oxygenation; ability
of the fetus to respond to stimuli. (NEGATIVE/REACTIVE IS
GOOD) (15 RATE INCREASE X 15 SECONDS)
ii. If the fetus does not elevate FHR or w/o movement= hypoxia, further
test is ordered. (POSITIVE/NONREACTIVE IS BAD) (NO 15
RATE INCREASE X 15 SECONDS.)
b. CST: used to determine fetal well being during contraction
i. A healthy placenta & fetus will be able to tolerate temporary
disruption of low oxygen levels during a uterine contraction
ii. Fetal Heart rate should remain same or accelerate immediately
following contraction-known as “variability” reactive.
iii. NEED 3 CTX’s ON A FETAL STRIP
iv. Contractions are produced by nipple stimulation or oxytocin challenge
which is a dilute amount of oxytocin IVPB (Intravenous Piggy-Back)
v. Explain the procedure to the mom
vi. NEGATIVE IS A GOOD TEST BECAUSE THERE IS NO DROP
IN FHR PRESENT.
vii. POSITIVE IS BAD AND REQUIRES FURTHER TESTING
BECAUSE THERE IS A DROP OF FHR AT LEAST 50% OF
THE CONTRACTIONS.
c. BPP: Biophysical Profile: test used to determine the overall condition of the
fetus.
i. It is a combination of a NST, an ultrasound, and a parameter which is
given
1. 10 is perfect
2. 8-10 is normal
3. <6 repeat or >36 weeks deliver baby
4. 0-2 Certain asphaxia; test for 120 min-persistent score, <4
deliver regardless of gestational age.
ii. Explain that the BPP is an US procedure and has an NST component
to it.
iii. The 5 parameters of fetal wellbeing are:
1. FHR
2. fetal breathing movements
3. gross fetal movements4. fetal muscle tone
5. amniotic fluid volume (fetus swallows 1L/day)
19. NST procedure what to do when you are monitoring and there is no fetal movement
what is your next steps (primary step)?
a. Feed the patient and give some fluids to accelerate the metabolism and wake
up the baby to establish fetal movement.
b. If doesn’t work, then reposition mom (left lateral side)
c. Reposition monitors
d. Vibroacoustic stimulators (not in use anymore because it is not healthy to
startle the fetus with this tool.)
20. Describe each of the stages of labor & and the nursing care associated with each of
the four stages.
a. First Stage: (Dilation & Effacement)
i. Begins with dilation of the cervix
ii. Ends with 10cm dilated and 100% effaced
iii. Assist with the comfort of the patient, supportive measures, education,
and hygiene.
b. Second Stage: (Delivery of Infant)
i. Begins with the patient being 10cm dilation and 100% effacement
ii. Ends with delivery of infant.
iii. Contractions may diminish or slow down but are still powerful.
iv. “The baby is coming” “I have to push.”
v. Nulliparous: @ 50-60 min (w/o epidural), @ 80 min (w/epidural)
vi. Mutliparas: @ 15-20 min (w/o epidural), @ 45 min (w/epidural)
vii. Assist with delivery, assessment of potential complications, assist with
infant bonding, breastfeeding, and hygiene.
c. Third Stage: (Delivery of the Placenta)
i. Begins with the delivery of the infant
ii. Ends with the expulsion of the placenta
iii. Is the shortest age: lasts 6 min, can go up to 30 min
iv. Normal separation there will be a “gush of blood” rise of uterus in the
abdomen, firmer uterus, lengthening and descent of the uterus.
v. There is no difference in time between nulliparous and multiparous.
vi. Pain with assist with breastfeeding and bonding, complications, and
hygiene.
d. Fourth Stage: (Recovery)
i. Recovery of the delivery
ii. Begins after delivery of the placenta
iii. Ends @ 4 hours placental delivery
iv. RN assesses fundal height/firmness, complicationsv. Vaginal bleeding (boggy fundus)
vi. VS & pain
vii. Bladder distention (deviated fundus)
viii. LOC
21. Be able to understand what and where various stations are located. The role of
cervical dilation and how it progresses (1-10)
a. Dilation: opening of the cervix from 0-10 centimeters.
b. Effacement: is the thinning of the cervix from 0-100%
c. Station: baby descending above, on, or below the ischial spines of the pelvis,
this tells us where the baby is sitting at.
i. Negative inside pelvis
ii. 0 is at ischial spines
iii. Positive is outside pelvis
22. Complete a drug card for each of the following medications: nursing implications &
side effects. Pitocin, Terbutaline, Folic Acid
23. Describe the nursing care of the patient receiving an epidural; possible side effects,
and nursing management.
a. Placed by an anesthesiologist or CRNA
b. Lasts longer than a spinal
c. (Duramorph, Ropivacaine) is injected into the epidural space and then the
patient can control the amount of pain medication when injecting.
d. S/S: HYPOTENSION!!!, bladder distention, prolonged delivery of baby,
catheter mitigation, C-section, fever, headache, pruritus, N&V, heaviness in
the legs
e. Explanation of the procedure, VS, bladder distention, assist with positioning
& repositioning, instruct the feeling of numbness may last several hours after
post-delivery.
24. Describe nonpharmacological pain management- effleurage, guided imagery,
hypnosis, distraction, counter pressure,
a. Effleurage: form of massage that uses the palm of the hand in a circular
motion.
b. Guided imagery: the use of words and music to evoke imaginary scenarios in
a subject with a view to bringing about a beneficial effect.
c. Hypnosis: induction to a state of consciousness highly responsive to
suggestion
d. Distraction: aromatherapy, breathing, mediation, prayer
e. Counter pressure: pressure in the location of pain.
25. What are vaginal assisted deliveries? (Forceps vs Vacuum) what are the
contraindications?
a. Vaccum: assisted-device via a suction mechanismb. Performed by an MD or CNM for both maternal and fetal indications:
i. Maternal exhaustion or inability to push any longer
ii. Fetal strip failure to rotate or descend placental separation
c. Contraindications: Fetal distress, high fetal station, disproportions
d. Risk factors: hematomas, trauma
e. Nursing Considerations: responsible for the on and off suction
f. Mom: bright red bleeding, edema, other tears
g. Baby: hematoma, cuts, swelling
h. Apply ICE PACKS, MONITOR
i. Forceps: like salad tongs
i. Fetal: placental separation, respiratory and cardiac issues, inability of
the mother to push, and strip failure.
ii. Contraindications: fetal distress, high fetal station, disproportion, no
face presentations, head down preferred
iii. Risks: trauma, laceration hematomas
iv. Nursing Considerations: Post delivery assess for trauma
1. Mom: bright red bleeding, edema, other tears
2. Baby: hematomas, cuts, swelling
3. APPLY ICE PACKS, MONITOR
26. Criteria for a labor to be induced? Bishop Score? Gestational Age?
a. 39 weeks of gestation
required
b. Medical Indication:
i. Infection
ii. Growth restriction
iii. Diabetes
iv. PIH
v. Fetal death
vi. Placental insufficiency
vii. <5 not favorable
viii. 6> favorable
ix.
27. What is the nursing care associated with augmentation of labor with Pitocin?
a. Explain the procedure
b. IV Pitocin 10 units in 1000 mL of LR starts at 1 mu/mL then progress until
contraction pattern is established
c. Monitor fetal heart rate & contractions q 15 minutes
i. UC: frequency, duration, strength
ii. HR: monitor for signs of distressd. Discuss plan for pain control
e. I & O
f. Keep MD updated on progress
g. Prepare for delivery
h. Support measures
28. What is the pre and post nursing care with an Amniotomy, what is the primary focus
post amniotomy?
a. Amniotomy: artificial rupture of the membranes
b. Typically performed during inductions, augmentations, and internal
monitoring.
c. Nursing Considerations: Assess color of fluid (clear vs. meconium; green),
amount of fluid (polyhydramnios & oligohydramnios)
d. ALWAYS assess Fetal heart tones before, during, and after the procedure to
ensure there is no prolapse cord.
e. Patient at risk for infection post rupture
f. Pre-procedure
i. Obtain baseline fetal heart tones
ii. Place multiple pads under the patient
iii. Assist MD with sterilization (sterile gloves, amnihook, or fingercot,
lubricant)
g. Post-procedure
i. Identify complications by monitoring fetal heart tones
ii. Clean patient up post procedure
29. Describe non-stress test (NST) vs. Contraction stress test (CST) on the pregnant
patient?
a. NST is a noninvasive just utilized fetal monitors to evaluate the fetus that is
not under any stress (no contractions)
b. CST is invasive if there is a need to start IV Pitocin this also utilizes the fetal
monitor to evaluate the fetus but it places the fetus under stress because there
are contractions associated with this type of test.
30. Describe the assessment of the fetus during labor and delivery?
a. Fetal assessment is performed through fetal monitoring
b. Looking for baseline fetal heart rate and fluctuations in that heart rate that will
tell the provider potential issues that may be going on.
c. Accelerations
d. Variability yes or no? How much?
e. Declarations what type?
31. Describe the various patterns of uterine contractions and fetal heart rate in
relationship to the fetal monitor. Be able to identify appropriate interventions for each
(if needed) of the types of decelerations.a. Baseline
i. Fetal Heart rate typically is around 110-160
b. Variables
i. Fluctuations in the baseline of the FHR within a 10-minute window
ii. Significant part of the FHR assessment because it shows adequate
oxygenation & evaluates the nervous system of the fetus.
iii. Causes: may be decreased like fetal sleep (narcotics), alcohol, drugs,
fetal sepsis, fetal tachycardia, prematurity, fetal anomalies, hypoxia,
maternal hypoxia
iv. Classified as:
1. Absent: undetectable
2. Minimal: Undetectable to <5bpm
3. Moderate: 6-25 bpm
4. Marked: >25bpm
c. Accelerations
i. An abrupt temporary increase in the FHR that should peak 15 beats per
minute x 15 seconds after 32 weeks, prior to 32 weeks is 10 beats per
minute x 10 seconds.
d. Decelerations
i. A decrease in the FHR below the normal range or the established
baseline
ii. Types
1. Early: occurs during a contraction, is okay, have a gradual
decrease, MIRROR contractions, not associated with fetal
compromise
2. Late: nonreassuring pattern caused by uteroplacental
insufficiency
a. Gradual but uniformed with a decrease in FHR that
begins mid contraction with a baseline return after the
contraction is over.
b. Can be intermittent, persistent, subtle, or prolonged
32. Describe the difference between external vs. internal (ISE/IUPC) monitoring. When
is an ISE/IUPC contraindicated?
a. External: monitors are applied on the outside of the mother via the US and
the TOCO.
b. Internal: monitors applied on the inside of the mother via the Internal (Fetal)
scalp electrode (ISE) and Intrauterine pressure catheter (IUPC), the fluid is
broken and has access to the baby’s head where the electrode is applied.
c. Contraindications:
i. Hepatitisii. Infection
iii. Herpes
iv. HIV
v. Structural abnormalities
vi. Prolapse cord
33. Identify what issues may occur that lead a patient to receiving a cesarean birth.
a. It is a safe surgical procedure.
i. Risks
1. Infection
2. Hemorrhage
3. Urinary tract trauma
4. Ileus
5. Deep vein thrombosis
6. Aesthesia complications
7. Fetal risks injury (lacerations, bruising, fractures) transient
tachypnea
b. Types of incisions
i. Classical (quick to perform easier visualization of the uterus; easier for
obese women)
ii. Low Transverse/Pfannenstiel (unlikely to rupture with other
pregnancies, less blood loss, easy to repair, less adhesion formation
c. Reason for a C-section
i. Fetal distress
ii. Prolapsed cord
iii. Fetal presentation
iv. ROM (Rupture of Membranes) over 24 hours
v. Failed VBAC attempt (Previous uterine incision must be low
transverse (need medical record of previous surgery.)
vi. Classical C/S (Caesarean section) incision history
vii. Active Herpes, HPV, Acute HIV +
viii. Placenta Previa or Placenta abruption
d. Nursing Considerations
i. Emotional Support
ii. Education pre and post procedure
iii. Promotion of safety (food intake, ambulation)
iv. Post-operative care
v. Monitor for complications
34. Responsibilities of nurse to prepare a patient for surgery.
a. Emotional support
b. Education pre and post-surgeryc. Promotion of safety (food intake, ambulation)
d. Post-operative care
e. SCD’s
f. Foley
35. Pt teaching regarding gestational diabetes- treatment, blood sugar monitoring, diet,
fetal monitoring
a. It is a carbohydrate intolerance of any variable severity that develops or
recognized during pregnancy.
b. Places patient at higher risk to develop type 2 diabetes onwards.
c. Risk Factors
i. Overweight
ii. Over the age of 25
iii. Previous birth outcome: neonatal macrosomia, maternal HTN,
unexplained congenital anomalies, previous fetal death
iv. GDM in previous Pregnancy
v. Family history
d. Perform Screenings
i. Glucose Challenge test
1. Done in 24 to 28th week of gestation
2. Low or high risk moms
3. No prep, not NPO
4. An oral glucose is ingested & blood work is taken 1 hour later
5. Blood serum glucose greater than 140 is considered positive &
a 3-hour glucose intolerance test is required.
ii. GDM is diagnosed when:
1. Fasting >95mg/dL
2. 1 hour >180mg/dL
3. 2 hours >155mg/dL
4. 3 hours >140mg/dL
iii. Management
1. Goal is to maintain normal glucose levels through exercise,
diet, and may need insulin for glucose control.
2. May have increased episodes of hyper/hypo-glycemia due to
change of metabolic needs during pregnancy.
3. Diet: 30 kcal/kg/day is recommended generally, or 25
kcal/kg/day is for an obese person, with a smaller % of
carbohydrate intake
4. Exercise: a graduated exercise plan5. Blood glucose monitoring: if there are repeated results
reflecting fasting (>95%) & postprandial (2 hours after food)
(>120)- insulin may be required
6. Fetal surveillance
a. Kick counts
b. NST
c. BPP
d. US
e. Fetal growth
36. Missed Quiz Concepts
a. What is a fundus?
i. The top of the uterus
b. What is Linea nigra?
i. A dark pigmented line from the fundus of the uterus to the pubic
symphysis.
c. What weeks is the glucose intolerance test performed?
i. 24 to 28 weeks
ii. Diagnosis hyperglycemia >140 mg/dL
d. Name Three Breech positions?
i. Frank, Complete, Footling
e. What are the four stages of labor?
i. 1st: Cervical dilation
ii. 2nd: Delivery of the baby
iii. 3rd: Delivery of the placenta
iv. 4th: Recovery Stage
f. Amniocentesis is performed?
i. 15-20 weeks
g. Quad Screening is performed?
i. 16-18 weeks of gestation
h. What is a version?
i. Ultrasound guided procedure performed ion 36 to 37 weeks of
gestation to externally manipulate the fetus into a cephalic lie.
ii. A fetus in a breech or transverse position >36 wk
[Show More]