*NURSING > STUDY GUIDE > NURSING NUR2115 Nutrition ATI Study Guide NUTRITON FOR NURSING EDITION 5.0 REVIEW MODULE STUDY MANUA (All)
NURSING NUR2115 Nutrition ATI Study Guide NUTRITON FOR NURSING EDITION 5.0 REVIEW MODULE STUDY MANUAL
Document Content and Description Below
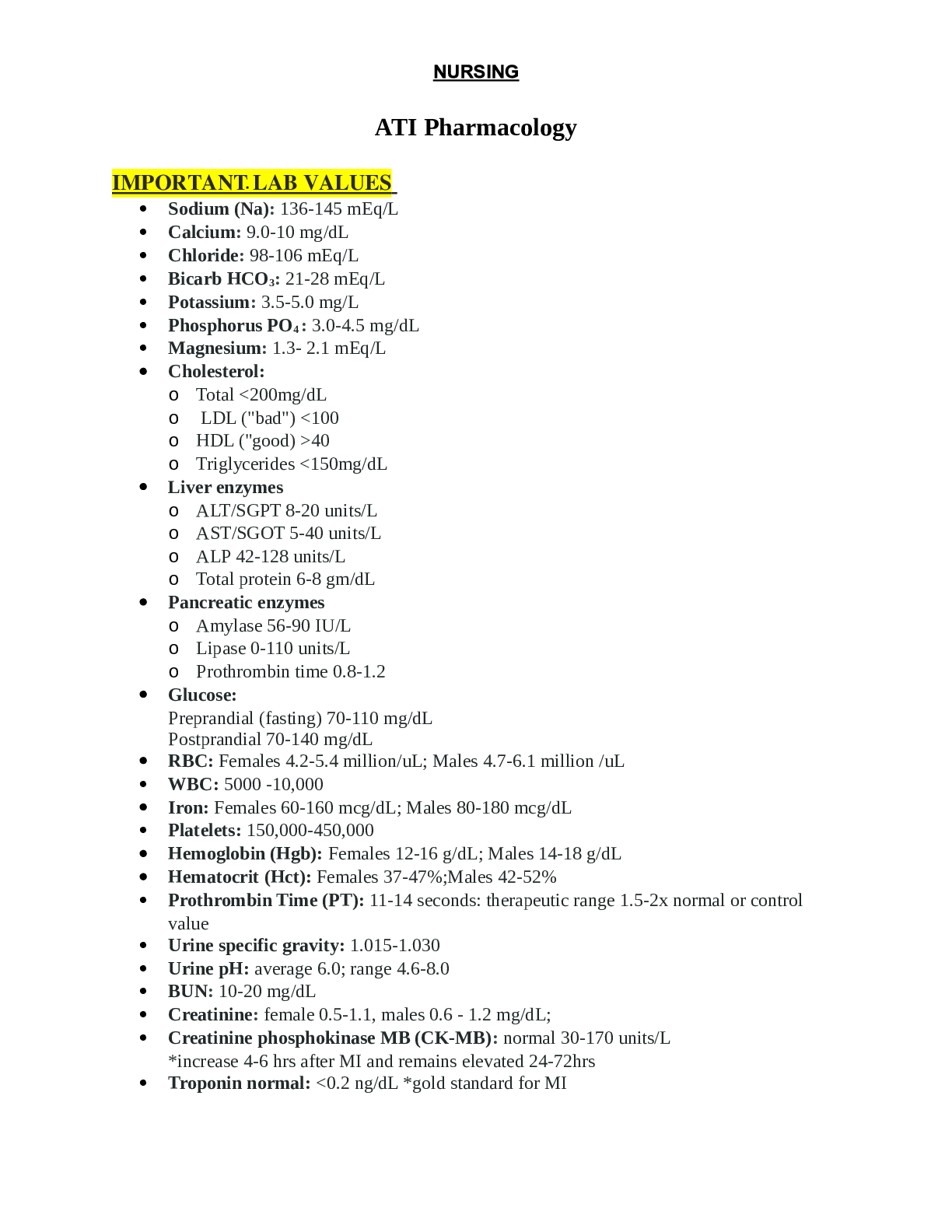
NURSING NUR2115 Nutrition ATI Study Guide NUTRITON FOR NURSING EDITION 5.0 REVIEW MODULE STUDY MANUAL Complete proteins: animals Incomplete proteins: plants Vitamin C citrus fruits, tomatoes... , peppers, green leafy veggies Folate liver, green leafy veggies, grains, legumes Vitamin D sun, milk, eggs Vitamin A fish liver oils, dark yellow/orange fruits/veggies Vitamin E veggie oils, grains, nuts, dark green veggies Vitamin K eggs, liver, green leafy veggies Sodium table salt, added salts, processed foods, butter Potassium oranges, tomatoes, avocados, bananas, broccoli Calcium dairy, broccoli, kale, grains, egg yolks Magnesium green leafy veggies, nuts, grains, milk, meats B6 anemia Folate megaloblastic anemia (pallor, weakness, palpitations, dyspnea, fatigue) B12 pernicious anemia (anorexia, indigestion, weight loss, diarrhea/constipation, paresthesia, decreased proprioception, poor muscle coordination, increased irritability, delirium) Vitamin A decreased vision, dry eyesVitamin D fragile bones Vitamin E hemolytic anemia Vitamin K increased bleeding time Prolonged stress, rapid growth periods, pregnancy, lactation, physical conditioning INCREASE metabolic rate Fever, involuntary muscle tremors, hyperthyroidism, cancer, cardiac failure, some anemias, hypertension, COPD INCREASE metabolic rate Burns, surgery/wound healing, HIV/AIDS INCREASE metabolic rate Somatotropin, prednisone, hydrocortisone, epinephrine, levothyroxine, glucagon, ephedrine INCREASE metabolic rate Amitriptyline DECREASES metabolic rate >60 yrs old, hypothyroidism, short/overweight, starvation/malnutrition DECREASES metabolic rate Normal BMI 18.5-24.9 Overweight BMI 25-29.9 Obese BMI greater/equal to 30 Protein measured by serum albumin Prealbumin measures malnutrition Increase consumption fiber rich fruits/veggies to 5 servings/day Choose monounsaturated/polyunsaturated fats from fish, meats, nuts, veggie oils (30% daily calories) Consume less than 2300 mg salt/day Limit saturated fats to 10% calories and cholesterol 300 mg/day Elevated LDL increase monounsaturated fats and soluble fiber Adequate fluid intake and 25 g fiber/day (women), 38 g/day (men)Reduce cancer increase high fiber plant based foods, limit saturated/polyunsaturated fat, increase monounsaturated fat or omega 3 fatty acids (nuts/fish), exercise regularly, avoid excess alcohol, limit sodium intake Foods high in vit K can decrease effects of anticoagulants like warfarin Foods high in proteins/amino acids/vit b6 increase metabolism for antiparkinsonism meds Licorice can cause hyperkalemia in those taking digoxin, ACE inhibitors, beta blockers, MAOIs, calcium channel blockers, spironolactone Tyramine increases risk for hypertensive crisis in those taking MAOIs, found in aged cheeses, red wines, smoked/pickled meats African americans higher in fats/proteins/sodium, lacking in potassium/calcium/fiber Asian americans high sodium intake Latino americans increased risk for TII diabetes, substantial weight gains 2,000-3,000 mL/day Pregnancy gain 25-35 lbs, protein=20% daily intake, fat=limited to 30% daily intake, carbohydrates=50% daily intake Protein=71 g/day Vitamin A=770 mcg/day Vitamin D=15 mcg/day Vitamin C=85 mg/day Vitamin K=90 mcg/day Vitamin E=15 mcg/day Folate= 600 mcg/day Calcium=1000 mg/day Iron=27 mg/dayLactating increase daily caloric intake Protein=71 g/day Vitamin A=1300 mcg/day Vitamin D=15 mcg/day Vitamin E=19 mcg/day Vitamin K=90 mcg/day Vitamin C=120 mg/day Folate=500 mcg/day Calcium=1000 mg/day Iron= 9 mg/day Nausea dry crackers/toast, avoid fats/caffeine/spices Constipation increase fluids/fiber PKU foods low in phenylalanine, avoid fish/poultry/eggs/nuts/dairy products, can cause mental retardation and behavioral problems Infancy breast milk/formula=sole source of nutrition for 4-6 months Semisolid food introduced at 4 months AVOID cow’s milk until after year 1 Offered breast immediately after birth, feeding 8-12 times in 24 hours, nursing 15- 20 minutes on 1st breast, feed every 4 hours Breast milk okay in fridge for 10 days, 6 months in freezer, don’t microwave breastmilk, don’t refreeze thawed milk Offer iron-fortified rice cereal 1st, introduce new foods once at a time for 4-5 days, delaying introduction of milk/eggs/ wheat/citrus fruits AVOID peanut butter/peanuts/honey Childhood (1-3) avoid foods like hot dogs/popcorn/peanuts/grapes/raw carrots/celery/ peanut butter/tough meats/candyLimit juice to 4-6 oz/day Provide whole milk Food serving size=1 TBSP/year of age Increased risk for choking until age 4 Iron deficiency anemia CONSUME VITAMIN C to enhance IRON ABSORPTION Limit milk to 24 oz VITAMIN D enhances CALCIUM ABSORPTION Preschoolers (4-6) 13-19 g/day complete protein Switch to low fat/skim milk after age 2 Iron deficiency anemia Adolescence 2000 cal/day (female), 4000 cal/day (male) Females require 15 g/day iron, males require 11 g/day iron 1300 mg/day calcium Adulthood/older adults 40%-55% carbohydrates, 10%-20% fat Reduce daily caloric intake, exercise regularly, and dehydration common Decreased absorption of b12, folic acid, calcium Hypertension Decreased renal function (potassium/sodium imbalances) 2000 cal/day=51+ men, 1600 cal/day=51+ women Clear liquid diet clear/liquid at room temp, water/carbohydrates, used for acute illness, reduction colon fecal material prior to diagnostic testing, acute GI disorders, post-op recoveryWater, tea, coffee, fat free broth, carbonated beverages, clear juices, ginger ale, gelatin Full liquid diet liquid at room temp, used for transition from liquid to soft diets, post-op recovery, acute gastritis, febrile conditions, solid food intolerance, CONTRAINDICATED FOR lactose intolerance or hypercholesterolemia All milk, soups, strained fruits/veggies, veggie/fruit juices, eggnog, ice cream/sherbet, refined/strained cereals, puddings Soft (bland, low fiber) diet whole foods low in fiber, lightly seasoned, easily digested, used for transition between full liquid and regular diets, acute infections, chewing difficulties, or GI disorders Fruits/veggies, coarse breads/cereals, beans excluded Mechanical soft diet require minimal chewing before swallowing, used for those with limited chewing abilities (dysphagia, poorly fitting dentures, no teeth, head/neck/mouth surgery, intestinal sutures Transnasal tubes (3-4 weeks) Gastrostomy (PEG tubes) inserted into stomach, tolerated well Standard formulas “polymeric” “intact” composed of whole proteins, require functional GI tract Hydrolyzed formulas “elemental” composed of partially digested protein peptides aka free amino acids, used for those with partially functioning GI tracts, or those with IBD, cystic fibrosis, or pancreatic disorders BOLUS FEEDINGS may cause DUMPING SYNDROME diaphoresis, dizziness, rapid pulse, pallor, light headedness Elevate head of bed at least 30 degrees during feedings, remain there for 30-60 minutes after feedings PN used when GI tract isn’t functioning or when they can’t physically or psychologically consume sufficient amounts of nutrients TPN amino acids, dextrose, electrolytes, vitamins, trace elements, used for those undergoing cancer treatment, bowel disorders, trauma/burnsAnemia fatigue, lethargy, nail bed pallor, cold intolerance Diarrhea/malabsorption syndromes low fiber diets (low residue foods), high fiber diets if fiber not causing diarrhea Nausea/vomiting easy to digest/ low fat carb foods Elevate HOB, avoid liquids with meals, good oral hygiene, avoid hot/spicy foods, eat room temp/cold foods, avoid high fat foods Anorexia decrease stress at meal times, assess for effects of meds, administer meds to stimulate appetite, assess/modify environment for unpleasant odors, remove items causing decreased appetite, assess/manage anxiety/depression, provide small/frequent meals avoiding high fat foods, provide liquid supplements Constipation exercise, increase fiber/fluids, assess elimination patterns, avoid laxative use chronically Dysphagia modify textures/consistency of foods/liquids, place in upright position to eat, provide oral care, allow adequate time for meals Dumping syndrome small/frequent meals, fat/protein each meal, avoid concentrated sugars/lactose, consume liquids 1 hr before eating or after eating, lie down after meals GERD avoid situations leading to increased abdominal pressure, avoid eating 2 hr before laying down, elevate body on pillows, weight loss, avoid trigger foods (citrus fruits/juices, spicy foods, carbonated beverages), avoid items that reduce lower esophageal sphincter pressure (fatty foods, caffeine, chocolate, alcohol, nicotine, peppermint/spearmint) Heartburn, painful swallowing, dyspepsia, regurgitation, coughing, hoarsness, epigastric pain Gastritis avoid eating frequent meals/snacks, avoid alcohol/nicotine, aspirin, NSAIDs, coffee, spicy foods, monitor for vitamin deficiencies Abdominal pain/discomfort, headache, lassitude, nausea, anorexia, hiccupping, heartburn, belching, sour taste in mouth, vomiting, bleeding, hematemesis PUD avoid frequent meals/snacks, avoid coffee, alcohol, caffeine, aspirin, NSAIDs, spicy foods, nicotineDull, gnawing pain, burning sensation, heartburn, constipation/diarrhea, sour taste in mouth, burping, nausea, vomiting, bloating, urea in breath, tarry stools Lactose intolerance avoid/limit intake of lactose, monitor for vitamin D and calcium deficiencies Abdominal distension, cramps, flatus, diarrhea Ileostomies/colostomies consume diet high in fluids/fiber, avoid foods that cause gas (beans, eggs, carbonated beverages), avoid foods that cause stomal blockage (nuts, raw carrots, popcorn), or foods that produce odor (eggs, fish, garlic), increase caloric intake/protein Diverticulosis/diverticulitis high fiber diet, avoid foods with seeds/husks Abdominal, pain, nausea, vomiting, constipation/diarrhea, fever, chills, tachycardia IBD crohn’s disease, ulcerative colitis, low residue/high protein & protein, vitamin/mineral supplementation, avoid nicotine and substances that cause diarrhea Nausea, vomiting, abdominal cramps, fever, fatigue, anorexia, weight loss, steatorrhea Cholecystitis (gall bladder inflammation) reduce fat intake, avoid coffee, broccoli, cauliflower, Brussel sprouts, cabbage, onions, legumes, highly seasoned foods Pancreatitis NPO, NG tube placement, low fat, high protein & carbohydrate diet/supplementation Pain, tenderness, rigidity of RUQ Liver disease increase protein, increased calories, supplementation, eliminate alcohol, nicotine, and caffeine Celiac disease eat gluten free foods, read labels Diarrhea, steatorrhea, anemia, abdominal distension, impaired growth, lack of appetite, fatigue, bloating, osteomalacia Coronary heart disease low fat & cholesterol diet, reduce cholesterol intake to 200 mg/day, conservative use of red wine, increase fiber/carb intake, avoidsaturated fats, decrease red meat intake, increase consumption of omega 3 fatty acids, exercise regularly, avoid tobacco use Lower cholesterol by trimming fat from foods, consume lean meats, remove skin, broil/bake/grill/steam foods, low fat/skim milk/cheese/ yogurt, use spices in place of butter/salt, avoid trans fat, read labels Hypertension BP greater than 140/90 DASH diet low sodium, high potassium/calcium diet used to lower BP, low fat dairy products Decrease sodium to less than 2400 mg/day Heart failure reduce sodium to 2000 mg/day or less, monitor fluid intake MI avoid caffeine, liquid diet is recommended at first, small frequent meals Pre stage CKD increase serum creatinine, fatigue, back pain, appetite changes Control glucose/hypertension, preserve remaining function, restrict phosphorus, carefully determine protein intake, restrict sodium End stage CKD fatigue, decreased alertness, anemia, decreased urination, headache, weight loss High protein, low phosphorus & potassium & sodium diet, fluid restriction, vitamin D/calcium concern imbalance Acute kidney injury decrease in urination, decreased sensation in extremities, swelling of lower extremities, flank pain, rising blood levels of urea/other wastes Potassium/sodium/calcium restriction, fluid restriction Nephrotic syndrome edema, high proteinuria, hypoalbuminemia, hyperlipidemia, hypercoagulation Minimize edema, replace lost nutrients, minimize renal damage, control hypertension, prevent protein malnutrition, low sodium diet, protein intake monitored, increase carbs, limit trans fat/cholesterol, supplementation Kidney stones diaphoresis, N/V, blood in urine Increase fluids, limit calcium/oxalates, limit purine foods ALL RENAL CONSIDERATIONSMonitor weight daily, monitor fluid intake, monitor urine output, monitor for constipation Type 1 diabetes autoimmune triggered by genetics or virus, absence of insulin production, under age 30 Type 2 diabetes genetic/environmental factors, insulin resistance, over age 40 Hypoglycemia too much insulin, inadequate food intake, delayed or skipped meals, extra physical activity, alcohol consumption without food, glucose less than 70 Shakiness, confusion, sweating, palpitations, headache, lack of coordination, blurred vision, seizures, coma Take glucose tablets, candies, juice/soda, honey Hyperglycemia imbalance among good, meds, activity Glucose over 250, ketones in urine, polydipsia (thirsty), polyuria (urination), polyphagia (hunger), hyperventilation (kussmall respirations), dehydration, fruity odor in breath, headache, decreased LOC, seizures, coma [Show More]
Last updated: 2 years ago
Preview 1 out of 10 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$7.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Mar 18, 2021
Number of pages
10
Written in
Additional information
This document has been written for:
Uploaded
Mar 18, 2021
Downloads
0
Views
68