*NURSING > Study Notes > NSG 307 Exam 2 Study Guide >Marian University - NSG 307 | RATED A (All)
NSG 307 Exam 2 Study Guide >Marian University - NSG 307 | RATED A
Document Content and Description Below
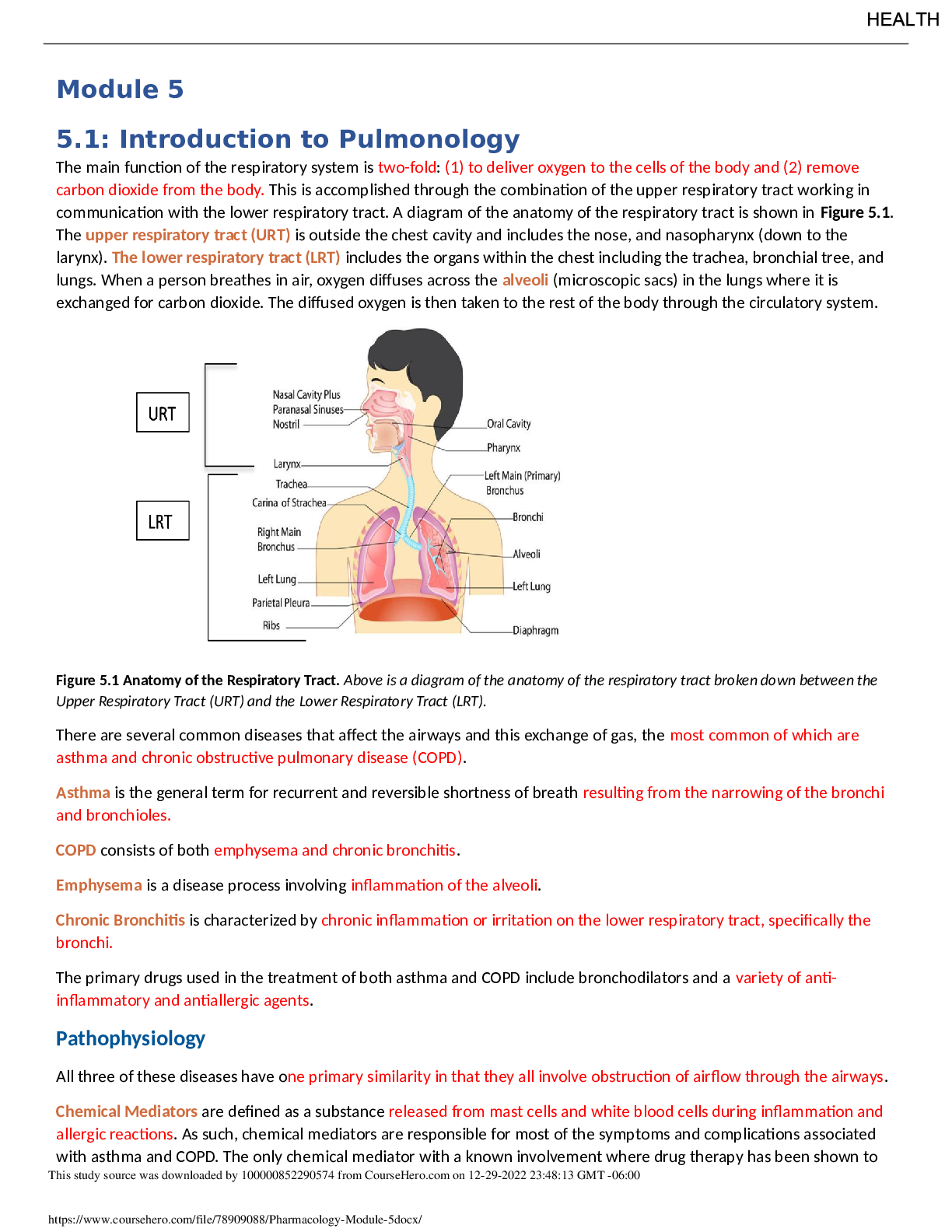
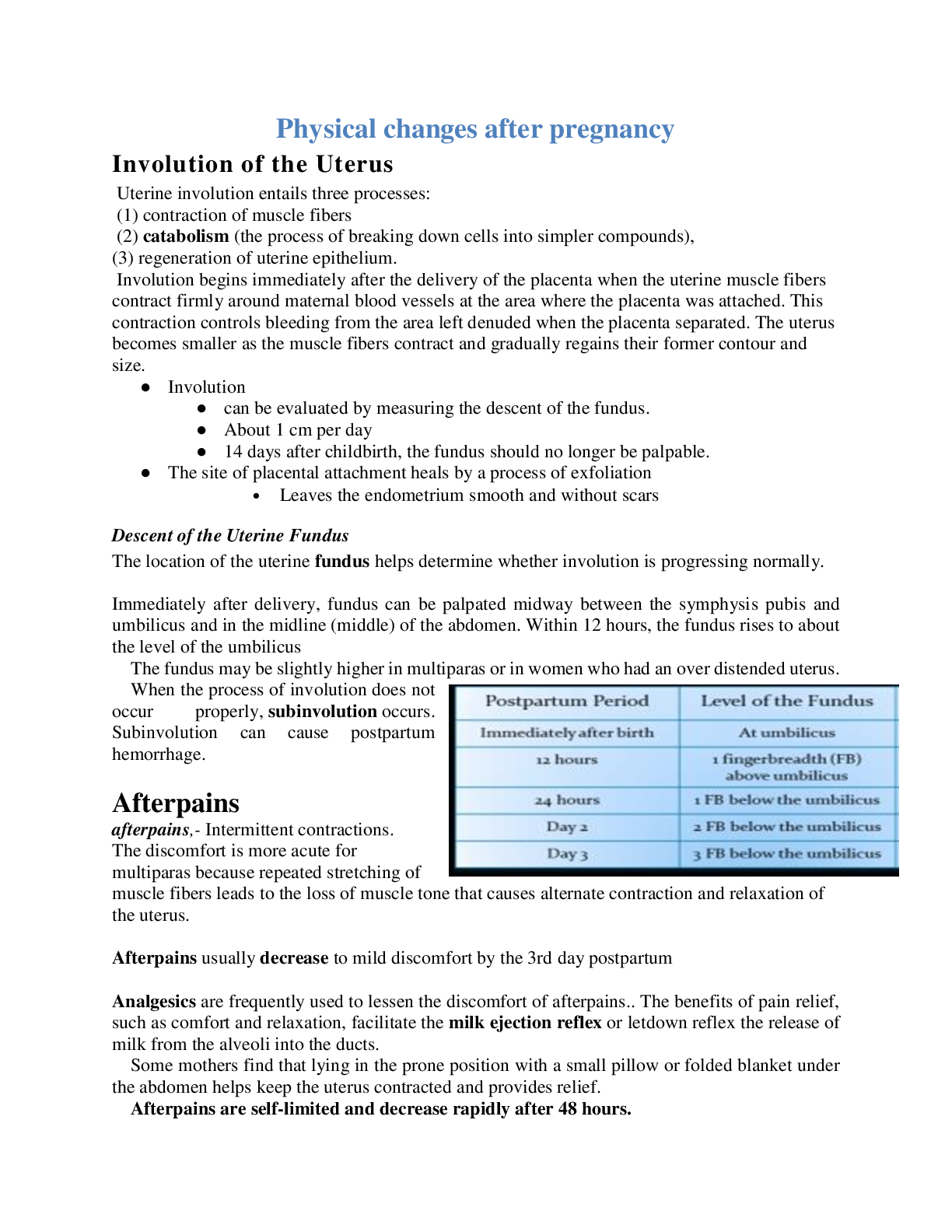
Ch 13 NSG 307 Care of the Childbearing Client Exam 2 Study Guide • Stages and phases of labor o 1st stage: onset of contractions – full cervical dilation ▪ Latent phase: labor onset to... active phase (longest phase of 1st stage) ▪ Active phase: 6-10 cm (rotate from resting upright) o 2nd stage: full cervical dilation (10 cm) until birth of baby o 3rd stage: birth of baby until placenta delivery o 4th stage: delivery of placenta until about 2 hours of recovery • 5 P’s of labor o Passenger: fetus – Fetal head: sutures & fontanels >> fetal presentation & position – Preferred attitude is “flexed” where the head is flexed into the chest w/ fetal back rounded with the arms and legs flexed in front of the fetus o Passageway: birth canal – relaxin: hormone to relax muscles of bony pelvis, preparing pelvis to receive & pass the baby through birth canal o Powers: Primary (frequency, duration, intensity, effacement (thinning of cervix – 0-100%), dilation (opening of cervix <1 cm-10cm), Ferguson reflex (urge to bear down)—Secondary (bearing down efforts delayed pushing o Position of laboring woman: upright, “all fours”, lithotomy, semirecumbent, lateral o Psychologic response “psyche” • Fetal Presentations: cephalic (LOA or LOT or ROA or ROT or LOA or LOP), breech (butt 1st), shoulder o Station: Ischial spines >> 0 station (above – number, below + number) o Engagement: largest diameter of fetal head in inlet – usually 0 station presenting part that no longer ballots out of the pelvis & has entered maternal pelvic brim & into the true pelvis & corresponds to “zero” station • Signs Preceding Labor o Lightening (1st time mothers: few weeks before)—bloody show/mucus plug—Stronger Braxton-Hicks – Surge of energy “nesting”—Cervical ripening (cervix positioned anterior & easier to reach soft, begins to dilate & efface) • Physiologic adaptations to Labor o Onset of labor= inc. uterine distention, aging of placenta, inc. estrogen & prostaglandins, dec. progesterone o Fetal adaptation: FHR= 110-160 (responds to how well oxygenated fetus is) ▪ Fetal circulation: affected by maternal position, contractions, BP, umbilical cord BF ▪ Preparation for fetal respirations: lung fluid clears through labor & vaginal birth dec. PO2, inc. PCO, dec. pH, dec. HCO3 ▪ PREVENT NEURO ISSUES DUE TO INADEQUATE FETAL OXYGENATION o Maternal adaptation: ▪ Cardiovascular: during contractions (blood shunting) peripheral resistance & BP inc. (check BP between contractions)– possible supine hypotension (remain off back & more side lying) – WBC inc. ▪ Respiratory: inc. O2 consumption with inc. activity & anxiety – Hyperventilation respiratory alkalosis, hypoxia, & dec. CO2 ▪ Renal: drink & urinate q1h to keep lower abdominal area more comfortable – Voiding difficulties & proteinuria ▪ Integumentary: perineal stretching ▪ Musculoskeletal: inc. muscle activity (leg cramps do NOT point toes) ▪ Neurologic: euphoria, serious, amnesia, elation/fatigue, endogenous endorphins ▪ GI: dec. GI motility, stomach-emptying time dec. & N/V Ch 14 ▪ Endocrine: dec. progesterone, inc. estrogen & metabolic rate, dec. glucose • Gate-control theory: pain sensations travel along the sensory nerve pathways up the spinal cord & to the brain, but only a limited # of sensations can travel these pathways at a time. By stimulating the nerves to transmit message, pressure, heat & cold, water therapy, positioning, helps to close the hypoethical gate of pain transmission along those same fibers. • Nonpharmacologic methods of pain management: knowledge & information— Lamaze/Psychoprophylactic method—Bradley: Husband-Coach Childbirth o Relaxation & breathing techniques: Focusing & relaxation (Imagery) o Effleurage & counterpressure—Touch & massage/therapeutic touch—Heat & cold— Acupressure & acupuncture—TENS unit—water therapy (hydrotherapy)—Intradermal water block • Systemic analgesia: IV/PCA/IM dose: provide sedation, euphoria, & rest—cross placenta (smallest dose is GOAL) & newborn effects (FHR, fetal sleep pattern, respiratory depression use more during early labor and not as labor is advancing) • Opioid agonists: No amnesic effect but create feeling of well-being or euphoria to enhance woman’s ability to rest between contractions—should be administered until labor is well established o Meperidine (Demerol): crosses placenta & cause prolonged neonatal sedation & neurobehavioral changes CANNOT BE REVERSED BY NALOXONE, Fentanyl (Sublimaze): rapidly crosses placenta so is present in fetal blood w/in 1 min., Remifentanil (Ultiva): OA is 1 min. & crosses placenta but metabolized quickly by fetus so no neonatal depression (PCA pump only)—RESPIRATORY MONITORING: hypoventilation & oxygen desaturations • Opioid agonist-antagonist: Nalbuphine (Nubain)—abstinence syndrome if opioid dependent & NO respiratory depression in newborn • Opioid antagonists: Naloxone (Narcan)—antidote for narcotic OD—CONTRA: opioid-dependent women—can cause excessive CNS depression in mother & newborn • Epidurals and spinals including nursing care o Local infiltration: given into perineal area (given just before birth for episiotomy & repair of laceration & Lidocaine) o Pudendal block: transvaginal injection to pudendal nerve – use end of 2nd & 3rd stages—provides broader area of pain relief can provide relief for a forceps delivery or vacuum assisted delivery o Spinal anesthesia: Bupivacaine, lidocaine – c/s births requires 500-1000 pre-hydration bolus w/o dextrose ▪ Advantages: no catheter placed for future dosing ▪ Disadvantages: hypotension (place on side wedge & IV bolus fluids), total spinal block, postdural puncture headache • Loss of sensations of contractions or urge to bear down during vaginal birth, use of vacuum extraction or episiotomy, full bladder = bladder distention, CSF may leak from puncture causing shift in brain & intense HA Epidural blood patch ▪ Nursing implications: sterile technique on insertion monitor for hypotension & has BP checked frequently o Epidural anesthesia: Used for vaginal birth or unplanned c/s: Bupivacaine, ropivacaine, or opioids (fentanyl) or both L4 or L5 ▪ Advantages: pain relief at all stages ▪ Disadvantages: hypotension, Dural puncture w/ resulting HA, bladder distention, prolonged 2nd stage ▪ Pre-hydration bolus, ephedrine ▪ CONTRAS: maternal hypotension, coagulopathy, infection at needle site, inc. ICP, allergies, maternal refusal, maternal cardiac conditions o General anesthesia: emergency situations or contraindications to nerve block anesthesia agents: Propofol, succinylcholine, isoflurane ▪ Nursing implications: NPO, sodium citrate (dec. acid out of stomach), uterine displacement, cricoid pressure ▪ AEs: maternal aspiration, maternal or neonatal respiratory depression, & uterine relaxation: pp hemorrhage • Effects of medications on mom and baby o Neonatal Crisis: CNS depression caused by narcotics or anesthetic agents respiratory depression, hypotonia or dec. muscle tone, unstable thermoregulating mechanism dec. alertness & responsiveness to stimuli, hard to console = may continue regardless of Narcan & may last 2-4 days Ch 15 • Factors affecting fetal oxygenation (decrease in oxygen supply) o Dec. BF through maternal vessels (hypotension or hypertension) o Dec. oxygen content in maternal blood (mom bleeding heavily or having asthmatic event) o Alteration in fetal circulation (impeded by pressure on umbilical cord or placenta separating from the uterine wall (abruption) o Dec. BF to intervillous space in placenta (tachysystole, HTN, diabetes) • What determines a normal fetal heart rate pattern: Normal FHR = 110-120 up to 160 bpm o Variability: tells us how well oxygenated out fetus is @ that time. This is the up & down or peak to trough movement of the FHR o Absent: No undulations. Sign that fetus is lacking oxygen. INTRAUTERINE RESUSCITATION o Minimal: <5 bpm amplitude range; can be normal variation if fetus is taking a nap if for longer period of time = dec. oxygenation o Moderate: 6-25 bpm amplitude range—adequately oxygenated fetus Normoxic o Marked: >25 bpm amplitude range—unspecified significance continue to monitor fetus for any signs of change in oxygenation o Tachycardia: >160 maternal infection, drugs, fetal anemia ▪ Check maternal temperature & ensure proper oxygenation minimal to absent variability re-position mom & place oxygen on a tight non-rebreather mask o Bradycardia: <110 for 10 min. fetal cardiac anomaly, viral infections ▪ Needs to differentiate from prolonged decelerations initiate intrauterine resuscitation • Fetal heart rate pattern interpretation: Early, late, variable decelerations o Early decelerations: transient fetal head compression o Late decelerations: Placental insufficiency: ▪ Turn Pitocin drip off—turn pt. on side—admin. oxygen via non-rebreather—inc. IVF to inc. maternal BP o Variable decelerations: umbilical cord compression = CHANGE MATERNAL POSITION o Prolonged decelerations: > 2 mins < 10 min o Accelerations: (15 by 15) peak > 15 beats above baseline & Duration > 15 seconds = OK • Factors affecting baseline, variability, accelerations, decelerations • Nursing interventions for abnormal fetal heart rate (FHR) patterns o Oxygen (non-rebreather face mask), lateral position, IV fluids o Interventions for specific problems: Hypotension & Tachysystole (can cause dec. fetal oxygenation because during a contraction BF to the uterus dec. or has a stais) by dec. amount of contractions, it will naturally allow for more O2 to be diffused through placenta (>5 contractions w/in 10 min.) • Reassuring vs non-reassuring FHR o Normal= reassuring patterns Abnormal = non-reassuring patterns Ch 16 • Assessment of laboring woman o Prenatal data: age, height, weight, OB history such as gravida/parity/bleeding/gestational HTN/DM/anemia/infections/EDD/fundal height/FHR/lab tests/previous deliveries o Interview: chief complaint: rupture of membranes (ROM) or bag of waters (BOW), onset of labor presence of bloody show, illness, allergies, last oral intake birth plan, infant feeding method, type of pain management, childbirth education, drug use o Lab workL urine, CBC (Hgb, Hct, platelets, blood type & Rh) o Assess amniotic membrane rupture Nitrazine (pH) test & Fern test (clear or meconium- stained) o s/s of potential problems: FHR, contractions, meconium-stained fluid, lack of progress, materbal fever, vaginal bleeding https://www.coursehero.com/file/81500089/NSG-307-Exam-2-Study-Guidedocx/ • True versus False Labor o True: strong & regular contractions—pelvic pain & lower back pain—mucus plug/bloody show—water breaks o False: irregular contractions relieved by re-positioning • Leopold’s Maneuvers: determine where fetus’ back is – performed using abdominal palpation • Care of the laboring woman at each stage through Stage IV o Stage I: General hygiene (showers, perineum care, oral hygiene, hair, hand washing, face, gown & linens)—Nutrient & fluid intake (oral fluids & solid foods & IV access)— Elimination (voiding q2h; ambulating to bathroom; woman on bed rest = bedpan, upright, privacy, side rails); urinary catheterization (insert catheter between contractions) o Stage II: maternal position changes can inc. the urge to push & enhance the progress— Bearing down—Birth in a delivery room or birthing room (Lithotomy position) ▪ Immediate skin-skin care & APGAR 1 & 5 min. – drying of the baby, removing wet linens & replace w/ warm/dry linens ▪ Perineal trauma: 1st (laceration that extends though skin & structures superficial to muscles) 2nd (laceration that extends through muscles of perineal body) 3rd (laceration that continues through anal sphincter muscle) 4th (laceration that extends completely through anal sphincter and rectal mucosa ▪ Vaginal (from forceps), urethral, cervical lacerations ▪ Episiotomy: incision to enlarge the vaginal outlet risks= trauma, hemorrhage, extensions, infections, bleeding, pain o Stage III: birth of baby – placental expulsion ▪ Placental separation & expulsion: uterus becomes globular in shape—lengthening of umbilical cord—inc. in vaginal bleeding—expulsion of placenta • Pitocin IV should be running @ fast rate—Hygiene—Pain relief (perineal pad)—assist in parent/infant bonding—breastfeeding & skin-skin—Assess perineum for lacerations • Q15 min. maternal BP, pulse & respirations o Stage IV: 1st 2 hours after birth ▪ Post-anesthesia recovery (assess sensory & mobility)—v/s: if bleeding BP will dec. & HR will inc—Fundus (firmness, level in relation to umbilicus)—Bladder (if distended boggy uterusresults in inc. bleeding)—Lochia (est. amount, color, odor)— Perineum (Use REEDA: redness, ecchymosis, edema, drainage, approximation) to evaluate • Vital signs: assess BP & pulse q15min. for 2 hours—Temperature assess q4h for 8h and then @ least every 8 hours Ch 18 • Maternal physiologic changes during the postpartum period o Breasts: breastfeeding mothers colostrum: yellow fluid (milk in 3-4 days) ▪ Engorgement (1-2 days): caused by a temporary inc. in blood & lymphatic fluid in the breasts ▪ Non-breastfeeding mothers: Engorgement (SHOULD NOT EXPEL)—Discomfort for 1-2 days & can use breast binder, inc, avoid stimulation • Specific system changes/adaptations o Reproductive System: initial blood loss = vaginal <500 mL & c/s < 1000 mL – Fundus descends 1-2 cm q24h ▪ Uterus: involution process begins immediately after delivery of placenta (SUBINVOLUTION is delay in involution – due to retained placental fragments & infection) Ch 19 ▪ Contractions: afterpains (multiparous women)—Placental site—Lochia (rubra/red 3-4 days, serosa/pinkish light brown 7-10 days, alba/whitish yellow to 1st menses)— Cervix—Vaginal & perineum (kegel exercises are encouraged to improve tone o Endocrine System: placental hormones (estrogen/progesterone are lowest 1 wk post-birth & hCG diminishes completely) ▪ hCS: the drop in this reverses the Diabetogenic stress of pregnancy = dec. blood glucose ▪ Prolactin: inc. when breastfeeding & dec. when bottle feeding • Breastfed women can DELAY menses due to inc. Prolactin o Urinary System: Postpartal diuresis = results from body ridding itself of tissue fluid accumulation & inc. blood volume during pregnancy—3 L or more each day for 1st 2-3 days ▪ Measure 1st 2 voids post-birth 150 mL ▪ Urinary retention can displace uterus out of midline uterine atony hemorrhage o GI System: appetite (fluid, food, clear liquids after c/s)—bowel evacuation (constipation: analgesia/anesthesia, sluggish peristalsis, & reluctance to evacuate) o Cardiovascular System: Blood volume (returns to pre-pregnant levels w/ average vaginal blood loss < 500 mL)—PP diuresis dec. the total volume ▪ Cardiac Output: inc. after birth due to uterine BF shifting to systemic circulation following delivery as BV dec. w/ diuresis CO is reduced to return 6-8 weeks ▪ v/s: HR dec (bradycardia)—inc. pulse (indicate pp bleeding or infection)— temperature elevate 1st 24h (pp infection)—inc. BP (preeclampsia & careful monitor for HTN) ▪ Blood components: Hct & Hgb drops moderately for 3-4 days • WBC: can inc. in L&D & pp period • Coagulation factors: inc. risk for DVTs ▪ Varicosities & hemorrhoids: should regress in pp period o Neurologic System: Headaches = watch for preeclampsia or from leakage of spinal fluid into epidural space after Dural puncture o Musculoskeletal System: Abdomen loses tone & slowly regains tonicity ▪ Joint & muscle aches – hypermobility early ambulation, good posture, body mechanics = help stabilize joints & dec. discomfort o Integumentary System: Melasma (chloasma of pregnancy tend to dec.)—Angiomas/Vascular spiders (tend to go away but Spiders may stay)—Loss of extra hair growth • Normal vital signs/signs of potential complications o v/s: low grade fever for 1st 24h can be normal due to dehydration after 24h can be due to infection >100.4 for 1st 10 days = infection ▪ BP consistent w/ BP readings during pregnancy (can take weeks/months for BP & pulse to return to pre-pregnancy levels)—rise in BP (140/90) during 1st week = preeclampsia ▪ Pulse: 50-90 bpm & resp 16-20 Inc. pulse & respirations = hemorrhage pale ashen, cool, clammy skin, & lightheadedness LATE sign of hemorrhage = dec. BP • Postpartum physical and psychosocial assessments and interventions o BUBBLE HE: ▪ B: Breasts, nipples, breath sounds – sore nipples = poor latch ▪ U: uterine fundus level, location & firmness – massage if soft ▪ B: bladder – distention or retention? Use squirt bottle to dec. infection & improve circulation & healing ▪ B: bowels & bowel sounds ▪ L: Lochia & legs – saturated peri pad in 15 min. or less & pooling of blood under buttocks – any edema or DVT ▪ E: episiotomy or stitches ▪ H: Hemorrhoids – Homan’s sign to assess for thrombophlebitis ▪ E: Emotional status & energy level ▪ Common painful sites in PP period o Uterine cramping NSAIDs (motrin, ibuprofen, Tordal, Naproxen) o Perineal trauma, swelling, lacerations, or episiotomy NSAIDs + opioid analgesic o Hemorrhoids o Sore nipp;es & breast engorgement o C/s surgical incision monitor respiratory depression for FULL 12h • Lab tests, medications o Hgb/Hct: esp. w/ history of anemia or inc. PP bleeding o Rubella & Rh status: AVOID PREGNANCY FOR 28 DAYS o Rh – mom & Rh + baby receive Rhogam w/in 72 hours of birth given to prevent mother from developing antibodies to Rh positive blood that she may have been exposed to • Promotion of health and prevention of complications including future pregnancies o Prevention of bleeding: maintain uterine tone—prevent bladder distention—unrepaired lacerations—excessive blood loss ▪ HYPOVOLEMIC SHOCK • Postpartum education on self and infant care o Proper perineal care: wipe front back, change perineal pads frequently & wash hands often o Promote rest & prevent PP fatigue cat nap or sleep when baby sleeps, anticipating that interrupted sleep she will get while caring for newborn 24/7 o Ambulation FALL PREVENTION; OH, prevent VTE, prevent constipation o Assess patient & infant breastfeeding attempts, providing tips & suggestions in how to have the best start w/ lactation, & helping woman to prevent or fix & issues o BOTTLE FEED MOMS: need education on how to suppress lactation engorgement 3-5 days & caused by inc. blood & lymph supply to breasts o SELF TEACHING: fever > 100.4 F, lochia changes color/amount/odor, pain @ incision, severe abdominal pain ▪ s/s of thrombophlebitis, mastitis, or UTI ▪ Follow-ups: BABY- 3-5 days post-birth & MOM – 6 weeks PP Ch 20 • Phases of maternal role attainment o Learning new skills & increasing confidence as a mother o PP “Blues” – very happy 1 moment & crying the next w/o clear reason why o Reva Rubin (1984) ▪ Taking-in phase 1-2 days: passive, somewhat dependent, but talkative about childbirth ▪ Taking-hold 3 days on: begin to take control of self & baby • Parent-infant bonding/attachment o Early contact & extended contact o Communication: the senses – touch, eye contact (en face position), voice, odor o Biorhythmicity: mother’s heart beat can soothe baby o Reciprocity: parent recognizes baby’s body movement or behaviors & in turn responds by holding the baby o Synchrony: when parent’s response = baby behavior (ex: baby cries & mother holds baby) o Engrossment: attachment & interest that Father’s develop for their newborn ▪ Touch & eye contact ▪ Social play v. caretaking ▪ Needs info & encouragement ▪ Needs time w/ newborn [Show More]
Last updated: 2 years ago
Preview 1 out of 9 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$9.50
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Mar 20, 2021
Number of pages
9
Written in
Additional information
This document has been written for:
Uploaded
Mar 20, 2021
Downloads
0
Views
80


.png)