*NURSING > STUDY GUIDE > HS MISC-OB Exam 2 study guide 45 pages.docx | (Obstetrics, progesterone, Identifying, Alteration). C (All)
HS MISC-OB Exam 2 study guide 45 pages.docx | (Obstetrics, progesterone, Identifying, Alteration). Chamberlain College of Nursing.
Document Content and Description Below
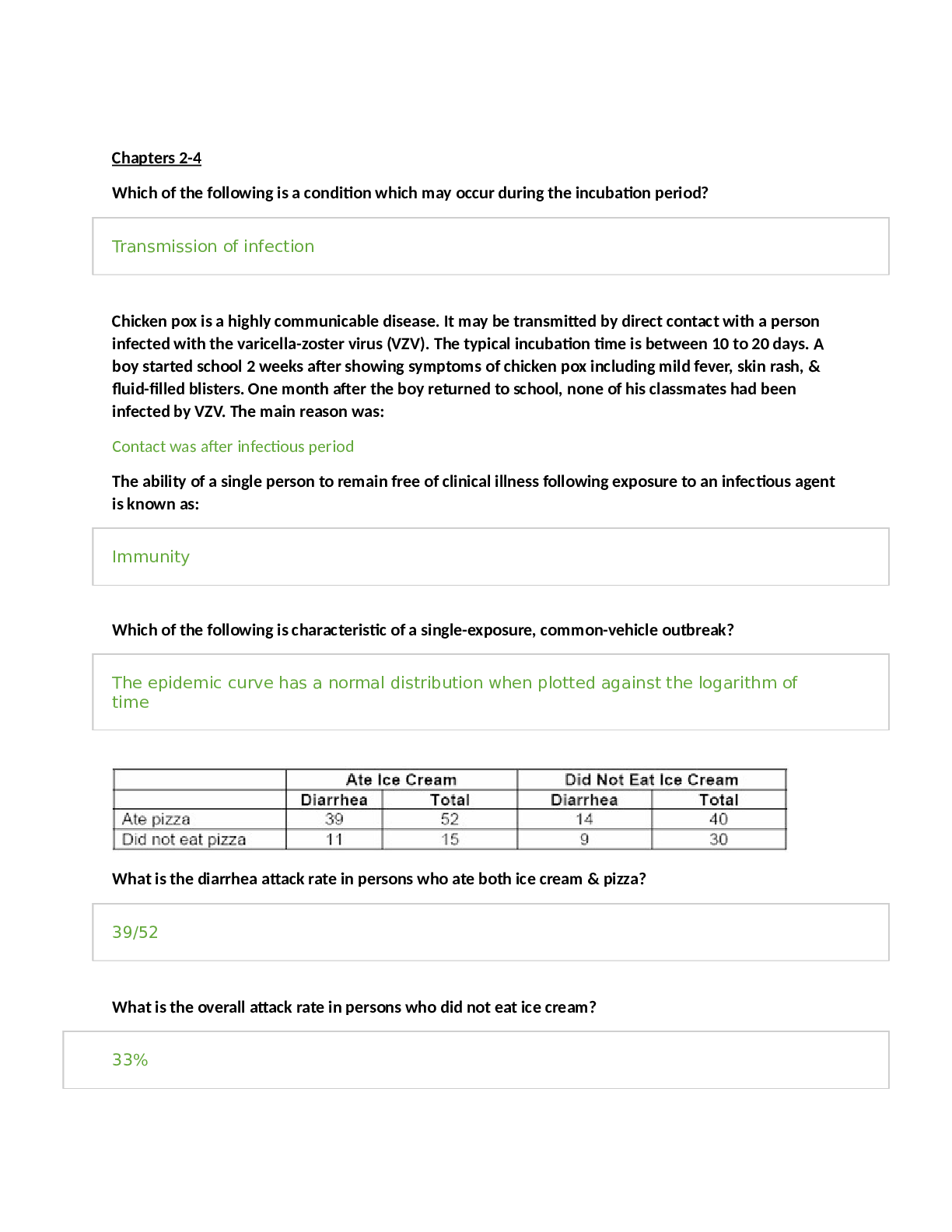
Self-fulfillment needs : Self - actualization Psychological needs: Esteem Love/Belonging Basic needs: Safety Physiological Chapter 8 – Lesson 10 • Adaptations to ... pregnancy (what does mom/dad/siblings/grandparents go through, how can they prepare) Mom 1st trimester = disbelief 2nd trimester = quickening (16-20wk) - Mom starts feeling baby move - Seperates baby from self 3rd trimester = anxious, nesting, tired of being preggo • Adaptation to Pregnancy o Maternal adaptation ▪ Accepting pregnancy ▪ Identifying w/mother role ▪ Reordering personal relationships – mom is no longer #1 ▪ Establishing relationship w/fetus--Emotional attachment o Preparing for childbirth ▪ Attend Childbirth classes – approx. 7mo (28wk) of preggo ▪ 7th month of pregnancy → Empathy belly used for family memb’s o Psychological Tasks of Mother ▪ Form foundation for mutual gratifying relationship w/infant ▪ Helps dev self-concept ▪ 1. Ensuring safe passage through pregnancy, labor, &birth • Seek competent prenatal care → Concerned for herself &unborn child • Read literature, observe/interact w/ new parents → View parenting differently • Acute sense of environmental threats o Perform self-care activities → Diet, nutrition • 3rd trimester, longs for birth though frightened ▪ 2. Seeking acceptance of child by others • Alteration of 1° support group PRN → Network must meet needs of pregnancy • Partner support & acceptance important → Work to encourage other children’s acceptance • If no partner – seek family or friend’s support o Baby-Daddy drama can keep her from reaching this stage ▪ 3. Seeking commitment &acceptance of herself as mother to infant • “Binding in” occurs o Binds to the role of being a mom o Occurs in 2nd trimester • 1st trimester – abstract idea • 2nd trimester – quickening, bonding &attachment begins • Imagines baby images → Motivation to become competent in role of mother ▪ 4. Learning to give of oneself on behalf of one’s child Dad • Paternal Adaptation to Pregnancy o Accepting pregnancy → Id’ing w/ father role o Reordering personal relationships → Est’ing relationship w/ fetus → Emotional attachment o Preparing for childbirth o Couvade – when dad becomes pregnant ▪ Unintentional dev of phys symptoms of preggo • Sympathy pains, etc. • Partner experiences Siblings • Sibling Adaptation o Reactions manifested in ’s o New baby marks beg’ing of sibling rivalry → Attempt to minimize prob’s during pregnancy o Involvement in planning &care (age approp) → Take to prenatal visit, sibling class → Visit mom & baby in hospital o Consistency is important ▪ Same care, person, things remain same → Same parental attention ▪ Discuss handling regressive or aggressive behavior o ’s should be made several wks prior to childbirth → give sibling time to adjust ▪ Move from crib to bed ▪ Toilet training → May regress &wet bed ▪ Weaning → May want bottle or breast again Grandparents • Grandparent Adaptation o Usually first informed of pregnancy ▪ Contribute family continuity → Supportive, mend fences o Intergenerational relationships shift → Most will lavish w/ gifts, advice o Younger grandparents → May Exhibit Less interest o Involvement dependent on cultural & familial factors → May attend classes Additional Info from Lesson 10 – not on study guide • Intrapartum Care o Doulas ▪ Specialized childbirth support person → Experienced in caring for laboring women ▪ Role: enhance comfort & decrease anxiety of laboring woman ▪ Provides support, encouragement → Facilitates communication w/ caregivers ▪ Provide support for the client & coach → ↑ Bonding ▪ No medical/RN care ---certification, no license ▪ Highered by mom • Postpartum: Parent-Infant Contact o Early contact → May facilitate attachment process – immed after birth o Extended contact → Optimizes family-centered care • Parental Role after Childbirth o Transition to parenthood o Maternal adjustment (P. 572) ▪ Dependent phase—taking-in ▪ Dependent-independent phase—taking-hold o Postpartum “blues” ▪ 1st few days after birth ▪ Transient period of depression • Tearful, anorexia, insomnia ▪ Occurs in 70% of all postpartal clients ▪ Changing hormonal levels ▪ Psychological adjustments ▪ Unsupportive enviro, fatigue, insecurity ▪ Resolve naturally w/in 10-14 days • Factors influencing parental responses: o Social support o Culture o Socioeconomic condition o Personal aspirations o Age – adolescent, > 35 y/o Chapter 9 – Lesson 9 Remb: – period b/t conception to the onset of labor (during preggo) Intrapartum – period from labor to just before delivery Postpartum – period from after delivery until 6 wk after delivery • Pregnancy hormones (estrogen, progesterone, relaxin, hCG, hpl): What does each one do? How do they help create or sustain pregnancy? o Physiological Changes of Pregnancy: Influence of hormones • Body secretes hormones essential to pregnancy o Human chorionic gonadotropin (hCG) • Source: Fertilized ovum & chorionic villi (trophoblastic cells) • Stim’s prod of progesterone (pregnancy hormone) &estrogen ▪ Estrogen gets you preggo ▪ Progesterone keeps you preggo • Preserves the corpus luteum (assumes role of placenta) ▪ Corpus luteum secretes progesterone until placenta b/g’s to secrete it – approx. 10wk • hCG – basis for pregnancy test ▪ ELISA: Enzyme-linked immune-sorbent assays o Specific antibody(anti-hCG) bonds w/ hCG in urine o Take 1st thing in the morning: need fresh urine sample o hPL - Human placental lactogen • Dev’s breasts for lactation • ↓’s maternal insulin sensitivity ▪ Can interfere w/ production of insulin, can cause GDM o Estrogen----Stim’s dev of uterine & breast tissue (2° female sex chara’s) • Causes ↑ in cervical cells, resulting in mucus plug • ↑ vaginal secretions • Breasts enlarge & areola darken • “Gets pregnancy started” o Progesterone---Maintains endometrium, smooth muscle relaxant. • Causes ↑ volume of air & ↓ air resistance • Clotting factors ↑, cardiac output ↑, RBC ↑, blood pools in lower extremities • ↓ peristalsis & delayed gastric emptying • ↑ skin pigmentation & relaxed joints • “keeps pregnancy going” o Relaxin---Causes ’s in collagen, connective tissue - Can cause falling! • Causes waddling • Signs of pregnancy (subjective, objective, &diagnostic): What are examples of each one? o Signs of Pregnancy • ’s women experience during pregnancy; • Used to diagnose the pregnancy itself o Subjective Changes—Presumptive • ’s the woman experiences & reports → can be caused by other conditions • Not considered proof of pregnancy • Examples: ▪ An ↑ in urination ▪ tender breasts ▪ N/V ▪ Quickening – fluttering of fetal movement – could be gas o Objective Changes—Probable • Reasonable to believe • Examiner can perceive changes → More diagnostic than subjective -- Does not offer definite dx • Examples: P. 190; Tbl 9-2 ▪ Pelvic organ changes o Hegar’s sign (Hay-gars) (pg 190, Figure 9-4) ▪ softening of isthmus (lower portion) of the uterus ▪ determined by examiner by vaginal examination o abdominal enlargement o Goodell’s sign – softening of the cervix o Chadwick’s – discoloration of the cervix ▪ McDonald’s – flexing of the body of the uterus if the cervix is pressed on ▪ Braxton Hick’s Contractions ▪ Skin pigmentation o Linea nigra o Nipples/areola ▪ Preggo tests – false +’s ▪ Uterine Souffle – whooping sound o Diagnostic Changes—Positive • completely objective - cannot be confused w/pathologic states • conclusive proof of pregnancy 1. Palpation of fetal movement by the examiner after 20 wks gestation 2. Visualization of fetus (ultra sound) 3. Listening to fetal heartbeat w/Doppler device • Assess mom’s heart rate 1st o Average HR 120-160 o Must be at least 8 weeks • Fetal scope (16-20 wks) Info not on study guide • Diagnosis of Pregnancy o Antepartum visit → obligated to seek care o Interview includes: • Health/Medical Hx • Medical or surgical cond’s • Look for medic alert bracelets • Limps or special shoes, pelvic d/o’s? → r/t complicated preggo • Allergies , Chronic diseases (HTN, DM are most common), Medications • Review of systems – head-to-toe assessment • Body system changes during pregnancy: What happens to the cardiovascular system? What happens to the respiratory system? What happens to the GI system? What happens to the Integumentary system? (cardiac output, constipation, SOB, deeper respirations, skin discolorations, etc) o Cardiovascular • Affected by ↑ progesterone & estrogen → Heart pushed up, left & forward ▪ √ patients w/ pre-existing heart disease • Cardiac output ↑ 30-50% (significant!!!)→ Peaks 25-30 wks ▪ if mom has pre-existing cond → visit cardiologist • Pulse: ↑ 10 – 15 beats/min above normal, systolic murmurs ↑ in preggo • Blood pressure: ↓ slightly in 1st trimester – progesterone is relaxing ▪ Lowest during 2nd trimester ▪ Gradually↑ to pre-pregnancy level during 3rd trimester • Enlarged uterus ▪ Pressure on pelvic & femoral vessels ▪ interferes w/ blood return from lower extremities → pooling of blood in lower extremities • S/S: ▪ Dependent edema - Varicose veins (legs, vulva, rectum) – normal in preggo due to pooling of blood in lower extremities ▪ Postural hypotension - due to enlarged uterus that puts pressure on vena cava - ↓ blood flow → maternal hypotension o Occurs in supine position o Reduces blood flow to ♥’s rt atrium ▪ Causes a condition called Supine hypotensive syndrome o ↓ placental perfusion → Affects fetal reserve ▪ Depletes the reserve, ↓ HR → hypoxia ▪ Uterus presses on aorta → Aortocava compression o S&S: ▪ Decreased BP, dizziness, clamminess, pale skin ▪ Supine hypotensive syndrome = vena cava syndrome = Aortocava compression (all the same thing) ▪ Nursing Interventions o Assist in side-lying position o Place pillow or wedge under right hip • Blood Volume Changes ▪ Progressively ↑ ▪ ↑ most significantly during 2nd trimester ▪ ↑ slower during 3rd trimester ▪ stabilizes during last wks of pregnancy o 40 – 45% ↑ pre-preggo level – by last wk of preggo o due to ↑ in erythrocytes &plasma → blood is watery (plasma) & RBC’s of immature • Blood Composition Changes ▪ ↑ level of RBCs to ↑ O2 delivery to cells - ↑ O2 in hemoglobin to baby ▪ Total erythrocyte (RBC) volume ↑ o 30% w/ iron supplementation o 18% w/out iron supplementation ▪ Plasma volume ↑50% o Hct measures conc. of RBC in plasma – a lot of plasma = ↑ water in blood o Hemodilution is manifested by a lower Hct - excessive plasma, diluting the blood ▪ Physiologic anemia of pregnancy (psuedoanemia) ▪ Not true anemia – is just a excess in plasma (water in blood) • Leukocyte production ↑ ▪ White blood cells (WBCs) - ↑ during pregnancy o 5,000 – 12,000 o May reach 25,000 or higher by time of delivery o This is normal → helps fight infxn • Clotting factors ↑ ▪ Factors VII, VIII, IX, &X – not exactly sure which ones ▪ Fibrin &plasma fibrinogen levels ↑ ▪ Hypercoagulable state → Risk for dev’ing venous thrombosis o ↑ coag = less bleeding during delivery ▪ Nursing Interventions: Monitor Homan’s sign o Respiratory • ↑ in O2 needs ▪ between 16 – 40 wks → O2 consumption ↑↑ 15-20% - ↑ O2 for mom & baby • Increasing levels of progesterone causes: remb: progesterone relaxes ▪ ↓ airway resistance → ↑ volume of air • Tidal volume ↑steadily • 30-40% rise from non-pregnant values – deeper respirations • Uterus enlarges…. ▪ Diaphragm elevates, *****Ribs flare ▪ ↑ anterior-posterior diameter****Up to 6 cm greater ▪ Breathing ’s from abdominal to thoracic breathing • S&S: ▪ Shortness of breath (SOB) → Hyperventilation → Thoracic breathing ▪ Nasal stuffiness (rhinitis) → Nosebleeds (epistaxis) o Due to estrogen o Urinary (not on study guide) • 1st trimester = uterus is a pelvic organ • 2nd trimester = uterus is an abdominal organ • Cause: ↑ size of uterus • Fxnal ’s: ▪ ↓ Bladder capacity → uterus is sitting on bladder - ↑ pressure ▪ Ureters elongate & dilate → glomerular filtration rate ↑ 50% & renal tubular reabsorp ↑ o Leading to ↑ voiding • S&S: ↑ urination, glycosuria (glucose in urine) o GI - Bowels • ↑ progesterone ▪ Smooth muscle relaxation ▪ Colon displaced • S&S: ▪ Peristalsis ↓→ Delayed gastric motility & emptying ▪ Constipation → Hemorrhoids → Varicosities of rectum ▪ Appetite fluctuates, taste ’s ▪ N/V – hCG, metabolism o Integumentary • Skin: ↑ estrogen, progesterone & melanocyte-stim’g hormone ▪ Pigmentation ’s: o Areolae, nipples, vulva → Linea nigra o Striae gravidarum – stretch marks ▪ 50-90% o Chloasma - Melasma gravidarum = Mask of pregnancy ▪ dark, irregular well demarcated hyperpigmented macules to patches ▪ commonly found on the upper cheek, nose, lips, upper lip, and forehead ▪ fades after pregnancy • Hair ▪ Rate of growth may ↓ o ↓ # hair follicle in resting or dormant phase ▪ Reports of Hirsutism common o unwanted, male-pattern hair growth in women o Fine hair growth ↑ • Hyperactive sweat glands o Musculoskeletal Changes (not on study guide) • Diastasis recti--Rectus abdominis muscle to separate • Cause: Pressure on abdominal muscles --Enlarged uterus • Nursing Interventions ▪ Teach about safe position ’s--Support joints ▪ Pregnancy belt, wrist supports--Wear support hose (knee or thigh-high)---Elevate lower extremities → ↑ BP, ↑ venous return, ↓ DVT’s ▪ Teach prenatal exercises ▪ Avoid muscle strain and overtiring Perform according to comfort level ▪ Partial sit-ups Knees flexed, feet flat on floor ▪ Stretch arms to knees---Head and shoulder off floor 5 reps ▪ Pelvic (abd) tilt or pelvic rock--Prevents/reduces back strain ---Strengthens abdominal and back muscles – relieves lower back pain (< 4mo’s preggo = laying; > 4mo’s = standing) • Kegel exercises o Strengthen muscles of pelvic floor, pubococcygeus muscles o ↑ elasticity-------------Elevator exercise Done any time, choose cue • Inner thigh exercises “Tailored sit” o Crossed-leg sitting position whenever possible o Stretches inner thigh muscles Prepare for child birth • Lab tests/blood studies (know any specific values that you were given)(Review all Blood Studies from Lesson 9; know all lab tests done for antepartal testing) o Antepartum Testing o Fetal Activity Monitoring p. 236 – b/g after 28wk • Cardiff Counting Method (28 weeks) – do if she wonders when the last time the baby moved was • Count fetal movements &record - or = 10 movements in 3 hours is normal • Vigorous activity = reassurance of fetal well being • ↓ or cessation = possible problem o Ultrasound • Visualization of fetus – transabdominal & transvaginal o Umbilical Artery Velocity Waveforms/ Doppler Blood Flow Studies • Noninvasive U/S • Meas’s blood flow ’s in maternal & fetal circulation • Assesses placental fxn o Percutaneous Umbilical Blood Sampling & Chorionic Villus Sampling – PUBS or CVS • Sample of umbilical blood - Small sample of chorionic villi • Transabdominally or transcervically • Products of conception tested directly – tests are exact • As early as 8 to 10 weeks • Test for genetic (1°), metabolic d/o’s • Only done if problem or ↑ maternal age ▪ Ex: 1st baby has down’s syndrome, 2nd preggo = PUBS test ▪ ↑ r/o miscarriage, infxn • RhoGAM PRN ▪ Due to invasive testing ▪ Blood can cross ▪ Indirect Coombs Test o Indirectly check on mom o Detects presence of Rh antibodies in maternal serum ▪ If non-sensitized (negative) ▪ RhoGAM immunoglobulin at 28 wks o Nonstress Test (NST) KNOW: RN interventions & how to read Fetal HR strips • If fetus has adequate O2 & intact CNS = accelerations of fetal HR (FHR)with fetal movement (FM) • Only done if prob: HTN, DM, hx of previous fetal demise • Mom pushes button if she feels FM • Reactive NST - normal ▪ 15 x 15: accelerations of 15 bpm lasting 15 sec’s w/each fetal movement (FM) ▪ 2 x 20: occurs 2 times in 20 minutes time frame – pt must stay on monitor for 20 min ▪ If 15 x 15 & 2 x 20 → RN int: document as reactive NST • Nonreactive NST - abnormal ▪ No accelerations of FHR w/ FM ▪ If no rxn in 20min → RN interventions: o 1. Cracker, juice (↑ glucose) or vibroacoustic stimulation (sound & vibrations shake baby awake) o 2. Monitor for add’l 20 min – 40 min max o 3. If no rxn → notify MD o Contraction Stress Test (CST) Remb: we want…. NST + CST - • Only done if it is suspected baby will not tolerate labor - done close to term • mom given Pitocin to induce contractions • Eval’s resp fxn of the placenta ▪ Negative CST: o Normal: healthy fetus will maintain a steady HR o 3 contractions last 40 sec + in 10 min - NO decelerations ▪ Rn int: Once this occurs STOP oxytoxin (Pitocin)!! ▪ Positive CST: o Stress of uterine contraction shows repetitive late deceleration w/more the 50% of the uterine contractions o ↓ placental sufficiency o RN int: prep for C/S o Amniocentesis • Needle inserted into uterine cavity to w/draw amniotic fluid • Performed early (15-16wks) – genetic abnormalities • Performed late (3rd trimester - 35-36 wk) – fetal lung maturity - L/S ratio ▪ L/S ratio 2:1 = 99% chance that lungs are fxn’ing (have adequate surfactant) ▪ If L/S ↓ →RN Int: Admin Celestone to mom →↑ baby’s production of surfactant • RN int: admin RhoGAM after procedure to all Rh – mom’s • Risks: ↑ r/o bleeding, infxn o Biophysical Profile - 1st choice for follow up fetal evaluations!!! • i.d’s compromised/healthy fetus • assesses placental fxn • each eval has possibility of 2 pnts • A. Fetal Breathing Movements – 1 episode of 30 sec in 30 min • B. Fetal Tone - at least 1 episode of extremity extension & flexion • C. Body Movement – 3 episodes in 30 min • D. Amniotic Fluid Volume – More than 1 pocket > 1 cm in 2 planes • E. Reactive NST – FHR ↑ w/activity o A.L.O.N.E. • Amniocentesis • L/S ratio (2:1) • Oxytocin Test (CST) • Non-stress Test (NST) • Estriol level – one of the 3 main Estrogens prod’d by the body (Remb: Estrogen keeps you preggo!) o Blood Tests Know specific values!!!! • Hemoglobin/hematocrit o Detects anemia, iron or folic acid deficiency ▪ Anemia = Hgb < 10, Hct < 35% - usually Hct is 2x Hgb ▪ Remb: during preggo, ↓ Hgb b/x of ↓ blood vol on board in mom o Preggo N: Hgb 10-14g/dL, Hct 32-42% o Eliminate symptoms – pale mucus membranes, susceptible to infection, tachy, pallor… o Correct deficiency – PNV and Fe tab – w / O2 • Sickle cell anemia o Abnormal hemoglobin molecule (hemoglobin S) in blood – causes sickle shape o Recessive hereditary, familial d/o o Mediterranean, Southeast Asians, or African-American descent o Monitor fetal well-being o Blood transfusions if severe, analgesia (Morphine), antibiotics • Thalassemia o Hereditary d/o – defective synthesis of hemoglobin molecule (alpa and/or beta) o Insufficient amt of globin to fill RBC’s o Meditarranean, Chinese, North African, Italian, Greek, African-American o Does not respond to iron therapy – bc it’s a heredity d/o, it’s just how the body prod’s it o Lifelong severe hemolysis, anemia (monitor mom & baby), and premature death • Blood type, Rh Status • Ex: A+ • A= blood type • Positive (+) = +RH factor (D antigen present on RBCs) o RPR---Rapid plasma reagin • Identifies women with untreated syphilis Non-reactive or Reactive • Fetus/Newborn Effects Congenital syphilis, jaundice, rhinitis, anemia, IUGR, and CNS involvement ▪ IUGR = intrauterine growth restrictions • Treatment: PCN G 2.4 million units IM to prevent placental transmission ▪ PCN G = Penicillin G ▪ Admin to mom as soon as it’s detected. Tx Dad too. o Rubella titer • Determines immunity to rubella--German measles or 3 day rash • Spread by droplets, direct contact with contaminated object • Immune if titer 1: 8 OR GREATER ▪ Really 1:10 or > if definitely immune • Fetus/Newborn Effect ▪ Transmitted through placenta Risks increases the earlier her exposure to virus ▪ IF NON-IMMUNE, NEG → VACCINE DURING POSTPARTUM PERIOD o Don’t get preggo for 3 mo’s after vaccine o Can BF → pass immunity to baby o Human Immunodefiency Virus (HIV) • USPHS recommends all pregnant women be offered antibody screening test • HIV testing using (ELISA) • Reduce likelihood of perinatal transmission ▪ Ethical issue, may refuse – informed consent ▪ Oral antiretroviral drugs BID from 14 wks gestation until birth, IV during labor (IV), oral syrup for newborn in first 6 weeks ▪ Birth is usually sched’d C/S – w/cauterization to ↓ / stop blood flow & ↓ r/o baby being exposed to mom’s blood ▪ Zidovudine decreases perinatal transmission • HCP must inform about HIV symptoms, testing, methods of decreasing transmission • Advocate for fetus BUT not at the expense of the pregnant woman • Pregnancy/Fetal/Newborn Effects ▪ Preterm delivery, premature rupture of membranes (PROM) Hemorrhage, GU Infections ▪ Prematurity, LBW (low birth weight) <2500 g – 5.5lb ▪ Public Health Service recommends to avoid Breastfeeding if HIV + in U.S. – transmitted through BF o Tuberculin skin testing • Assess exposure to tuberculosis – Mycobacterium tuberculosis • Carried on droplets and spread by airborne transmission • Those at risk: Immunocompromised (ie mom w/HIV), homeless, immigrants, injectable drug users • Assessment findings ▪ Fatigue, fever or night sweats, nonproductive cough, slow wt loss, anemia • Tine or PPD (purified protein derivative) tuberculin tests ▪ Intradermal, reddened induration within 72h ▪ Chest x-ray after 20 wks, sputum cultures to confirm • Treatment during pregnancy is the same as for general population ▪ Isoniazic, rifampin, ethambutol daily for up to 9 months. • Fetal effects – minimal risks for congenital anomalies • BF not contraindicated Teach not to cough, sneeze or talk directly into NB’s face • Other tests o Pap test- all mom’s • Screen for cervical neoplasia, Herpes simplex type 2, HPV • Vaginal or rectal smear--------------------Exposure to STI, Neisseria gonorrhea Chlamydia, HPV o GBS – Group B Streptococcus • Naturally occurring bacterium found on body • Asymptomatic most often May have UTI, uterine infection(after delivery) or chorioamnionitis ▪ Fetus/Newborn: Can be life-threatening to newborns Pneumonia or sepsis, meningitis – if baby comes through vaginal canal; C/S = no risk • CDC guidelines; Screen all 35-37 weeks Treat with PCN or Amp 4 h before birth • Baby will have CBC & blood cultures • Other tests cont’d. o Completion of TORCH panel o Urinalysis Infections o Renal disease Unsuspected diabetes mellitus o Hematuria CLIENTS THAT need additional screening - not on study guide • HAVE TYPE O BLOOD or Rh factor that is negative (D antigen absent) o ABO incompatibility or Rh incompatibility • Maternal Serum Antibody Screening o IF Patient has O Blood Type • Tests mother’s blood for anti-A, anti-B antibodies – IgM antibody • Positive results – monitor newborn closely after birth o IF Patient is RH negative (D antigen negative) • Tests for Rh antibodies (Indirect Coombs Test) – IgG antibody response o Positive results – monitor baby closely after birth o *********Negative results (good)--- prevent isoimmunization********RhoGAM at 28wks • Newborn/Fetal effects Fetuses at risk for developing erythroblastosis fetalis Hyperbilirubinemia in neonatal period • Review RhoGAM! o RhoGAM Immunoglonulin IM Injection at 28 wks PRN • Temporary Passive Immunity o Rh incompatibility does not affect 1st pregnancy • Must prevent antibodies o DO NOT GIVE IF: • Baby’s Rh factor is - • Ex: MOM – O- & BABY – O- = no RhoGAM • Mother is sensitized---Indirect Coombs + Exposed to Rh + blood • Direct or indirect Coomb’s is + ▪ b/c sensitivity has already occurred, can’t undo it o GIVE RhoGAM IM at 28 wks & w/in 72h after delivery IF: • Mother is not sensitized - indirect Coombs is - • Baby’s Rh factor is + & direct Coombs Test is - • Ex: MOM- O -, BABY – O + • Direct or indirect Coombs is - • TORCH panel: What is it? What does each letter stand for? o TORCH Infections • To: toxoplasmosis - parasite infxn ▪ from handling cat litter, raw meat ▪ wash fruits & veggies ▪ therapeutic abortion if diagnosed < 20 weeks ▪ stillborns &neonatal death common ▪ Assessment o Usually asymptomatic to mother o Flu-like symptoms o Fetal affects depend when infections occurred • R: rubella (German Measles) ▪ test mother for immunity, greatest risk 1st trimester • C: cytomegalovirus ▪ most common viral infection ▪ spread by body fluids ▪ common cause of mental retardation • H: herpes virus Type II ▪ Cesarean delivery to protect infant • Danger signs in pregnancy: What are they &what should patient be educated on? o Sudden gush of liquid from vagina • Rupture of membranes o Vaginal bleeding • Abruption placentae • Placenta previa • Bloody show o Abdominal pain • Premature labor • Abruption placentae o Temperature greater than 101°F & chills • Infection o Persistent vomiting • Hyperemesis gravidarum o Visual disturbances or muscular irritability, convulsions • Hypertension • Preeclampsia o Edema of hands/face, legs, feet • Hypertension • Preeclampsia o Severe headache • Hypertension • Preeclampsia o Epigastric pain • Preeclampsia o Dysuria • Urinary tract infection o Oliguria • Renal impairment, ↓ fluid intake o Absence of fetal movement • Maternal medication, obesity, fetal death Chapter 10 – Lesson 9 • GP & GTPALM: how do you document each one? o Documentation of OB Hx (pg 200-201) o Primigravida – preggo for 1st time o Primipara – woman delivered 1 potentially viable fetus o Multi – preggo many times o Nulli – never preggo o Term – born b/t 38-42wk o Premature – birth after 20wk but b/f completion of 37wk → 20wk, 1 day – 37wk, 6 days o Post-term – after 42wk o GP – Gravidity & Parity ▪ A two-digit system -documents # of pregnancies ▪ G_ P_ ▪ Gravida → # of pregnancies, including current pregnancy ▪ Para →pregnancies that have reached point of viability (viability = 20wk) • If # of wk is unknown, weigh to determine if fetus is > 500g ▪ Ex: G1P0: 1 pregnancy, did not reach viability o Acronym GTPAL – documents the # of infants; more detail ▪ G-Gravida ▪ T-Term ▪ P-preterm (does NOT mean para) ; after 20wk ▪ A- Abortions (Induced or spontaneous) ; b4 20wk ▪ L- living children (how many are alive TODAY) ▪ M- multiple gestations (twins, triplets, etc) o Critical Thinking Exercise: M.P has come to the clinic on Sept. 10th. Pregnancy test was +. States LMP was June 10th. Obstetrical HX: Had an abortion when she was 18. Had a miscarriage at 11 weeks last year. How would you document her obstetrical hx using the 2 method system? o G_3 P_0 o Critical Thinking Exercise: M.P has come to the clinic on Sept. 10th. Pregnancy test was +. States LMP was June 10th. She tells you: She had an abortion when she was 18. Had a miscarriage at 11 weeks last year. How would you document her obstetrical hx? Using GTPAL: G_3 T_0 P_0 A_2 L_0 OR (G30020) • Initial prenatal assessment (what happens to specific body systems?, what is normal?, what is abnormal?, what does nurse need to do?) o Initial exam to provide a baseline o Assess V/S, Height, Weight o Bladder should be emptied before pelvic exams o Head to toe by examiner • Review Assessment Guide (pgs 206-212) • Naegele's Rule: how do you determine due date? o LMP – 3mo’s + 7days + 1yr = due date o Critical Thinking Exercise: Determining Estimated Date of Birth o EDB using Naegele’s Rule: LMP:_July 10,2013_; Subtract 3 months April 10,2013 ; Add 7 days_April 17,2013 ;Add 1 year (prn) April 17, 2014 o EX: July 10th EDB or EBC or due date: April 17, 2014 o Figure 10-2 (pg 213) EDB wheel. The EDB wheel can be used to calculate the due date. To use it, place the “last menses began” arrow on the date of the woman’s LMP. Then read the EDB at the arrow labeled 40. In this case the LMP is September 8, &the EDB is _June 17 • Subsequent prenatal assessment (after the first visit, what is assessed?)(pgs 217-220) o q4wk = 1st 28wk (7mo) ; q2wk = 29 - 36wk ; q1wk = after 37wk • Fundal height measurements (what measurement equals what gestational age?) o Meas’d from the superior aspect of the symphysis pubis to the upper most part of the uterus = fundus o Correlate w/22-34 gestational wk o 22-24wk – fundus is level w/umbilicus o 38-40 wk – fundal height ↓ as lightening occurs • What is lightening? When does it normally occur? o Fetus drops & descends into the pelvis in preparation for birth ▪ Remb: lightening shoots to the ground o Occurs – 38-40wk Chapter 11 – Lesson 11 • Discomforts in pregnancy (Table 11-2). What can nurse do for each one? What can Mom do for each one? Education for each one? ****most complications of preggo can be relieved w/o meds!!!! o Pregnancy (pg 229-230, Table 11-2): o Morning Sickness - Nausea & vomiting (subjective info) ▪ Causes: diet ▪ 50-80% of pregnancies – • Should subside by 12 weeks ▪ Helpful hints • Small meals – GI tract has time to empty • Crackers/toast b4 rising • Avoid odors • Ginger • Avoid spicy/greasy food ▪ May lead to hyperemesis o Ptyalism (pronounced: tyalism) ▪ Excessive salivation • Usually before 8 weeks ▪ Helpful hints • Swallow frequently • Good oral hygiene • Mouthwash, hard candy, chewing gum • Avoid starch intake – breaks down oral cavity o Altered taste ▪ Usually bitter or sour ▪ Helpful hints • Brush teeth frequently • Use mouthwash • Use hard candy or chew gum o Bleeding gums ▪ Increased blood flow - ↑ ♥ output ▪ Good oral care (gum care) ▪ Will go away after pregnancy ▪ Encourage dental care (soft tooth brush), infection could lead to sepsis! o Breast tenderness ▪ Very common 1st trimester • ↑ estrogen & progesterone ▪ Helpful hints • Well-fitting support bra → no underwire • Warm showers → warms tissues o Urinary Frequency (subjective change) ▪ Common 1st & 3rd trimester → uterus is resting on bladder • If 2nd trimester urinary freq ~~ UTI??? ▪ Helpful hints • Kegel exercises • Limit fluid HS • Void regularly • Avoid caffeine - 5 cups = miscarriage o ****↑ caffeine in early preggo → miscarriage o Congested (rhinitis) or Bloody (epistaxis) nose ▪ ↑ estrogen & progesterone ▪ ↑ blood flow ▪ Helpful hints • Avoid decongestants & sprays • Use humidifiers, cool mist vaporizers • Use saline nose drops o Leukorrhea (Chadwicks sign/bluish hue) - ↑ WBC ▪ ↑ vaginal secretions (white) – usually due to Estrogen imbalance ▪ Rule out infections (itching/odors) • more susceptible to yeast infection ▪ Helpful hints • Good personal hygiene • Cotton panties • Minipads • Avoid douching • Washes away good flora • Vagina is acidic, becomes less acidic o Fatigue ▪ Rule out anemia • Lab: Hgb < 10 = anemic ▪ Body works overtime • Nourishing environment for the fetus • Adjustment to pregnancy: ↑ blood volume ▪ Helpful hints • More frequent rest periods • Active relaxation - yoga • Guided imagery o Heartburn ▪ Cardiac sphincter remains a little open during preggo ▪ Gastric reflux • Common in 2nd trimester ▪ Progesterone @ peak in 2nd trimester • Slows smooth muscle of GI tract ▪ Helpful hints • Small frequent meals • Avoid fatty foods – takes longer to digest • Drink milk prior to meals • Antacids – TUMS (calcium) o No Rolaid’s - magnesium • Avoid lying down after meals o Constipation ▪ Progesterone • Pressure &displacement of bowels ▪ Helpful hints • Drink lots of water • Increase roughage in diet • Exercise - walking • Use only laxatives prescribed by MD o Hemorrhoids ▪ 1st: Varicose veins of the rectum • Straining w/ constipation (usually) ▪ 2nd: can be r/t pressure of uterus ▪ Painful itching symptoms ▪ Helpful hints • Avoid straining by preventing constipation • Warm baths, ice packs, Tucks pads (witch hazel) • Creams or ointments prescribed by MD only → Prep H, ammusol o Faintness or Dizziness ▪ ↓ BP due to uterus compressing major arteries - supine position ▪ ↓ blood sugar ▪ ↓ iron ▪ Quickly ’ing positions ▪ Helpful hints • Move slowly when changing positions – rise slowly, dangle @ edge of bed • Avoid warm crowded areas – don’t lock knees • Rest on either side (not supine) o Round ligament pain ▪ Maintains uterus in ante-flexed position • Pelvic bone to pelvic bone • As uterus grows, round ligament stretches = round ligament pain • Pain in abd – usually when she moves & stands o If she lays down & rests it goes away ▪ Helpful hints • Avoid sudden jerking movements • Turn on side when getting up • Warm baths, heating pads (on low) - hydrotherapy • Non-constricting clothing → no low-rider jeans – rest on round ligament o Edema ▪ Normal – below the hips • Feet, ankles, & lower legs ▪ Abnormal • Face, tibia, anywhere else ▪ Helpful hints • Avoid remaining in one position → blood pooling • Rest frequently w/ legs elevated - ↑ venous return o Nocturia ▪ ↑ urine production • Affects sleep & rest needs of client ▪ Urinary freq – 1st & 3rd trimester is common ▪ Helpful hints • Avoid caffeine • Avoid drinking fluids late evening o Insomnia ▪ Large size of uterus ▪ Fetal activity ▪ Heartburn ▪ Nocturia ▪ Emotional factors ▪ Helpful hints • Support uterus while sleeping - preggo pillow • Semi-sitting to sleep (semi-folwers or high-fowlers) or L-Lateral preferred • More frequent rest periods • Elevate HOB o Varicose Veins ▪ Common- legs, vulva, & rectum (hemorrhoids) • Dull, throbbing pain ▪ Caused by ↑ pressure on the legs & pelvic veins (by gravid uterus) & by ↑ blood volume ▪ Helpful hints • Avoid constrictive clothing • Avoid prolonged standing or sitting or crossing legs often • Wear support hose o Lower backache ▪ Change in center of gravity ▪ Progressive lordosis - normal inward curvature of the lumbar and cervical regions of the spine ▪ Helpful hints • Good body mechanics (pg 234, Figure 11-4) • Good posture • Pelvic rock or tilt (pg 240, Figure 11-9) • Maternity girdle for support o Leg Cramps (pg 235, Figure 11-5) ▪ Sudden, painful, feels like toes are touching your heel • Cause is unclear (imbalance of minerals – Calcium & Phosphorous ▪ Helpful hints • Dorsiflex the foot till cramp is relieved • Press bottom of foot against a hard surface • Adequate diet in calcium o Shortness of breath ▪ Uterus pushing on diaphragm ▪ Helpful hints • Rib cage lift – consciously, while standing • Good body posture • Semi-sitting position to sleep – never supine o Braxton-Hicks contractions – In abd - intermittent, irregular, painless (usually) ▪ Starts at 3-4 month of pregnancy ▪ More obvious in 3rd trimester ▪ Helpful hints • Abdominal breathing • Active relaxation • Change activity • Make sure not dehydrated o Carpal Tunnel Syndrome ▪ Tingling, numbness, &burning in fingers especially thumb & next two fingers • Shoot your gun with your hand – those fingers ▪ Results because of excess fluid ▪ Helpful hints • Raise affected hand above head & flex hand • Splint hand while sleeping o Skin changes ▪ Due to fluctuations in hormones - Brown, blotchy patches may occur on the face, forehead, and or cheeks ▪ Mask of pregnancy or chloasma - Pigmentation may also ↑ in nipples o Skin and Hair ▪ Chloasma • Melasma gravidarum (Mask of pregnancy) - fades after pregnancy o Hair ▪ Rate of growth may decrease - ↓ # hair follicle in resting or dormant phase ▪ Reports of Hirsutism common - Fine hair growth ↑ o Hyperactive sweat glands o Stretch marks ▪ Pinkish, normally occur on abdomen, thighs, and buttocks ▪ Caused by rapid increase in weight - Stretching of connective tissue o Second Trimester Skin Changes ▪ ↑ estrogen, progesterone and melanocyte - stimulating hormone o Pigmentation changes ▪ Areolae, nipples, vulva - Linea nigra - Striae gravidarum - 50-90% Chapter 12 – Lesson 9 • Maternal weight gain (how much comes from what? (example: baby, placenta, fluid, etc) Pattern o 1st trimester = 3.5 – 5 lb o 2nd & 3rd trimester = 1 lb / wk o Twins: 2nd & 3rd trimester = 1.5 lb / wk Weight Distribution: o Fetus, placenta, amniotic fluid 11 lb o Uterus 2 lb o Increased blood volume 4 lb o Breast tissue 3 lb o Maternal stores 5 -10 lb • Nutritional needs during pregnancy & postpartum (calories &%) o RDA for almost all nutrients increase o Caloric intake 2nd & 3rd trimester Calories increase by 300 kcal/day o ↑ 300 kcal for preggo ↑ 200 kcal for BF = 500 total kcal increase if lactating ↓ 300 kcal for bottle feeding = 200 kcal • Nutrition in breastfeeding –v- bottlefeeding: how many calories added? How many calories subtracted? o During lactation: Increase another 200 kcal/day after birth o Formula Feeding: Reduce intake after birth by 300 kcal • Pica: what is it? What can it cause? o Pica--Intake of non-nutritive substances (not food) o Cause: unknown o Ice, laundry starch, clay o May cause iron deficiency anemia o Nutritional & electrolyte imbalances → an apple a day o Pt edu: ▪ Edu as to the dangers to self & baby ▪ Monitor adeq wt gain for mom & baby ▪ Avoid constipation • ↑ water • ↑ fiber ▪ Med’s – last resort • How does culture affect nutrition? How do different diets affect nutrition? (example: Vegan, LactoVegan) o Culture ▪ Greek Orthodox No meat or dairy when fasting ▪ Muslim No alcohol, pork or pork products ▪ Orthodox Jewish----No shellfish, pork, or non-kosher meats ▪ Roman Catholic---No food one hr before communion No meat on Ash Wed, Good Fri, Fri during Lent; ▪ Buddhist or Hindu Generally vegetarian o Diets ▪ Lacto-ovo vegetarians • Dairy & egg products • “Teaching Topic”: Most vegans need additional supplements o Vitamins B12, D, calcium o Food Plate ▪ Lacto-vegetarians • No foods from animal sources • What are good foods for pregnant to eat? What foods would be good for an adolescent? Preggo: o Carbohydrates Source of energy & fiber (↑ BM) ▪ Inadequate amount –protein metabolism – ketosis ▪ Dairy, fruit, vegies, whole grains o Proteins--Amino acids for uterine & breast tissue growth ↑ to 60 mg/day ▪ Animal products – meat, fish, poultry, eggs o Calcium*--Mineralization of fetal bones & teeth ▪ 1000 to 1300 mg/day 4 cups of milk or dairy alternative ▪ Legumes, dried fruits, dark leafy vegetables o Iodine--Fetal thyroid gland function ▪ ↑ to 220 mcg/day--Iodine salt or prescribed supplement ▪ Most people get it through water & table salt o Vitamins Maintains good maternal health ▪ Vit A, D, C ↑ ▪ Prenatal vitamins prescribed o Iron* Growth of fetus, placenta, ↑ blood volume ▪ ↑ to 27 mg/day ▪ Lean meats, dark green leafy veggies (kale, spinach, collards), eggs ▪ Whole grains, enriched breads & cereals, Dried fruits, legumes, tofu, shellfish, molasses ▪ foods to increase or decrease absorption o Folic acid or folate*--Prevent fetal neural tube defects ▪ 400 mcg daily ▪ Fresh dark green leafy vegetables, liver, peanuts, whole grain breads &cereals o Drink Plenty of Fluids!! ▪ Fluid intake---8 – 10 glasses of non-caffeinated beverages o Mercury in Fish--Threat to nervous system of fetus ▪ Avoid Mackerel, swordfish, tilefish, shark - lrg fish or dirty fish ▪ Eat a variety of fish 12 oz/wk (over 2 + meals) o Salmonella ▪ Avoid ingestion of raw eggs, cake batter, eggnog & Caesar salad dressing, undercooked chicken, sushi, raw meats Adolescent: o Adolescent = 12 y/o o Recommended wt gain is same as for adult o Plus expected wt gain of the adolescent → wt gain of adolescent + wt gain of pregoo o Nutritional needs: o More* → calcium*, iron*, & folic acid* Chapter 13 – Lesson 9 • How is the adolescent affected by pregnancy? How can they prepare? Does anything need to be done differently than w/an adult pregnancy? How is nutrition in the adolescent? What foods would you expect them to eat? o adolescent = 12 y/o o Assess pregnancy wt, menarche, lifestyle o Low wt gain, eating d/o’s ▪ Normal for adol. To be concerned w/wt gain & appearance o Recommended weight gain → Same as adult pregnancy + the expected gain of the adolescent o Nutritional Needs ▪ More iron, calcium, and folic acid o Caloric Needs---Varies o Satisfactory weight gain indicative of adequate caloric intake o Nursing management: ▪ Encourage enrollment in classes – spec to adol preggo client ▪ Group counseling with other teens ▪ Individualized counseling as needed ▪ Emphasize impact of nutrition on her well-being and her baby ▪ Teens are often focused on the present only---Figure 13-3 Prenatal classes for adolescents. Young adolescents may benefit from prenatal classes designed for them. Chapter 14 – Lesson 9 • What are factors that indicate high-risk pregnancy – Tbl 10-1 o Anything that may be associated w/ negative pregnancy outcomes including psychological, physiological, sociodemographic, or environmental factors, pre-existing medical cond’s • Review Summary of Screening & Diagnostic Tests (pg 287) • NST (what is it?, what does it do?, when is it used?, how is it done?, how is it measured/judged?, what can be done if it is nonreactive?, how long is it done for?) o Non-stress test (NST) is an assessment of fetal well-being that analyzes the response of the fetal heart rate to fetal movement ▪ Advantages • Noninvasive • Easily interpreted • Can be performed in an outpatient setting at a low cost • A good indicator of fetal well being ▪ Disadvantages • Higher number of false positive results caused by fetal sleep cycles, medications, & fetal immaturity • Not a good predictor of poor fetal outcomes ▪ Test Procedure • Client is placed in semi-Fowler’s position & an ultrasound transducer & tocodynamometer are used to record contractions & fetal heart rate • In some settings, the woman is asked to press a hand held button when fetal movement is felt which makes a mark on the fetal heart tracing • W/ this information, episodes of fetal movement can then be compared to changes in the fetal heart rate • Acoustical stimulation can be implemented in the absence of fetal movement o Fetal acoustic stimulation &vibroacoustic stimulation are used to stimulate the fetus while an NST is performed o The noninvasive sound &vibrations shorten the time for the NST ▪ Findings • The test is considered normal (reactive) if there are 2 or more accelerations of 15 beats per minute lasting for 15 seconds over a 20 minute period, the baseline is normal & the long-term variability of 10 or more beats per minute is present • If these criteria are not met w/in 40 minutes, the test is considered nonreassuring (nonreactive) & further testing is indicated o RN Int: give mom juice, cracker, or stimulate baby w/ vibroacoustic stimulator to wake baby, monitor add’l 20 min (40 min max), if non-reactive – notify MD • CST (what is it?, what does it do?, when is it used?, how is it done?, how is it measured/judged?, what can be done if it is positive?, how long is it done for?) o Contraction stress test (CST) o assesses the ability of the fetus to w/stand stress of uterine contractions & is a means of evaluating placental capacity for oxygen/carbon dioxide exchange o Since contractions reduce blood flow to the fetus, the CST can be used to predict a fetus that may not be able to tolerate the stress of labor ▪ Indications • Factors that place the fetus at risk for asphyxia such as intrauterine growth restriction, diabetes, postdates, nonreactive NST, & biophysical profile score less than 6 ▪ Contraindications • Third-trimester bleeding & previous cesarean birth w/ classical uterine incision • The advantages of the CST should be weighed against the danger of preterm labor in situations where this is a risk such as premature rupture of membranes or incompetent cervix ▪ Test Procedure • After the test procedure is explained to the client & informed consent is obtained, electronic monitoring of contractions &fetal heart rate are begun • After a baseline fetal heart tracing is obtained, contractions (if not occurring spontaneously) are initiated w/ intravenous oxytocin or breast self-stimulation ▪ Findings • When a pattern of at least 3 contractions of 40 to 60 second duration in a 10 minute time period is obtained, the fetal heart rate pattern is assessed • The test is reassuring (negative) if no late decelerations occur o RN Int: Once 3 contractions in 10 min → STOP oxytocin (Pitocin) • The test not reassuring (positive) if there are late decelerations w/ at least 50% of contractions o RN Int: If + → prep for C/S • The test is suspicious (equivocal) if there are intermittent late decelerations, significant variable decelerations, decelerations in the presence of hyperstimulation • Further assessment is needed w/ these results • BPP (what is is?, what does it measure?, when is it done?) o Biophysical profile is a method of assessing fetal well-being ▪ i.d’s compromised/healthy fetus ▪ assesses placental fxn o scores on five criteria including: ▪ Fetal breathing movements ▪ Fetal body movements ▪ Fetal muscle tone ▪ Fetal heart rate reactivity ▪ Amniotic fluid volume o The total score ranges from 0-10 ▪ If the findings for a criterion are normal, a score of 2 is given for each one ▪ If the findings are abnormal a score of 0 is given ▪ A total score of 8-10 is considered normal ▪ A score of 4-6 is interpreted as possible abnormal ▪ A score of less than 4 may indicate a need for delivery • Amniotic fluid values: What is normal? What is hydraminos? What is oligo? o AFI > 24cm = hydraminos (excess amniotic fluid) o AFI < 8 cm = oligohydramnios (deficient amniotic fluid) • CVS &PUBS (chorionic villus sampling &percutaneous umbilical blood sampling): What is each one? How is the procedure performed? What is being looked for? o Percutaneous Umbilical Blood Sampling & Chorionic Villus Sampling – PUBS or CVS ▪ Sample of umbilical blood - Small sample of chorionic villi ▪ Transabdominally or transcervically ▪ Products of conception tested directly – tests are exact ▪ As early as 8 to 10 weeks ▪ Test for genetic (1°), metabolic d/o’s ▪ Only done if problem or ↑ maternal age • Ex: 1st baby has down’s syndrome, 2nd preggo = PUBS test • ↑ r/o miscarriage, infxn ▪ RhoGAM PRN • Due to invasive testing • Blood can cross • Indirect Coombs Test o Indirectly check on mom o Detects presence of Rh antibodies in maternal serum ▪ If non-sensitized (negative) ▪ RhoGAM immunoglobulin at 28 wks Chapter 15 – Lesson 12 • Diabetes in pregnancy (both chronic & gestational) • Care, diagnosis, meds, symptoms & fetal risks associated w/ diabetes in pregnancy &during intrapartum/postpartum periods: How is it diagnosed? What should lab values be? How is it treated? Meds used? What should glucose levels be? How is mom affected? How if fetus affected? o Definition ▪ Endocrine d/o of carbohydrate metabolism ▪ Glucose metabolism is impaired ▪ Cells break down stores of fats & protein for energy ▪ Result: Negative nitrogen balance & ketosis o Classifications of DM ▪ Gestational Diabetes Mellitus (GDM) – dx w/DM S&S during preggo • Effect of Pregnancy on Glucose Metabolism: #1 problem during pregnancy is balancing insulin & glucose levels → glucogen builds up • 1st ½ of pregnancy - ↑ insulin production → glycogen stores o ↑tissue response to insulin o Fetal needs are minimal o Client eats less (N/V) • 2nd ½ of pregnancy – insulin resistance o Insulin needs begin to rise due to Human placental lactogen (hPL) ▪ hPL = insulin antagonist o Causes resistance to maternal insulin o Metabolism of fat instead (lipolysis) - ketones in urine (mom) o Results in ↑ circulating glucose for fetal use - glucose in urine (mom) o ↑ demand of maternal pancreas to make more insulin – to ↓ glucose o Baby will be hyperglycemic upon birth bc it is still making insulin • Influence of Diabetes on Pregnancy Outcome: o Maternal effects: ▪ Hydramnios – excessive amniotic fluid b/c - ↓ BG → ↑ thirst → ↑ urination in mom & fetus • Due to frequent fetal urination • Premature rupture of membranes (PROM) • Preterm labor ▪ Preeclampsia - eclampsia • Hypertensive d/o’s due to vascular changes • Goes hand in hand w/ diabetes ▪ Ketoacidosis • ↑ ketones which are acidic - from the breakdown of fats • ↓ gastric motility • Untx’d → coma & death of mom & fetus (just like regular diabetic patient) ▪ Infections • Yeast infections • UTI ▪ Can progress to DM1 & DM2 later in life o Effects of DM on Fetus: ▪ Produces own insulin – in resp to ↑ BG levels ▪ Obtains glucose from the mother ▪ ↑ maternal glucose stim’s fetal pancreas to make own insulin ▪ Macrosomia: > growth, > shoulder dystocia, C/S ▪ Big Mac Babies – bruising on face ▪ Hypoglycemia after birth: 2-4 hrs after umbilical cord cut ▪ Hyper-bilirubinemia – jaundice • Result of polycythemia (RBCs) ▪ Respiratory distress syndrome (RDS) • Insulin inhibits enzymes for surfactant dev • Delayed fetal lung maturity • Predisposed to RDS ▪ ↑ in incidence of congenital anomalies • Heart • CNS Sacral agenesis • Assessment of GDM o Risk factors • Skeletal system (sacral agenesis – lower portion of spine fails to dev) ▪ Over 40 y/o ▪ HTN ▪ Glycosuria ▪ Family w/ DM ▪ Maternal obesity – BMI < than expected ▪ Unexplained stillbirth ▪ Previous Large for Gestational Age (LGA) infant ▪ Chronic HTN o Assess for Hyperglycemia → my 3 Aunt Polly’s always eat sugar! ▪ Cardinal S/S of DM • Polyuria – ↑voiding • Polydipsia--- ↑ thirst • Polyphagia--- ↑hunger • Weight loss ▪ Symptoms • Blurred vision • Recurrent infections • Asymptomatic or very mild symptoms • ↓ wound healing • Tingling in hands • Clinical Therapy o Goal: Scrupulous maternal plasma glucose control o If pre-gestational diabetic, should receive extensive pre-conception counsel o Screen all women o 24-28 weeks ---If + risk factors, should be screened earlier • Lab & Diagnostic tests o 1-hour Glucose Tolerance Test (GTT) ▪ Drinks 50-g oral glucose solution ▪ Provides blood sample 1 hr later – non-fasting ▪ Abnormal finding • 1 hour sample is > 140 mg/dL = abnormal • Further testing indicated o 3-hour 100 –g oral GTT Preparation Required ▪ High carb diet x 3 day prior; Fast for 8 hrs prior to test ▪ Fasting serum glucose level drawn in AM ▪ Diagnostic lab values for 3h 100 –g GTT ▪ Plasma glucose levels drawn at 1, 2, & 3 h ▪ If borderline – will repeat in 1 month o Blood glucose monitoring ▪ Weekly fasting levels ▪ Postprandial levels - 2h after meals ~ 4x per day – waking, breakfast, lunch, dinner ▪ Self-monitoring ▪ Diet & insulin ▪ bed time snack to not bottom out during middle of night ▪ carb’s & protein → prevent hypoglycemia • 20-30 protein • 40-60 complex carbs • 25-40 fat ▪ May need insulin ▪ Oral hypoglycemic rarely used – last resort o glyburide (DiaBeta) can be administered ▪ fasting < 95 ▪ postprandial < 120 ▪ can control w/ diet - insulin not required o Glycosylated hemoglobin ▪ HbA1c blood test ▪ Provides long-term control information ▪ Previous 4-8wks ▪ Measures % of hgb w/ glucose bound to it ▪ Result > 10% - infant at risk for malformation - ♥, spinal, CNS prob’s in infant ▪ Need A1C to be < 10% ▪ Not reliable for gestational diabetic screening • Exercise o Same type &amount of exercise - ↑ glucose metab • Begin gradually if just beginning o Every day to prevent Blood Sugar fluctuations • After meals (when blood sugars are high) • Observe for s/s of hypoglycemia → cold, clammy → needs some candy o Hunger, clammy skin, irritability, slurred speech, seizures, tachycardia, h/a, pallor, sweating, disorientation, shakiness, blurred vision • Neumonic TIRED – Tachycardia, Irritability, Restless, Excessive Hunger, Diaphoresis/Depression o If untreated, coma or convulsions o BG < 60, take 20 g of carbohydrate – complex – peanut butter o Wait 20 minutes & retest o If still low, 20 grams again o Wait 20 minutes o If still low, call doctor o Fetal Well-being w/ DM mother ▪ MSAFP- maternal serum alpha-fetoprotein o strongly recommended 16-18 wks --> neural tube defects – anencephalic – no brain, just brain stem o if MSAFP is ↑, further testing → indepth U/S, amniocentesis ▪ Ultrasound to rule out cardiac or other physical anomalies around 18 weeks o Closely monitor size of fetus 18 weeks & 28 wks ultrasounds ▪ *Follow up visits twice a month during 1st & 2nd trimester ▪ *Weekly visits during 3rd trimester *Different from normal preggo ▪ Might undergo NST weekly at 28 weeks, 32 weeks twice a week o Management During L&D ▪ Commonly induced @ 37-38 weeks o To reduce injury to baby – remb - Big Mac Babies ▪ Diet controlled- no special needs during labor ▪ Insulin controlled --Need continuous insulin infusion during labor (finger stick every hour, change rate of infusion depending on glucose level) --IV insulin D/C’d at end of 3rd stage (delivery of placenta) ▪ Insulin requirements fall during postpartum - bc horm’s causing GDM are gone o Managed w/ sliding scale – rarely req’d ▪ Encourage breastfeeding ▪ Anti-hyperglycemics contraindicated – no BF w/oral insulin • Nursing care plan (pgs 312-314) • Anemia in pregnancy (know specific values &types; know maternal/fetal implications for each) (Table 15-4) o Most common medical d/o of pregnancy o Affects 20% pregnant women o Inadequate levels of hemoglobin ▪ r/t inadeq blood vol –Hgb < 10 o Results in reduction of the O2-carrying capacity of blood o Less than 11 during 1st & 3rd, less than 10 during 2nd o ♥compensates w/↑ cardiac output ▪ Iron Deficiency Anemia • 90% of cases of pregnancy anemia • Results in pathological anemia of pregnancy • Iron is actively transported across placenta • W/out iron therapy, well-nourished pregnant women will have an iron-deficit • Diet alone cannot replace gestational iron loss – PNV has iron • Causes: o Inadequate iron intake - diet o Increased need for Fe - ↑ blood vol o Closely spaced pregnancies - recommended – preggo’s 18 mo’s apart o Heavy menstrual flow • Maternal Implications o Activity intolerance o Weakness, Fatigue, Paleness, Dizziness, Lightheadedness o Hemoglobin (Hb) < 10 or Hct < 32% o Risk for: ▪ Infection, preeclampsia, ▪ Postpartum hemorrhage, ▪ Delayed episiotomy or incision healing • Fetal Implications o Low birth weight, Prematurity o Hypoxia during labor - ↓ O2 ▪ Impaired uteroplacental oxygenation o Stillbirth ▪ Increases w/ Hgb less than 6 - chronically • Management o Teach prevention o Foods↑ in iron – organ meats & dark leafy greens o Iron supplements ▪ Divide in 2-4 doses ▪ Take w/ orange juice – ↓ absorption bc of vit c ▪ Avoid caffeine drinks & milk – ↓ absorption o Teach how to deal w/ side effects – dark tarry stools & constipation ▪ Sickle Cell Anemia • Sickle Cell disease o Abnormal crescent-shaped (sickled) RBCs o Not deficient in iron • Occurs primarily in African-Americans • Mediterranean ancestry o Greeks, Italians, Arabs, Turks • Autosomal Recessive inherited d/o - genetic • Symptoms o Pain in extremities, joints, &abdomen o Fever o Recurrent attacks, ↑during pregnancy – Due to added strain on body • Maternal implications o Due to vascular occlusion – RBC accumulates in tiss’s = hypoxia o Tissue hypoxia, edema, RBC destruction o Risk of maternal infections ▪ UTI, pulmonary infections ▪ CHF, renal failure, leg ulcers, preeclampsia • Fetal Implications o Abortion - spontaneous o Fetal death o Prematurity o Intrauterine growth restriction (IUGR) • Management o Prevention of crisis – best management - Focus: hydration & infxn ▪ Drink 10-12 glasses/day of water --Dehydration & fever can cause crisis ▪ Seek treatment w/ early symptoms of infection – immed see MD o Reduce anemia & maintain good health ▪ Folate supplements ▪ Foods – green leafy vegetables, red meat, liver, fish, poultry, legumes, yeast - ↑ iron!!! o Prophylactic transfusions o During labor ▪ Assess FHTs, Admin O2, Admin intravenous fluids, Epidural for pain control – All to ↓ r/o crisis • Heart disease in pregnancy (symptoms, causes, care, meds) o Complicates about 1% of pregnancies o Pregnancy ↑: ▪ ↑Cardiac output ▪ ↑Heart rate ▪ ↑Blood volume o Heart disease – don’t have to know ▪ ↓ cardiac reserve ▪ Diminished capacity to handle pregnancy workload in ♥ o Heart D/o’s ▪ Congenital heart defects • Atrial septal & ventricular septal defects • Patent ductus arteriosus • Coarctation of the aorta • Tetralogy of fallot ▪ Rheumatic heart disease • Mitral stenosis ▪ Mitral valve prolapse • Peripartum cardiomyopathy - enlargement of the ♥ during prenatal period o Heart Disease Symptoms ▪ Dyspnea, SOB, Chest pain ▪ Exhaustion ▪ Pulse irregularities ▪ Peripheral edema (Other than feet & ankles) ▪ Any hx of heart disease? ▪ Watch for signs of heart failure @ blood volume peak (28-32 weeks) – close monitoring o Clinical Therapy ▪ Diagnosis • Echocardiogram & chest x-ray • Auscultation of heart sounds • Sometimes cardiac catheterization – last resort • Proper positioning of the client – semi-fowler’s position o Heart Disease Management ▪ Rest frequently --Well-balanced diet ▪ Medication • Digitalis • Fe supplements • Antibiotics • Lasix • Heparin ▪ Continual evaluation of edema ▪ Emotional support o Nursing Management ▪ Assess the stress of pregnancy on the heart’s functioning ▪ Limitation of activity • Monitor for signs of impending cardiac failure • S&S: crackles, frothy sputum, SOB, profound edema ▪ Health teaching • Evaluate maternal vital signs ▪ Maintain an atmosphere of calm - ↓ anxiety ▪ Fetal assessment - NST ▪ Family support o Nursing Management in L&D ▪ Should receive antibiotics during labor/birth (due to risk of endocarditis) ▪ Epidural - ↓ pain; remb: pain = ↑ BP ↑ Pulse ▪ Most critical after delivery of placenta • extra volume in her body, no longer going to baby, not perfusing to baby ▪ Ambulate early ▪ TED stockings o Impact on Mother & Pregnancy ▪ All women w/ chronic medical conditions ▪ Need ↑ vigilance ▪ May ↑ risks to the newborn ▪ Premature birth ▪ Low birth weight ▪ Growth retardation • Asthma in pregnancy (Table 15-6) o Bronchial asthma is a respiratory illness o Response to stimulus ▪ Narrowing of airways o Causes ▪ Allergens ▪ Temperature changes ▪ Emotional tension ▪ May be unknown o Can become a major problem w/ pregnancy – 4% of preggo women – ½ improve, ¼ same, ¼ worsen ▪ Severity ↑during 29-36 wks – uterus is at it’s largest • ↓ O2 to fetus • IUGR – small babies • Preterm births o Management ▪ Ultimate goal is to prevent hypoxic episodes ▪ Relieve acute attacks ▪ Prevent or limit later attacks ▪ Adequate maternal & fetal O2 ▪ Eliminate environmental triggers • Dust mites, animal dander, pollen ▪ Drug therapy • Bronchodilators ▪ Acute episodes • Albuterol, steroids, aminophylline, Brethine (terbutaline) • Almost all asthma meds considered safe during pregnancy ▪ Pulse oximetry & oxygen during labor Chapter 16 – Lesson 13 Bleeding during pregnancy: what are risks to mom & fetus • ↓ O2 carriying capacity • Maternal Risk: o ↑ anemia o ↑ infxn o ↑ preterm labor o ↑ preterm delivery • Fetal Risk: o ↑ blood loss or anemia o ↑ hypoxia o ↑ anoxia – completely w/o O2 o ↑ preterm birth • Causes: o Abortion o Ectopic preggo ***all hemorrhagic cond’s are med emergencies → can bleed out 8-10min Abortion: what is it, what kinds are there (spontaneous & induced), what are causes of each kind, what are the classifications of spontaneous abortions (Figure 16-1, page 332 [3rd; Figure 16-1, page 325 [4th]), what happens to mom during each kind of spontaneous abortion (symptoms, pain, bleeding, cervix, etc), general abortion symptoms, clinical therapy (hcg levels, US, medicine), nursing management ● Abortion Definition - Expulsion of fetus before viability o Expulsion of the fetus before 20 weeks’ gestation (our focus for abortion) --Expulsion of fetus less than 500g o Spontaneous: Occur naturally o Induced: Caused by medical or surgical means Abortion Symptoms ▪ Vary based on # of wks gestation ▪ Pelvic cramping and Backache --Reliable indicators ▪ Spotting or bleeding ● Unrelated to polyps or cervical irritation/erosion may include clots & tissue ▪ Cervical dilation ● Cervical os may be opened or closed depending on type of miscarriage • Spontaneous Abortion (miscarriage) o Causes: ▪ Chromosomal abnormalities • Majority of early miscarriages (< 12 wks) ▪ Implantation abnormality (can impact anywhere in uterus or cervix) ▪ Weakened cervix ▪ Teratogenic drugs ▪ Endocrine imbalances • Corpus luteum fails to produce hormones; Insulin dependent diabetes mellitus (IDDM) ▪ Trauma to mother • Gun shot wounds MVA’s ▪ Maternal infections and diseases →STI’s, Lupus o Classifications of Spontaneous Abortions – Fig 16-1; pg. 332 A. threatened; B. inevitable; C. incomplete; D. complete; E. missed ▪ A. Threatened hasn’t happened yet; can be stopped (usually w/bed rest) o Closed cervical os --Maybe mild cramping, backache --Placenta still attached o Spotting, some bleeding occurs ▪ B. Inevitable or imminent gonna happen; can’t be stopped o Bleeding increased - Moderate to heavy bleeding o Mild to severe cramping o Cervical os open (dilated) o Often membranes rupture o Placenta has separated from uterine wall ▪ Passage of products of conception will occur (complete) : Embryo or fetus, placenta, membranes ▪ Partial or complete expulsion ▪ C. Spontaneous Abortions: Incomplete o Heavy, profuse bleeding o Severe cramping o Slight Cervical dilation o ROM o Expulsion of fetus; Lost baby but Retained products of conception o Retention of placenta (usually) → Hemorrhage possible ▪ D. Spontaneous Abortions: Complete o Slight bleeding o Mild uterine cramping o All products of conception passed - lost baby & placenta. Everything came out o Cervix closed ▪ E. Missed Abortion o Fetus has died but not expelled →May be no bleeding or cramping o May report brownish vaginal discharge o Cervix closed --Products retained in utero several wks o Diagnosis: ▪ ↓ signs of pregnancy • Negative pregnancy test, ↓ uterine growth, ↓ breast changes ▪ Confirmed by ultrasound o Usually expelled spontaneously w/in 4-6 wks → If not expelled after 6 wks, hospitalization o 1st trimester - Dilation and curettage (D&C) or suction evacuation o 2nd trimester – labor induced or D&C ▪ Recurrent (Habitual) - Spontaneous o Loss of 3 or more consecutive pre-viable pregnancies o 25 – 30% chance of recurrent miscarriage ▪ Septic abortion - Spontaneous o Infection is present o May occur with the following: ▪ Unrecognized prolonged rupture of membranes; ▪ Pregnancy with intrauterine device (IUD) ▪ Abortion by unqualified persons Clinical Therapy ▪ hCG levels --↓ slowly; cannot confirm fetal/embryonic death ▪ Ultrasound: o Presence of viable gestational sac, fetal heart beat ▪ Medical therapy: o Bed rest and abstinence from sex (especially if there is a threatened abortion) o Sedation PRN (to ↓ activity) o Persistent bleeding →Hospitalization o IV therapy or blood transfusions o D&C or suction evacuation (output) Abortion: Nursing Management ▪ After abortion, she is considered post-partum – same treatment ▪ Assess vital signs o Assess FHT if 10-12 wks o Assess pain ▪ Assess for bleeding and infection o only threatened & missed have closed cervix but missed also still has the fetus inside o Fetus is now a foreign object → immune system will attack o Can have stone baby – layers of calcium deposited around the fetus inside mother. o All but threatened miscarriage can lead to infection o Monitor closely after D&C ▪ Anemia Hgb < 11g/dl; WBC count > 12,000/mm3 o Can become septic (blood culture!!)- Fever, abd tenderness, malodorous vaginal bleeding ▪ Assess coping mechanism and family response o Shock, disbelief, sadness, guilt or anger ▪ Provide analgesics ▪ Explain procedures prn ▪ Provide emotional support after loss ▪ Refer to other HCP, support groups o Grieve for 6 – 24 months ▪ Administer RhoGAM within 72 hours --Indicated for Rh negative clients if not sensitized Ectopic pregnancy: what is it, where does it most commonly occur, what are causes, what symptoms might the woman have, what kind of medicines might be ordered (review Methotrexate), what kinds of surgery(s) might she have, if she has surgery what is the care afterwards Ectopic Pregnancy (EP) • Definition --Implantation fertilized ovum in site other than uterus • Most common site - fallopian tubes (tubal pregnancy) • Initially symptoms of pregnancy exhibited • hCG present in blood • Chorionic villi grow into tube wall or other site -Various Implantation Sites EP Causes • Tubal damage, PID, endometriosis • Previous tubal surgery or EP • Congenital abnormalities of tube Clinical therapy • Determine LMP, pelvic exam • Progesterone 5-25 ng/mL (remember: nonviable < 5 mL; viable > 25 mL) • Transvaginal ultrasound → will see nothing in uterus • Rupture of fallopian tube and bleeding into the abdominal cavity occurs o Result is sharp unilateral pain and syncope; Referred shoulder pain, rigid abdomen o Lower abdominal pain, tender adnexal mass; Vaginal bleeding • Medical therapy: o IM methotrexate if future pregnancy desired ▪ methotrexate – used for Rheumatoid Arthritis ▪ destroys rapidly dividing cells w/in the fallopian tube. ▪ This preserves the fallopian tube for future pregnancies • Surgical therapy: o o (if non-ruptured fallopian tube) (if ruptured, remove tube) Ectopic Pregnancy Diagnosis & Management • Ectopic Pregnancy Management • Dependent on signs and symptoms → Goal is to maintain fertility and tube Treatment • Nonsurgical -methotrexate • Surgical o Unruptured – removal of products of conception o Ruptured – removal of tube Nursing Management • Monitor VS, pain, and vaginal bleeding; Inform what to expect, coping abilities ; IV access, consents • Pre/Postoperative care: o Watch for bleeding and infection o Administer analgesics & their effectiveness o Provide grief support • Methotrexate recipients: o Advise of mild abdominal pain X 24-48 hrs o More severe pain → evaluation needed o May need 2nd dose if needed, can mean ectopic pregnancy has not resolved o Report heavy bleeding, dizziness, tachycardia (Methotrexate SE’s) – o Return to office for F/U hCG testing Hyperemesis gravidarium: what is it, when does it usually occur in pregnancy, what symptoms might mom have, causes, maternal/fetal risks, how is it treated, nursing management First Trimester Metabolic Conditions • Conditions affecting the physiological integrity of nutrition: o Hyperemesis gravidarum o Anemia o Fe-deficiency o Sickle cell Hyperemesis Gravidarum • Intractable, excessive vomiting --During 1st half of pregnancy o Dehydration, wt loss ---Fluid and electrolyte imbalance, ketosis r/t imbalanced glucose o look @ alkalosis & Acidosis pics • Weight loss > 5% of pre-pregnancy body weight • Cause- theories: o High estrogen levels or hCG o Liver dysfunction o Vit B deficiency o Psychological (emotional factors) and social factors • Fetal risks: o IUGR (↓ nutrition o CNS malformation (↓ vitamins) o Fetal death • HG management: o Goals: Relieve nausea & vomiting → Resume normal appetite o Admin: Antiemetics; Parenteral nutrition - IV fluids with vitamins & minerals o NPO at first, then CL once N/V subsides o When responding well - limited oral fluids, bland diet ▪ High protein, low fat for optimum fetal growth o Assess: amount/color of emesis --- monitor I&O, weight, emotional status o Non-pharm mgnt: positioning, quiet, ↓ odors that cause N/V GTD: What is it, how does it develop, how does it affect a pregnant person, what kinds are there, what are the S/S of each, which one has higher occurrence of resulting cancer, what is the follow-up Gestational Trophoblastic Disease (GTD) → Molar pregnancy • 2nd Trimester Hemorrhagic Conditions • Cond Affecting Oxygenation 2nd trimester • Incompetent cervix • Abnorm dev of placenta • Pathologic proliferation of trophoblastic cells (i.e. Hydropic vesicles ) • Includes : o hydatidiform mole o Invasive mole (chorioadenoma destruens) o Choriocarcinoma, a form of cancer • Higher risk in early teens and over 40 • Etiology: Unknown, may be ovum defect or nutritional deficiency • Types of molar pregnancies : o Complete mole (classic mole) ▪ Fertilization of empty ovum (without nucleus) ▪ Sperm duplicates self ▪ Embryo dies early ▪ Assoc’d w/ choriocarcinoma (i.e. cancer) o Partial mole usually found after miscarriage ▪ 2 sperm or one sperm with 46 chromosomes fertilize normal ovum; 69 chromosomes ▪ Embryonic or fetal parts and amniotic sac noted ▪ Usually multiple anomalies ▪ Little chance of survival ▪ Noticed after miscarriage o Invasive mole - Similar to complete ▪ Involves uterine myometrium • GTD Signs & Symptoms • Initially, clinical picture similar to pregnancy • Classic signs: o Uterine enlargement greater than gestational age (fluid filled cells causes uterine enlargement) o HCG extremely ↑ o Vaginal bleeding ▪ Red or brown bleeding – (prune juice), bright red, scant or profuse, few days to wks o Hyperemesis gravidarum o HTN before 24 weeks • GTD Management o Confirm by US (ultrasound) - Most moles pass spontaneously o Remove molar tissue PRN ▪ 1st trimester – D&C ▪ 2nd trimester – Hysterotomy, hysterectomy o Admin: Rh immune globulin (RhoGAM) PRN if Mom is Rh - ▪ Closely monitor for one year DO NOT GET PREGGO!! ↑ r/o cancer for 1 yr ▪ Frequent physical and pelvic exams • HCG levels monthly X 6 months, ▪ then Q 2months for add’l 6 mos. = 1yr total ▪ Methotrexate PRN to stop proliferation of cells, to ↓ r/o cancer Incompetent Cervix: what is it, how does it affect pregnancy, treatment for it, S/S associated with it, nursing tx of cerclage Incomplete Cervix: • Cervix dilates prematurely → Usually in the 4th or 5th month • Assoc’d w/repeated 2nd trimester abortions • Possible causes: o Cervical trauma o Infection o Congenital cervical or uterine anomalies o ↑uterine volume o multiple gestations! • Dx: Positive hx of repeated 2nd trimester abortions • May not have spotting or bleeding • Pelvic exam reveals dilatation, bulging membranes through cervix • Usually painless, No contractions • Incompetent Cervix- Management o Cervical cerclage – Shirodkar procedure ▪ Reinforces the weakened cervix ▪ Purse-string suture is placed in cervix w/ needle & string – supports & closes cervix o Done in 1st trimester or early in 2nd trimester o Cesarean birth may be planned o Suture may be cut at term and vaginal birth permitted → Removal (of cerclage) @ 38-39 weeks • Nursing Management for Cerclage o Instruct to monitor for signs of preterm labor o Report contractions prior to 38 wks o Immed report rupture of membranes o Report any vaginal leakage HTN: study each kind (GHTN, chronic, mild and severe preeclampsia, ecclampsia, transient); know S/S of each one; know any associated labs of each one; know management/treatment of each one, medications) (Review Nursing Care Plan, Pg 344-346 [3rd] for TEST focus on GHTN, preeclampsia (mild/severe), & eclampsia Definition of HTN: BP = or > 140/90; Diastolic > 90 Incidence: HTN occurs in 10% of pregnancies --Major cause of maternal mortality Remember diurnal rhythms affect BP Pregnant women may develop several hypertensive states • Gestational hypertension • Preeclampsia • Mild preeclampsia or Severe preeclampsia • Eclampsia • Chronic HTN • Chronic HTN with preeclampsia or eclampsia Gestational HTN • Previously known as = Pregnancy Induced HTN (PIH) • Initially noted after 20 wks • NO protein in the urine • Defn: BP 140/90 or ↑ --On 2 occasions - At least 6 hrs apart • Gestational HTN WITHOUT protein in urine Gestational HTN Risk Factors • Patients at risk: < 17 y/o or > 35 • Poor prenatal care • Lower socioeconomic group • Maternal disease o Renal (HTN) o Cardiac (GHTN) - Preeclampsia • Defn: Gestational HTN (GHTN) BP of 140/90 or higher- On 2 occasions - At least 6 hs apart - After 20 gest wk o If proteinuria before 20th week --pathologic changes in the placenta, i.e., hydatidiform molar pregnancy. • GHTN WITH protein in urine - proteinuria • Most common HTN disorder in pregnancy: o Last 10 wks of pregnancy o During labor o First 48 hrs following delivery o A progressive disorder → from mild to severe ▪ remember: it is ALWAYS a progression - pre-eclampsia → mild pre-eclampsia → severe pre- eclampsia → eclampsia → etc…….. Mild preeclampsia: Signs & Symptoms • D/o can b/g w/implantation • Defn: GHTN: BP 140/90 + protein • UNDERLYING PATHOPHYSIOLOGIC CHANGES CAN PRECEDE S/S BY WKS OR MONTHS!! • look at Edema, Protein, & weight gain o Edema 1+ - 2+ o Proteinuria 1+ - 2+ (can appear late in disease) o Wt gain- 3lbs in 24 hrs or 4 lbs in 3 days Severe Preeclampsia: S&S • Defn: BP 160/110 or higher while on bedrest --2 occasions at least 6 hrs apart • Edema 3+ 4+ --Proteinuria 3+ - 4+ --2 random samples, at least 4 hours apart • Oliguria (small amount, concentrated urine) • Visual or Cerebral disturbances • H/A, vision changes, scotomata (organs are involved) • Impaired liver function -Epigastric pain (liver is enflamed) • Hyper-reflexia 3+ - 4+ • N/V • Spike in fever up to 102 – 103 • Pulmonary edema, cyanosis • Low platelet count (<100,000)--Normal – 150,000 to 350,000 Eclampsia is untreated preeclampsia • Most severe form of pre-eclampsia - can be treated w/proper GHTN & preeclampsia management • Generalized seizures or coma • Life-threatening, medical emergency • Can occur any time in pregnancy o Antepartum --Intrapartum – during labor --Early postpartum • Pre-eclampsia superimposed on chronic HTN • Eclampsia superimposed on chronic HTN --(the worst possibility) Transient HTN • Defn: GHTN with no signs of preeclampsia - No proteinuria --Occurs the first time after mid-pregnancy - After 20 weeks • --BP returns to normal < 12 wks after birth Chronic HTN Disorders – National Institute of Health • Chronic HTN --The most manageable • Hx of HTN (140/90 or higher) --Before pregnancy --Before the 20th week gestation --Past 42 days postpartum Pregnancy Complicated by Chronic HTN • Untreated HTN affects the baby -- as well as the mother • Damages blood supply → Affects placental exchange → Ages placenta prematurely o IUGR babies small babies because placenta ages prematurely Chronic HTN management • Prevent preeclampsia!!!!! • Ensure normal fetal growth o visits every 2 wks until 28 wks, then weekly o Ultrasound in 2nd and 3rd trimesters • Antihypertensives generally used - BP > 160/110 --methyldopa (Aldomet) no ACE inhibitors!! • 24 hour urine, serum creatinine --Diet (↓ sodium, ↓ fat), rest Women at Risk for Preeclampsia • Young 1st time pregnancy, teen • GTD • Hx of renal disease or chronic HTN • Twin pregnancy • Diabetes • Hx of preeclampsia • African Americans • Women over 35, especially primigravidas (1st baby) Women at risk for Eclampsia • Convulsions not caused by a neurologic disease (caused by ↑ BP). • Clinical presentation also meets criteria for preeclampsia. • Progressive worsening of preeclampsia HELLP syndrome: know what it is, how is it diagnosed, lab values, treatment HELLP Syndrome → life threatening Remember: it is ALWAYS a progression – chronic HTN → preeclampsia → eclampsia → HELLP • HTN state with symptoms in addition to preeclampsia. • Presents late 2nd or early 3rd trimester • Multiple-organ-failure syndrome • Poor maternal and perinatal outcomes • Lab diagnosis o Can only be diagnosed from lab values H - Hemolysis • Microangiopathic hemolytic anemic Fragmented RBCs – occur when passing through constricted, damaged blood vessels EL - Elevated liver enzymes • Caused by obstructed blood flow --Liver distention, epigastric pain -Hyper-bilirubinemia LP - Low platelets ---< 100,000/mm3 (pre-eclampsia) – thrombocytopenia Severely low < 50,000 • Platelets aggregate at damaged vascular sites and vasospasm Women at risk for HELLP • > 36 weeks gestation • White, multiparous • >25 wks gestation • Excessive weight gain • Pitting generalized edema Treatment of GHTN’s • Prevent convulsions (i.e. eclampsia) (MgSO4 prevents seizures!!! – Review drug info!!!!) • Maintain adequate kidney function • Monitor fetal status continuously for signs of utero-placental insufficiency • Stabilize the woman so birth can be accomplished • Definitive treatment --DELIVERY!!! GHTN treatments (Home) • Office visits twice a week (same for DM pt) • Bed rest • Frequent lab work • Fetal surveillance GHTN treatments (hospital) • Intense maternal monitoring (continuous) • Anticonvulsant medication (MgSO4) • Antihypertensive medication • EFM: Electronic Fetal Monitoring preferably internal (more accurate monitoring) • Nurse-to-patient ratio of 1:1 --VS q 15-30 minutes • Place woman in lateral recumbent or semi recumbent position (lying on side, off of back) -- • Hourly I/O (Foley) • ↓ stim from noise and light • IVF’s • Laboratory workups o Testing urine q 1 hour for protein • Assess hyper-reflexia q 1 hour • Have emergency equipment ready • Administration of magnesium sulfate (IV) --NEVER LEAVE PT ALONE!! HELLP Management • In addition to preeclampsia management • Monitor platelet count • Assess for clinical signs of bleeding • Administer blood products Evaluation • Minimal or decreased blood loss • Delivery of healthy newborn DIC: review • DIC = Disseminated Intravascular Coagulation → Complex clotting disorder • Predisposing risks: • Severe hemorrhage • Infection -Prolonged intrauterine fetal demise Common cause: sepsis, infxn • Assess for 1st signs- pallor, cold wet skin, oliguria, anxiety (these are S&S’s of hypovolemic shock) • FHT tachycardia and deceleration of heart beat • Correct hypovolemia o IV Fluids --NS or LR -PRBC o Platelets o Fresh frozen plasma • NO fibrin!!! Can bleed to death. Fibrin is deposited in tissues. None left to coagulate. • Overproduction of fibrin: deposited in tissues → tissue necrosis →bleeding because cannot clot • Insert Foley catheter- for hourly output • Administer O2 for fetus • Warmth for mother at 1st sign • Stop bleeding if possible --May not be possible • Maintain circulation volume --Elevate legs to ↑ perfusion to ♥ • Start IVF’s or increase rate • Prevent infection (antibiotics) → blood culture. Start on broad spectrum until results come back. Then treat with appropriate antibiotic specific to that bacteria [Show More]
Last updated: 2 years ago
Preview 1 out of 45 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$12.50
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
May 09, 2021
Number of pages
45
Written in
Additional information
This document has been written for:
Uploaded
May 09, 2021
Downloads
0
Views
67