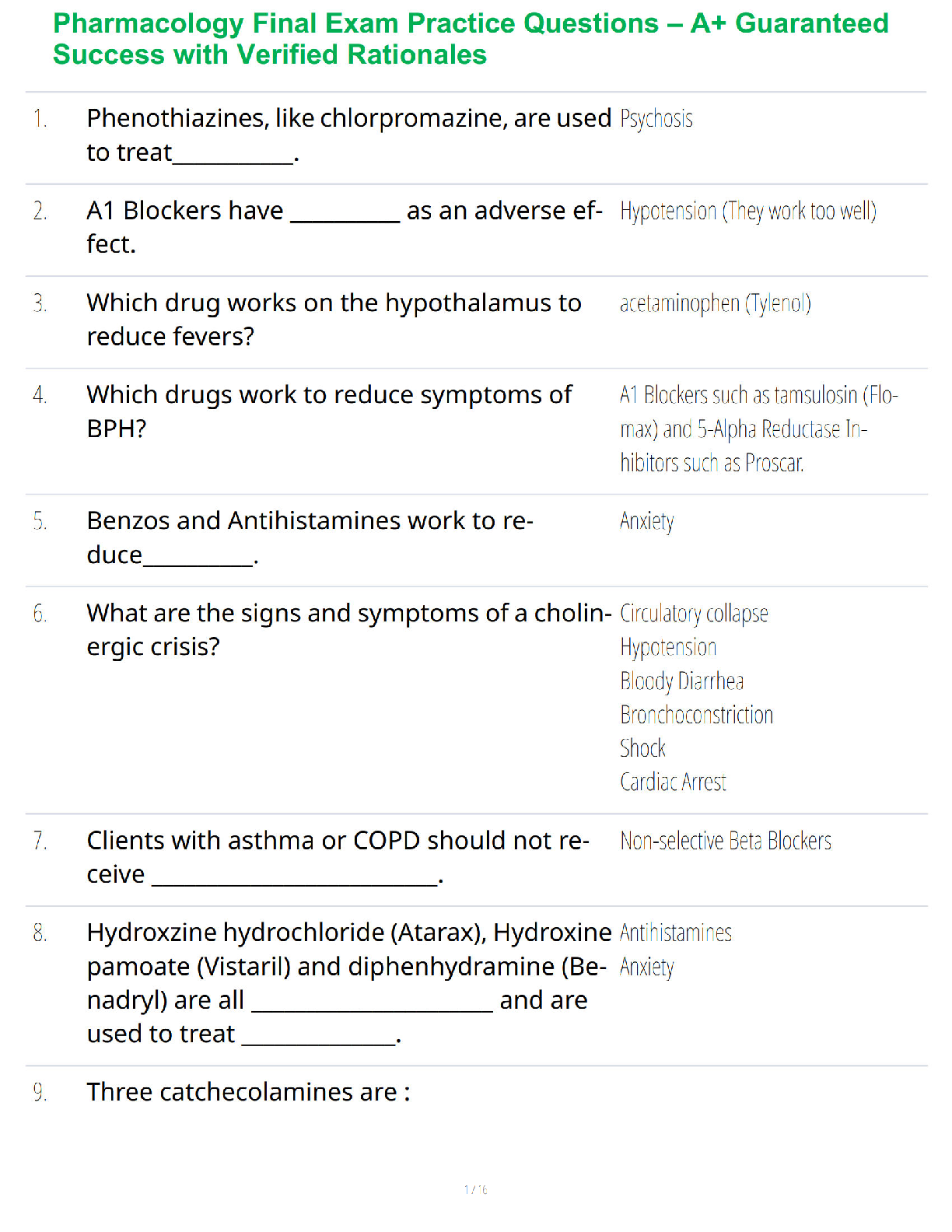
FINAL PHARMACOLGY EXAM STUDY GUIDE 2021-Anti-inflammatory Drugs
NSAIDS (ATI 279) – inhibits cyclooxygenase 1 & 2 : suppresses inflammation, relieves pain
Ibuprofen Salicylates (Aspirin)
-Block inflammatory response, a
...
FINAL PHARMACOLGY EXAM STUDY GUIDE 2021-Anti-inflammatory Drugs
NSAIDS (ATI 279) – inhibits cyclooxygenase 1 & 2 : suppresses inflammation, relieves pain
Ibuprofen Salicylates (Aspirin)
-Block inflammatory response, antipyretic (fever blocker), analgesic, antiplatelet aggregation
-Reye syndrome – from aspirin used for fever reduction in children or adults who have viral illness like chicken pox or influenza
-cause aspirin toxicity – progresses from salicylism (sweating, fever, acidosis, dehydration, electrolyte imbalance, coma, respiratory depression)
Acetaminophen (Tylenol)
-analgesic and antipyretic; not anti-inflammatory
-Inhibits synthesis of prostaglandin, blocks pyrogens at hypothalamus
-No more than 4g (4000mg) a day! Salicylism can occur: dizziness, tinnitus, HA.
-Increase risk of bleeding & take with no ALCOHOL!!
-antidote: acetylcysteine (mucomyst) – Prevents liver damage
Respiratory System Drugs
4 illnesses or diseases that impact URT and LRT? COPD, asthma, pneumonia
Upper Respiratory Tract
o Antitussives – suppresses non-productive cough/cough reflex
o Dextromethorphan (Robitussin)
▪ Cause dizziness, resp. depression, dry mouth
▪ Not for those that need to cough; not for those who have productive cough
o Benzonatate (Tessalon)
▪ Local anesthetic on resp. passages, mucus on lungs, pleura.
o Decongestants – decrease blood flow in URT and decrease production of secretions vasoconstricts/shrinks swollen mucus memb. Relieves nasal congestion. Tx allergic rhinitis and relief after removal of nasal polyps.
o Topical: Oxymetazoline (Afrin) & Tetrohydrozoline (Tyzine)
▪ May cause rhinitis medicamentosa (rebound congestion) if used longer than 3-5 days
o Oral: Pseudoephedrine (Sudafed)
o Topical steroid: Beclomethasone (Qvar) and Flunisolide
o Antihistamines – block inflammation and decreases secretions / expands airways
o Diphenhydramine (Benadryl) or Zyrtec (less sedative)
▪ Cause sedation anticholinergic effects: dry mouth, constipation
o Expectorants – increase production of cough to clear airway (for those with unproductive cough)
o Guaifenesis (Mucinex)
▪ Synergistic effect – combined action greater than each acting separately (used with antitussive or decongestant)
▪ Careful talking with OTC cold meds due to risk of OD
o Mucolytics – liquify secretions to aid the clearing of the airways. Treats cystic fibrosis / acute and chronic pulmonary disorders.
o Acetylcysteine (Mucomyst)
Lower Respiratory Tract
o Sympathomimetics – mimic SNS; bronchodilator. Epinephrine, Albuterol – treat asthma attacks
o Inhaled-short acting
o Oral-long-acting
o Anticholinergics – treat bronchospasms w/ COPD; relaxes bronchi muscles= bronchodilation
o Ipratropium (atrovent) – causes dry mouth, hoarseness
o Xanthines – main tx for chronic asthma/bronchospasms from COPD
o Aminophylline, Theophylline – don’t drink caffeine
o Therapeutic range: 10-20 mcg/ml
o 20-25: n/v, diarrhea, insomnia, HA, irritable
o More 30-35: hyperglycemia, decreased BP, arrhythmias, increased HR, death seizure
o Glucocorticoids – inhaled steroids
o Surfactants – used in lungs to expand alveoli
o Beractant
CARDIOVASCULAR!!
CARDIAC PART 1
Classification for Hypertension (JNC 8/9)
Causes for hypertension (know what meds cause it) NSAIDS, oral contraceptives, steroids, sympathomimetics, cocaine, steroids, licorice, herbs
Dx: 3 reads over 2-3 weeks (White coat hypertension) Know how to properly administer
Target organ damage and hypertension: it has long term effects; MI, heart failure, stroke, kidney disease, retinopathy (complication of diabetes that affects the eyes)
Modifiable vs non-modifiable (know therapeutic lifestyle changes)
-smoking, obesity, alcoholism, sedentary lifestyle vs age, genetics, race, family history
Normal ranges for BMIS (18.6-24.9)
Sexual dysfunction is common in antihypertensive drug use
Pregnancy: NO beta blockers in 1st trimester; NO ARBs or ACE Inhibitors
*Diuretics
Prototypes: Lasix (Black Box warning, makes you hypovolemic-really know BP and HR)
-BB WARNING: water and electrolyte depletion and severe diuresis, makes you hypovolemic
-risk of falls, orthostatic hypotension is expected
-signs and symptoms of hypokalemia (less than 3.5) and hypovolemia (blood volume depletion), hyponatremia (decrease in sodium levels, less than 135)….deadly, cardiac arrhythmias
-TREATS PULM. EDEMA FROM HF, HYPERCALCEMIA, HTN
Loop diuretics: give potassium chloride, hyperkalemia concern (last line). Lasix is K depleting – give K (banana, potatos, dried fruit, nuts, spinach, citrus fruit)
OTOTOXIC!!!
[Show More]