*NURSING > Solutions Guide > NUR 315 Pathophysiology (RATED A+) Study Guide. Download To Score An A (All)
NUR 315 Pathophysiology (RATED A+) Study Guide. Download To Score An A
Document Content and Description Below
Pathophysiology What is the patho (what is the disease) how does it happen and how does it show up in the pt? (Not need know how to treat a disease process). Know power points (under units) mainly ... and book is just if something is not clear. Use Emedicine (they are same authors as WebMD). Can’t memorize, must understand the concept bc way say in class might not be as ask on test. Assignments- not graded, optional. ABG and EKG practice really evaluate how to interpret blood gasses and EKGs. Def do these worksheets bc if not do well on them here, won’t do well on test. Syllabus- Room 407. Class is 8am-11am. 3 exams and then final exam during finals week- accumulative. Will get study guide for final exam except some new content and is 25%. Other 4.5% is weekly online quizzes- do whole week. She drops one lowest quiz grade. Posted usually by Monday Afternoon or Tuesday morning latest have until Sunday night 10pm to take quiz- 1 hour to do ten items, open book. Under Quiz section in BB. Hour before exam if sick need health care provider clearance to reschedule exam as for other classes. If miss exam on Monday other instructors told and need clearance to go to class. Student health clinic here on campus. Exam be rescheduled and can be in dif format. No makeup for online quizzes. Next week Joseph on Monday and Tuesday will teach 304 at this time slot. The following week caspi teaches in her spot Monday and Tuesday. Do have lecture content after exams. Exam is 1.5 min per item, so 60-75 questions usually so about 2.5 hours to do the test. Bet 9:30 and 10am is twenty min break. Pass around sheet to sign in after break. Good email response time- contact thru email. She will stress what’s important for testing. Review A&P and do reading for quizzes which delves into the patho. Chapter 2 Body tissues-embryonic origin and differentiate into many cells mainly ectoderm (..) and epithilu (over and into organs) A&P of cell. Cell metabolism- know when not receive enough perfusion oxygen etc what happens. Not tested on cell metabolism but know it for other things. Energy, metabolism- carbs and protein into energy for cell function. Get glucose and metabolize it to use as energy. If no oxygen- anaerobic metabolize the glucose, turn into pyruvate and then lactic acid which builds up and is detrimental. Without oxygen get lactic acidosis. With aerobic can use energy more efficiently but in terms of inflammatory and shock, if not get adequate oxygen flow lots of problems occur. Membrane transport mechanism- diffusion of molecules thru cell walls into cell tissues using transport protein- active transport as a carrier. Interchange ions and fluids thru membranes. KNOW: adaptive cellular response to stress Atrophy- shrinkage of the cell size (pt immobilized, not walking around fully ambulating within a week the muscles shrink in size) this is a way to adapt to lack of simulation and use Hypertrophy- increase in cell size, want it for when working out to stretch muscle and become bigger. Also when heart enlarges- most of time it does not do so on its own. It enlarges bc there is a dysfunction and heart trying to compensate Hyperplasia- increase in number of cells, breast enlarge when pregnant to breast feed. When woman has baby and stops feeding they go back to normal. Metaplasia- replace one mature cell by another. Happens when pt exposed to noxious irritant like a smoking pt the lungs scar and cells change and don’t have same efficient function as normal cell. This is compensatory to stress, irritants and toxins. Dysplasia- abnormal changes in size shape and organization of mature cell. See by virus or irritation like cancer. neoplasm- overt change. Just affect of stress. Neoplasms- altered cell differentiation and growth- not act like a normal cell. Sometimes doesn’t die, sometimes spreads, sometimes grows abnormally. Benign- tissue dies, abnormal cell but doesn’t invade other cells. Malignant- does invade other cells, metastasis, appearance and functions differently. Why cells die/injure? Phys agents- mechanical forces, electrical burns. Radiation Chemical- lead Biological- viruses Nutritional- malabsorption, etc. Free radical injury- general idea of it. Area of tissue not getting enough perfusion hypoperfusion- reactive species break away and free radicals form. Body has way to rid of byproducts of oxidation or stress- antioxidants like vitamin c and vitamin e that scavenge the free radicals and help rid of them bc if too overwhelming cause havoc. Local area of infection not getting enough oxygenated bloodflow and get free radicals its okay to be there but if blood pressure goes up and increase flow and free radicals get on systemically thru circulation they cause vessels to dilate and bp drop and crash to hypotensive. Not worry about formation of free radicals but when recirculate that blood. Any pt that had injurious dead tissue removal stroke, or heart attack means lack of good flow to certain organs but when flow to them get subsequent dropout- the free radicals went systemic and caused circulatory collapse. Reperfusion injury. Free oxygen species jump on and systemically cause reperfusion injury (steal electrons from other molecules and that causes physiological derangement in blood vessels to dilate and cause hypotensive episode and drop blood pressure.) KNOW: hypoxia and ischemia Hypoxia- low oxygen to cells, resulting in ischemia Ischemia- when hypoxia is prolonged not have enough nutrients, oxygen delivery and waste removal. If not have enough oxygen to cell not have enough glucose nutrients and energy to remove waste products. Hypoxia causes ischemia and ischemia is how lack of oxygen shows up in the body. Hypoxia for three minutes get resuscitated and fine but if not good resuscitation and down 10 min then hypoxic brain injury and death of brain cells. (global ischemia can turn into multi-organ failure. Kidneys half hour no good flow get injured. Brain within 5 minutes. Heart 20 min. gut longer like 4 hours. (if hypoperfusing then get free radicals and hypoperfusing get lactic acid building up). Ischemia can be reversible depending on the amount of time in that state. Consequences- anaerobic metabolism, lactic acid. Heart not like lactic acid bc changes in cells in myofibrils and heart not work. Bad byproducts of anaori meta and lactic acidosis. KNOW: apoptosis- Programmed cell death. Helps body filter out not so good cells. If clean them out cant become neoplastic and turn into cancers. Apoptosis eliminates old or injured cells that can cause havoc to a person. In cancer apoptosis is impaired and cells programmed not to die but to mutate and change. Apoptis occurs normally in cell tissues and during embryonic processes so no webbed feet. Endometrial cells during menses also to clean out uterus of cells that can be problematic. Breast tissue regression after breast feeding. In als lou gehrigs/alz and parkinsons implicated in these disorders. Necrosis- cell death in organ tissue that is still alove. Gangrene. When tissues die and become necrotic the tissue will self digest. They trigger an inflamm response. Types- liquefication etc not need know specifically. but if have wound with pus (debris of WBCs accumulating at area of infection) can be liquefied. Infarction not enough blood lfow to tissue and area around ischemic area dies off. Blockage in coronary artery n heart no flow there if not reverse quicly goes from ischemic to necrotic. Might be able to reperfuse or dies (necrotic, infracted) cant get back. Stroke- artery in brain blocked off area of ischemia try to resupply flow to but if not permanently dead tissue, infracted. Not from infection but lack of flow to that tissue bed. Gangrene- mass of tissue undergoing necrosis. Smoking pts constrict the vessels and flow not go thru so they lose their limbs. Young men in 30s have multiple amputations. Diabetes damage vessles and lack of flow. Dry gangrene- dead tissue sometimes chop off or falls off, black. Wet gangrene- due to infection it dies. Gas gangrene- anaerobic bacteria- bubbles and malodor coming from the site. (necrosis caused by many causes- dead tissue from infection, hemorrhage or inflame response. Infarction only because of lack of flow). Genetic disorders- Chromosomes footprint of individuals, info in chromosomes is genotype and phenotype way it is associated. Single gene inheritance- traits determinded by single gener. Multifactorail- controlled by a few generes or different places on same gene Autosomal dominant- male or female addected equally. If one parent affected 50 and if both 75% chance. Dominat so only takes one to be expressed in the offspring. Autosomal recessive- both parents need to have for kid to expres it. KNOW: auto rec if both parents unaff but are carries each offspring has 25% if being affected. Sex linked inheriatenc- if female and x link inheritance the double x protects her so not expressed, if male gets it bc xy then he expresses the disease. X link dominant- only one parent need be affted. May be lethal in males x linked dominant. X linked recesiive – KNOW HEMOPHELIA as example. Daughters of affected mael be carriers but sons be affected. Unaffected males of female carrier not give over. How many chromosome 22 pairs of 44 and then sex chromosomes 46 KNOW Female givers x male gives x or y. Dom rec traits- brown over green kids mostly get brown eyes. Genetic disorders- (patho how it shows up really know) Autosomal dominant MARFAN SYNDROME, KNOW males with long torso and anguinal hernia outpouching of intestine disease affecting connective tissue. Inherited disease fo connective tissue causing dysfunction on gene that codes for that connective tissue (connec tissue in joints but also muscles to ligaments in eyes, joints and heart valves.) Cardiovascular anomalies. Connec tissue in aorta blood vessels that can constrict and dilate. Marfan syndrome can affect many organs and affect males or females easily. Some have mild form and some severe. Can affect many organs. Depends how express itself in the dna. Diagnosis based on physical and family history. Many years they thought Lincoln has marfan syndrome. Offspring has 50% getting it. Know how it shows up. Retinal detachment- myopia. Joint hypermobility (loose joints, basketball player). Spinal deformities. Heart valve prolapsed sinking in of the valve. Aortic valve disease when aorta lining gets a tear (dissecting) separating from its lining. Aorta vessels has three layers, if dissects and opens too much then ruptures. KNOW SIGNS AND SYMPTOMS. Autosomal recessive- cystic fibrosis most common disorder. KNOW. Both parents must be carriers for offspring to get disease. If parents are carriers than 50% child is a carrier… defect in chloride transport chain. Sweating- method of transporting chloride and sodium and water follows sodium (sodium couples with chloride). In blood stream the sweat gland, sweats have chloride trapped bet skin supposed to be excreted with sodium. When sweat get rid of NaCL and cool off by losing water. But with cys fib defect in chloride transport and so increasing absorption of sodium and water into the tissues and not getting rid of it. Affects lungs, pancreas and found in the sweat. In sweat gland is increase in chloride bc cant reabsorb it into the bloodstream. The transport mechanism not allow it to be reabsorbed into blood and when reabsorb nacl hold onto water. With infections to get out need to cough out stuff and if cant (not loose) and stays in lungs turns into lower resp infection so bc of chloride transport mechanism cant reabsorb normally nacl but instead foes out of the body so water not be reabsorbed and so cant thin your secretions- spec at lungs and pancreas (not happen systemically, drinking water not help) the pancreatic juices and enzymes cant transport easily to duodenum and cant reabsorb nutrition. (can put a person on pancreatic enzyme, but lungs be chronically infected). Defect in transport of chloride back into the bloodstream (reabsorption). Lungs covered and have outlets for secretions to trachea and out of mouth, can cough em up- at this local level mechanism the chloride transport defective and cant thin our secretions. They test the sweat content see elevated chloride level bc not reabsorbed into blood stream and not where need to for secretion of lungs to be thinned and expectorated. Anything stay in body not supposed to be there gets infected and scars the lungs and eventually need lung transplant. Pt presents with lots of phlegm not cough up, problem is when chronic infections of secretion buildup. Supposed to reabsorb into blood but goes into skin. Increase in chloride in sweat and then cant thin out secretions (water doesn’t get reabsorbed) bc in pancreas, lungs and sweat glands. Very young have lots of infections and mucus, wet cough and shortness of breath. Causes an increase in congestion and mucus bc of failed chloride transport mechanism. Phenylketonuria (know the patho!) Child very fair. Defect in amino acid metabolism phenylalanine. Body cant convert this amino acid to tyrosine the precursor to melanin responsible for skin pigmentation. The brain cannot clear this and is toxic to brain and if not d diagnose quickly then accumulation causes mental retardation toxicity and cognitive problems. Light color hair and skin. Diet restriction of phenylalanine day 2 of birth mandatory blood test. Once feed infant see accumulation of phenylalanine and show signs of disease. Tay Sachs- Enzyme break fatty waste in brain cells and accumulations cause toxicity in all organs but mostly in brain. Spinal cord seizures blindess, death occurs by 2-5 years. Normal at birth but within 6-10 months show lack of attention and responsiveness and die within first years of life. Predomin in eastern hews. Carriers are screened bc death is inevitable, no treatment. Cherry red spot on retina is indicative of tay sachs- accumulation of the fatty waste products on the retina itseld. Chromosomal disorders- alter chromosome bc infection inflation or mutation. Downs syndrome- extra chromosome not 21 wide range of expressivity. Most common chrom disorder. KNOW RISK FACTOR- INCREASE IN MATERNAL AGE. Normal age mother less than 35 1 in 700 births and then over 35 Is 1 in 25 births. Maybe old eggs or more exposure to external factors not sure exactly why. Protruding tongue, flat nasal bridge, small ears, single palmar crease. Mental retardation, heart problems. Turner syndrome- x chromosome disorder, partial or ottal inactivation of x chrom. Spontaneous abortions. Diagnosed when girl go into puberty bc inability to have secondary sex characteristics. Degree of inactivation of x express differently. Shprt stature and webbing of neck, aorta is narrowed at point where suppl rest of body with bloo. Bicuspid affected- aortic valve is tricuspid but theirs is bicuspid. Absent ovaries amenorrhea. Normal intelligence but difficulty driving nonverbal problem solving, math. COA coarctation of aorta so narrows and not supply rest of body with blood. May need heart valve and surgery to fix that. Teratogenic agents- produce abnormalities during embryonic or fetal development. 2 months of preg without knowing it and many of these can occur based on timing and exposure. Maternal health also affect. Toxoplasmosis- exposure to cat feces, undercooked meat, others- varicella, zika, ● T-Toxoplasmosis ● O-Others (Varicella, listeriosis, leptospirosis, EBV) ● R-Rubellas ● C-Cytomegalovirus ● H-Herpes ● Can cause microcephaly, hydrocephalus, eye/hearing problems Chapter 3 Inflammation: Some content tested but inflam going to affect any pts who have had surgery have inflame- any pt with infection have inflame. Response to cell injury. If have infection, cut, injury, it will help trigger the immune inflammatory response it triggers mediator to get to area and clean it up. Phagocytise to remove damaged cell and tissue and increase blood flow to the area to help regrow tissue and heal. Like a papercut- tiny but hurts. Cut damaged tiny capillary vessels and trigger inflame response- trigger platelets to get there and trigger clotting cascade, clump and call fibrin and trigger clotting mechanism. Also trigger immune response macrophages to clean up debris- trigger WBCs to defend the host. Pulse on area of cut is opening vessels cause some capillary dilation and allowing mediators to cross over area of injury. As a result of that dilation (capillary permeability) it gets swollen, itchy, red and hot, causes pain but not bc of the cut but bc of the swelling, some exudates (drainage) to allow plasma mediators to get to area of damage. Neutralize toxins from the paper. Granulocytes- a white blood cell with secretory granules in its cytoplasm, e.g., an eosinophil or a basophil. Neutrophils are most abundant, then there are eosinophils, basophils and mast cells. They leave the blood and go to site of infection. Neutrophils use phagocytosis to destroy enemies. Eosinophils granules have toxic things that kill enemies. Basophils release histamine that triggers an immune response. Mast cells also have histamine and help with healing process. Agranulocytes-…Agranulocytes, also known as mononuclear leukocytes, are white blood cells with a one- lobed nucleus. They are characterized by the absence of granules in their cytoplasm, which distinguishes them from granulocytes. Two types are lymphocytes and monocytes. When monocytes leave circulation they turn into macrophages. Lymphocytes are three kinds- B cell, T cell and natural killer cell. B cells make antibodies that bind to pathogens and destroy them. T cells coordinate the immune response. (they remember past diseases and recognize them to fight them again). Normal inflammatory response- vasodilation, capillary permeability, leukocyte migration, phagocytosis SIRS KNOW!! System inflammatory response,, all capillaries open up vasodilate. Systemic inflammatory response syndrome to a major insult. (not just infection, could be inflame pancreas without infection, a clean surgery such as broken foot getting pins) all post-surgical pts have SIRS response. Heart rate compensate bc need more blood flow to area of insult- whole body responds. Respiratory rate higher- they breathe faster, temperature increases most of the time. Pt becomes febrile bc boosting up inflame response to defend the host. If pt in prolonged SIRS response the temp can be low, cant generate high temp and that’s a bad sign. Older pts might not generate high temp gets hypo. Some infections trigger sirs and make pt hypothermic (yeast in the blood is one example). WBCs usually shoot up higher than normal to help if for too long not enough to generate can be low. Low is for chronically ill or elderly. Most population increase in temp and wbcs. SIRS is systemic response to an insult manifesting in abnormal ways for body to compensate for what it sees as an attack (permeability- tiny capillary opens up and allows plasma to seep thru and in plasma is the mediators). KNOW: (identify and talk about dif cascades with SIRS to MODS) Sirs response not clean, will happen about 24-48 hrs after surgery or nay type of insult. It comes and goes on its own. But if sirs response is bc they have a bug bacteria, virus, organism, yeast, fungus- the damage becomes greater and pt considered SEPTIC. Bug or infection and heart rate higher, resp rate higher, wbc high get sepsis. Sepsis costs millions of dollars and bug problem in healthcare. Sirs + invading organism= sepsis. Severe sepsis= sepsis + organ dysfunction. Wait an extra hour to see if goes down. If because of infection- pt has nasty wound and has this criteria think sepsis. If pt has organ dysfunction- mental status gets funky, get agitated or confused maybe need more oxygen. Organ not working well and cant compensate bc of sepsis is severe sepsis. Vasodilating not making as good urine made now. Dysfunction in baseline, mental status and urination. Any so long a person can breathe 40 times a minute or 40 * Celsius temp before damage. If all vessels opened up then blood pressure drops. Bp think as garden hose and water the flower bed, and need hose over somewhere farther out, need to constrict hose that increase pressure and then can profuse a farther out distance. Normal. If vasodilate and open up garden hose and floods up close the father out place not get perfusion. Organs fail. To increase flow to farther out try to constrict and to supply to farther out need to give more fluid, fill up. If pt becomes hypotensive- vasodilated and no pressure in arteries to get flow farther out gives out fluid 2-3 liters, only have 5 liters of cardiac output at once give hald blood flow over there so blood pressure goes up, if still hypotensive after giving 2-3 litrers then in septic shock bc organs not get their perfusion. The brain kidneys heart gut then lastly skin. SIRS + bug + mental status SEPSIS+ hypotensive despite fluid replacement (if regular give fluid and back) now add constrictors/compressors. Powerful medication only get in ICU. If have fluid and vasocontricting with pressors and still not get flow the kidneys etc get ischemia and go into MODS multiorgan dysfunction syndrome- 2 or more organs down. Pt gets agitated then one system and if fluid given then kidneys affected if still not reach, the nephrons die- third system. Gut shuts down right away without blood flow no motility no abdominal sounds, cant tolerate getting fed. 4-5 systems have 80% mortality. KNOW: Mediators triggered to defend host (increase hr, rr, temp, and wbcs) when enemy comes. The blood vessel vasodilates to allow more leakage. The vessel wall getting permeable and the breaks in capillaries there so losing vessel wall integrity, gets damaged. Platelets triggered to come there and activated so SIRS cascade also triggers clotting cascade by platelets to clump at area of vessel wall damage. High risk for clotting- not such good perfusion bc losing fluid as vasodilate and can clot. When bacteria there and wall permeable the bacteria damages the vessels ability to vasoconstrict and vasodialte (autoregulatue) in septic shock. Not only that capillaries open up to try to help defend thehost, the septic shock the walls cant auto regulate. Give lots of fluid that seaps out into tissues and pt looks very swollen head to toe (periorbital edema skin around eye bulge, testicles size of watermelon, no folds In skin they breakdown, tongue bulge out, pt looks unrecognizable. Cant open eyes conjunctival edema) all fluid shifts into tissues. Organs fail then bc not get the perfusion. 60% mortality in septic shock. Most time prevent bc giving pt many times infections by not proper handwashing. (if fix and kidneys work there will be tons of fluid coming out after). Fever mechanisms: If bug cross hypothalamus try to reset temperature trigger SIRS (increase metabolic rate, fight the infection). Vasulcar stage- casofialation permeability, fluid shift into tissues. Cellualr- wbcs eneter injured tissue and destroy infections with tocins. Kinds of exudates (not test on it but might be a descriptor in a question): drianiage Serous- plasma like. Very thin yellow and clear, a little sticky. Oozes from any type of small cut. Hemorrhagic or sengounous is blood- frank red blood, dark. Fibrinous- stringy and usually tissue trying to regenerate. Membranous/pseudo- covers tonsils, membranes Purulent/suppurative- pus thicker, yellowish, whitish it is wbc debris collecting at site of infection needs to be cleaned out and may be a source of infection. (purulent wound think most likely infection behind it wbc clean out at a serious site that s infected.) 2/6/17 Chapter 8 Fluids & Electrolytes Edema vs third spacing Kknow as part of a clinical picture. Edema is fluid in insterstitial spaces (in tissues where not supposed to be) Dependent edema- when on feet all day. Ridge around ankles. Fluid shifts into a particular area. Third spacing is the shifting of fluid throughout the whole body- generalized edema. Swollen everywhere (conjunctiva, lips, periorbital, scrotum, arms, legs swollen). Third spacing is more of a systemic edema. The vessels are not holding in their fluid appropriately. In septic shock the capillaries dilate and become more permeable and fluid shifts from tight bound vessels to opening up and shift into tissues from head to toe. Electrolytes- substances that dissociate in soln to form ions. Os- pos or neg charged Cation + Anion – KNOW ELECROLYTE NORMAL RANGES (might see dif numbers in the book but know these) Na+ 135-145 mEq/L K+ 3.5-5.0 ** very strict bc incremental changes matter Cl- 95-105 Ca++ 8.5-10.5 mg/dl Mg++ 1.8-3.0 Phos 2.4-4.1 Serum osmolality 280-300 mOsm/Kg H20 Tiny differences isn’t a big deal Fluid and electrolyte shifts occur through: Diffusion- movement of particles across semipermeable membrane depending on size of molecules and concentration of soln. body strives to balance these. Sodium travels across! Though water follows sodium- we talking about normal. Abnormalities occur when too much water and not enough particles or too much particles and not enough water. With enough water to balance everything is a normal situation. If take away water the particles go up in conc bc not enough water to balance them. If body can compensate it will do that and then wont be a problem. In our class we focus on the PROBLEM. We focurs on ABNORMALITIES. Osmosis- water following conc of solute. Higher the osmolality, the more concentration the soln is. The conc of solute in fluids is the osmolality. Water moves to that higher conc of solute to balance. The compartments. Pt Is dehydrated not enough water to equal it out their osmolality goes up. If fluid overloaded then more water to solutes so osmolality goes down. Osmotic pressure: pulling power of soln to draw water across a semipermeable membrane. Isotonic soln- iso=same, a soln that has same osmolality, number of solutes, as body fluids. Nice hydrated cells. The fluid would stay in vascular space and not move in or out of cell. Stay where you put it. Pt with low bp- cuff on artery and compress it and measure pressure it takes to ill artery back up so very dependent on volume. Iv in a vein (vessel) fill isotonic fluid in there should stay in vessel so when check bp again it should go up. Good for bp hydration. Normal saline same number of solutes as plasma so stays in vascular space. Lactated ringers- has potassium and other solutes that it is isotonic- same osmolality conc of blood and stays in vascular space. Can give isotonic soln a lot to rehydrate the pt and give push for heart to perfuse organs. Hypertonic- has more solutes than plasma. Acts as mechanism to draw fluid out of cells and go into the vascular space. It is a pulling power from the cells and the cells become dehydrated and be like a raisin. You start to pee more bc increase fluid in vascular space. Someone with brain edema give them hypertonic soln to pull fluid from brain tissue and dump in urine. Hypotonic- has less solutes than plasma. D5w less osmolality then plasma so water shift into cells and rehydrate the cells. If rehydrate too much and too fast in can cause edema and can burst the cell. (5% dextrose in bag is isotonic but when body uses it it breaks down sugar and is just water and becomes hypotonic soln in water. Basically giving water which is a hypotonic soln) If drink hypotonic solution it can shift into your brain Not too much too quick cant bolus quickly for hypotonic (over permeates the cells)/hypertonic soln (really dehydrate). Can only quickly bolus isotonic. Pressure in cell- plasma protein albumin is a colloid (large molecule) Hydrostatic pressure- amount of pressure in vascular space pushing fluid into vessels towards the tissues and organs. What propels the fluids is the left ventricle of the heart to aorta. Pressure exerted on walls of the vessel usually bc of the pump the aorta. Oncotic pressure- pressure in vessles by big molecules like albumin and RBCs, plasma that maintain the fluid in the vascular space. They balance the pressure in the vessels and the hydrostatic pressure that’s pushing the flow to the end organs. The reason why tissues not flooded with fluid is bc have colloid pressure in the vascular space. If heart starts to fail the blood flow congests the heart (congestive heart failure), pump ot work then heart drowns and immediately the lungs suffer bc back up into lungs and into right side. Blocks breathing and oxygenation. If hydrostatic pressure not great enough to feed tissues then drown heart. If alcoholic and liver cant synthesize albumin all fluid go to tissues and fill up belly, cause edema and end organs suffer but fluids shift bc protein not being synthesized to keep fluid in the vascular space. If missing either colloid pressure or pump not working then have problems. Bad when both. Oncotic pressure- biggest component is Albumin. (hydrostatic pressure exerted on vessels towards organs and tissues. oncotic pressure keeps the fluid in the vascular space.) Filtration- fluid moves across.. Active transport- need carrier like sodium-K+ pump. Balanced as well. Sodium mostly INSIDE the cell. When give blood sample and send for electrolyte sampling and get normal lab values- they spin the sample and the RBCs float to bottom and plasma stay on top. Plasma is extracellular that’s what’s sampled for electrolyte balance, sampling extracellular not testing inside the cell. Get sodium mostly from what’s outside the cell. Water balance- have enough circulating volume to perfuse the tissues. Mechanisms to increase volume- Thirst Adh Raas cascade A & B KNOW the mechanisms! ADH and raas cascade going to be now, in cardiovasc, and renal. ADH: Normal water regulation- hypothalamus senses increase in osmolality. It senses when solutes are elevated or not as the blood flow goes across it. When raised osmolality it signals pituitary gland to release anti-diuretic hormone making you hold onto volume and not pee. Alchohol makes myou pee bc blocks adh production. Too many solutes so releases adh- makes kidneys holds onto water, increases blood pressure bc holds onto fluid. Now returning osmolality back to normal. Thirst happens before adh. If too much adh then the sodium level drops!! Too diluted. Bc holds onto water and then dilutes the sodium (not lose sodium, just diluted)!!! RAAS rennin-angiotensin aldosterone- kidney is very sensitive to fluid and volume. (rennin triggered by glomural) The kidney senses a decrease in perfusion pressure, blood pressure, blood flow, circulation and signals rennin to be released. Rennin is an enzyme that works on angiotensin a plasma protein that floats around inactive. Renin activates angiotensinogin 1 and triggered by Ace enzyme makes it 2 to hold onto sodium and water in the lungs and by doing this cascade in normal functioning kidney- angiotensin 2 is very potent vasoconstrictor. Vasoconstrictor increases blood pressure. If increase perfusion pressure raises bp and triggers ALDOSTERONE in the adrenal glands which works on sodium retension. Aldosterone holds onto sodium in the kidneys and also therefore water. 2 mechanisms activate by raas bc of decrease blood flow to kidney 1. Sodium retention 2. Vasoconstriction. Hopefully these cause kidneys to get more blood flow/perfusion. This happening in kidneys. If thirsty adh triggered. If thirsty and bp drops then RAAS kicks in. holds onto sodium and hopefully enough water in there to not be dehydrated. When thirsty not drink enough not pee a few hours now bp drops and kidney hypoperfused then RAAS takes over. Many drugs based on raas cascade. Increawe blood volume and then systemic vasoconstriction bc if go to core then not feed anything else. Aldosterone holds onto sodium (hopefully water, but wastes potassium so may need to replace it)!! Sodium is balanced with potassium so if hold onto sodium then excrete potassium. Normal ph is 6 in urine. Range 4.6-8.0. normal gavity how much sodium to water in the pee 1.005 to 1.030 greater than 1.030 means more concentration of solutes. Less than 1.030 is overloaded with fluids. if pt dehydrated kidney not enough water so increase in urine spec gravity. ANP and BNP- To oppose RAAS is atrial and b-type natriuretic peptide living in atria and ventricle of the heart. These peptides respond to stretching. If atria or ventricle stretch then too much fluid stretching them therefore the peptide is released and will oppose rennin and raas cascade. This effects volume status by getting rid of fluid (raas holds onto sedum, water and increase bp), if heart overstretch peptide released and start dumping urine. Worry more about B-type of left ventricle which perfuses organs (a does atria). Can measure level of dluif (crackles when listening to lungs and chest x-ray) and measure b type 1000s an d not 400 bc stretched ventricle and need to give diuretic to make them pee. Heart failure in low 1000s, 3 4 5 000 is really bad be in icu and intubated. Increase glomerular filtration rate bc vasodilate glomerular membrane in kidney causing you to make more urine. BNP shows up in pt high level excretion someone whose heart overloaded with fluid when trying to oppose rennin it was activated. Disorders of thirst and ADH Hypodipsia- not able to sense thirst. Elderly and dementia and infants cant tell/sense thirst. Stroke and hypothalamus damaged may not be able to enact thirst sensation Polydipsia- drinking to much water. There is psych disorder to drink a ton and throws electrolyte off. Di and SIADH from brain problems Disorders of water and sodium- fluid volume deficit Not have enough water= Pt is hypovolemic, losing water and electrolytes. Vomiting a lot in short amount of time, diaphoresis- excess sweating, polyuria (metabolite disorder and making a ton of urine), fever making sweat, nasogastric suction (sucking out large volume of flid)/ abnormal drainage, wound lossess need ccs/ml amount losing, (burns more third space losses, fluid shifts). Insufficenient intake- Anorexia, nauseas, impaired swallowing, confsuin, depression (not taking in enough fluid) KNOW CORRELATE HOW FLUID VOLUME DEFICIT SHOWS UP/CLINICAL MAIFESTATIOSN: (not need know percentages) 2% loss- mild fvd 8%= sever fvd Decrease tissue turgor- decreased elastcitiy, pinch skin on top of bony prominence it stays tented, Dry mucous menbranes Sunken eyeballs Decreased tearing Postural hypotension – change in bp from laying down to sitting or standing, changing position. Blood vessels uppoesd to tighten up but not enough volume in vascural space and perfusing brain which is why almost pass out. Hematocrit- excess when in fluid volume deficit URINE OUTPUT- hypovolemic, decreased urine output. Hypervolemia- too much volume, high bp. Body retains both water and sodium. Excess intake of sodium. Impaired fluid balance regulation- if pump not working, we want normal 2 L water intake a day but these pts even on 1 L /2 of what want still ion fluid volume excess. If heart week cant handle even 1 liter sometimes. Heart would get congested and go into lungs and not breather. Not activate RAAS cascade. Fluid serosis- albumin keeps fluid in the vascular space. Pts fluid can go into tissues and overflow the tissues. Also with liver have aldosterone levels off. Clinical manifestations- KNOW Weight gain – very sensitive indicator. Weigh the pt. Edema Hyptertension Adventitious breathe sounds – crackles** sound can auscultate over lung fields sounds like crackling JVD- jugular veinous distension. If laying 30 degrees in bed elevated. And juglar vein should be flat at 30 degrees if not talking. If at 30 deg see bulging of jugular vein then too much fluid in them, fluid volume overload. Blood count/hematocrit- amount of RBCs per volume. Percent of RBCs to volume normal is 35-45 or so, we go by hemoglobin usually. If hematocrit is component of volume and fluid volume overloaded then rbcs percentage is lower and becomes diluted and decreased in fluid volume excess. More concecntrated in fluid volume deficit. Serum osmolality – measure solute conc. Increase in solutes shows fluid volume deficit- not enough water to balance. Decreased serum osmolality shows too much water, fluid volume excess. Mechanisms that cause EDEMA: Fluid overload. Heart failure increases hyperstatic presure0 too much fluid cant pump out goes into tissues and causes edema. If heart not pumping out tissues cant get what need so kidney cant either and wants to activate RAAS. That’s where kidney can kil you bc fluid overloaded but not getting any so activate raas and go further into heart failure and edema. Increase membrane permeability- septic shock, burns, cause shifts- vasodilation. Out of capillaries they shift out and go into tissues. Need albumin to hold onto fluid in vessels and if not squishes tissues. If pt has oncotic fluid shifting into tissues- oncotic PULLS more fluid to the tissues which can cause further increase in edema. Lymph filters blood and gets overloaded and cant clear those proteins bc overworking. Oncotic protein not going where need to, shifting fluid, failure to remove sodium and water bc heart failing or vasodilating effect that causes fluid to shift into tissues. KNOW normal sodium but know key is NERVE FUNCTION/NERURO TRANSMISSION. Coupled with cl and Bicarbonate hco3 and water follows it. Low sodium less than 135 can be bc maybe too much water onboard which washes out sodium, if hypotonic holding on too much water, washed out sodium and cant concentrate urine so spec gravity is low bc sodium is dilute. Causes of hyponetremia- too low sodium Excess sweating Gi suction Salt free diets Adrenal insufficiency bc holds onto sodium Head injury stroke affects adrenal glands Diuretic therapy if lose too much water also lose electrolytes. KNOW SIGNS AND SYMOTOMS Malaise and muscle cramps MENTAL STATUS CHANGES, Headache, confusion, lethargy Nauseas vomiting, diarrhea Headache Convulsions and coma Apprehension- get figity, more agitated. If sodium is low bc water is high and can hurt brain- make coma and seizures Hypernatremia- Extra sodium, water loss, increased osmotic pressure carses fluid to move out of cells into the ecf Cell become dehydrated Plasa sodium aboce 145 Not have enough water on board to balance it out usually. The blood going to be bad flow and more concentrated and more prone to BLOOD CLOTTING. Hypovalemia and hypernatremia make blood more viscous and sluggish and clot easily. KNOW Clincal- Pt is thrisyu Dry mucous membranes Hypotension Rapid pulse for heart trying to compensate Not enough urine bc notenough volume Hypotension Confsion and lethargy Concentrated urine MENTAL status Potassium: INSIDE THE CELL- 3.5-5.0 normal Major cation of ICF Dietary source if too much banana avocado tomato etc, Regulated by kidneys. Potassium not stored well in the body. So if not good diet not have enough potassium. Aldosterone eliminates potassium. Insulin pushes potassium into the cell. Acid bas balance Exercise- muscle contraction triggers K+ release. Need healthy kidney to excrete potassium appropriately. If kidneys too much potassium need dialysis to filter them. Responsible for osmotic integrity fo cells with sodium pot pump Conduction of nerve impulse EFFECT ON CARDIAC MUSCLE- cardiac smooth muscle excitability in action potential. If K+ low: Muscle weakness and leg cramps ver common Fatigue Anorexia and nausea vomiting Decrease bowel sounds CARDIAC ARRYTHMIAS (changes depolarization of cardiac cycle)- cant stabilize cardiac contraction og the muscle HYpokolemia-inadequate intake Excess loss thru gi, kidney and diuretics … Hyperkalemia- KNOW Also cause cardiac arrhythmias Potassium relaxes cardiac muscle as well but too much relaxes too much at 6 seeing cardiac changes. At 7 the pt can arrest. Paresthesias Muscle and resp weakness Causes: Renal insuffiency- Ckd chronic kidney disease Autoimmune nephropathy- affects kidneys Acidosis Adrenal insufficiency if not enough aldosterone cant rid of K+ ACEI/ARBs (ace inhibitors and angio tensin blockers Potassium-sparing diuretics Icf to ecf Too much K+ administration RBC destruction- massive infection or trauma and RBCs break down they spill their contents which is mostly potassium so see it goes up and pt becomes very acidodic. Calcium 8.5-10.5 Stored in bone and ecreted by kidneys Found in icf regulated by pth … HYPOCALCEMIA If poor aborption in GI tract Pancrease grabs calcium and decreases it in blod Vitamin d helps to absorb calcium Renal failure Hypoparathyroidism hyperphosphatemia- with phosphate opposite so if calcium down then phosphate up KNOW SIGNS AND SYMPTOMS Bc of nerve transmission it will affect in dif ways- Tetany- the locking of jaw Trousseau sign when put bp cuff over arm and inflate it causes a spasm Chvostek sign- pain shooting down jaw when tap facial nerve Prolonged st and qt (arrhythmia not need to know) Laryngeal stridor- the larynx can become bc lack of neurotransmission tightens and cause threat to airway Impaired clotting- free floating activated calcium in blood is a clotting mechanism, if calcium low then cant clot Hypotension-arrest: cardiac conduction so makes pt hypotensive or cardiac arrest Hyeprcalcemia- Due to increase in porous bone release of calcium . higher blood conc of calcium and makes bone thin and break easily. Immobility: walking or running causes bone to become more dense and stronger and allows calcium to go into bone and make harder. Immobility does oppos Hypophosphatemia- makes phosphate low when calcium high Hyperparathyroidism- too much activate thyroid Increased GI absorption Clinical: Decreased LOC Ekg changes Av blocks See renal calculi- kidney stones usually of calcium deposition. Lots of dairy products/calcium will deposit in kidneys Bones thin so break- bone pain fractures Calcification- deposits of calcium on organs Band Keratopathy- deposits of calcium on the eyes Magnesium not stored well in body (like potassium) so must intake Helps with myocardial contraction Contracts the myocardium HYPOMAGNESEMIA- Due to malabsorption, gi tract infection/disease or not eating like alcoholics- most not eat Diuretics- rid of electrolytes with water KNOW PRESENTS: Cardiac arrhythmias Hyperreflexia Dysrythmias- forsaads form od cardiac arrest instead of shock and meds give magnesium bc alcoholic or suspect mag deficiency Helps calcium transport so can also have trousseau and chvotek but really for calcium Similar to hypocalcemia Hypermagnesemia- not see much. Only pts with kidneys not work have overload of magnesium Renal failure Cuases Slow resp rate Bradycardia (causes relaxation) Hyporeflexia Decreased loc Phosphate: 2.5-4.5 Anion fond most in icy In boe and teeth Component of atp Acid base Nerve and muscle activity Hyperphosphatemia is low calcium hypocalcemia trousseau chvotek Renal failure Excess intake Hypoparathroidism Hypocalcemia KNOW PRESENTS: Hyperreflexia s/s of hypocalcemia phosphate deposits in joints Hypophosphatemia- Absorption iissues Starvation Alcoholism Malabsorption Hyperparathyroidism Renal phosphate wasting If replace phosphate too quickly then calcium drops- NURSING INTERVENTION REPLACE PHOSPHATE SLOWLY OVER 4-6 HOURS bc if give quickly and calcium drops and pt goes into cardiac arrest its bad. KNOW presents: Dyspnea Muscle weakness Confusion Decreased cardiac contractility Sodium, pot, raas cascade ACID BASE BALANCE- Due assignment after lecture and study do worksheet. Know arterial gasses. KNOW YOUR NORMALS 7.35-7.45 normal in blood Acid olecule can dissociate and relase H+. base can accept or combine with H+ As H+ goes up in blood the ph goes down. Body cells sensitive to ph and can affect normal cell function. Ph is measure of relative balance bet acids and basis in soln. ot is neg log of H+ in mEg/L. Acids added to soln ph goes down <7.35 When base added to soln ph will go up >7.45 Sample of arterial blood and evaluate the gasses in it- can tell the pt true acid-base balance before blodometabolized in liver and messed up. Can tell what goes on in lungs but not metabolized by liver. 1 acid: 20 bases. Primary acid is CO2 and primary base bicarbonate HCO3. We talk about CO2 end product from lungs by clear CO2. If get venous smaple already metabolized. Areteriole not metabolized by liver just worked on by lungs and is co2 not hco3. Greater than 7.45 is alkalosis is ecll derangement/death. Lower than 7.35 is acidosis and also cell derangement/death. Chemical buffer system: 1. Bicarbonate buffer Kidneys can conserve or form new bicarbonate as needed if working. If pt is too acidodic the kidneys can hold onto more bicarb or synthesize more to make it more alkalotic bcbicarb is a base 2. Hydrogen-potassium exchange system. K+. hydrogen ions go into cell if too acidodic and kick out potassium too compensate. They switch plaes to compensate e for acidosis or alkalotic. To help buffer th blod. 3. Protein buffer system Acidosis- H+ diffuses into cells and drives out k+can stop heart, drive out k+ elevates k+ hyperkalemic. Alkalosis- h+ out of cells and k+ in but blood is hypokalemic. Give several scenarios and interpret whats going on. Kidneys can hold on or get rid of bicarb to help regulate. Lungs also can rid of co2 or hold onto co2. If alkalotic then hold onto co2 (co2=acid!!) if acidodic then rid of CO2. How? Control resp rate. Blow off co2 is rid of acid. By retaining co2 breathing less holding on to acid. When sleeping involuntary breathing- co2 starts to climb and central resp centers sense increase in co2 and say take deep breathe too let out more. Nrain stem and peripheral chemorecceptors in carotid branch and in central sense co2 level and respond to it. The only prolem is pts with lung disease- respond to low o2 levels to breathe more. Smokes, copd, have lung disease have dif mechanism. Can alter resp rate. Normal co2 level is 35 to 45 mm Hg! Can blow off more by breathing faster or decrease resp rate to retain co2. Kidneys also regulate ph by rid of h+ in urine if pt is acidodic can reabsorb bicarb into blood as well and make new bicarb from ammonia. Arterial blood gasses to get ph values. From artery to see how co2 elimnated and bicarb eliminated. Might see co2 and bicarb level on electrolyte panel- venous samples metabolized by liver and so dif numbers, Basic metabolic panel or complete metabolic panel. Here bmp and cmp and they not meant to indicate resp status or ph. Arterial blood gasses. Ph, acidosis, alkalosis Paco2 35-45 Bicarb 21-28 kidney working hold on or dump as needed and this is normal range Metabolic acidosis- Initially have low ph bc acidodic <7.35. metabolic reason for kidneys not doing job not resp. maybe anaerobic, or dead tissue somewhere so making more h+ ions maybe kidney not working, maybe loosing bicarbonate fluid via the gi tract- diarrhea (fluid from belly button down) so become acidotic, not need chloride. Too much acid ot losing too much bicarb Diabetic ketoacidosis too much h+ ions bc not feeding tissue sufficiently. Starvation ketocacidosis- breaking down ketones and become acidodic. Anaerobic metab Overdose if acids Renal failure/uremia Loss of bicarn Diarrhea Pancreatic … Imbalance so lungs okay bc metabolic problem. What lungs do? Can increase resp rate to blow off co2. So increase resp rate greater than 20 (greater than normal in adults) hypertachybnic to blow off more co2. Can also gave lactate containing soln like lactated ringer which is isotonic to replace bicarb stores. Really need to fix underlying cause. Kidney failure so need dialysis. If infection rid of it and perfuse those organs.. Metabolic alkalosis:high ph Too much bicarb or lose too much acid. Rid of fluid above bell button- vomiting. Increase bicarb levels Alkalosis- Excess base: Too much antacids Too much lactated ringers Lungs: can slow down resp rate to retain co2 too compensate for excess base. Breathing in a bag. Respiratory acidosis: Increase in co2 they initially try to breathe fast and then when sitting breathe too fast for long not enough energy feel lightheaded and dizzy bc blowing off co2 and vasodilate bp drops and you crash. Exhausting to breathe really fast for two min. Very quickly stop breathing and buld up co2. Gone past ability to compensate by blowing off co2. Caused by Acute disorders of ventilation- which pt not triggered to breathe bc have impaired function of medulla, brain stem injury (can’t breathe on won)and OVERDOSE pt. narcotic overdose stops the trigger of breathing and holds onto co2. Lung disease- copd cant compensate Chest injury Weakness of resp muscles- cant enervate diaphragm so cant breathe properly Airway obstruction Chronic disorders of ventilation: COPd- uses low o2 not high co2 as trigger to breathe. COPD has scarred lungs and have held onto co2 for a while by then. Body used to it. So not trigger them to breathe. They use low oxygen/hypoxia as trigger to breathe. If a pt needs oxygen and are copd you want to give lowest amount of o2 possible bc if give high levels may knock out trigger to breathe. Everyone else use high co2 as trigger to breathe but for copd use low o2 and go up sa needed. Pulmonary fibrosis- scarring of lung tissue and cant exchange gas properly accumulate co2 Increases oco2 production- Hypermetabolic they produce more co2. What can kidneys do? Take a while to hold onto h+ ions from blood so cant rely on for resp acidosis bc take too long. Resp alkalosis- Dece pco2 and increase ph. Caused by hyperventilation (rid of too much co2) Overstimulate resp center Not need third.. Pt usually in hypermetabolic state like Anxiety Pregnant Any infection Sepsis Febrile Exephalitis Makes them breathe daster, Hypoxemia can trigger increased resp rate. Deceased bicarb- decrease h+- high ph and can respond by dumping bicarb???? Mixed acidosis or alkalosis. Resp and metabolic acidosis or resp and metabolic alkalosis. Worst problem leads ph in that direction. Renal failure + narcotic induced resp depression= needs dialysis and ods so decreased resp rate and kidney cant dump H+ ions. Pt with copd gets gi bug cant compensate- resp acidosis and metabolic acidosis dumping bicarb. Gotta fix. T They cannot compensate. Some pts compensate with opposite . only compensated if ph is normal. Not treat number but the pt. opd ph normal but co2 high don’t fix number. If pt dropped to 7.31 acidodic then put on ventilator bc cant compensate. Pt not compensated unless ph is in normal range. Partial compensation exists as well. Get your normal values memorized. 1.Last name first Name abnormal acidosis or alkalosis, Determine if resp or metabolic problem 2. evaluate what going on in lungs 3. biacrb action Ph= 7.30 (7.35-7.45) paCO2=50 (35-45) HCO3 =24 (22-26) Acidodic, acidodic, normal Co2 (less than alk and greather is acid. Bicarb less than 22 is acid and greater than 26 is alk) ACID think resp, bicarb is normal. Respiratory acidosis. If bicarb going really alkolotic 32 that would be partial compensation bc kidneys trying to fix resp problem but there isn’t here so no compensation. 7.48, co2 44, bicarb alkolytic 32 Metabolic Alkalosis, normal, w/ no compensation 7.26 Acidosis, co2 normal bicarb acidodic Metabolic acidosis Lungs not trying to help Metabolic= bicarb Resp= co2 Kidneys- bicarb Lungs- co2 7.10 acidosis, c02 acidic (more co2=more acid), bicarbonate 15 is acidic MIXED bc kidney sdumping bicarbonate and going in acidic direction and so is co2 more present so more acidic. Metabolic and resp acidosis 7.54 Alkalosis, Co2= 20, alkalosis Bicarb 25- alkalosis towards. Mixed so metabolic and resp acidosis. (she wont use 26) 7.33, acidosis, co2- 25 alkalosis, co3- 20 acidosis Metabolic acidosis with partial compensation the alkalytic co2 trying to compensate. Sue two of the same and the other one is compensation. If ph was in normal range then be compensated- not normal but coimpensated so not call resp or metabolic problem. For compensated the numbers out of range but ph normal. 7.28 acidosis, 54 co2 acidosis, 20 hco3 acidosis Metabolic and respiratory acidosis. MIXED. 7.52 ALKALOSIS, co2- 48 is acid and hc03- 36 alk compensate Metabolic alkalosis with partial compensation (hco3 trying to fix but cant) Example of pt with resp rate 35 (breathing heavy) light headed and blood gas would suspect ph 7.49 in resp alkalosis. Can give directions of numbers this is high and this is low. Or give sample of numbers and you determine what it is. HW sheet use as a guide. Clinical example know also. 2/7/17 For Exam 1: Inflame and injury, genes, fluid and electrolytes and neuro on test. Most is what is the patho: not super cellular just basically. How does the disease show up/clinical manifestations: must understand the slides not memorize. Study by making sure not confuse different diseases. Do disease, the patho and how it shows up, the dif electrolytes. Neuro don’t confuse ms and mg- see how different. Memorize- electrolyte values and blood gas values. Use medscape and emedicine and webmd. Must comprehend. Follow the guides given in lecture- whatever she emphasized know and what she didn’t, just be glossed over, don’t bog down on it. Review lectures after class. 10% are pick all that apply bc on nclex at least 10% are pick all that apply. Bet 60-80 questions. 1.5 min for each item. The action potentials is how neurons communicate with each other. All based on interplay of potassium and sodium receptors (review!!). Spinal cord organization, cerebrospinal fluid. Pathologies- What makes pain subjective? Gate control theory: there are several factors involved in individual’s perception and tolerance of pain. Some factors are when have an injury there are emotional factors, cognitive factors (if understand what happened feel pain less), emotional factors, distracted from pain may feel it less. These things we talk about for pain in pt not just meds but distracting them playing music, a massage on dif part of body to distract nerve impulses. Someone cognitively impaired not understand the pain may feel it more. Medicine subscribes to this if affect the other factors can make pain felt less Pain threshold: point at which stimulus perceived as pain. Very subjective. Some people with a small cut ruins their day and others not really notice it Pain tolerance: point at which pain too unbearable. Very subjective. Some people higher pain tolerance than others. Nociceptive pain: pain activated by peripheral tissue injury Neuropathic pain: neuropathic/nerve bundle pain KNOW KINDS OF PAIN: Cutaneous pain: pain related to injury to skin and subcutaneous tissues Deep somatic pain: pain down to muscles and tendons like sprained ankle or joint pain Visceral pain: distension or eschemia of a body organ. If have gall bladder pain or gi bug and colon is inflamed (at the site) Referred pain: pain perceived at a different site than the actual organ that is involved. Gall bladder obstruction they get right shoulder pain. Pancreatitis can go to right shoulder or back KNOW DIF BETWEEN ACUTE AND CHRONIC PAIN! Acute pain: serves a purpose, telling the body something is not right, it indicates a problem. Signals the body there is injury or tissue damage Chronic pain: greater than 6 months in duration and doesn’t serve a purpose. TYPES OF HEADACHES KNOW!! Migraine: happens more commonly in women, about 18% of headaches are migraines. Can be genetic, can be hormonal related. Migraines have an aura attached to them- a feeling that it is going to come on can be hours or days before. They can be associated with other symptoms like nausea, vomiting and photophobia Cluster: more uncommon, men get them more often, pain behind one eye is the hallmark, usually lasts for a few days and goes away Tension-type: dull aching, more common and hat band distribution goes around the head Temporomandibular joint pain (TMJ): headache by imbalance in temporomandibular joint A headache you’ve never had before is most concerning, severe and never go away that is a dif pattern bc indicates something going on in the brain. KNOW TYPES OF MOTOR DISFUNCTION Plegia- stroke or paralysis Paresis- weakness Mono- one limb Hemo- both limbs one side Di/para- both upper Quadric/tetra- all 4 limbs Some involve upper or lower motor neurons. Upper send to lower and they said to nerves that enervate the muscles. Skeletal muscle problems: DISUSE ATROPHY- muscles shrink and lose ability to contract bc of immobilization and disuse (nothing patho wrong. Foot drop for immobilized if not contract foot they have permanent foot that cant contract. Use multipotus foot that keeps it flexed and extended appropriately. Denervation atrophy- no enervation of contraction. Typical of spinal cord injury pts bc not enervated for contractiokn MUSCULAR DYSTROPHY- genetic disorder damages muscle fibers bc absence of dystrophin a protein that maintains integrity of the muscle and so the muscle cannot contract. There is a spectrum of disorders for md Myasthena Gravis: Autoimmune disease- the body creates antibodies against certain tissues and attacks itself. No one knows why. Disorder of muscular junction that affects the motor neurons and muscle cells. Destruction of acetylcholine receptors bc of the antibodies that destroy them and block binding of acetylcholine. Acetylcholine helps muscle to contract so without the ability to use it at those junctions the muscle cant contract. Associated with thymus tunmor awhere antibodies are created or hyperplasia of the thymus gland (in adults the thymus atrophies so sometimes they just remove it). Women usually get more often in early adulthood. Gradual development of weakness proximal to distal portions of the body, if diaphragm is affected which is a muscle that drives respirations than have resp compromise. Only where skeletal muscle involved not cardiac or smooth uscle! Signs and symptoms: KNOW!! Insidious- out of nowhere. Smaller muscles affected first and then can get worse and become wheelchair bound. Muscle fatigue and progressive weakness. Muscle of eyes face mouth throat and neck affected first. DIPLOPIA or PTOSIS- double vision and drooping eyelid bc the EOMS are affected and levator muscle in keeping eyelids up. Cand have difficulty swallowing chewing choking and aspiration. When diaphragm affected ventilation in compromised. There is a spectrum. Autoimmune triggered by stress (alcohol, drugs etc) Periods of flare-ups/exacerbations and remissions, there is some ability to control with lifestyle changes but not easy. Usually younger individuals are involved. Stress, pregnancy, alcohol can cause crises. Use medication to conserve as much acetylcholine as possible in the body. Myasthena crises: stress event or not on meds can get severe muscle weakness, quadriplegia and resp insufficiency and extreme difficulty swallowing and risk for resp. Biggest problem would be not being able to swallow/breathe. Cholinergic crises: too much medication on board, caused by drug toxicity of cholinesterase drugs which prohibit breakdown of ach. SLUDGE: salivation lacrimation urination defacation gi upset and emesis: these signs and symptoms. Smooth muscle hyperactivity and excessive parasympathetic like activity. Bradycardia and increase sweating. Will be asked abt med- tensilon is a hallmark med for MG bc they diagnose MG. pt with symptoms give shot of Tensilon- very short acting to give increase uptake of acetylcholine- when they respond with improved symptoms in the office it’s a way to diagnose MG. Electromyogram- stimulate nerve bundle with electricity and see how it responds. Use dif labs to see as well. Treatment not need know- for all autoimmune bc its in inflammatory state use an immune-depressant med like steroids. Even chemo meds like cytozan is immune suppressant med. Plasmaphoresis- some pts hospitalized with myasthenia crises- filter plasma and filter out antibodies and throw away plasma. Filter the blood. If works it works within a week- usually pts with resp compromise and myasthenia crises. Peripheral nerve injury: ▪ Damage to LMN cell bodies in the spinal cord ▪ Damage to axons in the spinal or peripheral nerves ▪ Damage to myelin sheath (demyelination) ▪ Mononeuropathies ▪ Damage to one peripheral nerve ▪ For example, carpal tunnel syndrome ▪ Polyneuropathies ▪ Damage to many peripheral nerves ▪ For example, Guillain-Barre syndrome Guillain Barre Syndrome Demyelinating disorder but NOT autoimmune disorder, its caused by a virus/infection that triggers this event. Humoral and cell-mediated immune reaction directed at the peripheral nerves. Attacks peripheral nerves. A strep throat or any virus and not recover, instead the virus triggers inflammatory immune rxn to peripheral nerves. It affects longest axon first- ASCENDING PARALYSIS from lower limbs up! Motor paralysis Pt get out of bed then cant walk, in few hours paralyzed from bottom and goes up. When hits diaphragm they cant breathe and are on ventilator. When get over it its done and out of your system. Anyone can get it, not common though. SIGNS AND SYMPTOMS KNOW: Had to have infection 1-3 weeks before Ascending paralysis from bottom up Priority big concern- resp (airway breathing circulation) Treatment: Put pt on ventilator, plasmapheresis and iv immune globulin administration. Parkinson’s Disease KNOW PATHO: Degenerative disorder of the basal ganglia and the dopaminergic nigrostriatal pathway- the part of the brain that supplies dopamine. Dopamine depletion. Happens over time- degenerative not sure why but theoretically repetitive head injuries and concussions but also can be hereditary influence but cant say truly linked. Start in 40s and peak in 50s- prevalent in males. Dopamine inhibit movement in muscle fibers and ach is excitatory. Imbalance of dopamine and acetylcholine so have excess muscle contraction bc lacking the inhibitory influence of dopamine. SIGNS AND SYMPTOMS: Tremor at rest Rigidity (too much contraction it spasms, not flaccid/limp) Bradykinesia/akineasia- slowness in movement ntil cant walk at all Forward leaning gait as walk Dysphagia- muscles of throat and tongue become rigid Speech problems Dementia- in late stages only Depression Constipation- late stages Urinary retention- late stages Not true paralysis bc can send nerve impulses to muscles just lack of dopamine. Bilateral symptoms but usually stat on one side. Evaluation/Treatment: History of pt helps to diagnose, rule out secondary parkinsonism- brain tumor pressing on basal ganglia and stroke to basal ganglia and other meds could effect, no spec tests available Drugs for akinesia and deep brain stimulation- can implant in brain but not for everyone for deep brain stimulation. Amyotrophic Lateral Sclerosis/Lou Gehrig Disease: Degenerative disorder that involves BOTH UPPER AND LOWER MOTOR NEURONS resulting on progressive muscle weakness. No inflammation. Onset at any time from the fourth decade. More in males before menopause. Suspicion glutamate toxicity is involved to cause neuron degeneration theoretically though some meds of glutamate decrease symptoms SIGNS AND SYMPTOMS: Weakness may begin in any or all muscles of body Paralysis can occur with progressive muscle atrophy No mental sensory or autonomic symptoms preset. Have normal intellectual and sensory functions until death. Life expectancy 5 yrs after get symptoms. Evaluation/Treatment: See how much muscles respond to signals. Eventually need resp support bc diaphragm muscle not work. Stephen hawking the miracle of expected als. Multiple Sclerosis Demyelinating and IS autoimmne disorder inflammatory destruction of CNS myelin sheath. Onset bet 20-40 yrs. Female more prevalent. Some genetic association More common whites. T-cells attack myelin sheath and cause inflammation- inflammatory response. Plaques form with demyelination and axons do degenerate over time. The plaques that form cause a loss of nerve conduction and decrease in transmission of nerve impulses. This occurs with flare ups/exacerbations and remissions. SIGNS AND SYMPTOMS: Fatigue Parastheisia- numbeness of fingers and toes Optic nerve- visual field affected Ocular motor nerve- loss of eye movement cerebellum- loss of motor movements, Cerebellum system: loss of motor movements, feel weakness, loss of coordination and balance Evaluation: History and phys exam with mri Ct scan Treatment: Treat exacerbations and progressions Use immunosuppression drugs Use anti-inflammatory drugs to treat exacerbations Treat symptoms of pain, depression, bladder problems weakness (have problem with adl activities of daily life) Spinal Cord injury ▪ 7800 to 10000 persons each year ▪ Most are men between the ages of 16 and 30 years Injury to tissues thru forces that cant handka. Vertebral injurues compress the tissues Bones ligaments and joints may be damaged through fracture, dislocation or noth. Classified: ▪ Flexion ▪ Extension ▪ Compression KNOW: FIRST COMES SPINAL SHOCK, OCCURS AT TIME OF INJURY, LOSS OF RELEX FUNCTION BELOW THE LEVEL OF THE INJURY. Spinal cord injry at T3 pretty high may not be ale to send messages down and messages cant come up thru nervous system but peripheral nerves still work and activated by acetylcholamine. Initially lose peripheral reflexes below level of injry. Transection is where spinal cord injured through and through Reflex fintion lost below lesion Flaccid paralysis- loss of sensation Loss of bladder and rectal control Unopposed parasympathetic stimulation- will get hypotension/bradycardia (vagus innervations) Hypothermia below level of lesion Once acethylcholamine respond and reflexes come back some of this will come back. Peripherally still reflexes, some contraction may not be purposeful movement. If have spinal cord injury can elicit reflex in foot but they cant move their foot voluntarily. They respond to stimuli but not respond to impulses. Rigid and shaking and reflexes but all involuntarily. Cns is damaged that is why. Initially spinal shock flaccid- no stimulation no reflex. When spinal shock resolved have some reflexes and contraction but still paralyzed. Lasts 7-20 days and up to 3 months. TEMPORARY. Effects are with inflammatory response. When done then gets these peripheral reflexes back. Temporary loss of regulation, reflex and contraction. Hypotension and bradycardia and when swelling is done then all come back. Temporary loss of relflexes and peripheral nerve stimulation. Autonomy Dysreflexia/Hypperreflexia Can happen anytime of life of spinal cord injury pt after spinal shock resolves. Need intact peripheral nerve stimulation to occur Life threatening Happens with ots injured AT T6 OR ABOVE Some noxious/bad/painful stimuli below the level of the transaction and the peripheral nerves sense this bc still working so signal catecholamine serge/response which causes bp to go up very high, heart rate very high. Biggest example of noxious stimuli- full bowel or fll bladder. Constipation for a while or full bladder then catecholamine make systole 200 and can stroke out the pt and kill them. T6 or above is a bladder that full and straight cath not used to empty bladder and reflexes not working so cant empty own bowel/bladder without assistance. Below that level peripheral working and signal catecholamine surge and bp up. If leave empty syringe in bed and pt laying on it and signals something not right. Always check when last bowel and urination, is laying on something is something on body twisted. This can happen anytime of their life. SIGNS AND SYMPTOMS: Hypertension (>180) Pounding headache Blurred vision Sweating flushed skin Bradycardia to lower bp Symptoms can be one or more Most common causes are distended bladder or rectum. (over 180 systole is high. 140 is hypertension 160 urgency 180 is emergency) When cath the pt and digitally disimpact then bp lowers and they are okay. Must resolve the stimuli. Sometimes bp med iv stat. Partial spinal cord injury- not common, not need know well During spinal shock have swelling so not sure how much damaged, get swelling down and e.t. not sure affect til resolved. Partial area, anterior or one side. Central cord syndrome: loss of motor and sensation Anterior cord syndrome: loss of motor and temperature but do have touch Brown-Sequard syndrome: loss of motor on that side, pain and temp sensation other side ▪ Central cord syndrome: damage to axons near the gray matter Arms more affected than legs ▪ Anterior cord syndrome: damage to anterior section of cord Motor functions affected; touch sensation not affected ▪ Brown-Sequard syndrome: damage to one side of cord Motor function lost on that side; pain/temperature sensation lost from other side Not all spinal cord pt is alike bc some could have sensation but not move and no light sensation. Complete spinal cord injury much more common To upper motor neurons t12 and above- spinal reflees still work. No longer modulated by brain hypertonia, spastic paralysis (when pt say he moved that’s a reflex) To lower neurons t12 and below Cells in spinal reflex arcs damaged Flaccid paralysis Neuromuscular Part 2 Hypoxia- prolonged is eschemia. Inflammation of the area, swelling, disruption of the cell. Interferes with energy stores, nutrition to thecell and oxygenation. Intracranial Pressure The pressure inside the brain ventricles/folds of brain and put catheter can measure the pressure generated. Brain is made brain tissue, blood and CSF (cerebrospinal fluid) the monro-caley hypothesis is if change any one of the components, if swell brain have damage, if too much blood flow problem bc nowhere to go and too much csf floating around nowhere to go bc skull not stretch and can only go to hole where pons and medulla is by brain stem where breathing center is and then dead. This concept basis of all brain injury/damage. Intracranial pressure> arterial pressure- injury causing inflammation and swelling in brain crunches on blood flow and then causes further eschemia. No room to swell in thick compartment of skull. Arteries collapse and blood flow to brain cut off. Hydrocephalus: too much cerebrospinal fluid makes brain swell, nor oom Tumors- displace brain tissue and have nowhere to go Csf can be reabsorbed somewhat but its limited. If have too much it displaces brain tissue. Increased intracracnila pressure not need know stages- if too much pressure in brain then happen in stages 1-4. At 4 shifting brain tissue= herniating from area of higher to lower pressure to opening foremun and get brain death. SIGNS AND SYMPTOMS: Kids- bulging fontanels Sunset eyes (eyes look to top) Kids over 2 and adults- projectile vomiting from nowhere No aura of nausea Adults-Cheyne strokes- irregular patterns in breathing Headache Change in loc Pupils change quickly bc optic nerve pressed (ultrasound over eye can see and measure width of optic nerve and if optic nerve compression then know if swelling in the brain) Sluggish and dilated pupils Bradycardia (neuro exam is very important) Nrin herniation worst case scenario of intracranial pressure- brain tissue compressed and Hydrocephalus- excess fluid in cranial vault, subarachnoid space orboth Too much production or prevention of drainage wirhin the ventricular system or defective reabsorption. In kids noncommunicating hydrocephalus- obstruction within ventricles Adults- communicating hydrocephalus Traumatic brain injury- Most of the time the frontal and temporal lobes are affected. Primary injuries due to impact. Microscopic damage or bruising/contusion. Primary injury is the damage but the real problem is secondary injury- bleeding/swelling/infection from the damage with leads to increased intracranial pressure. Goal is reduce secondary injuries that occur. Hematoma: KNOW DIF BET EPIDURAL AND SUBDURAL BLEED IN BRAIN Hematoma bleeding in brain cause pocket of blood displaces the brain tissue. If it is an epidural arterial bleed its most devastating- arterial much stronger flow hallmark- loosed interval, they pass out then wake up fine then pass out and deteriorate. Thunderclap headache out of nowhere and then loosed period after unconsciousness. Subdural bleed- in small bridging veins, slower bleed can be chronic problem that can be managed. Not as bad as epidural bleed. Diffuse brain injury- Concussion or bruising not need know difs of concussions. Diffuse axonal injury DAI the worst- high speed injury rotational injury where brain knocked around in skull at high velocity not see one bleed but see punctuated bruising spots which is shearing of axons- not just one side but is diffuse. Global injuries and deficits. SIGNS AND SYMPTOMS Less than 25 do better with brain injury Change in LOC Change in relfees Change in pupils Change in resp pattern Change in function? Focal brain injury- neurological deficits Diffuse- GLASGOW COMA SCALE KNOW: Describe injury severity in brain injury and stroke Mild 13-15 Can be severe 3-8. Baseline gcs with brain injury is important and then check them throughout the day. Given a pt (a few qs) and get gcs Eye opening is spontaneous (walk in and they look at you) 4 eyes They open eyes with you introduce, is 3 Noxious stimuli and open eye 2 . None 1 Verbal response Jackson remember they talk to you right back 5 A little confused 4 Inappropriate response 3 (ask where was? Cat, name? banana) Incomprehensible sounds 2 No response to verbal 1 MOTOR RESPONSE 6 Obey commands Localize to pain try to stop stimuli 5 Withdraw from pain 4 Flexion to pain is abnormal response 3 (decordicating towards the core posturing trun in and rigid) Extend to pain worse 2 (deerebrate) None 1 If dead still get a 3 Cerebrovascular disorder- strokes: Runs in families More common in women Ischemia Hemorrhage Stroke= brain attack. Most are ischemic- lack of flow to area of the brain bc of a clot or plaque Hemorrhagic- not as common due many times to deformation in wall of artery- bulging or tearing that ruptured and cause bleed either from trauma/genetics or blood pressure. KNOW difs and Know TIA Transient ischemic attack- comes and goes, no residual effect. Might wake up with facial droop on one side and trouble talking or difficulty on one side of body or confusion bt not truly infracted or ischemic. Low flow to that area of brain but resolves within 24 hrs. No permanent damage but is bad bc sign of impending stroke. Strokes- KNOW MODIFIABLE VS NONMODIFIABLE RISK FACTORS Pt with thrombotic- from plaque from cerebral arteries, if have plaque in cerebral vessels and it damages vessel wall it then forms a clot. Plaque disruption causes a clot to be formed. That’s from coronary artery disease= thrombotic stroke. Risk factos= hardening of arteries and plaqe formation from cholesterol coronary artery diesaes atherosclerosis. EMBOLIC- clot from other artery to brain Heart disorder causing blood flow sluggish can have clot form in heart and go to brain. High blood pressure risk factor is hemorrhagic stroke punds arteries and can cause bleeding in brain Smoking- damage to vessels can cause Diabetes- high sugar damage vessels can cause ischemic or hemorrhagic stroke African American higher risk bc of high bp Alcohol abuse impairs clotting Higher age Family hc Nonmod- age, race, family hx Ischemic- lack of flow to brain bc of occlsion Thrombotic and embolic Risk factors: a-fib not allow heart to eject blood fully so etra in there that can clot prosthesis- can cause clot to form Hemorrhagic- main cause is HIGH BP, ruptures blood vessles. Ruptured aneurism- bulging of vessel that bleeds and vascualar fmalformation- weakingn in wall born with, Head trauma, anticoagulation use. SIGNS AND SYMPTOMS VARY DEPEND ON SIDE OF OBSTRUCTION OR SIDE OF BLEED (usually opposite side of head is affected) One side headache Loc Slurred speech Aphasia Altered mental status Motorsnsory loss Neck stiffness photophobia Mostly in frontal and temporal lobe Know what aneurism is: bulging of the vessel wall. If bulges enough and cause the symptoms and bursts have hemorrhage,. Aneurism caused by genetics or high bp Meningitis- (what is and how shows up) Infection of meninges. Can be acute or chronic NEED PORTAL OF ENTRY Infection in subarachnoid space, Resp tract, head injury, csf most common Bacteria meningitis- SYSTEMIC: Fever Tachycardia Chills Petechiae rash- red pinpoint marks on body from trail of the bug Severe headaches KNOW KERNIG SIGN- inability to flex leg at right angle when lying down causes pain KNOW BRUDZINSKI SIGN- put head to chest irritating jerking of the knee Changes in loc Projectile vomiting Seizures Need systemic a/b and it will resolve Diagnose the big and do lumbar punctures to see source. Treated aggressively. Encephalitis- Tissue infection of brain and spinal cord MOST COMMON CAUSE IS VIRAL WEST NILE VIRUS Signs and symptoms of meningitis is encephalitis. Brain tumor: Cause focal disturbance in area of brain affected by tumor. Damage based on size and location Seizures- Hallucinations Waeakness or palsies in spec areas Could be benign tumor but not in brain tumor. All malignant must be treated. Seizures: Explosive sudden discharge of cerebral neurona Alteration of brain function. Always rule out in new onset seizure a brain tumor. Brain injuries can cause seizures. Provoke seizures- due to fever electrolyte imbalances, hypoglycemia If give too much insulin to diabetics, cns infection or damage When not due to smth else and build up of seizures pt may have epilepsy the onset of seizures with no other known cause. ▪ Partial seizures Begin in one cerebral hemisphere ▪ Secondarily generalized seizures Begin in one hemisphere and spread to other ▪ Generalized seizures Involve both hemispheres Absence- blank out Atonic- loss of muscle tone Myoclonic- muscles contract Tonic-clonic- muscle contraction and Convulsion- jerkiness Generalized across both hemispheres, KNOW THINGS THAT HAPPEN BEFORE AND AFTER SEIZURE: aura: warning directly related to onset of seizure prodoma: early signs such as malaise that occur hr or few days before the event postictal phase: period following cessation of seizure, if generalized all their muscles contract in spams and use lots of energy can burn muscle high metabolic rate can break down muscle fibers, they are exhausted and can sleep for hours. Fatigue and no memory recall of the seizure. Status eilepticus- uncontrolled repetitive seizures, can lead to death- can cause resp failure to obstruct airway by using a ton of oxygen become anoxic- more than 5 min is dangerous. Give fast acting ativan benzodiazepams to get out of seizure KNOW Agnosia: cant recognize form and nature of objects Aphasia: loss of comprehension or production of language dysphasia : impairment of comprehension or production of language expressive dysphasia: cant express themselves receptive dysphasia: verbal comprehension deficits Alzheimers: Severe cognitive dysfunction in elderly Not sure why happens [supposed that ameloid plaques but not proven Pt initially forgetful then confused then cant participate in activities of daily living or take care of selves Their brains are different. Less brain activity/atrophy. Amyloid beta-forming plaques degenerate and cause tangled fibrils of plaque in the brain which normally body rids of but accumulates in alzheimers pt and cant have proper neurotransmission. KNOW STAGES: First: short-term memory loss can last a few yrs Second: confusional stage, disoriented lack of insight and impaired hygiene Third: incontinence and cant recognize family or friends Electrolyte quiz: 2/13/17 BEGIN EXAM 2 Test review meeting: can make appointments Wednesday to review test Disorders of the hematologic system Plamsa- carries antibodies and nutrients to tissues Consists mainly of proteins and albumin- oncotic pressure keeps fluid in interstitial spaces, globulin- produce antibodies to fight infection fibrinogen- clots Erythrocytes- rbc carry oxygen to tissue. Fake blood given to jahova witness to someone hemoglobin drop from 12 to 5 gave her synthetic form of blood hemapurin which didn’t work as well. Life span of rbc is 120 days. Nutritional requirements to form rbc- iron, folic acid, and B-12. When looking at anemia correlate deficiency with type of anemia= low red blood cell count. Triggers red blood cell production is drop in oxygen content in kidneys triggering them to signal the bone marrow to create more RBCs. If you have poor kidney function most likely will have anemia= hallmark. WBCs- leukocytes participate in inflame and immune response. Produced by bone marrpw. Dif types to fight infections. Normal range 5,000-10,000 Both Granulocytes and AgranulocytesTriggers Coagulation Cascase- know. Platelets job is first step in clotting-KNOW! Life span of 7-10 days. Platelets not last so long. If on meds that interfere with platelet function like aspirin (blocks platelet aggrigations) and others abt a week before meds stop working on platelets- if need emergency meds and been on plavix and aspirin get high isk of bleeding after sx which happens a lot. Platelets initially constrict blood vessels, form plugs and then trigger clotting cascade. Blood dyscrasias- abnormal conditions of the blood. Causes vary: Trauma- lose RBCs and have platelet dysfunction bc triggered to work and may run out of them. Trauma causes vessel damage which triggers clotting cascade. Gun shot wound, mva, stabbing etc. chronic diseases- GI tract Sx Malnutrition Drugs= some meds interfere with clotting and use up platelets Toxins Radiation Genetic and congenital defects- can also affect bone marrow suppression Sepsis- triggers clotting cascade with the vessel damage that occurs during vessel damage and call membrane permeability. DIFFERENTIATE THE ANEMIAS: Hemoglobin 12-14 g/dl is normal. Classified according to RBC size Hematocrit: percentage of RBCs to volume. Hemoglobin is the count but hematocrit is percentage to volume. 12 hemoglobin and hematocrit 3x the hemoglobin. 12 and 36. ACC on labs automatic cell count. Hematocrit is percentage of rbc to volume which goes up and down depending on pts volume- can change if dehydrated or fluid volume overload. If dehydrated hematocrit look falsely higher nbc it’s more concentrated. If not enough volume (bottle of water and add rbc to it and strain water and leave rbc sounds like more percentage rbc to volume) if same amount of rbc and add volume/water then seems diluted the count goes down. Look at percentage bc not that lose rbcs or gain just have more fluid or less. Hemoglobin is accurate to oxygen carrying capacity of rbc. Anemia: lower Mean corpuscular volume: the size of the RBC. Microcytic: <80 mcg cubed small hemoglobin Normal: 80-100 mcg cubed Megaloblastic/Macrocytic: >100 mcg Anemic: low hemoglobin count. Now see size of rbc to see why pt is anemic. Types of anemias: Iron deficient Vit b12 anemia Folic acid anemia Bone marrow depression- aplastic anemia: RBC count low, WBC count low, Platelets low. Gives suspicion that the bone marrow is not working bc ALL of the cells are down. Possibly chemical agent or virus or radiation attacked bone marrow. Hemolytic anemia: anemia where RBCs are broken down Sickle cell anemia Thalassemia: mutation in hemoglobin synthesis, mostly prevalent in asian, meditteranean, and black populations. Tailored to particular areas of origin Acquired hemolytic anemia: took a med that made RBc break down, device churning blood around and broke RBC down, cancers can do this to break RBCs down. NEED TO KNOW MICROCYTIC ANEMIA IRON DEFICIENY, WHAT IS AND PATHO Nicrocytic anemias 80 mcg cubed Red blood cell volume is small due to iron deficiency anemia: most common cause is blood loss. Hemorrhage, sx, trauma- broke down RBCs and not have enough iron stores to create more RBCs so rbcs are small. Mostly due to frank blood loss or chronic slow blood loss. Women more then men bc of monthly menses blood loss. Also common among individuals not taking in enough iron KNOW, so when make RBCs they are small. Cant make volume of hemoglobin normal. Vegetarians have to worry abt this not eat enough protein not enough iron. Substance abusers with abnormal diet not have enough iron. Causes: Supply of iron inadequate to form RBC Inadequate diet Problem in GI tract not absorbing iron Pregnancy is expansion of blood volume so need more iron to make more RBC Blood loss RBC trauma KNOW GENERAL SIGNS & SYMPTOMS: Develop gradually Hemoglobin at 7 or 8 g/dl get symptomatic Weak Fatigue Short of breath- Dyspnea -not enough oxygen carrying capacity Light headed Tachycardia- trying to compensate for lack of oxygen carrying blood cells Palpitations Weakness Pallor (very white) Brittle nails Cheilosis- cracking of the lips, skin not get perfusion along with other organs, last to get good bloodflow Sore, pale tongue- usually red and beefy Dizziness Hypoxia Pica- Pica compulsive eating of nonedible substances like dirt or chalk or bed linen Pacophagia- compulsive eating of ice At juncture of gas exchange only need hemoglobin of 3 they say. KNOW LAB FINDINGS IN RELATION TO IRON DEFICIENCY AENMIA: Iron stores deficient. Low ferritin- body’s major iron storage pretein increased total iron binding capacity TIBC- transfarin is protein that combines with iron for binding. Increased iron binding capacity means not enough iron to saturate those carrriers. An increase in total iron-transfarin binding capacity. Not enough iron to saturate those stores with increased TIBC. (more stores, nothing in them) Microcytyic RBC- MCV less than 80 KNOW in size Do a CBC and see Decreased rbc, HgB and Hct, decreased mcv Treat- blood transfusion, etc. MACROCYTIC: Large RBCs but still anemic- not many of them Vit b cs Pernicious anemia B12 helps make blood cells. Vit b12 anemia means not enough b12 on board. B12 important in neuro transmission so have signs and symptoms of anemia and dysfunctional neurotransmission Get b12 thru diets but if problem with stomachs ability to synthesize and absorb b12 then called pernicious anemia. Can be autoimmune destruction of parietal cells in the stomach. They cannot produce intrinsic factor which helps to absorb b12. VIT B12 can be anyone not getting enough nutrition. Just give b12 orally and be fine. Pernicious anemia prob with absorbing b12 so even if give bottles full of it not help. If remove stomach and/or part of duodenum that absorbs b12 also have pernicious anemia- cant use GI tract to absorb b12. Must get injection parenteral or goes into mucosa sublingual without using gi tract to replace b12. SIGNS & SYMPTOMS of pernicious and b12 anemaia regular anemia + neuro problems: Dizziness Muscle Weakness Tachycardia Fair hair coloring Confusion altered mental status Ataxia- loss of coordination Parasthesias Neurological symptoms Smooth sore beefy red tongue- lose villa becomes smooth and glossy bc hemoglobin is BIGGER Pallor Diagnosis of b12 anemia KNOW: Becomes a chronic problem. Megaloblastic is chronic malnourishment/absorption issue so gets bigger to compensate for lack of b12 > 100. Increase mcv size. Hallmark test KNOW- Schilling test rule ot b12 anemia vs pernicious anemia. Oral challenge of b12. They measure the urine and figure out how much is absorbed thru the urine which helps determine whether the gi tract was able to absorb the b12 or not. If not able to absorb load see thru urine excretion then has pernicious anemia bc gut not able to absorb. If could absorb the b12 then just deficient in b12. To treat can have either dietary intake or need replacement therapy thru blood for pernicious. Test if anemia due to gi absorption or not. Picture of pt with dietary vit b12 that parietal cells absorb intrinsic cell and bind to b12 in intestine and be absorbed. If miss piece of stomach or intestine or both- can make intestine size of golf ball and attach ileum to stomach and bypass duodenum that cant absorb b12 and other nutrients for gastric bypass pts- restricts absorption in stomach and intestine so they need lifelong replacement of b12 via shot or sublingual. 2/20/17 Talked about dif types of anemia- so far vit b12, aplastic anemias and B12: lack of enough b12 in your diet, just eat enough and be fine Pernicious anemia- must be admininstered in bloodstream bc cant get it thru gi tract. micrositic folic acid and macrosidic is b12. Hallmark for signs and symptoms: neurologic problems. With b12 and macrosidic iron deficiency anemia is the neuro problems. Folic acid deficiency anemia- folic acid need to create hemoglobin for RBCs. Folic acid for normal reb blood cell formation and get thru diet. Pts with malabsorption not have enough healthy gut (gastric bypass or intestinal disease), some meds can impede absorption like contraceptives. Etoh abuse not eating normal diets so lots of malnourishment also anorexia. Sign and symptoms: Pallor Progressive weakness Fatigue SOB Palpitations- make up for not enough rbc formation Gi symptoms No neuro problems RBC CBC must correlate on panel with folic acid deficiency anemia- chronic process- had to not have absorbed for period of time to get this anemia. Diagnosis- Cbc decreased rbc Increased MCV- increase size of RBC that are there- macrosidic anemia Treat- Oral folic acid supplements Increase dietary intake Sickle cell anemia- Hereditary disease. Hemolytic: break down of RBC. Autosomal recessive disorder. Defective hemoglobin S formation. Common in Africans 1 in 10 have the trait and life span is 40-50 yrs. KNOW Understand and correlate patho of sickle cell anemia Baby born with it.Few months after birth make hmg S- during period of stress (deoxygenation) the cell becomes sickle cell shaped. It can bend into small spaces small arterioles providing gas exchange to tissues but sickle cell cant do that malforms and becomes sickled so cant go into small areas- joints eyes heart where vessels get tiny they get trapped and cause occlusion there and cant do gas exchange in small capillary membranes. When not stressed its round and fine but by stress event it sickles and jams small capillaries and not give gas exchange they become fragile and breakdown causing hemolysis. Under low o2 levels the rbc sickles and jams the capillaries and infarc tissues like kidneys heart (strokes, heart attacks). Its reversible in that if pt never have stress event than wont sickle but hard to avoid a stress event. The organs without the gas exchange will suffer and have infarction- tissue/cell death. Not constant, only with stress sickling event and then resolves. Signs and symptoms: Anemia Pallor Jaundice- rbc breakdown so yellowing of mucosa and tissues and skin bc dead rbcs Irritability Chronic fatigue Sob Joint swelling Aching bones Localized and generalized pain Unexplained Dyspnea Leg ulcers Frequent infections Signs of crises: Severe pain esp in joints with the ischemia Hematuria- rbcs bloody in urine bc broken down Lethargy Irritability Pale lips, tongue palms and nail beds Spleen holds and filters rbcs and can get enlarged bc too much rbc breakdown too many fragments and splenomegaly and could rupture bc not have room to go- pt have spleen taken out. Always palpate the belly bc can feel splenomegaly. Stroke Seizures Avascular necrosis of long bones- bones infracting the joints If in nd out of crises a lot have more of them but if manage well then life can be better. Everyone has dif hypoxic threshold so some can handle it better. Whatever stresses that pt though can trigger the crises. Nntk Diagnosis- look at hemoglobin electrophoresis, genetic testing, increased in rbc formation but they breakdown Nntk Treatment- counseling, newborn screening, prophylactic a/b from 5 y/o vaccines, treat infections, avoid low o2 places. Iron deficiency not have enough iron for hemoglobin so microsydic megaloblastic- become larger sickle cell and then normal. Platelets: Thrombocytopenia platelet count less than 100,000mm cubed. Most common cause o fabnormal bleeding Hemorrhage from minor trauma and spontaneous bleeding <20,0000 Fatal gi cerebral and pulmonary hemorrhage Causes: Unknown, Other diseases, Viral infections, Chemotherapy or radiation, Hypersplenism or splenomegaly, Bypass or autotransfusion Heparin therapy Patho: Decreased or defective platelet production Increased destruction outside of the marrow Abnormality in the distribution of the platelets Idiopathic thrombocytopenia pupura ITP: Antibody destroy platelets in the spleen, not common Secondary thrombocytopenia: Very common, defect in production of platelets, due to meds, Bone marrow disorders, Chemotherapy or radiation KNOW HIT is Heparin induced thrombocytopenia- autoimmune disorder Platelets aggregation and thrombus formation Heparin used to prevent clot formation and given three times a day. After 5 days of administration pt can form antibodies against platelets so know definition- A reduction of 50% from baseline with recent heparin use and other causes platelet 200000 used as 200 on labs and within 5 days of heparin drops to 100000 and continues to drop down so suspect has antibody rxn to heparin and causing breakdown of platelets. If give heparin but they have septic shock and give 3L of fluid- hemodilution that means cardiac output is 5 L of fluid circulating in the body so if give 3L diluting the rbc and platelet count so must take into account could have diluted it. Rule out this and other things. If they are dehydrated and not fluid overload suspect HIT. In 3% of pts on heparin but much less on low molecular weight heparin. Signs & symptoms: Drop in count and antibody mediate rxn causes platelets to clump together and cause clotting and every time clotting and then body starts to breakdown the clot so exaggerated response of clotting and bleeding with HIT. Sudden onset of petechiae (red spots of bleeding little hemorrhages) or purpura (bruising) Epistaxis- bloody nose menorrhagia (women bleed) hematuria, gi bleeding Anemia signs- tachycardia sob altered LOC hemorrhage death Activity intolerance Any pts on Heparin watch their baseline platelets. Before administer heparin get the count and in first 5 days watch if drop 50% and continue to drop until stop heparin. Then send heparin antibodies and see if have HIT and if do then now have allergy to Heparin. Diagnosis- with cbc platelet count, coagulation studies PT/PTT normal bc talking about clotting cascade and know platelets first step of coagulation but once platelet trigger clotting cascade the other factors do their own thing (if pt/ptt okay then the problem is probably the platelets bc have enough clotting factors), platelet antibody studies (HIT or platelet dysfunction), bone marrow Treatment-steroids bc autoimmne disorder, platelet transfusions, splenectomy bc any platelet problem may need to remove spleen, educate on risk of bleeding, thrombocytopenic precatutions (not inject in muscle and not give aspirin- not do anything that will cause bleeding). Pt is anemic then know low rbc count and correlate what type of anemia with the MCV. Hemophilia- x linked recessive trait carried by women and since have 2 x’s give their disease to 2 males. Hemophilia really only affects boys and women are carries. Hemophilia A factor Viii (need factors to clot, in coagulation cascade injury platelets clump triggers a factor etc, if any step missed bc not have that factor then bleed, no back up. Must have all factors available to form healthy clots), or hemophila b factor IX then have hemophilia. Any trauma and miss factors can bleed into joints, muscles or have lifethreatening bleeding. Treatment is to give them factos- IV or subq of factor- infusions of factors to stop bleeding. Kids get on prophylactic factor replacement- once a week self infuse at home to live healthy lives and not worry abt falling and causing bleeding. KNOW SIGNS AND SYMPTOMS: Prolonged bleeding (no factors to stop it) Hemiarthrosis- bleeding into joints, don’t put anything warm on joint even with joint pain bc causes vasodilation Spontaneous hematuria Hematoma- bleeding Intracranial hemorrhage which may be fatal KNOW correlation and who at risk (any insult can trigger) DIC- Disseminated intravascular coagulation- not know who will get it bc not disease but a syndrome as secondary response to insult. Out of wack coagulation cascade- usually see when pts go to surgery and they bleed and clot excessively at the same time are in DIC. No real source of bleeding so not be at surgical site bt systemically in urine, stool, nose etc. (never give aspirin preop bc stops platelet clumping for ten days). Cant prevent this. Can happen to anyone to trigger DIC cascade. If clotting cascade is overloaded initially clot and risk for clots but right after break down clots and so see clinically bleeding. Insults: Infection (sepsis) try to defend the host but causes vessel damage and triggers DIC clotting then bleeding bc vessel expands and mediators and Neutrophils and cytokines trying to protect host all at once causes little bit of damage to vessel wall but it’s enough and triggers dic Pregnancy issues Trauma Burns Emboli Heart stroke Inflammation Shock Cardiac arrest. DIC cycle: Insult-> widespread clots so toes and joints look blue and cyanotic->hypoxia as clots disrupt o2 flow-> clots breakdown and widespread bleeding everywhere-> clotting factors used up. People die from it can bleed from eyes. Diagnosis- look at tests for clotting and bleeding Treat- nderlying cause, blood transfusion, clotting factors in plasma so FFP fresh frozen plasma Lymphomas- KNOW differences bet hodgkins and nonhodgkins Hodgkins- spreads thru lymph/nodes first sign is enlarged lymph nodes and by bipsy have reed-sternberg cells KNOW. Highly curable 85-93% curable and doesn’t come back- happens to pelple in early teens-50s. very treatable with chemo and radiation. No sx bc lymph node disease. Non Hodgkins- can spread outside of lymph and is more rare and has poor outcome. Remission in abt 60-80% of individuals. No reed sternbergs cell present in biopsy also have lymphadenopathy. Leukemia- cancer of blood or bone marrow Increase wbc count. Proliferation of immature WBC which take over bone marrow and cause underproduction of RBCs and platelets. Too much wbcs crowd bone marrow that don’t work properly. At risk for infection, bleeding and anemia. Bone pain and infections. Can be acute or chronic. Cardiac Rvw anatomy to understand the disorders Endocardium is on the inside so endocarditis is on the inside. Myocardium is the muscle. Pericardium lines the outside. Pericardial fluid is on the outside and compresses the myocardium. The pericardial layer holds 30-50mL of fluid, no tmuc, so layer not rub and stick against the heart so a little extra fluid compresses the heart. KNOW blood flow of heart! Right heart supr/infr vena cava right atria, ventricle, pulmonary artery, deox blood, to lungs, oxy, pulmonary veins to left ventricle, aorta, to rest of body. Pulmonary circulation from pulmonary artery. Pulm circulation receives blood flow from right side of heart. Left side of heart is stronger. Right passively receives bllod flow from boyd. High pressure in pulm circulation the right side suffers bc not meant for high pressures. Pulm circulation is low flow vasculature. Pulmonic goes to left side aorta and then systemic circulation higher pressures to push blood flow against gravity into aorta and then to brain and rest of body. KNOW importance of diastole. Diastole is relaxation of heart and blood fills right and left sides. Passive filling. LATE diastole is most important ohase bc though passive filling what happns is the atria contracts one last squirt providing 25% of cardiac output. Called atrial kick/contraction. The last atrial kick ventricles really fill up to get ready for ejection. If have atrial dysrythmias if atria not have good signals could lose kick and lose cardiac output and filling pressure. Can live with it but can suffer from it. Late diastole is when 25% of cardiac output supplied to ventricles during filling. Systole- contraction passes to ventricles. Blood from ventricles pumped to arteries and organs. KNOW preload, afterload and other terms. Preoload- represents the volume which we read as pressure. The volume/pressure generated at the end of diastole. At end of diastole the ventricles stretch bc of blood/volume. Preload is at end of diatole after the kick. Preload optimization- if under fill the ventricles not have good ejection and perfusion of organs. If overfill same problem bc ventricles and myofibrils work together like rubberband if stretch rubber band optimally can have good kick to fling it but if understretch not go far and if overstretch it weakens and lose elasticity and become floppy of overstretch it a lot over time and also not give good ejection over time. Cardiac care problem is when diuretics or fluids when overstretch or understretch to optimize preload. Optimize amount of blood going into heart with enough volume/pressure to fill ventricles to stretch and provide effusion. When too much fluid use diuretics. Where measure preload? Both right and left ventricles at end of diastole. Catherter in vena cava or right atrium and measure pressure can indicate how much volume generated. Afterload- resistance heart must overcome to contract- if have high pulmonary artery pressure the afterload will be high. On right side is pulmonary resistance and left side left ventricle fights against systemic vascular resistance which is aorta branching off into arterioles. If I’m constricted lots of pressure generated then vascular resistance be high. If dilated out then not a lot of resistance can push everything out easily and systemic and pulmonary resistance is slow. Systolic blood pressure is afterload. Heart can change force of contraction and can give meds to make stronger contractions. Heart rate is quickest way we regulate cardiac performance by changing heart rate- chronotropic drugs to increase or decrease heart rate which affects cardiac output. KNOW Cardiac output- how much liters per minute push out of heart to the rest of body. Normal cardiac output is 3.5-8 liters/min or about 5 liters/min. depends on size. 5 liters per minute. Cardiac output is also the same as stroke volume times the heart rate. Stroke volume is 50-100 mLs per heartbeat, a good ventricular beat times the heart rate gives abot 5 liters/minute cardiac output. If heart works well and slows down to bradycardic and still push out 5 liters of fluid a minute but most who aren’t athletes and less than 60 heart rate it goes down the cardiac output. Bradycardia sustained cant perfuse body bc not enough beats for output. If heart rate really high and above 140 cant fill every time I beat can affect cardiac output. Too high or too slow cant fill stroke volume and cardiac output. Tests for cardio- nntk. Pulses- help tell systemic arterial flow (not venous flow). Capillary refill-about arterial flow Auscultation- listen to heart and lungs for fluid status. Xray- if heart too big overstretches and becomes floppy Catscan Mri Stress test –treadmill EKG Electrocardiogram to see electric pulses in heart Echocardiogram- anatomic structures, normal ejection fraction KNOW. If put ultrasound probe on heart to see how much pumping out normal is 50-60% going in is going out. So half what goes in gets out every beat 50-60% normal ejection fraction. Less than 30% ejection fraction at high risk for sudden cardiac death. Cardiac catheterization- inject dye in coronary arteries to see if patent-opened up- or blocked. With coronary heart disease and mi use this. Cardiovascular disease-leading killer of adults in the US. Arteriole pronlems KNOW arteriolosclerosis- Abnormal thickening of the vessel walls, can be normal part of aging and contributes to cardiovascular disease. (not plaque formation) Know dif bet this and atherosclerosis. Artery has several layers and are dynamic that contrict, dilate have inflammation have colegin and change over time. Cant avoid bc part of aging. Atherosclerosis- Form of arteroscilerosis hardening of walls due to plaque formation. Can avoid bc has to do qith plaque and fat deposition on the vessel walls. See used interchangeably but they are NOT the same thing. Cholestorel deposits on artery which should be smooth vessel but it reacts and becomes inflamed and grows tissue over it and plaque becomes stable and bursts damaging the vessel lining- that triggers inflammation and clotting. Lipoproteins- low and high density proteins that can be deposited. Lipids, cholesterol. Low density are main carriers of cholesterol. High density proteins help remove cholesterol from blood and take to liver. KNOW want low density lipoprotein to be low and high density protein to be high bc removes cholesterol from blood stream to liver to be broken down and excreted. Ldl deposits extra cholesterol onto vessel walls. Too much Ldl deposit on arterial walls and have atherosclerosis. Aorta opened up and smooth vs plaques and calcification. The plaque is dangerous bc can sit fine and become stable but can interact with vessal wall lining and cause inflammation and become instable, rupture and pull out of vessel calling endothelial injury triggering inflammation and clotting. Narrowing bc of plaque flowing downstream and clot form at level of injury with plaque disruption. Vessel narrowing bc of plaques and unstable plaque causing vessel damage, inflammation and clot formation at site of injury. So further narrowing constricting flow. This causes heart attack, strokes and circulatory problems in lower extremities. Atherosclerosis Signs and symptoms due to tissue ischemia Stable angina- coronary artery disease Claudication- pain in legs when walk intermittent provocation PVD Stable plaques have thick fibrous caps and partially KNOW unstable thin fibrous caps, can rupeture and cause clot to form, can completely block an artery and the clot can break free and become an embolus travelling to another area of the body. Worry about unstable plaques and we not know when stable becomes unstable plaque. Atherosclerosis- Feel pulses listen for bruits (hear swishing sound in vessel, tumultuous flow in vessel), check tissue perfusion. Doppler ultrasonography, nuclear scanning and angiography. Treat- remove risk factos. Smoking constricts vessel to make more stiff and damage and lower cholesterol. Open vessel with catheterization put a metal stent o keep vessel wall open Aneurysm- dilated area of artery, outpouching True- all three layers False- has blood flow through one of the layers Thrombus- clot remaining in area Thromboembolus- clot disrupted and detaches Embolism- clot travelled and blocking flow in dif area of body. Aneurysms: Wall of artery weakens and stretches, risk of rupture and hemorrhage Peripheral arterial disease: Thromboangiitis Obliterans aka (Buerger disease) Raynaud Phenomenon and Disease Atherosclerosis of distal arc of aorta. Things below the arc of aorta feeding lower extremities and upper extremities. Thromboanglitis/burgers disease- Not atherosclerosis. Inflame disease of peripheral arteries affects midsize vessles and KNOW linked to smoking!. Young men more often get it. Spasm triggering inflammation of vessels and trigger clotting cascase and inflammation vasospasm and decrease flow to lower extremities. Get amputations. Pain tenderness, thick malformed nails, gangrene Treat- stop smoking and inc blood flow to lower extremities. KNOW Raynauds phenomenon- is and disease Vasospasm of the small arteries and arterioles. Not linked with atherosclerosis. Vasospasm and constriction. Usually due to secondary problem. More commonly COLD environments. Young women get reynauds in cold finger get blue and pain in fingers. When warm up are fine. This spasm can occur to fingers and toes and small vessels and triggers spasm and not to cold. Raynauds dsease put on calcium channel blocker to dilate the vessels. Phenomenon is secondary while disease is not. (?) ● Both are characterized by attacks of vasospasm in the small arteries and arterioles of the fingers, and less commonly, the toes ● Raynaud Phenomenon: is secondary to systemic disease such as pulmonary hypertension, cold environments ● Raynaud Disease: is a primary vasospastic disorder of unknown origin where endothelial damage and platelet activation do play a role. Hypertension: KNOW levels Normal <120 and <80. Prehypertension 120-39, 80-89. Hypertension-1 140-159, 90-99 Hypertension-2 >160, >100 Major us problem. Some reat to stress and get hypertension and others don’t. 90-95% is primary hypertension its idiopathic and 5-10% is other called secondary hypertension. Risk factors- Family hx Age Diet Etc. Blood pressure- systemic vascular resistance and the amount going out. Primary hypertension- no reason to rule out so primary. Secondary hypertension- more with kidneys or tumors secreting catecholamine surges. KNOW PHEOCHROMOCYTOMA- tumor on adrenal gland secretes catecholamines is little bursts making pt bp go up to 200 systolic (phentylamine until sx) High bop not produce symptoms until vascular changes in heart brain and kidneys occur End organs can only handle certain amount of high pressure until get beat up. Small vessels with high pressure in heart and lungs become less dynamic and can perform effective gas exchange. Must control bp or later on have problems. Sitting at rest with feet on floor and arm at level of heart and plant fo r5 min to get real bp. 3 dif occasions for at rest for 5 min to be abnormally high for diagnosis. Treat- nntk lifestyle then pharmacologic. KNOW orthostatic hypotension: Bp drops in both systole and diastole bc of change of position. Sitting to standing, laying to standing. When change position vessels in legs supposed to constrict and hold e.t. up so not raise pressure and heart rate goes up. Is not working and heart rate not compensate greater than 20 points drop systole in standing position and they pass out and break faces. Signs and symptoms: Dizziness Blurred vision Syncope Causes- drugs (If over medicate bp then too low), prolonged immobility (lose vascular tone within 2 weeks being in bed), starvation and exhaustion Elderly very susceptible (decreased venous tone and more dehydrated as well) Disease of veins KNOW varicose veins- veins where blood has pooled and produces distended tortuous and palpable vessels. This happens over time veins become incompetent for higher pressures. People on feet a lot get this. Wear compression stockings/socks. It’s partly genetic. Venous insufficiency- Inadequate venous return over long period of time these pts also have varicose veins usually. Veins cant keep in fluid and blood so become edematous- pt has two dif skintones light brown paint and dif tones. Peripheral vascular disease. Rbcs break down in tissues and cause tannish color- get edema. Any pressure or trauma causes venous stasis ulcers. Cell death and necrosis. DVT-deep vein thrombosis Immobility top cause of dvt. Triad of Virchow know in scenario which more risk for clot formation. Pt with immobility or endothelial/tissue injury- surgery or trauma cut into with a scalpel triggers coagulation/clotting cascade. Or have hypercoagulable state- dehydrated blood is thick and viscous bc more rbc to volume and makes blood sluggish and more prone to clotting. Either dehydration or factor deficiency. If pt has clot has pain to site, warm to touch but a lot og times no symptoms. Symptoms- pain to site, warm to touch See clot with ultrasound and use blood thinners and oxygenate bc knocks out part of the lungs. KNOW SVC syndrome- Superior Vena Cava Syndrome Obstruction to vena cava. Most of time due to something occurring- cancer, tumor, lymphoma (enlarged nodes press down on SUPERIOR vena cava), superior vena cava compressed drains blood flow from upper extremities and head. Venous return to right side of heart. So if have clot, tumor or mass press on vena cava and venous return is obstructed head can get huge and arms swollen and eyes bulge out. Secondary to obstruction of vena cava. Compressibility- clot, tumor or mass on supr vena cava itself. Symptoms- swelling in upper extremities, full feeling in head and head enlargement. See veins bc back up of flow they are engorged. Heart failure The inability of the pump to meet demands of the body. If not treated right within 5 yrs people die. CHF- Inability of heart to meet bodies metabolic requirements,. Right side failure the blood flow goes backup to circulation- lver engorged, lower extremities become edematous and get organ involvement. Left side failure backs up into lungs and more dangerous bc of airway obstruction. Usually a primary disorder heart not working can be due to cardiomyopathies, coronary artery diseases, valve disorders, Secondary- Renal failure- too much fluid and heart needs to work harder and gets congested Hypertension Pulmonary diseases Anemia- make heart work harder gets tired and becomes overloaded. Rik factors- hypertension, high cholesterol, age, smoking, obesity, proteinurea (lose proteins need) KNOW compensatory mechanisms- not normal in normal working heart. Hypertrophy gets bigger when metabolic needs not met. Ventricle gets larger If not getting enough bloodflow increase SNS stimulation increase heart rate and vasoconstriction to protect heart lungs and brain- mechanisms shunt blood to core Renal response- kidneys try to autoregulate and make more blood pressure and activate RAAS cascade must know and triggered when body need more blood flow. Causes activation of renin0- hold onto water and sodium and vasoconstrict to get more blood ot core. KNOW contrast left and right sided failure Left: blood flow back up flow and volume ot the lungs Sob Difficulty breathing (sleep sitting up or use 4 pillows and cant lay flat without getting sob is bad sign) esp with exertion or lying down Wheezing bronchioles constriction Dry cough Frothy or bloody sputum cough- that much fluid in worst shape but is sign of pulmonary edema for chf left Decreased urine output Right- more systemic signs Swollen ankles and feet Rapid weight fain Abdominal pain and fullness JVD jugular vein distention swollen neck veins Frequent urination at night Preload status in these pts is high- too much fluid so try to diurese the pt first. Signs and symptoms fluid overload General illness feeling Severe fatigue and weakness Irregular or rapid HR Loss of appetite Nausea and vomiting Severe signs and symptoms when fluid in interstitial space (around lining of lungs): Arrhythmias Clots form in heart left ventricular thrombus shoots from aorta maybe to brain or maybe systemically, could stroke Liver congested and can fail. Tests- chest xray, echo, ekg, electrolytes, serum osmolarity be low bc overloaded with fluid. Treat- get rid of preload volume, decrease afterload to slow down hr and vasodilate so heart not work quite so hard. Frank-sraeling if overstretch or understretch not get good ejection and contraction. Shock ● A pathophysiologic state characterized by circulatory dysfunction, profound tissue hypoperfusion and hypoxia ● Impaired cellular metabolism due to decreased nutritional blood flow Decreased tissue perfusion KNOW dif types of shock Shock not enough blood flow to tissues and they die. Impaired metabolism of cells and decreased perfusion and cell death. Lactic acid builds up . KNOW difs Hypovolemic shock- Not enough preload to go out and meet body needs. Loss of circulating volume. Trauma, gi, hemorrhage, burns peritonitis, excessive vomiting and diarrhea. Loss of volume. Tissues not get what they need Sympathtetic Hear rate resp rate bp pulses weak and skin Raas cascade actuvate Decreasded preload and increased afterload to core Legs look pale, cool to touch bc blood to core and sacrifice limbs Change in mental status and death Cardiogenic shock- Shock bc pump cant supply volume to body. Myocardial dysfunction. Impaired cardiac output. Causes- cardiac surgery, acs acute coronary syndrome- lots of heart atttacks, dysrhtmias, cardionyopethy- weakness of heart muscle, Whatever type of shock had the END stage is build up lactic acid and it affects the heart muscle depressing it see pt becomes acidodic and ekgs slow down about to go to arrest then leads to pump failure. Last manifestions of other forms of shock. All kinds of shock cause lactic acid but this is last ot other forms of shock. Decrease in stroke volume and cardiac output, decrease in blood pressure and blood flow and inadequate tissue perfusion. Signs and symptoms- Lack of good cardiac output. Cyanosis If have chf bp is initially high with all the fluid and if yrs later not control the heart starts to fail and bo low. Bp low in cardiogenic shock as late stage of heart failure. Resp rate high to compensate. Too much preload and cant pump out and low cardiac output. Change in neuro status bc cant perfuse brain. 3 forms of distributive shock change in blood vessel tone cant constrict and so fluid seeps into tissues and lose flow in heart and vessels. Loss of blood vessel tone and cant perfuse the end organs. Not have enough perfusion pressure Neurogenic- spinal cord injury Anaphylactic- allergic rxn causing systemic dilation of vessels, remove allergen and give vasocontrict meds then fine Septic shock- immune system reacts to source of infection! And cause vasodilation state to get mediators and cytokines to defend the host. Out of wack inflammatory response plus infection. SIRS + infection= sepsis Sepsis + organ involvement- severe sepsis So vasodilate cant keep fluid in vascular space, bp low cant perfuse end organs= septic shock. Septic shock- Ask if history of infection. Cannot constrict vessels with septic shock state bc immune response is powerful and all vasodilated the catecholamine cascade cannot appose the vasodilation- cannot constrict the vessels. Heart rte shoots up but vessels not respond to catecholamine surge. Decreased preload bc fluid goes into tissues and outside the vascular space but cardiac output is high bc if aorta and all arterioles open up not a lot of resistance to flow from heart so cardiac output is double than normal 10 liters but still with low systemic vascular resistance not mean making to organs bc vasodilation the whole way. A lot of blood coming out but goes into interstitial spaces 3rd spacing not making it to organs. Decreased resistance so better output, pulses be bounding!! Bc have no opposition to flow. The skin will be warm and pink but very swollen bc all the volume shifting into tissues. Bounding pulses bc no obstruction to flow but organs not getting that perfusion. (other types of shock constrict and shunt blood to core, here cant shift to vital organs and go into multi-organ failure. Not able to compensate. Blood pressure is low bc not have any resistance bc flow goes into interstitial spaces. High cardiac output but low preload. Decrease preload, increased cardiac output, decrased arterial constriction All shock states can put in multiorgan failure, resp distress, acute kidney injury, gi bleed organs fail. Septic shock can trigger dic- problems with vessles causing cascade Optimize cardiac output and preload, restore tissure perfusion, fluids not give in cardiogenic shock- try to diurese that pt. septic- reverse infection and if vasodilated put on vasoconstrictor meds like norepi- alpha agonists and beta 1 agonists. 2/27/17 Print out EKG packet Diorders of Cardiac roblems Problems of pericardium: Layer surrounds heart and holds a little fluid. When becomes inflamed: acute pericarditis- inflammation of pericardial sac. Double layered sac around heart with some fluid so notstick to heart wall. If gets inflamed causes pericarditis. Can be caused by a virus but many times idiopathic (no underlying cause). Can be caused by MI, heart attack, ure- not enough fluid can trigger pericaridits also surgeries, medications, and autoimmunedisorders (lupis). The pericardial membrane becomes inflamed and roughened and makes capillary walls vasodilate and fluid leaks out and triggers mediator release causing fluid release and exudates drainage at area of inflammation. Signs and symptoms KNOW significant ones: Sudden onset of severe retrosternal chest pain that mimics a heart attack KNOW- pain worsens when take a big breath in, inhalation bc pressing onto pericardial membrane. Chest Pain that worsens with respiration and laying down- pericardial sac more on top of heart. Pain ccan radiate to back Dysphagia, restlessness, irritability, anxiety, weakness, malaise- if underlying infective agent feel sick. Hallmark-inflammatory mediators SIRS response- low grade fever and sinus tachycardia and friction rub- listen with stethoscope over heart hear gritty coarse sandpaper sound. Ekg changes If inflammation occurs and capillary dilation and permeability and fluid accumulates then pt can become hypotensive and drop blood pressure bc fluid presses down on heart. Pulses paradoxis- drop in … Decrease in blood pressure Diagnosis and treatment- look at ultrasound of heart and see irritation and fluid of pericardial sac may take fluid out with needle- pericardiocentses. Anti-inflammatory agents c inflammation problem, treat underlying cause. If fluid increases-pericardial effusion- accumulation of fluid in pericardial cavity. Can be serous fluid – plasma and clear. Can be an exudates from infectious source or serosanguineous- bloody. Thoracic trauma so bleeding in the are. If heart cant pump out bc failing then fluid backs up can just be serious. When take fluid out they will differentiate the dif types of effusions fro sample to see infectious or trauma or due to heart failure. Dif cellular components of fluid shows this. Remove fluid based on symptomology, sometimes resolves no own. PERIDCARDIAL EFFISN VS CARDIAC TAMPONADE Cardiac tamponade- fluid accumulates to extent that compresses heart and affects cardiac output. Anything over 100mL can cause tamponade (not hold a lot of fluid in that space). Can happen due to any trauma or bleed in chest. A heart attack also can cause accumulation of fluid if heart not working as well the fluid backs up and compresses heart Signs and symptoms KNOW: Catheter in central big vein and heart not pumping well and fluid backs up have INCREASE CENTRAL VENOUS PRESSURE. Increased fluid in the vessels bc heart cant pump that fluid out. Increased cvp and also JVD sign of fluid overload. Bp still be low bc heart cant pump out and see in veins overloaded. Fluid overload in heart Hypotension Shock-like symptoms Low bp Heart rate high and if cant compensate be dead bc no cardiac output at end. CVP JVD, shock, heart sounds inaudible (we do baseline assessments on all pts bc over 50 can have heart attack and hear clear heart sounds this morning then ekg changes and cant hear heart sounds know he is tamponading). First Right side heart fails bc lower pressure system more susceptible to any constriction. Fluid backs into right side then lungs. Can see fluid on CT scan or Echo. Pericardiosentesis to remove fluid with needle and hopefully serous fluid coming back. Coronary Artery Disease- Any cv vascular disorder that narrows or occludes coronary arteries. 1/5 deeaths in us leading cause of death in IW. Death due to insufficient oxygen to heart muscle. Men >45 risk and women >55 KNOW risk factors for CAD: Number 1 ATHEROSCLEROSIS- narrowing of vessels due to plaque formation Dyslipidemia- increased LDL Hypertension- high pressure in coronary arteries damages vessel walls Smoking- irritates and constricts vessel walls DM Obesity Sedentary lifestyle- decreases HDL which helps cholesterol to be removed SIGNS & SYMPTOMS: SOB Syncope if MI White men chest pain radiating to left arm, everyone else has atypical signs- GERD, GI upset, heartburn bc heart lays on esophagus Abdominal complaints Nausea and vomiting Mental status changes Resting ekg abnormal See if ekg changes with resting and exercise Cad requires lifetime care- open vessel and prevent any clot from getting larger. Bypasss disease with bypass surgery with vessel from chest wall or leg. Can happen again if not change lifestyle or diet. Medications. Plaque tearing from vessel wall so injury to vessel wall and get clotting cascade- lack of blood flow to area of vessel wall is heart attack/MI. KNOW types of angina Acute coronary syndrome many times present with Angina. Chest pain and SOB Stable angina- symptoms occur only with exercise or stress and are relieved with rest. Lie down and within 15 min gone. Also take medications like nitroglycerin and pain is relieved. This indicates partial occlusion of coronary artery- not blocked entirely yet but is a warning sign. Prinzmetal’s angina- results from vasospasm of coronary vessels without underlying atherosclerosis- when look at vessels they are clear just a spasm. Women more get this. Also called vasospastic angina. Sont have athero, blockage or clot just put on calcium channel blockers Unstable angina- pain at rest, indicates MI, pain lasts longer than 20 min. can happen with minimal stress or exercise or just wake up in middle of night with chest pain showing substantial CAD. Acute coronary syndrome- for plaques or clots blocking flow to heart. Usually starts with stable angina. When exercise feel smth and then goes away- can last a few years. Once have unstable then need help. NSTEMI- Non ST elevation heart attack or MI- plaque formation causeing decreased flow toMyocardium and causing ischemia, muscle damage- heart attack. STEMi- st elevation MI. stemi is complete occlusion and if not act quickly then vessel will completely infarc and die (very small amount of time to open vessel and increase blood flow). Nstemi some flow and some ischemia but not as much occlusion. Know causes of MI Dysrythmias- make heart work hard or inappropriately makes problems in flow Embolus- clot in coronary artery Thrombosis- clot elsewhere traveling to coronary artery Atherosclerotic occlusion- can still have angina without plaque or clot- have vasospasm, Prolonged vasospam Triggers- rapid rise in bp, increased workload on heart, activation of blood clotting mechanism by infection or otherwise. Stable plaque leads to stable angina. Unstable plaque with ulceration or rupture and thrombosis-> acute coronary syndromes transient vs sustained ischemia. KNOW pathophys of MI: Cellular injury occurs bc of lack of oxygen to area of blood vessel. Greater than 20 min leads to cell death. when cell death occurs scar tissue replaces muscle and it does not contract. Decrease on contractility will lead to heart failure bc heart not working. Decrease flow in wall- reperfusion within that hr. Signs and symptoms KNOW: Sudden onset of pain can radiate to jaw arms abdomen or shoulder Tightness, crushing feeling Lasts 15-20 minutes Not relieved by nitroglycerin or rest! Heart compensates by becoming tachycardic Diaphoretic- sweating Tachypnea, Dyspnea Anxiety, feeling of impending doom LOC changes Nauseas/vomiting Cardiac dysrythmias Denial of symptoms EKG changes- electrical conduction of heart. Of not good flow then disrupts electrical conduction. Enzyme changes- enzymes spilled in blood when the heart is damaged- when muscle wall not getting enough flow so some enzymes elevate in blood from damage to myocardium. KNOW triponon level .2 Mcg/L. Triponin more spec to cardiac damage. They are significant for MI. some be 0.03 less than 0.5. a whole number is not normal, higher than 0.5 not normal. The levels should be drawn every 6-8 hours times 3 for 24 hours. Must stay and have serial triponins bc enzymes may not spill right away or accumulate after a few hours. Must do 24 hours if have risk factors for MI bc evidence based practice. Interfere with MI is kidney failure so if have dialysis triponin interfered with. So if positive not be so much so. If in kidney failure and high must see if cant clear triponin enzyme. Still not be more than 3. CPK sign of inflammation but know triponin. Rule out otherthings. Check electrolytes, cbc and blood gas. Check ECG 12 lead serially, chest x ray. Blood loss- not enough blood to heart have MI not related to CASyndrome or plaques can be from oxygen carrying capacity so cbc. Check angiogram- vessels echo to see function and stress test. Treat- oxygen, pain relief, not stress. Medications to bust clots and balance electrical conduction. Blood thinners to dissolve the clot. Lifestyle modification, rehab, exercise slowly to not stress heart too much. Cardiomyopathies: lack of function of heart muscle that are unavoidable not common but lots of pts have weak hearts. The cardiac muscle does not work properly- can be due to repeated MIs causing ischemia to heart. Several areas of heart scarred so not contract properly. Heart changes to get larger and hypertrophy and becomes floppy bc overused so wont constrict and contract well. Types: (get) Dilated- congenitally Hypertrophiv-- block left ventricle and cause inability of heart to fill Restrictive- like from lupus cant pump properly Causes- due to remodeling caused by myocadial and neurohumoral responses to ischemic heart disease and hypertension. Due to infection, toxins and nutrition deficiency. Virus can attack muscle and cause damage that is irreversible. Valvular defects: KNOW them Each of the four valves can be defective. We worry about left side more. The aortic valve and mytro valve bc they work hard. Left is where its at. Stenosis KNOW vs regurgiatiaton Stenosis- valve not open all the way harder to force blood thru it, narrowing of the vave. Aortic stenosis means aortic valve stenosed so left ventricle have to work harder to push blood flow so caused ventricular failure eventually which is a death sentence bc supplies blood to rest of the body. Within onset of symptoms if not get valve replaced thnen 80-1005 death within first yr. can have calcification cause this, Regurgitation- vlave cant close all the way. Backs up to atrium. Bicuspid stenosis then backs into atrium- not good filling and not good preload. They get used to more volume or cant pump until get valve fixed. Left side valve failures- Mitral valve disorders, mitral valve stenosis, mitral valve regurgitation- damage to valve many times from infectious source, mitral valve prolapsed, aortic valve disorders aortic valve stenosis, aortic valve regurgitation. Left side heart- mitrovalve regurgitation- back up flow into left atrium and stretches and enlarges. Atrium is where conduction begins so have conduction problems. Mytrovalve stenosis- difficulty dumping into left ventrile so left atrium enlarged. Aortic valve regurg- left ventricle is floppy and distended KNOW MITRO VALVE PROLAPSE what is and who affects They prolapsed and balloon back into left atrium- degeneration of the leaflets- cause mitro regurgitation. Common in young women and they not know have it. Bc mitro valve billow up into left atrium. May be asymptomatic but if a lot of regurg and left atrium enlarge have papitations and tavchy and ekg changes and they pass out and become fatigued. Damage to the leaflets holding up valve and have regurg risk for infection seeding onto valves. Mitro valve prolapsed higher risk of bacteria clump onto valves not working properly. Know Infective endocarditis- infection of inner heart spec attacking the valves. Must have portal of entry going to the blood and blood infection seeding and growing on the valves or a valve. Iv dug users have high risk of infective endocarditis- dirty needles right into the bloodstream. Any wound or infection or uti that crosses into bloodstream, even pneumonia can attack the heart. Usually iv drug users and dental periodontitis. Usually have to have source of infection, usually blood to cause bacteria to go to heart valve. They like them bc the cordae tendaney sitting there. A/B can be ineffective at treating those bacteria bc they clump there and form colony which can see on Echo. Can see huge clump of white on there called vegetations. They can be on a/b for 6-9 months to clear infection and if not work bacteria kils valve and heart needs new one. Signs and symptoms of infection: Fever Bacteria can flick off embolize and go to brain causing stroke. Can see petichiae clumps of red around body which are bacteria flicking off into circulation. Trat- A/B and replave valve Rheumatic Heart disease- inflame of myocardium, pericardium and heart valves due to rheumatic fever virus. Signs and symptoms: Strep infection- sore threat HA fever abdominal pain swollen glands Need A/B and sx- use for five yrs or until 21, affects young people. If pregnant nonviable fetus. Aortic valves not get infective commonly bc high pressure system. Mitro valve not as high force so get commonly Congenital heart defects- not go into so much. Atrial septal defects, centricular septal defects. Holes in heart or arteries branching off not where supposed to be. Need sx for these. Shunts- asd or csd require a shunt. Left side stronger pushes left to righ side is okay bc oxygenated. Right to left shunt not good shunt bc deoxy- they not lie long. EKG interpretation- Recognize the arrhythmias we will talk abt. Sinus rhythm, tac, brady a fib, v fib, a flutter. Electrical conduction of heart starts in Sinoatrial node and travel to ventricles. To evaluate the electrical activity of heart use electrodes which usually have gel in middle which is conducting gel to get electrical signal from sinoatrial node to ventricles. Shows dif areas of heart so matters where place them. Not need know placement. Looking at infr and lateral wall. With arrhythmia check if leads placed properly. Need be below heart to see if signals going across and down from heart. Signal from Sinoatrial node down ventricle is towards heart should be pos deflected. Camera looking at signal coming towards it. Look at leads two and three bc most heart attacks in infr and lateral walls. That’s where see change. Know all concepts bc we do simple ekg interpretation. Electric signal precede the action of the electricity. Need impulse to produce mechanical activity and muscle contraction which her in pulse and hear with stethoscope over heart. Listen- lub dub and feel is pulse. If look on screen nice ekg electrical conduction and no muscle contraction bc no pulse and no sound in heart. Electrical activity is electricity from intrinsic electrical conduction system. Abnormal beats show off impulses. Electrical activity prepares heart for mechanical contraction. Not always followed by mechanical activity. Recorded on paper as EKG tracing. Pacemakers of the heart KNOW SA node- dominant pacemaner of heart setting the beat intrinsic rate (on its own) 60-100 beats/minute. Self conducting. If SA node is wacked then use AV node. AV node- backs up with intrinsic rate of 40-60 beats/minute. Not sustain life for very long. If av node not working then ventricular cells Ventricular cells- 20-45 bpm not conducive for life. Normal impulse- SA node, AV node, byndle of His, bundle branches then right and left perkinje fibers. Electrical tracing on paper transmit electrical conduction as wave and defining specific areas. SA node is P wave of the heart and put leads that signal towards leads Positive conduction p wave. Bundle of His bundle branches and perkinje are PRS P wave- atrial depolarization signifying atrial depolarization. QRS- ventricular depolarization. Higher shows voltage and time. Higher voltage bc takes more energy to transmit that signal across the thick ventricular muscle so voltage needed is much higher than across atrial muscle. Voltage for p wave mch smaller than qrs for signals to cause muscle contraction. T wave when ventricles resting and repolarizing. Sodium and K+ and Ca+ channels getting to baseline getting rdy for next contraction. Atrial depolarization- atrial contraction/kick at end of diastole, this delay lets good filling before contraction is P-R interval. Bottom of Pwave befire Qrs. P to q is emptying atrium and qrs is contration. T is repolarizing. EKG paper KNOW normals: Small boxes and large boxes. Small within large bosxes set up in time increments. Ekg shows electrical conduction and waves over time and voltage. How much time get from sa node to av node to bundle then to vesicles. One small box -.04 s and one large box is 25 boxes and 0.20 s. horizontally. Vertically one large box voltage 0,5 mV millivolts. To contract gets very high. But if heart disease and not move much tiny voltage sometimes hard to see. For rhythm to interpret assume 6 second strip. Need minimum 6 sec strip to graph heart rhythm to interpret a correct finding! Calculate the heart rate!! P-R interval: 0.12-0.20 s to go from SA node to AV node. 3-5 boxes is normal. QRS .04-0.12 s and 1-3 boxes very narrow bc fast and forceful. (pr is sa node emptying into ventricles with atrial kick at end, conduction to left ventricle for depolarization here is very quick). If longer than that wide QRS something wrong. Normal sinus rhythm- electrical impulse in sa node conducted normally. Anything outside of that is arrhythmia. Can never cmbine normal and not normal. Normal sununs rhythm is 60-100 bpm. Regular rhythm means if mark it out if falls where supposed to. No caffeine than heart 62 62 63 but stay where supposed to not 65 78 43 62. Says at 62. Regular pattern. Falls where expected to fall. Caliper to measure distance falls where expected. Not shorter or longer intervals. P qave should be nice little round hill 12-20 secondes. Qrs 1-3 boxes narrow and .04-.12 s. Any deviation from these is arrhythmia. Arrhythmia formation- Sinus node problem, av cells, av junction or ventricular cells problems. Sa node can be too fast or slow. Sinus bradycardia is less than 60bpm. How count heart rate? Count QRS bc its conducting the ventricle, the beat. The narrow long spikes and multiply times 10 in 6 second strips. 3 * 10 = 30 bpm. (she give 6 second strips only). Too slow so sinus bradycardia. But PR interval is beginning of bottom start of P wave almost to Qrs start upward. Is 3-5 ok,, qrs 1-3 boxes is okay. So just too slow conduction.. Sinus tachycardia- 13 *10= 130 bpm too fast. Usually due to something else- heart rate 100-140 due to fever, hypovolemia to compensate, low bp, stress, cocaine use, dehydration, pain. We don’t treat sinus tachycardia with med for heart rate usually treat underlying cause first unless older and risk for MI.above 140 is heart problem to fix. Pr interval ok qrs okay. Everything narrow and look like supposed to. Look at length it takes conduction cycle to complete and the voltage. We not focus on voltage. Atria conducts using P qave, PR interval. If problem where sa node fire continuously too much P wave. Qrs try to do thing but have problem with p waves. Atrial flutter IKNOW- Continual firing somewhere in sa node. Bc not have one dominant p wave not called p waves bc not sure which dominant and which running like a circuit and firing over and over. If each was a p wave conducting into qrs would be 300 bpm. A flutter is every second or few impulse generates qrs and others blocked. P waves different bc pointy- “saw toothed waves”. A flutter not see in other arrhythmias is saw toothed waves/jagged teeth waves. We not know which real p wave so not call them that. Conduction of ventricle is ok bc qrs is narrow and fine. Every 3rd or fourth wavelets the ventricle kicks in. Its regular rhythm bc qrs deploys exactly when supposed to- same pattern. If felt the pulse, the qrs ventricular contraction, feel regular rhythm. If felt pulse not know a-flutter and they not know it bc qrs marks self out regularly. Rate 70 regular. Regular pattern p waves? Flutter waves, not p waves bc cant point to right one. PR interval? Cant say cant point to PR interval. Qrs duration? Normal 1-3 oces. Flutter. If primary pacemaker not sa node here bc crazy firing so losing during interval affecting the kick during pr interval. A flutter lose atrial kick bc lose PR interval time. Keeps firing ventricle and lose delay of ventricle and kick. Any atrial dysrythmia without pr interval and atrial kick the blood in atrial can pool and clot- high risk for clotting!! These pts on Coumadin and higher doses of heparin. Anticoags. Clot in h eart risk to go to brain and stroke. No pr interval and lose delay lose atrial kick the blood stays behind and pools and clots can also go to legs and cause dvts. Atrial cells can fire continuously from multiple foci- atrial fibrillation. Instead of same pathway continuously firing its everywhere firing a lot. A fib No orgainized atrial depolarization- no one normal P wave. Atria trying to fire a lot instead of contracting. Very common in elderly. A fib vs a flutter KNOW: Av node lets some pulses thru and have QRS but not happen in any patterned wat. HALLMARK- IRREGULARLY IRREGULAR PATERN bc qrs get in when can but no pattern to it. Rate 100 bom, regular? Irregular, p waves- none, pr interval- none, qrs duration 0.06 s. feel pulse irregularly no pattern. Can diagnose by feeling pulse. High risk for clotting bc no atrial kick. Ventricular cell problems: Can fibrillate as well. Fire continuously or it can go fast. Vent fib or v tachycardia. Ventricular tachycardia: Av node down and sa node down, vent cells take over. Bc conduction pathway from ventricle not narrow now bc get sa node signal its wide and bizarre. Ventricle itself generates own rhythm is wide complex. If ventricle kicks in 20-45 if go fast then alive a bit bt problem is not work long so high risk of dying arresting. V –tac with a pulse have some time. V-tac without pulse get cardiac arrest. No P waves, wide QRS. It is regular though@@ Rate- 16*10= 160 bpm. Regular? Regular rhythm! Regular pattern!!, p waves- none, pr interval- none, qrs WIDE >12 s ventricular tachycardia. With pulse shock pt at lower doses to repolarize them, or get med. Without pulse do cpr and defib- shock at higher dose. Ventricular fibrillation- No P wave and no P interval. NO QRS Cant count anything Rate- none, ref? irrefular p? none pr? None qes wide if recognizable in cardiac arrest! Know some of st elevation and nonst elevation- Most heart attacks in infr and lateral parts of heart. Problem with ischemia, necrosis, scarring- nor enough blood to heart see heart muscle damaged and electrical conduction damaged. KNOW st elevation changes: Before injury see ischemia leading to infarction- dying muscle irrevivable. During repolarization T wave see changes in T wave bc there is some obstruction to that conduction due to dying or dead tissue. ST elevation= NO FLOW, if repolarizing means heart resting and not contracting, blocked path so try to go around the blockage takes long time and ST elevation changes. Bc of diversion in conduction the st elevation would occur. Start with ischemia st depression than become st elevation when infracting. P fine and qrs there and fine but T wave takes longer to go around injured parts of heart so st elevation- more voltage needed and longer trip to go around injury. ST elevation MI. important bc if see on Ekg and not open up that area it will be dead tissue. More voltage around area of infarc and longer time. Electrical conduction must go around heart with more voltage to get through. Not completely obstructed though. Don’t need know q. ECG PACKET: P4 A FIB AND A FLUTTER BIGGEST CONCERN CLOTS AND STROKE. 4 questions: – 1. Are P-Waves present? – 2. Are P-Waves occurring regularly? – 3. Is there a P-Wave for each QRS? – 4. Are the P-Waves smooth, rounded, and upright in appearance? Rate 80. Normal sinus rhytm. P5 Cant say p wave cant say p wave for every qrs, regularly irregular so afib. Rate is 100, but cant say afib tachycardia!!! Or afib bradcardia!! Bc means sa node is primary pacemaker and p wave for evry qrs. If rate 105 afib with rapid ventricular response. Fast or slow afib but not afib tachy/bradycardia!! Regular rhytm but flutter waves. A flutter. Regular. V-tac. No p waves. Wide qrs. Bottom p6 90 beats still sinus rhythm, bc have p wave and qrs and regular Regular sinus rhythm P9 no p wave for every qrs. P wave not normal. Qrs is okay. Problem is atrial conduction. Rate is 70 normal. A flutter bc has 4 to 1, every fourth beat qrs, regular pattern. Middle is sinus bradycardia. Slow less than 60. . Bottom is notmal sinus rhythm P10 Super ven tachycardia not need to know. Rate 80 not p wave distinguished, irregular. Long gaps and shorter gaps. A fib Also a fib no p qave oor pr interval P11 rate 80 p wave before each qrs, rhytm normal. Normal sinus rhythm rate 50,p for every qrs, regular pattern, sinus bradycardia rate 120, p before every qrs and regular sinus tachycardia p7 top is rate 30. if too fast or slow output not good. Not fill enough. 3/6/17 Respiratory system (resp tract infections after exam, it’s not on exam ) Hemostasis, cardiac interpret ekgs, resp part 1 on exam Conducting airways- conducting ventilation. Not perform gas exchange. Lung disease affect conduct airways cause structural problems. Conducting airways end at the bronchii and when branch into aveoli get into resp ventilation and gas exchange. Conducting airway important but really gas exchange are. Type 1 alveolar cells- provide structure 99% are type 1. KNOW type 2 alveolar cells- secrete surfactant which reduces surface tension and increases compliance so makes alveoli very dynamic and elastic. They are responsible for compliance of alveoli. Little grapes at end of bronchioles and can expand and dynamic damage to type 2 cells makes alveoli become stiff without surfactant and not as dynamic and not as able to participate in gas exchange as effectively. Cpr with ambu bag- putting air into lungs. With someone with alveolar damage when bag the pt the bag gets stiff and cant press down on it bc lungs are stiff and noncompliant. Lung disease and alveolar injury of type 2 cells the alveoli become stiff and noncompliant and participate less and less with gas exchange. Alveolar macrophages- clear out infectious processes, debris and keep lungs clean. When breathe in take in particles of room and lungs filter all that if macrophages work properly. Pulmonary circulation part of gas exchange and delivers nutrients. Acts as a reservoir for the left ventricle. Serves as a filtering system to remove clots, air, and other debris from circulation Capillary system around aveoli and helps for waste removal. Not test on terminology but be part of stems of qs and descriptors. Ventilator- movements of air bet atmosphere and alveoli. Lung volumes- deep breathe in= tidal volume how much going in. 5-7mLs/kilo (nntk) it depends on size of the person and size of lung cage and how much expansion the alveoli can participate in (if stiff cant get in 300mLs needed) vital capacity- amount of air expired by forceful expiration- effort pushing out all air. Residual volume- amount if air in lungs after maximal expiration. Should have a bit of air leftover in alveoli but not a lot. Enough to keep them open. If a lot air leftover not participate in lung exchange its stuck in there. Dead space- area where no gas exchange taking place. Can be part of conducting airways. If tumor in lung it not get gas exchange bc obstruction impedes alveoli function around that. Due to tumor, a bunch of mucus, chunky decries and bacteria in the lung tissue. Minimizes gas exchange taking place. Clot in pulm vascular system- clot in bloodflow to part of bronchus so blood not take place in gas echange either- lungs and perfusion part of this when blocked and not part of gas exchange. Breathe in and out using muscle diaphragm push cage up and out and down and in. not enough protein on board diaphragm not work as well bc muscle. Accessory muscles- intercostals, ribs. Someone bringing with chest has 5 min before collapse bc takes a llot of energy and difficulty breathing. Elastic chest wall and lungs- surfactant. Big burn on chest and skin tight from scarring and damage might prevent proper inhalation and expiration. Resistance to air flow thru conducting airways- bronchioles are smooth muscle they constrict and dilate. If have constriction disorder there is more resistance to flow/gas exchange. Compliance0 how easily lungs can be inflated deoends on elastic and collagen fibers, water content- increase in water is stiffening of lung tissues and don’t conduct air effectively, alveoli surface tension. PaO2 partial pressure of oxygen in the lungs- amount of oxygen dissolved in the plasma. Oxygen buond to hemoglonbbin called oxyhemoglobin- certain conditions making oxygen more tightly or more reasily released from hemoglobin. 9not need know disorders). Normal 95-100% saturation of hemoglobin use pulse oximeter to measre- measures ox saturation. Arterial blood gas measures partial pressure disscolved in plasma 60-100% of paO2 off of a blood gas. Pulse ox not as sensitive as pao2 off a blood gas can be 20 point dif. 90% o2 sats and have pao2 of 60. Issue with oxygenation and pulse ox is good beter to get blood gas pao2. Blood gases- can look at paco2 partial pressure of co2 in blood 35-45mmHg normal- loosely bound to hemoglobin. Exhale lose co2 and bicarb ion kidneys rid of some co2 by dumping bicarb and lungs exhale co2. Can regulate co2 via resp rate. Most of us use central chemoreceptors in brain stem to measure co2. When sleep not think about breathing consciously – co2 can rise when sleeping, brain stem senses this co2 and ph and stimulates deeper breath. Most of us respond to increase in co2 to blow it off. COPD- these pts with lung disease their bodies adjust to high levels of co2 and become more used to it so use low oxygen as trigger to breath. Periph chemoreceptors in carotid artery and aortic arch measure o2 so when see low oxygen there they use as trigger to breathe. Stretch receptors increase lung volume. Coordinattoin of lungs and brainstem medulla and pons to inhale and exhale. Any brain injury, narcotic drug overdose, interferes with these signals and affects the rate. Resp switched on or off when speaking or singing. Signs and symptoms of pulmonary disease: Dyspnea- shortness of breath Abnormal breathing patterns- kussmal and cheyne stokes. Kusmal- rapid shallow breathing usually acidodic pts trying to blow off co2. Cheyne stokes- irregular breathing pattern like apnea and then rapid and then apnic, and also Tachypnea. Pt who is pretty much dying- impending resp arrest usually due to brain stem injury. Hypoventilation and hyperventilation Cough- what type, sputum, hemaptosis (blood in sputum), yellow green dif bacteria, pseudomonas is green usually Cyanosis KNOW LATE FINDING- blue fingers digits mouth central oral mucosa on dark skinned look at oral mucosa Pain when take breath Clubbing- rounded and flat fingers chronic hypoxic state- cardiac or resp disease process had for a while, nails last to get oxygen so change configuration Abnormal sputum- color and consistency Disorders KNOW HYpercapnea- increase co2 in arterial blood so need to have a blood gas to measure co2. Causes KNOW: Hypoventilation of the alveoli, not enough gas exchange so not enough removal of co2 so breathe too slow bc disease of medulla- tumor, trauma, CNS disorder depression of resp center by drugs (narcotics Opioids) Abnormalities of spinal conduction pathways Thoracic cage abnormalities- resp muscle problem or stab or multiple rib f problem bc cant take deep breathe Large airway obstruction Increased work of breathing- initially blow off co2 but when trying to breath really fast for a while get dizzy and fatigued and then start to retain co2. Tires you out. Tidal volume amount of volume per breathe if cant inhale big cant exhale big. No drive for resp rate by drug overdose or cns injury have low tidal volume x rate minute volume amount of exchange in one minute. Become acidodic and drop o2. Increases co2- not painful and makes you sleepy so have narcotics and then more sleepy- narcotizes you and so ppl die easily of overdose bc affect resp rate. Acidodic affects heart vasodilate drop bp and diee Hypoxemia- reduce ox concentration Not giving enough o2 content. Decreased O2 content of inspired gas Hypoventilation Diffusion abnormality- Alveoli little thin fragile sac with thin wall with one capillary wrapped around it- soggy capillary letting fluid or debris or junk seep have problem to diffuse gases across cap bed. Abnormal ventilation-perfusion ratios Pulmonary right to left shunt- congenital abnormalities Hypoxemia- obstructive lung disease, restrictive lung disease, pleural disease- cant exchange with blood. if hypo or hyper ventilate cant get enough o22 across so die. Cyanosis- bluish discoloration Causes: Decreased arterial oxygenation Pulm or cardiac right to left shunts Cold env Anxiety KNOW concept Ventilation-perfusion mismatching- blood not become oxygenated so areas of lung not getting perfusion or blood not go to parts of lung that does have o2. Due to mechanical problem. Clot in perfusion portion or scar tissue or tumor in lung tissue so mismatch bet perfusion and ventilation Pleural space problems- parietal lines wall and diaphragm; visceral lines lung itself. KNOW what pleural effusion is- in pleural space in lining lungs have pleural cavity lining the lungs with a bit of space bet two layers and if too much fluid there pushes against lung tissue and lacks ventilation to that lung area. An be do to too much fluid or too little removal of fluid. Can be due to fluid shift third spacing bc not enough albumin. Also infection cause fluid bc of debris. Also inflammation cascade- heart weak so fluid goes to all spaces including pleural space. Volume dependent so fluid pushes against lower lobes and alveoli cant inflate properly called atelectasis- collapse of the alveoli (not whole lung) KNOW bc be one of the descriptors. Bit of pleural space fluid push against lung and cant expand properly is atelecttasis. KNOW types of effusions: Transudative- watery fluid diffuses from capillary bed bc of changes in bp or capillary oncotic pressure. Third spacing also heart cant keep from seeping out. We drain it and test that effusion to see the origin. Depending on its components determines if transudative or exudative.. lack of oncotic pressure or bp. Exudative- drainage from pleural space indicates inflammatory process going on. Could have wbcs in it and plasma proteins. Pt has infection like pneumonia- when inflamed cap vessels in sirs dilate and let out fluid so exudates from infectious process can occur and have that type of drainage in the pleural space. Get debris from infectious process. Pus empyema- debris of infection dumped into pleural space. It is exudative but not just fluid easily drained but gets walled off itself- loculated. Difficult to drain have to go in and scrape out. Much harder to eliminate. Fluid pushes against lung tissue decrease in alveolar expansion and causes symptoms. Hemothorax- blood in pleural space from chest trauma or chest sx. On xray cant tell dif if blood watery or exudative fluid. Can see these on Xray- plural effusion. Sometimes ct scan too. Flail chest KNOW: Rib fracture- chest wall trauma contusion, mva, ejection, stab wound, etc- producing free floating sternum. More than 2 ribs broken have underlying lung contusion bruising and damage to lung tissue as well. HALLMARK - paradoxical chest wall movement. Shortness of breath, chest pain and when take breathe in it sinks down instead fo staying inflated. Pneumothorax- air or gas in pleural space caused by rupture in visceral pleura lining around lung. Fluid in pleural space cause effusion but if large enough that fluid/blood/air large enough compress lung get pneumothorax. Can have effusion without pneumothorax- lung still intact. In thorax enough fluid/gas that compresses lung tissue and not just alveoli. Impalement or stab wound can get open pneumothorax- take air in goes in thru hole and compresses lung tissue further= open communicating pneumothorax. Penumo=air, thorax. Air enters pleural cavity takes up space and restrict s lung expansion. Can be spontaneous- air filled blister on the lung ruptures. Traumatic- more common air enters chest injury and compresses lung underneath. Open phenumothrorax take breath in and air pushes against it collapsing it. When air released it expands. On inspiration lung collapses, exhale lung expands a bit again. KNOW. (heart not shift to one side bc air does get out) Tension pneumothorax KNOW- most dangerous kind Hallmark- great vessels and heart and lung pushed to opposite side. Large enough pneumothorax air goes in compresses lung and pushes great vessels and heart to opposite side. If push on great vessels blod flow gets restricted so drops or stops cardiac output. Decreases cardiac output or stops it – cardiac arrest. Hypotension and subsequent cardiac arrest. Need to evacuate that air immediately. HALLMARK- tracheal deviation trachea shifts from midline to opposite side. Right side impalement and now air filling up pleural space pushing lungs and trachea to opposite side left. Mediastenum to opposite side. If put stethoscope over that part of lung hear nothing bc lung moved to opp side or complete lt depressed so decreased or absent lung sounds there. cardiogenic shock drop bp to nothing bc compressed and no cardiac output. Needle decompression so resolves the situation (air not come out so not communicating) Signs and symptoms: Sudden pleural pain Tachypnea Possible mild Dyspnea Mediastinum moves to unaffected lung Cardiogenic shock- no output. Tension pneumo can occur with both air or blood fluid. Hemothorax also can cause a tension pneumothorax not just air. Atelectasis- collapse of alveoli Effusion and when cant take big breaths like wounds, incisions, open heart surgery. Collapse brings fluid and leads to infection. (Insentum spiramotor- not fully ambulatory plastic machine to take big breaths and get tidal volume bc every hr need to take 10 times an hour bc when sit around we take big breathe but not when bed bound. Prevent atelectasis. Tell them every hr do it bc fluid in lungs and get pneumonia. Not want while in hospital). External pressure against alveoli, Signs and symotoms’; Dyspnea, Cough Fever inflammatory response to infection Leukocytosis bc infection Come out of or biggest complication is atelectasis bc lying flat and not great ventilation. Post-op fever from atelectasis usually. Absorption atelectasis- using anesthetics and o2 washout from getting o2 artificially reduces surfactant which keeps alveoli open so now doesn’t. COPD chronic obstructive pulmonary disease- 3rd leading cause of death in us More than 50% adults not know have it. Smoker 30 yrs and say no copd and use inhaler everyday and use inhaled steroid but not label themselves that way, denial. Copd is umbrella term- airway obstruction that worsens with expiration. Cant exhale properly. It includes emphysema, bronchitis and asthma. Asthma can be acute and reversible disease- can grow out of it. If don’t grow out of it and don’t control it it turns into a chronic problem. KNOW dif bet 3 types of obstructive pulm diseases. COPD- pts have already structural lung disease not the reversible form. Irritant (always secondary to irritant) for most people smoking but if another type of irritant- work in factory, allergic to pollen types- causes inflammatory reaction and so with that seepage of fluid occurs bc of vasodilation and permeability of capillaries and the fluid shifts into lungs so have excess mucus and if happen continually that mucus obstructs some alveoli and cause damage to alveoli structure to lose surfactant and damage type 2 alveolar cells and lose lung elasticity. Mucus and fluid in lung tissue causes stiffening so alveoli become stiff and don’t participate in gas exchange- these scarred by mucus irritation causes air trapping and air trapped in stiffened alveoli cant participate in gas exchange. COPD HALLMARKs after structure alveoli damage- AIR TRAPPING. Risk factors- recurrent or chronic resp infections Allergies Alpha 1 antitrypsin deficiency- enzyme protects lung from injury, they do well with lung transplants Occupational exposures Air pollution Smoking- impairs macrophage function, triggers inflammation, mucus production and not enough alpha 1 to protect lungs from that damage Obs lung disease- air moves in and alveolar wall stretches and air in expiration gets stuck in there. due to mucus or scar tissue form damage. They can take breathes in but cant exhale it all bc scar tissue causes obstruction. KNOW asthma: chronic inflammatory obstructive lung disease. Affects ADLs. Can have acute reversible onset or become chronic problem KNOW RISK FACTORS AND ETIOLOGY: Heredity- genetic disposition linked to T disorder to fight irritants Exposure to allergens Emotional factors- trigger bronchoconstriction Enc factors Exercise- exacerbation Triggers: Excess sensitivity of the lungs to stimuli. Inhaled allergen/trigger- encounters macrophage, activates immune response/cascade KNOW IGE IS IMPLICATED IGE levels elevated with asthma exacerbation. Ige to mast cells are released and activate vasodilation and capillary permeability. Fluid shift into tissues have bronchoconstriction- bc fluid shift become constricted. Mucus formation and narrowing of airways with the edema. Asthma linked dif than bronchitis and emphysema bc triggers immune response releasing histamine and leukocytes causing vasodilation and permeability and fluid leaks out into tissues causing swelling, bronchoconstriction and edema. Airways swollen and less air going in and out of bronchioles. Asthma has a spectrum- pts can have mild, moderate or severe affecting co2 and oxygenation and can lead to death if become so hypoxic and percapnic (co2?) Pts with copd/ashma use TRIPOD POSITION know sit forward to let diaphragm hang and less restrictive. KNOW DIAGNOSTIC!! IGE LEVELS ELEVATED WITH ASTHMA HALLMARK Cbc- look for any anemia or increased WBC for infection Blood gases- oxygen and co2. Treat- Give pxygen and KNOW HYDRATION FOR ANY PT WITH MUCUS (Asthma produces mucus) bc thins the mucus making easier to expectorate- cough up. Drink 2 L a day 3 L in 24 hrs is pushing fluid. Decrease anxiety hypoxic get crazy and anxious. Change positioning. Reversal of beonchoconstriction give inhaled bronchodilators and steroids and mast cell stabilizers that went wack in immune response. Acute bronchitis- acute infection or inflammation of the airways or bronchi that follows a viral illness and is self-limiting- goes away on own. No infiltrates on xray. Similar symptoms to pneumonia. Treat with antifever, humidity, cough suppressants and a/b. can progress to pneumonia. Its in bronchioles only UPPER AIRWAY. Chronic bronchitis!! Inflammation of the bronchi RECURRENT AT LEAST 3 MONTHS OF THE YR FOR 2 CONSECUTIVE YEARS. Recurrent bronchiole infections. Incidence increase in smokers, workers eposed to ir pollution and elderly. Mostly smokers! Productive wet cough bc of mucus. Thick and hacking cough. Prolonged exposure to irritants inhaled, abnormal mucus production, inflammation leading to infection. Airways can collapse bc of the mucus leading to v-q mismatch. Mucus junking up bronchioles cant exhale that air. If occurs long enough have permanent structure damage to bronchioles. Mucus plugging from excess mucus from infections and air gets trapped. KNOW SIGNS AND SYMPTOMS: (compare and dif s&S of bronc, em, and asthma) HALLMARK- productive cough and SOB decreases exercise tolerance Wheezing Frequent pulmonary infections Hypoxemia (cyanosis) late sign- pulm vessels try to compensate eby vasoconstriction with chronic hypoxemia. Pulm vessels vasoconstrict so Right side of heart gets bigger and has to work harder. Not normal for pulm vessels to have higher pressure. The pulm vessels come from pulm artery and right side of heart low pressure passive system but chronic hypoxemia reflex is for pulm vessels to vasoconstrict causing higher pressure in pulm vessels PULMONARY HYPERTENSION leading to Right sided failure. Pulmonary hypertension KNOW air trapping in alveoli they become larger bc air trapped so lungs look hyperinflateed bc alveoli larger. Mucus obstructing in bronchitis. Expiration is passive usually while inhalation takes effort. So air can go in but not come out. Mucus trapping the air in. if alveoli air trapped enlarges them so thoracic cage becomes hyperinflated and have physiologic signs of increase in lung volumes. But higher lung volume not mean more gas exchange!- bc air trapped in there. balloon blow up inflates but if smth stuck in there some air go out but not all of it so lung cage get larger in chronic bronchitis or emphysema. Hyperinflation and increased residual volume and decreased volume capacity. Residual volume what leftover after exhale higher than normal bc trapped. Blood gases can be affected. If right side of heart start to suffer from pulm hypertension then see right side affect. Pt has exposure of irritant causing chronic inflamm response and mucus production- stop smoking, avoid irritants, break up mucus, a/b, open up lungs. Most pts need more hydration than diuretics. KNOW MUCUS TO BE COUGHED UP GIVE VOLUME- HYDRATE THEM TO THIN MUCUS UP TO 3L FLUID IN 24 HR PERIOD. KNOW Patients with bron and emp not deny oxygen but most have high level of co2 so low tolerance for high oxygen. Start with lower oxygen administration! Risk for infection bc of mucus- treat more often with a/b. pulse OX no one under 90 is okay. 88 and under treating. Less than 90 is low o2 sat so consider oxygen administration. 88-90 see copd live at. Start with low flow o2 and then work up. Emphysema- abnormal permanent enlargement of airways with destruction of alveolar walls. Not just mucus causing air trapping but destruction and scarring of alveoli- structural disease. KNOW AIRFLOW LIMITATION CAUSED BY LACK OF ELASTIC RECOIL IN THE LUNGS. STIFF AND HARD BC OF SCARRING AND DAMAGE OF ALVEOLI WALLS AND TRAP AIR BUT NOT BC OF MUCUS. Know dif bet bronchitis and em. Em HALLMARK- lung tissue damage scarring while bronch due to mucus! 1% is primary, not do to secondary cause but alpha 1 antitrypsin deficiency which protects lung from damage. Damage of the elastin of lung tissue. Autosomal recessive trait genetic cant preent this. Many times get lung transplants. 99% due to inhaled toxins like smoking, airpollution, chemical exposures, etc. the toxins damage lung tissue and protectant enzymes don’t work well enough to protect lungs from the toxins. Recurrent inflammation irreversible damage to alveoli, breakdown of elastin, lungs become less compliant. With normal expiration alveoli dynamic can collapse and elasticity to get rid of volume, with damage to alveoli walls cant expire lose elastic recoil and bronchioles collapse. KNOW SIGNS AND SYMPTOMS: SOB on exertion, when get short of breath? Walk of 6 ft, block, ½ mile. If cant go from bathroom to bed and breathe its pretty bad Barrel shaped chest from overdistension of alveoli an thoracic cage looks elongated and widened. Use accessory muscles to rid of co2 and expire When alveoli enlarged and stiff cant recoil air trapped in there not part of gas exchange- not more volume just air sitting in there not exhaling so co2 goes up. Pt has widened chest diameter but decreased breathe sounds bc exhalation is disturbed. Can diagnose when listen to lungs and cant hear anything. No air flow. Decreased breathe sounds bc not going out just trapped KNOW Hyperventilation to compensate breathe more shallow and quicker to rid of co2 PURSED LIP BREATHING- increases volume and trying to force out their breathe trying to push out more and exhale more forcefully to get rid of air. KNOW EM VS BRON: Emphysema co2 retention makes you vasodilate and look more pink and flushed so used to be called pink puffers not look hypoxic bc holding onto more co2 and increase resp rate and use accessory muscles and pursed lip technique Blue bloaters bronchitis- become more hypoxic and get pulm hypertension as reflex vasoconstriction occurs become more cyanotic and rbc increase in number polycythemia to compensate for hypoxia. This makes right side heart work more bc more viscous blood harder to get out. Cor pulmonale- right sided heart failure due to pulm disease KNOW. Increased total lung capacity but when blow out extra air stuck in increased residual volume. That high pressure flattens diaphragm. Not need know abg. Low o2 high co2 and high bicarb to balane out. Decrease o2 sat. Treat- avoid irritants, stop smoking to save wtvr alveoli are left. Inhaled anticholinergics, bronchodilators, low flow oxygen, hydration (some mucus still). Steroids, avoid infections amap, lung volume reduction surgery, lung transplant. Pulmonary vascular disease Pulm embolism- saddle embolism where branches go off to right and left. Big blood clot saddling both r and l pulm branches. v-q mismatch bc blood waiting to oxygenate but no flow to lung so mismatch of ventilation and perfusion blood flow to the alveoli. Dead space where clot is. Still ventilate but no perfuse. If have v-q mismatch on ventilation side is good blood flow but have scar tissue that’s dead or atelectasis so blood flow get to alveoli but that part of lung not have gas exchange so ventilation side mismatch. Pulm embolism- clot in pulmonary vessel. With infarction means whole area of lung not get enough perfusion and dies off. KNOW risk factors: #1 cause is DVT clots travel from legs to brain. Heart or lungs!! KNOW virchow’s triad: for pulm embolism and clot formation Hypercoagulability- thick blood, lots of rbcs, on estrogen. Thicker blood so easily clottable Venous stasis- pts with immobility, bed bound, sitting on airplane for 10 hrs Venous endothelial injury- pt had sx, tissue damage, trauma triggering the clotting cascade. Clot in plmary vessels cant oxygenate increase v-q mismatch, look at blood gases. See if clot from legs to lungs, see if dvt. D-dimer: lab value showing clot formation. Vq scan- inhales gas and shows in lungs if getting taken up somewhere. Ct scan. Ct angio- see if clot in any vessels. Rteat by bust clot and Coumadin, surgery high risk when pull clot out, ivc filter- infr vena cava filter if clot form in legs so block from going up to heart lungs or brain. SIGNS AND SYMPTOMS: SOB, decrease oxygen and HALLMARK-impending sense of doom and get agitated look bugeyed. Clot occluding part of lung. Pulmonary hypertension- high bp in pulmonary arteries than normal bc usually low pressure system. Right sided hypertrophy on echo see it. Signs and symptoms: Fatigue, sob, chest discomfort, Tachypnea, Dyspnea with exercise. Can be its own idiopathic cause- can just happen that pulm vessels vasoconstrict so put on meds to dilate pulm vessels./ KNOW cor pulmonale- right side heart failure secondary to pulm disease, hypoxic where pulm vessels constrict causing pressure to right side of heart and it fails. All signs and symptoms of resp problems: Decreased lung ventilation Pulm casoconstriciton Increase polycythemia making blood more viscous KNOW pulmonary vascular resistance and vessels are constricted so high afterload of right side heart= pulm vascular resistance so more rresistance to flow from right side of heart!! Right side used to lower pressures but if vessels constricted higher pressure to right side. Increased workload on heart Get filling defect cant fill right side and cant pump out so it backs up and fails. Clinical manifestations- exertion cant compensate, right ventricular hypertropjhy and larger, the valve becomes damaged. Find out on ekg, echo and physical exam. Lower pressures and try to fix resp problem. sometimes need heart and lung transplant. Lungs shot bc emphysemas and now right side failure need both. Acute resp disorders Acute lung injury KNOW ARGS Acute lung inflammation and alveolarcapillary injury noncardiogenic pulmonary edema. If heart not pump fluid out goes to left side heart and is pulmonary edema so backs up into left side into lungs. Ards look like pulm edem but not from heart but from insult to the lungs. NONCARDIOGENIC. Echo shows heart pumping great but just had infection, injury, etc and lungs affected most likely it is ARDS. Acute resp distress syndrome. Number one cause:SEOSIS AND MULTIPLE TRAUMA. Septic shock give lots of fluid bc goes into tissues head to toe systemic every organ fluid shifts also into lungs!! Pulmonary edema- overwhelming inflame sirge septic shock cascade. Pt multiple trauma and give lots of fluid only so much heart can do give lots of fluid go into lungs go into ARDS. Also bad infection with cap permeability and pneumonia. Burns, aspiration where food into lungs triggers inflame response and cause fluid seapage into lungs, drug overdose-not breathing, massive blood transfusion- too much so goes into lungs. HEART IS GOOD IN THESE PTS so it’s the insult causing lungs to get wet bc too much fluid admin or sirge permability to capillaries and vasodilation causeing leakage into tissues. Syndrome- exudates enters alveoli increase permeability triggers mediators athan fluid washes out surfactant and keeps alveoli open but loss of surfactant so stiff lungs and noncompliance. V-q mismatch blood flow fine to lungs but alveoli stiff and cant do gas exchange. Fluid washes out surfactant that helps alveoli open for gas exchange so cant do anymore. SIGNS AND SYMP” Fine crackles= fluids in lungs Physical exam Infiltrates on cxr see debris and congestion in lung fields Bronchoscopy Ct of chest If in ards high risk fluid in lungs become infectious- happens a lot. Reverse it and treat underlying cause. Mechanical ventilation HALLMARK- REFRACTORY HYPOXEMIA: GIVING MORE OXYGEN AND SAO2 OR PO2 LEVEL NOT CHANGE. GIVE OXYGEN BUT O2 LEVEL NOT GO UP BC LUNGS WET AND CANT DO GAS ECHANGE. Until treat underlying cause and rid of fluid might need mechanical ventilation to give pressures to keep alveoli open. KNOW Acute respiratory failure: pt is not able to compensate anymore. Hypoxemia is po2 on blood gas is 60 but we use 50 50 rule. In real world use 50. Normal 60-100 so less than 60 is hypoxemia and resp failure is 50 or less. Hypercapnia co2 greater than 50 with a ph that’s dropping less than 7.25, if 55 and ph 7.38 then compensating so not do anything. If become acidodic then problem. resp failure intubate less than 7.25 ph. Co2 greater than 50 and ph less than 7.25 in resp failure use mechanical ventilation from injury to lungs or other system failure cant oxygenate or ventilate. Hypoventilating v-q mismatch or disease processes ards, pulm embolism or hypoxic. Rapid shallow breathing Blow co2 quick but then cant resp alkalosis and then resp acidosis. Blow hard then get tired accumulate co2 acidodic. Sob Hypoxia Nonresponsive to oxygen therapy. If not treated acidodic then death. Look at whole picture before mechanical ventilate. Resp acidosis can lead to cardiac dysfunction- all acidosis. ECMO- extracorporeal membrane oxygenation- all blood out and clear it and oxygenate and put back in. (pt with amniotic fluid embolism) Quizzes 3/20/17 Respiratory Tract Infections Differentiate Common cold- Rhinoviruses- ages 5-40 common. Get them a lot bc there are many dif types of rhinoviruses. Parainfluenza- younger kids Resp synctial virus- in winter and spring ? Coronaviruses and adenoviruses- Main entry points- nasal and oral mucosa, eye conjunctiva. To prevent cold – hand washing KNOW! Most are viruses so not use antibiotics. Its dangerous to do that bc then get resistant strains so when need to fight them wont be able to. Rhinosinusitis- infection of sinus passage Acute: less than 12 weeks. facial pain, headache, purulent nasal discharge, decreased sense of smell, fever . Chronic: over 12 weeks. nasal obstruction, fullness in the ears, postnasal drip, hoarseness, chronic cough, loss of taste and smell, unpleasant breath, headache. Acute can be viral or bacterial. Viruses attach to tissues and allow bacteria to adhere more easily. Can have viral infection in any tissue and allow bacteria adhere so can have secondary bacterial infection. If lasts mreo than 4 weeks is bacterial and if symptoms return or persist have bacterial affect as well. Influenza- over 65 yrs old susceptible to serious problem. A B and C types. Big problem in country thru aerosol droplet or direct contact transmission. Upper resp is rhinotracheitis. Lower resp tract becomes pneumonia and is dangerous. Resp tract infection upper with nose vs further down to bronchioles and alveoli becomes systemic disease. Can get bacterial pneumonia. Incubation 1-4 days and contagious til 5 days after onset. 3 types cause disease not need know which types. A and b we sick and c is upper resp infection not get worse. Initially starts as upper resp infection and go lower to become pneumonia. Virus kills mucus secreting cells and goes to lower resp tract causing bacterial adhesion and pneumonia- gas exchange in alveoli impaired become hypoxic, pathogenic and systemic illness. KNOW difs. Signs: fever, chills, malaise, body aches, sore throat, non-productive cough, HALLMARK- rapid onset profound malaise feel like hit by truck and not want to get up. Affects of low gas exchange bc debris accumulating with viral and triggered mediators (bc infection) clogs lower resp tract and cant clear. Secondary complications- sinusitis, otitis media, bronchitis, bacterial pneumonia, secondary bacterial pneumonia from original influenza very common. Goal- limit infection to resp tract. Flu turned to pneumonia is systemic disease and bugs can spread to sinus, inner ear, bronchioles. Children can’t use aspirin for fever- reye’s syndrome attacks the liver. Cant push these pts to ambulate and move around bc alveolar gas exchange disturbance bc lower resp pneumonia so want them to rest. They need to decrease metabolic needs bc not have good oxygenation. Treat symptomatically. Decrease movement and KNOW hydrate!!!! so debris in lower lungs to mobilize and coughed up. If cant get enough by mouth use iv. Tamiflu within first 24-48 hrs and if too late then it replicated beyond control and not gonna work. Pneumonia- acute infection of lower resp tract. Effect elderly worse. How get it? Nosocomial/hospital acquired or community acquired. KNOW MOST COMMON: Community acquired- Streptococcus pneumoniae Nosocomial- Pseudomonas aeruginosa, and Staphylococcus aureus Immunocompromised pts susceptible to pneumonia. Barrel shaped chest KNOW nosocomial categorized vs community: Hospital lower resp tract infection not present or incubating upon admission. Surveillance cultures of pts nasal or rectal swab or sputum when pt comes to floor even from ER swabbed rectally for vancomycin resistant VRE and nose for MRSA and do this every week swabbed and this is why pt on contact precautions bc mrsa in nose or vre in rectum or other bugs grown spec to that institution. If comes with it can show insurance we didn’t give to them bc if got there not reimbursed for that care. Not bc sick from those bugs do on every pt. (never events- wrong site sx, uti, pressure ulcers, nosocomial pneumonia, catheter related bloodstream infections, fall in hospital and injured) KNOW hospital acquired pneumonia classification. Atypical pneumonia- nntk Portal entry-enters lung- pathogen replicates into alveoli- immune mediators fight- debris- impaired gas exchange in alveoli and no breath sounds in that area- cilia cant clear mucus so areas o flung dead tissue bc oxygen cant get thru mucus area of solidification (walls off that area from mucus and debris) and that wall is solid and can die off. Infection- inflammation- serous exudates- congestion productive cough (hydrate and rest pt) Systemic infection S&S deoxygenation: Cyanosis Diaphoresis HALLMARK- Fever/chills HA Malaise HALLMARK-Body aches NV Acidosis Chest pain Productive cough Crackles, rales (fluid or debris congestion Dullness on percussion (consolidation, fluid, no air) Decreased breath sounds Pleural friction rub Diagnose- CBC- WBC is elevated KNOW get blood cultures right away and sputum culture before Antibiotics (empiric a/b broad spectrum not spec to that bug) need to do culture beforehand to get specificity for bug. Treat- meds for oxygen bronchodilators to get stuff up and out of lings and antipyretics not let fever last bc hypoxic and antibiotics bc most likely bacterial pneumonia bc this sick, positioning head pf bed at least 30 degrees up enough to cough up stuff but not over 45 too high bc cant breathe, humidified treatment, monitor blood gases and oxygenation, give iv fluid if cant drink enough- hydrate a lot. Primary TB- World’s foremost cause of death from a single infectious agent. Can affect many organs but we focus on type affect lungs. Many drug resistant forms of this microbacterium which causes macrophages if not kill can wall off area of infection with waxy capsule and can be alive many years. Latent vs active TB. Mycobacterium tb an acid fast bacillus that affects lungs- KNOW affects immunosuppressed pts mostly high risk for it. Aerosiolized minute particles can go thru events and affect whole room or building. Hypersensitivity response with macrophages cause inflammatory response- if cant engulf and kill TB then wall off the area and pt has patchy area on lung that is difficult to permeate with bacteria so need antiTB meds for several months to get rid of TB. Dormant lesion can not be infectious for years but if immune affects by pregnancy or stress than TB can become activated and get re-infection and get spreadable and contagious TB. KNOW how transmitted- airborne droplets, coughing sneezing or talking. Bacilli inspired inupper lobes and go to lymph nodes and cause immune e response and area of TRB necome necrotic and caeseuous (cheesy). Can clear with immune system activated T cells- not everyone gets ful blown sick but some can. Primary TB- immune e response inadequate get progressive primary TB or latent KNOW difs. Areas walled off in lungs pic. KNOW s&S TB: Asymptomatic in latent TB (can walk around with cheesy thing in lung without knowing for yrs than stress event and become symptomatic) Fatigue Anorexic Weight loss Low grade fever diurnal release of TB that cause fluctuation in temp HALLMARK- night sweats Lethargy HALLMARK- Rust colored or bloody tinged sputum Pos TB skin test- hypersensitivity rxn for latent or active TB so tested once a yr as healthcare providers. Sputum culture- gives Acid fast basillus doesn’t take up stain. Treat- A/B for several months bc TB very resistant strains and also at least 6-9 months so compliance issues TB nnt sin test. Positive- false if get bcg vaccine in other countries mostly in kids than adults. Can occur a few yrs after vaccine False neg- cant mount immune response HIV aids hodgkins viral infections and getting corticosteroids or imminosuppressive drugs Treat- nntk lots of meds Wear N95 mask for TB. We not do bc not FIT tested. 3/27/17 Gastrointestinal System We have to figure out if there is a problem in the upper GI tract for something acute that may require surgery or heart attack – have to differentiate that. Acute diarrhea- correlate types of diarrhea with types of GI issues involved. 3-5 days worth of watery stool not bloody, purulent or greasy. Bloody- bleed or actual damage to the mucosa vs frequent stools. Purulent- infection of some sort, pus in the stool. Greasy- intestines not breaking down and absorbing fat and going into stool instead. Frequent stool. Acute < 3 weeks duration usually self-limited and just treat symptoms, keep pt well hydrated for wtvr virus/bacteria passing thru. Large vs small volume- to help differentiate issues. Large: viral or bacterial infection of large or distal small intestine can alter fluid and electrolyte balance bc in colon the stool gets dehydrated so stool becomes solid matter there and water and electrolytes gets absorbed in the colon. So if this is not occurring then altering fluid and electrolyte levels. As nurse, acute diarrhea pt always want to monitor fluid and electrolyte balance. Especially potassium loss in the stool. Small- freq small amounts of stool usually with real intestinal problem not just an infection- real problem with nutrient and fluid absorption and characteristic of ulcerative cholitis and crohn’s disease. These are inflammatory bowel disease actually affecting the tissue of small and large intestine. Other S&S If pt has fever ha, vomiting infectious process usually accompanied by pain, discomfort and general malaise Constipation- Not have true definition. Change in freq, size and consistency and ease of stool passing. Might have stool freq for 3 days and fine no pain, normal pattern. Another person goes every 3 days have problems going feel gassy and in pain. About how easy the stool is passed and any associated symptoms with stool pattern. This is main reason people get off medications. People start taking laxatives and get used to the laxatives and then cant get dumping reflex without laxative. In mind think if not poo everyday constipated. Very subjective but change in stool pattern more difficult to pass. Stools less than once very 3 days. Causes- dehydration- stool harder to pass and sometimes people withhold going bc hard to pass and gets worse- longer stool stays in rectal vaults the more dehydrated it gets and more firm and more harder to pass. Delayed gastric motility- pt with inflammation problems and not as much motility. Sedentary lifestyle. Low fiber diet- major cause of constipation. Psychogenic- in brain think you are and not go Medications- opioids slow down motility, narcotics, anticholinergics. Treatment- can be fecal impaction- be hard to pass and can cause other problems. Check for it double glove and dr. order to check bc finger in anus cause agal simulation and bear down and heart rate drop. Give pt an enema and no response to it, expands the rectal wall with fluid and causes dumping and stool not go thru it’s so hard cant pass so digital disimpaction and pull out hard stool and then rid of obstruction. Increase fluid, fiber, exercise and train the bowel to go at certain time of day. If these not work, laxative, stool softeners, enema and suppository but can affect rectal mucosa. Anorexia- loss of appetite or desire to eat food. Pt’s with gi upset not want to eat and also present as symptoms with problems not associated with gi track like anorexia nervosa- psychological disorder needs treatment. Nausea- Subjective, unpleasant sensation that may precede vomiting Caused by: Distention or irritation anywhere in the GI tract Stimulated by higher brain center The pt has problems with HA’s, cerebral irritation cause nausea. Vomiting- number one side effect of nausea and drug therapy Complex reflex mediated by vomiting center in the medulla oblongata of the brain KNOW Occur in response to: Excessive distention or irritation of the stomach or duodenum- body own reflex to get rid of virus or bacteria, Chemical stimulation- meds like opioid neurotransmitters, Pain- extreme and sever can trigger vomiting reflex and if this occurs usually happens once or twice and not a lot thruout the illness. Projectile vomiting with direct simulation of the vomiting center and intracranial pressure- stroke, hemorrhage and meningitis. Symptoms preceding vomiting: Nausea, tachycardia, sweating- primitive reflex to rid of toxins so associated with gi tract illnesses. KNOW types of abdominal pain Parietal Pain- caused by stimulation of pain receptors in the parietal peritoneum or abdominal wall. The pain is localized, sharp, intense, and one-sided (lateralized). Have pt point with one finger to pain it’s in one area is parietal. If in general diffuse it’s visceral. Visceral Pain- caused by stimulation of abdominal organs; pain is vague, diffuse (nonlocalized), and dull bc all the organs are squished together the pain radiates thru whole abdominal cavity so harder to assess the location. Referred Pain- is felt at a distance from the affected tissue or organ; is localized at some point along the afferent nerve pathway of the organ or tissue. Classic example- gall bladder pain radiate from belly to right shoulder. Intestinal obstruction- impaired movement of intestinal contents. KNOW mechanical vs nonmechanical causes. Obstruction- complete or partial not allowing gas or stool to pass distally to area of obstruction. Mechanical- actual object or smth obstructing. Tumor on colon or small intestine, adhesion, or scar tissue from prev sx or c-section sticks onto wall of intestine and obstructs gas or stool passage distally to that. Severe constipation that causes a fecal impaction. Proximally the size of intestinal wall distends leading to perforation proximally to obstruction and can cause septic shock and death. fills with gas, fluid and stool and perforate. Also, wall of intestine swollen and leak contents out of it as colon not sterile the contents are full of bacteria which can translocate in gut and go to bloodstream and cause infection. Intestinal obstructions also due to volvulus – twisting of intestines or intussusception- telescoping into itself where one part of intestine slides into the next like a telescope not as common. Obstruction can also cause vomiting of stool. Whether mechanical or nonmechanical have these S&s: Pain distention proximal to bowel loss of appetite diarrhea if partial obstruction liquid stool passes thru but not complete emptying of lumen bc stool left behind absent bowel sounds over distended area but initially might hear borborygmus hyperactive bowel sounds which is the gas building up in the proximal area of the lumen- high patched fast and frequent followed by absence where perforation now has occurred- dangerous bc no movement. Abdominal tenderness Rigidity- something perforation or bleeding in the belly can barely push down on belly distended some resistance to belly but can still push down but rigidity cant push down and hard and board-like. Medical emergency. sign of perforation or bleeding causing hardness Fever if inflammation going on also KNOW dif bet mechanical and nonmechanical obstruction Ileus- partial or complete nonmechanical blockade, bc peristalsis has stopped. Usually temporary and most commonly caused by abdominal surgery when cut into belly use anesthesia and stops belly moving so before get out of unit or go home need to be able to pass gas showing not obstructed and peristalsis is working. No tumor no scar tissue and no stool in vault just peristalsis shut down usually due to an insult to the gut, anesthesia, and medications. S&S: Cramping and Distension, nausea vomiting, failure to pass gas or stool These patients have absent or diminished bowel sounds bc peristalsis has seized. Treatment- Pts with obstruction need to do for them bc cant pass gas fluid accumulates in stomachs or proximal intestinal area and we need to decompress their stomachs so need NG tube to rid of extra gas and fluid that accumulates in stomach bc peristalsis stops in intestine and then stomach all backs up. Acute abdomen- Defined as an episode of severe abdominal pain that lasts several hours or longer and requires medical attention. Gall bladder, cholecsystits, appendix, intestinal ulcerations or sweating problems. Things that need sx to fix. Common gyn causes- lower quadrant pain: pelvic inflammatory disease (PID), fibroids, ovarian cyst Medical causes: lower lobe pneumonia, acute MI, diabetic ketoacidosis, acute hepatitis. Not need sx to fix but medicine. Appendicitis- triad of RLQ pain, anorexia, and leukocytosis is the most sensitive diagnosis tool. Needs sx. Need workup and may or may not need sx to fix. Peritonitis- pbstruction, ileus, mechanical or nonmechanical obstruction and wall of intestine becomes enlarged it can perforate. If perforate into gut the peritoneal cavity fluid moves into belly and blood or stool irritate peritoneal lining of the gut and the pt worst case can die from massive infection and septic shock bc intestine perforates. If ulcer perforates and also have bleeding peritonitis can occur. S&S: rebound pain- pt gets pain relief by pressing down over inflamed area and when release hurts more, protective mechanism due to the inflammation. Nausea vomiting- Rigid abdomen- medical emergency. Tachycardia/Shock-like state Increased CBCs. KNOW peptic ulcer disease definition- ulceration is breakdown of tissue and can bleed of upper gi mucosa exposed to acid secretions when there is an imbalance between gastric protective mechanism and irritating factors. alkaline measures for contents going from stomach into duodenum we have protective mechanisms. Too much acid in stomach or acid into duodenum (proximal portion of intestine or ileum) and make way down the tissue can ulcerate and breakdown. Normal stomach ph is 2. Normal mechanism- acid increase after meal to help breakdown fats symptoms associated with gastritis and gastric ulcer often improve with eating/antacid use. Certain foods can buffer aids and the ph goes up more alkalotic with some food inside of it. Duodenal and gastric ulceration and KNOW the differences. Causes- KNOW Used to say stomach ulcer due to stress but figured out a lot of peptic ulcer disease occurred bc of H. pylori- bacteria that can burrow into wall of stomach and duodenum and protects self from acid and burrows into mucosa and breaks that down causing ulceration. KNOW Excess use of NSAIDS and Aspirin inhibit prostoglandin which helps to protect mucosa of the stomach, they decrease inflammation but they also inhibit prostoglandin’s protection. Zollinger-Ellison- when too much acid builds up in stomach causes disease and these pts have multiple ulcerations. Stress ulcers- pts in hospitals on peptic ulcer protection omiprazole, propanizole the PPIs and H2 block which protect the stomach bc the pts are stressed and ill so need stress ulcer protection until eating full diet okay enough and not as stressed so not need protection medicine. If not eating enough sick and not protect self naturally at risk for ulcerations. Risk Factors: Advancing age- more prone to stress and acidity, Use of warfarin and NSAIDS, Corticosteroid use, Smoking H. Pylori Bacteria capable of growing, even flourishing, in the low pH (acidic) environment of the stomach and proximal duodenu. A gram-negative rod with flagella that propel it through the protective mucus layer to access the underlying tissues Cofactor of some gastric cancers and a cause of some types of chronic gastritis and most peptic ulcers KNOW If pts have H.pylori know relationship to gastric cancer bc any tissue continually irritated has ability to become neoplastic and cancerous bc cells start to morph and change. Chronically irritated tissue in any part of body prone to cancer so h. pylori can be precursor to cancer if not treat it. KNOW the patho- More acid than body can buffer Leads to break or ulceration in the mucosa of the stomach or duodenum. Breaks allow the mucosa to be subjected to an acid or alkaline environment. Autodigestion occurs and breaks self down. Decreased mucus production and acid breaks down prostaglandin protecting mucosa. Gastric ulcer- Duodenal ulcer (DU): 4 times more common than GU, 25-75 yrs. KNOW hallmark Epigastric burning 2-3 hrs after eating, after pt eats and mucosa coated alkalytically in the duodenum start to have pain sometimes wake up at night after dinner 2-3 hours; relief with foods or antacids. Awakening at 1-2 am with symptoms are common. Otherwise has periods of feeling well. KNOW hallmark Gastric ulcer : More common among NSAID users, 55-65 yrs. (rare prior to age 40). Pain often reported with or immediately after meals bc been ingesting food and fat and gastric acid secretions go into stomach and that’s when feel pain. N/V, weight loss is common want to avoid eating bc pain with it. S&S peptic ulcer disease: Dyspepsia- Pain when stomach is empty (duodenal) Pain immediately after or during eating (gastric) Weight loss (gastric)—weight gain (duodenal) Hematemesis Melena In severe cases can lead to perforation and hemorrhage H. pylori to gastric cancer. Any tissue continuously irritated can become neoplastic. Can be precursor to cancer if not treated. A/B to treat. PUD- more acid than body can buffer and breakdown of tissue KNOW patho. The breakdown makes mucosa subjected to acid and autodigestion occurs. Due to imbalance of decreased mucus production or too much acid. Duodenal more common than gastric ulcer. KNOW duodenal HALLMARK epigastric burning 2-3 hrs after eating so after pt eats and the mucosa is coated alkalytically in the duodenum they start to have pain- sometimes in middle of night after dinner. These pts eat more to feel better. Gastric ulcer- more for NSAID users and pain right after meals 1/2hr-1hr. all the secretions dump into stomach and have pain. Weight loss bc want to avoid the pain that comes with eating. PUD S&S Dyspepsia Nausea, vomiting Painful digestion Heartburn Weight loss/gain KNOW terms as descriptors: Hematemesis- vomiting up blood- bright red if profusely bleeding, if coffee grounds from stomach, upper bleed if ulcer proliferates and actively bleeds have this (hemoptysis is coughing up blood from the lungs) Melena- blood in the stool but changes characteristics of the stool. Lower gi tract is bleeding but has mixed with the stool and changed consistency to tarr thick pasty sticky and with odor (not brown and formed) this is lower gi bleed that worked thru gi tract. Gastric ulcer coughing up blood for a while the blood trickles thru lower gi tract and turns to melena. Expected finding as GI bleed resolves b cakes a few days to clear out of your system. Can be from upper ulceration as well, can be coffe ground, hematemesis and melena for PUD. Hematochezia- bright red blood in the stool- normal looking brown and formed stool- lower gi bleed that is profusely bleeding bc not mixing with the intestinal contents. Not working thru gi tract and not change characteristics if the stool. Lot worse than melena bc melena is slow bleed and couple days after proliferation. Lower ulceration bleeding profusely into stool is more significant. Perforation and hemorrhage Hx and physical- med use, onset of pain, what do to make feel better. Scope the pt and see ulceration in stomach colon or small intestine. Tests for h.pylori, upper gi studies, stool specimen occult blood, drink carbon isotope and h pylori break it down into urea and release in the breath as ammonia so breath before and after. Avoid foods with excess acid secretion, reduce NSAIDS, stop smoking, to reduce acid in stomach- h2 blockers and ppi proton pump inhibitors use. GERD KNOW what is Reflux of gastroduodenal into esophagus with or or without inflammation. Regurgiatation so acidic contents from stomach back up to esophagus many times the sphincter is not sealing well letting gas and acid climb backup. Too much acid production, delayed esophageal peristalsis so cant clear esophagus or delayed gastric emptying. Some foods and meds relax the sphincter. Lower tone of esophageal sphincter and let stuff back up to esophagus. KNOW S&S Heartburn acidosis Regurgitation Burning after eating so large meals increase fat in stomach triggering more acid emptying into stomach to break them down Bending over, lying down tight belt or jeans around belly cause pressure in lower esophogeal sphincter Pain radiating to arm Cough Hx of gastric cancer can occur with chronic irritation of the esophagus KNOW the stomach or esophageal mucosa more prone to gastric cancer Barret esophagus- scar tissue form bc of that irritation. It can close their esophagus and need that part removed. Sx is cut esophagus and bring stomach up to chest so listen to bowel sounds up there. Symptomatic relief- change diet PPIs H2 blockers, lose weight. Swallowing and see if cancer or other cause of acid back up. Barium lights up on xray to see if esophagus closed. Or endoscopy easier to see narrowing. Elevate bed so not have reflex, avoid large meals. Hiatul Hernia- KNOW what it is a condition in which the stomach protrudes thru the diaphragm- can herniate to the chest/thorax can twist the stomach and can block blood flow and ischemic and become necrotic. It can be asymptomatic or cause symptoms of GERD, diagnose with barium swallow or endoscopy. Treat the same as for GERD, may need sx. Pouching of stomach wall thru diaphragm compressing that area and that area can become necrotic/dead and 80% mortality if dead stomach. Mostly to overweight or obese. Diverticulitis- KNOW dif bet diverticulitis and diverticulosis. Diverticulitis-itis= inflammation. Inflammation of one or more diverticula (diverticulus) in the bowel wall with microperforation and abscess formation in the pericolic fat. Diverticulosis-Herniation of mucosa thru the muscular wall of the colon, found mostly in sigmoid colon but may occur anywhere in the GI tract. Higher in ppl with low fiber diet, bc fiber makes bolus of food move it down quickly thru the colon and if stays in colon bc of lack of fiber that stool stays in the intestinal tract and causes the intestinal wall to distend and pouch out and debris can accumulate there and trigger infection or inflammation. The pressure in wall too great bc of stuck stool and causes outpouching=Diverticula, which is harmless unless become infected or inflamed and then become diverticulitis. Diverticulosis is chance of becoming inflamed. KNOW S&S HALLMARK LLQ abdominal pain which is large colon. Abdominal guarding and rebound tenderness- inflammation of the diverticula so diverticulitis. Hx of constipation Low grade fever with inflammation Defecation causes more pain bc goes thru inflamed part of the colon. Nv and anorexia Diverticulitis if diverticula perforate can get blood in stool so Guiac-positive stools Abdominal mass noted with significant inflammation and abscess formation **Diverticula low fiber diet pouches for years then inflamed diverticulitis pain with defecation LLQ and it perforates have peritonitis.** No colonoscopy bc perforation from below. Appendicitis- inflammation of appendix. Hard piece of stool that has stuck itself in appendix wall and is called fecalith- not look like stool anymore and then triggers inflammation. Can be stricture/narrowing of appendix but mostly. Leading cause for abdominal sx. If notr removed can rupture KNOW S&S Acute periumbilical or epigastric pain localized to RLQ pain Atypical cough Anorexia and nv- related to severity of the pain (1 or 2 episodes) McBurney’s Point KNOW point bet belly button and the iliac crest a third of the way in RLQ if press ilicits severe pain RLQ rebound tenderness Rovsing’s sign KNOW bc nerves in stomach all bundled up have RLQ pain when palpating the LLQ. Can be very diffuse pain with inflammation. Psoas sign- pain with right thigh extension and pain goes up bc of how ligament attaches to lower quadrant Obturator sign- rotate leg causes pain in RLQ Pts w’ sudden onset of anorexia and severe abdominal pain shld be worked up for appendicitis. The danger is the perforation and cessation suddenly of pain and peritonitis. IBS irritable bowel syndrome- ibs s a functional bowel disorder in bowel habits- episodes of constipation and diarrhea. Distention, abdominal pain. Very common esp in females. Overload of stress to the gut- causes diarrhea and constipation. Hypersensitivity and abdominal pain. Disregulation of motor function. Not need know rome criteria- present with 2 or more criteria. Diagnosis based on symptomology. Meds to regulate the gut motility. Decrease stress. Control diet. Increase fluids for constipation. Inflammatory bowel disease KNOW dif bet Crohn’s and Ulcerative Colitis. Both triggered by exacerbations and remissions and stress. Familiar tendency. Often present in early adulthood. Ulcerative colitis- only affects colon and the mucosa throughout the whole section starts distally in colon and moves up but not affect small intestine. More nutritional imbalance in crohn’s so have weight loss cant absorb nutrients. Autoimmune disorder bc body attacking area of large intestine causing erythema, edema and ulceration. HALLMARK diarrhea and hematochezia bc going thru whole issue of colon causing ulceration and bleeding. Mild exacerbation less than 4 and more severe 6. Can become anemic, hemorrhages, chronic inflammation can cause colon cancer due to strictures, narrowing and scar tissue in the colon. Inflammatory process of mucosa so put on anti-inflammatory meds. Have to rest area of the bowel affected so may need permanent or temporary colostomy. Crohn’s chronic inflammatory of bowel patchy from submucosal layer and ileum and colon. Crohn’s disease affects both small and large intestine and has a skipping pattern. Cant identify the factors and antibodies triggered to attack itself in crohn’s and UC. Theoretically autoimmune. ulceration formation, fissues, breakdown of tissues, fistula- breakdown of tissue in organ blocking passage of fluid. Narrowing of lumen Diarrhea Pain HALLMARK MALABSORPTION- cant absorb fats properly, stool more mucoid fatty contents loses brown characteristics. Mucus in stool bc cant absorb fat bc small intestine cant break it down. KNOW Steatorrhea- fatty stool Uti NONBLOODY diarrhea Weight loss Electrolyte imbalance Low grade fever Anemia Abscesses and fistulas Cant absorb albumin Colicky pain RLQ uti need low residue- low fiber diet don’t want them using their gut. Not want a lot of stool. high protein and high calorie bc of absorption. TPN- if gut so inflamed cant use at all so nutrition with IV (big yellow bag). Antiinflam drugs and a/b for infection. Hepatobiliary Disorders Cholecystitis- inflammation of the gall bladder secondary to asymptomatic gallstones= cholelithiasis. Not always become symptomatic. Related to bile or cholesterol calculi. Fatty diets. KNOW when stone becomes impacted in the systic/gallbladder duct inflammation develops behind the obstruction. Impact affects pancreas, gallbladder and liver. Gallbladder not holds much bile but can distend and perforate. Pressure builds up and leads to distention, ischemia, gangrene and perforation with abscess formation and peritonitis. Due to estrogen links and synthesis of ile acids women more prone. Obese for high fat diets. Progesterone creates less movement of bile. Other causes are gall bladder sludge- dehydrated or gall bladder stasis makes the juice stagnant. Biggest cause is presence of obstructing gall bladder stones. S&S HALLMARK RUQ radiating to back or shoulder Biliary cholic pain is wavelike pain linked to peristalsis, okay for few min then pain then okay as peristalsis tries to move things forward. Attacks after fatty moves as bile tries to move to fats to break them down. Tenderness in epigastric and RUQ Positive Murphy’s sign palpate RUQ and have pain and tenderness Clinical findings only during an actual attack- no warning signs. Back up in common duct by stone- Liver has problems too so bile backs up leading to jaundice cant clear bilirubin from blood which is RBC breakdown used for bile. Jaundice means common bile duct obstruction backing up to liver and affecting clearance of billirubin there. Fever and chills Hepatomegaly Chronic- asymptomatic, dyspepsia after meals. Liver can be inflamed also from bile backing up and presents with jaundice. KNOW dif between cholecystitis-inflam of gallbladder obstruction of bile duct/common duct linked to fatty intake and cholelithiasis-gallstones. Hepatitis-acute of ir chronic inflame of hepatocytes liver cells but we use it to categorize VIRAL hepatitis. KNOW main points of what cause dif type of viral hepatitis- be able to differentiate source of the hepatitis. Viral hepatitis: Myalgia, fatigue, nausea, anorexia, aversion to cigarette smoking, mild fever, arthritis like fingers, skin rashes. If severe then liver gets affected. Hep A- KNOW how transmitted. Fecal-contamination of water and food. Fecal oral transmission. Workers not wash hands before prepare food or shellfish into dirty water or vegetables and fruit not cleaned. Low mortalty rate and self-limiting works self out usually. Hep B- exchange thru bodily fluids. Usually sexual contact, iv drug use needle sharing, occupational exposure for healthcare workers so we all get vaccinated. Worse than HI bc on surfaces. Hep HIV exposed to air dies bc anaerobic bug. B and C lives on outer surfaces. Transmit thru needle sticks. Can get thru saliva, semen, blood serum. Once treated can be not contagious anymore. Hepatomegaly with mild RUQ tenderness Splenomegaly Not jaundice Fatigue Hep C- blood and bodily fluids. Mostly blood (needle sharing) and bodily fluids and less sexual transmission. liver transplant bc of that. 60s and 80s transfused blood a lot before filter blood properly. That generation has Hep C a lot. Can be chronic condition that does or doesn’t make you sick. Hep D- only occurs if have Hep B virus/ same transmission as b- sex and blood. Rule out with antibodies for exposure and vaccination and active infection. Liver cirrhosis- liver tissue replaced by fibrous scar tissue. Alcohol, drug abuse, virla hepatitis or biliary diseae bile backs up so much causing ischemia thru liver channels an leafs to portal HTN and liver failure. Liver has 2 mechanisms of blood flow- portal vein bringing blood from whole GI tract. The portal vein receives blood from esophagus to rectum then portal vein uses blood to metabolize drugs, clear toxins in liver etc. most from portal vein then 25% to liver from hepatic artery and that is giving the liver its oxygen rich blood it needs to survive. If we have obstruction o flow like a tumor or scar tissue from alcohol abuse or hep nodules from viral hepatitis it obstructs flow from sinusoids and back up flow to vein (artery is higher pressure so keeps pumping blood to liver and go path of least resistance so any sarring to tissue backs up flow into portal vein. This causes higher pressures in the portal vein that use dto called portal HTN. Blood flow from esophagus to rectum and all in between to liver. From portal vein backs up into gut to esophagus to rectal vessels and everything in between and this engorges the vessels that come from the gut and have higher pressures. The higher pressures can lead to rupture of the vessels- gi bleed, esophogeal bleeding, rectal bleeding, intestinal bleeding. Lvier function not working so: Manufacture sand synthesisze albunmin keep fluid in vascular spaces so have ascites-albumin cant keep flow so fluid shifts into the tissues usally abdomen/belly. Also liver makes clotting factors with vit k so pts more prone to bleeding. It metabolizes drugs so get drug toxicity. It metabolizes fat so malnourishment. Conjugates and clears billirubin so have jaundice and increased bilirubin. RAAS system cant clear aldosterone so sedum and water is retained and overdiluted. It filters blood and clears wastes so pts more prone to infections. S&S: Weight loss Ascites- lack of albumin Hepatomegaly- scarring and congestion from backed up flow Jaundice- cant break down bilirubin Abdominal pain Portal HTN- back up flow so have varices- engorged and enlarged vessels so prone to rupture esophageal variceal bleed, gi bleeds. Endocrine disorders -Cant clear female or male hormones- testicular atrophy, gynecomastia, vessel changes bc lack of ability in clearing so facial red blood vessels broken seen on nose and cheeks, fragile RBCs. Gi bleed- can’t make clotting factors and now have engorged veins so easier to rupture. Hepatorenal syndrome- pts go into renal kidney failure bc of liver failure. Not sure why. Rectal bleed in stool is bright red hematochezia- from internal hemorrhoid rupture from portal htn vessel engorgement. Esophagus supposed to be smooth but engorged veins in esophagus itself. KNOW Hepatic encephalopathy- Liver cirrhosis effects many dif systems. It takes amino acds and converts from ammonia to urea and is excreted in urine and stool but when liver can tdo this conversion with protein so build up of ammonia in blood and brain hates it. Increase in ammonia levels causes Hepatic encephalopathy- brain not working right due to toxins, brain injury and liver not working. Ammonia toxic to brain and pt has mental status changes. If get rid of the ammonia the pt perks up and is fine but if not go confused then comatose state. Rid of ammonia then back not permanent damage. KNOW ammonia levels are up associated with liver cirrhosis and altered mental status sign of hepatic encephalopathy. KNOW give med to get rid of ammonia build up from hepatic encephalopathy specifically- lactulose to bind the ammonia in the gi tract in the stool. Gives a bowel movement and dumps ammonia in the stool. If not bm after lactulose then change dose to get rid of ammonia. it treats ammonia level and hepatic encephalopathy (gi bleed, infections, ascites but ammonia specifically for enceph so not give lactulose if AAOx3). Acute Pancreatitis- pancreas inflamed. Dangerous bc enzymatic breakdown of fats, protein and carbs usually hardy enzymes so if pancreas inflamed enzymes leak out and travel to surrounding tissues to lungs and cause severe systemic response. Once inflamed can do a lot of damage Number one cause of pancreatitis is gallbladder stones in common duct coming from liver and gall bladder and sharing the pancreatic duct entering into the duodenum. If that duct is obstructed it triggers inflammation of the pancreas. Another big cause is alcohol abuse. Hyperlipidemia- theory that it inflames pancreas Hyperparathyroidism- theory that it inflames pancreas Sx/trauma can inflame pancreas Also meds. KNOW S&S: HALLMARK Severe epigastric pain radiating to the back Pancreatic enzymes travel to lungs and interfere with surfactant that keeps aveoli open so pt can go into ARDS. Tachycardia Hypotension Fever Triggers inflammatory response HALLMARK labs increase serum in amylase and especially elevated lipase found only in pancreas Pancreas pockets of inflammation attract calcium from bloodstream so blood level calcium will be low with pancreatitis. Gall bladder obstruction-pancreatitis- multisystem failure. Can have shocklike symptoms 4/3/17 Endocrine System Function of the glands. A&P will help. Endocrine system about negative feedback system- negative shuts down a gland in presence of extra hormones/excess hormones. Hypothalamus gets input from blood flow of dif levels of hormones and depending on the levels either signal releasing structure whether to stimulate or shut down production of the hormone itself. Not go into the reproductive organ. TSH ACTH and growth we go into. Disorders of endocrine control of growth and metabolism. KNOW compare patho of different disorders by too much or too little hormone how the disease presents itself. ACTH anti diuretic hormone secretion. Syndrome of Inappropriate Antidiuretic Hormone SIADH problem with postr pituitary gland secreting inappropriate ADH hormone signals kidneys to make water retained. If pt has problem in hypothalamus-pituitary access right in middle of the brain such as tumor compressing hypothalamus or pituitary causes over excretion of ADH. Other things like injuries, stroke, poor perfusion or ischemia to brain causes this. If manipulate with sx causes hormone out of wack and some meds mimic ADH effects. If hold on to too much water- KNOW how labs look and pt present. Serum sample: sodium diluted by too much water so sodium goes down. HALLMARK of SIADH- sodium how looks in blood vs in urine. Decreased sodium osmolality in the blood (solutes to plasma, amount of solutes in volume) ~280. <280 is diluted. >280 about 300 is more concentrated solutes than water. If too much water than number low and if more particles than water than number higher. If tell kidneys to hold on to water, don’t pee then pt makes urine and sample it the urine is going to be concentrated bc not adding more sodium to urine but concentrating it bc pt holding onto water not getting rid of it so urine more concentrated with sodium so have higher osmolality more solutes to water in the urine. Urine dark and concentrated tea colored amber. You would think dehydrated but when looks at labs look diluted so something wrong, not correlate bc have SIADH. Pt has tumor/stroke/ischemia to pituitary, etc. when pt out of sx and see labs and urine can indicate stroke in the OR. S&S fluid overload/low serum sodium: HF, pulmonary edema, cramping, vomiting, urine sodium so neuro effects bc low sodium in body. Correlate the labs with SIADH Serum hyponatremia and hypoosmolality causing seizures changes in sensorium neurologic deficits congestive heart failure gastrointestinal cramping vomiting DI Diabetes Insipitus- not have to do with unregulated blood sugar (not bc of high glucose) its because not enough ADH. Lots of urine output so that’s why people thought diabetes. Caused y neurogenic CNSproblem and can also be due to kidneys not able to respond to ADH- like lack of good flow. Third cause pschogenic psychiatric disorder where pt thinks have to drink loads of water causing the imbalance and they sometimes need to be restrained. Make too much ADH cant cncentrare urine and excrete tons of fluid. Kdneys cant respond to ADH or lack of excretion from pituitary of ADH. Therefore these pts opposite of SIADH. They be dumping tons of water- increased urine output in many liters. If check blood losing water but not sodium with it, sodium stays. So pt with blood has picture of hypernatremia concentrated osmolality and in urine opposite bc dilute, decfeased sodium so polyuria, nocturia and look clinically dehydrated. Not make sense bc dehydrated urine output decreases. Sodium 150 and making tons of urine it’s DI not the usual way. Presents very dehyrdrated but has lots of urine output. Serum increased sodium and osmolality S&s Mental status changes, seizures cardiovascular collapse. Bp low bc dumping tons of fluid can go into hypovolemic shock Adh deficiency is problem so give synthetic and fix kidneys problem and fix psychogenic as much as can. KNOW dif bet tertiary, second and primary Tertiary- from brain itself (cns injury, tumor) from hypothalamus hypothalamus sending too much/little signal of releasing hormone Secondary- at level of stimulating hormones of the pituitary (need to find underlying cause- or pituitary too muc or little stimulating hormone Primary- gland itself problem with secretion. When see labs can distinguish them a bit, active form of thyroid hormone t3 or t4 high or low look at thyroid stimulating hormone levels are off or thyroidtropin from hypothalamus is the problem. try to find which step not functioning. Number one cause of pituitary adenomas- cause hypo or hyperpituitarism present with tumor in brain- changes in vision, mental status, slurred speech. Benign mostly. Acromegaly- INcreased sectreion of growth hormone. In kids and adolescents called gigantism. Adlts- connective and bony tissue proliferate not grow tall but still have large head, jaw, thick tongue, forehead, barrel chest and large hands and feet. KNOW S&s of acromegaly here (signs of overgrowth). Thyroid insufficiency- lack of iodine made in thyroid gland. T3 and t4 active forms of the gland. If they aren’t being made but no problem with pituitary then thyroid stimulating hormone high bc still try to signal thyroid gland to release t3 and t4. Thyroidtropin and stimulating hormones high to make t3 and t4 bc in neg feedback not have enough t3 and t4 that’s how see underlying problem in labs. Not enough t3 t4 so see if thyroid, pituitary or hypothalamus. If thyroid cant make t3 and 4 and that’s the problem then tsh and trh are elevated bc they trying to signal more release of t3 and t4 doing their job. When thyroid overworking gets large and many times compensatory to try to make t3 and t4 but cant causing a goiter. Hypothyroid- not enough t3 and t4. Some born this way, rare. Others acquired hashimoto thyroiditis autoimmune destroy thyroid itself with antibodies- cant prevent it. If pt has thyroid cancer and nodules and remove thyroid cant maket3 and t4. Hyperthyroid- hyperacting thyroid gland. Graves disease autoimmune attack thyroid gland itself to make too much t3 and t4 though tsh and trh say not to make anymore bc of all the t3 and t4 floating in neg feedback system. Thyroid tumors can also stimulate more secretion of t3 and t4. Thyroid –regulates metabolic rate KNOW. Not enough thyroid so body slows down. KNOW compare S&s of hypo and hyper. Hyper- increased metabolic rate- overactive thyroid hormone. Sob, weight loss, cardiac output up, lose weight, exopthalmus. Hypo- slow down, gain weight, bradycardia, heart can fail, constipation, coarse dry skin, myxedema, cold intolerance Graves/hyperthyroid: fibroblast tissue (fibrin deposits) to form behind the eye KNOW exopthalmus pushing the eye forward. Pts going to be revved up, tremors, high heart rate and hot all the time, heat intolerance and anxiety. This can effect the vision as well, visual changes. Overworking thyroid causes goiter. Underworking also cause goiter bc compensatory mechanisms trying to grow more to stimulate more t3 and t4 release. Goiter- enlarged thyroid palpable (thyroid not usually palpable) can be hyper or hypo thyroid. Graves/hyper- autoimmunue disorder, antibodies attack and stimulate more thyroid hormone release. Attack t3 and t4 itself. THIS IS CORRECT-thyrotropin antibodies attack thyroid gland itself and stimulate t3 and t4. Thyrotropin antibodies not hypothalamus or pituitary but attack thyroid gland itself causing more stimulation of t3 and t4. The neg feedback now is t3 and t4 a lot so decrease the tsh bc lotsof t3 and t4 around but tsh shuts down bc not want anymore t3 and t4 but thyroid attacked by antibodies to make more t3 and t4 though tsh saying to decrease it. Excess of t3 and t4. Autoimmune disorder attack t3 and t4 but cause oerstiumlation of t3 and t4 even though pituitary and hypothalamus want to shut down t3 and t4 production. PRIMARY problem bc at gland itself. Measure the whole thyroid panel- trh tsh and and see too much t3 and t4 and low tsh. Treat- slow down function by thyroidectomy or radiate iodine. If take out thyroid get hypothyroid. Danger Thyroitoxic crises- so much danger to vital signs so hypermetabolic, tachycardia, hyperthermic, dehydrated can have heart attacks and die. Get pth and beta blocker meds. Know ideology of primary hypothyroidism or secondary with pituitary gland failure. Inability to make thyroid hormone so all slows down. Weakness, fatigue, loss of appetite, weight gain, mental dullness and HALLMARK: myxedema. Affect connective tissue and too much fat deposition in the tissue and causes doughy edema throughout the body. Not myxedema coma. Affects a lot of organs but not all- skeletal muscle, retinal. Low t3 and t4 circulating so pituitary signal thyroid release more so tsh thyroid stimulating hormone from pituitary elevated but t3/t4 gland not working so be low. High tsh and low t3/t4. Myxedema and everything slows down. Iodine deficiency not co01111111mmon, Iatrogenic hypothyroidism- when remove thyroid low so need to replace hormone Autoimmune thyroiditis- hashimoto’s disease- most common antibodies attack, idiopathic disorder caused by autoimmune thyroid antibodies that destroy the gland Labs KNOW (not numbers just general high or low) TSH high in primary and low in pituitary and t3/t3 always low. KNOW concept of treatment- replace thyroid hormone thru medications. Generic t3 and t4 but best is synthroid. Thyroid carcinoma- risk factors having had radiation therapy to head or neck. Feel tumor press on esophagus/trachea and feel nodules and do iodine scanning and see where thyroid not take it up and need to remove it or chemotherapy. Alterations of PTH parathyroid function- regulates calcium. If too much calcium in the blood it kicks in and tries to get calcium in thebones. If not enough in blood then break down more from bones to be released into the bloodstream.also increase vit D absorption thru kidneys to help absorption of calcium in the intestine/gut. KNOW Hyper vs hypo Hyperparathyroidism- too much secretion hypercalcemia in blood more release of calcium from bone into blood making bone thinner and more porous. Hypoparathyroidism- not enough calcium released from bone so circulating levels in blood inhypocalcemia. Hyperpth- due to disease or tumor in parathyroid gland. Pts release too much calcium and bones get thin. S&S bone pain, kidney stones (too much calcium so forms stones) adrenal cortical hormones- adrenal release estrogen and progresterone- stress/fight or flight hormones. These triggered by sympathetic nervous system. Shut down gut, ability to fight infection in a fight. Need more glucose and tachycardia and higher bp for fighting. When stress hormones activated. Catecholamines and mineral corticoids. Alterations of adrenal function KNOW cushing syndrome vs disease Cushing syndrome- due to tumor on pituitary or adrenal glands secreting too much cortisol. Cushing disease- hyperadrenalism too much adrenal hormone secretion- primary in adrenal gland itself above the kidneys. Secondary to access of acth tropic hormone on the pituitary. Increased cortisol so shut down infection, increase blood sugar and pressure. steroids antagonize insulin so increase glucose in blood. break down protein so cant deposit protein in muscle they get thin and wasted and causes skin to be thin and weak and blood vessels weak. Capillaries break down in skin, fragile bruising skin. Increased protein loss also fluid shifts into tissues. KNOW S&S Steroid psychosis, changes in mental status, mood swings, weakness, decreased libido, overweight, water and sodium retention, MOON FACE- large and swollen face, deposition of fat on back give buffalo hump, susceptibility to infection, hold onto water so hypertensive high BP, hyperglycemia, insulin pushes potassium into the cell and the high glucose and low insuloin causes hypokalemia. Cortisol levels elevated. KNOW suppression test vs stimulating test Give pt a load of glucocorticoid causes if neg feedback if supply the hormone synthetically the levels should go down- suppression test is administer the hormone the hypothalamus should read as has enough so shut down. If cortisol levels still elevated after glucocorticoid then have overstimulation of cortisol in cshings disease. Give hormone exogenously and test level a few hours later to see if neg feedback worked and suppressed cortisol released, but if still high then problem and overproducing this hormone. Suppression should show decrease in level bc giving that hormone but if still high than problem. (Random cortisols in real life and more worried about not too much. Usually have not enough cortisol release.) Work up pt for underlying cause, treat HTN and diabetes. With release of protein and fat can get plaque in coronary arteries and HTN causes cardiac problems like hypertrophy, pressure and volume. Hyperaldosterone- nntk. Hypoadrenalism- • Primary – Adrenal insufficiency with inadequate production of cortisol and aldosterone caused by autoimmune destruction of the adrenal cortex • Secondary – hypocortisolism caused by withdrawal of corticosteroid therapy is also sometimes (incorrectly) called Addison disease. Pituitary disease with decreased secretion of ACTH is another cause of adrenal insufficiency see clinically secondary- see pts stressed for long time and very sick shot their adrenal gland- excess stimulation in illness now not working enough. Cortisol low. Can’t fight infection, low bp. Autoimmune destruction of adrenal gland is true disease itself primary. Addison’s disease: Mineralcorticoids & Glucocorticoids destroyed. Aldosterone decease- tied to sodium absorption. Decrease in stimulation decrase in absorption. High sodium and water excretion so hypovalemia- leading to orthostatic hypotension- and if sodium low so potassium goes up, decrease in potassium excretion so hyperkalemic in blood so worry about cardiac. Deceased cortisol leading to Hypoglycemia losing sugar giving confusion and weakness. Correlate addisons with these lab findings KNOW. (tall tented t waves and qrs widen) KNOW correlate Addison’s problem with potassium excretion, cortisol decrease. S&S Weakness, fatigue, anorexia and nausea Poor stress responders, hyperpigmentation Adrenotropic tertiary signal gland not work acth goes up to try to compensate and this causes melanin hyperpigmentation. Decreased cortisol levels in blood and urine and acth elevated in Addison. Mineralcorticoid replacement therapy and incease dietary sodium and avoid potassium foods for life. Hypotensive, hypoglycemic, lose weight high infection risk, hyperkalemia. Pancreatic exocrine and endocrine function. Glucose brought into cell with insulin so can have a lot of glucose in blood but not enough insulin so glucose not go into cells. Main nutrient source for brain in glucose KNOW. So pt’s hypoglycemic- seizures and brain death. Endocrine of pancreas- insulin and glucogan into bloodstream to regulate glucose uptake. Alpha cells glucagon opposes insulin beta cells in pancreas do insulin delta cells somatostatin regulates digestion. Islet of langerhans not work sufficiently or at all KNOW dif types of diabetes where langerhans cells not work enough or at all. Glucagon releases stored food in to blood. decrease insulin increases glucagon as long as pancreas and liver working. KNOW type 1 vs type 2 diabetes mellitus. Type 1 autoimmune complete beta cell destruction- pancreas attacked and speculate combination of possible hereditary and env and viruses that at early stage type 1 have destroyed islet/beta cells of pancreas. Beta cells that produce insulin destroyed. Type 2- dysfunction of ceta cell and insulin resistance. Gestational diabetes- pregnant women. Type 1- genetic predisposition in chromosome 6 and not always become diabetes so genetic with env multifactorial causes making autoimmune antibodies to islet cells and destroy beta cells. Alpha cells affected too. Decreased insulin, increase glucagon and become hyperglycemic. KNOW No production of insulin in type 1 diabetes. And so glucose increased in bloodstream but can’t get into tissues without insulin so tissues without glucose start to shrink and rupture and die. HALLMARK- both hyperglycemia but if body craves glucose looks to nonglucose stores for energy like fatty acids so body not replace insulin hyperglecima then breakdown lipid and protein stores, the fatty acid byproduct increases ketones in urine and ketoacidosis only occurs in type 1 bc no insulin go to nonglucose stores and break down and have acid byproducts shown up as ketones and get ketoacidosis. Tissues not getting sugar they need so pt have fatigue, with high glucose in the blood pulls fluid from the tissues (osmotic diaresis, large molecules like glucose in blood pulls fluid to itself from the tissues into the vascular space) extra fluid in vessels now need to be peed out so HALLMARK polyuria, polydipsia bc all the fluid pulled in and going out so get thirsty, polyphasia bc tissues starving not getting enough glucose. Hungry thirsty lots of urine and weight loss. If ketones go up and acidosis so cells die too- complication diabetic ketoacidosis- emergency of type 1 diabetes. Diagnosis- symptoms, family hx, labs KNOW hemoglobin A1C glycosylated hemoglobin look at glucose content from whole lifespan about 120 days and RBC lives about 120 days so if pt test blood sugar glucose just at that moment glucose in blood. hemoglobin A1C shows glucose of that rbc for last 2 to 3 months- longer view. If pt says controlled and go into clinic but A1C above 5 is not normal. Above 7 means sugar out of wack a while not good glucose control. 2-3 months 60-120 days. These pts need insulin for life unless get pancreatic transplant. Insulin, diet (less simple carbs) subq injections. Hypoglycemia is risk for too much insulin. Type 2 dm- acquired diabetes and big problem in US linked to poor diet and exercise. Pancreas worn out. More common in some ethnicities and diagnosed usually late 4, 5, 6th decade. Women affected more than men. Since pancreas still secretes some insulin body not go into DKA. Mostly env factors. Pancreatic cell dysfunction- if not use sugar turns to fat so fat deposition and protein deposition in tissues. Hyperglycemia, dyslipidemia. Start with prediabetes- glucose high so oral agents to decrease then worsen to using insulin exogenously. Use sub q insulin as well. Most pts if change lifestyle might revert to non-insulin dependent. Could save islet cells. Get to point hyperglycemia too much so need insulin. In both DM I & II- High glucose bad for tissues bc surrounding tissues not get nutrients they need. Therefore small structures first and most effected small vessels around eyes, kidneys heart and brain and the joints- fingers, toes and feet. Also high glucose is caustic damaging on small capillaries and vessels which become stiffer and less dynamic to gas exchange so tissues also not get good gas exchange. Bugs like to grow in high sugar so pts prone to infections- poorly healed skin and high risk of infection. Type II- onset more insidious, slow progressive over time. Battle for a while before insulin or meds. Type I- precipice pt goes over and young eople and kids. Present with DKA have hyperglycemia and ketoacidosis and go to ER and diagnosed with it usually. Type I or II- visual problems, infection risk, parasthesia tingling in toes and fingers lack of good blood flow to them, weight gain for type II bc extra sugar turn to fat, polyuria, polydipsia, osmotic diaresis. Type II- A1C elevated. Electrolytes. Small arteries and arterioles to kidneys affected so risk for kidney disease. Glomerular bed around nephrons affected by high sugar- cause Glomerular bed damage to small capillary membrane and allow protein to get into urine (filter is damaged by high sugar) abnormal finding bc too large for urine usually. Glucose tolerance test drink glucose then blood test to see how regulated or random glucose over 200 is diagnostic. Now use A1C. Treat- lose weight, hypoglycemia meds. Opthalmic checks- diabetes and HTN number one cause of blindness, amputations, kidney failure, and need podiatry- feet have neuropathy and they cant fell their feet bc small nerves affected by impaired blood flow and gas exchange. Can’t feel pebble in shoe. Need multidisciplinary team. BP and cholesterol controlled bc coronary arteries can become stiff also- so if have HTN and high cholesterol really bad for heart not want more glucose there stiffening it up. KNOW somogyi effect- hypoglycemia occur in evening. Release of glucose and insulin is cyclical in the day. If in evening then counter release of sugar in morning. Gets insulin at night and hypoglecmic at night then in morning sugar spikes up and think need to increase insulin but makes at night the sugar block again. It is due to too much insulin in evening or not eat at night, eat at 6 then insulin and sugar down at night and in morning elevated. Any elevated sugar risk of tissue damage. Rebound hyperglycemia from low blood sugar in the evening. How treat? Give snack at night. Not happen to everyone but can happen to a lot of people. KNOW dawn effect- abnormal morning release of glucose hyperglycemia also but die to liver have surge or glucose neogenesis. Liver when sleeping and not eating releases stored glucose (glucose neogenesis) so can’t regulate and sugar high in morning so test blood sugar at night it is normal not low and in morning is high. Time their insulin so more effective in morning or extra dose in morning. DIF is check at night and in morning. Somogyi low at night high rebound hyperglycemia in morning. Dawn normal/elevated at night and rebound hyperglycemia in morning. Hypoglycemia- <60 blood sugar can happen after get insulin, skipping meals. Want to make sure they eat after insulin admin bc if take insulin and skip meals the blood sugar low. S&S Can lose consciousness and coma, tachycardia, palpitations, diaphoresis, tremors, pallor, anxiety. Too much insulin pushes potassium into cell hyperkalemia and kills pt pretty quickly. KNOW DKA- only type I diabetes. More extremes polyuria, polydipsia. Breakdown fat so ketones in the urine ketosis. A pt who is stressed drug sugar levels increase (cortisol release increase) so increase fever, source of infection and exercise too much and release more glucose but not enough insulin so stressor or can also be noncompliance with insulin so pt breaks down ketones and becomes acidodic. High sugars than 7.3 or below acidodic ph. Kussmauls’ respiration- high glucose and ketone formation, high resp rate to blow off CO2 resp to compensate for acidosis by blowing off co2 so more tachypnic and also shallow! Ketones formed in bloodstream and excreted in urine makes fruity odor and carbs also make that smell. Acididoc, nausea and vomiting Type 1 DKA and type 2 complications need to correct fluid balance first! Think first insulin so sugar in cells and stop dying and ketones resolved so give insulin right away but if in cardiovascular collapse and low bp and low volume do fluids first then fix insulin. Bp 80/40 and severely hypotensive. When give fluids corrects the high potassium. Hypovolemic shock fix then fix sugar with insulin. HHNK/HHNS complication of type II diabetes- high blood sugars greater than 600 mg/DL. See more in middle age to older population. Same S&S of DKA but not acidosis! Not have potassium shift out of cell so potassium not a problem. polyuria, polydipsia, osmotic diaresis. Older pts and more signs of not getting enough nutrient delivery to brain- coma state or change in mental status, lethargy. Hospitalize them and give fluids bc hypotensive and insulin if needed. Complications of diabetes- peripheral vascular disease (arms and legs) small vessels first, need amputations, diabetic neuropathy, retinopathy visual changes, nephropathy kidney problems, foot problems. Strokes and heart attacks bc arteries affected. Infections, CKD. Immune disorders from last week continued: Autoimmune disorder problem is suppressor t-cells bc they activated inappropriately to attack pts’ own tissues. Problem for HIV affected is helper T-cells that up-regulate immune response. Inflammatory response- immune reponse triggered normally by injury, infection, something attacking the host. Triggers allow mediators to protect host. Leukocytes go to place and leukocytosis- increase in WBCs and if abnormal SIRGE response and prolonged not good and if limited normal. Sirge- systemic inflame response to insult HR up RR up and temp extremes and WBCs high and low- vasodilation, permeability fluid out of vessels so bp drops. Shock-like state and circulating cytokines depress heart function at end stage shock and death. SIRS + infection= sepsis Organs affected- severe sepsis Septic shock- severe sepsis, hypotension and unstable pt even after fluid administered. Multi-organ dysfunction syndrome when prolonged sirs response and lack of perfusion to the organs and so they fail. Hypersensitivity and allergy- allergy normal response to Haptens normal in env- pollen, dander, dust, grass, trees, perfume. Harmless particles that trigger a hypersensitivity response. Type 1- allergic rxn dander, dust mites, penicillin, meds Systemic or anaphylactic Local or atopic rxns- skin: rhinitis, food allergies, bronchial asthmas, hives, atopic dermatitis. T cell- b cell-mast cells release histamine all the mediators cause vasodilation where fluid goes into tissues causing bumps/hives on skin as a rash or in lungs opens up and fluid shift ointo bronchial tissue and narrows airways like in asthma. Hx of exposure to allergens, nose stuffy, rashes. local controlled rxns. Anaphylaxis KNOW- SYSTEMIC release of histamine from allergen exposure type 1 from degranulation of mast cells causing that histamine release making bp drop and shock and death if not treat and remove allergen immediately. Acetylcholine, kinins etc constrict airways and cause bronchoconstriction. Shock and airway obstruction. If pt difficulty breathing or swallowing call dr right away ABC problem. Facial swelling and tongue swelling also call dr bc may need to intubate. Rash can be precursor. Have exposure once to allergen and built antibodies and then second exposure causes allergic response usually. Hypersensitivity to LATEX- mild contact dermatitis, rash itching swelling rhinitis, conjunctibitis, urticaria (itching on skin, bronchospasm to anaphylaxis. Rubber gloves ok but latex causes the allergy. Iv lines, catheters, hemodialysis going to skin or blood is route of exposure. Latex condoms, airways, catheters and nipples on bottle. KNOW healthcare workers at risk exposed to latex product, manufacturing latex., demales and individuals allergic to other related foods. Anaphylactic quick rxn and delayed type hypersensitivity others 12-24 hrs after exposure. Pruritis, edema, vesicles, papules and crusting and thickness of the skin. To decrease immune response give antiflammatory STEROIDS to suppress immune system. (high dose long time give cushings syndrome) Type 2 hypersensitivity- igm or igc attack antigens on cell surfaces- on RBC or WBC give wrong blood so destroys the RBCs and clog arteries and kill them. Rh disease-mom and baby dif blood types not treated for. Drug rxns. KNOW HALLMARK Type 3- creation of antigen-antibody circulating immune complex. These complexes deposit self in body organs/tissues. The antibodies and mediators triggered form complex and go to tissue and interferes with its function. Autoimmune vasculitis- in Lupus the vessels become inflamed, inflammatory cascade Glomerulonephritis- glomerular bed becomes inflamed serum sickness- rare nntk Arthus reaction- rare nntk Damage wall of organ or tissue that is triggering the inflammation. Body decides a tissue is bad and going to attack it by forming coplex and trigger inflame cascade on this specific tissue. Type IV hypersensitivity Cell mediated: t cells attack antigen Direct cell-mediated cytotoxicity Viral reactions Delayed-type hypersensitivity Tuberculin test Allergic contact dermatitis Hypersensitivity pneumonitis Responsible for transplant rejection bc organ cells attack host. Antibodies react with the graft with the organ and have to remove the organ bc can kill the pt. KNOW dif between immune deficiency and autoimmune disorder Immune deficiency- absence of immune bodies, component not there or was attacked and not functioning. Congenital or primary. Acquired- HIV Decrease immune function- age extremes very young and old, frequent infection pts get on antibiotics less flora and more susceptible to fight infection, to fight infection use nutritional component is protein! Use of cortico steroids and alcohol and drug abuse. KNOW transmission of HIV virus- by transfusions in 80s and 90s! body fluids Transmitted by body fluids Sexual contact Breast milk Blood-to-blood contact: Contaminated needles, Transfusions, During pregnancy or birth Cd4 proteins and receptors- T helpers really ignite immune response and KNOW hiv attacks cd4 so body cant turn on that immune response and fight infections. S&S: Infection that goes into seroconversion and hiv disappears, latent period while virus replicating, that AIDS illness. Opportunistic affect respiratory system, nervous system, strange malignancies, wasting syndrome with diarrhea and weight loss. KNOW dif bet immune deficiency and autoimmune disease. Autoimmune disease has immune system overworking and cant recognize self anymore and so attacks itself certain tissues. Breaksdown tissue and antibodies appear in the blood depending on which tissue. – Systemic Lupus Erythematosus (SLE) – Scleroderma – Ankylosing Spondylitis Immune deficiency like AIDS can’t fight infection- it’s the illness that kills them. LUPUS- systemic inflame disease causing major organ failure. Exacerbations and remissions and scleroderma. If pt well controlled and hydrated, no stress or infections, no substance abuse can live years without exacerbations. If stressed can get exacerbations and organ failures. Type 3 hypersensitivity form on connective tissue and collagen the complex forms. Connective in skin and lining the organs and these deposits lead to necrosis so gi tract, pleura of heart and lungs affected. Cause restrictive problems with organ bed. No cure. Defect of genetic disposition or something else- some meds cause lupus-like affects, stress like sunlight/uv/pregnancy. Sunlight on skin can cause bc connective tissue. Immune antibody complex. KNOW ASSESSMENT FINDINGS: *event triggered by stress event/sunlight/meds/illness/pregnancy/abuse Dry scaly rash *Low grade fever *Joint pan Erythema of the palms *Butterfly erythema on the face Anemia- nntk Pos ANA antibodies Elevated sedimentation rate Can affect lining of heart, lungs, kidneys and skin KNOW Scleroderma vs Lupus Chronic connective tissue disease similar to SLE that is characterized by inflammation, fibrosis and sclerosis. Also hardens the connective tissue. Lupus not cause hardening of connective tissue. Esophageal lining, gi, heart, lungs, and kidneys, CREST C-Calcium deposits in skin R-Raynoud’s- spasms of blood vessels E-Esophageal dysfunction- acid reflex and less mobile S-Sclerodactyly thick and tight skin on finger snd hands T-Telangiectasias- dilation of capillaries causing red marks on surface of skin S&S Pain weakness muscle weakness Stiffness Pitting edema of hands and fingers Skin tight and taut and lose facial characteristics Dysphagia Less range of motion Cant do ADLs Lose mobility Chest pain get restrictive cant breathe well Resp issues 4/10/17 Disorders of skin integrity and Function Male and female genome is small, skin integrity small and kidney biggest and small musculoskeleteal of final. 20 qs on cumulative stuff- stuff need to know before go. Study guide for it and she stick to it a lot. 80-100 qs. Most on new material. Skin infections- ringworm athletes foot – eat skin off foot called tinea cappitus head or corperus body facialis on face. Not a worm but a fungus. It’s a rxn to fungus toxins- excrement that skin is reacting to. Most fungal infections like to grow in moist and dark warm places like skinfolds. Can be superficial or deeper and invades ther aeras like gi tract, mouth, vagina, etc. once in the blood really bad bc antifungal meds (a/b and antifungals) toxic to kidneys usually and can cause many problems. Need infectious disesase and pharmacy to approve the meds bc so caustic on kidneys. Bacterial skin infections- Impetigo- contagious eruptions that occurs, plaque with pus pustules contagious in bedding, towels, skin to skin contact. Precluded by strep or staph infection- upper resp infection, sore throat than impetigo. Very contragious. KNOW Viral skin infections differences Verrucae warts- benign tissue tumors neoplasms and can spread and once have them they can come back. Herpes simplex- cold sores type 1 precluded by aura- tingling or pain in lip oral mucosa where it occurs. Herpes zoster- shingles eruption for people who had chicken pox (varicella) before and some of it dormant many years and stress event or trigger reactivates the virus but not getting varicella type skin eruption instead get shingles. KNOW HALLMARK one Dermatome nerve pathway attacked so nerve pain is tingling and more severe BURNING. Rash in dermatome pattern across one area of lower back or side flank or belly. Dangerous when on face and ca affect optic nerve and can cause blindness- medical emergency. Antivirals to go away but many times recurs. Over age 50 for those who had chicken pox before should get vaccinated. immunocompromised or over age 50 susceptible to it. Varicella- extreme puritis itching macules>vesicles>scabs. Remember what these are like pustule vs blister KNOW the terminology from health assessment. Macules start as rash than turn to blister than pops and scabs so macules turn to vesicles and then into scabs. Which cause warts? Viruses. Face itches and burns on one side red bumps? Shingles. Linear one area rash and burning Acne- disorder of sebaceous glands. Clogged pores and oil production- hormonal stimulation based occurs in puberty and early adulthood and should diminish. If not, see dermatologist. (acutane kilss people’s livers). Type 1 allergies hypersensitivity dermatoses- inflammatory rxn to an antigen. KNOW type 1 typically consist of. Atopic eczema, urticaria and epidermal edema- swelling. Hypersensitivity causing itchy, runny eyes, stuffiness. Involves the skin. Mediator mostly onvolved IgE causing vasodilation, permeability from mast cells triggering histamines. Type 2 helper cells react to antigen. In first exposure sensitization to antigen is occurring and antibodies being formed and sent to lymph nodes so on second or further exposure the antibody reaction occurs. first time not have reaction. On subsequent exposures have reaction. Histamine from mast cells causes inflammatory response, bronchoconstriction bc if capillary walls let fluid shift into tissues they become swollen so airway gets swollen and tight causes airway restriction but if happens in skin it becomes swollen and redden. Drug induced skin eruptions- rxns to drugs either right after use or hours later or days later. Erythema multiforme- hives blister after herpes simplex infection even like a week later and after second exposure happens within a few hours. Can be chemical or viral Steven-johnson syndrome- drug rxns cause this where skin tissue sloughs off. Becomes friable and fragile and peel off. <10% skin affected. Other than anaphalactic it is severe form also TENs. TENs toxic epidermal necrolysis- >30% of skin detaches and 30-35% mortality rate. KNOW papulosquamous dermatososes focus on psoriasis. Hyperplasia overgrowth of skin cells with rosaciou. Transient and related to viral exposure. Rash with one herald spot and spreads thru body quickly due to viral spreading. Transient so comes and goes full body rash after one spot and self limiting goes away on own. Lichen planus- papules that are flat and overgrown and scaly immunological rxn causing itching and worsens with the itching. Immunologic. Pts can be prone to it. Tissue constantly itching and broken down risk of cancer neoplastic malignancy. Psoriasis KNOW- not sure what causes it could be viral or immunologic to have overexaggerated T cell activation in the skin. Autoimmune where body causes this rxn and causes rapid cell turnover and hyperplasia. Too many skin cells being produced. This rxn causing papules to form ad be swollen and hardened usually in joints like elbows and fingers and becomes inflamed. They use UV light to kill or down regulate those cells and these pts will benefit from immune suppressant meds like cancer drugs if really disfiguring or debilitating. Not about size of cells but amount of cells. Rapid cell turnover due to immune mediated response. Flat which is what papules are flat overgrowths. (not round like blister). Dry and scaly no liquid coming out of them, no blister formation. Sun exposure- UV radiation which is harmful to the skin. 15-20 min all need for full vit d. Increase risk of skin cancer. Basal cell cariconoma- most common and invades locally. Squamos cell carcinoma- higher risk of spreading metastisis 10% . more prone is malignant melanoma to metastasize. Malignant melanoma- cancer from melanocytes can spread very quickly, if catch when still local like mole that changed before metastisis than 5 yr survival is 90% but if spread to other years 5 yrs 15-20% survival. Do full body dermatological checks if have hx of sun exposure. Malignant melanoma- cancers from melanocytes, asymmetry of mole, border irregularity, color variegation- change in color, diameter >0.6cm, changes over time. Types of melanoma not need to know. KNOW malignant melanoma associated with worse prognosis. Skin conditions of infancy- in brief. Birthmarks born without and as age develop, diaper dermatitis- diaper rash, prickly heat- heat rash in folds of skin caused by blocked sweat glands go into skin instead of out causing rash, cradle cap- right after birth flaking or mark on head, infectious disease rashes- roseaola, rubeola up with lack of vaccination these days, rubella, varicella, KNOW elderly skin disorders, actinic- due to solar damage spots from sunburned before that show up and changes in melanin keratoses- premalignant lesion that can lead to squamos or basal cell carcinoma so get checked to spot early lentigines- liver spots age related light brown or black due to hx of sun exposure. Vascular lesions: skin disorders happen in elderly as vessels become more fragile in the skin Angiomas- areas of vascularities cherry red Telangiectases- small blood vessels burst in skin can see on cheeks or nose due to fragile vessel and hormones not cleared well by liver in elderly age related Venous lakes- dark blue compressible papules sign of dilation of the veins venules in the skin allowing some blood to go in there look like dark bruises on top of skin but not from trauma but from breakdown fo vessels from fragility and age. Cant prevent these 3 really. Burns- Main focus is calssify burns. Injury from thermal, chemical or electrical agent more than body can tolerate causing skin damage 1st 2 nd or 3rd degree. Full thickness or partial thickness 1st degree or superficial KNOW both terms bc in community using them. Not considered threatening only very top layer of skin damaged so predispose to cancer in future but as burn itself just use creams or gels. Mild to moderate sunburn for example. Skin intact, no blistering or opening of the tissue. If see pic know how to classify 2nd degree or partial thickness burn to epidermis and dermis. Open wound causing blistering which eventually pops to be an open oozing wound. Open is partial thickness wound. This can be dangerous to health of person and also affects appendages of hair follicles and the nerve bundles so HURTS. 3rd degree or full thickness is burn goes into fat, muscle or connective tissue. Not hurt much bc nerves burned away. If large area edges not meet so need skin grafted bc no matrix layer or base at all to build skin tissue. Tough, leathery, waxy white to black. Dry edema. 4th degree down to bone burns. Slide of characteristics. Little pain. Dry, leathery, black, exposed bones, tendons and/or muscles. Requires grafting, flaps of muscle or amputation. Acid burn to skin and go into bloddstream and nburn internal organs vs flash burn superficial or 2nd degree. Location of injury matters- face risk is airway bc all swell up bc smoke into lungs. Circumferential burn around extremity constrict blood vessels and lose blood flow to arm called compartment syndrome and can lose extremity. Burn nurse and physician categorize the injury. KNOW How classify extent of burn RULE OF 9s look at pt body exposed and chart bidy surface area of burn.9 9 torse abdomen, 9 9 legs, 4 arms. Percent os prognosis and outcomes- greater than 20-30% to burn center and if burn extends and if not cool down with fluids than can extend. 2nd and 3rd degree we categorize with rule of 9s but not 1st degree. London broder- more specific to body sections, more accurate. If epidermis dermis down to fat and tissue burned than triggers massive SIRGE response! This causes swelling inflammation mediator response and capillaries dilate fluid shifts out and if have skin gone fluid shifts out. Surrounding skin can suffer from lack of perfusion so burn can get worse even after event over. Increase burn depth and depth of tissue? To get back to stable perfusion takes a while. Anytime fluid shift out of vessels into tissues have electrolyte disturbances, temperature loss bc skin protects temperature and risk for infection bc openwounds. Hypermetabolic from SIRGE response cannot give them enough calories 4000 ca and still lose body fat and muscle bc significant burn over 30%> inhaled anything toxic fumes can hurt lungs si pulmonary injuries. priorities- airway ABCs then lots of volume bc SIRGE response though skin swelling and edematous still need to perfuse the skin so give volume, high protein fat and calorie and prevent infection and pain. Treat- cover wound. Skin graft fro 3rd to 4th degree full thickness lost all skin and edges cant approximate need grafting. Nntk type of graft. Compartmnent synfdrome KNOW nerve and blood vessel damage that results from swelling and edema. Pressure in compartment in extremity and clamps down on arteries and arterioles feeding the tissues. Small vessels cant perfuse the tissue if extreme pressure so lose pulses, have pain, pallor, parasthesia, and tissue necrosis. This occurs in arms and legs usually but can be circumferential chest wound. Treat- open skin of compartment syndrome quickly to release that pressure. sliced the fasia open. Use heat element to cut open and cauterize at same time to scald the tissue so not bleed instead of scalpel. Use bovi. Time is muscle and time is tissue so not wait for OR. Elts arterioles perfuse the organ. Compartment syndrome of chest prevents chest muscles expanding to let us beethe 1st slide partial thickness 2nd degree. Slide 38 blister and eweping but skin still there. Slide 39 1st degree sunburn superficial burn Slide 40 leathery an ddry not weeping bc burned evssels and nerve endings. Not look human and nonblanchable so no blood flow. Dead tissue. Full thickness 3rd degree. Slide 41 burn to left upper extremity needed skin gradting so donor site was thigh. Stretch ths kin and holes to cover more body surface area. Skin graft always has ugly appearance but lets small amount skin stretch and optimize to adhere to tissue and hopefully grow. Less likely to reject own graft then donor graft. Pressure ulcers: KNOW differentiate and don’t confuse with burn classification! Stage I-Redness, unblancheable. Skin only relayted to pressure non blanchable due to prolonged pressure and now ischemia to that area. Skin inteact, reddened acan be after half hour of pressure. get pt off that area! Stage II-Partial thickness to full thickness. Some skin breakdown. If pt has diaper rash not pressure ulcer bc look same but not related to pressure not decubitous. Nonblanchable skin breakdown. Tape peal off alos not pressure ulcer Stage III-SQ tissue, yellow white looks like chicken fat. Extends into subq tissue. Stage IV-SQ to muscle/bone or tendon. Once a stage iv always a stage iv if have graft there not same as normal skin say stage iv healed skin intact bc that area of issue never the same gonna always be prone to reulceration or damage. Same as with stage 2 and 3 KNOW. Stage 2 healed but not gone. But never the same. No reverse staging Unstageable- not know where it is bc cant tell. Tissue must be removed first to see how deep it is usually hard black or brown, nonblanchable, tan leathery. Turn and reposition every 2 hrs. 4/25/17 Final Study guide is partial under assignments covers is accumulative until musc and gu. The rest of the content not part of it. Musculoskeletal- also include autoimmune disorders affecting joints Function of bones. Joints- provide stability and mobility Immoveable joints synarthrosis- sutures in the skull, Slightly moveable ampiarthrosis- ribs Movable- diarhthrosis Skeletal mucle- body positioning, stabilization. Not tested on hyperplasia but know bc terminology. Hyperplasia- increase in number of cells. Atrophy- muscles decrease in size and become flaccid and not usable. Neuro disorder and cant enervate muscles so not able to use. But if bc not in use and bed bound than can return to use. hypertrophy- increase in size KNOW dif between strain and sprain. Joint injuries. Strain- trauma to muscle or tendon stretching beyond capacity. Tissue tears or ruptures. Both involve inflammation/swelling of joint and pain. Healing takes weeks. Strains increase with age bc lack of collagen and elasticity. Strain is overwork or overstretch like exercise too much. Sprain- stress or tearing of LIGAMENTS usually excess movement of joint beyond capacity. Trauma and inflammation take time to heal. Also pain and swelling. Sprain like fall or trip and sprain ankle out of proportion. Joint dislocation- bone displaced from position can be completely or partial. Can see on xray the misaligned joints can be traumatic or congenital born with it. If due to trauma hear popping noise and pain with ROM. Realign joint either manually or surgery. KNOW dif of fractures. Complete fracture- bone is broken all the way through but skin is intact Incomplete fracture- hairline fracture, bone is damaged but still in one piece. More prone to it is children bc more pliable and smaller crack in bone without going all the way through Closed fracture- skin is closed Open fracture- skin is open. Problem can be infection bc break through the skin and gets dirty. Comminuted fracture- most deleterious (harmful) bc lot of soft tissue damage, bone shattered in 2 or more places and lot of soft tissue injury and can be nerve damage as well. Can’t be casted need rod(s) and pin(s) to replace the bone bc bone cant heal. Many times think of fractures as traumas but have pathological fractures from any of these types that occur without trauma. Pts with very thin and brittle bones easily fractured. KNOW osteoporosis- density or mass of bone is reduced. Makes bone more porous, weaker, fragile and brittle. Imbalance between bone resorption and formation. Bone resorption- calcium leaked out of the bone and makes it less dense. Reformation- calcium taken up by bone to be more stronger and dense. Osteoporosis- calcium leaking out of bone making it less strong. Happens either in one area or is more systemic throughout the bones. osteoporosis the bone becomes more porous with gaps in it and more brittle. Person loses bone stature and bone density. KNOW Risk factors: Multifactorial- inadequate calcium intake for bone, not enough magnesium bc also reg parathyroid secretion and calcium absorption, lack of exercise- to help bones stronger do impact weight bearing exercises, lack of vitamin d- helps calcium absorption in the intestine, low estrogen- affects more women after menopause bc menopause make osteoclasts to reduce bone because estrogen helps bone production and when women have less estrogen than osteoporosis can kick in, family hx- genetic component. Caffeine blocks calcium absorption, high phosphorus decreases calcium absorption. Imbalance of bone formation takes a few months up to 2 yrs to occur. Imbalance of resorption. KNOW S&S: depends on bones involved Pain- as bone is lost and thins out it causes pain Bone deformity Fractures- early sign is pathological fracture (no trauma) Lost of height Kyphosis (forward bending of spine) Dowager’s hump (abnormal outward curvature of the vertebrae of upper back) KNOW Osteomyelitis- infection of the bone. Problem bc hard for A/B to permeate and reach bone. Difficult to treat and can many times recur. Bacteria microbes from portal of entry to the bone site. Most frequently from years 3-12 years old bc of injuries- falls. Infection from outside the body go in or bloodstream infection and carries bacteria to the bone site and grows there. Bacteria causes pus, debris and death can occur to the bone bc of the infection and the bone can form around the area of pus debris and infection. Bone becomes devitalized become ischemic and die. Usually not spread throughout bone just that area dies but source of infection can travel around. Sometimes need to amputate. Treat the infection as well so not seed other areas. Poor wound healing like diabetics. KNOW sources and risk factors: Primary source is cutaneous- wound laceration or cut Sinusitis- osteomyelitis of facial bones Iv drug use- right into bloodstream dirty needles. Dental work can cause osteomyelitis of the mandible Hip replacements Bites Blows to the mouth Open bone fractures Pts who are immune suppressed Diabetics Patho- inflammatory response, pus accumulation, ischemia necrosis and death. new bone formation around necrotic part. Difficult for A/B to get through bone formed around the infection. S&S: Depends on portal of entry, level of infection, age of person, site and the initiating event. If systemic in the bloodstream infection than very bad. Even ear infection can cause osteomyelitis of inner ear bones. Infection symptoms- Fever Chills Malaise Fatigue Pain Inflammation and injury at site of pain KNOW Osteoarthritis- a form of arthritis degeneration of cartilage in sanovial joints and vertebrae. We have cartilage that cushions the joints and synovial fluid lubricates the joints. If that cushioning breaks down have arthritis. This is bone on bone pain. When bone scrapes against self causes changes to bone itself and damage to the joint. When cartilage erodes away have scraping of bone on bone, spurring and eroding of cartilage. Can happen idiopathically or secondary. Usually it is secondary: to rheumatoid arthritis, dm, congenital deformities, joint trauma, and most commonly wear and tear of joint due to repetitive motion. KNOW risk factors: Trauma Long term mechanical stress Inflammation of joint structure- rheumatoid arthritis causes inflammation of joint structure and then damage the synovial membrane and capsule and cartilage and cause osteo arthritis Joint instability- if not stable not press down in right spot causes wear and damage to joints Neurologic disorders- vertebrae damage in the spinal cord in vertebral column or herniation or bulging of disc or wear and tear of spinal column get osteoarthritis Congenital or acquired skeletal deformities Hematological or endocrine disorders- autoimmune disorders that affect the synovial membrane or connective tissue cartilage. Drugs Overweight or obese- more mechanical stress on joints more prone to osteoarthritis, more wear and tear. NOT related to nutritional intake or calcium intake. Not about bone too thin but bone compressing on joints and synovial membrane damaged and that surface area becomes fissured and broken down and damages joint. Bone contours to be jagged and can break off and cause inflammation in cartilage. Thickens the cap. Bone not smooth- it becomes jagged. Have joint pain and problems moving the joint properly. KNOW S&s- Dull aching pain in joint- relieved by rest bc joint not engaged Numbness or tingling at night if nerve entrapped Crepitus- crunching sound on joint with movement Edema and stiffness of affected joint Decreased ROM Heberden’s nodes- distal buckle. Hard nodules in distal interphalangeal joints Bouchard’s joints- buckle at the knuckle. Hard nodules in proximal interphalangeal joints. Can be spectrum. Inflamed go away and then have underlying bone damage so takes time to develop. KNOW Rhematoid arthritis- SYSTEMIC autoimmune disease that affects the joint and connective tissue. Affects more women than men. Antibodies attack connective tissue called rheumatory factors that attack tissue primarily in the joints. Synovial membrane and fluid and T cells activated attack the cartilage tissue causing inflammatory response and eventual damage to the joint with inflammation. Juvenile Rheumatoid Arthritis- large joints are affected and joint pain not as severe. Kids can get this. Systemic so can have rheumatoid nodule pockets of inflammation around the body. Cause of Rhematoid Arthritis is unknown Activation of inflammatory cascade attacking cartilage in the joints. The synovial digests the cartilage itself and breaks it down. S&S: autoimmune disorder symptoms Low grade fever Fatigue Body aches Joint swelling Decrease ROM Joint tenderness and stiffness worse in the morning. RA vs OA- OA is repetitive motion better with rest while RA is joint tenderness worse in morning when wake up and have more stiffness then too. Not related to activity like oa is. They have to work themselves out thru the day to feel better Extrasynovial rheumatoid nodules in skin, fingers, elbows in 20% of people. Pockets of fluid in other parts of the body. Spectrum of characteristics for criteria to diagnose. Systemic. Oncology Patients showing up for any other reason could have cancer. Stumbled on. 1 in 3 have cancer. Cancer-any disease characterized by abnormal cell growth and development caused by damaged DNA. When cancer cells replicate mutate and form own cancer cell. KNOW what makes a cancer cell a cancer cell and really what makes it malignant neoplasm is it performs division differently, differentiate differently and even perform apoptosis dif than normal. Divide differently and differentiate dif than normal cells and die differently than normal cells. Any new growth is neoplasm- not necessarily a cancer cell but can be benign neoplasm not cancerous or malignant neoplasm which is cancer. Neoplasm is not interchangeable with cancer bc can be benign. Cancer have many types and affect any stage of life. Try to do early screening and detection before metastasis. Screening in early stages make much more treatable. The second leading cause of death in kids 1-14 is cancer. Cancer? Group of diseases in which normal cells have mutations causing abnormal growth of the cell and spread. Most cells when touch other cells don’t move but cancer cells able to metastasize- spread. Malignant tumors after multiple mutations. Can’t use only one drug bc of multiple mutations. Abnormal growth and lose designated appearance and have large or multiple nuclei. Cancer cell loses function and migrate. They lose contact inhibition where stop when touch other cells. Malignant tumors- usually not encapsulated (benign encapsulated) and have irregular shape and have fingerlike projections that invade surrounding tissue. Dif bet benign and malignant tumor? biopsy by seeing under microscope. KNOW Risk factors: #1 smoking Lifestyle- tobacco, alcohol, diet, sexual behavior, obesity, stress Genetics- family hx Environment Personal- age, fitness, race, job, reproductive hx, hormones. Even healthy get it. KNOW Warning symptoms CAUTION: Change in bowel or bladder habits freq, urge, bloody stool, pain w/ defecation, change in stool appearance A sore that doesn’t heal Unusual bleeding or discharge, esp vaginal bleeding in woman postmenopausal. Thickening or lump in breast or elsewhere Indigestion or difficulty swallowing, reflux hx bc prone to strictures and cancer Obvious changes in wart or mole Nagging cough or hoarseness KNOW Metastasis- ability of cancer cells to migrate and invade other tissues and form secondary tumors. It’s the major cause of death from cancer. If pt has metastasis it dif treatment of curative or palliative. KNOW major metastatic sites in the body: Lung- lots of nodes in chest cause cancer metastasized from another area to the lung Brain Liver- rarely a primary site of cancer. If have liver cancer or nodules usually it is secondary to metastasis bc all blood of intestines and gi tract goes to liver so great way for cancer cells to migrate Bone cancer Esp uterine, ovarian and prostate cancer since pelvis has lots of bones around it easy to spread to those bone sites. Metastasis can be direct invasion of nearby organ and tissue, through a structure like pelvis or abdomen, can cause skin and ulcerations of the tissue and not orderly spread. If take out and not get all of it even that one cell can multiply and cause another cancer outbreak. Must take out surrounding tissue as well. Diffusion through serous cavities such as pelvis. Lymphatic spread- local or distant lymph nodes via lymphatic drainage, sometimes asymptomatic. Enlarged lymph nodes and early sign/later sign that it is spread throughout. Hematologic spread- through bloodflow. KNOW Another cancer that is commonly spread thru bloodflow is colon cancer and spreads to liver through portal vein circulation. Most common cancers in USA are prostate cancer. 80% males have some after age of 80. So controversial if get screened by bloodmarker at advanced age bc have prostate CA at 80 and chemo might be worse for them than the actual disease. KNOW common cancer deaths by gender most in women – breast cancer, men- prostate ca. In both genders the leading cause of DEATH from cancer in both is- lung cancer. Women who smoke- uterus lining is fertile and always regenerating. Smoking might as well put in uterus bc fertile breeding ground for cells in the lining and adding carcinogen to it is nice way for cancer to grow and spread. Not need to know specific sites. Breast ca- grows in dif area of breast tissue. KNOW risk factors: #1 Family hx- first generation relative sibling or parent with breast ca increases the risk abt 5-10% Age Nullipara or late first pregnancy (after 35) never having childbirth until after 35. Having kids means less menstrual periods so less estrogen. Early menarche or late menopause- exposure to estrogen. Early menarche or late menopause. Mences at 10 and menopause at 65 more estrogen around so higher risk for estrogen related breast ca. late menarche and early menopause is less exposure to estrogen so less risk for breast ca. High fat diet- fat linked to prostate and breast ca. with breast ca cholesterol mimics estrogen and increases risk of breast ca. Breast cancer tumor is metabolite of cholesterol and it can then signal estrogen bc women more fat on bodies to bear babies and signal estrogen and reproduce but high levels of cholesterol can also trigger tumor growth and signal more estrogen release and cause breast ca. Alcohol or tobacco use Obesity- fat tissue increases estrogen Dense breast tissue- more fibrous and can increase risk of breast ca. KNOW S&S: Painless lump or mass on palpation- sign of cancer Clear, milky or bloody discharge Asymmetry of breasts Change in skin tissue- dimpling, inflammation Change in breast tissue- thickening Nipple retraction or scaly skin around nipple Arm edema- sign of lymph node involvement Enlargement of the cervical, supraclavicular or axillary lymph nodes. Prostate ca- slow growth of cancer cells in the form of tumors that originate in the postr prostate gland. Can progress to widespread bone metastasis and death. Primary prostatic lesions can invade the ejaculatory ducts and seminal vesicle. Malignant prostate carcinoma- urethra goes thru bladder and prostate gland so early indicator is straining when peeing. Cant tell if BPH where prostate growing vs prostate ca until get biopsy. KNOW risk factors: Age over 50- men get digital rectal exam, feels like almond and got smooth borders but if feel irregular borders can be sign of tumor Family hx- big risk factor High-fat diet- activates protein in abdominal cavity that increases cell proliferation. S&S: BPH symptoms Difficulty initiating stream of pee Painless hematuria Urine retention Pain with sexual orgasm Firm nodular mass with sharp edge Edema of the scrotum or leg (metastasis) Bone pain (metastasis) Lung Cancer- leading cause of death in both men and women. Malignant tissue rising from the lung tissue. Anaplastic is worse but rare very aggressive cell. KNOW risk factors: Smoking Any exposure to carcinogens: asbestos, arsenic Genetic predisposition S&S: Cough pattern change KNOW Hemoptysis- Coughing up blood is usually lung cancer or TB Decrease breath sounds over a tumor area Colerectal cancer- very treatable if screened early. Starts as a noncancerous polyp which develops on the lining of the colon or rectum. Adenomas are the polyps that can become cancerous. Takes years for polyp to become cancerous so colorectal screenings are very important. (people not do because prep is hard) Risk Factors: Excessive animal fat intake High carb and low fiber diet- it causes constipation and causes irritation to mucosa and continuous irritation causes cancer growth Family hx Any GI tract disesase Age over 50 Alcohol Hx of ulcerative colitis S&S: Rectal bleeding- also can be occult blood not seen Change in bowel habits Bladder cancer- higher in Caucasians and more in men, malignant tumor that develops in the bladder wall or grows into the wall, invading the underlying muscles. Not very common. May metastasize to surrounding organs. Risk Factors: Chronic bladder irritation- chronic UTIs or renal kidney stones Indwelling urinary catheters Use of cytoxan- cancer immunosuppressant med that can affect the bladder Exposure to chemicals and radiation Cigarette smoking Excess coffee and sodium intake S&s: Suprapubic pain after voiding Flank pain and tenderness Changes in urine stream Painless hematuria Dysuria pain with peeing Anuria is blockage from tumor and cant pee Fever and chills Melanoma of the skin- not need to know types. If exposed to sun getting yearly full body check. S&S: Sore that doesn’t heal Changes in moles, birthmarks, freckles, scars or warts Persistent lump or swelling Lesions on ankles or inside of knees Pigmented lesions on palms, soles or under the nails Elevated tumor nodules that may bleed Irregular bordered lesion with tan, black or blue colors Gynecological cancer- not go into specific. Highest mortality is ovarian cancer (kills more people but not as common) because it is usually asymptomatic and is diagnosed late, only know smth wrong when affects other organs like abdominal pain or fullness and by then has metastasized. Cervical cancer- can be screened early with a PAP smear. Genitourinary System Renal blood flow- kidneys receive 20% of blood during rest and gets reduced a bit during physical or emotional response. Drop in blood pressure almost immediate drop in Glomerular filtration rate. Very small arterial node feeds each glomerular bed. Actual minute filtration of sodium water happens in the tubules. Immediate filtration of large molecules vs smaller ones happen in the glomerular bed just the sifting of the molecules but the actual regulation of acid-base balance, fluid and electrolyte filtration water and sodium happens in the tubules. If have tubular damage then have problems with acid-base. If have problem with glomerular bed then allow larger particles like protein and sugars to go through that shouldn’t be going through. One is a large sieve the other is for minute particle filtrate. Function of kidneys- be aware of bc when it fails know what presentation the pt will have. Hormonal-endocrine role- KNOW RAAS cascade. Kidney functions to regulate blood pressure and blood volume. Increase in more osmolality so less fluid and more particles so fluid status is fluid volume deficit dehydrated. If too many solutes then most likely dehydrated and this triggers the cascade to hold onto sodium and water, triggering ADH and for kidneys a decrease in blood pressure to the kidneys triggers RAAS cascade. The Renin releases angiotensin and turns into Angiotensin I. Then angiotensin I is converted to Angiotensin II which increases blood pressure by vasoconstricting and stimulates adrenal cortex to secrete Aldosterone. Aldosterone secretion causes the retention of sodium and water. Urine production rate- not be tested on the values but will be part of questions. Oliguria- decrease in urine output less than minimal expected production rate. <400-500 mL in 24 hours Anuria- no urine output <100 mL in 24 hours Normal 1800 mL in 24 hours Not too much into structures of kiney Urethra- women much shorter urethras then men so more frequent UTIs and male urethra much longer. Disorders of glomerular function- not overloaded of nephritic vs nephritic syndrome. Some are due to inflammation and others autoimmune processes that cause inflammation. Nephritic syndrome- problem with the glomerular bed. Glomerular bed with each arteriole feeding it will filter. Like any filter with holes things pass through so if damge to the filter than more permeability from things not supposed to like protein. If protein lost in the urine but tubles still intact so still be able to regulate acid base balance and signal RAAS rascade. Not problem with tubule but actual glomerular bed so protein be lost in the urine. Decrease in GMR than nephron and tubules can get damaged but not part of this syndrome. Increase in protein loss in the urine and blood loses protein so hypoproteinemia and protein allows oncotic pressure to stay in glomerular bed keeping fluid in vascular system and not shift in tissues so if decrease in oncotic pressure the fluid seeps into the tissues and pt gets edema. The liver will try to compensate for protein loss by releasing fat into the blood and pt gets hyperlipidemia in the blood. Glomerular disorders- filtration in the nephron so changes. KNOW Gromerulonephritis- inflammation of the glomerulus/glomerular bed. This is inflammatory response occurring at glom bed due to infection, lupus or vascular disease- collagen disease. KNOW If acute process it is due to infection. After pt had even a sore throat for a week or 2 like strep throat that same infectious process can cause antigen-antibody accumulation and damage at the glomerular bed level. Strep throat, staph, chicken pox mumps or measles can trigger glomerulonephritis. Rapidly progressing glomerulonephritis (RPGN) can be due to underlying disease process like lupus nephritis triggers antigen-antibody process due to the autoimmune disorder. Vasculitis- inflammation of small vessels can trigger this as well. Chronic glomerulonephritis- also lupus or vasculitis. KNOW S&S: inflammatory signs and symptoms Proteinuria- varies based on underlying disease and how much glomerular bed is damaged. Flank or back pain Hematuria- RBCs in urine not supposed to be there and got in Decreased urine output- affects Glomerular filtration rate so now less urine coming out Edema- kidney damage, cant regulate bp so nephron has decreased GFR. Malaise Fatigue HA Anorexia Nausea HTN- kidney damage, decreased GFR KNOW Contrast glomerulonephritis with nephrotic syndrome KNOW Nephrotic syndrome- massive proteinuria spec 3.5 grams or greater in 24 hours. Losing a lot of protein in the urine. Can be due to autoimmune attack of glomerular bed seen in children. In adults due to lupus severe exacerbation. Diabetics with uncontrolled diabetes, damage small vessels arterioles when out of control so get nephrotic syndrome. KNOW S&s: Proteinuria- massive shifts Hypoalbuminia Edema- really swollen Hyperlipidemia- break down fat to make up for oncotic pressure decrease Lipiduria- foamy urine is fat in the urine Decreased vit d- vit d binds to protein so loss of binding bc loss of protein and subsequent less calcium uptake KNOW Upper UTI vs. Lower urinary tract infections Urinary Tract Infections- bacteria enter through the urethra. Host defends with washout phenomenon- make urine and wash out the bacteria, protective mucus- lines the bladder, local immune responses and IgA, and normal bacterial flora. Tell women urinate after intercourse and that helps washout phenomenon occur. Risk factors: Age extremes Sexually active women Indwelling catheter Lower urinary tract obstruction diabetes mellitus immunosuppression KNOW culprit is usually E.coli usually due to HYGIENE (wiping front to back). Women more prone bc of anatomy. Lower urinary tract infection- cystitis inflammation of the bladder wall caused by an infection. More common in females. UTI that extends to the bladder but not beyond. Lower uti- urethritis. Inflammation of urethra caused by staph and other infections. In-house give nosocomial infection with indwelling catheters and can lead to urosepsis- septic shock. KNOW dif between lower tract UTI vs. upper tract UTI: S&s: All urinary tract infections show with pain, frequency, urgency, bearing down in order to urinate and may have hematuria pyuria- pus in the urine, bacterial growth evident in the urine. Fullness in bladder, bladder spams. Also cloudy and foul odor. With this info assume lower urinary tract infection. NO FEVER in lower UTI- fever means from bladder onto kidneys and ureters more complex uti. Also no flank pain and costovertebreal tenderness- this is pyelonephritis higher up in the kidney. Upper urinary tract infection- pyelonephritis. Bacteria moves up to kidneys. Can happen after chronic UTIs with scarring in bladder or ureters or anatomic reasons like peristalsis stops and backs up the urine leading to infection. From bladder to ureters, renal pelvis and renal parenchyma (actual tissue of the kidney) S&s: more systemic infection symptoms Tachycardia *Fever chills *Flank or back pain/tender costal vertebral angle (TVA) Abdominal colicky discomfort coming in waves bc urine tries to be expelled from kidney in waves (peristaltic pain) Nausea and vomiting- due to pain General malaise or fatigue Dysuria, urgency, frequency, hematuria, pyuria nocturia Urinary tract obstruction- obstruction from urethra all the way to renal pelvis where ureters attach to kidney itself. Can lead to renal failure. Urgent attention needed bc kidney has hard shell on it and cortex cant swell easily so if urine backs up it increases pressure in the tissue and obstruct flow and kidney become ischemic and nephrons start to die. Medical emergency Causes: renal calculi, a neurogenic bladder- Not enervating the bladder and ureters to expel urine so CNS stroke, brain injury cancerous tumors obstructive uropathy obstructive uropathy-urine backs up from ureters into the kidney. Factors affecting the severity of the OU is location of the lesion whether one or both upper urinary tracts are involved, the severity of the obstruction the length of times of obstruction and the nature of the obstruction. Calculi, tumors, strictures. Anything restricting flow can cause uropathy. Hydroureter- abnormal enlargement of the ureters Hydronephrosis- abnormal enlargement of the kidney Uretohydronephrosis- abnormal enlargement of the ureters and kidney proximal to the obstruction (anything above it becomes enlarged) Upper urinary tract obstruction- most common cause is kidney stones. Pathophysiology of kidney stones/renal calculi- urine becomes concentrated insoluble material and crystals form which can then block surrounding tissue. Hydronephrosis can occur completely blocking outflow of urine. KNOW risk factors: Age Gender Fluid intake- usually flush out crystallized but if dehydrated not able to flush out the materials and they will accumulate in the urinary tract *Excess vitamin d and calcium intake - Calcium deposits are most common cause of kidney stone formation Lack of exercise *Location- temperature, humidity and rainfall. Living in sunbelt is higher risk bc of dehydration Calcium stones are most common-High amount of calcium circulating in the blood and exercise high impact lets calcium go into the bone so those pts might also have underlying osteoporosis as well bc with bone resorption release of calcium into the blood as well if they are immobilized. Magnesium ammonium phosphate stones- form usually in infected urine Uric acid stones- related to Gout and accumulation of uric acid in the diet Cysteine stones- rare, kidney defect not allow cysteine be removed Stones can form anywhere in urinary tract usually in renal pelvis or calosis? Causes: Dehydration Infections Changes in urine pH- urine acidity usually 4-6 so if alkalinize too much than stones can form Obstruction- backup of flow Immobilization Diet- too much calcium Metabolic factors Diabetics more prone to calculi KNOW S&S: Dull aching flank pain travel from lower back to sides Different from pyelonephritis which is usually localized in CVA. Kidney stones is radiating flank pain going down to groin, lower back and sides Colicky Wavelike peristaltic pain as well- as body tries to expel urine and calculi Nausea vomiting Hematuria Abdominal distention from the blockage Oliguria- decrease in urine output if the blockage affects urine output Lower urinary tract obstruction- due to tumor in the bladder, enlarged prostate (urethra passes thru prostate in male anatomy), stricture, many STIs can cause scar tissue in bladder. May involve the bladder, bladder neck, prostate or urethra. S&S: alterations in urine excretion symptoms Daytime voiding frequency Nocturia Poor force of urinary stream Intermittency of urine stream Bothersome urinary urgency, sometimes with hesitancy Incomplete bladder emptying Benign or malignant tumors renal cell carcinoma- most common renal neoplasm KNOW Risk factors: Tobacco use- carcinogens Obesity Long term analgesic use- acetaminophen, NSAIDS cleared by the kidneys and make them overwork causes mutations S&S: Hematuria Flank pain Palpable flank mass Unexplained weight loss- cancer causes person to use up a lot of energy Bladder tumors- scope like other cancers Renal Failure- KNOW differentiate the types of renal failure understand the concept behind the classification of renal failure. Renal insufficiency- occurs with decrease in renal function Renal failure- can be acute or chronic Acute renal failure- further divided into prerenal, intrarenal and postrenal. Chronic renal failure/ chronic kidney disease comes in stages 1-5– not need to know. Could have chronic kidney disease and then slipped into acute renal failure. Chronic kidney disease the patient can compensate with the kidney function they have however limited it is. Once a pt is in true kidney failure need to dialyze the pt. AKI acute kidney injury or acute renal failure-the sudden inability of the kidneys to regulate fluid and electrolyte balance and to remove toxic products from the blood. overwhelming trauma or shock to the kidneys and loss of glomerular function or tubular function. KNOW classifications of acute renal failure Prerenal- the flow of blood volume into the kidney. Intrarenal failure- actual damage to glomerular bed or tubules. Postrenal- simple obstruction of urine output from the kidney. Prerenal- most common and reversible form of renal failure. Lack of volume output into the kidney. Fix the flow problem quickly and it is fine. KNOW causes: with volume or pump Pump problem decrease in cardiac output the kidneys feel it very quickly Cardiac tamponade MI Cardiovascular disorders- cant perfuse the kidney. Within half hour of decreased perfusion the kidney shuts down. Major sign is decreased urine output Hypovolemia/hemorrhage- decrease in volume, GSA, massive surgery etc. losing lots of fluid Burns Dehydration Diuretic overuse Peripheral vasodilation- vasodilate too much with sepsis causes permeability and vasodilate arterioles so don’t get enough perfusion pressure for GFR to be met. Decreases perfusion to arterioles and decreases GFR Antihypertensive drugs Sepsis Renovascular obstruction- renal artery obstruction (must be flow to kidney so arterial flow), renal artery tumor compressing it tumor Lack of good flow to kidney but not damaged, kidney still doing its job. Not enough perfusion pressure and not enough GFR. If not catch quick enough the tubules can start to die off. Prolonged prerenal failure can turn into intrarenal. Intrarenal failure- Prolonged prerenal failure where either glomerular bed or tubules start to have problems. Caused by: Massive glomerulonephritis affected the glomerular bed decreases GFR not going to be able to perfuse the nephrons Pyelonephritis- infection with inflammation affects tubules and glomerular bed Polycystic kidney disease- multiple cysts that form within the kidney tissue, when they rupture they bleed or multiple stones also cause damage to the kidney Diabetes mellitus and high blood pressure- damage the glomerular bed Transfusion reaction- wrong blood causes huge antigen-antibody complex and clog up the glomerular bed and knock off flow to the kidney and occlude glomeruli and tubules Severe crush injury- causes muscle cells released into bloodstream and obstruct the tubules *Acute tubular necrosis- ATN most common form of acute intrarenal injury bc occurs due to prolonged septic shock/ischemia to the tubules. Prolonged septic shock is a form of prolonged prerenal and if vasodilated not perfusing nephrons than tubules suffer and become necrotic and die off. 2 most common causes of acute tubular necrosis is prolonged ischemia due to prolonged septic shock state (Any pt can get infection that gets septic and get acute tubular necrosis) and medications that damage the kidneys- NSAIDS (glomerular damage) Aminoglycosides (antibiotics damage tubules)- nephrotoxic to tubule itself so always monitor the peak and trough to make sure therapeutic levels of vancomycin but not toxic if too much kidneys not clearing then kidney starts to fail. Keep vancomycin and aminoglycosides at trough level. Pathophys- renal capillary swelling and cellular proliferation due to cortical involvement of vascular, infectious or immunologic processes. This decrease in GFR occurs secondary to obstruction of glomeruli by edema and cellular debris causing oliguria- decrease in urine output. PostRenal- anything blocking flow from kidney and ureters and bladder and out. Lack of flow and causes buildup of pressure and can cause hydronephrosis. Fluid backs up into kidney and it starts to swell. That increased pressure leads to decreased GFR (a pressure gradient from arterial to glomerular bed) back up of flow impedes GFR. Prolong prerenal and postrenal can lead to intrarenal. bladder obstruction Anticholinergics- if pt not have stimulation/bladder reflex need to be straight cathed like spinal cord injury pts cant enervate bladder reflex Autonomic nerve dysfunction Lack of flow and causes buildup of pressure and can cause hydronephrosis. Fluid backs up into kidney and it starts to swell. Infection Tumor Urethral obstruction Prostatic hyperplasia or tumor Urethral obstruction Blood clots Calculi Edema Inflammation Hemorrhage Surgery Uric acid crystals Acute renal failure pt have difficulty getting rid of toxins and waste products. BUN and creatinine rise get irritable, ha and anorexia, some CNS issues, nausea and vomiting and cant rid of fluid, can’t regulate hydrogen ion balance and circulating toxins can cause coma state, drop in urine output, increased acidosis. KNOW manifestations of renal failure esp in your labwork!! Better hallmark of intrarenal nitro or creatinine? Creatinine better marker bc that is the actual filtration at the tubular level which is damaged. Blood urea nitrogen BUN is signal of protein and muscle breakdown. Prerenal failure better marker is BUN bc that means pt not enough flow perfusion and clearance cant get rid of product but actual nephron not damaged yet. S&S: Azotemia- elevated BUN and serum creatinine Elevated BUN Elevated serum creatinine Metabolic acidosis-Kidney rids of hydrogen ion and holds onto bicarb so a pt in metabolic acidosis means have problems clearing hydrogen ions. Cant excrete H+ Cant conserve bicarb Anuria Oliguria Can’t concentrate the urine Electrolyte imbalance Edema with Excess water and sodium retention bc nephron cant respond to adh and respond to aldosterone so RAAS cascade out of wack. Can’t rid of water. High Potassium which triggers calcium to be held on so low serum calcium Low serum calcium anemia Deficient in erythropoietin production- cant signal RBC production in bone marrow and regulate blood pressure so pt becomes hypertensive Hypertension Have pt on low protein- bc less work for the kidney and elevated BUN which shows level of protein and there is trouble excreting it so low protein. Also bc holding lot of water give low sodium and low potassium. Give calcium supplements bc being held in the bone. KNOW labs: Hyperkalemia and hyponatremia bc fluid overload dilutes the sodium levels, hyperphasphatemia and hypocalcemia go together, increased BUN, increased creatinine and metabolic acidosis, anemia. Chronic renal failure- happens over time and could have a sudden onset with further destruction. S&S of chronic renal failure: same as acute failure Hypervolemia, labs same as acute, azotemia, metabolic acidosis, anemia, peripheral neuropathy Uremic frost- excess of uremia that kidney cant filter from ammonia breakdown and have froth and odorous on pt’s skin and makes them very itchy. KNOW treatment- need to give diuretics initially to rid of volume and hypertensives and support ability to make new RBCs so give vit D, iron, folic acid and epogen- synthetic erythropoietin. May need to dialyze them. KNOW uremia and its indication for dialysis- filtration of their blood by a machine. They have to have acidosis, hyperkalemia, hypertension altogether. Increased creatinine and bun. They have changes to their CNS system- affect brain function and neuro status, confusion, lethargy or coma sign they are uremic and need to be dialyzed. When pt is uremic have systemic affects from the circulating toxins and electrolytes. Toxins can also interfere with platelet aggregation so the pt is at risk for bleeding called uremic bleeding can have spontaneous gi bleeds or other bleeds. Uremia is the manifestation of the renal failure systemically with possible bleeding, platelet dysfunction, cns changes, hyperkalemia, and acidosis. These are indications for dialysis. Male Genitourinary system: KNOW erectile dysfunction- inability to achieve and maintain an erection sufficient to permit satisfactory sexual intercourse. 10-20% is neurogenic- Parkinson’s, stroke, cerebral trauma: can’t get an erection Hormonal- decrease in androgen levels Vascular issues- hypertension, stenosis of the common penile artery Drug induced- antidepressants antipsychotic, antiandrogens and antihypertensives- beta blockers Psychogenic- performance anxiety, strained relationship with a sexual partner, depression Penile disorders Balanitis- inflammation of the glans: head of the penis. Diabetics more at higher risk. Balanoposthitis- inflammation of the glans and prepuce (foreskin) so must have foreskin and not circumcised. Can occur with phimosis: tight foreskin where foreskin cannot retract. Many times caused by Chlamydia and mycoplasma. Really it is guys with foreskin who are unhygienic. Peyronie disease- plaque usually due to trauma that forms in the shaft of the penis and depending on where it forms if it on anterior surface the bow will go upward and if posterior then penis go downward and cause painful erection and painful intercourse. KNOW priapism- involuntary prolonged erection greater than 4-6 hours and it risks blood flow to surrounding tissue and causes ischemia. Urologic emergency. It can occur at any time. Sickle cell disease and neoplasms are most common cause in boys age 5-10. During deoxygenation cells sickle and clot off and stop blood flow to tissues so cause abnormal engorgement to penis and priapism. Causes primary- trauma, infection and cancer neoplasm. Secondary- hematologic such as lupus, sickle cell anemia thrombocytopenia or neurologic- stroke or spinal cord injury. Renal failure, meds and alcohol also can cause priapism. Embryonic development of the testes- this channel should close after birth- but if not the testicles can slide down and cause testicular herniation- Diverticulum goes down into the testes. KNOW difs bet hydrocele, hematocele, and spermatocele Hydrocele- herniation that goes into testes and fluid can form there associated with inguinal hernia Hematocele- usually due to trauma accumulation of blood in the tunica vaginalis in that channel Spermatocele- sperm containing cysts that develops in the epididymis. Has pain. Usually asymptomatic. Varicocele- enlargement of the vein in scrotum where blood backs up bc of enlarged vein and testes temperature gets warmer and can affect sperm casing infertility. KNOW Testicular torsion- twisting of the spermatic cord in younger adult. Can be anatomic or traumatic. KNOW S&S: Pain NV Tachycardia Abnormality in testes such as large and tender Absent cremasteric reflex- when stroke ipsilateral thigh causes small elevation in testes 3-5cm. Can cause ischemia in testes so have 6 hours to untwist the cord or sx remove it. Epididymitis- inflammation of epididymis inflammation of the duct behind the testes where sperm passes thru the vast eporons? Transports mature sperm so has to do with ejaculation and can be nonsexual or most commonly STI related. Pain swelling erythema fever if infectious elevated WBCs and since mostly STIs screen sexual partners. Orchitis- infection of testes precipitated by UTI found mostly in adolescent males. Mumps orchitis- associated with mumps, infection of parotid glands. Fever, pain, enlargement of the testes. Risk for sterility. Which testicular disorder mostly by trauma? Hematocele Testicular cancer- most common cause of cancer in young males. Highly curable. Possible genetic component and related to cryptorchid or undescended testes. Might have enlarged testes, pain, tenderness. Diagnose by tumor markers. Disorders of prostate Prostate surrounds urethra so any change in size compresses urethra and causes urinary strain- weak stream, urgency, dysuria, discharge. Urethra is walnut sized gland between bladder and penis. Prostate gland should have smooth edges so if not need further workup. Prostatis- not need know classifications. Inflammation of prostate. Usually asymptomatic and related to infections. KNOW dif bet BPH and prostate CA KNOW BPH- nonmalignant enlargement of the prostate. Related to age as testosterone increases than prostate to compensate increases in number of cells hyperplasia. Decrease in testosterone release the prostate will increase in cells to compensate so overgrowth of prostate and obstructs the urinary stream. KNOW Prostate CA- most common male cancer in the USA but not kills most people like lung cancer. PSA screening mechanism but as men age prostate not work as effectively so prostate secrete PSA (prostate specific antigen) so have lots of false positives so PSA is controversial. Digital rectal exam after 50 and biopsy. Unclear ideology. Risk factors- family hx, age, high fat diet activates protein in abdominal cavity which increases tumor growth. Asymptomatic at early age then symptoms similar to BPH at later stage. Childhood disorders- Hypospadias- congenital disorder urethral groove further in the ventral surface of the penis Undescended testicles-10% of kids Epispadias- urethra opening on dorsal surface, less common Phimosis- tightening of prepuce/foreskin that prevents retraction over the gland and must be uncircumcised. Redness and swelling of the prepuce and can happen from infection or multiple UTIs or forceful retraction of the foreskin. Nurses insist on cleaning when push back and penis edematous and can’t get foreskin over gland/head of penis. Paraphimosis- medical emergency where covering can.t go back over and glans penis can become necrotic. Only in uncircumcised pts. Crytorchidism- undescended testes, most common in kids. Familial component related to premature infancy. This can be a problem and cause infertility but solved with hormones or sx. Female Genitourinary system Disorders of the external genitalia- Bartholin’s gland cyst and abscess, leukoplakia and vulvodynia Bartholin’s Gland Cyst and Abscess- a fluid filled sac results from occlusion of the duct system of the gland and can cause abscess- walled off area of infection. Most commonly follows an STI. Tender and painful. Infected gland that will protrude either on the inside walls of labia or externally. Risk for reoccurring. Leukoplakia- white lesions of the vulva usually due to irritation. Inflammatory process with itching, painful intercourse, hyperpigmentation so lichen is white and most common in post-menopausal women. Can be inflammatory and autoimmune but the scratching of it makes it more complex. Lichenification so whitening of skin after scratching and becomes plaquelike. Vulvodynia- unexplained vulvar pain. Can be due to nerve injury, trauma or muscle spasms or hormonal changes. Pain during intercourse or generalized burning pain throughout ADLs. Enervation of muscles of pelvic region are abnormal and highly sensitive. KNOW Vulvar carcinomas- 5% of female genital cancers in younger women often preceded by neoplasia so we check by PAP smear to show cell mutation. Related to HPV genital warts. In older women not usually HPV related but usually due to lichenification of tissue and itching and repeated injury to the tissue which can cause mutation in cell an squamos cell hyperplasia. Vaginal bacterial flora- many dif species of bacteria. Estrogen helps to maintain this flora by maintaining glycogen and glucose for the flora to live on. If have interruptions in estrogen levels and glycogen availability then your pathogens can overgrow. The acidity of the flora can change and allow other organisms to grow where the normal vaginal flora should be present. Antibiotics can also disrupt normal bacterial flora. Never advise women to deuche: instilling soaps and fragrances to clean inside of vagina. Vaginitis- inflammation of the vagina. Foul odor, Discharge, Redness, Swelling, Pain with urination, Pain with intercourse Caused by: irritants, foreign bodies, infectious agents, low estrogen levels in premenarche girls so inspect vagina but not with objects. Also antibiotics can change flora and pH of the tissue and increase risk of infection Not common Cervicitis- inflammation of cervix. Can be due to tampons, STIs, diaphragms and baby powder. Discharge and pain. KNOW and differentiate anatomic abnormalities cystocele, rectocele and uterine prolapse Causes- multiple vaginal deliveries, anal sex for rectocele, constipation can cause straining increasing pressures KNOW cystecele- herniation of bladder into vagina “the fallen bladder”. Muscle that supports bladder is weakened. S&S: Bearing down sensation Difficulty emptying bladder Frequency Urgency KNOW rectocele- herniation of rectum into vagina S&S: Difficulty in defecation KNOW uterine prolapse- uterus bulging into the vagina. Endometrial disorders Endometritis, pelvic inflammatory disease, endometriosis, endometrial cancer, leiomyomas Endometritis- not very common many times after abortion, delivery or instrumentation into uterus. Causes infection, bleeding, tenderness, fever, malaise, foul smelling discharge Pelvic inflammatory disease- infection that ascends through the uterus to fallopian tubes to the ovaries. Can be related to STIs. Non pregnancy related is known as PID. If not treated can cause infertility. If scar tissue forms than can have ectopic pregnancy. KNOW S&S: inflammatory response *Pain in lower abdomen and cervix (deeper pain than STI) Purulent discharge Increased WBC count Increased C-reactive protein Endometriosis- tissue from uterus attaches outside of uterus to abdominal cavity all the way to kidney and small bowel adhesions, peritoneum. Not sure why. Retrograde menarche so instead of products of menstruation being completely evacuated they lodge up the abdominal cavity and stay there and shed every menarche and affected by estrogen changes thru the menarche cycle. They have longer periods, increased pain, increased bleeding. Ectopic implants shed and respond to estrogen secretion every period. This can be cause of adhesion and scarring. Uterine leiomyomas- fibroids most common benign tumor growths of smooth muscle in the uterus. Can be asymptomatic until large enough to cause bleeding, hydroureter or bladder problems. Ovarian disorders- Ovarian cysts and polycystic ovary syndrome Ovarian cyst- most common form of ovarian tumor. Cyst filled with fluid or blood usually benign. Can be developed any stage of life. Not need know follicular or functional. They are asymptomatic until obstruct tissue and they can rupture with hormonal changes or just stay until become painful. Polycystic ovary syndrome- not sure why happens can be genetic. Increase in male androgen hormones that interfere with release of eggs. Though have menstrual cycle where follicle matures have LA surge and follicle opens and ovulation occurs but with POS the LH level continues but not have subsequent dropping of the egg/ovulation. Increase in LH hormone but decrease in follicle stimulating hormone so no ovulation. S&S: Hyperinsuilinemia- insulin resistance, possible relationship of insulin in adrenal cortex. Obesity- high blood sugar DM II HTN Hyperlipidemia Menstrual irregularities Hirsutism/acne/infertility- increased androgen, women trying to get pregnant and not able to. Can stimulate the follicular maturation but not able to stimulate release of the follicle. Menstrual cycle disorders- Primary Amenorrhea, secondary amenorrhea, dysmenorrhea, premenstrual syndrome, menopause Primary amenorrhea- failure to menstruate by 15 yrs old and 13 without secondary sex characteristics. Suspect a congenital or hypothalamic-pituitary-ovarian acis disorder. So check for pituitary tumor. Secondary amenorrhea- menses that stopped after 6 months of regular cycle. Also look for tumors. Alteration of fat to muscle ratio can also cause the disorders. Fat helps estrogen so athletes with low fat have trouble getting periods. Dysmenorrhea- pain with menses. Can be due to excess prostaglandin production or structural problems. Can be fibroids, adhesions, scar tissue, pelvic inflammatory disease, etc. KNOW the changes in Premenstrual syndrome- physical emotional and behavioral changes. PMS molomina-mild symptomology of irritability or HA PMS- mild to moderate changes PMDD- premenstrual dysphoria disorder, severe mood disorder that has real changes in personality and irritability treated with hormones or antidepressants. Can kill husbands S&S: Painful swollen breasts, Bloating, abdominal pain, HA, backache, Depression, irritability, Behavioral changes KNOW affects of Menopause- cessation of ovarian function and estrogen. Precede 4 yrs before by premenapause symptomology. KNOW Estrogen helps bone calcium reuptake so with menopause get osteoporosis and also estrogen lowers cholesterol so menopause have same risk for coronary heart disease as men. Decrease in breast tissue, body hair, skin elasticity, SQ fat. Ovaries etc become friable. S&S: hot flashes, palpitations, dizziness, HA, insomnia, irritability, anxiety, depression, osteoporosis, coronary artery disease [Show More]
Last updated: 3 years ago
Preview 1 out of 115 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$12.50
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Jul 07, 2021
Number of pages
115
Written in
All
Additional information
This document has been written for:
Uploaded
Jul 07, 2021
Downloads
0
Views
138




.png)



 V1-V2.png)
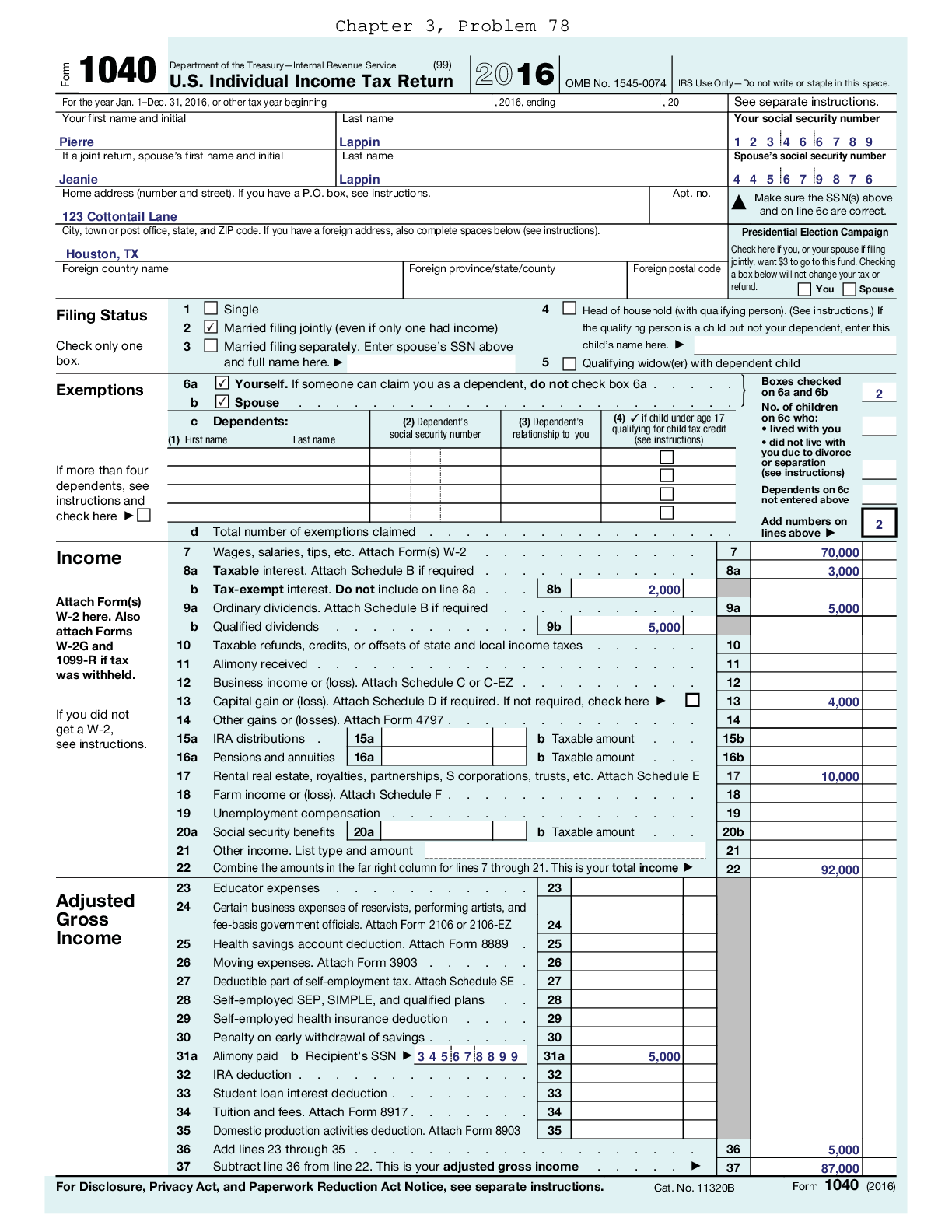
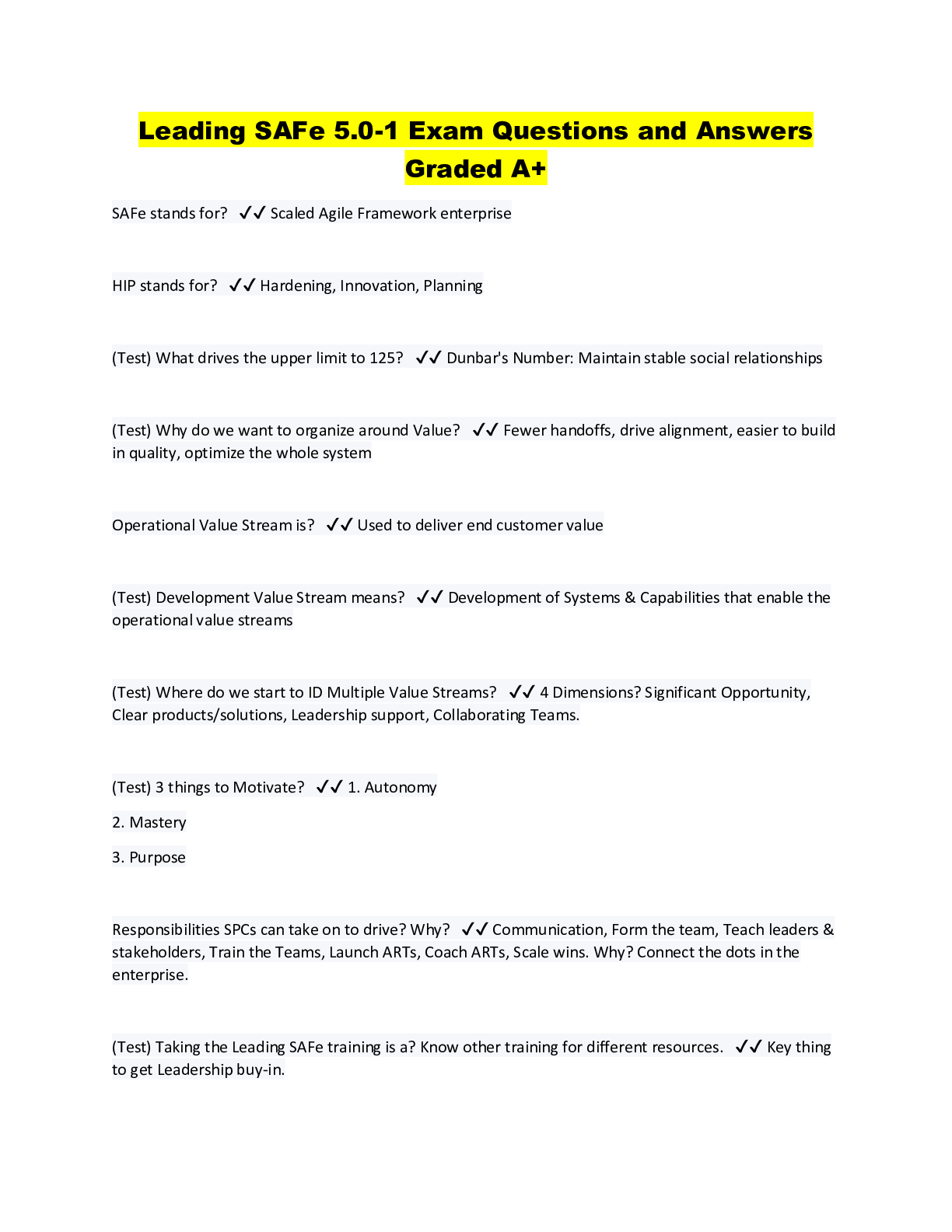

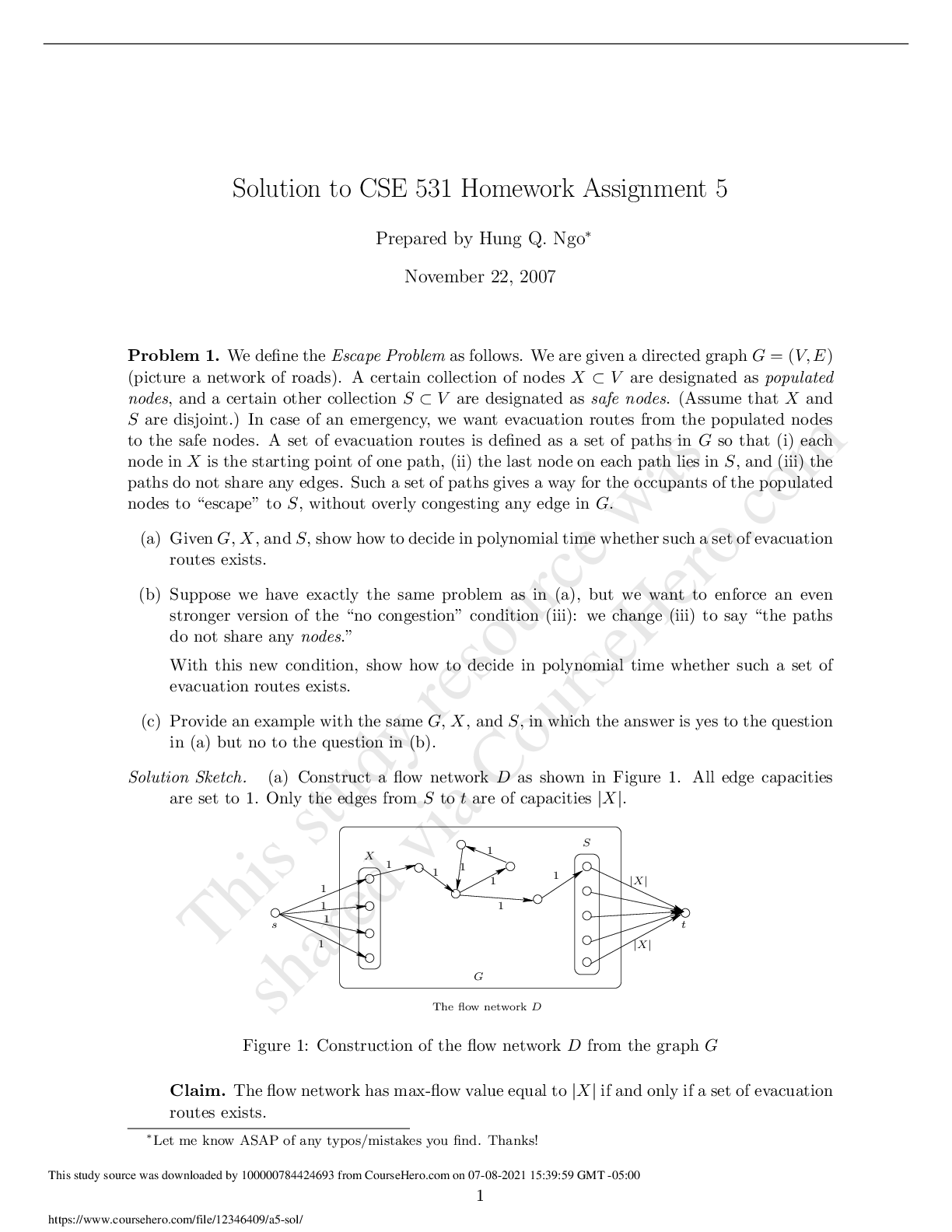
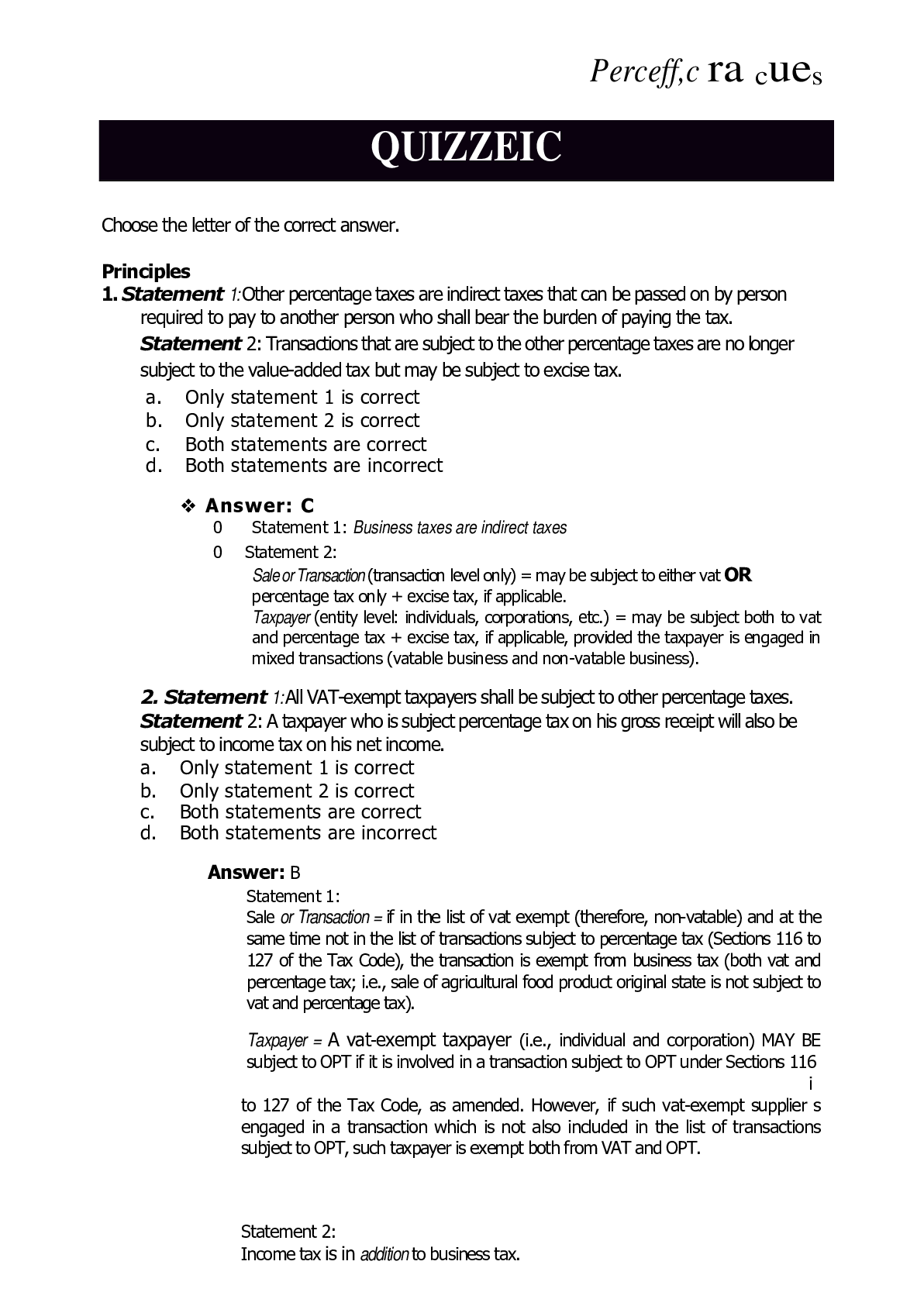
.png)

