Pearson Edexcel Level 1/Level 2 GCSE (9-1) Time 1 hour 30 minutes Geography B Paper reference 1 GBO/02 PAPER 2: UK Geographical Issues
$ 7
.png)
California DMV Permit Test Questions and Answers Verified A+ Work
$ 10
Test_Bank_for_Managing_Supply_Chains_A_Logistics_Approach_International
$ 15
2023 GCSE Combined Science Chemistry A Gateway Science J250/09: Paper 9 (Higher Tier) Question Paper & Mark Scheme (Merged)
$ 7

1183-c-interview-questions-and-answers[100% verified
$ 9
eBook Gravity and Magnetic Exploration: Principles, Practices, and Applications 1st Edition by William J. Hinze, Ralph R. B. von Frese, Afif H. Saad
$ 30

PSPO I, PSM I e SOLVED 2023 EXAM ALREADY PASSED.
$ 19
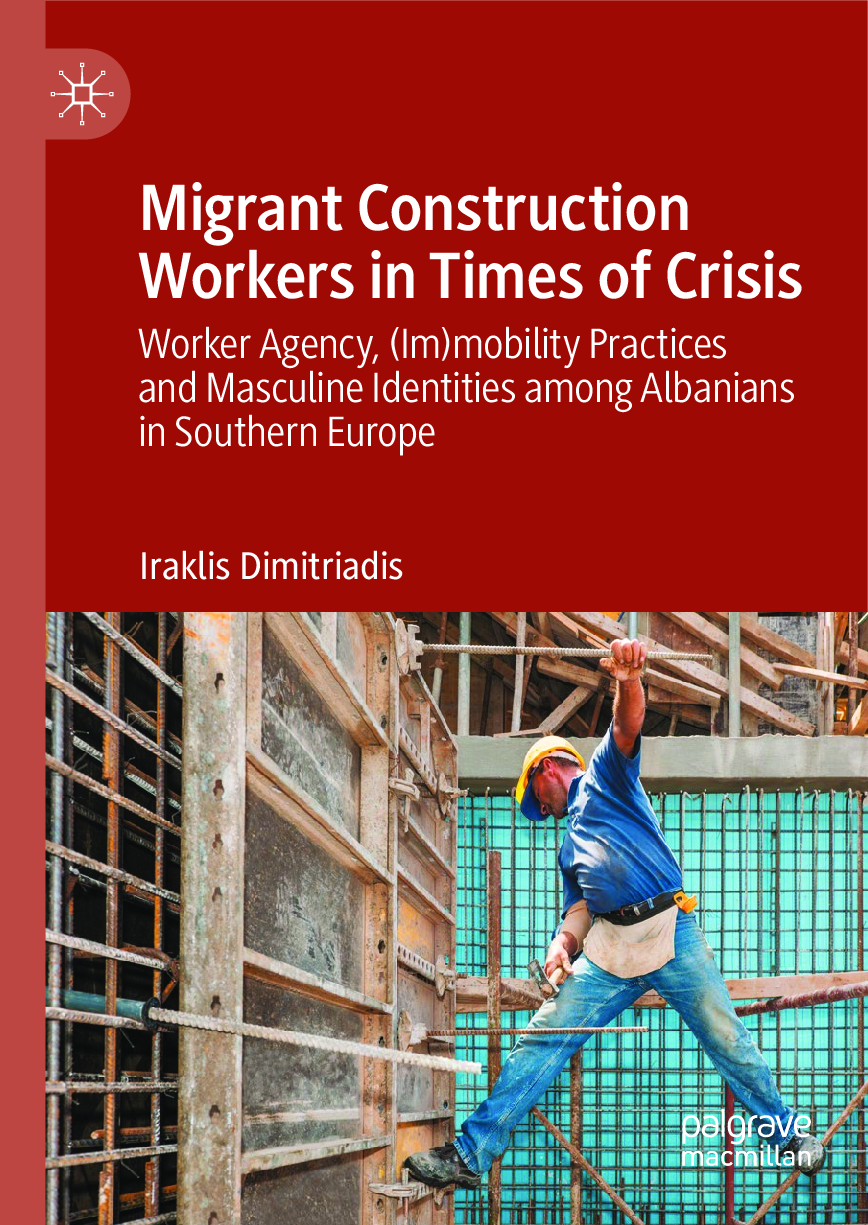
eBook [PDF] Migrant Construction Workers in Times of Crisis Worker Agency, (Im)mobility Practices and Masculine Identities among Albanians 1st Edition By Iraklis Dimitriadis
$ 29
Innovative and Strategic Thinking / D081 Study Guide / WGU 2025 Update & Task Prep
$ 7.5
Grand Canyon UniversitySEC 510Classroom Management Philosophy.
$ 5

Worcester Polytechnic Institute - BME 2210BME2210_B17_HW5.
$ 7
RSPT 2325 Exam Guide With Complete Solutions
$ 9

[Test Bank] for Electric Circuits, 12th edition By James W. Nilsson, Susan Riedel
$ 25
Solutions Manual for Computer Networking A Top-Down Approach 6th Edition
$ 14

WGU 468 - OA Information Management and the Application of Technology( Questions And Answers).
$ 12

NAPSRX PRACTICE QUESTIONS- TEST PREP
$ 10
NCLEX STUDY GUIDE FOR EXAMS 2023
$ 15
Architecture Appreciation Test 2 | 81 Questions with 100% Correct Answers | Verified
$ 10
WGU C182 Final Exam Study Set Latest Updated 2022 Graded A+ (195 Questions with Correct Answers
$ 9

Pennsylvania State University - EA 3L08 & L09 Focus Question Response ( WITH WELL DETAILED ANSWERS )
$ 7
[eBook] [PDF] Hands-On Ethical Hacking and Network Defense, 4th Edition by Robert Wilson, Michael Simpson, Nicholas Antill
$ 25
[eTextBook] [PDF] International Environmental Law Text, Cases and Materials 1st Edition By Malgosia Fitzmaurice, Meagan Wong, Joseph Crampin
$ 29

NSG 6430 Week 10 Knowledge Check (Q&A)
$ 4
D335 ITSW 3126 Introduction to Programking with Python - Latest FA Review Q & S 2024
$ 11
EXAMINATION QUESTION AND ANSWERS IN BASIC AND PHYSIOLOGY MULTIPLE CHOICE QUESTION;CHAPTER 1 - Organisation of the Body
$ 6
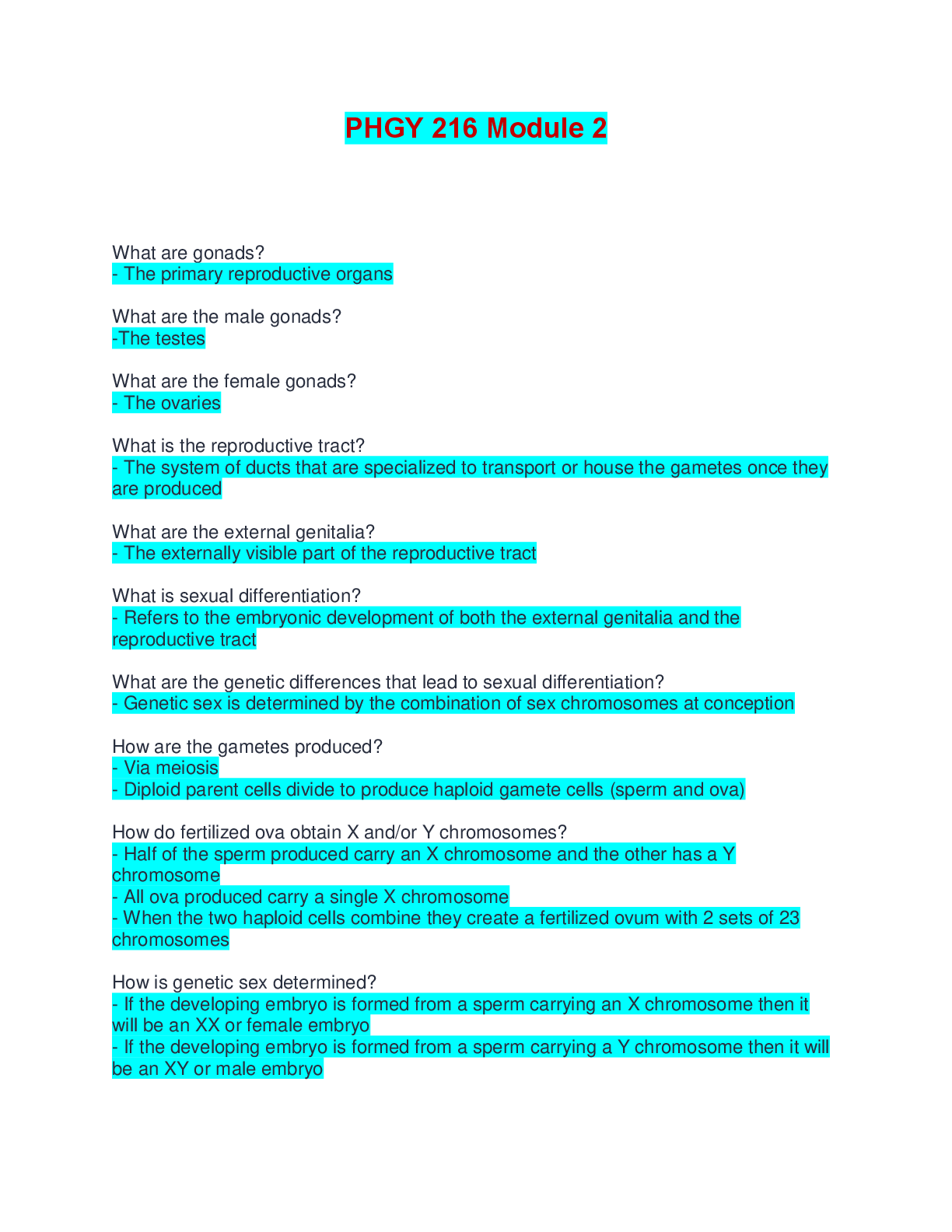
PHGY 216 Module 2 Exam | Questions with 100% Correct Answers