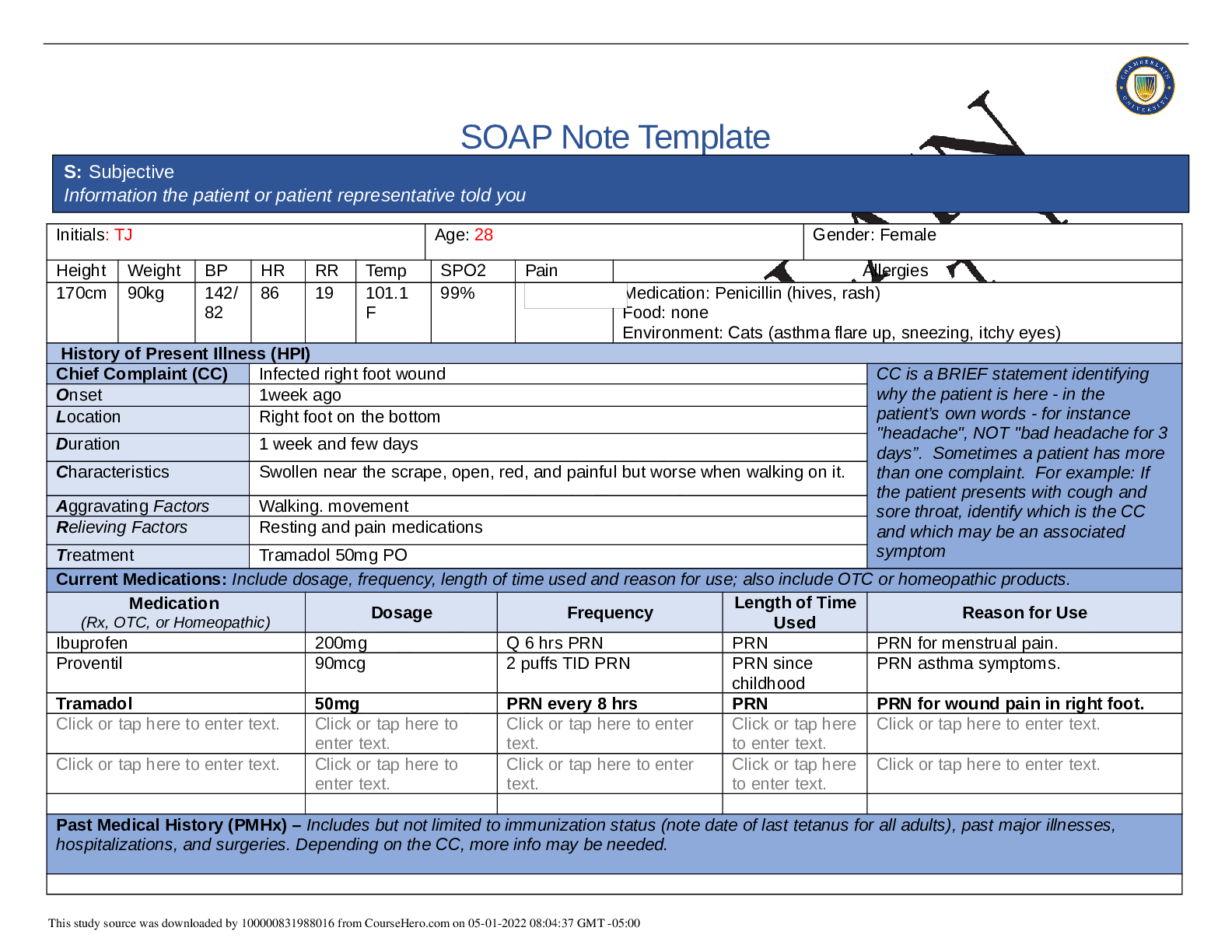
SOAP Note Template
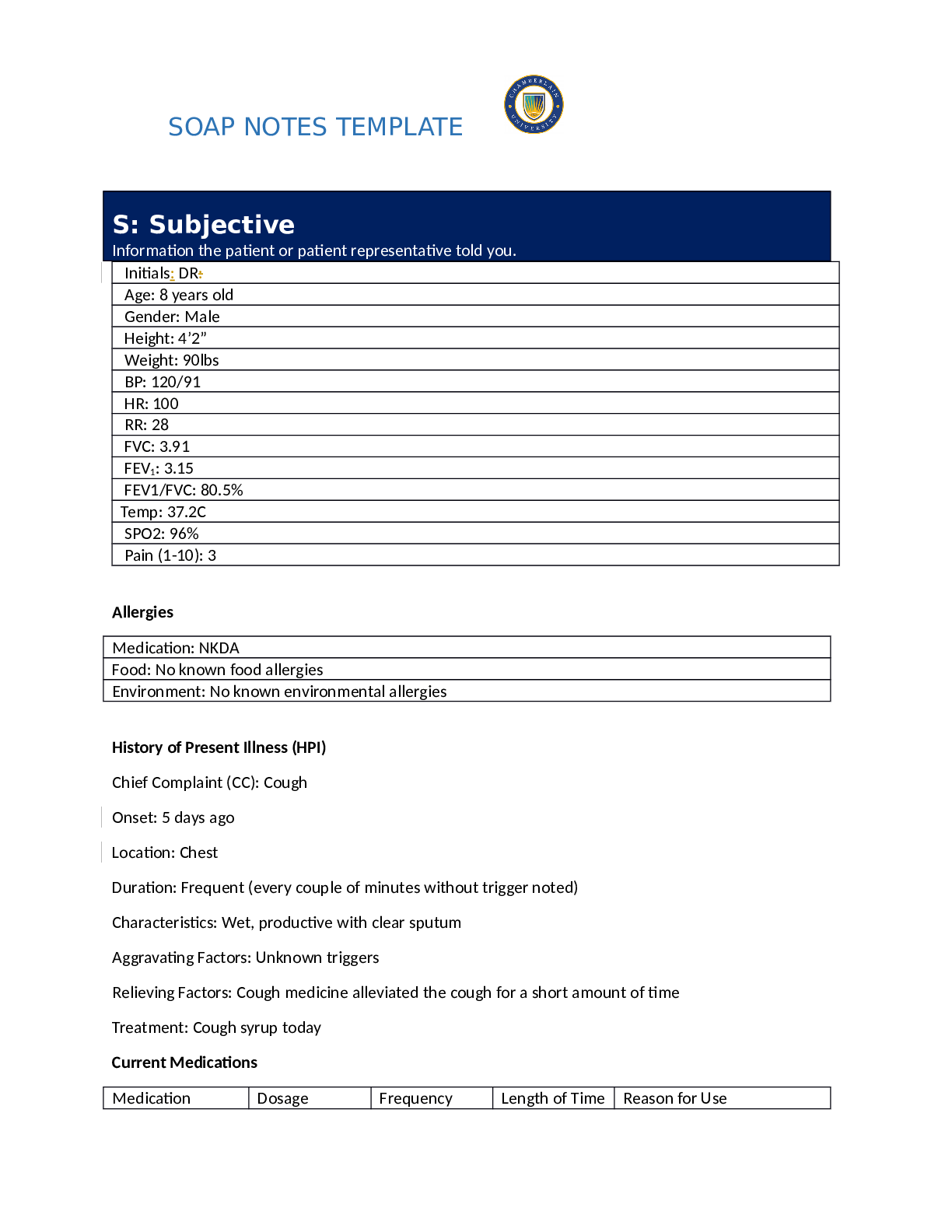
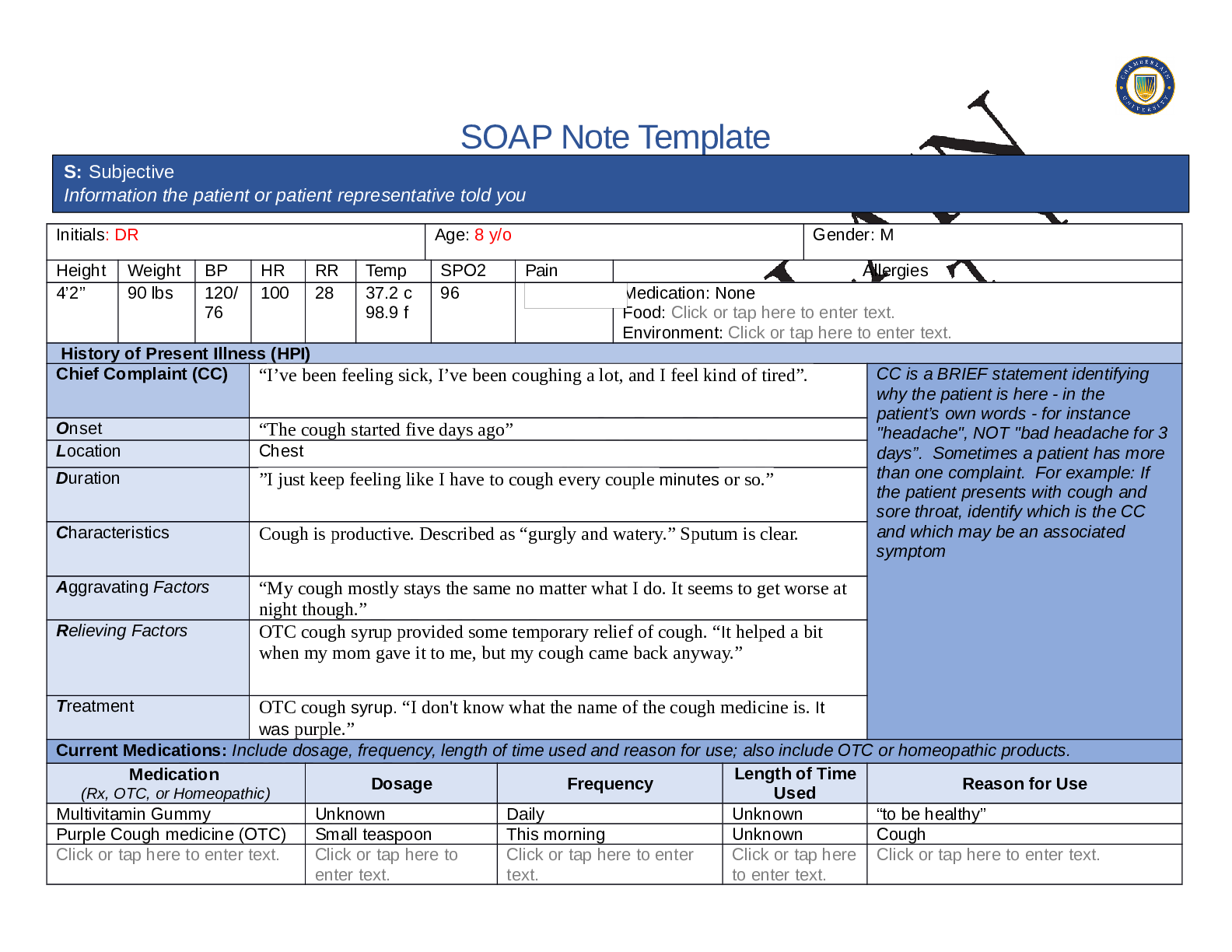
Initials: D.R. Age: 8 Gender: male
Height Weight BP HR RR Temp SPO2 Pain Allergies
4’2 90lbs
per
patient(
unable
to get a
standin
g
weight.
120/
76
100 28 37.2c 96% Medication: Denies
F
...
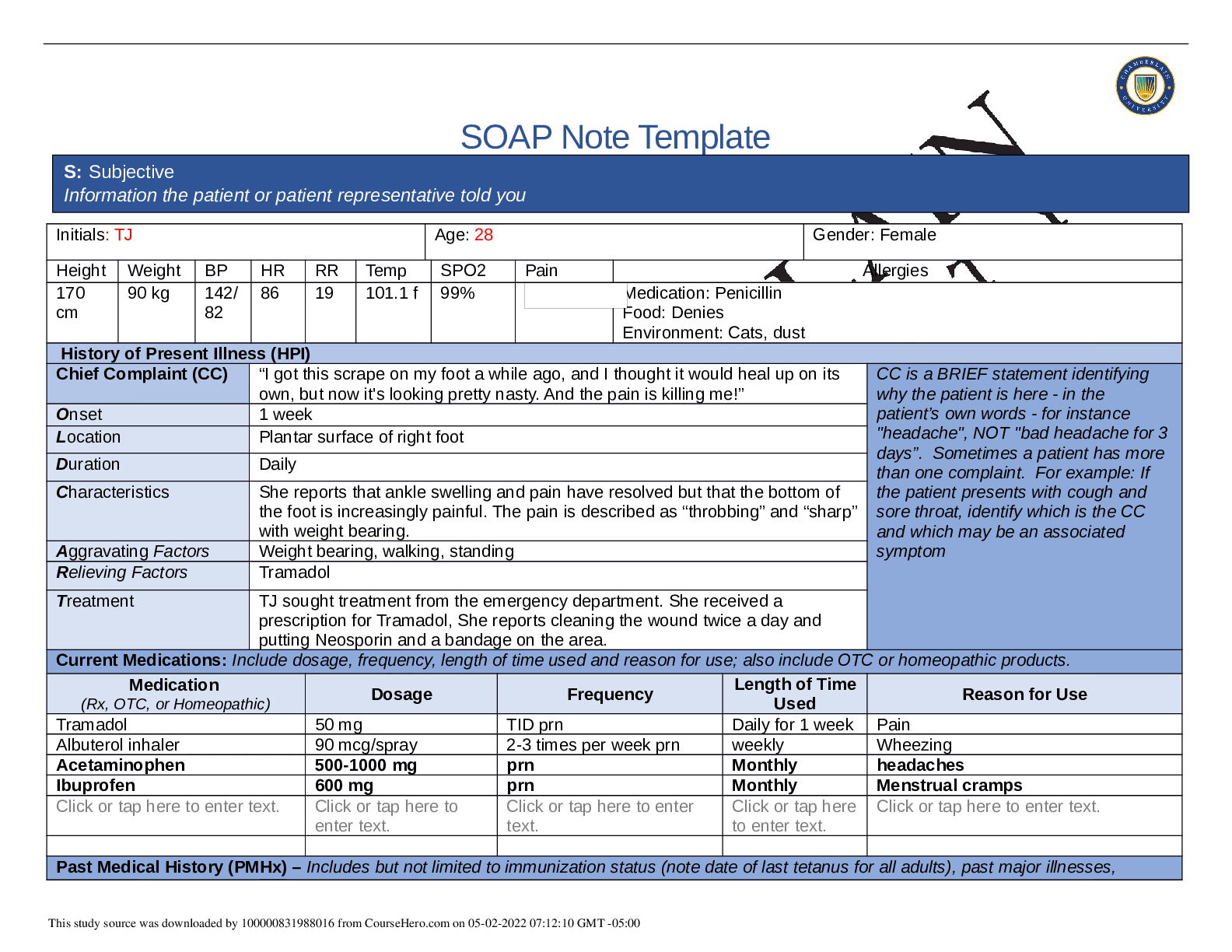
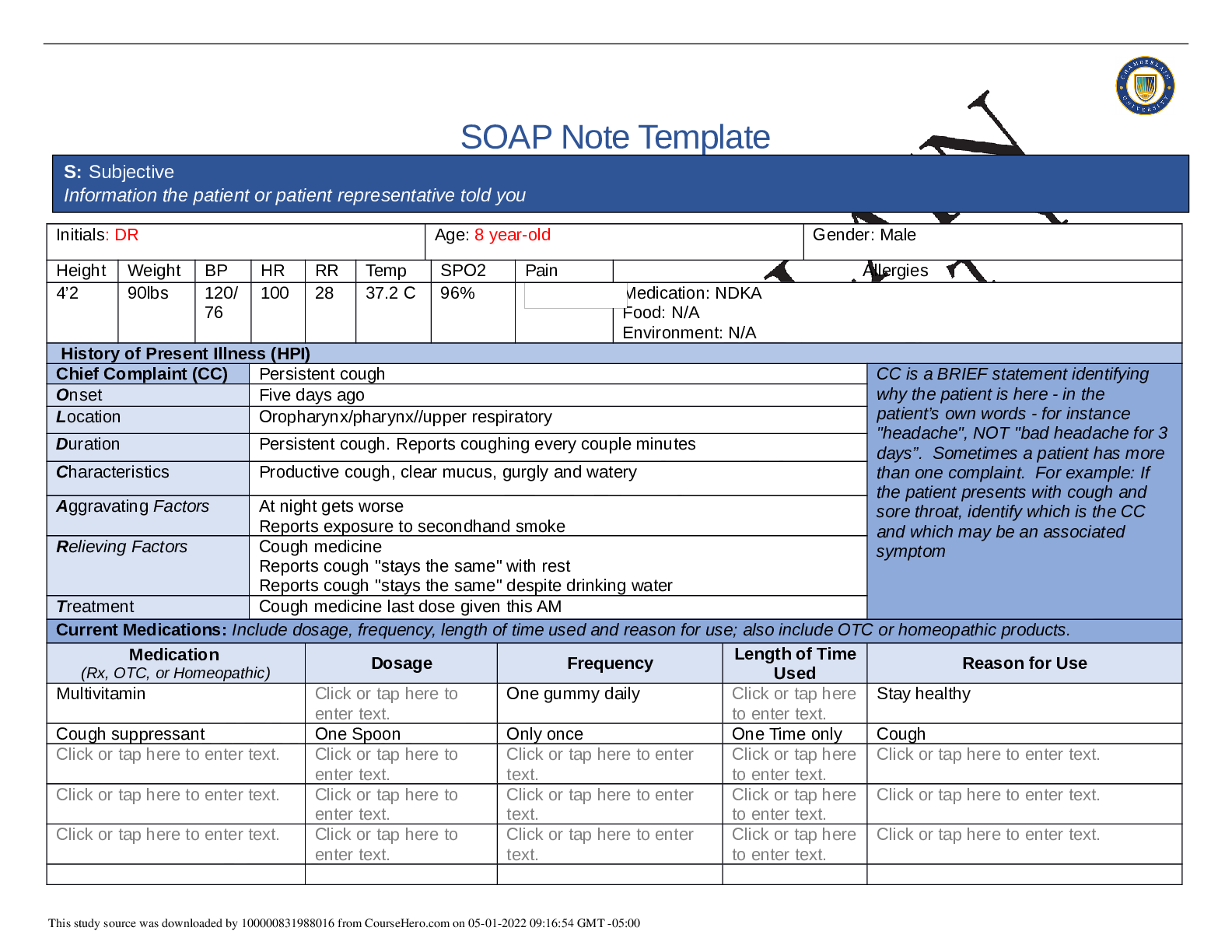
SOAP Note Template
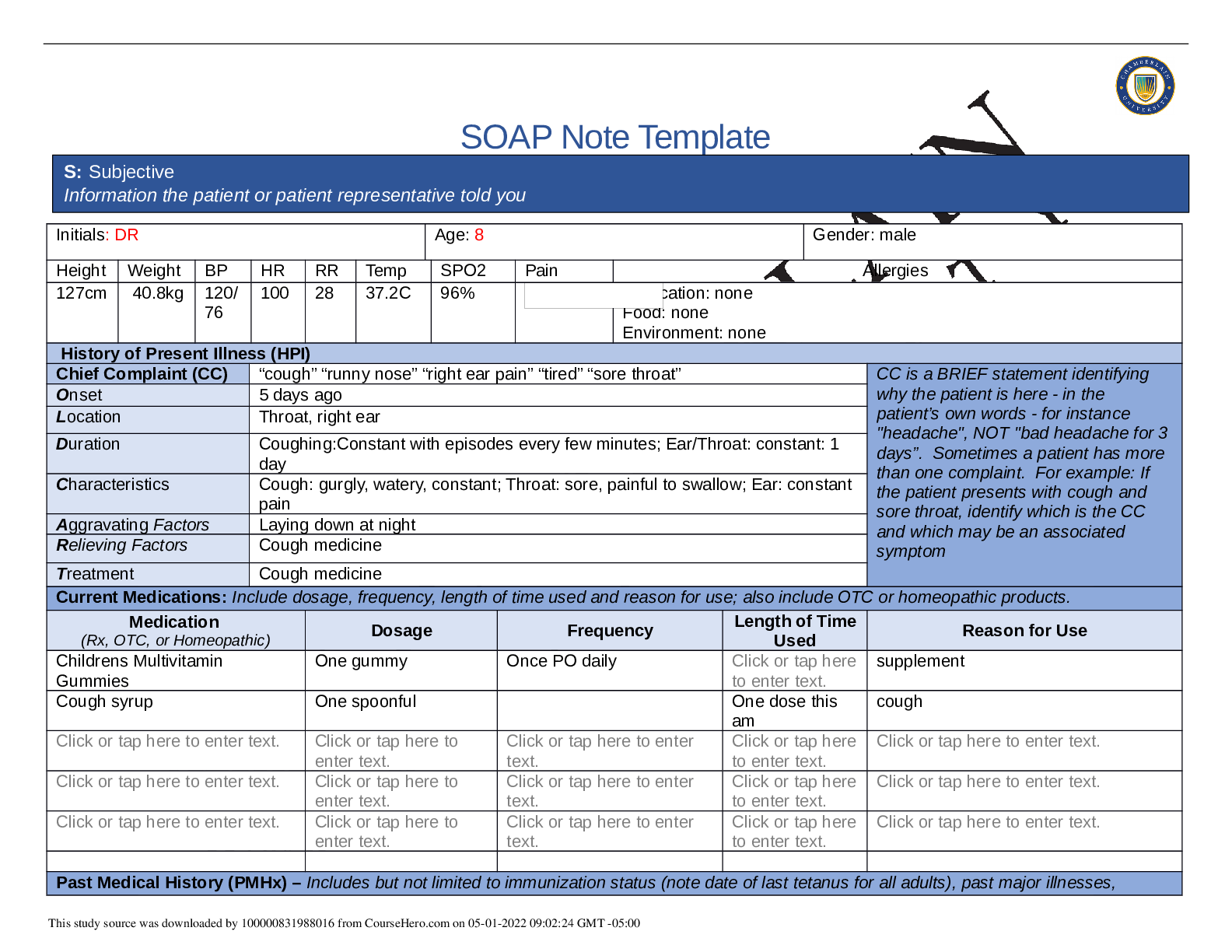
Initials: D.R. Age: 8 Gender: male
Height Weight BP HR RR Temp SPO2 Pain Allergies
4’2 90lbs
per
patient(
unable
to get a
standin
g
weight.
120/
76
100 28 37.2c 96% Medication: Denies
Food: Denies
Environment: Denies
History of Present Illness (HPI)
Chief Complaint (CC) Cough CC is a BRIEF statement identifying
why the patient is here - in the
patient’s own words - for instance
"headache", NOT "bad headache for 3
days”. Sometimes a patient has more
than one complaint. For example: If
the patient presents with cough and
sore throat, identify which is the CC
and which may be an associated
symptom
Onset Cough started 5 days ago
Location throat
Duration Coughing every few minutes lasting 1-2min , for the past five days.
Characteristics Productive cough rated a 5 out of 10 with clear and thin sputum, cough
worsens at night. Associated symptoms of sore throat and earache,(gargly and
watery associated with sore throat)
Aggravating Factors Worse at night. Reports cough stays the same no matter what I do. (cough at
night think CHF, GERD, Asthma...)
Relieving Factors Cough medicine “helped a little”
Treatment resting
Current Medications: Include dosage, frequency, length of time used and reason for use; also include OTC or homeopathic products.
Medication
(Rx, OTC, or Homeopathic) Dosage Frequency Length of Time
Used Reason for Use
Gummy multivitamin 2-4 gummies daily Unable to
answer my
question when
asked.
“to stay healthy”
Cough medicine “ a spoonful” One time “Once this AM” Cough
N/A Click or tap here to Click or tap here to enter Click or tap here Click or tap here to enter text.
S: Subjective
Information the patient or patient representative told you
enter text. text. to enter text.
N/A Click or tap here to
enter text.
Click or tap here to enter
text.
Click or tap here
to enter text.
Click or tap here to enter text.
N/A Click or tap here to
enter text.
Click or tap here to enter
text.
Click or tap here
to enter text.
Click or tap here to enter text.
Past Medical History (PMHx) – Includes but not limited to immunization status (note date of last tetanus for all adults), past major illnesses,
hospitalizations, and surgeries. Depending on the CC, more info may be needed.
-Reports frequent colds and Rhinorrhea. Reports no fever last few times mother checked temperature. Hx of frequent earaches at 2 yrs old.
-Pneumonia last year at 7 years old, missed school for 2 weeks, treated at an urgent care with unknown antibiotics (can’t recall the name).
-Hearing checked 1 month ago at school: reports it was normal.
-Last dental visit 2 months ago: reports no cavities.
-Denies any previous surgeries. Stated has tonsils still and no ear surgeries. Denies prior hospitalizations.
According to patient chart immunizations up to date at this time. No influenza vaccine, last 12 months.
Social History (Soc Hx) - Includes but not limited to occupation and major hobbies, family status, tobacco and alcohol use, and any other pertinent
data. Include health promotion such as use seat belts all the time or working smoke detectors in the house.
Student: 3
rd grader. Only child.Exposed to second hand smoke by father who smokes inside the house sometimes.
Lives with Abeula (maternal grandmother), mother,Papi (father), and Abuelo (grandfather). Mother is a stenographer. Father is a security officer for
court. States: “ I always feel safe at home. I have a good family!”. No pets in household. Reports drinks 7-8 glasses of water/ day. Goes to gym
class everyday at school for exercise and plays at the park after school or sometimes on weekends. Hobbies: play video games, read, try to write
stories with best friend Tony. Denies using tobacco or alcohol use.
Family History (Fam Hx) - Includes but not limited to illnesses with possible genetic predisposition, contagious or chronic illnesses. Reason for
death of any deceased first degree relatives should be included. Include parents, grandparents, siblings, and children. Include grandchildren if
pertinent.
Lives with grandparents and parents.
Mother: DM2, HTN,hypercholesterolemia, obesity.
Father: Current Smoker (couple of times a week, smokes inside) history of childhood asthma. HTN , hypercholesterolemia.
Maternal Grandma:DM type 2, HTN
Maternal Grandpa: doesn’t see a doctor
Paternal grandma: died in a car accident (52yrs. Old)
Paternal grandpa: unknown (estranged)
Review of Systems (ROS): Address all body systems that may help rule in or out a differential diagnosis Check the box next to each positive
symptom and provide additional details.
nstitutional Skin HEENT
☒Fatigue “ tired, because
my cough keeps me up at
night”
☐Weakness denies
☐Fever/Chills denies
☐Weight Gain denies
☐Weight Loss denies
☒Trouble Sleeping “cough
has made it hard to fall
asleep”
☐Night Sweats denies
☐Other:
Click or tap here to enter
text.
☐Itching denies
☐Rashes denies
☐Nail Changes denies
☐Skin Color Changes
d
☒Other:
Has dry skin on legs.
THINK 3 A’s
Allergy,asthma,atopic
dermatitis.
☐Diplopia denies
☐Eye Pain denies
☐Eye redness denies
☐Vision changes denies
☐Photophobia denies
☐Eye discharge denies
☒Earache Right ear pain
started 1 day ago.
☐Tinnitus denies
☐Epistaxis denies
☐Vertigo denies
☐Hearing Changes denies
☐Hoarseness denies
☐Oral Ulcers denies
☒Sore Throat started 2 out of
10 pain, cobblestoning and
erythema.
☐Congestion denies
☒Rhinorrhea reports always a
little runny but the clear runny
nose worse the last 5 days.
☒Other:
Right ear canal erythema,
tympanic membrane- pearly
gray, intact, no bulge.
Respiratory Neuro Cardiovascular
☒Cough reports productive cough,
started 5days ago
☐Hemoptysis denies
☐Dyspnea denies
☐Wheezing denies
☐Pain on Inspiration denies
☐Sputum Production
☐Other: clear thin sputum
☐Syncope or
Lightheadedness denies
☐Headache denies
☐Numbness denies
☐Tingling Click or tap denies
here to enter text.
☐Sensation Changes
☐Speech Deficits denies
☐Other: Click or tap here to
enter text.
☐Chest pain denies
☐SOB denies
☐Exercise Intolerance denies
☐Orthopnea denies
☐Edema denies
☐Murmurs denies
☐Palpitations denies
☐Faintness denies
☐OC Changes denies
☐Claudications denies
☐PND denies
☐Other: Click or tap here to
enter text.
MSK GI GU PSYCH
☐Pain denies
☐Stiffness denies
☐Crepitus unable to assess
☐Swelling denies
☐Nausea/Vomiting denies
☒Dysphasia states swallows okay but
throat is sore.
☐Diarrhea denies
☐Urgency denies
☐Dysuria denies
☐Burning denies
☐Hematuria denies
☐Stress denies
☐Anxiety denies
☐Depression denies
[Show More]