SOAP Note Template
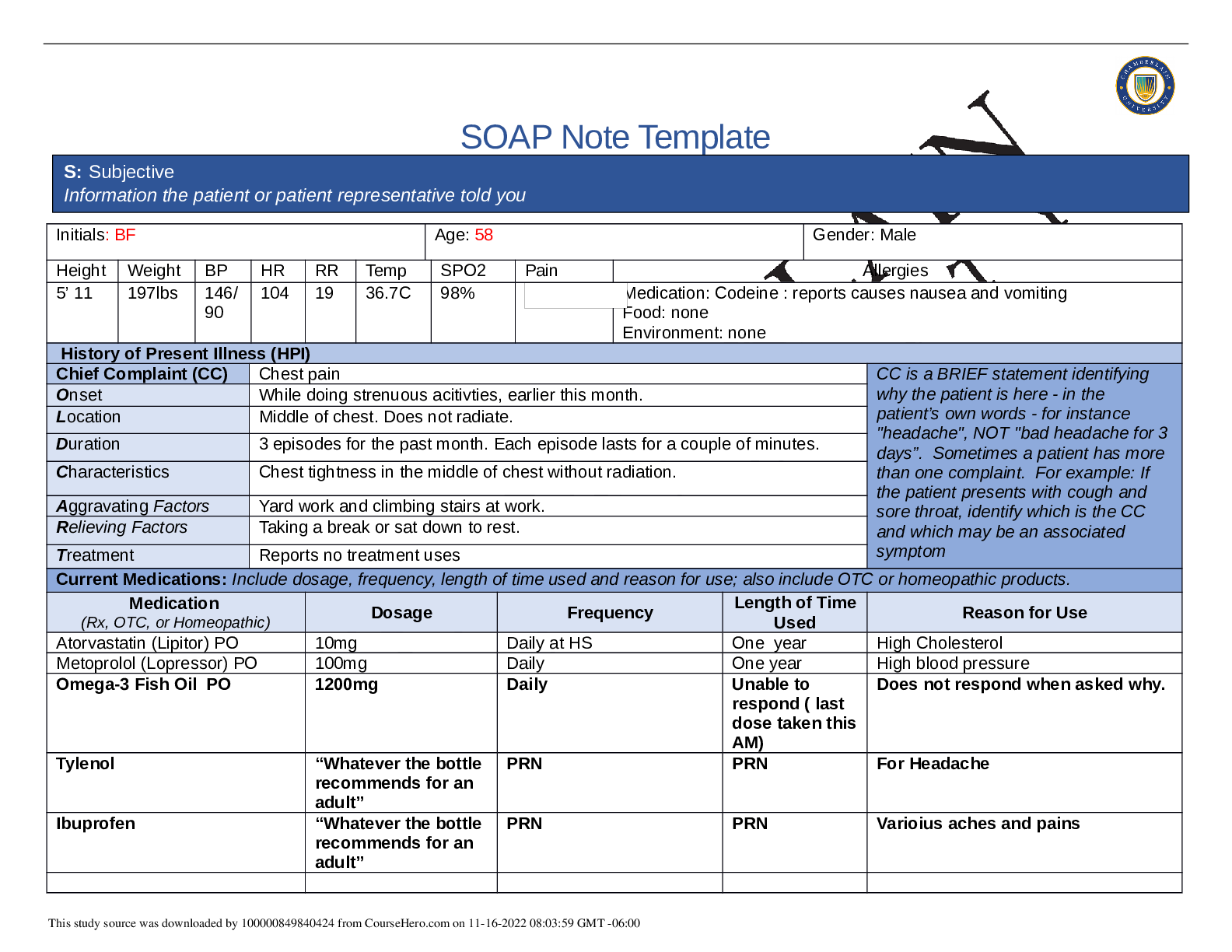
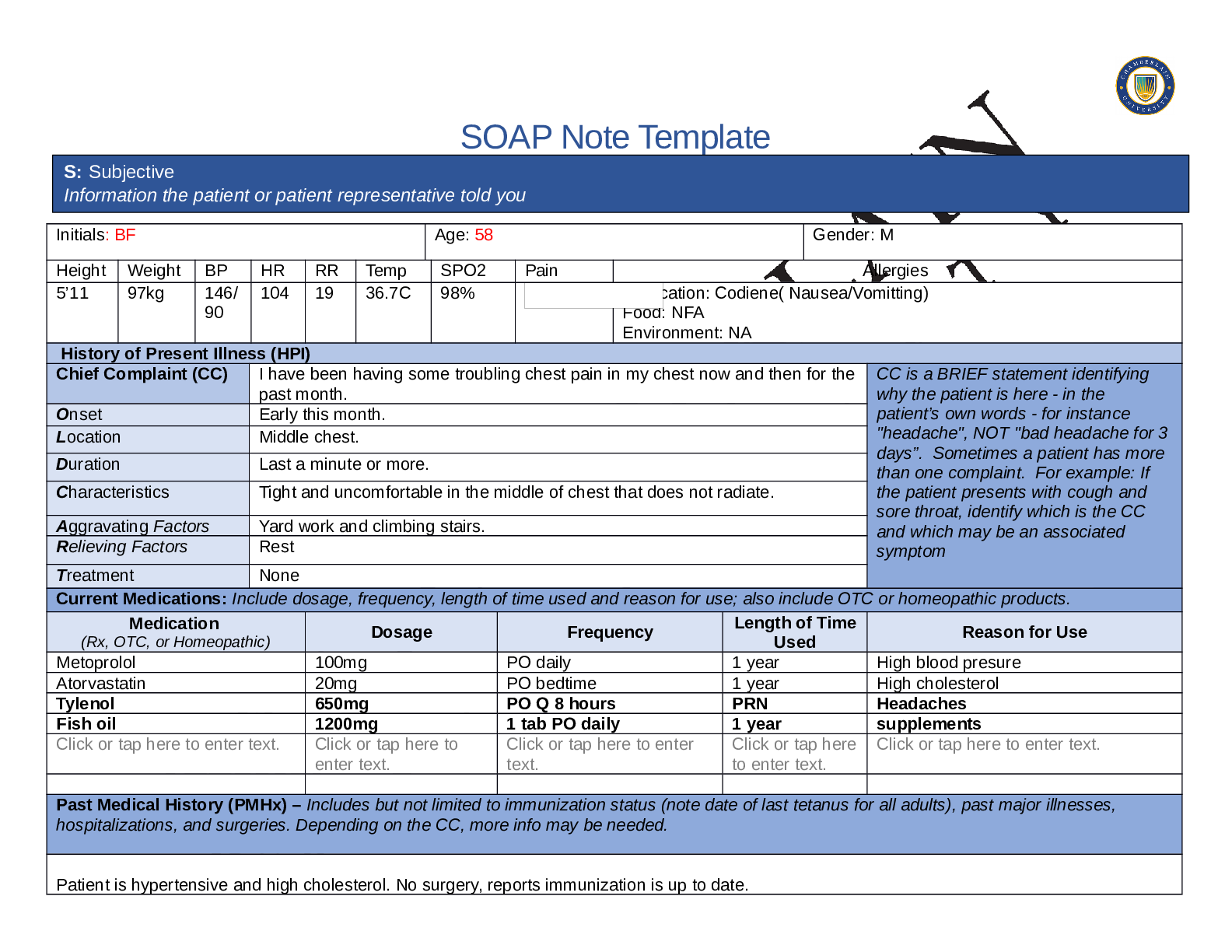
Initials: BF Age: 58 Gender: Male
Height Weight BP HR RR Temp SPO2 Pain Allergies
5’ 11 197lbs 146/
90
104 19 36.7C 98% Medication: Codeine : reports causes nausea and vomiting
Food: none
Enviro
...
SOAP Note Template
Initials: BF Age: 58 Gender: Male
Height Weight BP HR RR Temp SPO2 Pain Allergies
5’ 11 197lbs 146/
90
104 19 36.7C 98% Medication: Codeine : reports causes nausea and vomiting
Food: none
Environment: none
History of Present Illness (HPI)
Chief Complaint (CC) Chest pain CC is a BRIEF statement identifying
why the patient is here - in the
patient’s own words - for instance
"headache", NOT "bad headache for 3
days”. Sometimes a patient has more
than one complaint. For example: If
the patient presents with cough and
sore throat, identify which is the CC
and which may be an associated
symptom
Onset While doing strenuous acitivties, earlier this month.
Location Middle of chest. Does not radiate.
Duration 3 episodes for the past month. Each episode lasts for a couple of minutes.
Characteristics Chest tightness in the middle of chest without radiation.
Aggravating Factors Yard work and climbing stairs at work.
Relieving Factors Taking a break or sat down to rest.
Treatment Reports no treatment uses
Current Medications: Include dosage, frequency, length of time used and reason for use; also include OTC or homeopathic products.
Medication
(Rx, OTC, or Homeopathic) Dosage Frequency Length of Time
Used Reason for Use
Atorvastatin (Lipitor) PO 10mg Daily at HS One year High Cholesterol
Metoprolol (Lopressor) PO 100mg Daily One year High blood pressure
Omega-3 Fish Oil PO 1200mg Daily Unable to
respond ( last
dose taken this
AM)
Does not respond when asked why.
Tylenol “Whatever the bottle
recommends for an
adult”
PRN PRN For Headache
Ibuprofen “Whatever the bottle
recommends for an
adult”
PRN PRN Varioius aches and pains
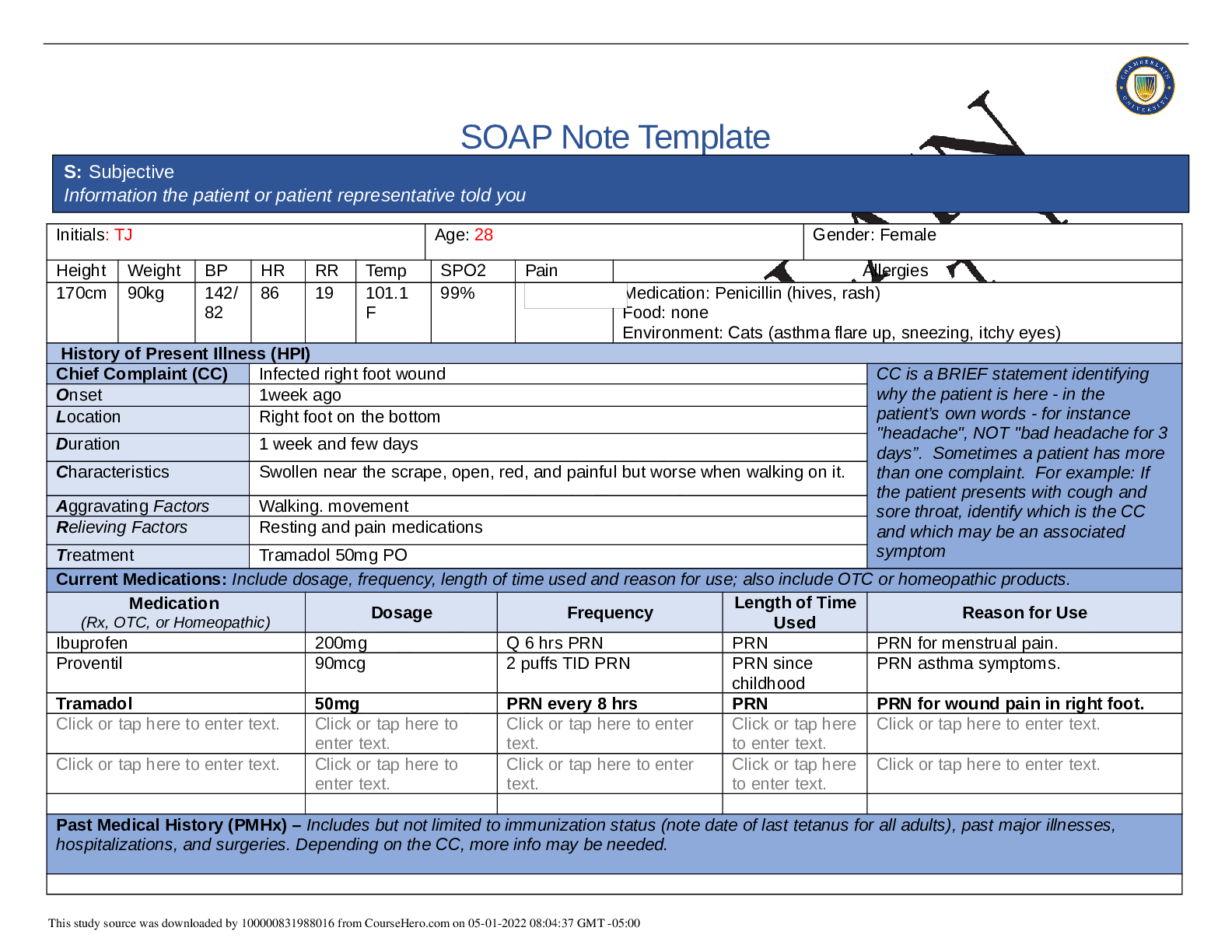
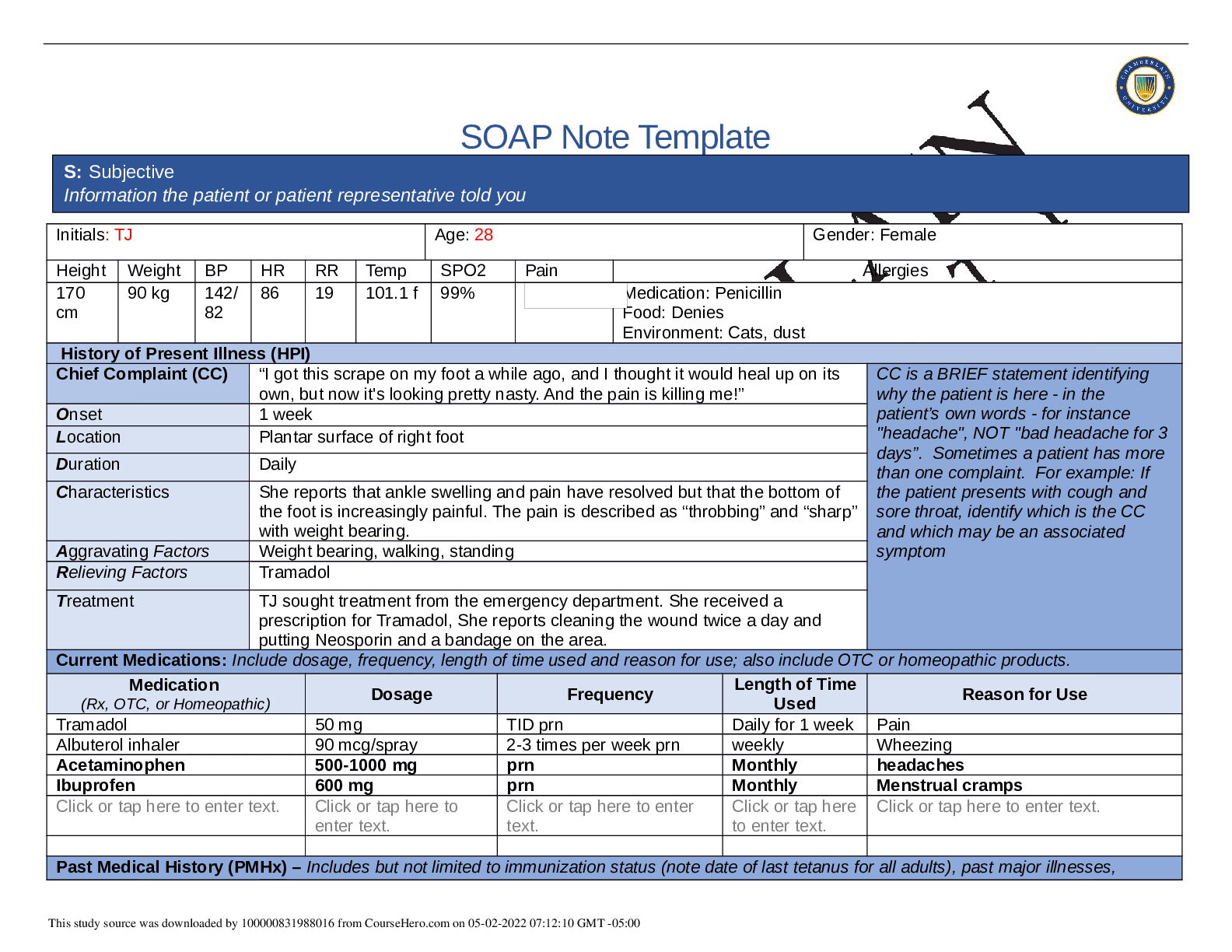
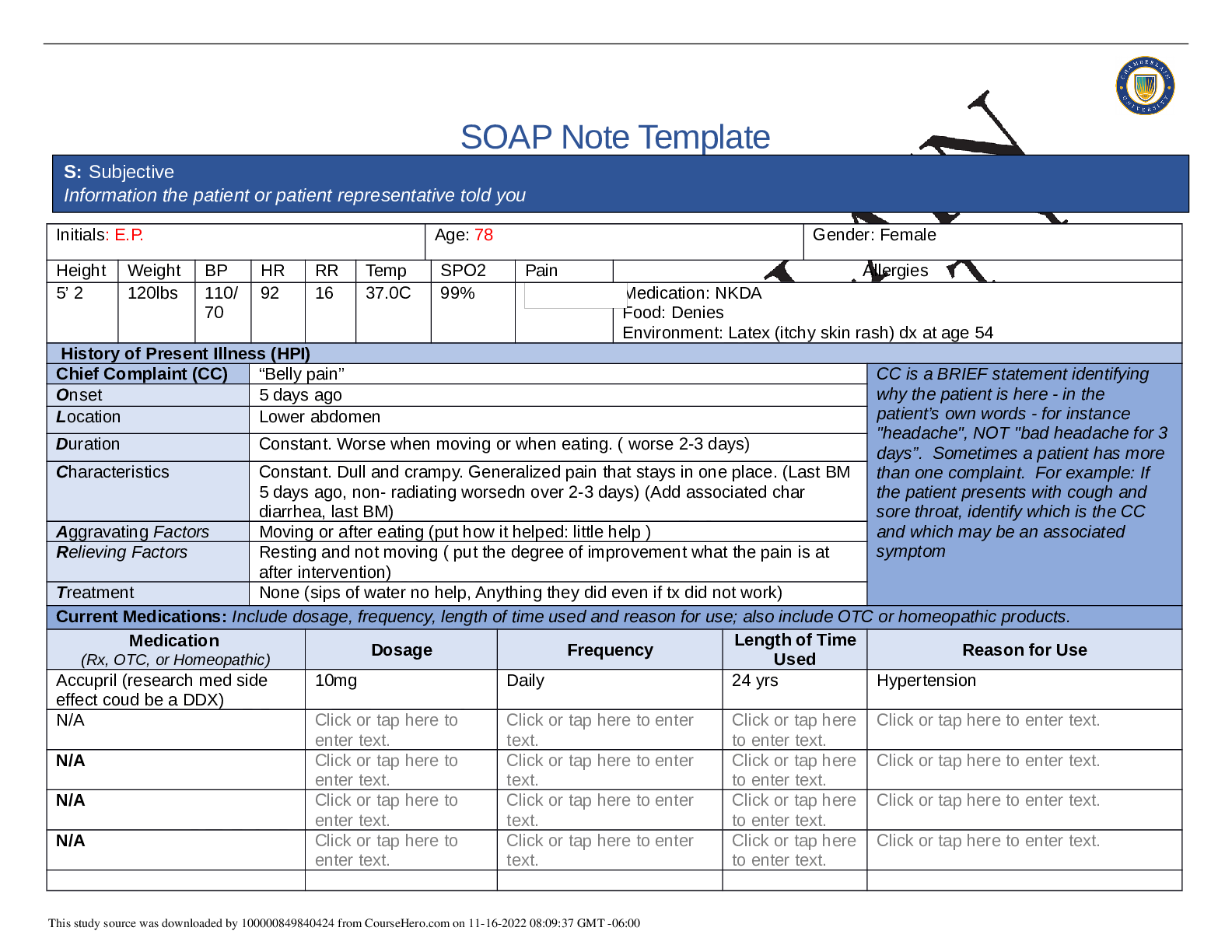
S: Subjective
Information the patient or patient representative told you
This study source was downloaded by 100000831988016 from CourseHero.com on 05-01-2022 08:54:36 GMT -05:00
Past Medical History (PMHx) – Includes but not limited to immunization status (note date of last tetanus for all adults), past major illnesses,
hospitalizations, and surgeries. Depending on the CC, more info may be needed.
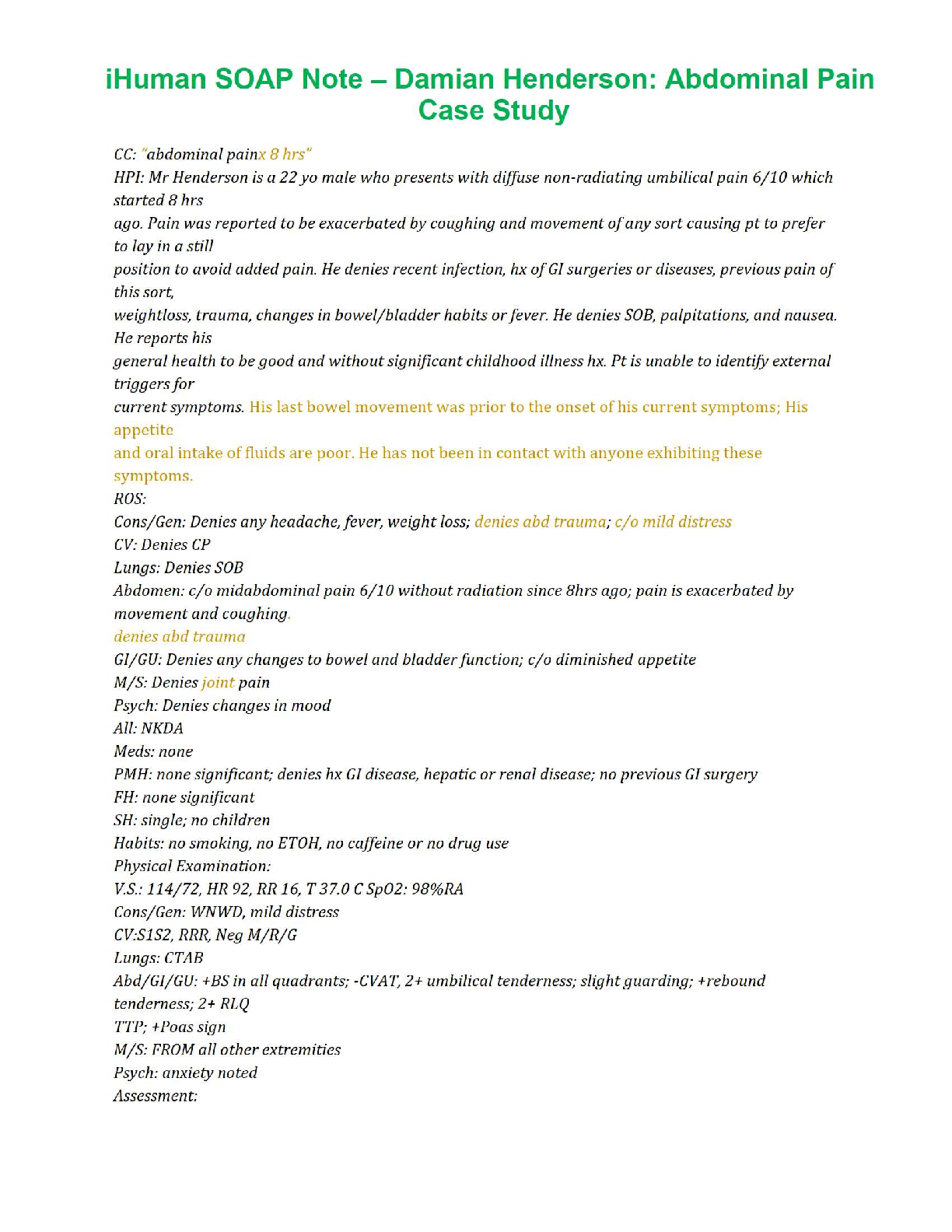
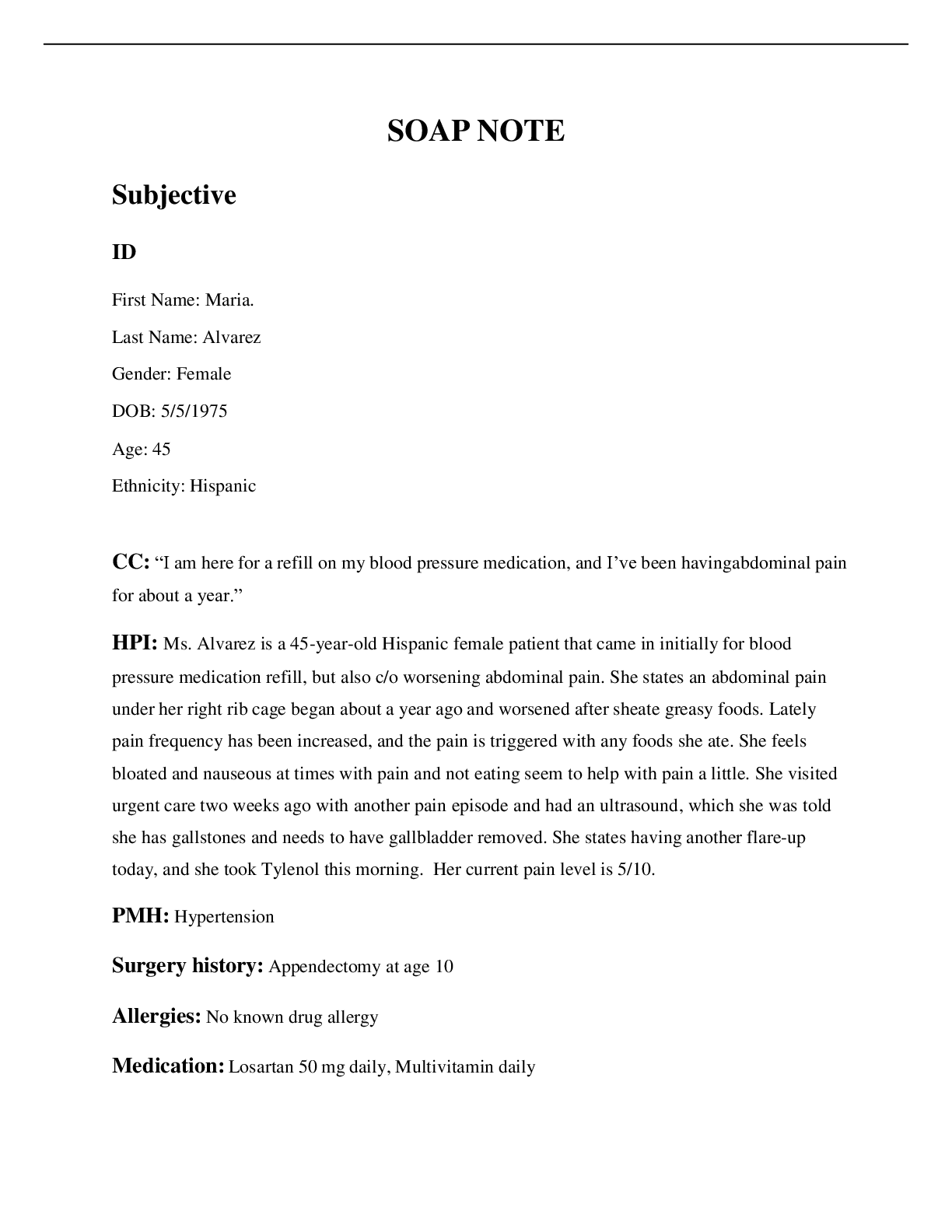
3 episodes of 5/10 chest pain with physical activity, that resolved with rest after 2 min. Reports no shortness of breath. History of hypertension and
hyperlipidemia. Reports Stress test 4 mo ago: normal. EKG: NSR with no ST changes. Last annual exam by PCP: 3 months ago. Reports never
hospitalized. Reports no surgical history. Threw out back few years ago and took codeine, but reports allergy to codeine. Unable to recall last
Pneumovax vaccine. Tdap: last on 10/2014. Influenza : received this flu season. Regular caffeine intake 1-2 cups daily.
Social History (Soc Hx) - Includes but not limited to occupation and major hobbies, family status, tobacco and alcohol use, and any other pertinent
data. Include health promotion such as use seat belts all the time or working smoke detectors in the house.
Patient is married, lives with wife and daughter. Son lives in town. Patient is a
Civil Engineer (denies working out in the field) Goes over work proposals. Denies chemical exposure. Hobbies include: fishing, sports, going to see
son’s body building competitions. Family dynamic is great. Low stress. Denies cigarette smoking.Denies tobacco use. Denies current illicit drug
use. Reports history of cocaine use 30 yrs ago. Reports drinking 1-2 cups coffee daily. Reports 2-3 alcohol drinks per weekend (typically drinks 2-
3beers in one sitting). Denies hx or current suicidal ideation. Denies Depression. Denies regular exercise.
Family History (Fam Hx) - Includes but not limited to illnesses with possible genetic predisposition, contagious or chronic illnesses. Reason for
death of any deceased first degree relatives should be included. Include parents, grandparents, siblings, and children. Include grandchildren if
pertinent.
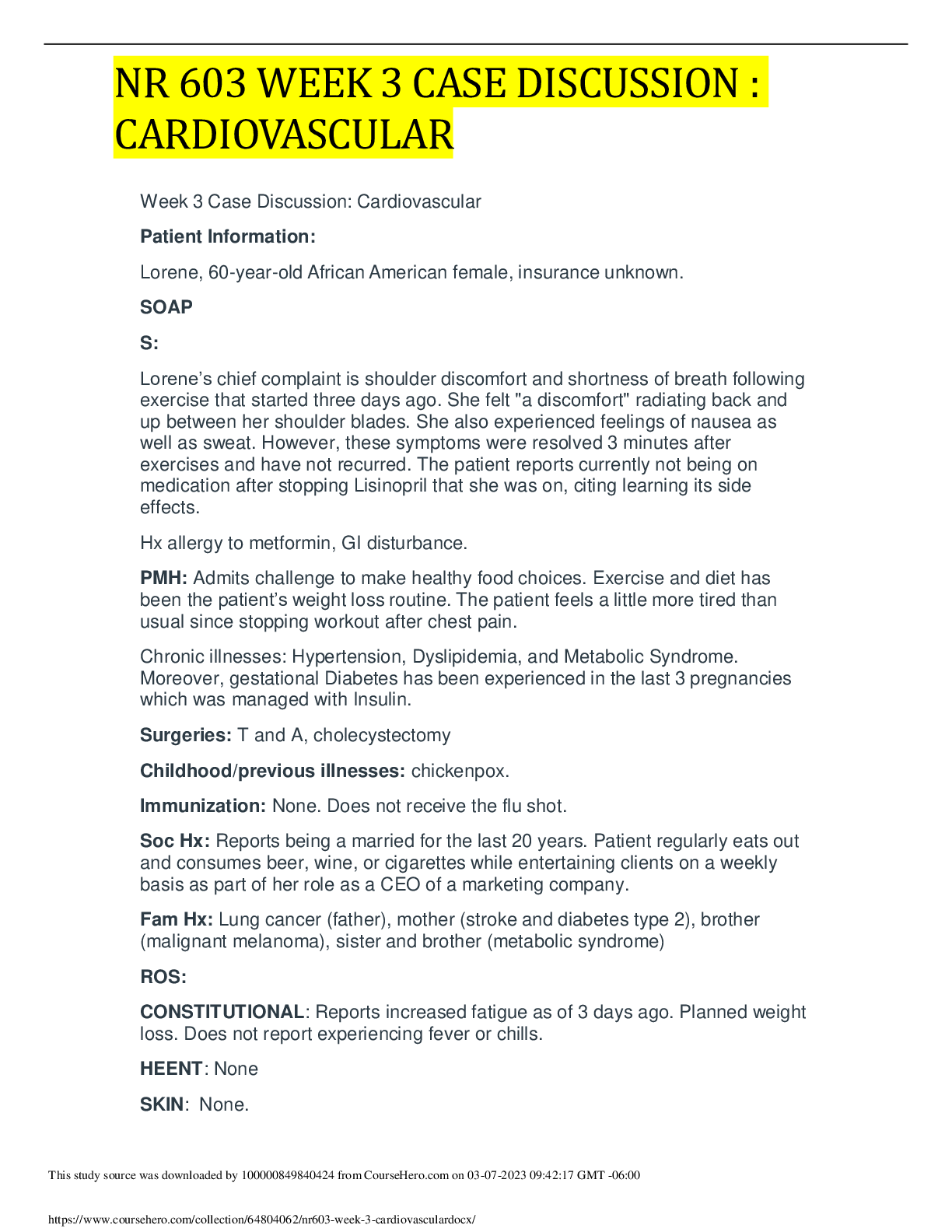
Mother 80 y.o.(living)- Type 2 Diabetes and hypertension
Father-Deceased at 75y.o. from colon cancer. Hx obesity, hypertention, and hyperlipidemia
Spouse (Maria) 51 y.o. : Denies illnesses
Son (Sam) 26y.o. : reports is healthy, is a competitive body builder
Daughter(Allie) 19y.o. : Asthma
Sister: 52 y.o.living- Type 2 Diabetes and hypertention
Brother: deceased at 24y.o. from a car accident.
Paternal grandpa- died at 85y.o. unknown
Paternal grandma- died at 78 y.o from pneumonia.
Maternal grandpa- died at 54 from a heart attack.
Maternal grandma- died at 65 from breast cancer.
Review of Systems (ROS): Address all body systems that may help rule in or out a differential diagnosis Check the box next to each positive
symptom and provide additional details.
Constitutional Skin HEENT
This study source was downloaded by 100000831988016 from CourseHero.com on 05-01-2022 08:54:36 GMT -05:00
☐Fatigue Denies
☐Weakness Denies
☐Fever/Chills Denies
☒Weight Gain reports 15-
20 lbs last 2 years.
☐Weight Loss Denies
☐Trouble Sleeping Denies
☐Night Sweats Denies
☐Other:
Click or tap here to enter
text.
☐Itching Denies
☐Rashes Denies
☐Nail Changes Denies
☐Skin Color Changes
Denies
☐Other:
Click or tap here to
enter text.
☐Diplopia Denies
☐Eye Pain Denies
☐Eye redness Denies
☐Vision changes Denies
☐Photophobia Denies
☐Eye discharge Denies
☐Earache Denies
☐Tinnitus Denies
☐Epistaxis Denies
☐Vertigo Denies
☐Hearing Changes Denies
☐Hoarseness Denies
☐Oral Ulcers Denies
☐Sore Throat Denies
☐Congestion Denies
☐Rhinorrhea Denies
☐Other:
Click or tap here to enter text.
Respiratory Neuro Cardiovascular
☐Cough Denies
☐Hemoptysis Denies
☐Dyspnea Denies
☐Wheezing Denies
☐Pain on Inspiration Denies
☐Sputum Production
☒Other: Fine crackles in bilateral
posterior, lower lobes
☐Syncope or
Lightheadedness Denies
☐Headache Denies
☐Numbness Denies
☐Tingling Denies
☐Sensation Changes
☐Speech Deficits Denies
☐Other: Click or tap here to
enter text.
☒Chest pain 3 episodes the last month,
each episode last 1-2 minutes and
resides with rest.
☐SOB Denies
☒Exercise Intolerance Reports unable
to exercise because afraid of chest pain
occurring again
☐Orthopnea Denies
☐Edema Denies
☐Murmurs Denies
☐Palpitations Denies
☐Faintness Denies
☐OC Changes Denies
☐Claudications Denies
☐PND Denies
☐Other: Click or tap here to
enter text.
MSK GI GU PSYCH
☐Pain chest pain
☐Stiffness Denies
☐Crepitus not assessed
☐Swelling Denies
☐Limited ROM
☐Redness Denies
☐Misalignment not assessed
☐Other: Click or tap here to enter
☐Nausea/Vomiting Denies
☐Dysphasia Denies
☐Diarrhea Denies
☐Appetite Change Denies
☐Heartburn Denies
☐Blood in Stool Denies
☐Abdominal Pain Denies
☐Excessive Flatus Denies
☐Food Intolerance Denies
☐Urgency Denies
☐Dysuria Denies
☐Burning Denies
☐Hematuria Denies
☐Polyuria Denies
☐Nocturia Denies
☐Incontinence Denies
☐Other: Click or tap here to
enter text.
☒Stress low stress
☒Anxiety Little anxious about
the chest pain
☐Depression Denies
☐Suicidal/Homicidal Ideation
Denies
☐Memory Deficits Denies
☐Mood Changes Denies
☐Trouble Concentrating
This study source was downloaded by 100000831988016 from CourseHero.com on 05-01-2022 08:54:36 GMT -05:00
text. ☐Rectal Bleeding Denies
☐Other:
Click or tap here to enter text.
Denies
☐Other: Click or tap here to
enter text.
GYN
☐Rash N/A
☐Discharge N/A
☐Itching N/A
☐Irregular Menses N/A
☐Dysmenorrhea N/A
☐Foul Odor N/A
☐Amenorrhea N/A
☐LMP: N/A
☐Contraception N/A
☐Other:Click or tap here to enter text.
O: Objective
Information gathered during the physical examination by inspection, palpation, auscultation, and palpation. If unable to assess a body
system, write “Unable to assess”. Document pertinent positive and negative assessment findings.
This study source was downloaded by 100000831988016 from CourseHero.com on 05-01-2022 08:54:36 GMT -05:00
Body System Positive Findings Negative Findings
General
N/A Pleasant 51 year old male sitting on exam table with normal
stature. Alert and oriented x 4. Clear speech. No signs of current
distress. No signs of pain or shortness of breath at this time. Able
to follow commands and answer questions appropriately.
Skin
Inspected skin looks pale Inspected skin no scars, intact, no rash. Warm and dry. No
tenting. Fingernails and toe nails inspected no abnormal color.
HEENT
N/A Inspected face: No visible abnormal findings.
Respiratory
Adventitious breath sound: Fine crackles heard
[Show More]