SOAP NOTES TEMPLATE
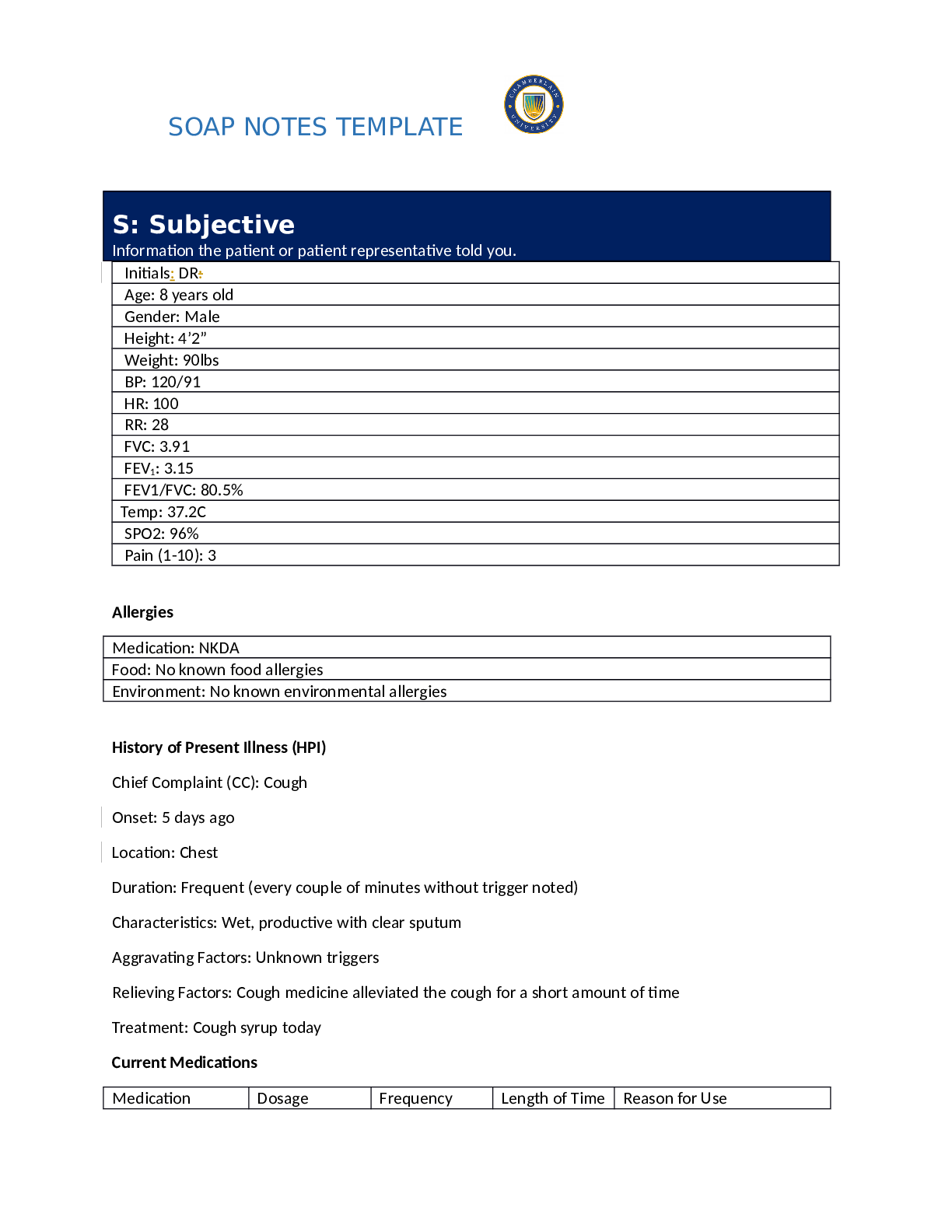
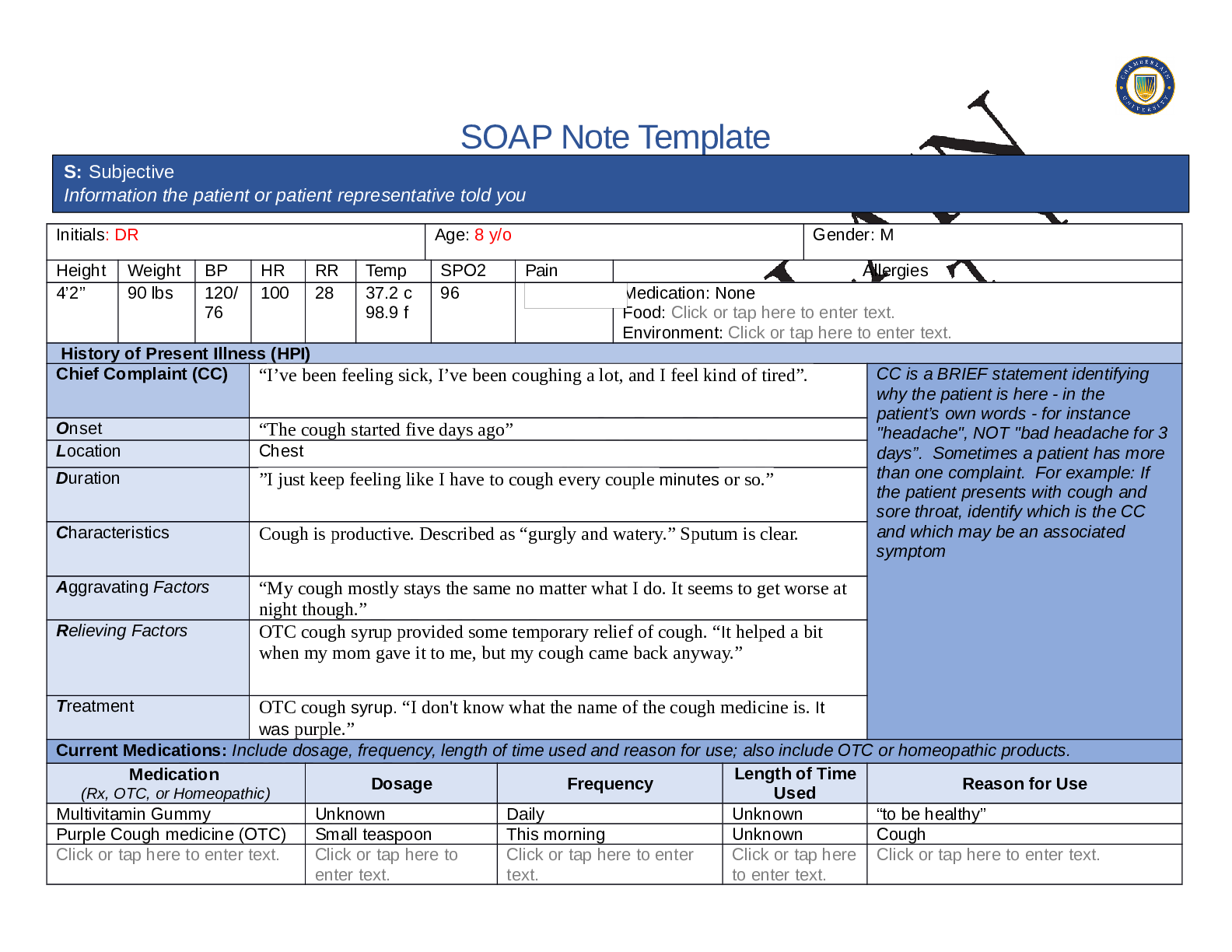
S: Subjective
Information the patient or patient representative told you.
Initials: DR:
Age: 8 years old
Gender: Male
Height: 4’2”
Weight: 90lbs
BP: 120/91
HR: 100
RR: 28
FVC: 3.91
...
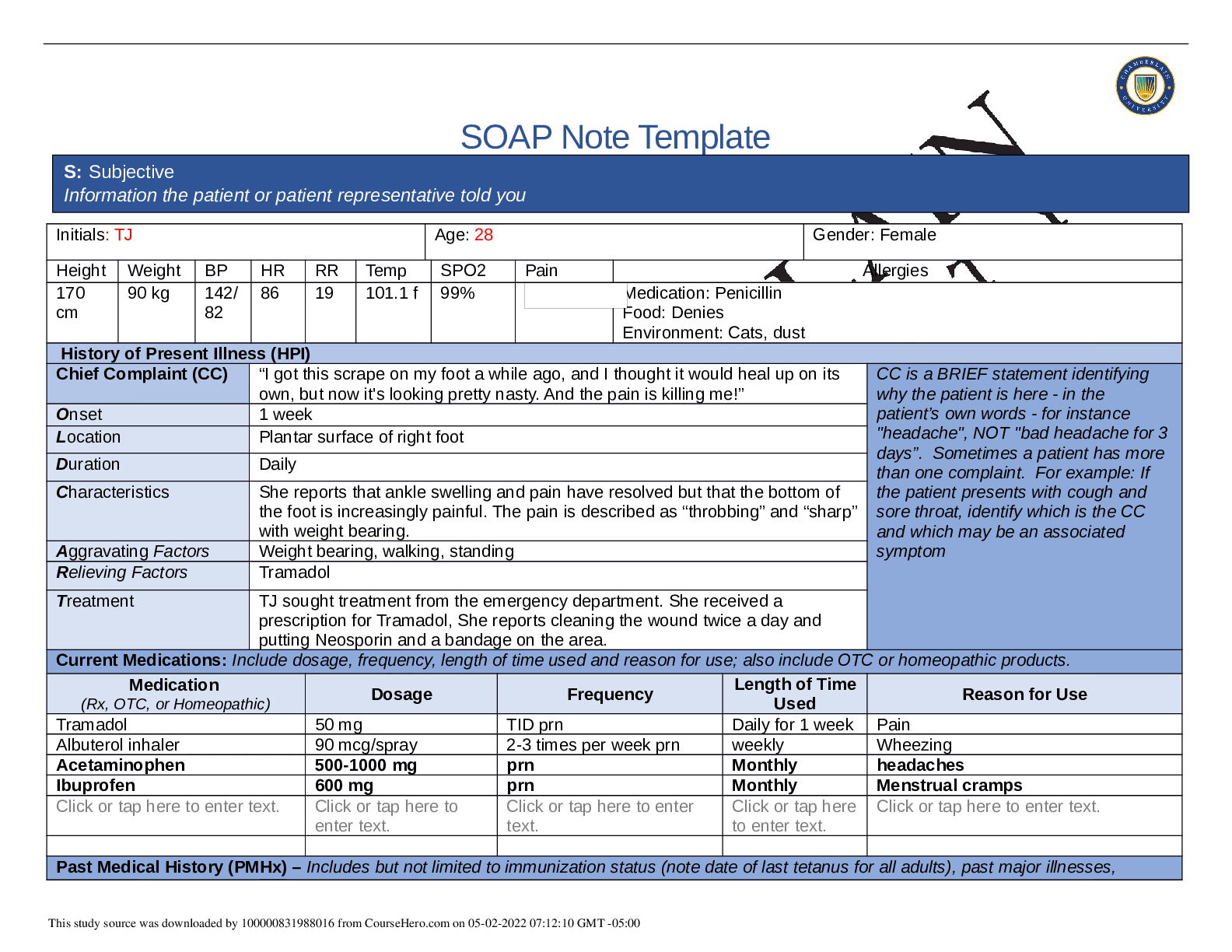
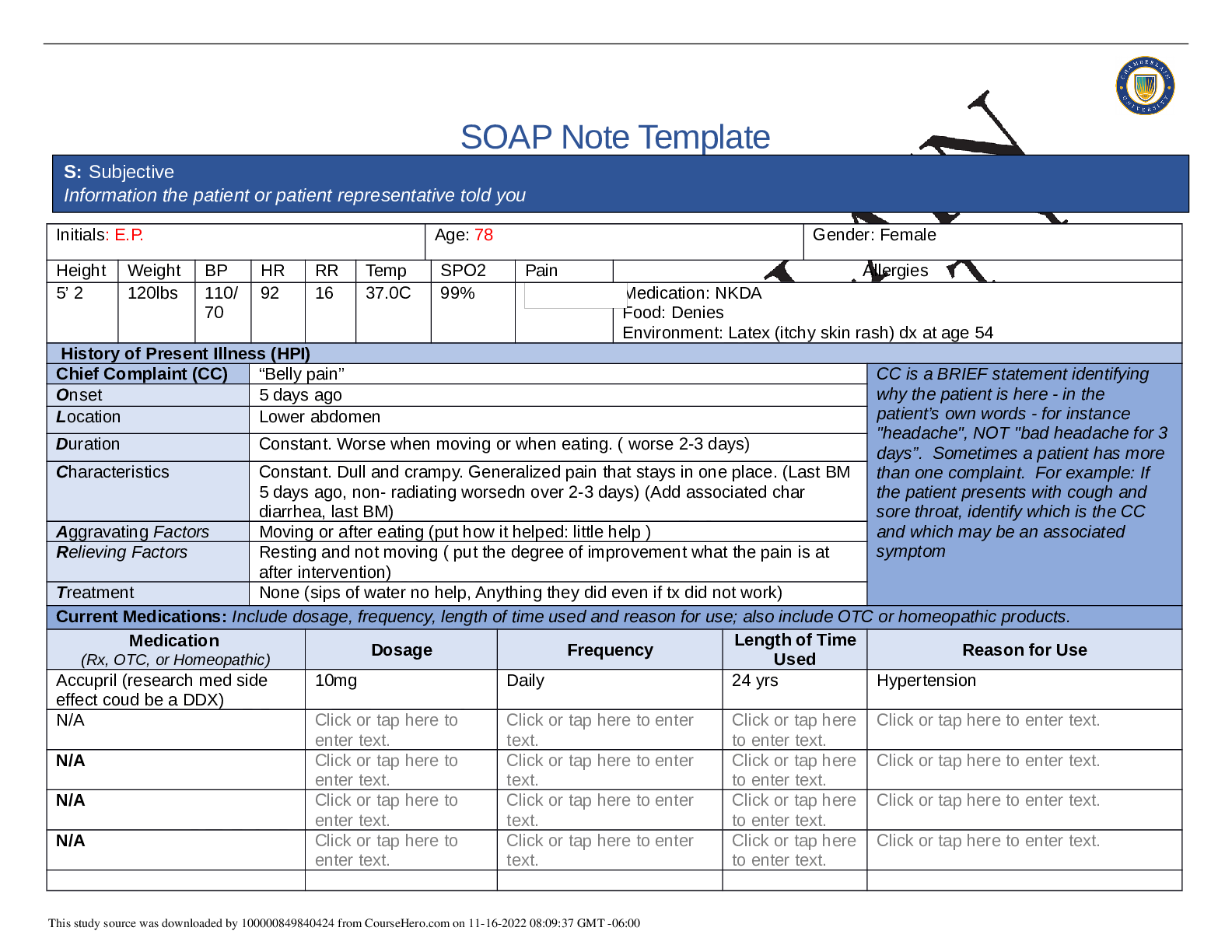
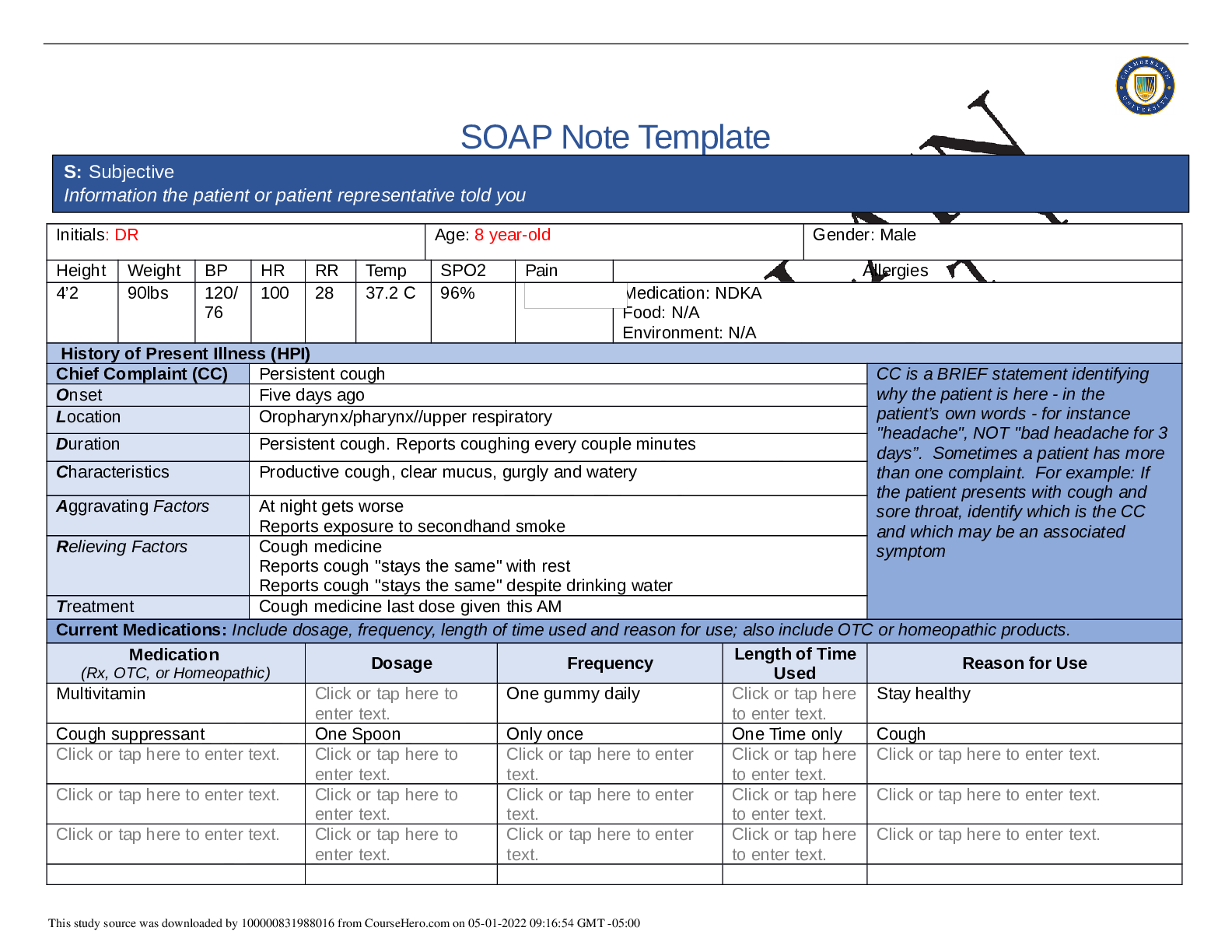
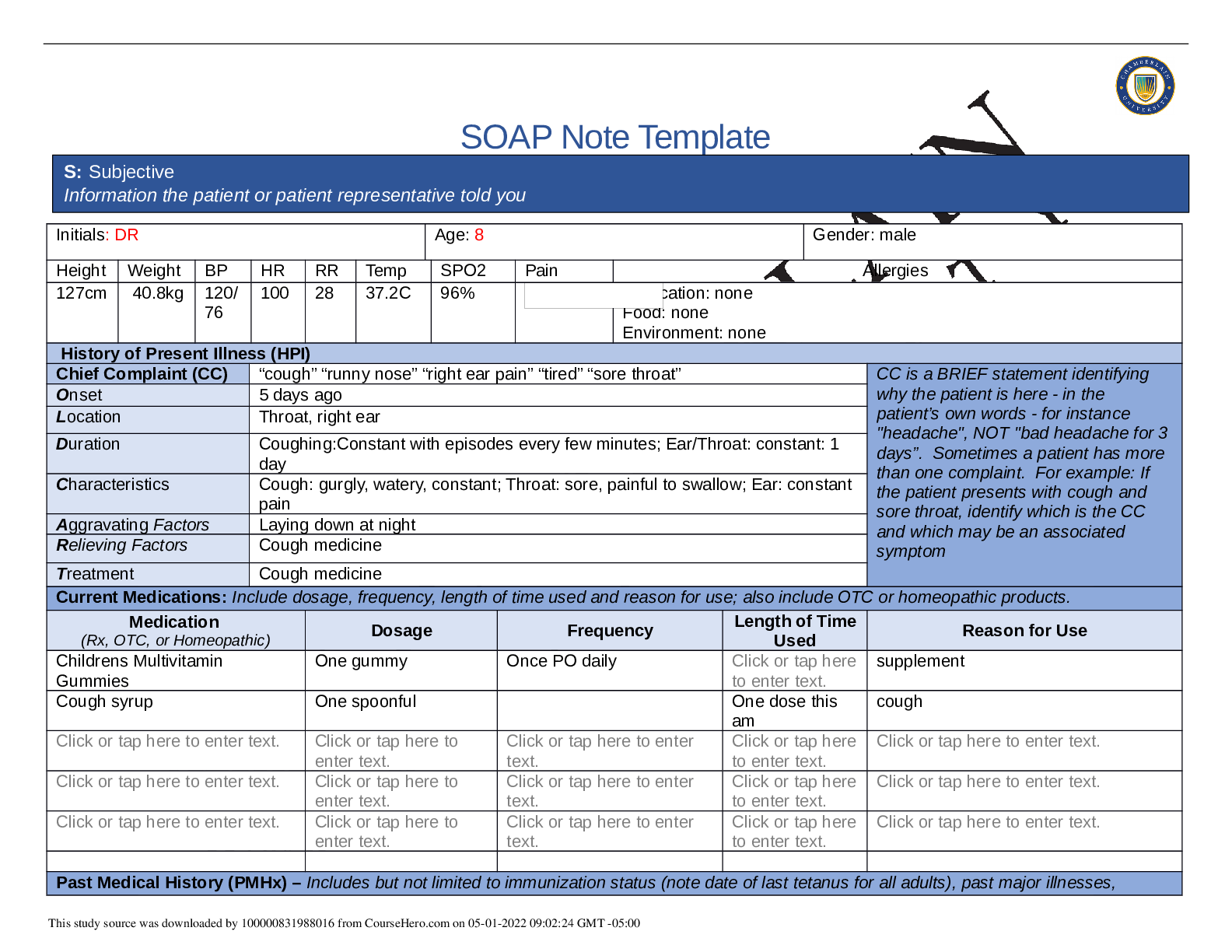
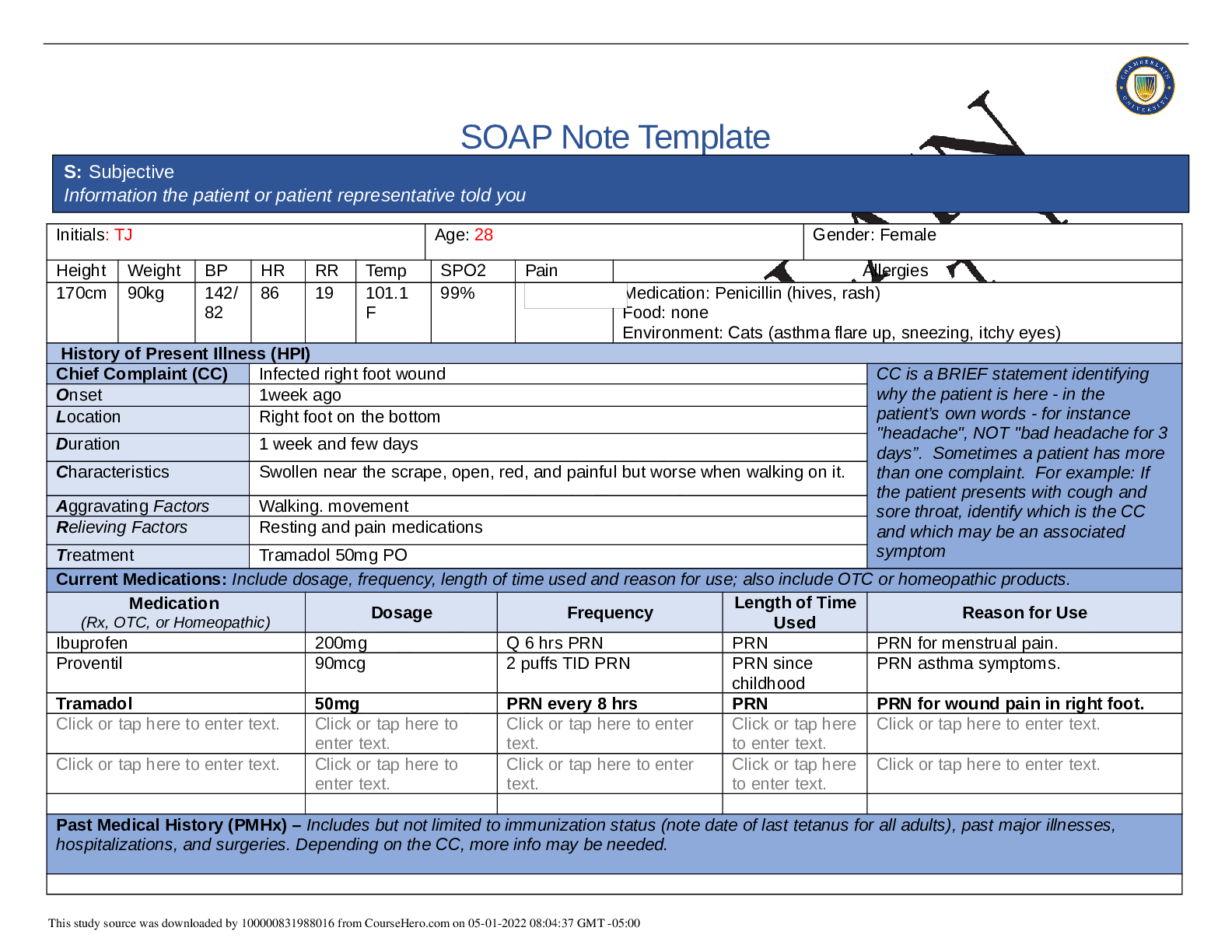
SOAP NOTES TEMPLATE
S: Subjective
Information the patient or patient representative told you.
Initials: DR:
Age: 8 years old
Gender: Male
Height: 4’2”
Weight: 90lbs
BP: 120/91
HR: 100
RR: 28
FVC: 3.91
FEV1: 3.15
FEV1/FVC: 80.5%
Temp: 37.2C
SPO2: 96%
Pain (1-10): 3
Allergies
Medication: NKDA
Food: No known food allergies
Environment: No known environmental allergies
History of Present Illness (HPI)
Chief Complaint (CC): Cough
Onset: 5 days ago
Location: Chest
Duration: Frequent (every couple of minutes without trigger noted)
Characteristics: Wet, productive with clear sputum
Aggravating Factors: Unknown triggers
Relieving Factors: Cough medicine alleviated the cough for a short amount of time
Treatment: Cough syrup today
Current Medications
Medication Dosage Frequency Length of Time Reason for Use
SOAP NOTES TEMPLATE
Used
Kids Multivitamin
Gummies
Recommended
dosing
Daily Unknown Health maintenance
Cough Syrup Recommended
dosing
PRN Unknown Cough treatment
Past Medical History (PMHx)—
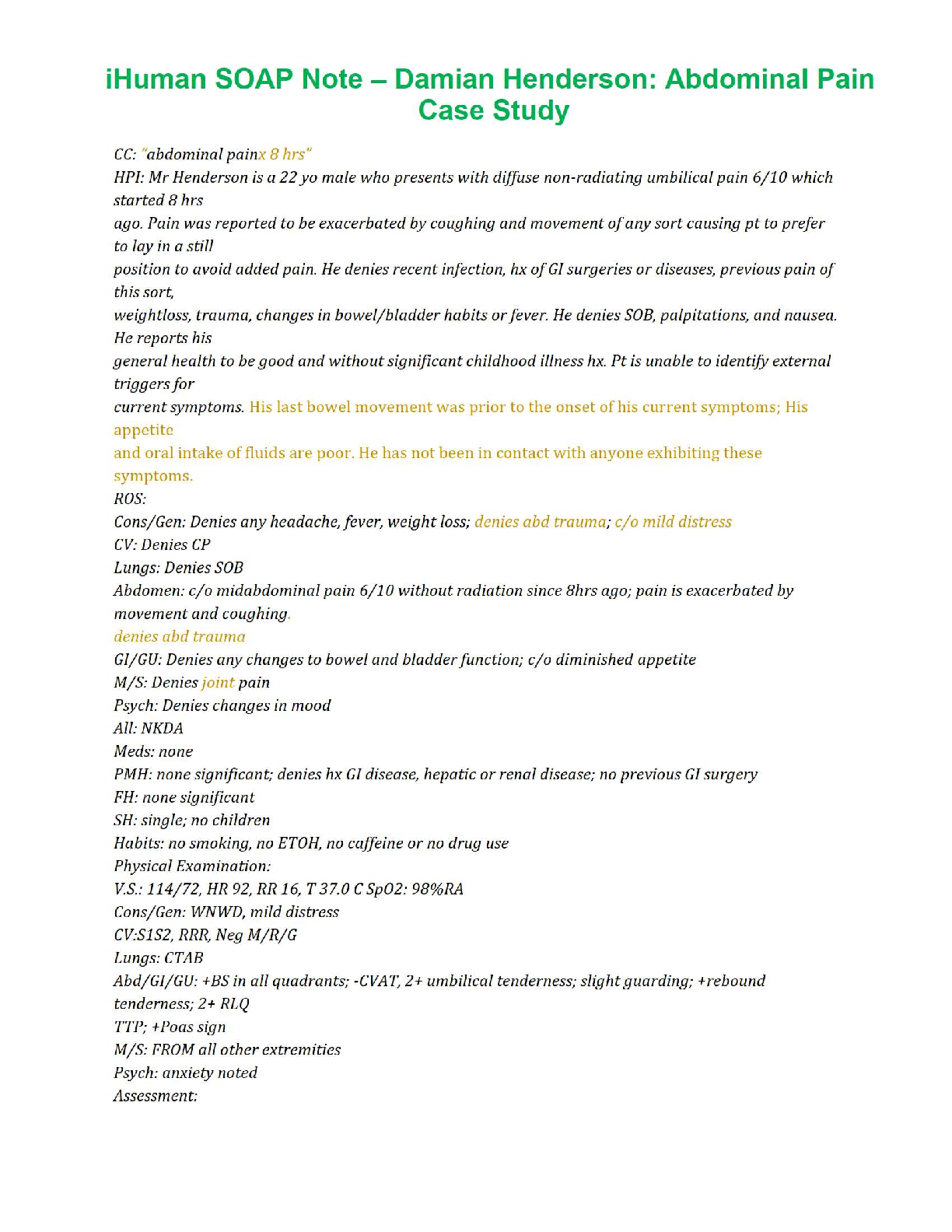
Danny is an 8-year-old male that denies any history of allergies to medications, foods, seasonal, latex or
environmental agents. He reports having frequent colds and being diagnosed with pneumonia last year.
He takes a daily dose of children’s multivitamin gummies as well as PRN doses of cough syrup to treat
episodes of coughing. He reports that his immunizations are up to date and denies any other history of
major illnesses (including asthma), hospitalizations, or surgeries.
Social History (Soc Hx)—
Danny is a 3rd grade student with a reported history of missing school for two weeks last year due to
pneumonia. He lives with his mother and father and is cared for by his grandmother while his parents
are working. English is the primary language spoken in the home with Spanish as an alternate language
utilized.
Family History (Fam Hx)—
Danny’s mother has type II diabetes, hypertension, hypercholesterolemia, spinal stenosis, and is obese
Danny’s father is a smoker (cigars), and has hypertension, hypercholesterolemia, as well as a childhood
history of asthma
Danny’s grandparent’s history:
Maternal—
Grandmother: type II diabetes and hypertension
Grandfather: Smoker and eczema
Paternal—
Grandmother: died in a car accident at 52 years of age
Grandfather: No known history
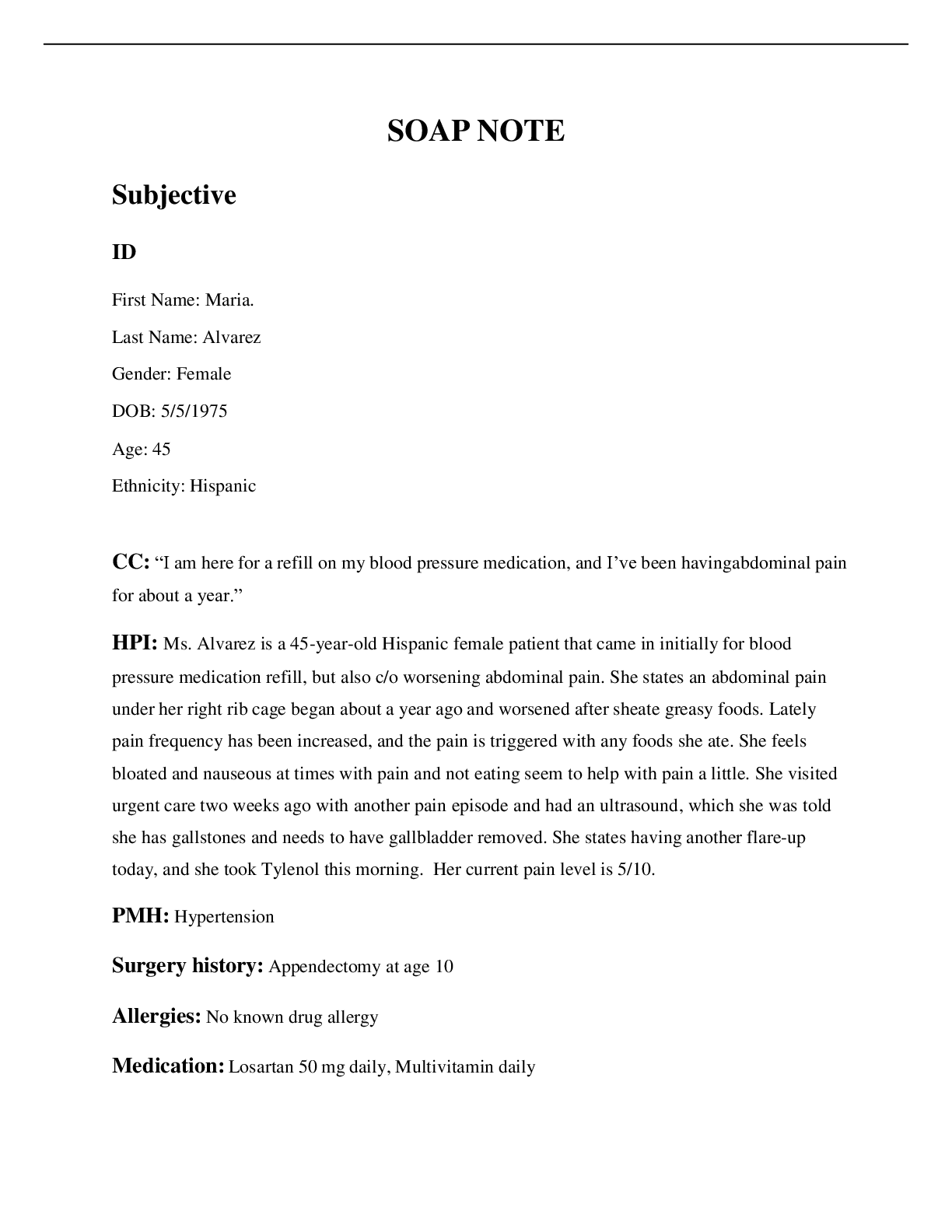
Review of Systems (ROS): Address all body systems that may help rule in or out a differential diagnosis
Constitutional
If patient denies all symptoms for this system, check here:
Check the box next to each reported symptom and provide additional details.
Check if Symptom Details
SOAP NOTES TEMPLATE
Positive
x Fatigue “kind of tired”
Weakness Denies
Fever/Chills Denies
Weight Changes Denies
Trouble Sleeping Denies
Night Sweats Denies
Other Denies
Skin
If patient denies all symptoms for this system, check here: Denies all symptoms
Check the box next to each reported symptom and provide additional details.
Check if
Positive
Symptom Details
Itching
Rashes
Nail
Skin Color
Other
HEENT
If patient denies all symptoms for this system, check here:
Check the box next to each reported symptom and provide additional details.
Check if
Positive
Symptom Details
Diplopia Denies
Eye Pain Denies
Eye redness Denies
Vision changes Denies
Photophobia Denies
Eye discharge Denies
Eye discharge Denies
x Earache x2days, right ear
Tinnitus Denies
Vertigo Denies
Hearing Changes Denies
Hoarseness Denies
x Sore Throat Reports “a little” pain and soreness
x Congestion “my cough seems kind of wet and gurgly”
x Rhinorrhea “my nose always runs a little, but it is worse since
the cough started”
SOAP NOTES TEMPLATE
Other Denies
Respiratory
If patient denies all symptoms for this system, check here:
Check the box next to each reported symptom and provide additional details.
Check if
Positive
Symptom Details
x Cough Frequent coughing without much relief from cough
syrup
Hemoptysis Denies
Dyspnea Denies
Dyspnea Denies
Pain on Inspiration Denies
Other Denies
Neuro patient denies all symptoms for this system, check here: Denies all symptoms
Check the box next to each reported symptom and provide additional details.
Check if
Positive
Symptom Details
Syncope or Lightheadedness
Headache
Numbness
Tingling
Sensation Changes RUE
LUE
RLE
LLE
Speech Deficits
Other
Cardiac and Peripheral Vascular
If patient denies all symptoms for this system, check here: Denies all symptoms
Check the box next to each reported symptom and provide additional details.
Check if
Positive
Symptom Details
Chest pain
SOB
Exercise Intolerance
SOAP NOTES TEMPLATE
Orthopnea
Edema
Murmurs
Palpitations
Faintness
Occlusions
Claudications
PND
Other
MSK
If patient denies all symptoms for this system, check here: Denies all symptoms
Check the box next to each reported symptom and provide additional details.
Check if
Positive
Symptom Details
Pain
Stiffness
Crepitus
Limited ROM RUE
LUE
RLE
LLE
Redness
Misalignment
Other
GI
If patient denies all symptoms for this syste
[Show More]


.png)