SOAP Note Template
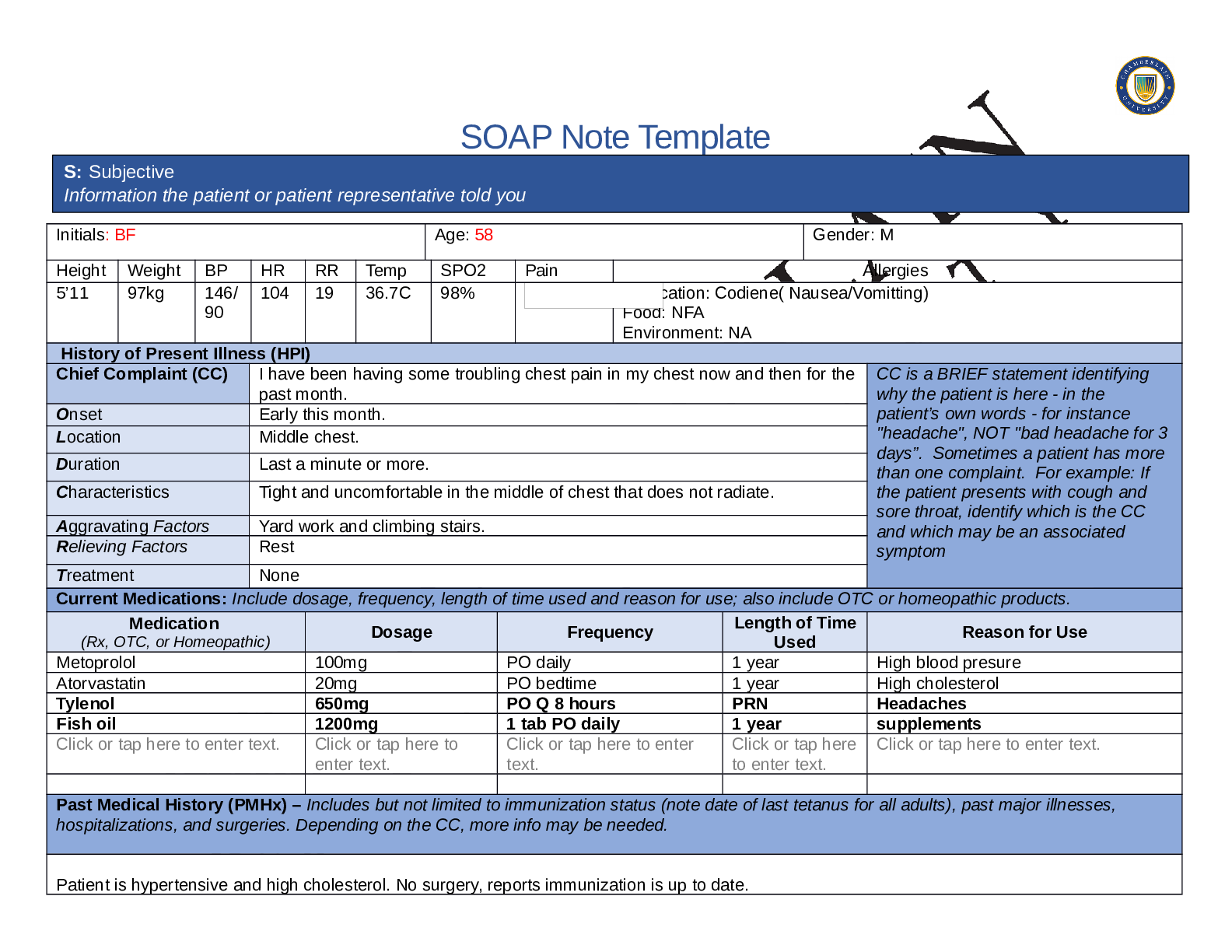
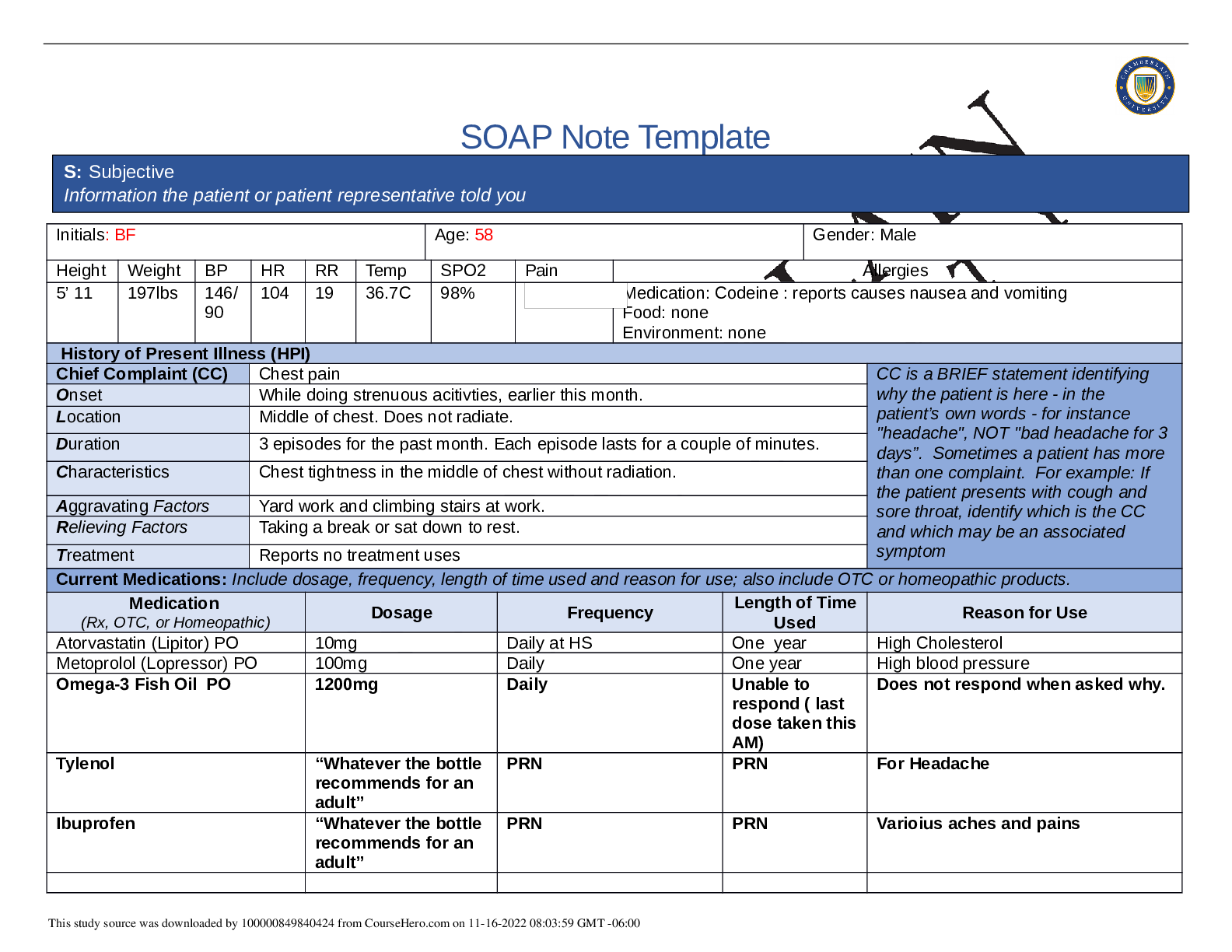
Initials: BF Age: 58 Gender: M
Height Weight BP HR RR Temp SPO2 Pain Allergies
5’11 97kg 146/
90
104 19 36.7C 98% Medication: Codiene( Nausea/Vomitting)
Food: NFA
Environment: NA
History of Pr
...
SOAP Note Template
Initials: BF Age: 58 Gender: M
Height Weight BP HR RR Temp SPO2 Pain Allergies
5’11 97kg 146/
90
104 19 36.7C 98% Medication: Codiene( Nausea/Vomitting)
Food: NFA
Environment: NA
History of Present Illness (HPI)
Chief Complaint (CC) I have been having some troubling chest pain in my chest now and then for the
past month.
CC is a BRIEF statement identifying
why the patient is here - in the
patient’s own words - for instance
"headache", NOT "bad headache for 3
days”. Sometimes a patient has more
than one complaint. For example: If
the patient presents with cough and
sore throat, identify which is the CC
and which may be an associated
symptom
Onset Early this month.
Location Middle chest.
Duration Last a minute or more.
Characteristics Tight and uncomfortable in the middle of chest that does not radiate.
Aggravating Factors Yard work and climbing stairs.
Relieving Factors Rest
Treatment None
Current Medications: Include dosage, frequency, length of time used and reason for use; also include OTC or homeopathic products.
Medication
(Rx, OTC, or Homeopathic) Dosage Frequency Length of Time
Used Reason for Use
Metoprolol 100mg PO daily 1 year High blood presure
Atorvastatin 20mg PO bedtime 1 year High cholesterol
Tylenol 650mg PO Q 8 hours PRN Headaches
Fish oil 1200mg 1 tab PO daily 1 year supplements
Click or tap here to enter text. Click or tap here to
enter text.
Click or tap here to enter
text.
Click or tap here
to enter text.
Click or tap here to enter text.
Past Medical History (PMHx) – Includes but not limited to immunization status (note date of last tetanus for all adults), past major illnesses,
hospitalizations, and surgeries. Depending on the CC, more info may be needed.
Patient is hypertensive and high cholesterol. No surgery, reports immunization is up to date.
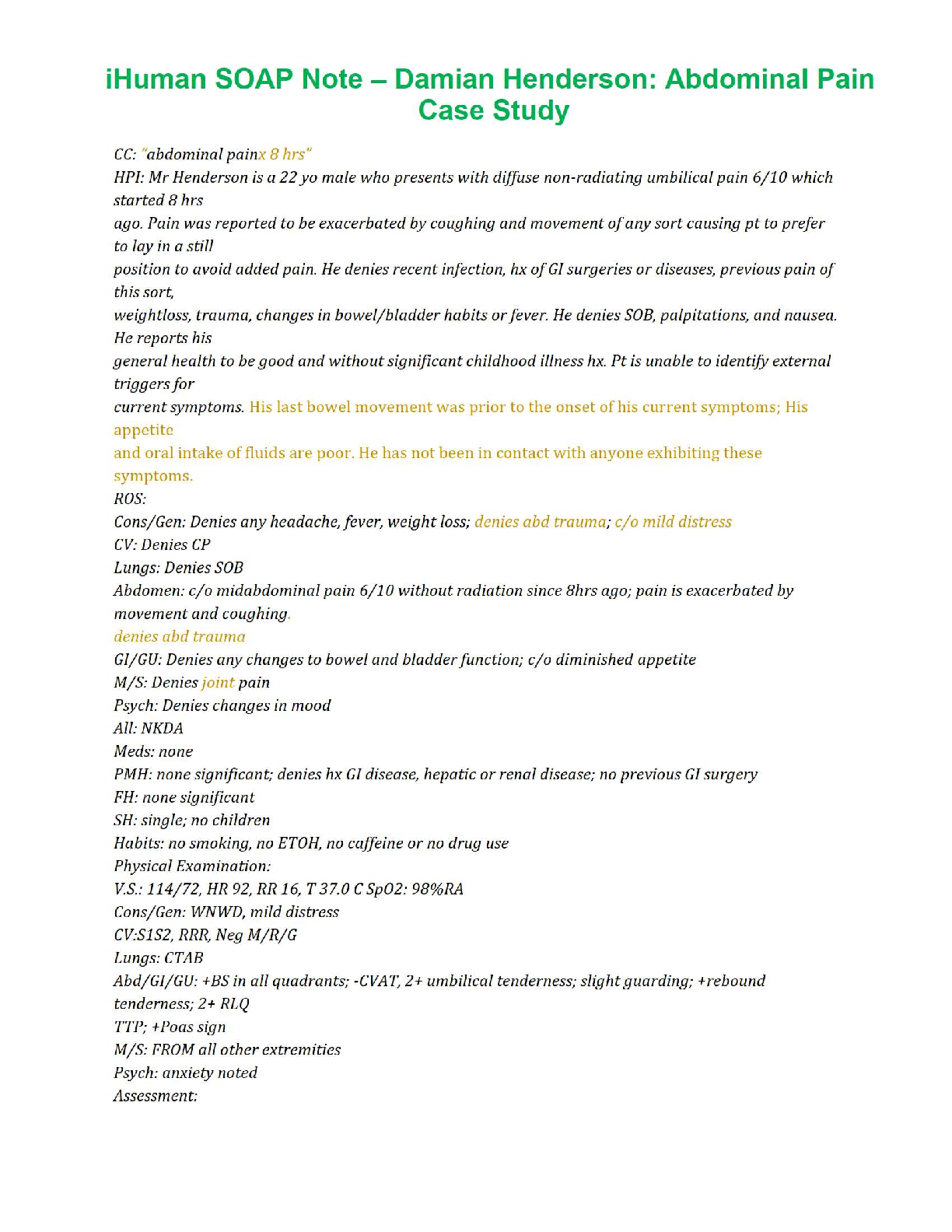
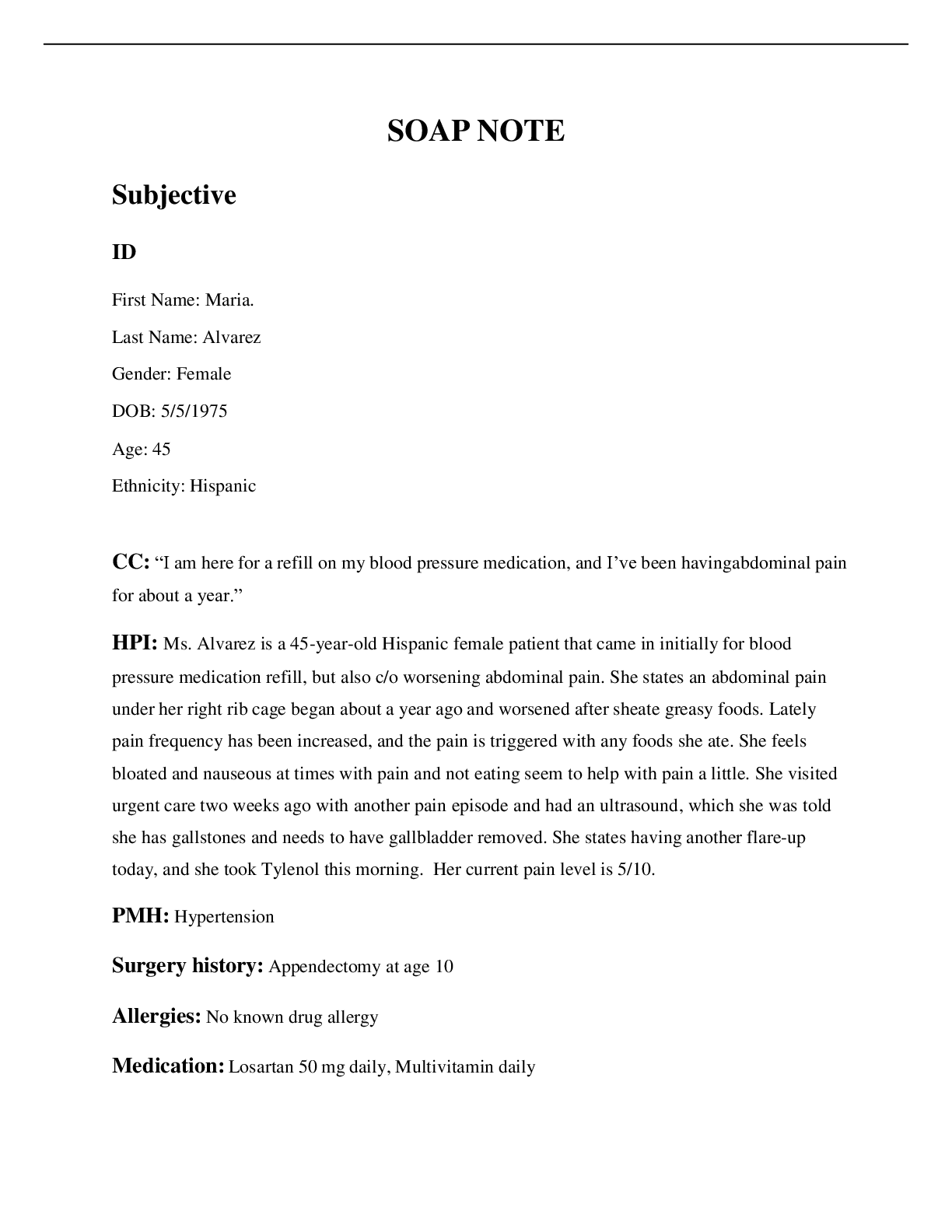
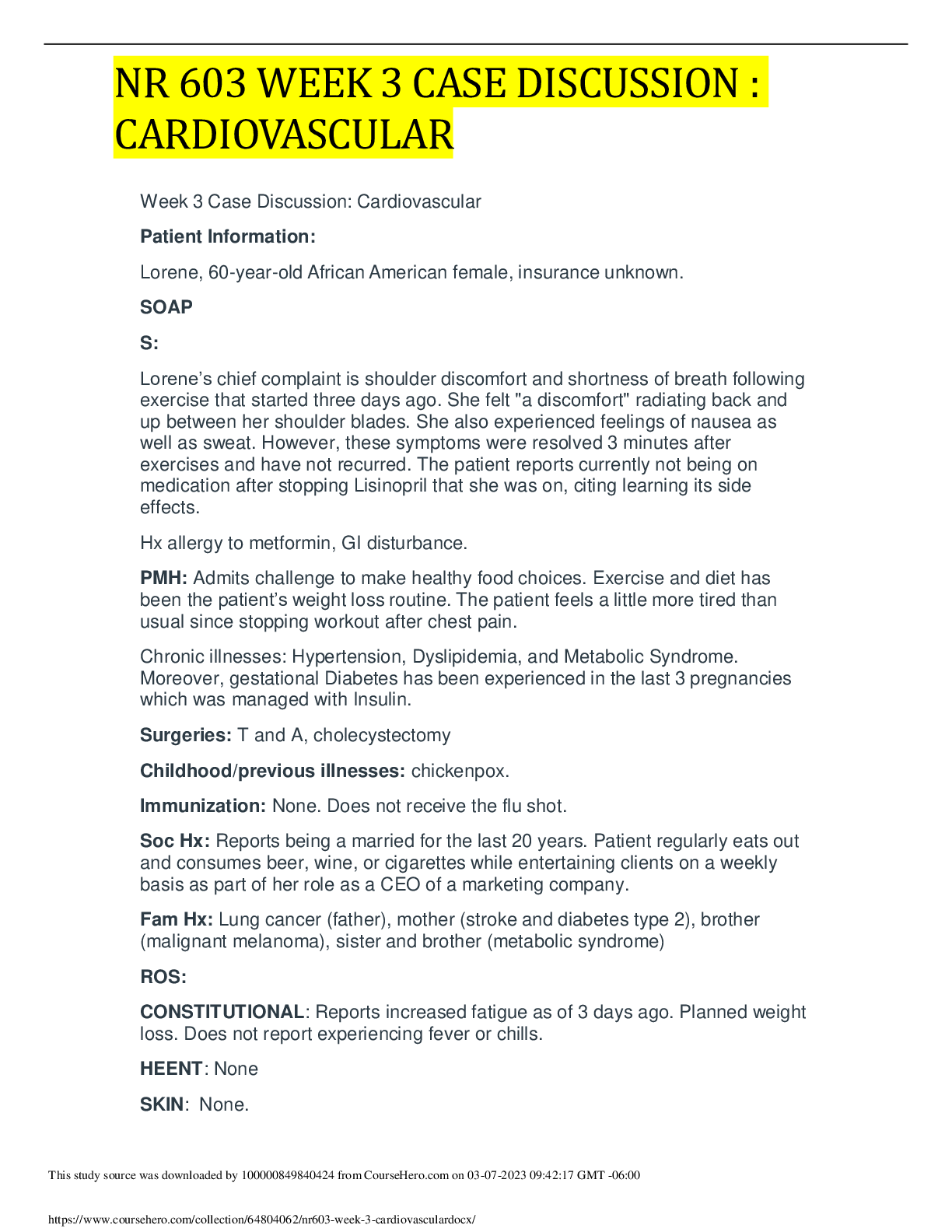
S: Subjective
Information the patient or patient representative told you
Social History (Soc Hx) - Includes but not limited to occupation and major hobbies, family status, tobacco and alcohol use, and any other pertinent
data. Include health promotion such as use seat belts all the time or working smoke detectors in the house.
Patient is married, lives with his wife and 2 children.He is a civil engineer and enjoys riding his bike a lot but has not done so in 2 years since it got
stolen. Denies illcit drug use or tobacco.Social drinker,drinks 2 to 3 bottles on the weekends. Uses his seatbelt while driving and has working smoke
detectors at home. Denies routine exercise.
Family History (Fam Hx) - Includes but not limited to illnesses with possible genetic predisposition, contagious or chronic illnesses. Reason for
death of any deceased first degree relatives should be included. Include parents, grandparents, siblings, and children. Include grandchildren if
pertinent.
Dad : Died of Colon cancer.
Mom: Living High blood pressure and Type 2 Diabetics.
Brother: passed at 24 years old from a MVA.
Sister:Living 52yo Type 2 diabetics and hypertension.
Paternal grand dad: Died at 85yo unknown causes.
Paternal grand mom: Died at 78 from pneumonia.
Maternal grand dad: Died at 54 from a heartattack.
Maternnal grand mom:died at 65 from Breast cancer.
Review of Systems (ROS): Address all body systems that may help rule in or out a differential diagnosis Check the box next to each positive
symptom and provide additional details.
Constitutional Skin HEENT
☐Fatigue Click or tap here
to enter text.
☐Weakness Click or tap
here to enter text.
☐Fever/Chills Click or tap
here to enter text.
☒Weight Gain Gained 15
pounds in a couple of
yearschest
☐Weight Loss Click or tap
here to enter text.
☐Trouble Sleeping Click or
tap here to enter text.
☐Itching Click or tap
here to enter text.
☐Rashes Click or tap
here to enter text.
☐Nail Changes Click
or tap here to enter
text.
☐Skin Color Changes
Click or tap here to
enter text.
☐Other:
Click or tap here to
enter text.
☐Diplopia Click or tap
here to enter text.
☐Eye Pain Click or tap
here to enter text.
☐Eye redness Click or
tap here to enter text.
☐Vision changes Click or
tap here to enter text.
☐Photophobia Click or
tap here to enter text.
☐Eye discharge Click or
tap here to enter text.
☐Earache Click or tap here
to enter text.
☐Tinnitus Click or tap here
to enter text.
☐Epistaxis Click or tap
here to enter text.
☐Vertigo Click or tap here
to enter text.
☐Hearing Changes Click
or tap here to enter text.
☐Hoarseness Click or tap here
to enter text.
☐Oral Ulcers Click or tap here
to enter text.
☐Sore Throat Click or tap here
to enter text.
☐Congestion Click or tap here
to enter text.
☐Rhinorrhea Click or tap here
to enter text.
☐Other:
Click or tap here to enter text.
☐Night Sweats Click or tap
here to enter text.
☐Other:
Click or tap here to enter
text.
Respiratory Neuro Cardiovascular
☐Cough Click or tap here to enter
text.
☐Hemoptysis Click or tap here to
enter text.
☐Dyspnea Click or tap here to enter
text.
☐Wheezing Click or tap here to enter
text.
☐Pain on Inspiration Click or tap here
to enter text.
☐Sputum Production
☐Other: Click or tap here to enter
text.
☐Syncope or
Lightheadedness Click or tap
here to enter text.
☐Headache Click or tap here
to enter text.
☐Numbness Click or tap here
to enter text.
☐Tingling Click or tap here to
enter text.
☐Sensation Changes
☐Speech Deficits Click or tap
here to enter text.
☐Other: Click or tap here to
enter text.
☒Chest pain chest pain my chest now
and then for the past month.
☐SOB Click or tap here to enter text.
☒Exercise Intolerance Experienced
while climbing the stairs at work.
☐Orthopnea Click or tap here to enter
text.
☐Edema Click or tap here to enter text.
☐Murmurs Click or tap here to enter
text.
☐Palpitations Click or tap
here to enter text.
☐Faintness Click or tap here
to enter text.
☐OC Changes Click or tap
here to enter text.
☐Claudications Click or tap
here to enter text.
☐PND Click or tap here to
enter text.
☒Other: S3 sound heard
MSK GI GU PSYCH
☐Pain Click or tap here to enter
text.
☐Stiffness Click or tap here to
enter text.
☐Crepitus Click or tap here to enter
text.
☐Swelling Click or tap here to enter
text.
☐Limited ROM
☐Nausea/Vomiting Click or tap here to
enter text.
☐Dysphasia Click or tap here to enter
text.
☐Diarrhea Click or tap here to enter
text.
☐Appetite Change Click or tap here to
enter text.
☐Heartburn Click or tap here to enter
☐Urgency Click or tap here to
enter text.
☐Dysuria Click or tap here to
enter text.
☐Burning Click or tap here to
enter text.
☐Hematuria Click or tap here
to enter text.
☐Polyuria Click or tap here to
☐Stress Click or tap here to
enter text.
☐Anxiety Click or tap here to
enter text.
☐Depression Click or tap here
to enter text.
☐Suicidal/Homicidal Ideation
Click or tap here to enter text.
☐Memory Deficits Click or tap
☐Redness Click or tap here to
enter text.
☐Misalignment Click or tap here to
enter text.
☐Other: Click or tap here to enter
text.
text.
☐Blood in Stool Click or tap here to
enter text.
☐Abdominal Pain Click or tap here to
enter text.
☐Excessive Flatus Click or tap here to
enter text.
☐Food Intolerance Click or tap here to
enter text.
☐Rectal Bleeding Click or tap here to
enter text.
☒Other:
Liver palpated 1cm beleow costal
margin
enter text.
☐Nocturia Click or tap here to
enter text.
☐Incontinence Click or tap
here to enter text.
☐Other: Click or tap here to
enter text.
here to enter text.
☐Mood Changes Click or tap
here to enter text.
☐Trouble Concentrating Click
or tap here to enter text.
☐Other: Click or tap here to
enter text.
GYN
☐Rash Click or tap here to enter text.
☐Discharge Click or tap here to enter text.
☐Itching Click or tap here to enter text.
☐Irregular Menses Click or tap here to enter text.
☐Dysmenorrhea Click or tap here to enter text.
☐Foul Odor Click or tap here to enter text.
☐Amenorrhea Click or tap here to enter text.
☐LMP: Click or tap here to enter text.
☐Contraception Click or tap here to enter text.
☐Other:Click or tap here to enter text.
O: Objective
Information gathered during the physical examination by inspection, palpation, auscultation, and palpation. If unable to assess a body
system, write “Unable to assess”. Document pertinent positive and negative assessment findings.
Body System Positive Findings Negative Findings
General
NA Pt is alert and oriented x4.No sign pf distress noted.denies pain
or shortness of breath. Able to follow commands.
Skin
NA Skin warn and dry to touch.No tenting.
HEENT
NA Head and neck is symmetrical, no sweeling noted.
Vision 20/20 in L,R and both eyes.PERRL noted.
Nose at midline and pink and mosit
Mucosa memberane pink and mosit.
Ears symmetrical bilaterally.
Respiratory
Fine crackles in right and left posterior lower lobes. Chest is symmetrical.
Breath sounds clearclear in all anterior lobes.
No shortness of breath noted.
Neuro
NA
Alert and oriented X4. No loss of consciousness noted.
No dizziness or light headness noted.
Cardiovascular
BP 146/90, HR 104
S3 hear sound heard.
PMI displaced laterally brisk and tapping less than 3cm
Bruit presence and +3 thrill in right carotid artery.
Popliteal,tibal aned dorsalis pedis pulse no thrill +1,
Chest symmetrical
S1 and S2 heart sounds heard.
JVP 3cm above sternal angle.
Cap refill less than 3 seconds in all extremities.
Brachial,radia, femoral pulses no thrill +2
Musculoskeletal
NA Range of motion equal in all exteimities.
Gait is steady
Gastrointestinal
Liver palpated 1cm below costal margin Abdomen soft and round. No tenderness or distention or masses
noted.Bowel sounds present in all 4 quadrants.Spleen and
kideneys not palpable .All areas of the abdomen are tympanic.
Genitourinary
NA Kidneys are not palpable bilaterally.
Problem List
1. Chest Pain 6 PMI displaced baterally brisk and
tapping
11 Weight gain
2 High blood pressure 7 RUQ Abdomen light tenderness 12 Diminshed popliteal arteries
3 Tachycardiac 8 RLQ/LLQ abdomen Light tenderness 13 Popliteal,tibal and dorsalis pedis
pulses. No thrill +1
4 Bruit and +3 Thrill found in right Carotid
pulse
9 liver palpated 1cm below costal margin 14 Click or tap here to enter text.
5 Fine crackles in lungs 10 Activity intolerance 15 Click or tap here to enter text.
Diagnosis ICD-10 Code Pertinent Findings
Coronary artery disease with
stable angina
125.119 Chest pain and tightness,High BP, tachycardia.
Congestive heart failure 150.20 Fine crackles, hypertension, S3 heart sound and weight gain.
Carotid artery disease 165.21 Presence of bruit and thrill +3 on right carotid pulse.
Diagnostics: List tests you will order this visit
Test Rationale/Citation
Chest Xray Chest Xray will shows images of the heart, lungs which can help diagnose heart failure.Fine crackles
in lungs shows some heart problems as evidence by S3 and bilaterally displaced PMI.Also chest xray
helps to depict changes in the lungs that sterm from heart failure. Fluid in the lungs will mean
pulmonary edema present in heart failure (mayoclinic.org 2019)
Echocardiogram Because pf the S3 sound heard around the mitral area and Echo will be recommended. An
echocardiogram uses sound waves to produce images of your heart. Parts that move weakly may
have been damaged duri
[Show More]