SOAP Note Template
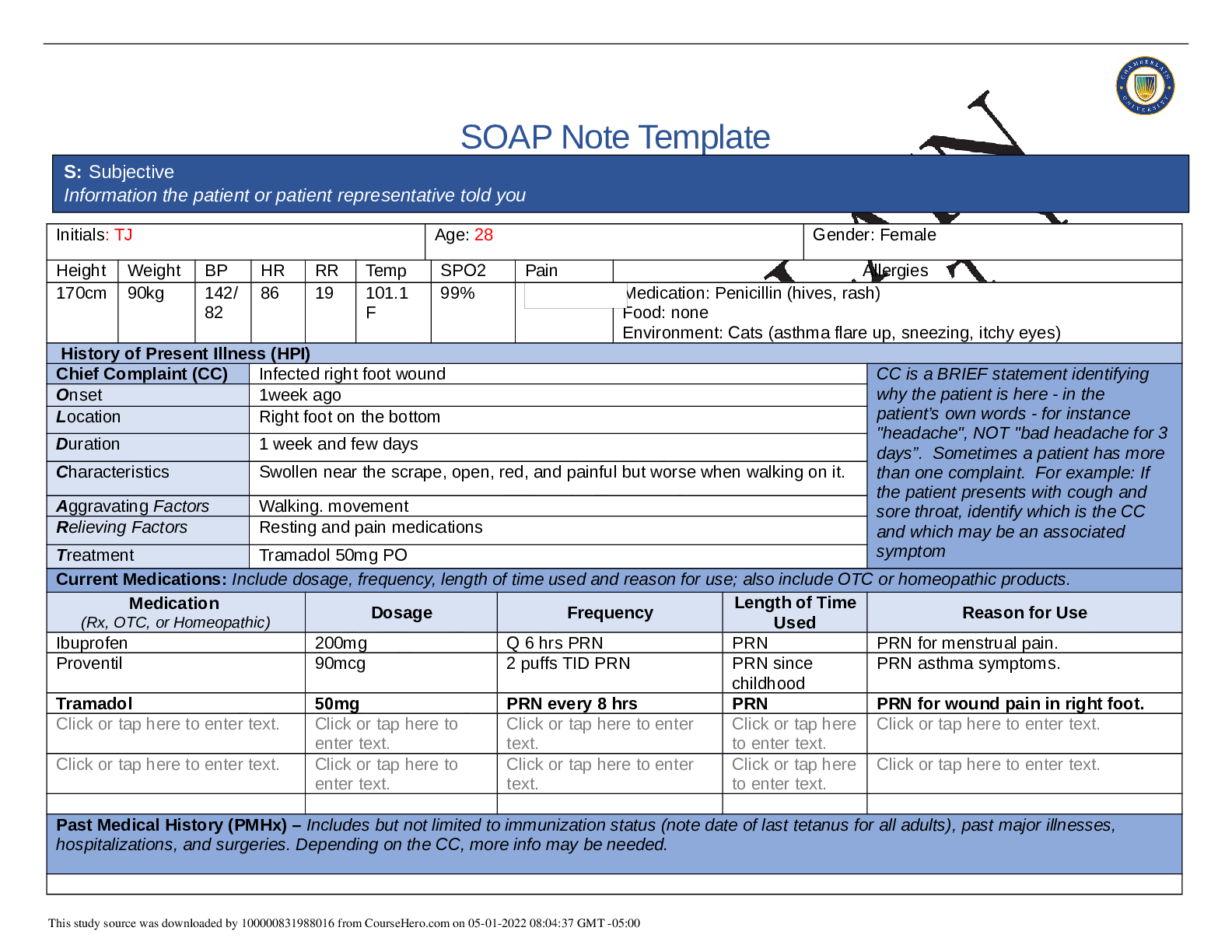
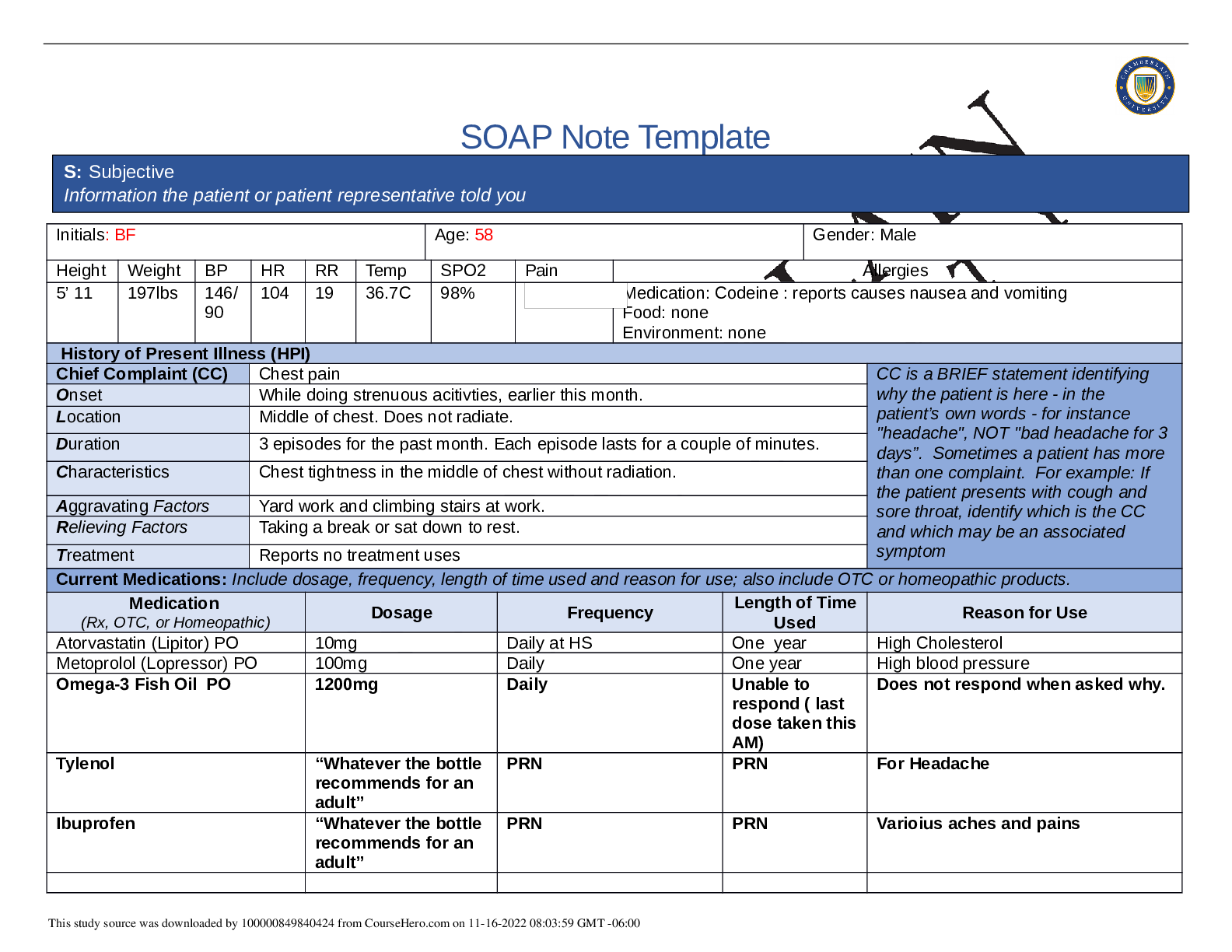
Initials: TJ Age: 28 Gender: female
Height Weight BP HR RR Temp SPO2 Pain Allergies
170cm 89kg 140/
81
89 20 98.5 97% Medication: penicillin-rash/hives
Food: none
Environment: Seasonal, Dust, Ca
...
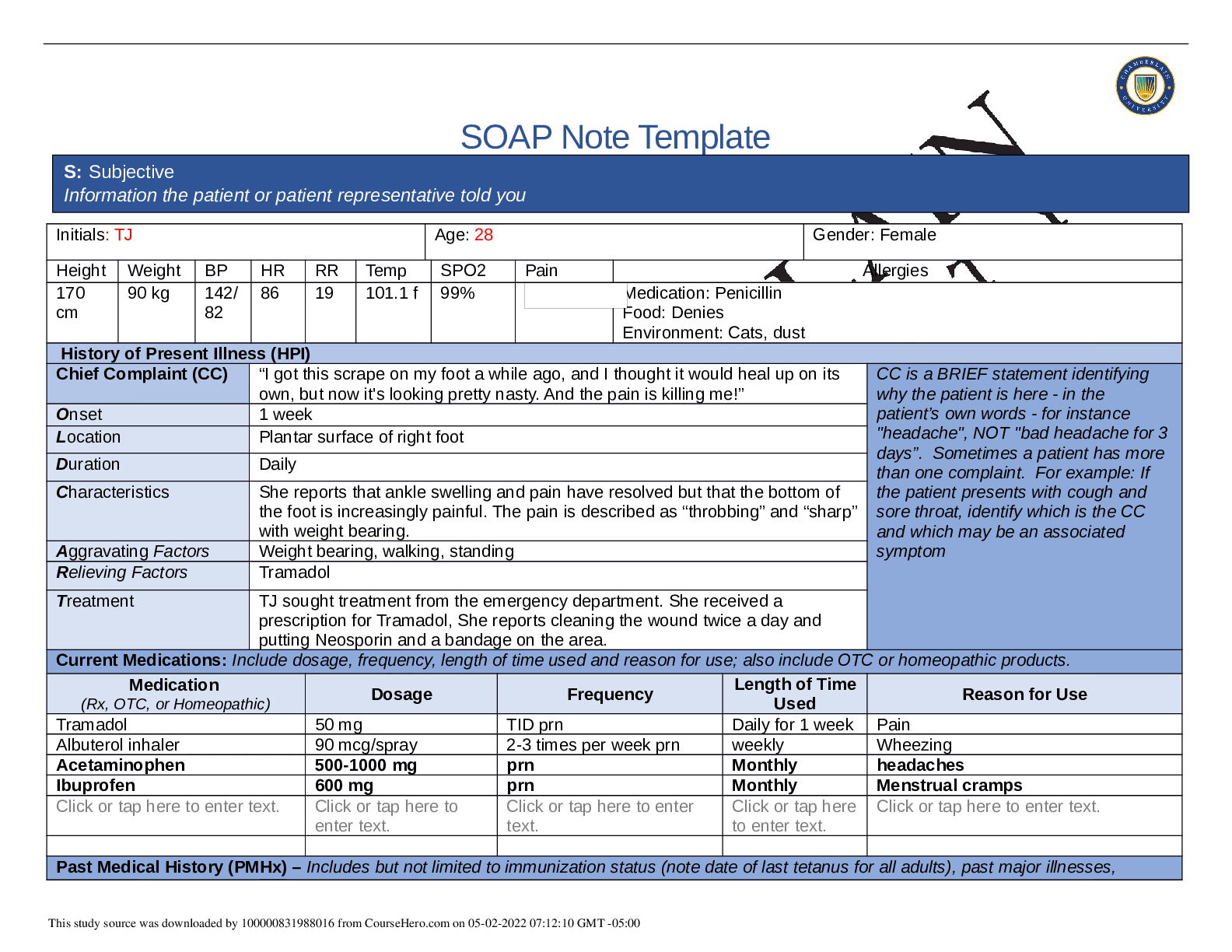
SOAP Note Template
Initials: TJ Age: 28 Gender: female
Height Weight BP HR RR Temp SPO2 Pain Allergies
170cm 89kg 140/
81
89 20 98.5 97% Medication: penicillin-rash/hives
Food: none
Environment: Seasonal, Dust, Cats- sneezing, wheezing, itchy eyes,
pruritis
History of Present Illness (HPI)
Chief Complaint (CC) “Shortness of Breath” CC is a BRIEF statement identifying
why the patient is here - in the
patient’s own words - for instance
"headache", NOT "bad headache for 3
days”. Sometimes a patient has more
than one complaint. For example: If
the patient presents with cough and
sore throat, identify which is the CC
and which may be an associated
symptom
Onset 2 days ago
Location Chest, Lungs
Duration Every four hours since original exacerbation, each episode lasting several
minutes
Characteristics Chest tightness, difficulty taking air in, wheezing, coughing, not relieved with
use of inhaler
Aggravating Factors Exertion, dust, cats, lying down
Relieving Factors Rest, inhaler, avoidance of allergens
Treatment Albuterol Inhaler
Current Medications: Include dosage, frequency, length of time used and reason for use; also include OTC or homeopathic products.
Medication
(Rx, OTC, or Homeopathic) Dosage Frequency Length of Time
Used Reason for Use
Click or tap here to enter text. Click or tap here to
enter text.
Click or tap here to enter
text.
Click or tap here
to enter text.
Click or tap here to enter text.
Albuterol Inhaler 90mcg-2 puffs Q4h prn Two days Asthma
Tylenol OTC extra strength 500mg PRN Intermittent Headache
Advil OTC 600mg (takes 3
200mg tablets)
PRN Intermittent Menstrual cramps
Click or tap here to enter text. Click or tap here to
enter text.
Click or tap here to enter
text.
Click or tap here
to enter text.
Click or tap here to enter text.
Past Medical History (PMHx) – Includes but not limited to immunization status (note date of last tetanus for all adults), past major illnesses,
hospitalizations, and surgeries. Depending on the CC, more info may be needed.
S: Subjective
Information the patient or patient representative told you
Past Medical History: Diabetes Melittus; Asthma: diagnosed at age 2.5years, HTN
Vaccinations:Resports being up to date with Pneumonia vaccine : 1 year ago; Tetanus Vaccine: 1 year ago. No current with Flu vaccine. Reports
that all childhood vaccines were received.
Past surgical history: None
Past hospital admissions: 3mo since last physical and check up.; apx. 5 hospital admissions for asthma exacerbations; Last admission related to
astma was when patient was 16.
Social History (Soc Hx) - Includes but not limited to occupation and major hobbies, family status, tobacco and alcohol use, and any other pertinent
data. Include health promotion such as use seat belts all the time or working smoke detectors in the house.
Marital Status: Single;
Current birth control methods: Abstinance; History of PO birth control (Last used 2 years ago)
Occupation: Works as a supervisor at Mid-American copy and shit
Education: attending college to obtain a bachelor’s degree in accounting.
Living arrangements: Lives with mother and sister.
Hobbies: Enjoys reading watching tv series and documentaries
Religion: Active in local church
Substance use: Denies tobacco use and current recreactional drug use. Reports marajuanna use 3 years ago
Drinks alcohol socially (apx twice a month). Last alcoholic beverage, 3 weeks ago.
Family History (Fam Hx) - Includes but not limited to illnesses with possible genetic predisposition, contagious or chronic illnesses. Reason for
death of any deceased first degree relatives should be included. Include parents, grandparents, siblings, and children. Include grandchildren if
pertinent.
Mother: Hypertension, High cholesterol
Father: (Deceased) at age 58 in mva: HTN, Type II DM, high cholesterol
Paternal Grandfather: (Deceased): Colon CA. Type II DM, HTN, high cholesterol
Paternal Grandmother: HTN, high cholesterol
Maternal Grandmother: HTN, high cholesterol
Maternal Grandfather: (Deceased): Cardiovascular Accident. HTN, High cholesterol
Sister: Asthma
Brother: No health history
Review of Systems (ROS): Address all body systems that may help rule in or out a differential diagnosis Check the box next to each positive
symptom and provide additional details.
Constitutional Skin HEENT
☒Fatigue recent-due to
waking up coughing at
night
☐Weakness denies
☐Fever/Chills denies
☐Weight Gain denies
☐Weight Loss denies
☒Trouble Sleeping due to
coughing
☐Night Sweats denies
☐Other:
Click or tap here to enter
text.
☒Itching with exposure
to cats
☐Rashes denies
☐Nail Changes denies
☒Skin Color Changes
skin on neck
☐Other:
Click or tap here to
enter text.
☐Diplopia denies
☐Eye Pain denies
☐Eye redness denies
☒Vision changes
worsening vision over
past 2 years
☐Photophobia Click or
tap here to enter text.
☐Eye discharge denies
☐Earache denies
☐Tinnitus denies
☐Epistaxis denies
☐Vertigo denies
☐Hearing Changes denies
☐Hoarseness denies
☐Oral Ulcers denies
☐Sore Throat denies
☐Congestion denies
☐Rhinorrhea denies
☒Other:
runny nose on occasion
Respiratory Neuro Cardiovascular
☒Cough with asthma past two days
☐Hemoptysis denies
☒Dyspnea Click or tap here to enter
text.
☒Wheezing Click or tap here to enter
text.
☐Pain on Inspiration denies
☐Sputum Production
☐Other: denies sputum
☐Syncope or
Lightheadedness denies
☒Headache on occasion
☐Numbness denies
☐Tingling denies
☐Sensation Changes
☐Speech Deficits denies
☐Other: Click or tap here to
enter text.
☒Chest pain during astma attack
☒SOB Click or tap here to enter text.
☒Exercise Intolerance Click or tap here
to enter text.
☒Orthopnea Click or tap here to enter
text.
☐Edema Click or tap here to enter text.
☐Murmurs denies
☐Palpitations denies
☐Faintness denies
☐OC Changes denies
☐Claudications denies
☐PND denies
☐Other: Click or tap here to
enter text.
MSK GI GU PSYCH
☐Pain denies
☐Stiffness denies
☐Crepitus denies
☐Nausea/Vomiting denies
☐Dysphasia denies
☐Diarrhea denies
☐Urgency denies
☐Dysuria denies
☐Burning denies
☒Stress managed by attending
church and talking
☐Anxiety denies
☐Swelling denies
☐Limited ROM
☐Redness denies
☐Misalignment denies
☐Other: Click or tap here to enter
text.
☐Appetite Change denies
☐Heartburn denies
☐Blood in Stool denies
☐Abdominal Pain denies
☐Excessive Flatus denies
☐Food Intolerance denies
☐Rectal Bleeding denies
☐Other:
Click or tap here to enter text.
☐Hematuria denies
☒Polyuria reports high water
intake
☒Nocturia Click or tap here to
enter text.
☐Incontinence denies
☐Other: Click or tap here to
enter text.
☐Depression denies
☐Suicidal/Homicidal Ideation
denies
☐Memory Deficits denies
☐Mood Changes denies
☐Trouble Concentrating
denies
☐Other: Click or tap here to
enter text.
GYN
☐Rash denies
☐Discharge denies
☐Itching denies
☒Irregular Menses menses every 6 weeks to 2
months
☒Dysmenorrhea reports very heavy periords
with severe cramps
☐Foul Odor denies
☐Amenorrhea denies
☐LMP: denies
☐Contraception Previously: Denies current use
☒Other:Abstinence/ not currently sexually active
O: Objective
Information gathered during the physical examination by inspection, palpation, auscultation, and palpation. If unable to assess a body
system, write “Unable to assess”. Document pertinent positive and negative assessment findings.
Body System Positive Findings Negative Findings
General
Patient alert/ oriented x4; Well groomed/kept; Distress, Odor
Skin
Acanthosis nigricans, Acne Cyanosis, palor, vascular discoloration, wounds, lesions,
diaphoresis
HEENT
Watery eyes, runny nose, voice clear Redness or eyes, nose, throat; Visual or auditory aid;
Respiratory
Symmetric chest expansion, bilateral and equal fremitus, lung
sounds and resonance in all lung fields, Wheezing and fine crackles
in bilateral middle and lower lung fields, cough
Evidence of trauma, pectus excavatum, use of accessory
muscles or intercostal retraction while breathing, stridor, rhonchi,
rales.
Neuro
Orientation, free movement in all extremities
Confusion, hallucinations, aphasia, paresthesia, memory loss,
dizziness
Cardiovascular
Respiratory distress, fatigue Jugular vein distention, edema, vascular discoloration
Musculoskeletal
Free movement of extremeties Inflammation/ swelling of joints, deformities
Gastrointestinal
Rounded Evidence of gastrostomy, surgeries, taut appearance
Genitourinary
Click or tap here to enter text. Click or tap here to enter text.
Psychiatric
Pleasant but concerned about breathing; Hallucinations, anxiety, depression
Problem List
1. Asthma 6. Knowledge Deficit of HTN 11 Click or tap here to enter text.
2 . Diabetes 7 . Knowledge Deficit of Diabetes 12 Click or tap here to enter text.
3 . Hypertension 8 Click or tap here to enter text. 13 Click or tap here to enter text.
4 . Obesity 9 Click or tap here to enter text. 14 Click or tap here to enter text.
5 . Dysmenorreha 10 Click or tap here to enter text. 15 Click or tap here to enter text.
Diagnosis ICD-10 Code Pertinent Findings
Asthma J45.909 Wheezing, coughing, tightness in chest, shortness of breath;
Exacerbated by dust, allergens, exercise, stress, and
worsening of symptoms at night.
Diabetes E11.65 Elevated blood glucose readings, Acanthosis nigricans,
positive family history,, history of taking metformin
Hypertension RO3.0 High blood pressure reading without the presence of a
diagnosis of hypertension, family history of hypertension,
Diagnostics: List tests you will order this visit
Test Rationale/Citation
CXR To rule out other causes for cough and respiratory distress, such as an infectious process, cardiac
dysfunction, or pneumothorax. (Ash & Diaz, 2017).
Spirometry To measure the amount of air inhaled and exhaled from an individual. After a patient takes a full breath
in, a TLC or total lung capacity is measured; A forced vital capacity (FCV) can be measured by
measuring the amount of air pushed out on expiration. A residual volume (RV), is then measured,
when the lungs have been emptied. In an asthmatic patient, this procedure is completed. A treatment
of a bronchodilator can then be administered to open the airways. A repeat test is then completed. An
A: Assessment
Medical Diagnoses. Provide 3 differential diagnoses which may provide an etiology for the CC. The first diagnosis (presumptive
diagnosis) is the diagnosis with the highest priority. Provide the ICD-10 code and pertinent findings to support each diagnosis.
P: Plan
Address all 5 parts of the comprehensive treatment plan. If you do not wish to order an intervention for any part of the treatment plan, write
“None at this time” but do not leave any heading blank. No intervention is self-evident. Provide a rationale and evidence-based in-text citation for
each intervention.
improvement of the pulmonary function testing after administration of a bronchodilator can aid in the
diagnosis and treatment effectiveness for asthmatic patients. (Dempsey and Scanlon, 2018).
FeNo Testing FeNo testing uses a device to measure the amount of exhaled nitric oxide, which in an individual
during an asthmatic event, will elevate as the inflammation in the airways causes the nitric oxide levels
to increase. ( Asthma and Allergy Foundation of America (AAFA), 2019).
Provocation (Trigger) Test Administered to the patient is small doses of an irritant, to assess for asthma triggers, exercise, to
assess for activity intolerance, and methacholine, to assess for other causes of respiratory distress.
(AAFA, 2019).
Peak Flow Meter Testing The patient will be instructed and given a peak flow meter for testing how well air is moving in and out
of the lungs. This meter may be beneficial in noting if the patient is nearing an asthmatic event, and
also if medications are successful. (AAFA, 2019).
Medications: List medications/treatments including OTC drugs you w
[Show More]