*NURSING > SHADOW HEALTH > NURSING 202 FINAL-ANSWER_KEY-PPH Unfolding Reasoning Postpartum Hemorrhage (PPH) Brenda Jackson, 22 (All)
NURSING 202 FINAL-ANSWER_KEY-PPH Unfolding Reasoning Postpartum Hemorrhage (PPH) Brenda Jackson, 22 years old
Document Content and Description Below
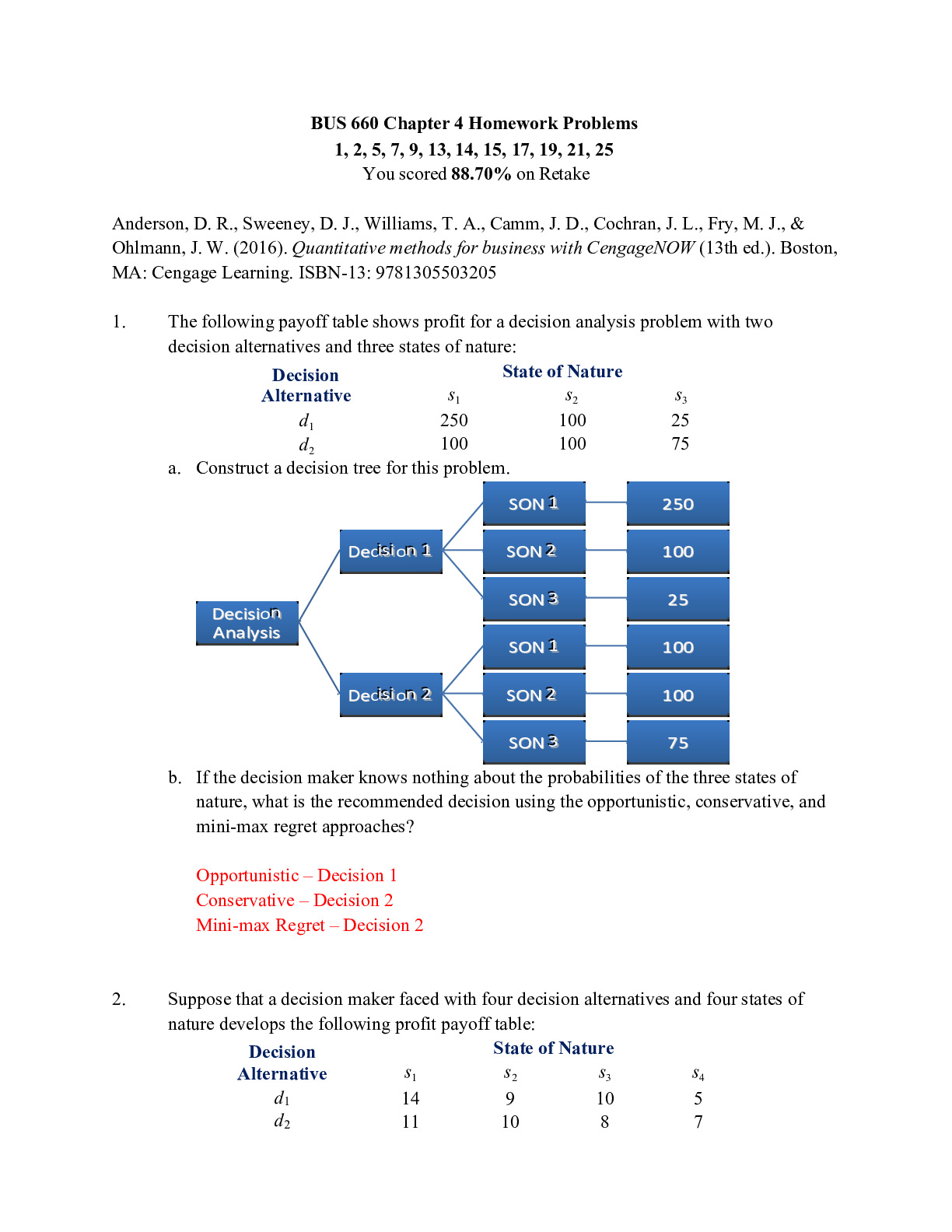
NURSING 202 FINAL-ANSWER_KEY-PPH Unfolding Reasoning Postpartum Hemorrhage (PPH) Brenda Jackson, 22 years old © 2016 Keith Rischer/www.KeithRN.com Postpartum Hemorrhage (PPH) Brenda Jackson, 22 ... years old Primary Concept Perfusion Interrelated Concepts (In order of emphasis) 1. Clotting 2. Clinical Judgment 3. Patient Education 4. Communication 5. Collaboration© 2016 Keith Rischer/www.KeithRN.com UNFOLDING Reasoning Case Study: Postpartum Hemorrhage (PPH) History of Present Problem: Brenda Jackson is a 22-year-old African American, G-1, now T-1 P -0 A- 0 L-1 who is Group B strep positive and was treated with four doses of penicillin G. She had a vaginal delivery over an intact perineum after 19 hours of labor at 39 weeks gestation. She has been clinically stable and is about to be transferred to the postpartum unit after a two-hour recovery period. Oxytocin 20 units in 1000 mL of Lactated Ringer’s is infusing at a fixed rate of 125 mL/hr in a 20 g. peripheral IV in her left hand. Type and screen done on admission, Hgb 12.6/Hct 38. Her last set of vital signs were: T: 99.4 F/37.4 C P: 95 R: 18 BP: 110/67. She has gotten up to void once and had 50 mL of blood-tinged urine. Her fundus is firm at the umbilicus, and has a small amount of dark red lochia. She is physically exhausted and has been anxious since delivery because her labor and delivery were harder than she ever expected. Personal/Social History: Brenda is an advanced nursing student in her final year. She is single and remains in a relationship with her boyfriend, who is also the father of her baby. She lives at home with her parents, who are supportive. What data from the histories are RELEVANT and have clinical significance to the nurse? RELEVANT Data from Present Problem: Clinical Significance: Group B strep positive and was treated with four doses of penicillin G. She is a G-1, term 39-week gestational vaginal delivery P: 95 BP: 110/67. Group B streptococcus (GBS) is a type of bacterial infection that can be found in a pregnant woman’s vagina or rectum. This bacteria is normally found in the vagina and/or rectum of about 25% of all healthy, adult women. Women who test positive for GBS are said to be colonized. A mother can pass GBS to her baby during delivery. GBS affects about 1 in every 2,000 babies in the United States. Not every baby who is born to a mother who tests positive for GBS will become ill. Although GBS is rare in pregnant women, the outcome can be severe for the newborn. Physicians include testing as a routine part of prenatal care. She is a first-time parent, with a low-risk prenatal history, delivery without complications, and normal BUBBLE-HE assessment Though this HR is not >100, it is close enough that it must be recognized as a clinical RED FLAG. This is not an acceptable ambiguity! It may be due to post-delivery pain or a compensatory response to hypovolemia based on physiologic compensation to maintain cardiac output. Remember the patho equation CO=SVxHR! This is now very relevant to clinical practice! Though this is the first BP in this scenario, emphasize the importance of TRENDING all clinical data especially in the context of this scenario when the worst possible/most likely complication is post-partum hemorrhage. The BP as well as HR are ALWAYS RELEVANT! IMPORTANT POINT to emphasize: Pregnancy increases circulating volume by 40% at term. This increase will conceal blood loss by maintaining the BP longer. Blood pressure in the immediate postpartum period should be normal; any deviation should be reported. Increased blood pressure can indicate gestational hypertension. Decreased blood© 2016 Keith Rischer/www.KeithRN.com pressure can be related to orthostatic hypotension, shock, or dehydration (side effect of epidural anesthesia). Loss of <1000= orthostatic tachycardia Loss 0f <1500= resting tachycardia, orthostatic hypotension Loss of < 2500=resting hypotension Loss of >2500= oliguria C-V collapse and obtunded. (CMQCC, 2015) RELEVANT Data from Social History: Clinical Significance: Advanced nursing student in her final year She is single who is still in with relationship with her boyfriend who is also the father of her baby. She still lives at home with her parents who are supportive. Nursing is a stressful major, as every student can testify! She will need support and a plan to successfully manage and balance the demands of a new baby and her college education. Because she is single, it is important to assess the degree of social as well as family support and to involve social services as needed. Since she has a supportive significant other, this will likely not be needed but must be noted by the nurse. Has adequate support from parents, and/or boyfriend. What is the RELATIONSHIP of your patient’s past medical history (PMH) and current meds? (Which medication treats which condition? Draw lines to connect.) PMH: Home Meds: Pharm. Classification: Expected Outcome: G1-T1-P0-A0-L1 Prenatal vitamin (PVI) 1 tab PO daily Ferrous gluconate 325 mg PO daily 1. Vitamins 2. Iron supplement 1. Prevention of deficiency or replacement of essential vitamins 2. Treatment and prevention of iron deficiency in pregnancy Patient Care Begins: Brenda arrived in her room ten minutes ago. You were delayed by another mother who required pain medication, but the nursing assistant collected the first set of vital signs posted below. You introduce yourself, orient her to the room and unit, and begin your BUBBLE-HE assessment: What VS data are RELEVANT and must be recognized as clinically significant by the nurse? RELEVANT VS Data: Clinical Significance: P: 105 (regular) This is a clinical RED FLAG. This is not acceptable ambiguity! It may be due to pain postdelivery or a compensatory response to hypovolemia based on physiologic compensation to maintain cardiac output. Remember the patho equation CO=SVxHR! This is now very relevant to clinical practice! TRENDing all relevant data, including vital signs, is an essential component of clinical reasoning. The heart rate remains elevated and increased from previous HR of 95. Current VS: P-Q-R-S-T Pain Assessment (5th VS): T: 99.9 F/37.6 C (oral) Provoking/Palliative: Vaginal delivery P: 105 (regular) Quality: Cramp R: 22 (regular) Region/Radiation: Lower abdomen BP: 110/75 Severity: 6/10 O2 sat: 98% room air Timing: Started one hour after delivery© 2016 Keith Rischer/www.KeithRN.com R: 22 (regular) BP: 110/75 She is tachypneic. This is also an increase from her most recent reported rate of 18. This elevation is slight but must be noted. It could be due to a number of factors including pain, exhaustion after delivery, or an early sign of hypovolemic shock. Anticipating the most likely complication in any patient care setting is an important responsibility of the nurse and will be addressed more intentionally later in this study. After delivery, the woman is autotransfused from delivery of the placenta so she is able to maintain her BP until about a 20% loss of circulating blood volume. Knowing that every postpartum patient is at risk for bleeding, the BP is ALWAYS relevant, even if normal. What assessment data is RELEVANT and must be recognized as clinically significant by the nurse? RELEVANT Assessment Data: Clinical Significance: GENERAL APPEARANCE: Appears uncomfortable, restless CARDIAC: Pink, warm/dry, no edema, heart sounds regular with no abnormal beats, equal with palpation at radial/pedal/post-tibial landmarks UTERUS: Right of umbilicus, slightly boggy, palpable bladder BLADDER: Voided 50 ml after delivery, bladder distended LOCHIA: Rubra. Soaked entire peri pad with 10- 12” diameter puddle Though it is expected for the mother to be uncomfortable and in pain after a vaginal delivery, this mother is also restless. The nurse must step back and ask why? Is this expected, and if not, what could be causing this finding? Knowing that she is tachycardic, her CV status must be closely assessed by the nurse and this data clustered to determine if a problem is present. Though normal at this time, it must be TRENDED to identify a change in status. Her uterus is slightly boggy and displaced to the right and high, bladder is filling with urine. Small void prior to transfer. This is relevant data that must be recognized by the nurse. What is the consequence of a boggy uterus? It has a much higher risk of resulting in a postpartum hemorrhage! Though this finding is at the end of this assessment box, stress that in clinical practice this would likely be the first thing that would be determined after vital signs. The tachycardia suggests a possible hemorrhage and this is the easiest and most obvious way to confirm. The other clinical data in this assessment clustered together confirms this problem and must also be quickly noted. The nurse must recognize that this is a clinical emergency. Because the uterus is slightly boggy, the bleeding will likely continue and pads/chux will need to be weighed to closely assess amount of bleeding until the uterus is firmed up! Current Assessment: GENERAL APPEARANCE: Appears uncomfortable, restless RESP: Breath sounds clear with equal aeration bilaterally, nonlabored respiratory effort CARDIAC: Pink, warm/dry, no edema, heart sounds regular with no abnormal beats, equal with palpation at radial/pedal/post-tibial landmarks NEURO: Alert and oriented to person, place, time, and situation (x4) BUBBLE-HE BREAST: Lactating; soft, non-tender with evidence of colostrum UTERUS: Right of umbilicus, slightly boggy BLADDER: Voided 50 ml after delivery, bladder distended BOWELS: Abdomen soft/nontender, bowel sounds audible per auscultation in all four quadrants LOCHIA: Rubra. Soaked entire peri pad with 10-12” diameter puddle of blood weight= 450 mL HOMANS: Negative EPISIOTOMY: Perineum intact© 2016 Keith Rischer/www.KeithRN.com Lab Results: What lab results are RELEVANT and must be recognized as clinically significant by the nurse? RELEVANT Lab(s): Clinical Significance: TREND: Improve/Worsening/Stable: Hgb: 8.9 Hct: 28 Platelets: 158 Hgb and Hct levels parallel each other and are frequently used to evaluate anemia or, in this scenario, the lack of RBCs that are causing this to drop due to hemorrhage. Though it is not in textbooks, I have observed clinically that a drop of 1 g of Hgb approximates the loss of 1 unit of blood. Number of RBCs, or packed cell volume, expressed as a percentage of whole blood. For example, a packed cell volume, or Hct of 45% means that a 100-mL sample of blood contains 45 mL of packed RBCs. Platelet aggregation is the beginning of the clotting cascade to stop any bleeding. Though normal, it is low. If bleeding persists, may require this blood product in addition to PRBCs. Continue to monitor. WORSENING WORSENING Stable What lab results are RELEVANT and must be recognized as clinically significant by the nurse? RELEVANT Lab(s): Clinical Significance: PT/INR: 0.9 PTT: 30 Fibrinogen: 44 Measures time required for a firm fibrin clot to form and measures the length of time for the clotting cascade. Measures the length of time (in seconds) required for clotting to occur when certain reagents are added to plasma. Essential component in the process of hemostasis or clot formation. In the common final pathway of the coagulation process, thrombin converts fibrinogen to fibrin. Though normal, these coag studies are RELEVANT and confirm that there is no progression to DIC or a clotting disorder responsible for her PPH Complete Blood Count (CBC): Current: High/Low/WNL? Previous: WBC (5-15.0 mm 3/Pregnant) 14.5 HIGH 13.5 Hgb (12-16 g/dL) 8.9 WNL 12.6 Hct (33-45%) 28 LOW 38 Platelets (150-450x 103/µl) 158 WNL 140 Neutrophil % (42-72) 72 HIGH 68 Coags: Current: High/Low/WNL? PT/INR (0.9–1.1 nmol/L): 0.9 WNL PTT (29-35 seconds): 30 WNL Fibrinogen (<80 mg/dL): 44 WNL© 2016 Keith Rischer/www.KeithRN.com Lab Planning: Creating a Plan of Care with a PRIORITY Lab: Lab: Normal Value: Clinical Significance: Nursing Assessments/Interventions Required: Hemoglobin Value: 8.9 g/dL Male: 13.2-17.3 g/dL Pregnant Female: 11.5-14.0 g/dL Critical Value: <6.6 or >20 Primary protein of erythrocytes that is composed of heme (iron) and globin (protein) *Carries O2 to cells and CO2 back to lungs *Parallels Hematocrit, which is the % of RBC in proportion to total plasma volume *GOLD STANDARD for evaluating blood/RBC adequacy (anemia, blood loss) THINK BLOOD LOSS/ANEMIA *Identify early signs of blood loss: tachycardia, then hypotension *Assess for signs of tissue hypoxia (see above) *Assess skin color as well as tolerance to activity Van Leeuwen & Bladh, (2015). Clinical Reasoning Begins… 1. What is the primary problem that your patient is most likely presenting with? Early post-partum hemorrhage (PPH) 2. What is the underlying cause/pathophysiology of this primary problem? Defined as a blood loss of greater than 500 mL after giving birth vaginally or a blood loss of greater than 1,000 mL after a cesarean section. Because many women lose at least 500 mL of blood during childbirth and do not experience any symptoms, a more accurate way to define PPH is losing 1% or more of the body weight after delivering a baby (1 mL of blood weighs 1 g). For example, a patient weighing 175 lb (80 kg) would need to lose 800 mL of blood to be classified as having a PPH. ACOG (2015) reports that a PPH is defined by a cumulative blood loss of > 1000 or blood loss accompanied by signs of hypovolemia within 24 hours following birth. Trigger 500-999 ml should increase supervision and potential interventions. Vital Sign RED FLAGS include: HR over 110 BP 85/45 or less Causes of postpartum hemorrhage: Though bleeding is the problem, identifying the CAUSE is essential to STOP the bleeding! The number one cause of early PPH is uterine atony, a condition in which the uterus does not adequately contract and clamp down, allowing increased blood loss from the placental site of implantation. After the placenta is delivered, the uterus needs to contract to seal off the iliac arteries. If the uterus is contracted, the placental site is smaller, causing less bleeding. Lacerations of the perineum, vagina, and cervix can occur during a vaginal birth. Lacerations of the cervix occur with rapid dilation or with pushing before complete dilation. During the second stage of labor, vaginal, perineal, and periurethral tears occur. Failure to repair these lacerations adequately can result in a slow, steady trickle of blood (Sommers & Fannin, ( 2015). Use the 4 T’s to simplify the most common causes of PPH: T=tone uterine atony (full bladder, Pitocin, large babies, multip, many causes) T=tear unrepaired (cervix, vaginal) T=tissue (placenta left in uterus) T=thrombin (blood clotting issue)© 2016 Keith Rischer/www.KeithRN.com Collaborative Care: Medical Management Care Provider Orders: Rationale: Expected Outcome: Establish large bore peripheral IV Administer 0.9% Normal Saline 1000 mL IV bolus Oxytocin 20 units in 1000 mL Lactated Ringers (LR) infuse over 30 minutes. Titrate to vaginal bleeding (AWHONN Guideline) Methylergonovine 0.2 mg IM x1stat The following meds are standing orders and in the hemorrhage cart to be given as needed if oxytocin ineffective: Carboprost 250 mcg IM PRN Misoprostol 800 mcg rectal or SL PRN Complete blood count (CBC) PT/INR, PTT, Fibrinogen Contact OR for possible D&C or repair and address other Will require aggressive fluid resuscitation and likely blood products. At a minimum, a 20-gauge IV catheter is needed and preferably an 18-gauge or green hub catheter wiil be used. The larger the gauge or smaller the number, the larger amount of fluid that can be administered quickly in an emergency Though normal saline does not carry oxygen, it will restore fluid volume deficit that is present due to bleeding. It will also increase blood pressure, which will increase perfusion to vital organs, especially the kidneys, that are sensitive to fluid volume deficit. Stimulates uterine smooth muscle which produces inuterine contractions similar to those in spontaneous labor. Also has vasopressor and antidiuretic effects. Run at 999 mL/hr on the pump to get it in ASAP if actively bleeding! Directly stimulates uterine and vascular smooth muscle causing uterine contraction. Causes uterine contractions by directly stimulating the myometrium and controls postpartum bleeding. Causes uterine contractions which will help control postpartum bleeding In this context, the most important labs that must be noted are the hemoglobin and hematocrit as well as platelets. The current findings must be compared to the most recent if present in the chart and trended to determine the trend in this scenario. I have observed in my clinical practice that a loss of 1 g of hemoglobin is comparable to 1 unit of blood Bleeding times to rule out/monitor for the complication of DIC This patient is at a very high risk of requiring additional interventions, including hysterectomy, to stop the bleeding if oxytocin is not effective. IV established IV fluids administered with decrease in HR and increase in BP if adequate resuscitation obtained Replace 3 ml to 1 ml. anticipate PRBC 1-2 units, anticipate FFP after 1-2 units of PRBC. Uterus contracts and blood loss diminishes Uterus contracts and blood loss diminishes Uterus contracts and blood loss diminishes Uterus contracts and blood loss diminishes Both Hgb and Hct will likely be low due to known blood loss n/a OR ready if needed with all staff needed© 2016 Keith Rischer/www.KeithRN.com PRIORITY Setting: Which Orders Do You Implement First and Why? Care Provider Orders: Order of Priority: Rationale: Oxytocin 20-40 units in 1000 mL. Infuse over 30 minutes and titrate to blood loss. Methylergonovine 0.2 mg IM x1stat Establish large bore peripheral IV x 2 Administer 0.9% Normal Saline 1000 mL IV bolus Contact OR to prepare for possible case 1. Establish large bore peripheral IV 2. Oxytocin 10 units infused at 20–40 milliunits/min. 3. Methylergonovine 0.2 mg IM x1stat 4. Administer 0.9% Normal Saline 1000 mL IV bolus 5. Contact OR for possible D&C or repair This is an excellent example of the relevance of the ABCs to setting priorities in practice. The nurse must be able to recognize and identify which interventions impact A, B or C. This is why the nurse must also understand the physician’s plan of care and interventions! 1. C-priority. Second large bore IV must be established to administer intravenous fluids and prepare for possible blood products 2. C-priority. Oxytocin is a close second. It will stop bleeding and resolve the problem if effective. 3. C-priority. Oxytocin is a close second. It will stop bleeding and resolve the problem if effective. 4. C-priority. This is also a circulatory priority.It will replace fluid volume deficit and elevate blood pressure. 5. Though this is not the least important intervention, it is something that would be delegated to another nurse and done immediately. But it is not an ABC priority and therefore filters toward the bottom of priority setting. Medication Administration: Medication/Dose: Mechanism of Action: Nursing Assessment/Considerations: Oxytocin 20 units/1000 mL LR IV gtt Stimulates uterine smooth muscle which produces intrauterine contractions similar to those in spontaneous labor. Also has vasopressor and antidiuretic effects. Anticipate the most common side effect of painful contractions Assess character, frequency, and duration of uterine contractions; resting uterine tone Assess for increase in uterine tone and reduction in postpartum bleeding Monitor maternal BP and pulse frequently Vallerand, Sanoski, & Deglin, (2014). Methylergonovine 0.2 mg IM x1stat Directly stimulates uterine and vascular smooth muscle, causing uterine contraction. Avoid with asthma, liver disease or C-V disease Monitor amount and type of vaginal discharge. Notify physician or other health care professional immediately if symptoms of hemorrhage (increased bleeding, hypotension, pallor, tachycardia) occur. Carboprost 250 mcg IM x1 stat Causes uterine contractions by directly stimulating the myometrium and controls postpartum bleeding. Avoid with elevated BP or preeclampsia. Can cause diarrhea and nausea. Most common side effects include diarrhea, nausea, vomiting, fever, chills Life-threatening side effects include uterine rupture and anaphylaxis. Misoprostol 800 mcg rectal or SL x1 stat Causes uterine contractions which will help control postpartum bleeding Not FDA approved; often used rectally, starting to be used SL Most common side effects include abdominal pain, diarrhea Vallerand, Sanoski, & Deglin, (2014)© 2016 Keith Rischer/www.KeithRN.com Collaborative Care: Nursing 3. What nursing priority(ies) will guide your plan of care? (if more than one-list in order of PRIORITY) Fluid volume deficit related to blood loss 4. What interventions will you initiate based on this priority? Unit and nurse readiness! All maternal child nurses need to be prepared to deal with a postpartum hemorrhage by possessing a DEEP knowledge of PPH; the effect of pregnancy on C-V system; standing orders for a standardized approach; and blood product policies including massive transfusion policies, location of supplies and equipment-including operation of equipment, hemorrhage cart stocked and available. Team simulation participation when available. Nursing Interventions: Rationale: Expected Outcome: Contact primary care provider Establish a second large bore peripheral IV Prepare to administer 0.9% Normal Saline 1000 mL IV bolus Administer O2 to keep O2 sat >95% NPO Fundal massage and express clots Empty bladder Frequently assess fundus, lochia In order to provide definitive care in a crisis, the primary care provider must provide orders including the need for intravenous fluids and Pitocin. Recognizing the gravity of this situation, the primary nurse can delegate this initial contact to another nurse. By the time the care provider calls, the primary nurse should be in a position to talk directly and facilitate the plan of care. If the patient has an IV present, the size of the IV must be determined. If it is a small gauge (20-22), this is too small to quickly administer intravenous fluid resuscitation. A second large bore IV must be established (typically an18 gauge IV catheter). Depending on the hospital protocol there may be a standing order to administer intravenous fluids of normal saline in this situation. If so, hang the IV fluids. If not, have them ready to administer once the primary care provider confirms the present plan of care. Standard of care to improve oxygenation with shock The nurse must be proactive and recognize where this scenario could quickly go. The bleeding may not be able to be managed and patient will need to go to surgery. Therefore, making this patient strict NPO is prudent and proactive. Massaging the fundus is something the nurse can do immediately to attempt to cause the uterus to contract and help clamp off and diminish or stop the bleeding, depending on where it is located. Start right away before IV fluids. Someone else can handle IV. Patient may void per bedpan or straight catheter. The nurse must continue to closely Contact established and orders received. Care provider should come to the bedside and examine. In real-world practice, this is done as a team effort with an additional nurse. 18 g. IV established IV fluids administered with decrease in HR and increase in BP if adequate resuscitation obtained O2 sat >95% n/a Uterus begins to firm with decrease in bleeding if effective 600 ml clear yellow urine out© 2016 Keith Rischer/www.KeithRN.com Frequently assess HR, BP Weigh peri pads/chux assess the bogginess of the fundus as well as the amount of bleeding or lochia. This will confirm if fundal massage has been effective. Emptying the bladder will help in most cases. Closely assessing the heart rate and BP in the context of a postpartum hemorrhage is essential. The heart rate will typically increase to compensate for decreased cardiac output and the blood pressure will drop if there is significant loss of blood. Both heart rate and blood pressure must be assessed frequently and trended closely together to determine the trajectory of this patient. This is also the essence of clinical reasoning. By carefully weighing all peri pads or chux that are soaked with blood, the nurse can accurately estimate the actual loss of blood. 1gm equals 1 mL of fluid volume. Depends on source/location of bleeding Decrease in HR and increase in BP if adequate resuscitation obtained Accurate assessment of amount of vaginal bleeding 5. What body system(s) will you assess most thoroughly based on the primary/priority concern? Circulatory 6. What is the worst possible/most likely complication to anticipate? Progressive hypovolemic shock with a need to undergo emergent D&C or tissue repair, insertion of a balloon tamponade, possible B-Lynch suture or hysterectomy. The nurse must anticipate and make the mental shift from a low-risk vaginal delivery to potential emergency. Postpartum hemorrhage is a preventable cause of maternal mortality and severe morbidity. Disseminated intravascular coagulation (DIC) Some facts that are relevant to PPH: Two to three women die every day in the United States from complications that occur while giving life. Approximately half of these maternal deaths have been determined to be preventable. African American women have three to four times more deaths than women of all other racial/ethnic groups. A woman in the United States almost dies of pregnancy-related complications every 10 minutes. Postpartum hemorrhage is a leading cause of these complications, with an estimated 2.9% of the women who give birth in the U.S. will bleed too much. This means about 125,000 women a year are affected. In the last 10 years, there was a 183% increase in the number of women who had a blood transfusion around the time they gave birth. In 1998-1999, compared to 2008-2009, there was a 75% increase in the number of women who suffered serious injuries while giving birth. The U.S. is one of the only countries where maternal deaths and injuries have increased. AWHONN Hemorrhage (2013)projecthttp://www.pphproject.org/maternal-morbidity-mortality.asp 7. What nursing assessments will identify this complication EARLY if it develops? The assessment findings are essentially the same between DIC and hypovolemic shock because the problem of excessive vaginal bleeding is the same. The only way to differentiate the cause is to obtain a coag panel of PT/INR, PTT, and fibrinogen. Hypovolemic shock Continued vaginal bleeding Ongoing INCREASE in heart rate Late DECREASE in BP© 2016 Keith Rischer/www.KeithRN.com Disseminated intravascular coagulation (DIC) Continued vaginal bleeding Ongoing INCREASE in heart rate Late DECREASE in BP 8. What nursing interventions will you initiate if this complication develops? Hypovolemic shock Titrate Pitocin to obtain adequate uterine contraction Anticipate operating room preparation for D&C or tissue repair, insertion of a balloon tamponade, possible BLynch suture or hysterectomy. Embolization may be utilized- notify radiology of potential case. Disseminated intravascular coagulation (DIC) Packed red blood cells are used to improve oxygen delivery by increasing the hemoglobin content of the blood. Fresh-frozen plasma replaces many of the clotting factors, whereas cryoprecipitate is the best source of fibrinogen and factors VIII and XIII. Platelet transfusion is used when the platelet count falls below 100,000/mm3 (Sommers & Fannin, ( 2015). 9. What psychosocial needs will this patient and/or family likely have that will need to be addressed? Emotional support Knowledge and education about what is taking place and what the care priorities will be in the days ahead 10. How can the nurse address these psychosocial needs? Emotional support o BE PRESENT and AVAILABLE. See the section on caring at the end of this case study for more information. Knowledge and education about what is taking place and what the care priorities will be in the days ahead o The nurse can integrate patient/family education naturally while providing care by simply explaining at their level everything that the nurse/physician has ordered and WHY it needs to be done. This is why it is essential for the nurse to know and DEEPLY understand the rationale for both the physician and nursing plan of care; so it can be readily taught and explained to the patient/family at a level they can understand. Evaluation: Evaluate the response of your patient to nursing and medical interventions during your shift. All primary care provider orders have been implemented that are listed under medical management. Fifteen minutes after the oxytocin bolus of 20 units is administered, the nurse collects the following clinical data: Current VS: Most Recent: P-Q-R-S-T Pain Assessment (5th VS): T: 97.8 F/36.6 C (oral) T: 99.9 F/37.6 C (oral) Provoking/Palliative: Movement P: 118 P:104 (regular) Quality: Cramping R: 24 R: 22(regular) Region/Radiation: Lower abdomen BP: 88/46 BP: 105/76 Severity: 7/10 O2 sat: 98% 3 liters n/c O2 sat: 92% room air Timing: Since transfer to room© 2016 Keith Rischer/www.KeithRN.com 1. What clinical data is RELEVANT that must be recognized as clinically significant? RELEVANT VS Data: Clinical Significance: P: 118 R: 24 BP: 88/46 Heart rate remains elevated and is trending upward despite intravenous fluid resuscitation with normal saline and oxytocin to control bleeding. This is a clinical RED FLAG that makes it clear that she is trending in the wrong direction and will likely require an emergent hysterectomy. Tachypnea in this scenario is likely due to hypovolemic shock. This is another clinical RED FLAG that must be recognized by the nurse. Clustered with the other vital sign findings, the blood pressure is trending in the wrong direction and confirms that she is clearly in progressive hypovolemic shock and has not improved despite medical intervention. The likely next step will be an emergent hysterectomy. RELEVANT Assessment Data: Clinical Significance: UTERUS: Firm with massage LOCHIA: Soaked entire peri pad with 8” diameter puddle of blood on chux. 600 mL based on weight of peipad and chux Though the tone of the uterus has increased slightly, it remains boggy and as a result, the hemorrhage continues. Confirms the ongoing vaginal bleeding has not been controlled and is significant in its amount. 2. Has the status improved or not as expected to this point? Both the vital sign and assessment data clearly reveal that Brenda’s condition is deteriorating and she is in need of emergent rescue! 3. Does your nursing priority or plan of care need to be modified in any way after this evaluation assessment? Yes. Medical management to this point has been ineffective to control the hemorrhage. 4. Based on your current evaluation, what are your nursing priorities and plan of care? In order to stop the bleeding and save her life, she must undergo an emergent hysterectomy. The essence of the nursing priority at this time is to facilitate transfer to the OR where this definitive treatment can take place. The primary care provider is at bedside and has contacted the OR to prepare for a D&C or possible repair. The OR is ready to receive the patient. Current Assessment: GENERAL APPEARANCE: Uncomfortable, restless RESP: Breath sounds clear with equal aeration bilaterally, slightly labored respiratory effort CARDIAC: Pale, cool and dry, no edema, heart sounds regular with no abnormal beats, peripheral pulses weak, equal with palpation at radial/pedal/post-tibial landmarks NEURO: Alert and oriented to person, place, time, and situation (x4) BUBBLE-HE BREAST: Lactating, soft, non-tender with evidence of colostrum UTERUS: Firm with massage only, midline BLADDER: Voided 600 mL clear, yellow urine in last hour BOWELS: Abdomen soft/nontender, bowel sounds audible per auscultation in all four quadrants LOCHIA: Soaked entire peri pad with 8” diameter puddle of blood on chux. 600 mL based on weight of peripad and chux HOMANS: No calf pain EPISIOTOMY: Intact© 2016 Keith Rischer/www.KeithRN.com SBAR: Nurse-to-Nurse Effective and concise handoffs are essential to excellent care and if not done well can adversely impact the care of this patient. You have done an excellent job to this point, now finish strong and give the following SBAR report to the OR nurse who will be responsible for this patient: Situation: Name/age: Brenda Jackson is a 22-year-old woman BRIEF summary of primary problem: She had a vaginal delivery after 19 hours of labor at 39 weeks gestation. She was stable and transferred to the postpartum unit. She developed a postpartum hemorrhage. saturating peri pads, and had at least 1200 mL hemorrhage with a boggy uterus that did not respond to oxytocin gtt. Has been NPO since delivery. Background: Primary problem/diagnosis: Severe Postpartum hemorrhage RELEVANT past medical history: Healthy, G-1, now P-1 with no prior medical history. RELEVANT background data: Brenda is an advanced nursing student in her final year. She lives at home with her parents, who are supportive. Assessment: Most recent vital signs: T: 97.0 F/36.3 C (oral) P: 118 R: 24 BP: 76/44 O2 sat: 98% 3 liters n/c RELEVANT body system nursing assessment data: GENERAL APPEARANCE: Uncomfortable, restless RESP: Breath sounds clear with equal aeration bilaterally, slightly labored respiratory effort CARDIAC: Pale, cool and dry, no edema, heart sounds regular with no abnormal beats, peripheral pulses weak, equal with palpation at radial/pedal/post-tibial landmarks UTERUS: firm with massage, midline U-1 LOCHIA: Soaked entire peri pad with 8” diameter puddle of blood on chux. 600 mL based on weight of peipad and chux RELEVANT lab values: Hgb: 8.9…most recent 12.6 Hct: 28…most recent 38 TREND of any abnormal clinical data (stable-increasing/decreasing): Hgb is dropping significantly How have you advanced the plan of care? IV established x2 and has received 1000 mL NS Continuous IV gtt of Oxytocin infusing Given Methylergonovine 0.2 mg IM x1stat© 2016 Keith Rischer/www.KeithRN.com Education Priorities/Discharge Planning 1. What will be the most important discharge/education priorities for Brenda? How to check her own fundus and do a fundal massage. Inform the patient to contact the physician for the following: o Boggy uterus that does not become firm with massage o Excessive bright red or dark red bleeding, many large clots o Fever above 100.4°F o Persistent or severe perineal pain or pressure If iron supplements are provided, teach the patient to take the drug with orange juice and expect some constipation and dark-colored stools. If antibiotics are ordered, teach the patient to finish the prescription, even though the symptoms may have ceased (Sommers & Fannin, 2015). Standards of Postpartum Care Mom Rest (sleep when baby sleeps, if possible) No driving for 3 days Limit walking up stairs first week; do not lift more than 10 pounds for the first few weeks after delivery. If breastfeeding, add 300 calories daily; general nutrition: increase fiber and fluids, do not “diet” without talking to your health care provider. Bleeding should lighten up in color and amount over the next few weeks. There should be no foul odor. Report episiotomy pain or difficult bowel movement to your provider. Report bleeding that soaks a pad every hour for 2 hours. Report fever of 100.4 F/38.0 C or greater, swelling, redness, separation or discharge from the episiotomy site. Change pads every few hours. When urinating, be sure to wipe from front to back. Report pain with urination, foul odor, feeling of fullness after urination. If breastfeeding, wear a supportive bra, and allow nipples to airdry after breastfeeding. Feed every 2-3 hours during the first few weeks of life (on demand), allowing newborn to empty both breasts completely. If bottle feeding, you may experience milk coming in. Wear a supportive bra, and use ice if your breasts become painful. When showering, keep the warm water away from your breasts. Your menstrual cycle is usually delayed with breastfeeding; most women resume menses 7-9 weeks postpartum; nursing mothers usually resume menstrual periods by 12th week postpartum. It is possible to become pregnant before the return of menses; use birth control during intercourse to prevent pregnancy. Bowel function will resume within 3 days; report any problems with bowels after 3 days. You may experience baby blues during the first few days after giving birth. This will resolve in a few days. If it does not, or if it is so severe you cannot take care of yourself or your baby, it is important to call your health care provider. Patient response: Continues to bleed. INTERPRETATION of current clinical status (stable/unstable/worsening): Unstable Recommendation: Suggestions: Transfer to the OR for D&C (for possible retained placental tissue) and need for possible tamponade balloon.© 2016 Keith Rischer/www.KeithRN.com Other symptoms to report to the provider include: visual disturbances; severe headache;, flu-like symptoms; pain or redness in one or both breasts; pain, warmth, tenderness or swelling in your legs, especially in the calves; or frequent nausea and vomiting. Your health care provider would like to see you in the office in 6 weeks. Baby If breastfeeding – on demand, usually every 2-3 hours. Your baby should have 6-8 wet diapers daily after the fourth day of life; this is a sign that the baby is getting enough breast milk. Baby’s stools will be loose, and the baby may have a bowel movement with each feeding because breast milk is so easily digested. Breastfed babies often have runny, mustard- colored seedy stools, about 6-8 times daily. Bottle feeding – Prepare and store formula per manufacturer’s instructions. Do not keep bottles that the baby has already used – throw out the formula. Never microwave formula. Feed your baby formula at a temperature he/she prefers. Do not prop bottles. Your baby will probably want to feed every 2-4 hours at first. Your baby will probably have yellowish- tan stools, these can vary from 6-8 times daily. Talk with the baby’s doctor to be sure all your questions are answered about how to feed your baby. Newborns sleep for 2-3 hours at a time during the first few months, and wake up around the clock. Plan your rest periods to match the baby’s. Always place your baby on his/her back to sleep to prevent Sudden Infant Death syndrome (SIDS). Tummy time is important, too, but must be supervised. NEVER SHAKE YOUR BABY – Shaken Baby syndrome causes irreversible brain injury. If you need a break, place your baby in a safe place and walk away. Call another adult to help you and get a break. Wash the diaper area thoroughly with each diaper change, and dry gently. There is no need for lotions or creams unless your health care provider instructs you to use them. If your baby develops diaper rash, you can apply a little diaper rash cream or petroleum jelly after you wash and dry the area. Sponge bathe your baby until the umbilical cord falls off, usually at about 2-3 weeks. The umbilical area should be kept dry until the cord falls off. There is no other special care for the umbilical cord. After the cord falls off, you can bathe your baby in a tub. NEVER leave your baby unattended while bathing, and ensure that the water will not burn your baby by using the inside of your forearm to test the water temperature, or use a thermometer. Check your baby’s skin every day to see if it is becoming more yellow. Report increased yellow skin to the health care provider. Your baby will have fussy periods almost every day, usually around the same time. Take the time to comfort your baby. Irritability, lethargy, and loss of appetite can signal illness in a newborn. Take your baby’s temperature, as directed by your health care provider if you think the baby is sick. Call the provider if the baby’s temperature is above 100 degrees or below 97.2 degrees. Always use a car seat. Make sure you place the car seat in the back seat and that it is rear-facing. Never leave the baby in a car by him/herself. Your health care provider would like to see your baby in 2-3 days. Please make sure to make an appointment promptly, so the baby can be seen in time. Call 911 immediately if you baby turns blue or has pale-colored skin. Call the office if the baby becomes more yellow, if there are patches of white found in the baby’s mouth, if eating poorly or refusing to eat or no stool for 48 hours or fewer than 6 wet diapers in 24 hours. Report any drainage or foul odor around the umbilicus, temperature of 100 degrees or more, difficulty breathing, repeated vomiting or several refused feedings in a row, listlessness, crying excessively without a known cause, frequent fluid bowel movements (you will see a water ring on diaper), drastic behavior changes such as increased irritability, excessive crying without cause, extreme sleepiness or floppy arms/legs, congested cough, running eye or nose.© 2016 Keith Rischer/www.KeithRN.com 2. What are some practical ways you as the nurse can assess the effectiveness of your teaching with this patient? After any education has been completed with the patient or family, one of the more effective strategies to assess effectiveness of teaching is to have them restate the essence or most important points of your teaching after it has been taught and then later in the shift to ensure retention. Include patient demonstration if possible. This is especially relevant with all teaching involving the care of the baby. Caring and the “Art” of Nursing 1. What is the patient likely experiencing/feeling right now in this situation? The nurse needs to put her/himself in the place of the patient to identify what is being experienced in this situation. The patient is likely aware of the seriousness of her change in status and may be fearful and anxious. Support her and her family intentionally by giving them as much information about her current status and explain the plan of care from both a nursing and medical perspective. KNOWLEDGE is POWER from a patient’s perspective.When the nurse provides this information, it will DECREASE anxiety and fear and make a real difference in her well-being. Even in the context of a patient who is critically ill, when you simply and matter-of-factly share what you are doing and why, it demonstrates the caring and support that is needed. 2. What can you do to engage yourself with this patient’s experience, and show that he/she matter to you as a person? After surgery, the reality of what has just happened will begin to sink in. Remain present, allow her to verbalize and share her feelings to clearly communicate caring in this context. Allow questions. If she went to ICU, try to incorporate family-centered care in the ICU. Regardless of the clinical setting, remember the importance of touch and your presence as you provide care. If you are using Swanson’s Caring framework (which I encourage you to do–see my “Teaching Caring” tab on KeithRN.com), the following practical caring interventions can be “tools” in your caring toolbox to use depending on the circumstance and the patient needs (Swanson, 1991). o Comforting Little things to comfort–whatever it may be–are needed and appreciated! i.e. hand or foot massage for pain control o Anticipating their needs Staying one step ahead and not behind, especially in a crisis is essential! Is everything where the patient can reach it before you leave the room? o Performing competently/skillfully Remember that when a nurse or student nurse does their job well and competently, this demonstrates caring to the patient! o Preserving dignity Maintaining privacy at all times is essential and is all too easily forgotten due to pressing physical needs. Pulling the curtain as well as covering exposed genitalia are all that is needed. They are little things, but so important to preserve human dignity. How to accomplish bodily functions which are disrupted with someone else present is significant. Be respectful of privacy issues. o Informing/explaining–patient education Even in a crisis, simply explain all that you are doing. If your patient is not able to respond but family are present, do not forget to explain to them all that you are doing and why. This is truly the “art” of nursing and makes such a difference when done in practice! Use Reflection to THINK Like a Nurse Reflection-IN-action (Tanner, 2006) is the nurse’s ability to accurately interpret the patient’s response to an intervention in the moment as the events are unfolding to make a correct clinical judgment. 1. What did I learn from this scenario? Have students share and reflect 2. How can I use what has been learned from this scenario to improve patient care in the future? Have students share and reflect© 2016 Keith Rischer/www.KeithRN.com Author Peggy Cowling, APN, MSN, RNC-OB, C-EFM, Clinical Instructor, University of Illinois at Chicago Reviewer Ruth Lathe, RNC, MSN, Assistant Professor, Harcum College, Bryn Mawr, Pennsylvania References [Show More]
Last updated: 2 years ago
Preview 1 out of 17 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$14.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Nov 08, 2022
Number of pages
17
Written in
Additional information
This document has been written for:
Uploaded
Nov 08, 2022
Downloads
0
Views
330