*NURSING > SHADOW HEALTH > Postpartum Affective Disorder UNFOLDING Reasoning Brittany Horton, 28-year-old female (All)
Postpartum Affective Disorder UNFOLDING Reasoning Brittany Horton, 28-year-old female
Document Content and Description Below
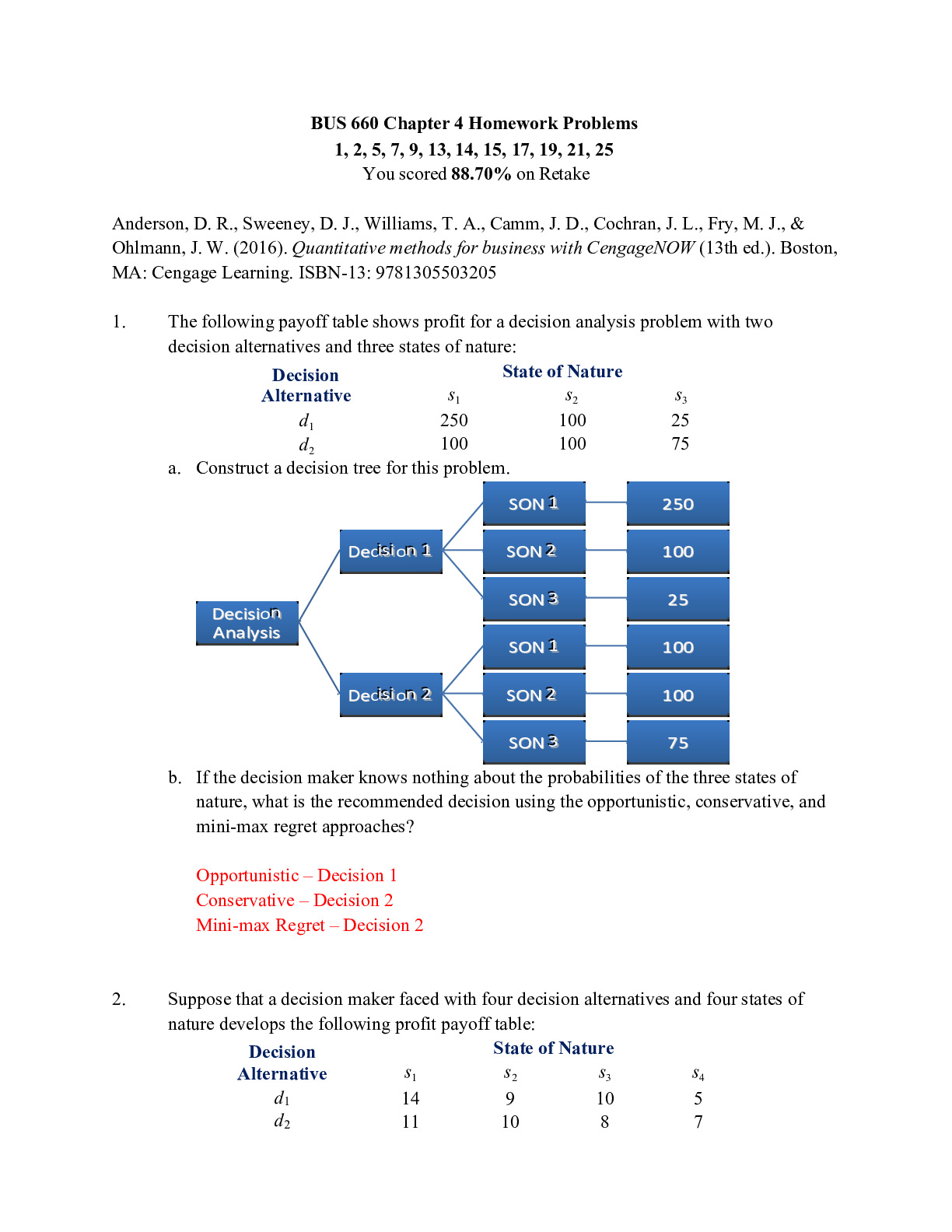
Postpartum Affective Disorder UNFOLDING Reasoning Brittany Horton, 28-year-old female Copyright © 2018 Keith Rischer, d/b/a KeithRN.com. All Rights reserved. Postpartum Affective Disorder UNFOLD... ING Reasoning Brittany Horton, 28-year-old female Primary Concept Mood and Affect Interrelated Concepts (In order of emphasis) • Stress • Coping • Clinical Judgment • Patient Education • Communication • Collaboration NCLEX Client Need Categories Percentage of Items from Each Category/Subcategory Covered in Case Study Safe and Effective Care Environment • Management of Care 17-23% ✓ • Safety and Infection Control 9-15% Health Promotion and Maintenance 6-12% ✓ Psychosocial Integrity 6-12% ✓ Physiological Integrity • Basic Care and Comfort 6-12% ✓ • Pharmacological and Parenteral Therapies 12-18% ✓ • Reduction of Risk Potential 9-15% ✓ • Physiological Adaptation 11-17% ✓ This study source was downloaded by 100000826504961 from CourseHero.com on 06-20-2022 06:51:57 GMT -05:00 https://www.coursehero.com/file/72531007/Metavee-Rynott-Post-Partum-Affective-Disorder-UNFOLDING-Reasoningpdf/Copyright © 2018 Keith Rischer, d/b/a KeithRN.com. All Rights reserved. History of Present Problem: Brittany Horton is a 28-year-old female, G1 P1, who delivered baby boy Mitchell 36 hours ago via primary cesarean section due to breech presentation. Brittany was 39 3/7 weeks gestation and had an uneventful pregnancy. Brittany’s blood type is B+ and she is GBS negative. Brittany weighs 190 pounds (86.1 kg) and has a pre-pregnancy BMI of 32.6. Brittany gets out of bed independently but lets the nurses or her significant other do most of the care for Mitchell. Her Foley catheter was removed 12 hours ago and she is voiding without difficulty. She is using hydrocodone bitartrate and acetaminophen (Norco) 5/325 mg and Ibuprofen 600 mg as needed for pain and states her pain is well controlled. Her significant other, Mark, is at the bedside and is helping care for Mitchell so Brittany can rest. Personal/Social History: Brittany and Mark have been together for four years and are planning to get married in six months. Mark is a loan officer at a local bank. Brittany is attending college and not working outside the home. She is worried about the extra expense of a new baby and is considering getting a job. Brittany’s family lives an hour away, and Mark’s family lives three hours away. Brittany has a history of depression and quit taking Sertraline when she became pregnant. What data from the histories are RELEVANT and must be interpreted as clinically significant by the nurse? (Reduction of Risk Potential) RELEVANT Data from Present Problem: Clinical Significance: RELEVANT Data from Social History: Clinical Significance: Patient Care Begins: What VS data are RELEVANT and must be interpreted as clinically significant by the nurse? (Reduction of Risk Potential/Health Promotion and Maintenance) RELEVANT VS Data: Clinical Significance: Current VS: P-Q-R-S-T Pain Assessment: T: 98.5 F/36.9 C (oral) Provoking/Palliative: Movement P: 74 (regular) Quality: Burning R: 16 (regular) Region/Radiation: Incisional BP: 110/60 Severity: 5/10 O2 sat: 98% room air Timing: Worsens with getting out of bed This study source was downloaded by 100000826504961 from CourseHero.com on 06-20-2022 06:51:57 GMT -05:00 https://www.coursehero.com/file/72531007/Metavee-Rynott-Post-Partum-Affective-Disorder-UNFOLDING-Reasoningpdf/Copyright © 2018 Keith Rischer, d/b/a KeithRN.com. All Rights reserved. What assessment data are RELEVANT and must be interpreted as clinically significant by the nurse? (Reduction of Risk Potential/Health Promotion and Maintenance) RELEVANT Assessment Data: Clinical Significance: Complete Blood Count (CBC) WBC HGB PLTs % Neuts Current: 14.1 10.6 302 70 On Admission: 9.8 11.9 358 58 What lab results are RELEVANT and must be interpreted as clinically significant by the nurse? (Reduction of Risk Potential/Physiologic Adaptation) RELEVANT Lab(s): Clinical Significance: TREND: Improve/Worsening/Stable: Current Assessment: GENERAL APPEARANCE: Calm and quiet appears tired. Baby in crib next to the bed RESP: Breath sounds clear with equal aeration bilaterally ant/post, nonlabored respiratory effort CARDIAC: Pink, warm & dry, heart sounds regular with no abnormal beats, pulses strong, equal with palpation at radial/pedal/post-tibial landmarks, brisk cap refill, 1+ pitting edema in lower extremities bilaterally NEURO: Alert and oriented to person, place, time, and situation (x4) INTEGUMENTARY: Low abdominal incision intact with surgical glue and open to air. No drainage noted. Skin slightly pink surrounding entire incision. No temperature change in skin and no edema surrounding incision. BUBBLEE BREAST: Lactating; soft, non-tender with evidence of colostrum UTERUS: Fundus firm 1 cm below umbilicus and midline BLADDER: Voiding without difficulty. Denies any burning with urination BOWELS: Abdomen soft/tender at incision, bowel sounds audible per auscultation in all four quadrants, positive flatus, no BM since delivery LOCHIA: Small amount of rubra, no clots noted EPISIOTOMY: Perineum intact EMOTIONAL: Quiet, appears fatigued, currently not interacting with baby, EPDS 8. This study source was downloaded by 100000826504961 from CourseHero.com on 06-20-2022 06:51:57 GMT -05:00 https://www.coursehero.com/file/72531007/Metavee-Rynott-Post-Partum-Affective-Disorder-UNFOLDING-Reasoningpdf/Copyright © 2018 Keith Rischer, d/b/a KeithRN.com. All Rights reserved. Education Priorities/Discharge Planning What educational/discharge priorities will be needed to develop a teaching plan for this patient and/or family? (Health Promotion and Maintenance) Education PRIORITY: PRIORITY Topics to Teach: Rationale: Two Weeks Later What assessment data are RELEVANT and must be interpreted as clinically significant by the nurse? (Reduction of Risk Potential/Health Promotion and Maintenance) RELEVANT Assessment Data: Clinical Significance: Brittany was discharged from the hospital after 48 hours of care with no complications. She is returning to her OB provider’s office for a routine two-week post-op checkup. You take her back to the exam room and get ready to see the doctor. You notice Brittany looks unkempt, her hair doesn’t look like it has been washed or brushed in a few days, she is not wearing any make up, she has dark circle under her eyes and appears very exhausted. You ask her how she is adjusting to motherhood and she becomes tearful. She states all she wants to do is sleep. You ask her if she has any help at home and she states her mother is staying with her and caring for Mitchell and doing all of the cooking and cleaning. You question her about her daily routine and she states she just sits on the couch or in her bed and stares at the television or sleeps. You ask her about her appetite and she states she isn’t very hungry and if she is, she can’t decide what to eat. She begins sobbing and states she feels like she is a horrible wife and mother. She knows she should be taking care of Mitchell, but she just doesn’t want to. You provide Brittany with the Edinburgh Postnatal Depression Scale and she completes it with a score of 15. You ask Brittany if you can call Mark and have him come to the office and she agrees, so you leave to go call him. You notify the provider of the results and he comes in to talk with Brittany. This study source was downloaded by 100000826504961 from CourseHero.com on 06-20-2022 06:51:57 GMT -05:00 https://www.coursehero.com/file/72531007/Metavee-Rynott-Post-Partum-Affective-Disorder-UNFOLDING-Reasoningpdf/Copyright © 2018 Keith Rischer, d/b/a KeithRN.com. All Rights reserved. Clinical Reasoning Begins 1. Interpreting relevant clinical data, what is the primary problem? What primary health-related concepts does this primary problem represent? (Management of Care/Physiologic Adaptation) Problem: Pathophysiology of Problem in OWN Words: Primary Concept: Collaborative Care: Medical Management (Pharmacologic and Parenteral Therapies) Care Provider Orders: Rationale: Expected Outcome: Sertraline 50 mg PO Daily Referral to Community Mental Health Clinic Provide contact information for postpartum depression support group Dietician referral Collaborative Care: Nursing 2. What nursing priority (ies) will guide your plan of care? (Management of Care) Nursing PRIORITY: PRIORITY Nursing Interventions: Rationale: Expected Outcome: This study source was downloaded by 100000826504961 from CourseHero.com on 06-20-2022 06:51:57 GMT -05:00 https://www.coursehero.com/file/72531007/Metavee-Rynott-Post-Partum-Affective-Disorder-UNFOLDING-Reasoningpdf/Copyright © 2018 Keith Rischer, d/b/a KeithRN.com. All Rights reserved. 3. What is the worst possible/most likely complication(s) to anticipate based on the primary problem of this patient? (Reduction of Risk Potential/Physiologic Adaptation) 4. What psychosocial/holistic care PRIORITIES need to be addressed for this patient? (Psychosocial Integrity/Basic Care and Comfort) Psychosocial PRIORITIES: PRIORITY Nursing Interventions: Rationale: Expected Outcome: CARE/COMFORT: Caring/compassion as a nurse Physical comfort measures EMOTIONAL (How to develop a therapeutic relationship): SPIRITUAL: Evaluation: Four Weeks Later Worst Possible/Most Likely Complication to Anticipate: Nursing Interventions to PREVENT this Complication: Assessments to Identify Problem EARLY: Nursing Interventions to Rescue: Four weeks later, Brittany, Mark, and Mitchell return for Brittany’s six-week check-up. Brittany is well-kempt and smiling. She is holding Mitchell and talking to him. You ask how she is feeling and she states she is feeling much better. Her mom went home five days ago, and Mark is back to work full-time. She is caring for Mitchell and even getting out of the house with Mitchell to run errands and found a new parenting support group she goes to each week. She states she continues to see her therapist at community mental health and still attends the postpartum depression support group. She states Mark has been so supportive and helping with the middle of the night feedings so she can sleep. She also states she has been taking Mitchell for walks each day and that seems to help her feel better. She is still taking her Sertraline every day. You provide Brittany with the Edinburgh Postnatal Depression Scale, and her score is a zero. This study source was downloaded by 100000826504961 from CourseHero.com on 06-20-2022 06:51:57 GMT -05:00 https://www.coursehero.com/file/72531007/Metavee-Rynott-Post-Partum-Affective-Disorder-UNFOLDING-Reasoningpdf/Copyright © 2018 Keith Rischer, d/b/a KeithRN.com. All Rights reserved. 1. What data is RELEVANT and must be interpreted as clinically significant by the nurse? (Reduction of Risk Potential/Health Promotion and Maintenance) RELEVANT Assessment Data: Clinical Significance: 2. Has the status improved or not as expected to this point? Does your nursing priority or plan of care need to be modified in any way after this evaluation assessment? (Management of Care, Physiological Adaptation) Evaluation of Current Status: Modifications to Current Plan of Care: 3. Based on your current evaluation, what are your CURRENT nursing priorities and plan of care? (Management of Care) CURRENT Nursing PRIORITY: PRIORITY Nursing Interventions: Rationale: Expected Outcome: This study source was downloaded by 100000826504961 from CourseHero.com on 06-20-2022 06:51:57 GMT -05:00 https://www.coursehero.com/file/72531007/Metavee-Rynott-Post-Partum-Affective-Disorder-UNFOLDING-Reasoningpdf/Copyright © 2018 Keith Rischer, d/b/a KeithRN.com. All Rights reserved. Caring and the “Art” of Nursing What is the patient likely experiencing/feeling right now in this situation? What can you do to engage yourself with this patient’s experience, and show that he/she matters to you as a person? (Psychosocial Integrity) What Patient is Experiencing: How to Engage: Use Reflection to THINK Like a Nurse Reflection-IN-action (Tanner, 2006) is the nurse’s ability to accurately interpret the patient’s response to an intervention at the moment as the events are unfolding to make a correct clinical judgment. What did I learn from this scenario? How can I use what has been learned from this scenario to improve patient care in the future? [Show More]
Last updated: 2 years ago
Preview 1 out of 8 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$14.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Nov 08, 2022
Number of pages
8
Written in
Additional information
This document has been written for:
Uploaded
Nov 08, 2022
Downloads
0
Views
80