*NURSING > SHADOW HEALTH > Breastfeeding Newborn RAPID Reasoning Amanda Stevens, 26 years old and baby Grace (All)
Breastfeeding Newborn RAPID Reasoning Amanda Stevens, 26 years old and baby Grace
Document Content and Description Below
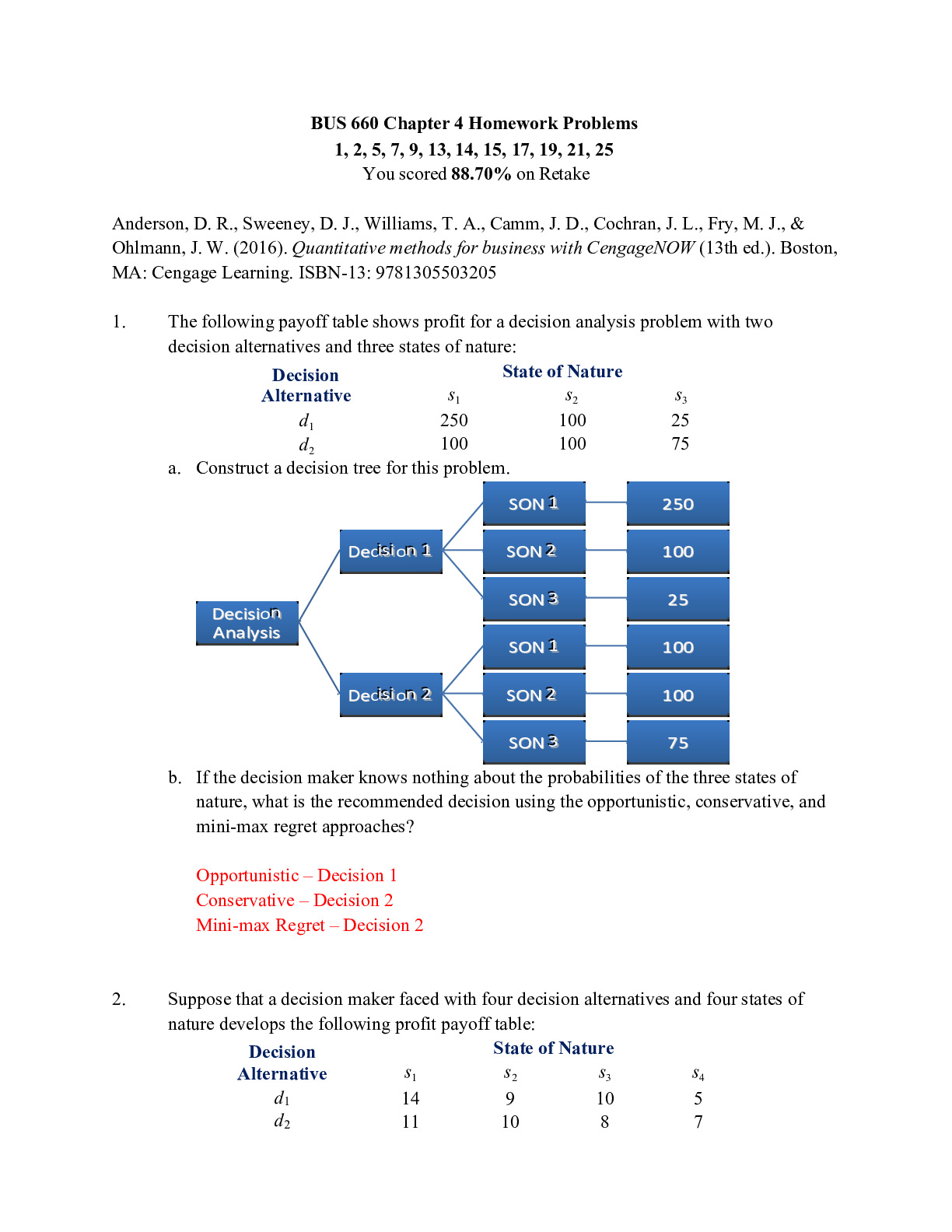
Breastfeeding Newborn RAPID Reasoning Amanda Stevens, 26 years old and baby Grace Copyright © 2018 Keith Rischer, d/b/a KeithRN.com. All Rights reserved. Breastfeeding Newborn RAPID Reasoning A... manda Stevens, 26 years old and baby Grace Primary Concept Reproduction Interrelated Concepts (In order of emphasis) • Pain • Patient Education • Clinical Judgment NCLEX Client Need Categories Percentage of Items from Each Category/Subcategory Covered in Case Study Safe and Effective Care Environment • Management of Care 17-23% ✓ • Safety and Infection Control 9-15% Health Promotion and Maintenance 6-12% ✓ Psychosocial Integrity 6-12% ✓ Physiological Integrity • Basic Care and Comfort 6-12% ✓ • Pharmacological and Parenteral Therapies 12-18% ✓ • Reduction of Risk Potential 9-15% ✓ • Physiological Adaptation 11-17% ✓History of Present Problem: Amanda Stevens is a 26-year-old female, G1 P1, accompanied by her husband, Brad. She presented to the maternity unit complaining of contractions every five minutes for the past three hours. She was dilated to 6 cm, 50% effaced, -2 station and admitted for labor. Brad was very supportive throughout her labor. She received an epidural for pain control and delivered by spontaneous vaginal delivery (SVD) a baby girl 12 hours later at 39 5/7 weeks gestation. Amanda’s blood type is A+ and is Group B strep (GBS) negative. Baby Grace was 7 pounds 8 ounces (3.4 kg), 20 inches (50.8 cm) long with APGARS of 9 at one minute and 9 at 5 minutes. Delayed cord clamping for one minute occurred and then she immediately went to breast and latched with minimal assist and nursed for ten minutes. Initial newborn assessment was completed with no abnormal findings. Her vital signs at birth were HR: 158, R: 54 T: 98.1 F/36.7 C axillary. Personal/Social History: Amanda and Brad have been married for two years and live 15 miles from the hospital in a small, rural community. Brad is a security guard at a prison located 30 miles from home and Amanda is a preschool teacher for the local preschool in her town. She will be taking eight weeks off from work before returning full time. Amanda’s parents live two hours away and will be coming tomorrow to stay with Amanda for a few days when she and the baby are discharged. Brad’s parents live out of state and will be coming to visit next month. Amanda’s sister lives an hour away and has a toddler and has offered to help Amanda if she needs it. Amanda and Brad just moved to their home six months ago and do not have many friends in the area. What data from the histories are RELEVANT and must be interpreted as clinically signifcant by the nurse? RELEVANT Data from Present Problem: Clinical Significance: 1. Immediately went to breast and latched for five minutes. 2. No abnormal findings of newborn at birth 1. This is a great sign! Patient may feel confident going forward, but this also may not be a full representation of breastfeeding moving forward. We would want to continue to encourage patient and be prepared to provide support. 2. There are no barriers to breastfeeding with the newborn thus far. RELEVANT Data from Social History: Clinical Significance: 1. Married for 2 years 2. Husband works 30 miles from home 3. Patient is taking off 8 weeks from work 4. Patient’s parents live two hours away – will be staying with patient for a few days after discharge. 5. Husband’s parents will come to visit next month 6. Patient’s sister offered to help if needed, but sister also has toddler 7. Do not have many friends in the area 1. This couple is new to marriage; they may still be settling into life as a married couple, adding extra strain. But they could also be still in the “honeymoon” phase. We have to be prepared to provide support regardless. 2. Once discharged, husband won’t be immediately available for help while he’s at work 3. The patient may desire to breastfeed for an extended period of time and this may make it difficult 4. The patient will have some support once discharged, even when husband is at work 5. There will be additional help 6. Sister has offered help. Sister may also have experience with breastfeeding and might be able to offer support 7. Once parents and in-laws go home, the patient doesn’t have much continuous supportPatient Care Begins One Hour After Delivery: What data from report is RELEVANT and must be interpreted as clinically signifcant by the nurse? RELEVANT REPORT DATA: CLINICAL SIGNIFICANCE 1. Grace has not breastfed well since the initial feeding after birth 2. Amanda is having difficulty getting Grace to latch. Grace will latch, suck a few times and then pulls off 3. Amanda is not able to express colostrum 4. Amanda is not asking for help and states that Grace must not be hungry 5. Grace has not voided since delivery and had one small meconium 1. There may be an anatomical issue or something preventing Grace from latching well or staying latched. Grace is not receiving nutrients or fluid. She is at risk for dehydration, weight loss, FTT 2. Baby is able to latch for a few sucks and then pulls off; this may be due to a physical limitation 3. Colostrum should be able to be expressed in the first 24 hours after birth 4. Amanda may be misinformed, embarrassed, frustrated feeling something else causing her to not want to ask for help. She may truly believe that the baby isn’t hungry, especially if Grace isn’t crying. 5. Grace should void for the frst time in the frst 24 hours. She passed a small meconium but should pass a full amount of stool within the frst 24 hours, and no later than 48 hours. Infants that are fed early pass stool sooner (Perry, Hockenberry, Lowdermilk, & Wilson, 2018, p. 536) Hockenberry, M. J., Olshansky, E. F., & Perry, S. E. (2018). Maternal child nursing care. St. Louis, MO: Elsevier. Current VS: Amanda P-Q-R-S-T Pain Assessment: T: 99.0 F/37.2 C Provoking/Palliative: When infant breastfeeds P: 78 (regular) Quality: Cramps R: 18 Region/Radiation: Abdominal BP: 110/68 Severity: 4/10 O2 sat: 98% on room air Timing: Constant cramping but worsens with breastfeeding You received shift report on Amanda and Grace and are about to go in and complete your morning assessments. The night nurse reported Grace has not breastfed well since the initial feeding after birth. Amanda has difficulty getting Grace to latch. Once she does latch, she only sucks a few times and pulls off. Amanda is not able to express any colostrum. She doesn’t ask for help with nursing and states that Grace must not be hungry. Grace has not voided since delivery and had one small meconium stool since birth.What VS data are RELEVANT and must be interpreted as clinically signifcant by the nurse? RELEVANT VS Data: Clinical Significance: 1. Cramping pain, 4/10 in abdomen, occurs when breastfeeding 1. This is a normal occurrence. Breastfeeding causes oxytocin to be released, resulting in contractions of the uterus. The cramping may cause breastfeeding to become aversive to the Amanda. Current VS: Baby Grace NIPS Pain Assessment: T: 98.0 F/36.7 C ax Facial Expression: Relaxed HR: 128 Cry: No cry R: 44 Breathing Pattern: Relaxed Legs: Relaxed State of Arousal: Alert NIPS Score: 0 RELEVANT VS DATA: CLINICAL SIGNIFICANCE: Vital signs/NIPS pain assessment are both normal There are no abnormal findings with the infant at this time Current Assessment: Amanda GENERAL APPEARANCE: Awake, states she didn’t sleep much last night. Holding baby Grace. RESP: Breath sounds clear with equal aeration bilaterally ant/post, nonlabored respiratory effort CARDIAC: Pink, warm & dry, heart sounds regular with no abnormal beats, pulses strong, brisk cap refill, 1+ bilateral pedal edema NEURO: Alert and oriented to person, place, time, and situation (x4) BUBBLE-HE BREAST: Soft, intact with no bruising. Nipples flat, no bleeding or open areas UTERUS: Firm, midline 2 cm below umbilicus BOWEL: Bowel sounds active x4, passing flatus, no BM since delivery BLADDER: Voiding without difficulty. Denies any burning with urination and able to empty bladder. LOCHIA: Moderate amount rubra, no clots noted EPISIOTOMY: Perineum intact, no episiotomy or laceration HOMANS: No signs of DVT, no pain, redness or edema in calves bilaterally EMOTIONAL: Appears fatigued, talking to baby, caresses baby’s head, positive bonding, EPDS 2 Current Assessment: Baby Grace GENERAL APPEARANCE In mom’s arms, awake, sucking on hands RESP: Breath sounds clear, resp. even and nonlabored CARDIAC: Pink with acrocyanosis, no edema, no murmurs noted, brisk cap refill NEURO: All reflexes intact GI Bowel sounds active. One small meconium since birth GU No void since birth What assessment data are RELEVANT and must be interpreted as clinically signifcant by the nurse?RELEVANT ASSESSMENT DATA: Amanda CLINICAL SIGNIFICANCE 1. States she didn’t sleep much last night 2. Holding baby grace 3. Uterus is firm, midline 2 cm below umbilicus 4. Appears fatigued but talking to baby 1. Lack of sleep can affect her ability or desire to bond and/or care for baby, but it appears as though she is bonding 2. Positive bonding 3. Appropriate for time after delivery 4. Lack of sleep can affect her. 5. She’s consistently bonding with her baby RELEVANT ASSESSMENT DATA: Grace CLINICAL SIGNIFICANCE 1. Grace is wide awake, sucking on hands 2. No void since birth 1. This is a great time to try to feed, since she’s awake. She is showing signs of being hungry by sucking on her hands. 2. She has not fed since immediately after birth; she should urinate for the first time in the first 24 hours Lab Results: Complete Blood Count (CBC:) Current: Admission High/Low/WNL? WBC (4.5–11.0 mm 3) 13.6 8.5 high Neutrophil % (42–72) 68 60 WNL Hgb (12–16 g/dL) 10.2 11.5 Low Platelets (150-450 x103/µl) 240 280 WNL What lab results are RELEVANT and must be interpreted as clinically signifcant by the nurse? RELEVANT Lab(s): Clinical Significance: WBC 13.6 Hgb 10.2 A high WBC count can indicate infection or stress on the body. In this case, it’s most likely elevated due to labor and delivery causing stress on the body. This is most likely due to the pregnancy and blood loss associated with deliveryWhat assessment data are RELEVANT and must be interpreted as clinically signifcant by the nurse? RELEVANT Assessment Data: Clinical Significance: TREND: Improve/Worsening/Stable: 1. Tried various breastfeeding positions with minimal success 2. Briefly latched to right breast but only sucked a few times, then would not latch again 3. Grace appears sleepy 4. Hand expressed several drops of colostrum onto a spoon and gave it to baby 5. Amanda states “I feel like such a bad mom. What am I doing wrong” 6. Grace fell back asleep 1. Grace may be too sleepy or there may be something else making it difficult for her to stay latched 2. This can happen when both mom and baby are learning to breastfeed 3. She may just be too sleepy to adequately latch and work for the milk 4. This method worked to get some of the colostrum into the baby. This also shows that Amanda is producing colostrum 5. She is becoming increasingly frustrated and discouraged because of the difficulty. She needs empathy and reassurance 6. Baby is still very sleepy 1. Same 2. Same 3. Same 4. Improving 5. Worsening 6. Same Over the past hour, you have assisted Amanda with breastfeeding and have tried various breastfeeding positions with minimal success. Grace did latch onto the right breast briefly but sucked only a few times and pulled herself off and would not latch again. Grace appears sleepy, which is common in the first 24 hours after birth. With your guidance, Amanda hand expressed several large drops of colostrum onto a spoon. This milk was given to the baby. Amanda is becoming very discouraged and states, “I feel like such a bad mom. What am I doing wrong?” You assure her she is doing everything correctly and it takes some babies a little longer to learn how to latch correctly. Grace is now sleeping so you encourage Amanda to let her sleep and will try to latch again later.Clinical Reasoning Begins… 1. Interpreting relevant clinical data, what is the primary problem? What primary health related concepts does this primary problem represent? (Management of Care/Physiologic Adaptation) Problem: Pathophysiology of Problem in OWN Words: Primary Concept: Patient is having a difficult time breastfeeding newborn due to newborn being too sleepy. This is causing mom to become increasingly frustrated/discouraged. It’s normal for the infant to be very sleepy in the first 24 hours after birth. Breastfeeding requires work on the infant’s part and this infant may just be too sleepy to properly latch, stay latched and feed. The initial feeding right after birth was in the time period when infants are very much alert. Reproduction: breastfeeding Collaborative Care: Medical Management (Pharmacologic and Parenteral Therapies) Care Provider Orders: Rationale: Expected Outcome: Encourage breastfeeding a minimum of 8 times in 24 hours. I and Os for Grace Lactation consultant referral Daily weight for Grace If Grace does not feed eight times in 24 hours, encourage breast pumping. This will maximize opportunity, increasing the chance of success. It will also provide for opportunities to practice. Need to make sure grace is getting enough and isn't becoming dehydrated a lactation consultant can help maximize breast feeding positions and technique ensure grace is gaining weight, indicating that feeding is going in the right direction any less than eight times in 24 hours is not adequate enough to keep grace hydrated and gaining weight appropriately With each opportunity, Amanda And grace will experience increasing success with breastfeeding Grace will have adequate intake and output Amanda will find success in breastfeeding through working with the lactation consultant Grace will continue to gain appropriate weight, indicating that she’s eating enough Grace will continue to gain weight and be hydrated Collaborative Care: Nursing 2. What nursing priority (ies) will guide your plan of care? (Management of Care) Nursing PRIORITY: Breastfeeding support PRIORITY Nursing Interventions: Rationale: Expected Outcome: Encourage breastfeeding a min of 8 times in 24 hours (Md orders) I/O for Grace (MD orders) Lactation consultant referral Daily weight for grace (md order) Encourage pumping if grace is not eating 8 times per 24 hours (md orders) Maximize times that Grace is awake – teach to lightly stimulate to keep awake so she doesn’t fall asleep at the breast Encourage fluids for Amanda See Above It’s important for Grace to be able to breastfeed, instead of falling asleep once latched Oral hydration will help with milk production and See above Grace will breastfeed for short periods of time without falling asleep at the breastEncourage rest for Amanda Provide resources for mom groups and breastfeeding support groups Offer support and guidance every time in the room with patient supply Getting enough rest will help mom to not feel so overwhelmed There are many support groups available that can really help moms; each mom has their own experience and may be able to resonate with Amanda. Letting the patient know the RN is there to help and empathizes can help the patient to feel heard and understood Amanda’s milk supply will be consistent Amanda won’t feel as overwhelmed Amanda will feel as though she has additional support, especially when she goes home The patient will feel heard and feel as though she can ask for help from the RN3. What body system(s) will you assess most thoroughly based on the primary/priority concern? (Reduction of Risk Potential/Physiologic Adaptation) PRIORITY Body System: PRIORITY Nursing Assessments: Amanda: Reproductive system Emotional state Grace: Urinary, GI, skin, fontanel, tears (or lack therof) Aman da: Lochia/vaginal discharge, fundus, breasts, milk supply Ability to cope, how she’s feeling about current situations Grace: I/O’s, wet diapers (weight), stool in diapers 4. What is the worst possible/most likely complication(s) to anticipate based on the primary problem of this patient? (Reduction of Risk Potential/Physiologic Adaptation) Worst Possible/Most Likely Complication to Anticipate: Grace begins to lose weight, doesn’t have adequate wet diapers and isn’t passing stool. Grace becomes dehydrated. Nursing Interventions to PREVENT this Complication: Assessments to Identify Problem EARLY: Nursing Interventions to Rescue: Lactation consultant referral; encourage BF 8x/24hr; encourage pumping if Grace is not feeding at least 8x/24hrs Mom reports still having difficulties feeding. Assess and identify a lack of wet diapers, lack of stool passed, skin turgor poor, sunken eyes, no tears when crying and sunken fontanelle Advise mom to pump milk and provide bottle. If unable to pump milk, offer donated milk or formula. If infant is still not latching properly, she may need feeding via NG tube in order to stabilize 5. What psychosocial/holistic care PRIORITIES need to be addressed for this patient? (Psychosocial Integrity/Basic Care and Comfort) Psychosocial PRIORITIES: Addressing anxiety and stress as a new mother PRIORITY Nursing Interventions: Rationale: Expected Outcome: CARE/COMFORT: Caring/compassion as a nurse Show empathy and allow Amanda to voice her concerns and frustrations. Let her know she’s not alone. Ask how she will feel helped the most and provide that help as best as possible. Physical comfort measures Provide Amanda with distraction options; try to help distract her from the anxiety she’s feeling (tv, talking to her friend while husband has baby, etc). Teach her how to deep breath, offer help with meditating, etc. The nurse is the primary and frontline source of support in the hospital setting; the patient needs to feel supported and understood, especially regarding anxiety as a new mother. New mothers feel many emotions, and they need to feel validated in those feelings without being judged. Anxiety can be emotionally taxing, but also physically exhausting. Providing Amanda with distraction options and ways to relieve the anxiety is imperative. The patient will feel heard, understood and better equipped as a new mom, leading to less feelings of anxiety. The patient will feel less physical repercussions of anxiety and feel more knowledgeable about how to relieve it. EMOTIONAL (How to develop a The nurse must establish rapport and trust in order The patient will be able to form atherapeutic relationship): Discuss the following principles needed as conditions essential for a therapeutic relationship: • Rapport • Trust • Respect • Genuineness • Empathy for the patient to want to talk about such intimate and personal things. This begins with mutual respect and showing that the nurse is capable of empathy and is absolutely genuine in his/her practice. With some patients, establishing this time of care can take more time, but it’s imperative to quality care, resulting in good patient outcomes. therapeutic relationship with the nurse, resulting in quality care.Grace breastfed for five minutes on the left breast 4 hours ago and just breastfed for three minutes on the right breast. The lactation consultant assisted with each feeding. Grace had one small void two hours ago and no meconium on your shift. Education Priorities/Discharge Planning What educational/discharge priorities will be needed to develop a teaching plan for this patient and/or family? (Health Promotion and Maintenance) Education PRIORITY: Breastfeeding techniques and principles & how to ensure baby is getting enough. Emotional wellbeing PRIORITY Topics to Teach: Rationale: 1. Breastfeeding holds 2. How to maximize supply 3. How to pump effectively 4. How to avoid mastitis and other complications r/t breastfeeding 5. What to look for in diaper amount/color/weight 6. Signs of dehydration in infant 7. Ideal times to try to breastfeed 8. Emotional health during breastfeeding and early days of being a new mother 1. Providing different options for holds during breastfeeding will allow the patient to find things that work for her and baby 2. Maximizing supply and making sure supply is wellestablished allows the patient to focus her attention on other things, especially since stress can affect the supply 3. Using the right pump and doing it effectively can help the supply rather than hurt it. It will also give the patient another option if the baby takes to bottles better. 4. Complications with breastfeeding can cause setbacks and increased anxiety regarding breastfeeding 5. This will empower parents to know that baby is hydrated 6. This will empower parents to be able to recognize if something is wrong 7. Maximizing on feeding times will help baby to feed appropriately and adequately 8. Emotional health is important for new moms, especially when this mom has already experienced anxiety related to breastfeeding and being a new mom Caring and the “Art” of Nursing What is the patient likely experiencing/feeling right now in this situation? What can you do to engage yourself with this patient’s experience, and show that he/she matters to you as a person? (Psychosocial Integrity) What Patient is Experiencing: How to Engage: The patient is probably feeling the following: 1. Tired from delivering a baby and not sleeping 2. Anxious due to baby not eating and being a new mom 3. Frustrated because breastfeeding is hard 4. Sad/disappointed Talk to the mother and ask her how she will feel helped. Ask openended questions about her expectations as a new mom and how it’s affecting her that the expectations haven’t been met. Giving her time to vent, cry, talk and ask questions can make a world of difference. And let her know that her feelings are valid.Use Reflection to THINK Like a Nurse Reflection-IN-action (Tanner, 2006) is the nurse’s ability to accurately interpret the patient’s response to an intervention at the moment as the events are unfolding to make a correct clinical judgment. What did I learn from this scenario? How can I use what has been learned from this scenario to improve patient care in the future? What did you learn: I learned that there was a lot about breastfeeding that I didn’t know! I learned that something as simple as the infant being tired can domino into many other “problems.” In this case, it caused concern for the infant’s health and well-being since she wasn’t eating, it caused the mom the doubt herself and, overall, it caused anxiety. I was prepared for something more significant to be wrong, but I learned that this IS significant! I learned a lot more about what to expect in the first 24 hours after birth as well; the amount of diapers and the amount of feeds was solidified for me. [Show More]
Last updated: 2 years ago
Preview 1 out of 12 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$14.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Nov 08, 2022
Number of pages
12
Written in
Additional information
This document has been written for:
Uploaded
Nov 08, 2022
Downloads
0
Views
100